Abstract
Introduction
Meckel's diverticulum is anatomically considered as a true diverticulum, with its embryological origins arising from a persistent omphalomesenteric duct. In adults, the disease is usually asymptomatic, often being accidentally diagnosed during imaging tests or surgery to treat other diseases, or due to further complications.
Presentation of the case
We report the case of a 26-year-old female patient was admitted to the emergency room complaining of pain and abdominal distension for 3 days, progressing to cessation of the elimination of gas for 1 day together with nausea and vomiting. Since the cause of the obstruction was not clearly identified, the patient's clinical status did not improve with non-operative measures and laparoscopy was not available, an exploratory laparotomy was conducted. In the cavity inventory, an approximately 20 cm wide MD was found in the terminal ileum adhered to the distal portion of the anterior abdominal wall.
Discussion
MD is the most common congenital anomaly of the gastrointestinal tract, with an estimated prevalence of between 0.3 % and 2.9 % in the general population. The clinical picture is usually asymptomatic, with the diagnosis made either via imaging tests performed to investigate other diseases, or during surgery to treat complications.
Conclusion
MD is the most common anomaly of the digestive tract, despite its low prevalence. It presents even rarer complications, including obstruction, digestive bleeding, or diverticulitis. It is important to consider the diverticulum as a diagnostic hypothesis in cases of obstruction without apparent causes, but it does not alter the initial management of the patient.
Keywords: Meckel diverticulum, Intestinal obstruction, Hernia, Case report
Highlights
-
•
MD is the most common anomaly of the digestive tract
-
•
In adults, the disease is usually asymptomatic.
-
•
Treatment depends on how the disease was diagnosed
1. Introduction
Meckel's diverticulum (MD) is anatomically considered as a true diverticulum, with its embryological origins arising from a persistent omphalomesenteric duct [1], [2]. It is the most common congenital anomaly of the digestive tract, more frequently seen in male children. It usually manifests with bleeding, obstruction, and inflammation (diverticulitis), and requires surgical treatment [3]. In adults, the disease is usually asymptomatic, often being accidentally diagnosed during imaging tests or surgery to treat other diseases, or due to further complications, with obstruction and diverticulitis being the most frequent symptoms in this age range [4].
Among the various diagnostic tests, ultrasonography, Computed Tomography (CT), Nuclear Magnetic Resonance, technetium-99 m scintigraphy and angiotomography are the most prominent. Ultrasonography is the usual choice for children, due to the good accuracy and absence of radiation, while CTs are more used in adults, and it is responsible for most diagnoses [5]. As for the management of MD, there are divergences between the literature and the authors, especially concerning cases of incidental findings of diverticula during surgeries for unrelated reasons. Some authors are in favor of resection in cases of intra-operative findings of MD during elective and non-severe surgeries, while others believe that the chances of complications are higher, opting for non-resection [6], [7]. There are also authors who have specific criteria to recommend resection based on the development of long-term complications. It is a consensus among studies that symptomatic cases, especially those resulting from aggravations such as inflammation, perforation, hemorrhage and obstruction, should be treated with a diverticulectomy or a small bowel segmental resection [1], [8]. This case follows 2020 SCARE guidelines for reporting cases in surgery [9].
2. Presentation of case
A 26-year-old female patient was admitted to the emergency room complaining of pain and abdominal distension for 3 days, progressing to cessation of the elimination of gas for 1 day together with nausea and vomiting. She denies having any allergies, associated comorbidities, or history of past surgeries. She presented stable vital signs with mild tachycardia (BP 132 × 95 mmHg, HR 109, Sat 97 %). Physical examination confirmed that the distended and tender abdomen, and diffuse peritonitis. Abdominal radiography demonstrated the presence of dilated bowel. To proceed with the investigation, a CT scan of the abdomen was taken, which confirmed the existence of dilation in multiple loops of the small intestine, without colonic dilatation or pneumoperitoneum, but with a mesentery torsion (Fig. 1). Since the cause of the obstruction was not clearly identified, the patient's clinical status did not improve with non-operative measures and laparoscopy was not available, an exploratory laparotomy was conducted.
Fig. 1.
Abdominal CT scan showing distension and mesentery torsion.
