Abstract
Type 2 diabetes mellitus (T2DM) is a chronic metabolic disease, which is characterized by hyperglycemia, chronic insulin resistance, progressive decline in β-cell function, and defect in insulin secretion. It has become one of the leading causes of death worldwide. At present, there is no cure for T2DM, but it can be treated, and blood glucose levels can be controlled. It has been reported that diabetic patients may suffer from the adverse effects of conventional medicine. Therefore, alternative therapy, such as traditional Chinese medicine (TCM), can be used to manage and treat diabetes. In this review, glycyrrhizic acid (GL) and its derivatives are suggested to be promising candidates for the treatment of T2DM and its complications. It is the principal bioactive constituent in licorice, one type of TCM. This review comprehensively summarized the therapeutic effects and related mechanisms of GL and its derivatives in managing blood glucose levels and treating T2DM and its complications. In addition, it also discusses existing clinical trials and highlights the research gap in clinical research. In summary, this review can provide a further understanding of GL and its derivatives in T2DM as well as its complications and recent progress in the development of potential drugs targeting T2DM.
Keywords: glycyrrhizic acid, glycyrrhetinic acid, ammonium glycyrrhizinate, diammonium glycyrrhizinate, type 2 diabetes mellitus, diabetic complications, insulin resistance, glucose tolerance
1. Introduction
Diabetes mellitus (DM) is a chronic metabolic disease which is characterized by a persistent excess of glucose in the blood, known as hyperglycemia, and it leads to severe and irreparable damage in different organs over time, especially the heart, blood vessels, eyes, kidneys, and nerves [1,2]. International Diabetes Federation pointed out that about 537 million adults (20–79 years old) are living with DM in 2021, of which 3 in 4 live in low-and middle-income countries, and more than 95% of DM patients are type 2 DM (T2DM) patients. Moreover, the total number of people living with DM is expected to increase to 643 million by 2030 and 783 million by 2045 [1,3]. T2DM is caused by a combination of two primary factors: defective insulin secretion by pancreatic β-cells and chronic insulin resistance in insulin-sensitive tissues [4]. Multiple drugs with hypoglycemic actions for the treatment of T2DM are available in the market nowadays, including sulfonylureas, meglitinides, biguanides, thiazolidinediones, α-glucosidase inhibitors, dipeptidyl peptidase-4 inhibitors, sodium-glucose transporter inhibitors, and glucagon-like peptide-1 (GLP-1) receptor agonists [5,6]. However, most of them have adverse effects, such as nausea, bloating, diarrhea, weight gain, stomach pain, hypoglycemia, and secondary failure of therapy, which may influence medication adherence in patients [5]. In addition, iminosugars, such as miglitol, were shown to be another promising therapeutic agent for T2DM [7,8], and studies were focused on the research and development of miglitol derivatives [9,10,11]. Moreover, T2DM patients are susceptible to develop into poorly controlled diabetic patients, who are highly associated with diabetic complications. As a result, there is no doubt that current conventional anti-diabetic drugs have certain limitations to the minimization of side effects and long-term glucose management, thus anti-T2DM drugs still need to move toward more comprehensive and accessible treatments.
Licorice, the dried root and rhizome of Glycyrrhiza uralensis, Glycyrrhiza inflata or Glycyrrhiza glabra in the Fabaceae family, is a traditional herbal medicine which is extensively used in Europe and Asia [12,13]. Glycyrrhizic acid (GL), also known as glycyrrhizin, is the principal bioactive constituent in licorice and exists as two isomers, 18α-GL and 18β-GL, which make up 5–9% of licorice. Moreover, the aqueous extracts of licorice contain 10–20% GL [14,15]. Studies have shown that GL has many pharmacological effects, including anti-inflammatory [16,17], anti-oxidative [18,19], anti-viral [20,21], immunoregulatory [22,23], anti-cancer [24,25], and anti-diabetic [26,27] activities. In particular, GL exerts therapeutic effects on T2DM, such as reducing blood glucose levels [28], decreasing serum insulin levels [29], enhancing insulin sensitivity [30,31], improving glucose tolerance and homeostasis [28,32,33], and regulating lipid metabolism [33,34,35]. Meanwhile, GL also displays beneficial effects on diabetic complications, including cardiovascular disease [36], cerebrovascular disease [37,38], diabetic nephropathy [39,40], diabetic neuropathy [41], and diabetic retinopathy [31,42,43].
To the best of our knowledge, there is no review summarizing the therapeutic effects and related mechanisms of GL and its derivatives in T2DM. Therefore, we conducted a comprehensive review of GL and its derivatives for the treatment of T2DM and its complications. The related literatures were retrieved from PubMed, Web of Science, and Google Scholar. The search algorithm for PubMed was as follows: (“glycyrrhizic acid” OR “glycyrrhetinic acid” OR “ammonium glycyrrhizinate” OR “diammonium glycyrrhizinate” OR “dipotassium glycyrrhizinate”) AND (“diabetes” OR “insulin” OR “lipid”) with no other restrictions. Similar but adapted search terms were also used for other search engines. Through a comprehensive reading of the retrieved literatures, we have excluded literatures of Type 1 DM, review articles, and other non-related articles. After exclusion, 54 articles were selected, which were related to the treatment of T2DM by GL and its derivatives. Firstly, we provide an overview of GL and its derivatives. Then, we focus on how GL and its derivatives exert therapeutic effects on T2DM and its complications. Finally, we discuss the clinical applications of GL in T2DM patients and provide clinical perspectives. Therefore, this comprehensive review can provide a further understanding of GL and its derivatives in T2DM as well as its complications and recent progress in the development of potential drugs targeting T2DM.
