Abstract
Introduction
Congenital diaphragmatic hernia (CDH) occurs in 1/2500 new-borns. Morgagni hernia (MH) is a very rare type of congenital diaphragmatic hernia found in the anterior aspect of the diaphragm between the costal and sternal portions of the muscle. It accounts for approximately 3 % of all diaphragmatic hernias. Most of these hernias are recognised and treated in childhood however, a very small portion present in adults.
Case presentation
We present a 30 year old female who presented with intestinal obstruction and was found to have a MH with strangulated ileum at operation. Strangulated ileum was resected, primary anastomosis done and suture repair of the defect done.
Conclusion
MH can present in adulthood and should be considered as a deferential diagnosis among patients presenting with mechanical intestinal obstruction with no obvious cause.
Abbreviations: CDH, congenital diaphragmatic hernia; MH, Morgagni hernia
Keywords: Strangulated, Morgagni, Hernia, Adult, Case-report
Highlights
-
•
Morgagni hernia can present as intestinal obstruction with strangulated ileum in an adult.
-
•
In resource limited settings with no CT scan and gastrografin, a high index of suspicion is necessary to make the diagnosis.
-
•
Suture repair may be sufficient in small defects.
1. Introduction
Congenital diaphragmatic hernia (CDH) is a very rare condition that is usually diagnosed at birth [1] or early childhood [2]. This hernia occurs due to failed proper formation of diaphragm during embryogenesis [1]. The intra-abdominal contents usually herniate into the Chest cavity resulting in different degrees of impaired lung development depending on the severity of the defect [2]. When the defect is not very severe to result in impaired lung development, at times the diagnosis is delayed and diagnosis can even be made in an elderly patient [3]. The frequency of late presentation has been reported to be between 0.17 and 6 % [1]. Patients may be asymptomatic or have mild to severe respiratory or gastrointestinal symptoms, and sometimes haemodynamic instability [1]. Posterolateral hernias (Bochdalek hernias) are the commonest type (>80 %) of congenital diaphragmatic hernia and are found on left in 85 %, than right (13 %) or bilateral (2 %) [1]. Morgagni hernia (MH) is a very rare type found in the anterior aspect of the diaphragm between the costal and sternal portions of the muscle [4].
MHs account for approximately 3 % of all diaphragmatic hernias [4]. Hernia contents include the omentum, colon, small bowel, stomach, and portions of the liver [4]. These contents may sometimes become ischemic, perforate, or cause intestinal obstruction [5], [6], [7]. Other contents may herniate through the defect like a ventriculo-peritoneal shunt that was reported to migrate through MH [8]. The treatment of MH is usually in early childhood and this can be open or laparoscopic [2], [9], [10], [11] and Robotic Surgery has also been used [6]. The surgery can be a tissue repair or a mesh repair [11]. Though recurrence is not common after repair, cases have been reported in which it occurred [1], [2], [4], [12], [13], [14], [15]. This draft is describing a rare case of an adult with MH with strangulated ileum, managed at a regional referral Hospital in a poor resource setting and has been reported in line with the SCARE criteria [16].
2. Case presentation
A 30 year old female presented with an 8 day history of moderate diffuse colicky abdominal pain associated with bilious vomiting, abdominal distension failure to pass stool and flatus with no history of fever. Patient had been managed for peptic ulcer disease in a district hospital, and referred with a diagnosis of suspected perforated peptic ulcer. Patient had no history of trauma or previous surgery.
On examination she was a middle-aged woman fully conscious afebrile with no pallor of mucus membranes, and BP = 130/70, PR = 98 bpm, RR = 30 cpm SPO2 = 93 % on room air.
Abdomen was distended, moving with respiration, with moderate tenderness in right hypochondria with no guarding or rebound tenderness. Patient also had a hyper-resonant percussion note and increased bowel sounds. The rectum was empty and rest of physical examination was unremarkable.
