Abstract
Background
Levels of maternal and neonatal mortality remain high in sub-Saharan Africa, with an estimated 66% of global maternal deaths occurring in this region. Many deaths are linked to poor quality of care, which in turn has been linked to gaps in pre-service training programmes for midwifery care providers. In-service training packages have been developed and implemented across sub-Saharan Africa in an attempt to overcome the shortfalls in pre-service training. This scoping review has aimed to summarize in-service training materials used in sub-Saharan Africa for midwifery care providers between 2000 and 2020 and mapped their content to the International Confederation of Midwives (ICM) Essential Competencies for Midwifery Practice.
Methods
Searches were conducted for the years 2000–2020 in Cumulative Index of Nursing and Allied Health Literature, PubMed/MEDLINE, Social Science Citation Index, African Index Medicus and Google Scholar. A manual search of reference lists from identified studies and a search of grey literature from international organizations was also performed. Identified in-service training materials that were accessible freely on-line were mapped to the ICM Essential Competencies for midwifery practice.
Results
The database searches identified 1884 articles after removing duplicates. After applying exclusion criteria, 87 articles were identified for data extraction. During data extraction, a further 66 articles were excluded, leaving 21 articles to be included in the review. From these 21 articles, six different training materials were identified. The grey literature yielded 35 training materials, bringing the total number of in-service training materials that were reviewed to 41. Identified in-service training materials mainly focused on emergency obstetric care in a limited number of sub-Saharan Africa countries. Results also indicate that a significant number of in-service training materials are not readily and/or freely accessible. However, the content of in-service training materials largely met the ICM Essential Competencies, with gaps noted in the aspect of woman-centred care and shared decision making.
Conclusion
To reduce maternal and newborn morbidity and mortality midwifery care providers should have access to evidence-based in-service training materials that include antenatal care and routine intrapartum care, and places women at the centre of their care as shared decision makers.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12909-022-03772-2.
Keywords: Midwifery, Competence, In-service training, Education, Sub-Saharan Africa
Background
Despite the target set out by the Sustainable Development Goals (SDG) “to reduce the global maternal mortality ratio (MMR) to less than 70 per 100,000 livebirths by 2030” (SDG 3.1) [1], the global MMR in 2017 was estimated to be 211 per 100,000 livebirths. Of these deaths, 66% were estimated to take place in sub-Saharan Africa, where the estimated regional MMR was 542 in 2017 [2]. Similarly, with a neonatal mortality rate of 27 per 1,000 [3], the sub-Saharan Africa region lags behind the SDG target to reduce neonatal mortality rate to at least as low as 12 per 1,000 livebirths (SDG 3.2) [4]. With access to evidence-based, quality care the majority of these deaths are preventable [5]. Midwifery care, within an enabling environment has the ability to improve quality of care [6, 7]. However, despite a rise in the numbers of women giving birth with skilled health personnel [8], reductions in mortality rates have not fallen proportionately [9]. This may be explained by system deficiencies that influence the provision of high-quality maternity care including a lack of appropriately trained and qualified midwifery care providers.
Pre-service training courses that prepare midwifery care providers for the workforce differ substantially in their length, content and quality [10, 11]. This impacts on the ability of midwifery care providers to perform obstetric and neonatal services [12, 13] and reduces their competence and confidence levels [14]. A form of continuous professional development, in-service training acts to provide updates as new evidence for practice develops, as well as overcome the shortfalls of pre-service training and thereby has the potential to improve quality of care. In sub-Saharan Africa, a number of in-service training packages have been developed and implemented to strengthen the quality of maternity care services [15–17] These have predominantly focused on emergency obstetric care [15–18] with a much smaller number focusing on physiological childbirth [19] and respectful care [20]. In-service training on routine antenatal, intrapartum and postnatal care is basic and vital for positive health outcomes. Midwifery care providers who are trained are competent to identify potential complications and treat them before they develop into more serious and potentially life-threatening complications. To be effective, in-service training materials need to be evidence-based, incorporate up to date local guidelines, and promote autonomy, focusing on multidisciplinary team approaches and woman-centred care. Time needs to be made for midwifery care providers to undertake training to ensure that they can provide evidence based quality of care. The modus in which in-service training is delivered should also be considered as this may influence the impact the training has on care provision in both the short and long term [21].
The International Confederation of Midwives (ICM) “Essential Competencies for Midwifery Practice” outline the minimum set of knowledge, skills and professional behaviour expected of an individual completing their midwifery training when joining the workforce. The ICM Essential Competencies Framework is organised into four inter-related categories; (1) general competencies, (2) pre-pregnancy and antenatal, (3) care during labour and birth and (4) ongoing care for women and newborns. Within each of these, knowledge and skills/behaviour are defined [22]. This Framework is a useful tool in the evaluation and design of previously used, current and future in-service training materials for midwifery care providers.
This scoping review was conducted as part of the Action Leveraging Evidence to Reduce perinatal morTality and morbidity in sub-Saharan Africa (ALERT) project (Trial registration number: PACTR202006793783148) [23]. The objective of the ALERT project is to develop and evaluate a multifaceted intervention to (i) strengthen the implementation of evidence-based interventions and responsive care and, (ii) reduce in-facility perinatal mortality and morbidity through a multidisciplinary approach in Benin, Malawi, Tanzania and Uganda. To achieve this, the ALERT project aims to develop and implement a co-designed in-service midwifery training package with a focus on routine intrapartum care. To inform this process this review has identified in-service training materials for midwifery care providers that will be considered when developing the in-service training packages.
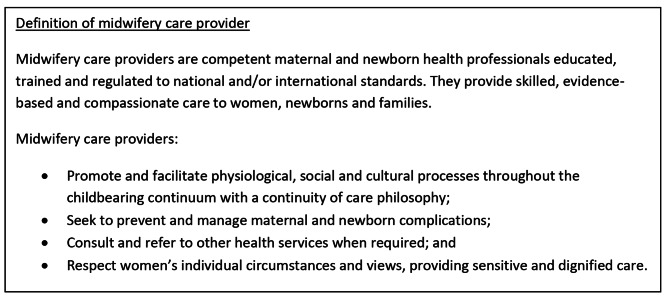
In this review we have used the term “midwifery care provider” which is defined in box 1.
Box 1.
Definition of midwifery care provider (based on Renfrew et al. 2014, WHO 2018 [24, 25])
Methods
Study design
The study protocol was published in the BMJ Open in 2021 [26] and outlines the methodology for the design and conduct of the scoping review. Arksey and O’Malley’s [27] scoping review framework was applied in line with the five stages (i) identifying the research question; (ii) identifying relevant studies; (iii) selecting studies; (iv) charting the data; and (v) collating summarizing and reporting the results. This scoping review was conducted to identify in-service training materials used for midwifery care providers in sub-Saharan Africa between 2000 and 2020. It was conducted according to the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) Checklist (http://www.prisma-statement.org/Extensions/ScopingReviews), which is outlined in Additional file 1.
Stage 1: identifying the research question
All authors discussed and agreed on the research questions. The aim of the scoping review was to summarize existing in-service training materials used in sub-Saharan Africa between 2000 and 2020, and map their content to the ICM Essential Competencies for Midwifery Practice [22] (ICM 2019). Our review posed the following questions:
What in-service training materials are available, freely accessible and have been used for midwifery care providers in sub-Saharan Africa from 2000 to 2020?
How does the content of these in-service training materials align with the ICM Essential Competencies for Midwifery Practice?
The review sought to include only in-service training materials that are freely available to midwifery care providers. We acknowledge that there are other sponsored and freely available training materials for midwifery care providers. Access to these however, is inequitable as they are only free to those midwifery care providers working in health care facilities where such sponsored training is implemented.
The study protocol outlined that in-service training materials would also be mapped to the Quality Maternal and Newborn Care framework [24]. However, it was noted that the five components of the framework were too general and following further consideration, the decision was made to map the training materials to the ICM Essential Competencies only.