2. GL and Its Derivatives
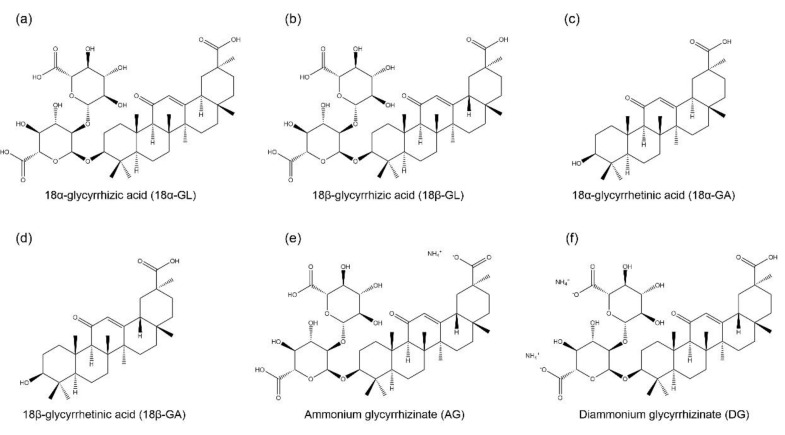
GL is an amphiphilic compound, its hydrophilic part is represented by the glucuronic acid residues, and its hydrophobic part is the glycyrrhetinic acid (GA) residue [44]. GA is not only a hydrolytic product of GL, but it is also one of the main bioactive components of licorice with two isoforms, 18α-GA and 18β-GA [45,46]. GL and its aglycon, GA, have promising therapeutic effects, which have attracted the researchers to develop them into clinical medicine, including anti-cancer, anti-inflammatory, anti-viral, anti-diabetic, and hepatoprotective effects [47,48]. However, studies found that the oral administration of GL is poorly absorbed from the gut, but it is slowly converted into 18β-GA under intestinal bacterial hydrolysis, and the hydrolysis product 18β-GA is absorbed in the gut [49,50]. Therefore, due to the poor bioavailability of GL, it has been designed to conjugate with various metals or ammonium to form water-soluble salts for improving its bioavailability, including ammonium glycyrrhizinate (AG), diammonium glycyrrhizinate (DG), and dipotassium glycyrrhizinate [51,52,53]. The structures of GL, GA, AG, and DG are shown in Figure 1.
Figure 1.
Chemical structures of glycyrrhizic acid (GL) and its derivatives. They include two isomers of glycyrrhizic acid, namely, (a) 18α-glycyrrhizic acid (18α-GL) and (b) 18β-glycyrrhizic acid (18β-GL); two isomers of glycyrrhetinic acid (GA), namely, (c) 18α-glycyrrhetinic acid (18α-GA) and (d) 18β-glycyrrhetinic acid (18β-GA); (e) ammonium glycyrrhizinate (AG); and (f) diammonium glycyrrhizinate (DG).
3. Anti-Diabetic Mechanisms of GL and Its Derivatives in T2DM
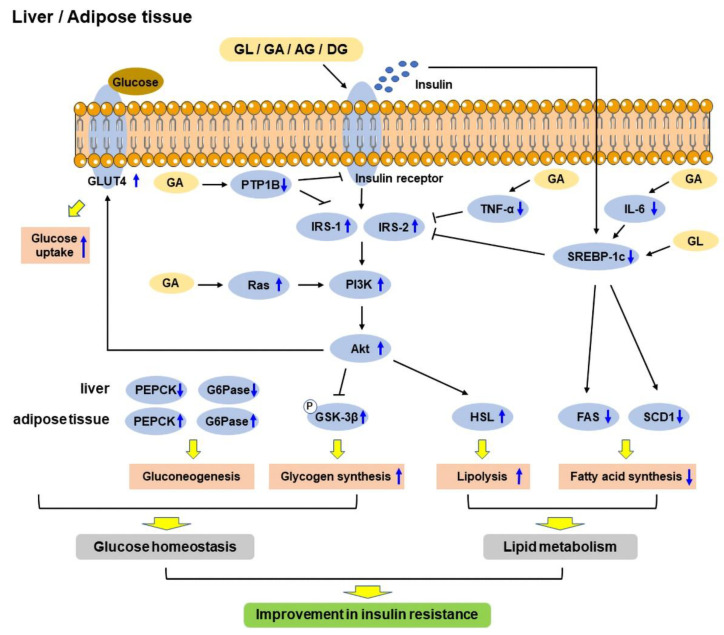
T2DM is mainly characterized by hyperglycemia, which eventually results in chronic insulin resistance in insulin-sensitive tissues and defective insulin secretion by pancreatic β-cells [4]. The anti-diabetic effects of GL and its derivatives have been confirmed in vitro and in vivo. The mechanisms include improving glucose tolerance [33] and insulin sensitivity [28], regulating glucose homeostasis [28] and lipid metabolism [54], and enhancing insulin secretion [55]. A schematic diagram shows the mechanisms of GL and its derivatives in improving insulin resistance in the liver and adipose tissue (Figure 2).
Figure 2.
