Abstract
Introduction and importance
A two-step process involving ureteral stenting and surgical repair is generally recommended to manage a delayed diagnosis of postoperative ureteral injury; however, retrograde stenting is often difficult.
Case presentation
A 35-year-old female-to-male transgender person who underwent laparoscopic gender-affirming total hysterectomy with bilateral salpingo-oophorectomy developed right ureteral injury at 2 months postoperatively. Initially, the stenting guidewire could not pass through the stenotic tract and was diverted into the abdominal cavity. Using a 0.014-in. microguidewire and a 2-Fr microcatheter, both of which are designed for angiography, the ureteral stent was ultimately placed. The patient underwent surgical repair using the Boari flap technique. The double J catheter was removed at 1 month postoperatively, and postoperative retrograde pyelography revealed no urinary leakage or ureteral stricture.
Clinical discussion
Immediate primary repair is desirable for intraoperative ureteral injuries. However, up to 70 % of ureteral injuries are diagnosed during the postoperative period. For a delayed diagnosis of ureteral injury, urinary diversion with ureteral stent, nephrostomy, or both, followed by delayed repair, is recommended to avoid the inflammatory phase. In this patient, ureteral stenting was difficult on the first attempt. Thin microguidewires designed for angiography could be useful in such difficult situation.
Conclusion
A ureteral injury at the mid-ureter diagnosed at 2 months postoperatively was successfully managed using a two-step process involving ureteral stenting and surgical repair. A microguidewire and a microcatheter are useful for successful stenting in patients with late-diagnosed, severe ureteral strictures.
Keywords: Ureteral injury, Ureteral stenting, Surgical repair, Gynecological surgery, Iatrogenic, Case report
Highlights
-
•
The majority of iatrogenic ureteral injuries occur during gynecological procedures.
-
•
A two-step process is recommended for delayed-diagnosed ureteral injuries.
-
•
Thin microguidewires are beneficial in difficult retrograde ureteral stenting.
-
•
The Boari flap technique is useful for patients with long lower ureter deficits.
1. Introduction
Iatrogenic ureteral injury may occur in various settings, including pelvic surgery for colon or rectal cancer; vascular surgery, such as aortoiliac or aortofemoral bypass; and ureteroscopic procedures. Most ureteral injuries occur during gynecological procedures. Immediate repair should be attempted if an iatrogenic ureteral injury is observed intraoperatively; however, 50–70 % of ureteral injuries are diagnosed postoperatively and require a two-step process involving ureteral stenting and surgical repair. Retrograde stenting is often difficult in patients with a delayed diagnosis of ureteral injury, and antegrade stenting via a percutaneous nephrostomy is required.
In this report, the management of a ureteral injury that developed after a gender-affirming laparoscopic hysterectomy is presented. As the patient had received surgery in another country and diagnosed to have ureteral injury after returning to his country, details of the operation were unavailable, which made diagnosis and management complicated. As the patient did not develop hydronephrosis, a percutaneous nephrostomy could not be performed. Retrograde ureteral stenting was successfully performed using thin microguidewires typically used for angiography. The patient underwent surgical repair using the Boari flap technique. This case report has been reported in line with the SCARE Criteria [1].
2. Presentation of case
A 35-year-old Japanese female-to-male transgender person underwent laparoscopic gender-affirming total hysterectomy with bilateral salpingo-oophorectomy at a hospital in Thailand because this surgery could not be performed in Japan. The patient returned to Japan 3 days after surgery. He had been aware of abdominal discomfort since his return to Japan and developed ileus postoperatively that was treated conservatively. An abdominal computed tomography (CT) scan performed at 2 months postoperatively revealed massive intra-abdominal fluid. Ureteral injury was suspected, and the patient was referred to our hospital.
Except for the gender-affirming surgery, the patient had no medical history or drug use. The patient was afebrile. The serum creatinine and urea nitrogen levels were 1.03 mg/dL and 10 mg/dL, respectively. A CT scan at the delayed excretory phase revealed an outflow of contrast medium from the right ureter (Fig. 1A), leading to the diagnosis of right ureteral injury. On retrograde pyelography, the contrast medium flowed easily into the abdominal cavity, and the right proximal ureter was barely visible (Fig. 1B). Ureteral guidewires (0.035 and 0.025 in.) were inserted but entered the abdominal cavity and could not be advanced into the proximal ureter. As retrograde ureteral stenting was difficult, percutaneous nephrostomy was attempted; however, this also was difficult as the patient did not develop hydronephrosis. Therefore, retrograde stenting was attempted again. A 0.014-in. microguidewire was passed through the injured ureter (Fig. 2A) followed by a 2-Fr microcatheter. The microcatheter was replaced with a 4.7-Fr double J catheter at 10 days after the procedure and with a 6-Fr double J catheter at 2 months after the procedure. Retrograde pyelography conducted at 6 months after the procedure revealed no signs of urinary leakage, but severe ureteral strictures were noted (Fig. 2B).