Stage 2: identifying relevant studies
Inclusion criteria
The research questions were assessed, and studies selected specific to the following Population, Concept, Study Design and Context criteria presented in Table 1. All studies and grey literature that included information on available in-service training materials used for midwifery care providers in sub-Saharan Africa were included for review. As the focus of the scoping review was on training materials based on evidence, only those developed and used after 2000 onwards were included as evidence of clinical care changes constantly and new guidelines and recommendations are updated to ensure best practice.
Table 1.
Inclusion criteria for identifying eligible studies
| Inclusion Criteria | |
|---|---|
| Population | Any in-service training on midwifery care aimed at any health professional who provides midwifery care. |
| Concept | Mapping the content of in-service training materials used for providers of midwifery care to the ICM Essential Competencies. |
| Study Design | Studies and reports/documents that report on the implementation of in-service training materials and in-service training resources identified through searches of grey literature. |
| Context | In-service training in sub-Saharan Africa. |
Exclusion criteria
Articles were excluded from the scoping review if:
The country in which the in-service training took place was not located within sub-Saharan Africa.
The health personnel who had undertaken the in-service training were not considered to be midwifery care providers.
The content of the in-service training did not relate to the provision of midwifery care.
The in-service education and training materials were created before 2000.
There were no details provided on the content of the training sessions.
The content of the in-service training materials was not freely available online.
Search strategy
The search strategy was conducted for all relevant existing literature, without language restrictions, based on search terms relating to the research questions and restricted to the years 2000–2020 using the following online bibliographic databases: Cumulative Index of Nursing and Allied Health Literature, PubMed/MEDLINE, Social Science Citation Index, African Index Medicus, and Google Scholar. Additional file 2 contains terms used for searches of the electronic databases. The search in Google Scholar generated 6,350 results. The authors reviewed the first 150 titles returned by Google Scholar as relevance diminished after this stage.
Grey literature searches were performed and included organizations known to be active in global maternal and newborn health improvement (i.e., United Nations Population Fund (UNFPA), World Health Organization (WHO), Johns Hopkins Program for International Education in Gynecology and Obstetrics (JHPIEGO), International Confederation of Midwives (ICM), International Federation of Gynecology and Obstetrics (FIGO), International Pediatric Association (IPA). The reference list of all eligible studies was hand-searched to identify any additional relevant studies.
Stage 3: study selection
Following the searches outlined above, the citations were imported into Covidence (https://www.covidence.org), an online tool developed to support the screening and data extraction processes. The imported citations underwent independent title and abstract screening by two reviewers (A-BM and JW). Screened abstracts identified for inclusion had their full texts independently reviewed by two reviewers (A-BM and JW). Two identified full-texts were written in French and were screened by A-BM. Reasons for exclusion of full texts were documented. See additional file 3 which shows the PRISMA flow diagram charting this process.
Stage 4 and 5: charting the data and collating, summarizing and reporting the results
A pre-designed data extraction tool in Microsoft Excel was used to extract data from included studies. Information retrieved included study characteristics (country, year of study and setting). Data collected pertaining to in-service training and educational area of focus, those trained, as well as details related to the design of the in-service training (formal education sessions, training facilitators, on-site training, off-site training, use of simulation, ongoing mentorship, online training), as well as details of identifiable in-service training materials.
JW and HH mapped the training materials to the ICM Competencies, and a third reviewer A-BM randomly checked 20% of the mapped training materials to ensure agreement. To map the content of the in-service training materials to the ICM Essential Competencies for Midwifery Practice, the educational area of focus of the in-service training materials was identified, and content mapped to the corresponding pertinent categories and indicators within the ICM Competencies [22]. Presenting our results using descriptive statistics, as outlined in our protocol paper, was therefore not appropriate, as comparisons between tools would be meaningless. Results are therefore presented using narrative description based on themes arising.
Results
Literature search.
The search of electronic databases yielded 2009 articles. Removal of 125 duplicates left 1884 articles whose titles and abstracts were screened independently by two reviewers. A total of 170 articles were selected for full text review. The full text review led to a further 83 articles being excluded. The most common reason for exclusion was “not in-service training” meaning the study did not report on in-service training. See the PRISMA diagram in additional file 3 for full details of the reasons for exclusions. A further 66 articles were excluded during the data extraction phase as the in-service training materials were not identifiable and/or were not freely available. Corresponding authors were contacted in cases where the materials could not be located. Of those that responded the following responses were given; authors no longer had access to the training materials and advised us to contact the organization who had developed the training materials. This organization was contacted but did not respond; some authors could not share the training materials as they are not freely available to the public; and one author was able to share a scanned copy of the first few pages of the training materials. Following a search, we were able to obtain a soft copy of the training materials from a colleague working in the low-and-middle-income country where the materials had been developed. However, as these materials were not freely available online, we did not include them in the review.
Websites of organizations known to be active in maternal and newborn global health improvement (i.e., UNFPA, WHO, JHPIEGO, ICM, FIGO, IPA) were searched. This process identified a further 44 in-service training materials. However, during the mapping phase, nine of these were excluded. In one third of these cases, the reason for exclusion was difficulty in accessing the training materials online. Where possible, the appropriate organizations were contacted and asked for support to obtain, but no responses were received.
Study characteristics
Details of the studies [28–48] included in the review are provided in Table 2. Included studies were concentrated in eight countries, Ethiopia, Ghana, Kenya, Malawi, Mali, Sudan, Tanzania and Uganda with one third of the studies reporting on in-service training in Tanzania. Two studies reported on the implementation of in-service training across multiple countries (including India, Kenya, Malawi and Tanzania).
Table 2.
Included articles
| Author(s) | Title | Publication Year | Country | Participants | Setting | Topic | Identified Training Material |
|---|---|---|---|---|---|---|---|
| Yigzaw et al. [28] | Comparing the effectiveness of a blended learning approach with a conventional learning approach for basic emergency obstetric and newborn care training in Ethiopia. | 2019 | Ethiopia | Midwives, nurses, health officers | Health centres. | BEmONC | Federal Democratic Republic of Ethiopia Ministry of Health: Basic Emergency Obstetric and Newborn Care |
| Weinberg et al. [29] | Helping Babies Survive Training Programs: Evaluating a Teaching Cascade in Ethiopia. | 2019 | Ethiopia | Midwives, nurses, house officers | Urban and rural. Hospitals. | Neonatal Resuscitation and Neonatal Care | American Academy of Pediatrics: Helping Babies Breathe, Essential Care for Every Baby, Essential Care for Small Babies |
| Thomsen et al. [30] | Health workers’ experiences with the Safe Delivery App in West Wollega Zone, Ethiopia: a qualitative study. | 2019 | Ethiopia | Nurses, midwives, health extension workers | Urban and rural. Health centres and hospitals. | BEmONC, EmONC, Neonatal Resuscitation | Safe Delivery App |