Schematic diagram showing the mechanisms of glycyrrhizic acid (GL) and its derivatives in improving insulin resistance in the liver and adipose tissue. GL and its derivatives act on the insulin receptor to regulate gluconeogenesis and enhance glycogen synthesis via PI3K/Akt signaling pathway, and increase glucose uptake via GLUT4, thus regulating glucose homeostasis. On the other hand, they increase lipolysis through PI3K/Akt/HSL pathway and reduce fatty acid synthesis through downregulating SREBP-1c/FAS/SCD1 pathway, thereby regulating lipid metabolism. Therefore, GL and its derivatives improve insulin resistance through improving glucose homeostasis and lipid metabolism. FAS: Fatty acid synthetase; G6Pase: Glucose-6-phosphatase; GLUT4: Glucose transporter 4; GSK-3β: Glycogen synthase kinase-3β; HSL: Hormone-sensitive lipase; IGF-1: Insulin-like growth factor 1; IL-6: Interleukin 6; IRS-1: Insulin receptor substrate 1; IRS-2: Insulin receptor substrate 2; PEPCK: Phosphoenolpyruvate carboxykinase; PI3K: Phosphoinositide 3-kinase; PTP1B: Protein tyrosine phosphatase 1B; SCD1: Stearoyl CoA desaturase 1; SREBP-1c: Sterol regulatory element-binding protein 1c; TNF-α: Tumor necrosis factor-α.
3.1. Insulin Resistance
Insulin is a hormone produced by the pancreas that controls glucose levels in the blood and helps in storing glucose in the insulin-sensitive organs, including skeletal muscle, fat, and the liver, where it is used to provide energy. The inability of responding to insulin in insulin-sensitive metabolic tissues, known as insulin resistance, is one of the main pathophysiology of T2DM, thus the tissues cannot uptake glucose from the blood easily. As a result, the pancreas produces more insulin to help in reducing blood glucose levels [56,57]. At a later stage, the pancreatic β-cells cannot compensate for the high demand of insulin; therefore, this eventually leads to β-cell dysfunction and defect in insulin secretion, and hyperglycemia occurs [58]. Studies have shown that GL, GA, and DG could improve insulin sensitivity in diabetic rodents [28,30,31,33,54,59,60,61,62,63,64,65,66,67,68].
There are several indicators of insulin resistance, including homeostasis model assessment of insulin resistance (HOMA-IR), homeostatic model assessment of β-cells (HOMA-β), and quantitative insulin sensitivity check index (QUICKI) [69]. HOMA was developed by Matthews et al., and it is used to quantify insulin resistance and β-cell function from fasting blood glucose and insulin levels [70], while QUICKI is another similar mathematical transformation from fasting blood glucose and insulin levels [71]. A study found that GL reduced HOMA-IR index [28,54,60,63,64,65,66], and increased HOMA-β and QUICKI indices [63] in diabetic rodents, indicating that GL could improve insulin sensitivity. Moreover, impaired fasting blood glucose levels is another indicator of insulin resistance and is characterized by a notable increase in hepatic insulin resistance [72]. GL and 18β-GA were demonstrated to reduce fasting blood glucose levels in diabetic rodents [28,33,54,59,60,63,65,66,67]. In addition, high fasting serum insulin levels is another sign of insulin resistance [73], and GL was found to decrease fasting serum insulin levels in diabetic rodents [28,33,54,66,67].
The insulin sensitivity of metabolic tissues plays a vital role in reducing blood glucose levels, and these tissues mainly include liver, adipose tissue, and skeletal muscle [74]. White adipose tissue (WAT) is an endocrine organ, which stores energy as triacylglycerols, and secretes hormones to regulate glucose homeostasis and adipokines to regulate inflammation. It was suggested that hypertrophy in WAT is associated with insulin resistance [75]. High-fat diet (HFD) was shown to increase visceral adipocyte size and induce adipose tissue inflammation in HFD-induced obese rats. In contrast, GL could decrease the size of adipocytes, thereby reducing body and WAT weights [30]. Moreover, it also reduced the adipocyte size and area in the subcutaneous WAT of rats [65,68]. Similarly, GL and DG could reduce the weights of WAT in HFD-induced obese rodents [30,61]. Furthermore, peroxisome proliferator-activated receptor-γ (PPAR-γ) is a nuclear receptor, which is highly expressed in adipose tissue [76]. The activation of PPAR-γ has been shown to upregulate the expressions of genes that are related to insulin signaling, thus enhancing insulin sensitivity [77]. Studies found that the GL treatment improved insulin sensitivity via upregulating the expression of PPAR-γ in the WAT and skeletal muscle [28,54,59]. On the other hand, the liver is responsible for glucose uptake and lipid synthesis and metabolism [78]. HFD increased liver weight, and GL reduced the liver weight and hepatic steatosis in HFD-induced diabetic mice [33].
Insulin receptor (IR) is a transmembrane receptor, which can be activated by insulin and insulin-like growth factor (IGF). IR and insulin receptor substrate (IRS) play a vital role in regulating glucose homeostasis in the pancreas and insulin-sensitive tissues [56]. IRS acts as a secondary messenger to transmit signals from insulin to downstream intracellular pathways, thus enhancing insulin sensitivity and the transcription of insulin-related genes [79]. GL was found to increase IR mRNA expression and its phosphorylation to enhance insulin sensitivity [30,31]. In addition, another study found that GL enhanced insulin sensitivity through the phosphorylation of IRS-1 and IRS-2 in HFD-induced diabetic mice [33]. Moreover, protein tyrosine phosphatase 1B (PTP1B), the main enzyme involved in IR desensitization, regulates insulin and leptin levels [80]. It is a negative regulator of insulin signaling pathway, and its inhibitors have become an attractive strategy to treat T2DM and obesity [81]. Interestingly, 18α-GA and 18β-GA were identified as competitive PTP1B inhibitors [82,83]. Two other derivatives of GA, namely, indole- and N-phenylpyrazole-GA, also showed potent non-competitive inhibition of PTP1B [84].