Fig. 1.
Computed tomography and retrograde pyelography images at diagnosis of the right ureteral injury.
(A) A computed tomography image obtained during the delayed excretory phase reveals urinary leakage to the intraperitoneal space from the right ureter (orange arrow).
(B) A retrograde pyelography image reveals urinary leakage to the intraperitoneal space. The proximal ureter is also visualized (orange arrow).
Fig. 2.
Retrograde pyelography images at the successful stenting and at 9 months after the ureteral injury.
(A) A retrograde pyelography image shows the successful insertion of a 0.014-in. microguidewire.
(B) The retrograde pyelography image at 9 months after the ureteral injury shows severe ureteral stricture (orange arrow).
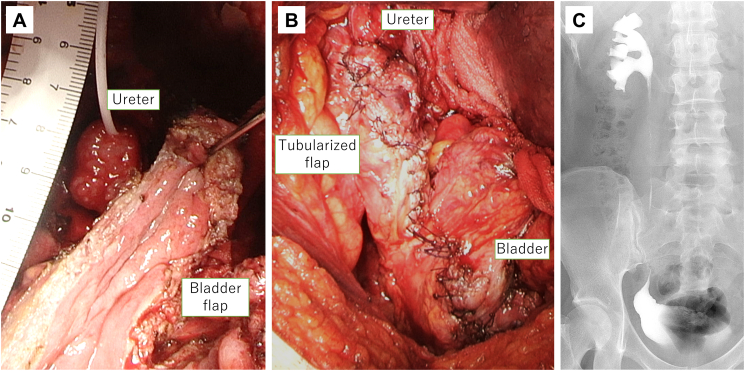
Surgical repair of the ureteral strictures was performed by a urologic surgeon (TK) with 20 years' experience at 9 months after the hysterectomy. As the lower ureter showed inflammatory changes and was not suitable for anastomosis, a ureterovesical anastomosis was conducted using the Boari flap technique. The right ureter was divided at the mid-ureter above the ureteral stricture, and the lower ureter was resected. The bladder was opened on its right anterior surface, and the bladder flap was mobilized cranially for anastomosis (Fig. 3A). Then, the tubularized bladder flap was anastomosed to the proximal right ureter (Fig. 3B). The patient's postoperative course was uneventful. The double J catheter was removed at 1 month postoperatively. The postoperative retrograde pyelography revealed no urinary leakage or ureteral stricture (Fig. 3C). The patient has been doing well without pain, urinary tract infection, or hydronephrosis for 1 year after surgical repair.
Fig. 3.
Intraoperative view of the Boari flap anastomosis and postoperative retrograde pyelography image.
(A) An intraoperative view prior to the Boari flap anastomosis shows the distal end of the right ureter and the bladder flap to be anastomosed.
(B) An intraoperative view after the Boari flap anastomosis shows the anastomosis of the right ureter to the tubularized bladder flap.
(C) A retrograde pyelography image obtained at 3 months postoperatively reveals no hydronephrosis or ureteral stricture.
3. Discussion
Immediate primary repair is desirable for intraoperative ureteral injuries. However, ureteral injury is detected intraoperatively in as few as 8.6 % of patients; up to 70 % of ureteral injuries are diagnosed in the postoperative period [2]. Early repair of ureteral injuries is controversial, though may be possible if the injury is discovered within the first 72 postoperative hours. After this period, urinary diversion with ureteral stent, nephrostomy, or both, followed by delayed repair is recommended with an interval of at least six weeks to avoid the inflammatory phase [3]. Furthermore, in some patients, the long-term placement of a ureteral stent may allow for complete healing of the ureteral injury and obviate the need for subsequent surgical repair. Cormio et al. [4] recommended conservative management with stenting for strictures <2 cm in length or for small fistulas, in which the continuity of the ureteric wall is preserved. However, ureteral stenting is difficult in recently diagnosed patients as the stent does not penetrate the stenotic tract and is diverted into the fistulous gap.