| Lund et al. [31] | Association Between the Safe Delivery App and Quality of Care and Perinatal Survival in Ethiopia: A Randomized Clinical Trial. | 2016 | Ethiopia | Nurse, midwives, health extension workers | Urban and rural. Health centres and hospitals. | BEmONC, EmONC, Neonatal Resuscitation | Safe Delivery App |
| Mirkuzie et al. [32] | Standard basic emergency obstetric and neonatal care training in Addis Ababa; trainees’ reaction and knowledge acquisition. | 2014 | Ethiopia | Nurses and midwives |
Urban. Health centres. |
BEmONC | Federal Democratic Republic of Ethiopia Ministry of Health: Basic Emergency Obstetric and Newborn Care. |
| Eblovi et al. [33] | Retention and use of newborn resuscitation skills following a series of helping babies breathe trainings for midwives in rural Ghana. | 2017 | Ghana | Midwives |
Rural. Health centres. |
Neonatal Resuscitation | American Academy of Pediatrics: Helping Babies Breathe |
| Innerdal et al. [34] | Reduction in Perinatal Mortality after Implementation of HBB Training at a District Hospital in Mali. | 2020 | Mali | Birth attendants |
Rural. Hospitals and health centres. |
Neonatal Resuscitation | American Academy of Pediatrics: Helping Babies Breathe |
| Draiko et al. [35] | Knowledge, skills and competency retention among health workers one year after completing helping babies breathe training in South Sudan. | 2019 | Sudan | Medical officers/doctors, nurses, midwives, maternal child health officers, community health workers, and clinical officers |
Urban. Hospitals. |
Neonatal Resuscitation | American Academy of Pediatrics: Helping Babies Breathe |
| Arabi et al. [36] | Perinatal outcomes following Helping Babies Breathe training and regular peer-peer skills practice among village midwives in Sudan. | 2018 | Sudan | (Village) Midwives |
Rural. Medical centres. |
Neonatal Resuscitation | American Academy of Pediatrics: Helping Babies Breathe |
| Arabi et al. [37] | Skills retention in Sudanese village midwives 1 year following Helping Babies Breathe training. | 2016 | Sudan | (Village) Midwives |
Rural. Medical centres. |
Neonatal Resuscitation | American Academy of Pediatrics: Helping Babies Breathe |
| Alwy Al-Beity et al. [38] | Predictors of change of health workers’ knowledge and skills after the Helping Mothers Survive Bleeding after Birth (HMS BAB) in-facility training in Tanzania. | 2020 | Tanzania | Doctors, nurse-midwives, auxiliary providers |
Rural. Hospitals and health centres. |
Bleeding after Birth | JHPIEGO (ICM, FIGO, UNFPA, WHO, MCSP, AAP): Helping Mothers Survive Bleeding After Birth |
| Egenberg et al. [39] | Impact of multi-professional, scenario-based training on postpartum hemorrhage in Tanzania: a quasi-experimental, pre- vs. post-intervention study. | 2017 | Tanzania | Nurse-midwives, doctors |
Rural. Hospitals. |
Bleeding after Birth | JHPIEGO (ICM, FIGO, UNFPA, WHO, MCSP, AAP): Helping Mothers Survive Bleeding After Birth |
| Egenberg et al. [40] | “No patient should die of PPH just for the lack of training!“ Experiences from multi-professional simulation training on postpartum hemorrhage in northern Tanzania: a qualitative study. | 2017 | Tanzania | Nurse-midwives, doctors, and medical attendants |
Urban. Hospitals. |
Bleeding after Birth | JHPIEGO (ICM, FIGO, UNFPA, WHO, MCSP, AAP): Helping Mothers Survive Bleeding After Birth |
| Neilssen et al. [41] | Clinical performance and patient outcome after simulation-based training in prevention and management of postpartum haemorrhage: an educational intervention study in a low-resource setting. | 2017 | Tanzania | Nurse-midwives, medical attendants (nurse aides without formal medical education), and ambulance drivers (without formal education) |
Rural. Hospitals. |
Bleeding after Birth | JHPIEGO (ICM, FIGO, UNFPA, WHO, MCSP, AAP): Helping Mothers Survive Bleeding After Birth |
| Wilson et al. [42] | Helping Babies Breathe implementation in Zanzibar, Tanzania. | 2017 | Tanzania (Zanzibar) | Nurse-midwives, clinical officers |
Urban and rural. Clinics. |
Neonatal Resuscitation | American Academy of Pediatrics: Helping Babies Breathe |
| Neilssen et al. [43] | Helping mothers survive bleeding after birth: an evaluation of simulation-based training in a low-resource setting. | 2014 | Tanzania | Nurse-midwives, medical attendants (nurse aides without formal medical education), and ambulance drivers (without formal education) |
Rural. Hospitals. |
Bleeding after Birth | JHPIEGO (ICM, FIGO, UNFPA, WHO, MCSP, AAP): Helping Mothers Survive Bleeding After Birth |
| Mesmo et al. [44] | Newborn mortality and fresh stillbirth rates in Tanzania after helping babies breathe training. | 2013 | Tanzania | Health care providers |
Urban. Hospitals. |
Neonatal Resuscitation | American Academy of Pediatrics: Helping Babies Breathe |
| Williams et al. [45] | “Practice so that the skill does not disappear”: mixed methods evaluation of simulator-based learning for midwives in Uganda. | 2019 | Uganda | Doctors, nurse, midwives and “others” |
Urban and rural. Hospitals and health centres. |
Neonatal Resuscitation and Bleeding after Birth |
American Academy of Pediatrics: Helping Babies Breathe. JHPIEGO (ICM, FIGO, UNFPA, WHO, MCSP, AAP): Helping Mothers Survive Bleeding After Birth |
| Hanson et al. [46] | Effects of the Helping Mothers Survive Bleeding after Birth training on near miss morbidity and mortality in Uganda: A cluster-randomized trial. | 2021 | Uganda | Maternity providers |
Rural. Hospitals and health centres. |
Bleeding after Birth | JHPIEGO (ICM, FIGO, UNFPA, WHO, MCSP, AAP): Helping Mothers Survive Bleeding After Birth |
| Bang et al. [47] | Helping Babies Breathe (HBB) training: What happens to knowledge and skills over time? | 2016 | Multi-county (India and Kenya) | Nurses and doctors (India). Nurse-midwives (Kenya) | Hospitals. | Neonatal Resuscitation and Neonatal Care | American Academy of Pediatrics: Helping Babies Breathe |
| Evans et al. [48] | Competency-based training “Helping Mothers Survive: Bleeding after Birth” for providers from central and remote facilities in three countries. | 2014 | Multi-country (India, Malawi, Tanzania incl. Zanzibar) | Health orderlies (Zanzibar only), Auxiliary nurse midwife (India only), Nurses/nurse- midwives (all 3 countries), Clinical officers, medical assistants, and doctors (all 3 countries) |
Urban and rural. Health facilities. |
Bleeding after Birth | JHPIEGO (ICM, FIGO, UNFPA, WHO, MCSP, AAP): Helping Mothers Survive Bleeding After Birth |
In-service training materials
From the 21 studies included in the review, six in-service training materials were identified. Two studies reported on the implementation of more than one in-service training material. The most commonly implemented in-service training materials used were the American Academy of Pediatrics “Helping Babies Breathe” (n = 10) and the JHPIEGO “Helping Mothers Survive – Bleeding After Birth” (n = 8). In countries where more than one study took place it was noted that the same training materials were repeatedly implemented. In Sudan for example, there were three studies, all of which reported on the use of the American Academy of Pediatrics “Helping Babies Breathe”. Similarly, five of the seven studies in Tanzania reported on JHPIEGO’s “Helping Mothers Survive Bleeding After Birth”.
Table 3 shows all 41 in-service training materials identified from the literature search and the grey literature search of websites of organizations known to be active in maternal and newborn global health improvement. The authors grouped the in-service training materials into eight main categories; family planning, antenatal care, intrapartum care, postnatal care - women, postnatal care – newborn, combined in-service training materials (materials that covered aspects of care across the antenatal, intrapartum and postnatal continuum), post abortion care, and whole life course (generic topics relevant to all aspects of care). There was a lack of in-service training materials focused solely on antenatal care (n = 4) and intrapartum care (n = 8). Sub-categories were used to identify training materials focused on uncomplicated and complicated aspects of antenatal care, intrapartum care, and postnatal care for women and the newborn. In these categories there was an equal or higher number of materials focusing on complications compared to uncomplicated antenatal, intrapartum and postnatal care. Additionally, all in-service training materials in the combined in-service training materials category, contained some elements related to the provision of care for complications.
Table 3.