Insulin-like growth factor-1 (IGF-1) is a growth hormone that can enhance glucose uptake and reduce hepatic glucose production, thereby improving insulin sensitivity [85]. Insulin and IGF-1 regulate many signaling pathways, including Ras/mitogen-activated protein kinase (MAPK), and phosphoinositide 3-kinase (PI3K)/Akt pathway [56]. The activation of Ras is involved in the development of T2DM, and the inactivation of Ras genes improved insulin sensitivity [86]. In addition, PI3K/Akt pathway was identified as one of the vital pathways that are associated with insulin resistance [87]. GA was shown to improve glucose uptake and reverse insulin resistance by targeting Ras proteins and activating PI3K/Akt pathway, respectively [62]. Moreover, studies found that advanced glycation end products (AGE)-receptor for AGE (RAGE) axis activated oxidative stress and pro-inflammatory pathways, which contributed to insulin resistance [88,89]. GL was found to improve insulin resistance and downregulate RAGE expression spontaneously, suggesting that GL might improve insulin sensitivity via suppressing AGE-RAGE axis [60].
GLP-1, a 30-amino acid peptide hormone, is secreted by gut enteroendocrine cells, which improve insulin resistance in adipocytes [90]. It is currently used as a T2DM therapeutic. In addition, the inhibition of intestinal farnesoid X-activated receptor (FXR) or FXR deficiency was shown to promote GLP-1 secretion [91], and DG was also found to improve insulin resistance and glucose tolerance through downregulation of FXR [61].
Studies have shown that inflammation is associated with insulin resistance, and the most vital pro-inflammatory mediators include tumor necrosis factor-α (TNF-α) and interleukin 6 (IL-6). The inhibition of pro-inflammatory mediators was suggested to be one of the strategies for preventing the development of insulin resistance and the pathogenesis of diabetes [92,93,94,95,96]. GA was shown to reduce fasting plasma TNF-α and IL-6 levels to enhance insulin-responsive pathways [62].
3.2. Glucose Tolerance and Homeostasis
Glucose tolerance is another indicator of diabetes and defined as the ability of the body to dispose glucose. Impaired glucose tolerance is often occurred in T2DM, and the progression from normal to impaired glucose tolerance is caused by insulin resistance [97]. Studies have shown that GL could improve glucose tolerance in diabetic rodents [28,33,67].
Glucose homeostasis can be affected by many factors, including insulin, glucagon, concentration of free fatty acids (FFA), and nutritional factors [98]. Gluconeogenesis is the process of glucose production, and gluconeogenic enzymes play a vital role in this process, including phosphoenolpyruvate carboxykinase (PEPCK), fructose-1,6-bisphosphatase (FBPase), and glucose-6-phosphatase (G6Pase) [99]. Glycogenesis is the process of glycogen synthesis, in which glucose is converted and stored as glycogen in the liver, which is activated by insulin in response to high blood glucose levels. Pyruvate dehydrogenase (PDase), an essential enzyme in glycogen synthesis, is also a substrate of glycogen synthase kinase 3β (GSK-3β), and GSK-3β induces pyruvate dehydrogenase E1α (PDH-E1α) phosphorylation in response to insulin to promote glycogen synthesis [100]. 11β-hydroxysteroid dehydrogenase (11β-HSD) is an enzyme involved in the pathogenesis of metabolic syndrome, which is characterized by hyperglycemia, dyslipidemia, diabetes, and arterial hypertension, and has two isoforms, 11β-HSD1 and 11β-HSD2 [101]. 11β-HSD1 is highly expressed in insulin-sensitive tissues, including liver, WAT, and skeletal muscle [102]. The inhibition of 11β-HSD1 ameliorated hyperglycemia and improved insulin sensitivity in diabetic mice [32]. In addition, PEPCK is a critical enzyme in gluconeogenesis, and the improved activity of PEPCK leads to elevated glucose output and aggravation of diabetes, whereas the defects of PEPCK result in lethal hypoglycemia [103]. Hexose-6-phosphate dehydrogenase (H6PDH), an enzyme that is localized in the endoplasmic reticulum lumen, converts glucose-6-phosphate (G6P) and nicotinamide adenine dinucleotide phosphate (NADP) to produce nicotinamide adenine dinucleotide phosphate hydrogen (NADPH). It provides a high [NADPH]/[NADP+] ratio for 11β-HSD1 amplification of intracellular active glucocorticoid production [104]. Moreover, increased 11β-HSD1-dependent active glucocorticoid production is associated with insulin resistance, T2DM, and its cardiovascular complications [105].
Studies found that GL could reduce PEPCK and G6Pase mRNA expressions to suppress gluconeogenesis, and upregulate PDase and GSK-3β mRNA expressions to increase glycogen synthesis in the liver [30,33,66]. Similarly, GL reduced PEPCK activities in the liver and kidney of normal rats [65], and alleviated the over-activities of PEPCK and G6Pase in the liver and kidney in rats with metabolic syndrome [54]. In addition, GL could reduce H6PDH activities in the liver, kidney, WAT, and muscle [65,66]. Moreover, GL could decrease the activities of 11β-HSD1 and 11β-HSD2 in the liver, kidney, WAT, and muscle to reduce blood glucose levels [64,65,66]. Furthermore, two isoforms of GA have different inhibition activities on 11β-HSD; 18α-GA selectively inhibits 11β-HSD1, but not 11β-HSD2, while 18β-GA favorably inhibits 11β-HSD2 [106].