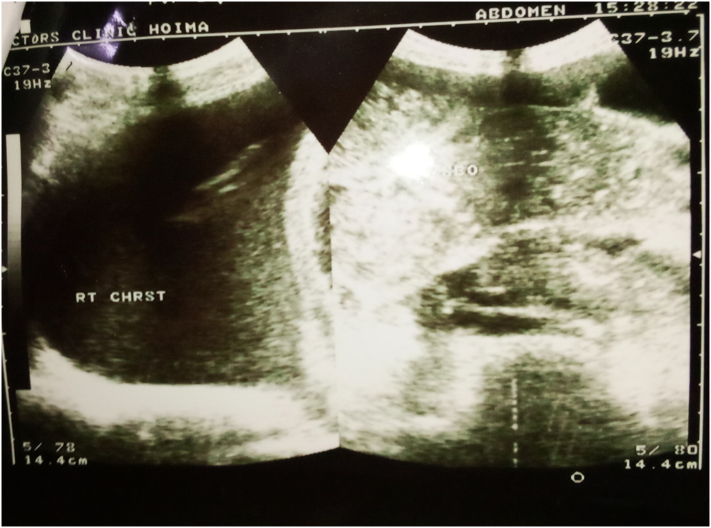
Ultrasound scan only revealed distended bowel loops and a pleural effusion on the right (Fig. 1). Chest and abdomen radiographs revealed distended bowel loops, air fluid levels and a right pleural effusion. An abnormal air lucency most likely a bowel loop was seen in the right lower lobe possibly representing hernia (Fig. 2). Preoperatively, a diagnosis of Intestinal obstruction was made, but the cause could not be ascertained. The presence of pleural effusion on ultrasound scan further confused the picture and the fact that there were no clear air-fluid levels in the hemothorax on chest Xray, made diagnosis by Xray difficult. A complete blood count revealed leucocytosis and left shift, but equipment for lactate levels were not available as was gastrografin and CT scan which could have made it possible to make a pre-operative diagnosis of diaphragmatic hernia.
Fig. 1.
An ultrasound scan image showing distended bowel loops and a pleural effusion on the right side of the chest.
Fig. 2.

Erect abdominal X-ray showing air-fluid levels and an abnormal air lucency on the right side of the chest.
Following pre-operative preparation, patient underwent an emergency laparotomy with a specialist general surgeon as the lead surgeon. At operation, a defect about 3 by 3 cm was found on the right diaphragm (Fig. 4) containing 50 cm of gangrenous ileum (Fig. 3) about 5 cm from the ileocecal junction with straw coloured fluid in the pleural cavity. Resection and Ileo-ascending double layer suture anastomosis was done. Primary suture repair of the defect was done using Nylon number one. A Chest tube was placed. Post operatively patient remained stable, antibiotics and analgesics were given in addition to ambulation and physiotherapy. She was discharged on the 5th post-operative day, and had no complaint during the follow up visits for a period of 12 months at Hoima Regional referral hospital.
Fig. 4.
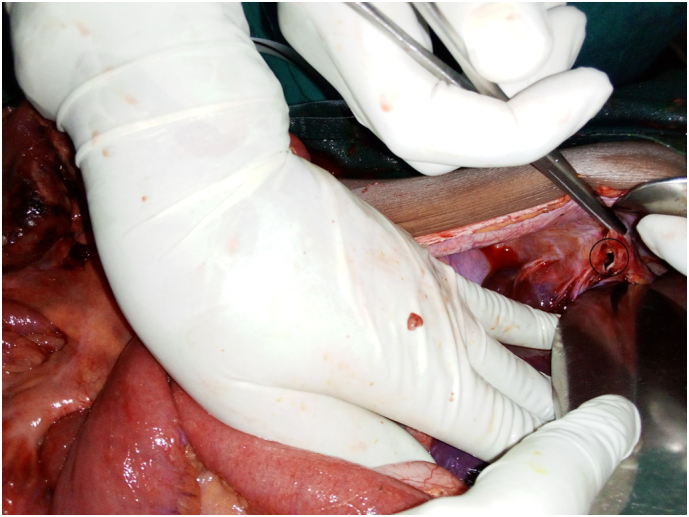
Intraoperative image showing a diaphragmatic defect (black circle).
Fig. 3.
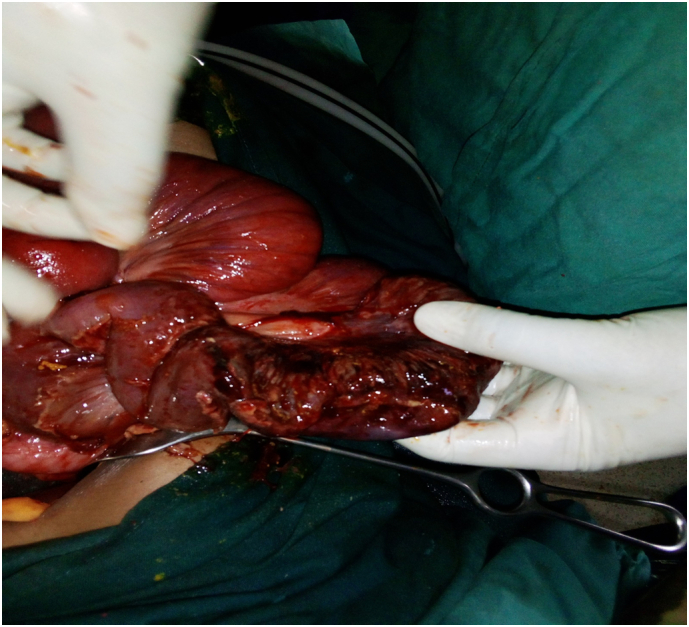
Intraoperative image showing gangrenous ileum.