Identified in-service training materials
| Educational area of focus | ID No. | Training package title | Author | Year | Type of material | Link to material |
|---|---|---|---|---|---|---|
| Family planning | 1 | Immediate contraception post obstetrical event (ICPOE) – 2021 | Pan American Health Organization | 2021 | Online learning resource | Immediate contraception post obstetrical event (ICPOE) − 2021 | Virtual Campus for Public Health (VCPH/PAHO) (https://www.campusvirtualsp.org) |
| 2 | Postpartum family planning | Global Health Learning Centre | 2016 | Online learning resource | Postpartum Family Planning | Global Health eLearning Center (https://www.globalhealthlearning.org) | |
| 3 | Updates on contraceptive technology Part 1 | Geneva Foundation for Medical Education and Research | 2013 | Online learning resource | https://www.gfmer.ch/SRH-Course-2013/family-planning/pdf/Updates-contraceptive-technology-Part1-Vogelsong-Festin-2013.pdf | |
| 4 | Updates on contraceptive technology Part 2 | Geneva Foundation for Medical Education and Research | 2013 | Online learning resource | Updates on contraceptive technology. Part 2 (https://www.gfmer.ch) | |
| 5 | Workshop on Comprehensive Postpartum Family Planning Care | JHPIEGO (USAID and ACCESS Family Planning Initiative) | 2008 | Soft copy - available online | http://www.reprolineplus.org/resources/workshop-comprehensive-postpartum-family-planning-care-learning-resource-package | |
| Antenatal care - Uncomplicated | 6 | Antenatal care | Global Health Learning Centre | 2005 | Online learning resource | Antenatal Care | Global Health eLearning Center (https://www.globalhealthlearning.org) |
| 7 | Basic Maternal and Newborn Care: Basic Antenatal Care | JHPIEGO/Maternal and Neonatal Health Program | 2004 | Soft copy - available online | Antenatal Care Module: Course Handbook for Participants: Basic Maternal and Newborn Care Learning Resource Package | ReproLinePlus / Antenatal Care Module: Course Notebook for Trainers: Basic Maternal and Newborn Care Learning Resource Package | ReproLinePlus (https://reprolineplus.org/) | |
| Antenatal care - Complicated | 8 | Prevention and Control of Malaria in Pregnancy (3rd edition) | JHPIEGO | 2018 | Soft copy - available online | Prevention and Control of Malaria in Pregnancy, Third Edition, 2018 Update | ReproLinePlus(https://reprolineplus.org/) |
| 9 | Malaria in pregnancy | Global Health Learning Centre | 2012 | Online learning resource | Malaria in Pregnancy | Global Health eLearning Center (https://www.globalhealthlearning.org) | |
| Labour care -Uncomplicated | 10 | Helping Mothers Survive: Essential Care for Labour and Birth | JHPIEGO | 2019 | Soft copy - available online. Also available as online learning resource | Helping Mothers Survive Essential Care for Labor & Birth (African Graphics) | ReproLinePlus(https://reprolineplus.org/) |
| 11 | Alternative Birth Positions | Maternal and Child Survival Program | 2016 | Soft copy -available online | Alternative Birth Positions training materials (https://www.mcsprogram.org) | |
| Labour care - Complicated | 12 | Helping Mothers Survive: Pre-eclampsia and Eclampsia | JHPIEGO | 2017 | Soft copy - available online. Also available as online learning resource | Helping Mothers Survive Pre-Eclampsia & Eclampsia Training Package: English (African Graphics) | ReproLinePlus (https://reprolineplus.org/) |
| 13 | Helping Mothers and Babies Survive: Threatened Preterm birth care | JHPIEGO | 2016 | Soft copy - available online | http://reprolineplus.org/HMS-PTB-LRP | |
| 14 | Managing Prolonged and Obstructed Labour | JHPIEGO | 2012 | Online learning resource | Jhpiego: Log in to the site (https://learning.jhpiego.org/login/index.php) | |
| Postnatal - Mother - Uncomplicated | 15 | Postpartum care | Global Health Learning Centre | 2019 | Online learning resource | Postpartum Care – Maternal Health Task Force (https://www.mhtf.org) |
| Postnatal - Mother - Complicated | 16 | Helping Mothers Survive: Bleeding After Birth | JHPIEGO | 2017 | Soft copy - available online. Also available as online learning resource | Helping Mothers Survive Bleeding After Birth Complete Training Package: English (International Graphics) | ReproLinePlus / (https://reprolineplus.org/)www.learning.jhpiego.org |
| 17 | The evidence-based management of postpartum haemorrhage | Geneva Foundation for Medical Education and Research | 2013 | Online learning resource | The evidence-based management of Postpartum Haemorrhage (https://www.gfmer.ch) | |
| 18 | Managing Postpartum Haemorrhage | JHPIEGO | 2012 | Online learning resource | Jhpiego: Log in to the site (https://learning.jhpiego.org/login/index.php) | |
| 19 | Managing Puerperal Sepsis | JHPIEGO | 2012 | Online learning resource | Jhpiego: Log in to the site (https://learning.jhpiego.org/login/index.php) | |
| Postnatal - Baby - Uncomplicated | 20 | Helping Babies Survive: Essential Care for Every Baby | American Academy of Pediatrics (not freely available from AAP, but freely available from UNHCR) | 2014 | Soft copy - available online | UNHCR - Essential Care For Every Baby - Provider Guide (ENG) (https://www.unhcr.org/publications/brochures/5db073c64/essential-care-baby-provider-guide-eng.html?query=essential%20care%20of%20every%20baby) |
| 21 | Essential Newborn Care | JHPIEGO | 2012 | Online learning resource | Jhpiego: Log in to the site (https://learning.jhpiego.org/login/index.php) | |
| 22 | Cord Care | Ghana Health Service and USAID, Maternal and Child Survival Program (on JHPIEGO website) | Unknown | Online learning resource | Jhpiego: Log in to the site (https://learning.jhpiego.org/login/index.php) | |
| Postnatal - Baby - Complicated | 23 | Helping Babies Survive: Essential Care for Small Babies | American Academy of Pediatrics | 2015 | Soft copy - available online | UNHCR - Helping babies survive - Essential care for small babies: Facilitator Flip Chart (ENG) (https://www.unhcr.org/publications/brochures/5e14a8724/helping-babies-survive-essential-care-small-babies-facilitator-flip-chart.html?query=helping%20babies%20survive) |
| 24 | Care of low-birth-weight babies through Kangaroo Mother Care | JPHIEGO | 2015 | Soft copy - available online | http://reprolineplus.org/resources/KMC-LRP | |
| 25 | Helping Babies Breathe | American Academy of Pediatrics | 2016 | Soft copy - available online | UNHCR - Helping Babies Breathe - Facilitator Flip Chart (ENG) (https://www.unhcr.org/publications/brochures/5db040554/helping-babies-breathe-facilitator-flip-chart-eng.html?query=helping%20babies%20survive) | |
| 26 | Managing Newborn Problems: A guide for midwives, doctors and nurses. | JHPIEGO | 2004 | Soft copy - available online | http://reprolineplus.org/resources/managing-newborn-problems-guide-midwives-doctors-and-nurses-learning-resource-package | |
| Combined (antenatal, intrapartum, postnatal) | 27 | Safe Delivery App | Maternity Foundation. University of Copenhagen. University of Southern Denmark. | Constantly updated | App available online | Need to download |
| 28 | Basic Emergency Obstetric and Newborn Care | Federal Democratic Republic of Ethiopia. Ministry of Health | 2013 | Soft Copy - available online | Final BEmONC -Training package.pdf (https://www.ethernet.edu.et) | |
| 29 | Best Practices in Maternal and Newborn Care: A learning resource package for essential and basic emergency obstetric newborn care | JHPIEGO | 2008 | Soft copy - available online | Best Practices in Maternal and Newborn Care: A Learning Resource Package for Essential and Basic Emergency Obstetric and Newborn Care | ReproLinePlus (https://reprolineplus.org/) | |