Glucose transporter type 4 (GLUT4) is an insulin-regulated glucose transporter, which is involved in rapid glucose uptake in various kinds of cells to regulate glucose homeostasis, and its downregulation is closely associated with the development of glucose tolerance [107,108,109]. GA was found to promote GLUT4 expression by targeting Ras protein to regulate MAPK pathway [62]. Similarly, GL elevated GLUT4 expression in the skeletal muscle of HFD-induced diabetic rats to improve glucose homeostasis [28]. Moreover, GL and GA were shown to enhance insulin-stimulated glucose uptake in 3T3L-1 adipocytes [55].
Due to the poor bioavailability of GL, it has been formulated as nanoparticles. GL-loaded nanoparticles improved lipid profile and lowered fasting blood glucose levels in nicotinamide plus streptozotocin (STZ)-induced T2DM rats. Interestingly, the dosages used in GL-loaded nanoparticles were only a quarter of the dosages of the pure GL form [110,111]. Moreover, a combination of GL-loaded nanoparticles and thymoquinone-loaded nanocapsules was applied, displaying better anti-diabetic activities than when administered separately in nicotinamide and STZ-induced T2DM rats, including decreased blood glucose levels and improved lipid profile [111]. Glycosylated hemoglobin A1c is another biochemical parameter that is used to estimate the severity of diabetes, and its high level is an indicator of poor control of blood glucose levels [112]. Moreover, GL-loaded nanoparticles decreased the level of glycosylated hemoglobin A1c [110,111]. Furthermore, GA, as an efficient liver-specific ligand, was made to be a liver-targeted drug delivery carrier and conjugated with chitosan lactate and poly(ethylene glycol) to form nanoparticles containing siRNA-CREB regulated transcription coactivator 2 (CRTC2). These nanoparticles were shown to be accumulated in the liver after 2 h of treatment, reduce blood glucose levels, and inhibit hepatic gluconeogenesis in rats [113,114].
3.3. Lipid Metabolism
The liver is responsible for the regulation of lipid metabolism, uptake of FFA, and export of fat [115]. In T2DM, lipid metabolism is altered, and fat uptake and delivery are imbalanced, which is linked with the over-production of very low-density lipoprotein (VLDL) [115,116]. Many studies found that HFD or high-fat-high-sucrose diet increased serum and hepatic triglyceride (TG), total cholesterol, low-density lipoprotein (LDL) cholesterol, and FFA levels, and decreased high-density lipoprotein (HDL) cholesterol levels in rodents [30,33,54,117,118]. In contrast, GL could improve serum lipid parameters, including decreases in serum and hepatic FFA, TG, total cholesterol, LDL cholesterol, and VLDL levels, but an increase in HDL cholesterol levels in diabetic rodents [30,33,54,68,110,111,117,118]. Similarly, GL-loaded nanoparticles could also decrease total cholesterol, TG, LDL, and VLDL levels, and increase HDL levels in diabetic rats [110]. Meanwhile, GL could also increase lipid uptake in cardiac and skeletal muscle [54].
Lipoprotein lipase (LPL) is a multi-functional glycoprotein enzyme, which plays a vital role in lipid parameters, such as the levels of TG, LDL cholesterol, HDL cholesterol, and VLDL, and its activity is upregulated by apolipoprotein C-II and downregulated by apolipoprotein C-III [119,120]. Increased LPL activity can be used as an indicator of enhanced lipid uptake into tissues [121]. GL was shown to upregulate LPL expression in the kidney, heart, muscle, and WAT [54,59,68,117]. In addition, other studies showed that GL promoted TG metabolism by inducing LPL activity, which upregulated hepatic apolipoprotein C-II expression and suppressed apolipoprotein C-III expression in HFD-induced diabetic mice [33].
Excess FFA and lipid droplets lead to intramuscular accumulation of lipid intermediates, which results in the inhibition of insulin signal transduction to impair insulin sensitivity [122]. GL was shown to decrease lipid deposition in the liver, kidney, heart, and muscle in HFD-induced diabetic rodents [33,117]. Interestingly, a study showed that GL treatment improved insulin sensitivity in HFD-induced obese rats, which might be through decreased lipid deposition [117]. Moreover, hepatic lipogenesis is regulated by a transcription factor, sterol regulatory element-binding transcription factor 1c (SREBP-1c), which is activated by insulin and regulates the genes that are involved in fatty acid and TG synthesis, including fatty acid synthetase (FAS) and stearoyl CoA desaturase (SCD) 1 [123]. GL was shown to improve lipid metabolism mainly through reducing hepatic lipogenesis and improving fatty acid metabolism, via downregulation of SREBP-1c, FAS, and SCD1 expressions, and upregulation of peroxisome proliferator-activated receptor-α (PPAR-α), carnitine palmitoyl transferase 1α (CPT1α), and acyl-coenzyme A dehydrogenase (ACADS), respectively [33]. GL and GA were also found to reduce the early stage of adipogenesis and lipid accumulation in 3T3-L1 adipocytes through downregulating CCAAT/enhancer-binding protein (C/EBP)-β and C/EBP-δ, PPAR-γ, and SCD expressions [55,124]. Similarly, 18β-GA was found to inhibit lipid accumulation, suppress adipogenic differentiation via inhibiting Akt phosphorylation and downregulating PPAR-γ and C/EBP-α expressions, and stimulate lipolysis via upregulation of adipose TG lipase (ATGL), hormone-sensitive lipase (HSL), and perilipin (Plin-1) expressions in 3T3-L1 adipocytes [35]. However, Yamamoto et al. showed that GL did not stimulate lipolysis in 3T3-L1 adipocytes [124].