3. Discussion
MH is a rare condition that arises from the defect of the septum transversum caused by the failure of closure of the pars sternalis with the seventh costochondral arch [4]. This type of hernia usually occurs on the right side as was seen in this patient, despite protection from the liver [4]. The content of the hernia is usually omentum in infants and children, but as they grow the defect becomes bigger and other abdominal organs can herniate through. In this patient only the ileum was found in the defect even though the size of the defect was relatively small. The enlargement of the defect may be facilitated by exercise and other types of exertion causing symptoms in a previously asymptomatic patient [12], and in this patient no history of exertion or unusual strenuous exercise was reported prior to the onset of symptoms.
Symptomatic patients usually complain of abdominal or chest pain and respiratory distress. Patients can present with an acute abdomen due to intestinal obstruction as was seen in this patient who presented with abdominal pain, vomiting and failure to pass stool or flatus, but this is a very rare occurrence in an MH [4]. Radiology can confirm the diagnosis usually by presence of a mass containing solid areas or fluid levels at the cardiophrenic angle in the retrosternal space when a lateral view is taken. However in the absence of bowel gas pattern as occurred in our patient, diagnosis is challenging since it becomes difficult to confirm that there is bowel in the chest [1]. CT scan is the gold standard as it demonstrates omental fatty tissue and intestinal air out of their localization, but in resource limited hospitals where CT scan is not available, contrast studies may be helpful if not contraindicated as was in our patient [4]. The plain X-ray was inconclusive in our patient and our patient would have benefited from a CT scan, but because our hospital does not have a CT scan, it was not done which possibly delayed diagnosis resulting in gangrene of the ileum. If exposure to radiation is a concern, then magnetic resonance imaging is a useful modality that can demonstrate fat density [12].
The definitive management for MH is Surgery, but since the prevalence of MH is not certain, operative and no operative management outcomes have not been compared [1]. For this reason the actual benefit of surgery is unknown [4]. Primary repair can be done thoracoscopically, laparoscopically, by open thoracotomy or Laparotomy, with thoracic approach providing easier dissection of the hernia sac off the mediastinal and pleural structures [12]. Laparotomy and laparoscopic approaches make reducing of hernia contents easier and offer chance for evaluating the contralateral diaphragm for additional defects, and concomitant evaluation and repair of other intra-abdominal pathology [4]. We did a laparotomy since even at operation we were not certain of the diagnosis and the only certain indication was Intestinal obstruction whose conventional approach is laparotomy. The fact that at operation the abdominal cavity was clean and the only obvious finding was distended bowel, it was difficult to identify the pathology till we decompressed and followed the ileum and noted that the cecum was retracted to the right upper quadrant and we were able to see the defect in the diaphragm. The loops of bowel in the Chest were carefully retracted back into the abdomen after extending the defect of the diaphragm and then resection and anastomosis was done and the defect repaired with a non-absorbable mono filament suture interrupted. Re-enforcement with biological mesh was not considered since the defect was small. But also biological mesh was not available in the hospital and synthetic mesh would increase risk of infection since there was gangrenous gut and resection had been done. Recurrence after surgery is rare and during our follow-up of the patient for one year following surgery, there were no features suggestive of recurrence.
In a hospital with poor medical support, where equipment for diagnosis like CT scan and gastrografin is not available, a high index of suspicion would help to have a chance of making the diagnosis of strangulated MH among patients presenting with features of intestinal obstruction plus chest symptoms. Concerning management, a non-absorbable suture repair may be sufficient, but if the defect is large, re-enforcement with biological mesh should be considered.
4. Conclusion
If a patient presents with respiratory distress and symptoms suggestive of gastrointestinal obstruction, MH should be included among the differential diagnosis. Following Surgery, recurrence is unlikely and outcome usually good, hence even in asymptomatic patients, surgery should be considered to prevent complications.
Consent
We obtained written informed consent from the patient for the publication of the case report and the images. A copy of the consent is available for review by the editor in chief of this journal on request.
Ethical approval
Not applicable.
Funding
This case report did not receive any specific grant from funding agencies in public, commercial, or not for profit sectors.