| 30 | Life-Saving Skills Manual for Midwives | American College of Nurse-Midwives | 2008 | Soft Copy - available online | ACNM Global Publications | ACNM Publications (https://www.midwife.org) | |
| 31 | Basic Maternal and Newborn Care: A guide for skilled providers | JHPIEGO | 2004 | Soft Copy - available online | Basic Maternal and Newborn Care: A Guide for Skilled Providers (https://www.reprolineplus.org) http://reprolineplus.org/system/files/resources/bp_mnc_ppts_0.pdf | |
| Post Abortion Care | 32 | Post abortion care | JHPIEGO | 2012 | Online learning resource | Jhpiego: Log in to the site (https://learning.jhpiego.org/login/index.php) |
| 33 | Post abortion care | JHPIEGO (USAID, ACCESS) | 2010 | Soft copy - available online | Post abortion Care Learning Resource Package | ReproLinePlus (https://reprolineplus.org/) | |
| Whole Life course | 34 | ICM Respect Workshop | International Confederation of Midwives | 2020 | Soft copy -available online | Respect Toolkit (https://www.internationalmidwives.org) |
| 35 | Infection Prevention and Control Module 1: Introduction to Infection Prevention and Control | JHPIEGO | 2018 | Soft copy - available online | Infection Prevention and Control. Module 1: Introduction to Infection Prevention and Control | ReproLinePlus (https://reprolineplus.org/) | |
| 36 | Infection Prevention and Control Module 2: Hand Hygiene | JHPIEGO | 2018 | Soft copy - available online | Infection Prevention and Control. Module 2: Hand Hygiene | ReproLinePlus (https://reprolineplus.org/) | |
| 37 | Maternal infections | Geneva Foundation for Medical Education and Research | 2015 | Online learning resource | Maternal Infections e-Learning Course (https://www.gfmer.ch) | |
| 38 | Gender Based Violence | JHPIEGO | Unknown | Online learning resource | Jhpiego: Log in to the site (https://learning.jhpiego.org/login/index.php) | |
| 39 | Maternal and child vaccinations | JHPIEGO | Unknown | Online learning resource | Jhpiego: Log in to the site (https://learning.jhpiego.org/login/index.php) | |
| 40 | Maternal nutrition | JHPIEGO | Unknown | Online learning resource | Jhpiego: Log in to the site (https://learning.jhpiego.org/login/index.php) | |
| 41 | Nurses and midwives’ contribution to an HIV free generation | JHPIEGO | Unknown | Online learning resource | Jhpiego: Log in to the site (https://learning.jhpiego.org/login/index.php) |
Approaches used to conduct in-service training
Table 4 outlines approached used to conduct the in-service training in the 21 studies included in the scoping review. Of note, whilst studies reported on how in-service training was conducted, the finer details relating to facilitation of learning were limited. One study reported in-service training taking place off-site, 12 reported on training taking place onsite and eight studies did not specify where the training took place. Face to face lectures were used in 20 of the 21 studies, with only three studies reporting the use of e-learning. Nineteen studies reported that simulation was used as a teaching tool, whilst almost half (10 studies) reported that ongoing mentorship was used to support in-service training.
Table 4.
Approaches used to conduct in-service training
| Author(s) | Country | Identified Training Material | Location of training | Online lectures | Face to face lectures | Simulation | Mentor- ship |
E-learning |
|---|---|---|---|---|---|---|---|---|
| Yigzaw et al. [28] | Ethiopia | Federal Democratic Republic of Ethiopia Ministry of Health: Basic Emergency Obstetric and Newborn Care. | Offsite | x | x | x | ||
| Weinberg et al. [29] | Ethiopia | American Academy of Pediatrics: Helping Babies Breathe, Essential Care for Every Baby, Essential Care for Small Babies | Onsite | x | x | |||
| Thomsen et al. [30] | Ethiopia | Safe Delivery App | Unknown | x | x | |||
| Lund et al. | Ethiopia | Safe Delivery App | Unknown | x | x | |||
| Mirkuzie et al. [32] | Ethiopia | Federal Democratic Republic of Ethiopia Ministry of Health: Basic Emergency Obstetric and Newborn Care. | Unknown | x | x | |||
| Eblovi et al. [33] | Ghana | American Academy of Pediatrics: Helping Babies Breathe | Unknown | x | x | x | ||
| Innerdal et al. [34] | Mali | American Academy of Pediatrics: Helping Babies Breathe | Onsite | x | ||||
| Draiko et al. [35] | Sudan | American Academy of Pediatrics: Helping Babies Breathe | Unknown | x | x | x | ||
| Arabi et al. [36] | Sudan | American Academy of Pediatrics: Helping Babies Breathe | Onsite | x | x | x | ||
| Arabi et al. [37] | Sudan | American Academy of Pediatrics: Helping Babies Breathe | Onsite | x | x | x | ||
| Alwy Al-Beity et al. [38] | Tanzania | JHPIEGO: Helping Mothers Survive Bleeding After Birth | Onsite | x | x | x | ||
| Egenberg et al. [39] | Tanzania | JHPIEGO: Helping Mothers Survive Bleeding After Birth | Onsite | x | x | x | ||
| Egenberg et al. [40] | Tanzania | JHPIEGO: Helping Mothers Survive Bleeding After Birth | Unknown | x | x | |||
| Neilssen et al. [41] | Tanzania | JHPIEGO: Helping Mothers Survive Bleeding After Birth | Unknown | x | x | |||
| Wilson et al. [42] | Tanzania (Zanzibar) | American Academy of Pediatrics: Helping Babies Breathe | Onsite | x | x | |||
| Neilssen et al. [43] | Tanzania | JHPIEGO: Helping Mothers Survive Bleeding After Birth | Unknown | x | x | |||
| Mesmo et al. [44] | Tanzania | American Academy of Pediatrics: Helping Babies Breathe | Onsite | x | x | x | ||
| Williams et al. [45] | Uganda |
American Academy of Pediatrics: Helping Babies Breathe. JHPIEGO: Helping Mothers Survive Bleeding After Birth |
Onsite | x | x | x | ||
| Hanson et al. [46] | Uganda | JHPIEGO: Helping Mothers Survive Bleeding After Birth | Onsite | x | x | x | ||
| Bang et al. [47] | Multi-county (India and Kenya) | American Academy of Pediatrics: Helping Babies Breathe | Onsite | x | x | x | ||
| Evans et al. [48] | Multi-country (India, Malawi, Tanzania incl. Zanzibar) | JHPIEGO: Helping Mothers Survive Bleeding After Birth | Onsite | x | x |
Alignment with the ICM essential competencies for midwifery practice
The content of the in-service training materials largely met the ICM Essential Competencies [22]. However, the in-service training materials largely lacked focus on woman-centred care and shared decision making. Additional file 4 contains the mapped in-service training materials.
Discussion
To our knowledge this is the first scoping review to map the content of in-service training materials to the ICM Essential Competencies for midwifery practice [22]. Whilst we found the content of the training materials to mostly align to the pertinent ICM Competencies, a lack of focus on woman-centred care and shared decision-making was noted. This finding is in line with recent evidence that suggests rather than being woman-centred, maternity care in sub-Saharan Africa is institution centred [49]. Evidence from Malawi and Ghana indicates that midwifery care providers do not explain to women the reasons for procedures or ask for consent prior to carrying out procedures and furthermore, that women do not feel they can ask questions [50, 51]. This finding is not isolated to countries in sub-Saharan Africa. In high-income countries women-centred care has been the rhetoric since the 1990s, but women still report that they are not as involved in decision making about their care as they would like [52]. This finding is important as it highlights an important gap in in-service training content. Evidence suggests uptake of skilled birth attendance is influenced by respectful, woman-centred care. Using in-service training to ensure the current midwifery workforce are both educated about, and able to provide respectful woman-centred care, may help to increase skilled birth attendance, and therefore improve maternal and newborn outcomes [53].