In the cavity inventory, an approximately 20 cm wide MD was found in the terminal ileum adhered to the distal portion of the anterior abdominal wall (Fig. 2), passing through intestinal loops into the internal hernia, in addition to the presence of stenosis of the ileum with approximately two centimeters at the origin of the diverticulum (Fig. 3, Fig. 4). It was decided to proceed with the lysis of adhesions, followed by segmental intestinal resection of the diverticulum and two-layer latero-lateral primary anastomosis using polypropilene in the terminal ileum. The cavity was washed, and after the plane suture the material was sent for histopathological analysis. The patient recovered well, stable, without further complaints for 7 days, and was discharged on the eighth postoperative day, after receiving antibiotic treatment. Histopathology was compatible with MD, with no signs of malignancy.
Fig. 2.
A Meckel's diverticulum adhered to the abdominal wall.
Fig. 3.
Product of enterectomy resection with Meckel's diverticulum.
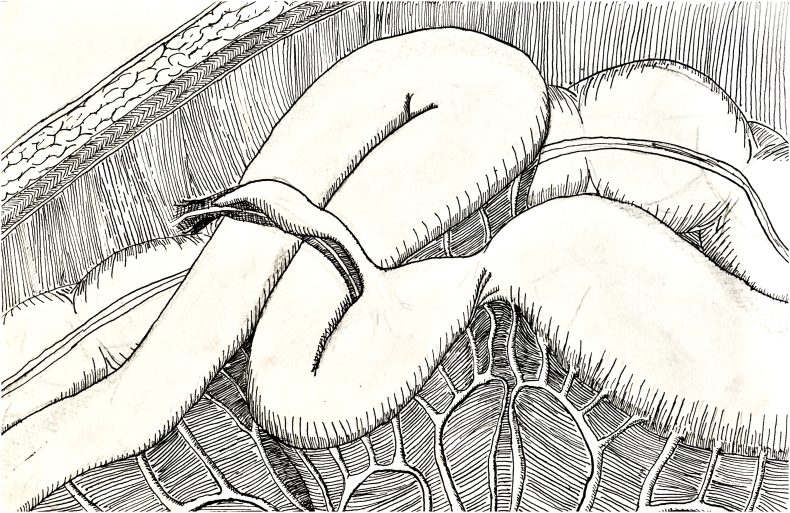
Fig. 4.
Schematics of intraoperative vision as well as the probable mechanisms of mechanical obstruction.
3. Discussion
MD is the most common congenital anomaly of the gastrointestinal tract, with an estimated prevalence of between 0.3 % and 2.9 % in the general population. It originates from the persistence of the vitelline duct and is a true diverticulum encompassing the 4 histological layers that make up the digestive tract: mucosa, submucosa, muscular and serous layer. It is located on the antimesenteric border of the ileum, usually between 7 and 200 cm from the ileocecal valve. MD is asymptomatic in most cases, manifesting in younger patients through complications, the main ones being obstruction, digestive hemorrhage, and inflammation [10], [11]. Tumoral processes within a diverticulum are rare, with the most common histological type being the carcinoid tumor; however, the presence of lipomas, leiomyosarcomas, mucoceles and leiomyomas have been reported in the literature. A study including 806 patients undergoing resection of asymptomatic diverticula observed the presence of a case with a metastatic adenocarcinoma [6].
The clinical picture is usually asymptomatic, with the diagnosis made either via imaging tests performed to investigate other diseases, or during surgery to treat complications related to the diverticulum and other pathologies. The risk of complication throughout life is from 4 to 6 %, with 40 % of them occurring in children under 10 years old [2], [4]. When present, the clinical manifestations are usually associated with worsening of the symptoms or further developments, and it is difficult to make a differential diagnosis between an aggravated MD and other diseases of the digestive system (intestinal obstruction and acute appendicitis, for example). In the pediatric age group, the most common complication is bleeding, accounting for 50 % of cases, followed by obstruction. While in the adult age group, the latter is the main complication, followed by inflammation resulting from the obstruction of the diverticular base. The mechanisms of intestinal obstruction related to Meckel's diverticulum are diverse: intussusception, volvulus, abdominal hernia, entrapment of the diverticulum in the mesentery, among others [2], [4].
According to anatomical and histological analyses, in 50 % of cases the diverticulum is formed by ectopic tissue, with the gastric mucosa being the most common and associated with cases of hemorrhage, inflammation as well as perforation. There are also reports on pancreatic tissue [3], [5]. The presence of these ectopic tissues strengthens the theory that justifies the etiopathogenesis related to MD aggravations. In the pediatric age group, especially under 10 years of age, there is an immaturity of the hormone axis related to acid secretion. This factor, associated with the knowledge that males produce a gastric secretion with a higher acid content, justifies the most prevalent complication in this group: hemorrhages, caused by diverticular mucosal injury [1], [4], [6].