3.4. Insulin Secretion and Protection of Pancreatic β-Cells
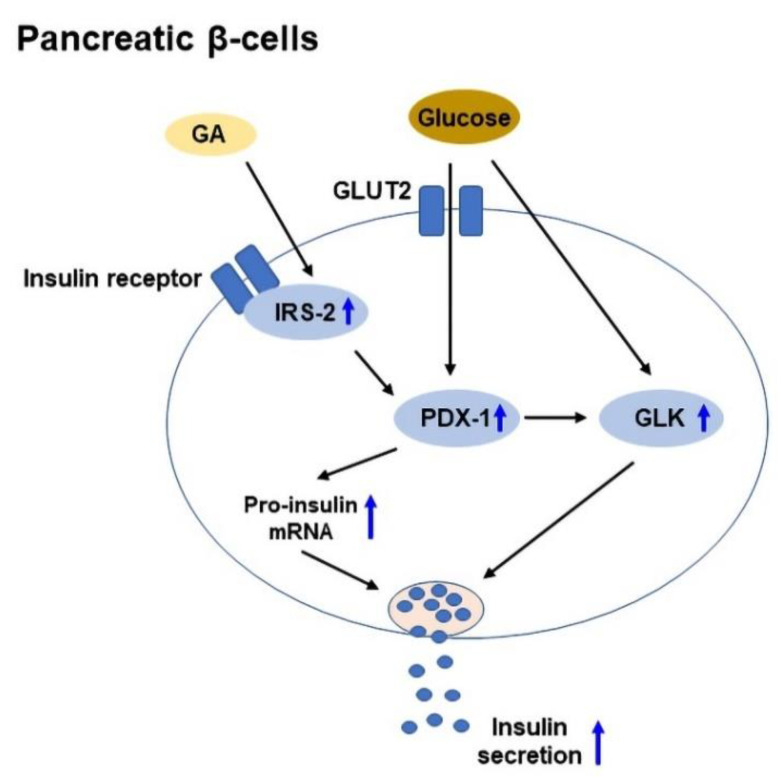
Insulin is a hormone, which is produced by pancreatic β-cells in the islets of Langerhans, and it promotes glucose uptake from the blood into tissues. Insulin secretion is regulated by pancreatic β-cells in response to the increase in blood glucose levels [125]. In T2DM, chronic insulin resistance and a progressive decline in β-cell function result in β-cell dysfunction and defect in insulin secretion [126]. IRS-2 plays a vital role in the preservation of β-cell mass [127], while pancreas duodenum homeobox-1 (PDX-1) plays a role in β-cell survival and function [128]. In addition, glucokinase (GLK) acts as a glucose sensor to regulate insulin secretion [129]. GA was shown to enhance glucose-stimulated insulin secretion in isolated mouse islets, and upregulate IRS-2, PDX-1, and GLK expressions to improve β-cell viability [55]. A schematic diagram of GA-mediated glucose-stimulated insulin secretion in pancreatic β-cells is shown in Figure 3.
Figure 3.
The mechanisms of glycyrrhetinic acid (GA)-mediated glucose-stimulated insulin secretion in pancreatic β-cells. GA upregulates IRS-2, PDX-1, and GLK expressions to protect β-cells and increase insulin secretion. GLUT2: Glucose transporter 2; GLK: Glucokinase; IRS-2: Insulin receptor substrate 2; PDX-1: Pancreas duodenum homeobox-1.
4. GL and Its Derivatives for the Treatment of T2DM Complications
In patients with T2DM, many years of poorly controlled hyperglycemia can lead to multiple complications that mainly affect small blood vessels (microvascular disease) and large blood vessels (macrovascular disease). The microvascular complications include diabetic retinopathy, nephropathy, and neuropathy, while the major macrovascular complications include diabetic cardiovascular and cerebrovascular diseases [130]. Studies showed that GL and its derivatives exerted different protective effects on diabetic microvascular and macrovascular diseases, which will be discussed in more detail in this part.
4.1. Diabetic Retinopathy
Diabetic retinopathy is a microvascular disorder, which is caused by high blood glucose levels damaging the back of the eyes (retina), thus leading to blindness [131]. It is mainly associated with inflammatory processes [132], and studies found that GL improved diabetic retinopathy by inhibiting inflammatory responses [31].
High mobility group box 1 (HMGB1) is a nuclear protein that regulates many gene expressions. When it is activated under pathogenic conditions or stress, it is translocated to the cytoplasm and released into the extracellular environment. Then, the extracellular HMGB1 interacts with its receptors RAGE and toll-like receptor 4 (TLR-4) to trigger pro-inflammatory responses, including interleukin (IL)-1β, IL-6, and TNF-α secretion [133]. It plays a vital role in diabetic retinopathy, and is one potential upstream regulator of TNF-α affecting insulin resistance [134,135] and exhibiting angiogenic effects [136]. Its level is higher in the vitreous fluid of proliferative diabetic retinopathy patients when compared with non-diabetic patients [43,137]. GL, a HMGB1 inhibitor from natural source, suppresses HMGB1 activities through direct binding to HMGB1 [138]. It was found that GL inhibited HMGB1 expression and reduced TNF-α secretion to protect the retina against ischemia/reperfusion-induced damage. In addition, GL was shown to increase IR and IRS-1 phosphorylation in high glucose-induced primary human retinal endothelial cells, thus improving IR signaling [31]. Moreover, high glucose induced the upregulation of HMGB1 and signal transducer and activator of transcription 3 (STAT-3) phosphorylation in human retinal Müller glial cells. In contrast, GL could counteract this effect [139].