There are 46 countries in sub-Saharan Africa, yet our scoping review found published literature reporting on in-service training for midwifery care providers in only eight of these countries (Ethiopia, Ghana, Kenya, Malawi, Mali, Sudan, Tanzania and Uganda). The lack of reports from other countries could be because in-service training is not provided or that no research on in-service training is performed. Still, it begs the question as to whether input and resources from high income countries are being centralised to the few rather than the many. This scoping review underlines the previous finding that where in-service training is provided, the focus is on emergency obstetric care with little focus on routine intrapartum care. This is justifiable on the grounds that obstetric haemorrhage is still one of the leading causes of maternal mortality in low-income countries [54]. However, this raises the question as to the focus of in-service training. Preventative and promotive midwifery care that has the potential to improve maternal and neonatal outcomes has largely been overlooked. A study conducted in Uganda revealed that midwifery care providers failed to provide appropriate antenatal, intrapartum and postnatal care for the 872 women enrolled in their study [55]. With routine care standards falling below WHO recommendations, strategies need to be found to improve quality of care provision [55]. Our findings therefore provide clear guidance that routine antenatal, intrapartum and postnatal care need greater attention on the in-service training agenda to ensure women and newborns receive needed and timely care to prevent emergency situations. High quality antenatal care for example, has the potential to support women to adopt a healthy lifestyle, prepare for childbirth, and furthermore, allows midwifery care providers to identify potential risks that may compromise the ongoing pregnancy and birth [56]. Equally, education on routine intrapartum care may help midwifery care providers identify complications during labour, which if acted on, may prevent a number of obstetric emergencies from occurring. With the main focus of included studies being emergency obstetric care, and in particular Helping Mothers Survive Bleeding After Birth, it is interesting to note that despite all this training, postpartum haemorrhage remains a leading cause of maternal death in sub-Saharan Africa. This questions the effectiveness of current in-service training programmes. Whilst evidence from Tanzania suggests training and on-site clinical mentorship improves the self-reported performance of midwifery care providers, further research is needed to assess the long-term effects of such training [21].
Where information was provided, it was noted that the majority of in-service training took place onsite with face-to-face lectures and simulation used as the main teaching techniques. Whilst a strong body of evidence reveals that in-service training has a limited impact on improving outcomes [18, 57], there is evidence to suggest that the use of low-dose-high-frequency simulation techniques improve the efficacy of in-service training [58]. Given the limited impact in-service training has on quality of care and maternal and newborn outcomes, it could be argued that resources aimed at improving the knowledge, skills and behaviours of midwifery care providers should be steered towards improving pre-service education and training. However, improvements to pre-service education and training will not be felt by the current midwifery care provider workforce. It is therefore essential that despite its documented limitations, in-service training that focuses on routine antenatal, intrapartum and postnatal care should continue. In providing the current workforce with the opportunity to develop their knowledge and clinical skills, improvements may be seen in the provision of evidence-based, quality care, which in turn has the potential to reduce maternal and newborn morbidity and mortality [18, 57, 58].
Implementing and gathering evidence on the implementation and outcomes of in-service training could be viewed as altruistic. It is surprising therefore, that in excess of 50 studies were excluded from this scoping review because the in-service training materials they reported on were not easily and/or freely available. Of the studies included, the majority provide little detail on how in-service training was conducted. Failing to report on and evaluate methods of educational approach reduces the ability of others to identify effective practice or learn from possible good practice/mistakes as they go on to implement in-service training. Moving forwards and in light of the current COVID-19 pandemic, the use of e-learning methodologies may be required to ensure midwifery care providers can continue to be trained to perform evidence-based care.
Finally, although not a main focus of this scoping review, very little information was provided on the costs of implementing in-service training, thereby limiting the possibility to calculate the cost-effectiveness of such an intervention. Collectively, these issues limit the ability of midwifery care providers to learn from previous experiences of implementing in-service education, thereby reducing the possibility for successful training approaches to be replicated.
Strengths and limitations of the review
The main strength of this review is that it is the first study to our knowledge that provides an overview of available in-service training materials used in sub-Saharan Africa between 2000 and 2020. Furthermore, it is the first study to our knowledge that maps the content of in-service training materials to the ICM competencies. Limitations of the review include our inability to access and review all in-service training materials used in sub-Saharan Africa between 2000 and 2020. Furthermore, we have been unable to review fully the approaches used to conduct in-service training.
Conclusion
This scoping review found that the majority of in-service training materials identified focused on emergency care for postpartum haemorrhage, and that studies reporting their use were concentrated in a small number of African countries. To reduce maternal and newborn mortality across sub-Saharan Africa, it is essential that midwifery care providers in all countries have access to evidence-based in-service training. The review revealed that a significant number of in-service training materials are not readily and/or freely available. If we truly want to meet the targets of the SDGs and improve maternal and newborn care and outcomes, in-service training materials that are successful in improving provider knowledge and skills, need to be shared and readily available for use. The content of the identified in-service training materials largely met the ICM Essential Competencies, with gaps noted in the aspect of woman-centred care and shared decision making. Placing women at the centre of their care and involving them in decision making may improve their satisfaction with care and their desire to access care. Incorporating aspects of woman-centred care into future in-service training materials should therefore be a priority. It is also important that in-service training is not used as a substitute for poor pre-service training, and the quality of pre-registration courses should be such that midwifery care providers are competent professionals when they qualify.
In conclusion, to reduce maternal and newborn morbidity and mortality midwifery care providers should have access to evidence-based in-service training that includes antenatal care and routine intrapartum care, and places women at the centre of their care as shared decision makers.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
None.
List of abbreviations
- FIGO
International Federation of Gynecology and Obstetrics.
- ICM
International Confederation of Midwives.
- IPA
International Pediatric Association.
- JHPIEGO
Johns Hopkins Program for International Education in Gynecology and Obstetrics.
- MMR
Maternal mortality ratio.
- UNFPA
United Nations Population Fund.
- WHO
World Health Organization.
Author contribution
JW and A-BM conducted the searches, screened the titles, abstracts and full texts, and completed data extraction. JW and HH mapped the in-service training materials to the ICM competencies, and A-BM checked 20% of the mapped materials to ensure agreement. JW wrote the original manuscript. A-BM substantively revised the manuscript. All authors JW, A-BM, HH, MMG and CH have contributed to the manuscript and approved the final version.
Funding
This scoping review is part of the ALERT project which is funded by the European Commission’s Horizon 2020 (No. 847824) under a call for implementation research for maternal and child health (CH).
Publication fees paid by University of Gothenburg, Sweden (ABM).
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Open access funding provided by University of Gothenburg.
Data Availability
The datasets supporting the conclusions of this article are included within the article (and its additional files).
Declarations
Ethics approval and consent to participate
Scoping review – no ethics required.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Sustainable Development Goals [https://sustainabledevelopment.un.org/index.html].
- 2.WHO, UNICEF, UNFPA, The World Bank Group, United Nations Population Division . Trends in maternal mortality: 2000 to 2017: estimates by WHO, UNICEF, UNFPA, The World Bank Group and the United Nations Population Division. Geneva: World Health Organization; 2019. [Google Scholar]
- 3.United Nations Inter-Agency Group for Child Mortality Estimation. Levels and Trends in Child Mortality: Report 2020, Estiamtes developed by the United Nations Inter-Agency Group for Child Mortality Estimation. In. New York; 2021. [DOI] [PMC free article] [PubMed]
- 4.Department of Economic and Social Affairs: The Sustainable Development Goals Report. 2021. In. New York, United States of America; 2021.