Among the diagnostic tests, ultrasonography is the usual choice for children, due to its greater sensitivity and no use radiation. CT scans are used in adults, although in the absence of complications it does not always reveal the existence of the diverticulum [12]. This dilemma regarding visualization is caused by the similarity between the loops of the small intestine and the Meckel's diverticulum, along with the fact that the examination is often not performed specifically for the diverticulum. Routine magnetic resonance imaging also has a limited application in the incidental diagnosis for the same reasons. In specific situations, such as in cases of complications, the identification is facilitated. Access to the equipment coupled with the time needed to perform the exam makes this method inferior to the CT approach in such cases. Technetium-99 m scintigraphy is another more recent diagnostic modality of nuclear medicine, capable of identifying MD by its mechanism of action: locating ectopic gastric tissue [5], [12].
Intervention should be via laparoscopic surgery whenever possible [10]. In the case reported herein, video-surgery was not an option due to unavailability in the unit. The presence of the diverticulum is usually an incidental diagnosis, and its resection is debatable when asymptomatic [7], [11]. When complications arise, such as torsion, obstruction, volvulus or perforation, its removal is mandatory.
A literature review motivated authors to compile the main reasons that justify a resection of Meckel's diverticula found accidentally, based on factors that would increase the risk of future complications, such as patients 50 years old or younger, male, presence of a diverticulum greater than 2 cm wide, proof of the existing ectopic mucosa, narrow base aspect, and connection of the diverticulum with the umbilical scar through a connective tissue (relative indication). On the other hand, there are situations that discourage such intervention, including patients with advanced age, diffuse or local peritonitis, perforation of the appendix or intestinal loop, damage to other abdominal organs and patients who were victims of trauma in multiple organs [7], [8], [13].
The size of the diverticulum may be related to the possibility of torsion or adhesions, with an average size of 2.9 cm, and some larger with 12 cm [7]. In the case reported above, the diverticulum was greater than 20 cm, constituting one of the largest in the literature. It is important to mention that the initial management of the patient with intestinal obstruction is independent of the diagnosis since the problem will only be evidenced during surgery.
4. Conclusion
MD is the most common anomaly of the digestive tract, despite its low prevalence. It presents even rarer complications, including obstruction, digestive bleeding, or diverticulitis. MD tends to be asymptomatic in most cases, except in aggravated cases, which leads to incidental diagnosis during imaging exams or during surgical exploration due to other complications, one of which being the formation of adhesions and strictures in the small bowel. It is important to consider the diverticulum as a diagnostic hypothesis in cases of obstruction without apparent causes, but it does not alter the initial management of the patient.
Informed consent
Written informed consent was obtained from the patient's family for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Fundings
No fundings available.
Research registration
N/A
Guarantor
Edirany dos Santos Villalaz.
Provenance and peer review
Not commissioned, externally peer-reviewed.
CRediT authorship contribution statement
Edirany Villalaz, Juan Rodriguez and Zuriel Nunes contributions to conception, design, collected the patient details and wrote the paper. Edirany Villalaz, Thais Printes and César Façanha Neto made contributions to patient management. Valéria Bivaqua, Edirany Villalaz and César Façnha Neto critically revised the article. All authors read and approved the final manuscript.
Declaration of competing interest
This report does not present conflicts of interest by the authors.