4.2. Diabetic Nephropathy
Diabetic nephropathy, a major cause of end-stage renal disease, is caused by high blood glucose levels damaging the blood vessel clusters in the kidneys that filter waste in the blood. The development and progression of diabetic nephropathy are associated with some signaling pathways, including oxidative stress, inflammatory responses, activation of transforming growth factor-β (TGF-β) 1, connective tissue growth factor, and MAPK pathway [140]. GL and its derivatives exerted protective effects on diabetic nephropathy by inhibiting oxidative stress [39,141,142], mitochondrial dysfunction [141] and inflammatory responses [40,141], and preventing renal fibrosis [39,143].
Evidence shows that AMP-activated protein kinase (AMPK) downregulation by high glucose is associated with various disturbances during diabetic microvascular complications [144], while sirtuin 1 (SIRT1), a NAD+-dependent class III protein deacetylase, is activated to exert cytoprotective effects by inhibiting inflammation, oxidative stress, and apoptosis [145,146]. The activation of SIRT1 results in the downregulation of HMGB1 [43]. A study showed that GL protected NRK-52E renal tubular epithelial cells against high glucose-induced oxidative stress and cell proliferation through the upregulation of AMPK and SIRT1 expressions, and downregulation of TGF-β1 expression [142]. GL was also shown to decrease blood albumin/creatinine levels, reduce reactive oxygen species production, and attenuate renal fibrosis and apoptosis in the kidney via activating AMPK/SIRT1/peroxisome proliferator-activated receptor-gamma co-activator 1α (PGC-1α) signaling in db/db mice [39]. In addition, TGF-β1 plays a vital role in tissue fibrosis by enhancing matrix protein synthesis, suppressing matrix degradation, and altering cell-cell interaction [147], and alpha-smooth muscle actin (α-SMA), a marker protein in smooth muscle cells and myofibroblasts that is often used to identify pathological fibroblasts [148]. A study found that GL protected against renal fibrosis in db/db mice by reducing the expressions of TGF-β1 and α-SMA in the kidney [39]. Moreover, GL was found to inhibit HMGB1 expression to reduce inflammatory responses and alleviate the progression of diabetic nephropathy, which was through the downregulation of TLR-4, nucleotide-binding domain leucine-rich repeat and pyrin domain-containing receptor 3 (NLRP3), IL-1β expressions and inhibition of nuclear factor kappa B (NF-κB) pathway in the kidney of Zucker diabetic fatty rats [40]. Another study found that GA could suppress the secretion of connective tissue growth factor and collagen IV in high glucose-exposed mesangial cells, indicating that GA could be used for the prevention of mesangial fibrosis that could lead to diabetic nephropathy [143]. Furthermore, 18α-GA reduced mitochondrial dysfunction and oxidative stress through enhancing adenosine triphosphate (ATP) production, suppressing MAPK pathway and activating nuclear factor-erythroid 2-related factor 2 (Nrf-2) pathway in fructose-exposed HK2 proximal tubular epithelial cells, respectively. Moreover, it alleviated inflammation through the inhibition of NF-κB pathway [141]. Meanwhile, it protected against fructose-induced renal injury in mice through alleviating oxidative stress [141].
4.3. Diabetic Neuropathy
Diabetic neuropathy is one type of nerve damage that is caused by diabetes. The development and progression of diabetic neuropathy are associated with several factors, including persistent hyperglycemia, microvascular insufficiency, oxidative and nitrosative stress, defective neurotropism, and autoimmune-mediated nerve destruction [149,150]. GL was shown to exert protective effects on diabetic neuropathy by alleviating hyperalgesia and inflammation [41].
GL targeted HMGB1 to ameliorate thermal hyperalgesia in Zucker diabetic fatty rats, in which it alleviated neuroinflammation with decreasing expressions of NLRP3, TLR4, and HMGB1 in the dorsal root ganglia [41]. In addition, it inhibited the expression of HMGB1 in the spinal cord dorsal horn, which is released from the neuronal cells to the cytoplasm or the extracellular space. C-X-C chemokine receptor type 4 (CXCR4) is widely expressed in the sensory neurons of the peripheral and central nervous system, and contributes to the pain signaling in both systems. Its increased expression in the dorsal root ganglia neurons of diabetic rats was reduced after GL treatment [41]. Moreover, AG was shown to prevent high glucose-induced cytotoxic effect, apoptosis, and mitochondrial fragmentation through downregulating HMGB1 expression and NF-κB pathway in SH-SY5Y neuroblastoma cells [151]. Furthermore, aluminum plus fructose could induce hyperinsulinemia and insulin resistance. GL ameliorated aluminum-induced neurotoxicity and memory deficit through anti-inflammatory and anti-oxidative effects on the brain tissue of insulin-resistant rats [29]. In addition, it significantly alleviated insulin resistance in aluminum-induced nephrotoxic insulin-resistant rats, and reduced renal oxidative stress and inflammatory responses and kidney dysfunction [152]. Moreover, GL protected against aluminum-induced renal injury via the inhibition of TLR-4/NF-κB signaling pathway [152].