- 5.Kruk ME, Gage AD, Joseph NT, Danaei G, García-Saisó S, Salomon JA. Mortality due to low-quality health systems in the universal health coverage era: a systematic analysis of amenable deaths in 137 countries. Lancet. 2018;392(10160):2203–12. doi: 10.1016/S0140-6736(18)31668-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Homer CS, Friberg IK, Dias MA, ten Hoope-Bender P, Sandall J, Speciale AM, Bartlett LA. The projected effect of scaling up midwifery. Lancet. 2014;384(9948):1146–57. doi: 10.1016/S0140-6736(14)60790-X. [DOI] [PubMed] [Google Scholar]
- 7.Sandall J, Soltani H, Gates S, Shennan A, Devane D. Midwife-led continuity models versus other models of care for childbearing women. Cochrane Database Syst Rev 2013(8):Cd004667. [DOI] [PubMed]
- 8.Montagu D, Sudhinaraset M, Diamond-Smith N, Campbell O, Gabrysch S, Freedman L, Kruk ME, Donnay F. Where women go to deliver: understanding the changing landscape of childbirth in Africa and Asia. Health Policy Plan. 2017;32(8):1146–52. doi: 10.1093/heapol/czx060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ng M, Misra A, Diwan V, Agnani M, Levin-Rector A, De Costa A. An assessment of the impact of the JSY cash transfer program on maternal mortality reduction in Madhya Pradesh, India. Glob Health Action. 2014;7:24939. doi: 10.3402/gha.v7.24939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bogren M, Alesö A, Teklemariam M, Sjöblom H, Hammarbäck L, Erlandsson K. Facilitators of and barriers to providing high-quality midwifery education in South-East Asia-An integrative review. Women Birth 2021. [DOI] [PubMed]
- 11.Bogren M, Banu A, Parvin S, Chowdhury M, Erlandsson K. Findings from a context specific accreditation assessment at 38 public midwifery education institutions in Bangladesh. Women Birth. 2021;34(1):e76–83. doi: 10.1016/j.wombi.2020.06.009. [DOI] [PubMed] [Google Scholar]
- 12.Hobbs AJ, Moller AB, Kachikis A, Carvajal-Aguirre L, Say L, Chou D. Scoping review to identify and map the health personnel considered skilled birth attendants in low-and-middle income countries from 2000–2015. PLoS ONE. 2019;14(2):e0211576. doi: 10.1371/journal.pone.0211576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Michel-Schuldt M, McFadden A, Renfrew M, Homer C. The provision of midwife-led care in low-and middle-income countries: An integrative review. Midwifery. 2020;84:102659. doi: 10.1016/j.midw.2020.102659. [DOI] [PubMed] [Google Scholar]
- 14.Filby A, McConville F, Portela A. What Prevents Quality Midwifery Care? A Systematic Mapping of Barriers in Low and Middle Income Countries from the Provider Perspective. PLoS ONE. 2016;11(5):e0153391. doi: 10.1371/journal.pone.0153391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Evans CL, Bazant E, Atukunda I, Williams E, Niermeyer S, Hiner C, Zahn R, Namugerwa R, Mbonye A, Mohan D. Peer-assisted learning after onsite, low-dose, high-frequency training and practice on simulators to prevent and treat postpartum hemorrhage and neonatal asphyxia: A pragmatic trial in 12 districts in Uganda. PLoS ONE. 2018;13(12):e0207909. doi: 10.1371/journal.pone.0207909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ameh CA, Kerr R, Madaj B, Mdegela M, Kana T, Jones S, Lambert J, Dickinson F, White S, van den Broek N. Knowledge and Skills of Healthcare Providers in Sub-Saharan Africa and Asia before and after Competency-Based Training in Emergency Obstetric and Early Newborn Care. PLoS ONE. 2016;11(12):e0167270. doi: 10.1371/journal.pone.0167270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Crofts JF, Mukuli T, Murove BT, Ngwenya S, Mhlanga S, Dube M, Sengurayi E, Winter C, Jordan S, Barnfield S, et al. Onsite training of doctors, midwives and nurses in obstetric emergencies, Zimbabwe. Bull World Health Organ. 2015;93(5):347–51. doi: 10.2471/BLT.14.145532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gavine A, MacGillivray S, McConville F, Gandhi M, Renfrew MJ. Pre-service and in-service education and training for maternal and newborn care providers in low- and middle-income countries: An evidence review and gap analysis. Midwifery. 2019;78:104–13. doi: 10.1016/j.midw.2019.08.007. [DOI] [PubMed] [Google Scholar]
- 19.Makowiecka K, Achadi E, Izati Y, Ronsmans C. Midwifery provision in two districts in Indonesia: how well are rural areas served? Health Policy Plan. 2008;23(1):67–75. doi: 10.1093/heapol/czm036. [DOI] [PubMed] [Google Scholar]
- 20.Fujita N, Perrin XR, Vodounon JA, Gozo MK, Matsumoto Y, Uchida S, Sugiura Y. Humanised care and a change in practice in a hospital in Benin. Midwifery. 2012;28(4):481–8. doi: 10.1016/j.midw.2011.07.003. [DOI] [PubMed] [Google Scholar]
- 21.Mwansisya T, Mbekenga C, Isangula K, Mwasha L, Mbelwa S, Lyimo M, Kisaka L, Mathias V, Pallangyo E, Edwards G, et al. The impact of training on self-reported performance in reproductive, maternal, and newborn health service delivery among healthcare workers in Tanzania: a baseline- and endline-survey. Reprod Health. 2022;19(1):143. doi: 10.1186/s12978-022-01452-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.The International Confederation of Midwives. The International Confederation of Midwives (ICM) Essential Competencies for Midwifery Practice Framework 2019. In. The Hague; 2019.
- 23.Akuze J, Annerstedt KS, Benova L, Chipeta E, Dossou JP, Gross MM, Kidanto H, Marchal B, Alvesson HM, Pembe AB, et al. Action leveraging evidence to reduce perinatal mortality and morbidity (ALERT): study protocol for a stepped-wedge cluster-randomised trial in Benin, Malawi, Tanzania and Uganda. BMC Health Serv Res. 2021;21(1):1324. doi: 10.1186/s12913-021-07155-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Renfrew MJ, McFadden A, Bastos MH, Campbell J, Channon AA, Cheung NF, Silva DR, Downe S, Kennedy HP, Malata A, et al. Midwifery and quality care: findings from a new evidence-informed framework for maternal and newborn care. Lancet. 2014;384(9948):1129–45. doi: 10.1016/S0140-6736(14)60789-3. [DOI] [PubMed] [Google Scholar]
- 25.World Health Organization. Defining competent maternal and newborn health professionals. In. Geneva; 2018.
- 26.Welsh J, Gross MM, Hanson C, Hounkpatin H, Moller AB. Protocol for a scoping review to identify and map in-service education and training materials for midwifery care in sub-Saharan Africa from 2000 to 2020. BMJ Open. 2021;11(3):e047118. doi: 10.1136/bmjopen-2020-047118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. doi: 10.1080/1364557032000119616. [DOI] [Google Scholar]
- 28.Yigzaw M, Tebekaw Y, Kim YM, Kols A, Ayalew F, Eyassu G. Comparing the effectiveness of a blended learning approach with a conventional learning approach for basic emergency obstetric and newborn care training in Ethiopia. Midwifery. 2019;78:42–9. doi: 10.1016/j.midw.2019.07.014. [DOI] [PubMed] [Google Scholar]
- 29.Weinberg S, Jones D, Worku B, Kumera M, Bose C, Patterson J. Helping Babies Survive Training Programs: Evaluating a Teaching Cascade in Ethiopia. Ethiop J Health Sci. 2019;29(6):669–76. doi: 10.4314/ejhs.v29i6.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Thomsen CF, Barrie AMF, Boas IM, Lund S, Sørensen BL, Oljira FG, Tersbøl BP. Health workers’ experiences with the Safe Delivery App in West Wollega Zone, Ethiopia: a qualitative study. Reprod Health. 2019;16(1):50. doi: 10.1186/s12978-019-0725-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lund S, Boas IM, Bedesa T, Fekede W, Nielsen HS, Sørensen BL. Association Between the Safe Delivery App and Quality of Care and Perinatal Survival in Ethiopia: A Randomized Clinical Trial. JAMA Pediatr. 2016;170(8):765–71. doi: 10.1001/jamapediatrics.2016.0687. [DOI] [PubMed] [Google Scholar]