Author contribution
Joshua Muhumuza managed the patient and wrote the first draft. Denis Bitamazire supervisor in patient management, review and editing of the paper, Jethro Atumanyire involved in patient management, review and editing of the paper, ByaMungu Kagenderezo, Franck Katembo Sikakulya and Vivian Akelo review and editing of the paper.
Guarantor
Joshua Muhumuza.
Research registration
Not applicable.
Declaration of competing interest
None.
Acknowledgment
Dr. George Kalema, Sister Akusekera Yunia, Dr. Lawrence Kalute for their involvement in the care of the patient.
Provenance and peer review not commissioned, externally peer reviewed.
References
- 1.Testini M., Girardi A., Isernia R.M., et al. Emergency surgery due to diaphragmatic hernia: case series and review. World J. Emerg. Surg. 2017;12(1):1–18. doi: 10.1186/s13017-017-0134-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Journal I., Current OF. Bilateral L., et al. International journal of current medical and large bilateral morgagni hernia in adult patient with. 2021;7(04):5680–5683. [Google Scholar]
- 3.Aslam M., Husain S., Akami K., Ansari M.J., Ali S. A rare case of Morgagni hernia in an elderly female. ANZ J Surg. 2021 doi: 10.1111/ans.17010. Published online. [DOI] [PubMed] [Google Scholar]
- 4.Lee S.Y., Kwon J.N., Kim Y.S., Kim K.Y. Strangulated Morgagni hernia in an adult: synchronous prolapse of the liver and transverse colon. Ulus Travma ve Acil Cerrahi Derg. 2018;24(4):376–378. doi: 10.5505/tjtes.2017.99045. [DOI] [PubMed] [Google Scholar]
- 5.Chaudhary A., Ansari F.U., Ramole Y., et al. Obstructed right Morgagni hernia with multiple congenital anomalies : a rare presentation. 2020;7(12):4217–4220. [Google Scholar]
- 6.Cubas R., Garcia M., Mukherjee K. Robotic repair of incarcerated Morgagni hernia in an adult on the acute care. 2021;78(1):91–94. doi: 10.31053/1853.0605.v78.n1.28299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mitrovic M., Jankovic A., Kovac J.D., et al. 2021. Perforated appendicitis and bowel incarceration within Morgagni hernia: a case report. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lundy P.A., Partington M.D., Tuchek C.A., Garcia D.M. Intrathoracic migration of ventriculo-peritoneal shunt via Morgagni hernia. Childs Nerv. Syst. 2021;37(1):345–347. doi: 10.1007/s00381-020-04926-7. [DOI] [PubMed] [Google Scholar]
- 9.Altın Ö., Kaya S., Sarı R. Laparoscopic and single incision laparoscopic repair of Morgagni hernia in adults. Turk. J. Thorac. Cardiovasc. Surg. 2021;29(4):513–519. doi: 10.5606/tgkdc.dergisi.2021.20983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Debi R.A., Oflazoglu K., Schouten R., Smeets S.J.M. Laparoscopic repair of an incidental Morgagni hernia during Roux-En-Y gastric bypass in a severe obese adult : a case report. 2021;02(01):1–6. [Google Scholar]
- 11.Pacifico F., Russo M., Schettino M., Fontanella G., Biondo F.G., Mastella F. Laparoscopic prosthetic mesh repair of Morgagni hernia containing liver lobe. Clin Surg. 2020;5:4–6. doi:Clin Surg. 2020; 5: 2831. [Google Scholar]
- 12.Raza R., Shakil A., Khan D. Adult Morgagni’s hernia with intestinal obstruction and strangulation : the need for clinical awareness, early diagnosis and immediate surgical intervention. Open J Clin Med Case Reports is an Int. 2017:3. [Google Scholar]
- 13.Puligandla P.S., Skarsgard E.D., Offringa M., et al. Diagnosis and management of congenital diaphragmatic hernia: a clinical practice guideline. CMAJ. 2018;190(4):E103–E112. doi: 10.1503/cmaj.170206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Williams R. Congenital diaphragmatic hernia: a review. Hear Lung J. Acute Crit. Care. 1982;11(6):532–540. doi: 10.1186/s40748-017-0045-1. [DOI] [PubMed] [Google Scholar]
- 15.Shakil A. Adult Morgagni’s hernia with intestinal obstruction and strangulation: the need for clinical awareness, early diagnosis and immediate surgical intervention. Clinical & Medical. 2019;(January 2017):0–5. [Google Scholar]
- 16.Agha R., Franchi T., Sohrabi C., Mathew G., for the SCARE Group The SCARE 2020 guideline : updating consensus Surgical CAse REport (SCARE) guidelines. International Journal of Surgery. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]