In this patient, ureteral injury was detected very late (at 2 months postoperatively), and ureteral stenting was difficult on the first attempt. Using a 0.014-in. microguidewire and 2-Fr microcatheter, both of which are designed for angiography, the ureteral stent was ultimately placed. Conservative management was continued with the expectation of spontaneous cure of ureteral injury by long-term stenting. However, unfortunately, severe ureteral stenosis remained; therefore, surgical repair was performed.
General principles when repairing the ureter include debridement, spatulation of the ureteral ends, watertight mucosa-to-mucosa anastomosis, the use of absorbable sutures, and isolation of the injury with the peritoneum or an omental patch [5]. The surgical repair methods for ureteral injuries depend on the severity and location of the trauma. For distal ureteral injuries, a Psoas hitch or Boari flap is recommended to bridge the deficit. For longer deficits, the Boari flap can be combined with a Psoas hitch, with a success rate of 81–87 % [6]. In the current patient, a Boari flap was successfully performed, achieving tension-free reimplantation of the right mid-ureter to the bladder with no complications.
As gender-affirming surgeries are not performed in every region, patients may visit other regions for surgery, in which case they may not receive sufficient postoperative follow-up. In our case, the patient underwent gender-affirming surgery in another country (Thailand) and developed a postoperative complication after returning to Japan, which delayed diagnosis of ureteral injury and made management more difficult. This report adds to existing literature on the successful treatment of late-diagnosed intraoperative ureteral injury with insufficient information of previous surgery.
4. Conclusion
A ureteral injury at the mid-ureter diagnosed at 2 months postoperatively was successfully managed using a two-step process involving ureteral stenting and surgical repair. A microguidewire and a microcatheter are useful for successful stenting in patients with late-diagnosed, severe ureteral strictures. The Boari flap technique is recommended for patients with long deficits of the lower ureter.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical approval
This study is exempt from ethical approval in our institution.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Guarantor
Toshiki Kijima MD.PhD.
Provenance and peer review
Not commissioned, externally peer-reviewed.
CRediT authorship contribution statement
Gaku Nakamura: Writing - Original Draft.
Akinori Nukui: Investigation.
Issei Suzuki: Investigation.
Kohei Takei: Investigation.
Toshiki Kijima: Conceptualization, Investigation, Writing - Review & Editing.
Takao Kamai: Supervision.
Declaration of competing interest
None.
Contributor Information
Gaku Nakamura, Email: ga3143ku@dokkyomed.ac.jp.
Akinori Nukui, Email: akinukui@tochigi-cc.jp.
Issei Suzuki, Email: i-suzuki@dokkyomed.ac.jp.
Kohei Takei, Email: takei-74@dokkyomed.ac.jp.
Toshiki Kijima, Email: tkijima@dokkyomed.ac.jp.
Takao Kamai, Email: kamait@dokkyomed.ac.jp.
References
- 1.Agha R.A., Franchi T., Sohrabi C., Mathew G. The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 2.Ostrzenski A., Radolinski B., Ostrzenska K.M. A review of laparoscopic ureteral injury in pelvic surgery. Obstet. Gynecol. Surv. 2003;58:794–799. doi: 10.1097/01.OGX.0000097781.79401.0B. [DOI] [PubMed] [Google Scholar]
- 3.Witters S., Cornelissen M., Vereecken R. Iatrogenic ureteral injury: aggressive or conservative treatment. Am. J. Obstet. Gynecol. 1986;155:582–584. doi: 10.1016/0002-9378(86)90283-8. [DOI] [PubMed] [Google Scholar]
- 4.Cormio L., Battaglia M., Traficante A., Selvaggi F.P. Endourological treatment of ureteric injuries. Br. J. Urol. 1993;72:165–168. doi: 10.1111/j.1464-410x.1993.tb00680.x. [DOI] [PubMed] [Google Scholar]
- 5.Smith A.P., Bazinet A., Liberman D. Iatrogenic ureteral injury after gynecological surgery. Can. Urol. Assoc. J. 2019;13:S51–S55. doi: 10.5489/cuaj.5936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wenske S., Olsson C.A., Benson M.C. Outcomes of distal ureteral reconstruction through reimplantation with psoas hitch, Boari flap, or ureteroneocystostomy for benign or malignant ureteral obstruction or injury. Urology. 2013;82:231–236. doi: 10.1016/j.urology.2013.02.046. [DOI] [PubMed] [Google Scholar]