References
- 1.Lequet J., Menahem B., Alves A., Fohlen A., Mulliri A. Meckel's diverticulum in the adult. J.Visc.Surg. 2017;154:253–259. doi: 10.1016/j.jviscsurg.2017.06.006. [DOI] [PubMed] [Google Scholar]
- 2.Lindeman R.J., Søreide K. The many faces of Meckel's diverticulum: update on management in incidental and symptomatic patients. Curr.Gastroenterol.Rep. 2020;22 doi: 10.1007/s11894-019-0742-1. [DOI] [PubMed] [Google Scholar]
- 3.Tartaglia D., Cremonini C., Strambi S., Ginesini M., Biloslavo A., Paiano L., Quilici F., Castagna M., di Saverio S., Coccolini F., Chiarugi M. Incidentally discovered Meckel's diverticulum: should I stay or should I go? ANZ J. Surg. 2020;90:1694–1699. doi: 10.1111/ans.16189. [DOI] [PubMed] [Google Scholar]
- 4.Kuru S., Kismet K. Meckel's diverticulum: clinical features, diagnosis and management. Rev.Esp.Enferm.Dig. 2018;110:726–732. doi: 10.17235/reed.2018.5628/2018. [DOI] [PubMed] [Google Scholar]
- 5.Chatterjee A., Harmath C., Vendrami C.L., Hammond N.A., Mittal P., Salem R., Miller F.H. Reminiscing on remnants: imaging of Meckel diverticulum and its complications in adults. Am. J. Roentgenol. 2017;209:W287–W296. doi: 10.2214/AJR.17.18088. [DOI] [PubMed] [Google Scholar]
- 6.Blouhos K., Boulas K.A., Tsalis K., Barettas N., Paraskeva A., Kariotis I., Keskinis C., Hatzigeorgiadis A. Meckel's diverticulum in adults: surgical concerns. Front.Surg. 2018;5 doi: 10.3389/fsurg.2018.00055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rahmat S., Sangle P., Sandhu O., Aftab Z., Khan S. Does an incidental Meckel's diverticulum warrant resection? Cureus. 2020 doi: 10.7759/cureus.10307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zyluk A. Proceeding with incidentally discovered, unchanged Meckel's diverticulum - a review. <sb:contribution><sb:title><sb:maintitle>Polish</sb:maintitle></sb:title></sb:contribution><sb:host><sb:issue><sb:series><sb:title>J. Surg.</sb:title></sb:series></sb:issue></sb:host>. 2019;91:1–5. doi: 10.5604/01.3001.0013.3400. [DOI] [Google Scholar]
- 9.Agha R.A., Franchi T., Sohrabi C., Mathew G., Kerwan A., Thoma A., Beamish A.J., Noureldin A., Rao A., Vasudevan B., Challacombe B., Perakath B., Kirshtein B., Ekser B., Pramesh C.S., Laskin D.M., Machado-Aranda D., Miguel D., Pagano D., Millham F.H., Roy G., Kadioglu H., Nixon I.J., Mukhejree I., McCaul J.A., Ngu J.Chi-Yong, Albrecht J., Rivas J.G., Raveendran K., Derbyshire L., Ather M.H., Thorat M.A., Valmasoni M., Bashashati M., Chalkoo M., Teo N.Z., Raison N., Muensterer O.J., Bradley P.J., Goel P., Pai P.S., Afifi R.Y., Rosin R.D., Coppola R., Klappenbach R., Wynn R., de Wilde R.L., Surani S., Giordano S., Massarut S., Raja S.G., Basu S., Enam S.A., Manning T.G., Cross T., Karanth V.K., Kasivisvanathan V., Mei Z. de WildeS.SuraniS.GiordanoS.MassarutS.G.RajaS.BasuS.A.EnamT.G.ManningT.CrossV.K.KaranthV.KasivisvanathanZ.Mei, The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 10.Hansen C.C., Søreide K. Systematic review of epidemiology, presentation, and management of Meckel's diverticulum in the 21st century. Medicine. 2018;97 doi: 10.1097/MD.0000000000012154. (United States) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mora-Guzmán I., Muñoz de Nova J.L., Martín-Pérez E. Meckel's diverticulum in the adult: surgical treatment. Acta Chir. Belg. 2019;119:277–281. doi: 10.1080/00015458.2018.1503391. [DOI] [PubMed] [Google Scholar]
- 12.Choi S.Y., Hong S.S., Park H.J., Lee H.K., Shin H.C., Choi G.C. The many faces of Meckel's diverticulum and its complications. <sb:contribution><sb:title><sb:maintitle>J. Med. Imaging Radiat.</sb:maintitle></sb:title></sb:contribution><sb:host><sb:issue><sb:series><sb:title>Oncol.</sb:title></sb:series></sb:issue></sb:host>. 2017;61:225–231. doi: 10.1111/1754-9485.12505. [DOI] [PubMed] [Google Scholar]
- 13.Maia D.S., Ferreira-Júnior M., Viegas R.G., Silva E.E.C., de T.V. de Oliveira P., da Silva R.C.A., Caetano A.J., Ferreira N.G. Obstrução intestinal por divertículo de Meckel. Arq. Bras. Cir. Dig. 2013;26:244–245. doi: 10.1590/S0102-67202013000300018. (São Paulo) [DOI] [PubMed] [Google Scholar]