- 32.Mirkuzie AH, Sisay MM, Bedane MM. Standard basic emergency obstetric and neonatal care training in Addis Ababa; trainees reaction and knowledge acquisition. BMC Med Educ. 2014;14:201. doi: 10.1186/1472-6920-14-201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Eblovi D, Kelly P, Afua G, Agyapong S, Dante S, Pellerite M. Retention and use of newborn resuscitation skills following a series of helping babies breathe trainings for midwives in rural Ghana. Glob Health Action. 2017;10(1):1387985. doi: 10.1080/16549716.2017.1387985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Innerdal M, Simaga I, Diall H, Eielsen M, Niermeyer S, Eielsen O, Saugstad OD. Reduction in Perinatal Mortality after Implementation of HBB Training at a District Hospital in Mali. J Trop Pediatr. 2020;66(3):315–21. doi: 10.1093/tropej/fmz072. [DOI] [PubMed] [Google Scholar]
- 35.Draiko CV, Yamarat K, Panza A, Draleru J. Knowledge, skills and competency retention among health workers one year after completing helping babies breathe training in South Sudan. Pan Afr Med J. 2019;33:175. doi: 10.11604/pamj.2019.33.175.17560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Arabi AME, Ibrahim SA, Manar AR, Abdalla MS, Ahmed SE, Dempsey EP, Ryan CA. Perinatal outcomes following Helping Babies Breathe training and regular peer-peer skills practice among village midwives in Sudan. Arch Dis Child. 2018;103(1):24–7. doi: 10.1136/archdischild-2017-312809. [DOI] [PubMed] [Google Scholar]
- 37.Arabi AM, Ibrahim SA, Ahmed SE, MacGinnea F, Hawkes G, Dempsey E, Ryan CA. Skills retention in Sudanese village midwives 1 year following Helping Babies Breathe training. Arch Dis Child. 2016;101(5):439–42. doi: 10.1136/archdischild-2015-309190. [DOI] [PubMed] [Google Scholar]
- 38.Alwy Al-Beity F, Pembe AB, Marrone G, Baker U, Hanson C. Predictors of change of health workers’ knowledge and skills after the Helping Mothers Survive Bleeding after Birth (HMS BAB) in-facility training in Tanzania. PLoS ONE. 2020;15(5):e0232983. doi: 10.1371/journal.pone.0232983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Egenberg S, Masenga G, Bru LE, Eggebø TM, Mushi C, Massay D, Øian P. Impact of multi-professional, scenario-based training on postpartum hemorrhage in Tanzania: a quasi-experimental, pre- vs. post-intervention study. BMC Pregnancy Childbirth. 2017;17(1):287. doi: 10.1186/s12884-017-1478-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Egenberg S, Karlsen B, Massay D, Kimaro H, Bru LE. "No patient should die of PPH just for the lack of training!“ Experiences from multi-professional simulation training on postpartum hemorrhage in northern Tanzania: a qualitative study. BMC Med Educ. 2017;17(1):119. doi: 10.1186/s12909-017-0957-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nelissen E, Ersdal H, Mduma E, Evjen-Olsen B, Twisk J, Broerse J, van Roosmalen J, Stekelenburg J. Clinical performance and patient outcome after simulation-based training in prevention and management of postpartum haemorrhage: an educational intervention study in a low-resource setting. BMC Pregnancy Childbirth. 2017;17(1):301. doi: 10.1186/s12884-017-1481-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wilson GM, Ame AM, Khatib MM, Rende EK, Hartman AM, Blood-Siegfried J. Helping Babies Breathe implementation in Zanzibar, Tanzania. Int J Nurs Pract 2017, 23(4). [DOI] [PubMed]
- 43.Nelissen E, Ersdal H, Ostergaard D, Mduma E, Broerse J, Evjen-Olsen B, van Roosmalen J, Stekelenburg J. Helping mothers survive bleeding after birth: an evaluation of simulation-based training in a low-resource setting. Acta Obstet Gynecol Scand. 2014;93(3):287–95. doi: 10.1111/aogs.12321. [DOI] [PubMed] [Google Scholar]
- 44.Msemo G, Massawe A, Mmbando D, Rusibamayila N, Manji K, Kidanto HL, Mwizamuholya D, Ringia P, Ersdal HL, Perlman J. Newborn mortality and fresh stillbirth rates in Tanzania after helping babies breathe training. Pediatrics. 2013;131(2):e353–60. doi: 10.1542/peds.2012-1795. [DOI] [PubMed] [Google Scholar]
- 45.Williams E, Bazant ES, Holcombe S, Atukunda I, Namugerwa RI, Britt K, Evans C. "Practice so that the skill does not disappear”: mixed methods evaluation of simulator-based learning for midwives in Uganda. Hum Resour Health. 2019;17(1):24. doi: 10.1186/s12960-019-0350-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hanson C, Atuhairwe S, Lucy Atim J, Marrone G, Morris JL, Kaharuza F. Effects of the Helping Mothers Survive Bleeding after Birth training on near miss morbidity and mortality in Uganda: A cluster-randomized trial. Int J Gynaecol Obstet. 2021;152(3):386–94. doi: 10.1002/ijgo.13395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bang A, Patel A, Bellad R, Gisore P, Goudar SS, Esamai F, Liechty EA, Meleth S, Goco N, Niermeyer S, et al. Helping Babies Breathe (HBB) training: What happens to knowledge and skills over time? BMC Pregnancy Childbirth. 2016;16(1):364. doi: 10.1186/s12884-016-1141-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Evans CL, Johnson P, Bazant E, Bhatnagar N, Zgambo J, Khamis AR. Competency-based training “Helping Mothers Survive: Bleeding after Birth” for providers from central and remote facilities in three countries. Int J Gynaecol Obstet. 2014;126(3):286–90. doi: 10.1016/j.ijgo.2014.02.021. [DOI] [PubMed] [Google Scholar]
- 49.Bradley S, McCourt C, Rayment J, Parmar D. Disrespectful intrapartum care during facility-based delivery in sub-Saharan Africa: A qualitative systematic review and thematic synthesis of women’s perceptions and experiences. Soc Sci Med. 2016;169:157–70. doi: 10.1016/j.socscimed.2016.09.039. [DOI] [PubMed] [Google Scholar]
- 50.Afulani PA, Phillips B, Aborigo RA, Moyer CA. Person-centred maternity care in low-income and middle-income countries: analysis of data from Kenya, Ghana, and India. Lancet Glob Health. 2019;7(1):e96–109. doi: 10.1016/S2214-109X(18)30403-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hughes CS, Kamanga M, Jenny A, Zieman B, Warren C, Walker D, Kazembe A. Perceptions and predictors of respectful maternity care in Malawi: A quantitative cross-sectional analysis. Midwifery. 2022;112:103403. doi: 10.1016/j.midw.2022.103403. [DOI] [PubMed] [Google Scholar]
- 52.Care Quality C. 2015 Survey of women’s experiences of maternity care. Statistical release. In. Newcastle upon Tyne; 2015.
- 53.Hulsbergen M, van der Kwaak A. The influence of quality and respectful care on the uptake of skilled birth attendance in Tanzania. BMC Pregnancy Childbirth. 2020;20(1):681. doi: 10.1186/s12884-020-03278-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Say L, Chou D, Gemmill A, Tunçalp Ö, Moller AB, Daniels J, Gülmezoglu AM, Temmerman M, Alkema L. Global causes of maternal death: a WHO systematic analysis. Lancet Glob Health. 2014;2(6):e323–33. doi: 10.1016/S2214-109X(14)70227-X. [DOI] [PubMed] [Google Scholar]
- 55.Muwema M, Kaye DK, Edwards G, Nalwadda G, Nangendo J, Okiring J, Mwanja W, Ekong EN, Kalyango JN, Nankabirwa JI. Perinatal care in Western Uganda: Prevalence and factors associated with appropriate care among women attending three district hospitals. PLoS ONE. 2022;17(5):e0267015. doi: 10.1371/journal.pone.0267015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.World Health Organization: WHO recommendations on antenatal care for a positive pregnancy experience. In. Geneva, Switzerland; 2016. [PubMed]
- 57.Leslie HH, Gage A, Nsona H, Hirschhorn LR, Kruk ME. Training And Supervision Did Not Meaningfully Improve Quality Of Care For Pregnant Women Or Sick Children In Sub-Saharan Africa. Health Aff (Millwood) 2016;35(9):1716–24. doi: 10.1377/hlthaff.2016.0261. [DOI] [PubMed] [Google Scholar]
- 58.Bluestone J, Johnson P, Fullerton J, Carr C, Alderman J, BonTempo J. Effective in-service training design and delivery: evidence from an integrative literature review. Hum Resour Health. 2013;11:51. doi: 10.1186/1478-4491-11-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets supporting the conclusions of this article are included within the article (and its additional files).