4.4. Diabetic Cardiovascular Disease
High blood glucose levels from diabetes can damage blood vessels and nerves and affect the heart, which can eventually lead to diabetic cardiovascular disease over time [153]. The risk factors of diabetic cardiovascular disease include obesity, hypertension, and dyslipidemia, which are common in patients with T2DM. Moreover, several factors, including increased oxidative stress, inflammation, endothelial dysfunction, and insulin resistance, are often present in patients with T2DM and may directly contribute to the development of diabetic cardiovascular disease [154,155]. GL was shown to exert protective effects on diabetic cardiovascular disease through inhibiting oxidative stress [36] and inflammation [36,156,157,158], alleviating cardiomyocyte atrophy [36], ameliorating endothelial dysfunction [156], and protecting against apoptosis in heart tissue [156].
HMGB1 level was shown to be increased in diabetic patients and db/db mice, and it impaired endothelium-dependent relaxation, an initial critical step that leads to various vascular complications in patients with diabetes, through TLR-4/endothelial nitric oxide synthase (eNOS) pathway. GL could attenuate endothelium-dependent relaxation impairment through eNOS-dependent pathway in the aortas of mice [157]. In addition, GL treatment reduced serum HMGB1 level and upregulated eNOS expression in recombinant HMGB1-treated aortas of db/db mice. Zucker diabetic fatty rats with myocardial remodeling were treated with GL, and it ameliorated cardiomyocyte atrophy, which was evidenced by counteracting the alterations of connexin43 (Cx43), troponin-I (TnI), and voltage-gated sodium channel (Nav1.5) protein expressions in the diabetic heart tissue. Moreover, GL alleviated inflammatory responses via the inhibition of CXCR4/stromal cell-derived factor 1 (SDF1) and TGF-β/p38 MAPK signaling pathways, and improved oxidative stress via the activation of Nrf-2 signaling pathway and downregulation of RAGE expression in the diabetic heart tissue [36]. In addition, GL exerted cardioprotective effects in Zucker diabetic fatty rats with myocardial remodeling by decreasing collagen deposition and apoptosis in the heart tissue, and inhibiting NF-κB signaling pathway to suppress inflammatory responses in the cardiac tissue [36,158]. AGE was found to trigger and aggravate endothelial damage in diabetic vascular complications [159]. A study found that GL protected against AGE-induced endothelial dysfunction in human umbilical vein endothelial cells (HUVECs) through anti-apoptotic, anti-inflammatory, and anti-oxidant activities, via inhibiting RAGE/NF-κB pathway, suggesting that GL can be used for the prevention and treatment of diabetic vascular complications [156]. Furthermore, 18α-GA, as a gap-junction inhibitor, attenuated acetylcholine-induced endothelium-derived hyperpolarizing factor-type relaxation in the mesenteric arteries of T2DM rats [160].
4.5. Diabetic Cerebrovascular Disease
Diabetic cerebrovascular diseases are cerebral vascular damage, which is induced by diabetes with high levels of glucose and fat, thus leading to intracranial large and small vessel diseases [161]. Hyperglycemia can promote damage following cerebrovascular disorders, which are associated with oxidative stress, impaired leukocyte function, increased blood-brain barrier permeability, and inflammatory responses [162]. GL was shown to exert protective effects on diabetic cerebrovascular disease by inhibiting inflammation and ameliorating hippocampal microglial and astrocyte activation [37,38].
GL inhibited HMGB1 to protect against hippocampal inflammation and cognitive deficits in high-fat-high-fructose diet-induced obese rats, in which GL prevented HMGB1 translocation from the nucleus to the cytoplasm, suppressed TLR-4 and NF-κB expressions in the hippocampus, reduced plasma and hippocampal IL-1β, TNF-α and IL-6 levels, and attenuated hippocampal microglia and astrocyte activation [37]. Moreover, GL alleviated cerebral ischemia/reperfusion injury in HFD plus STZ-induced diabetic mice through reducing infarct volume, brain edema and neuronal loss, suppressing microglial activation, and inhibiting pro-inflammatory responses, via the downregulation of HMGB1, TLR-4, NF-κB, IL-1β, IL-6, and TNF-α expressions [38].
5. Clinical Use of GL and Its Derivatives in T2DM and Its Comorbidities
GL and its derivatives have been shown to exert remarkable therapeutic effects on T2DM and its complications. However, the practical use of GL and its derivatives in T2DM and its complications is limited due to insufficient clinical trials. To date, only GL and DG have been tested in clinical trials for the treatment of T2DM and its comorbidities (Table 1). A 24-week clinical study was conducted to investigate the effects of the combination of metformin and DG enteric-coated capsule (DGEC) for the treatment of non-alcoholic fatty liver disease (NAFLD) in patients with T2DM. One hundred and sixty-three patients were randomized into three groups, metformin treatment (50 patients), DGEC treatment (50 patients), and metformin plus DGEC treatment (46 patients). This study found that metformin plus DGEC treatment had better effects than metformin alone or DGEC alone in lowering metabolic parameters, the levels of liver enzymes and lipids, and alleviating hepatic fibrosis [163]. Similarly, another 6-month clinical study was also conducted to investigate the combined effects of DGEC and metformin for the treatment of NAFLD in T2DM patients. Seventy-six patients were randomized into two groups, acarbose plus simvastatin (38 patients), and metformin plus DGEC (38 patients). They found that the combination of DGEC and metformin improved metabolic parameters, hepatic function, and lipid profile in patients with NAFLD and T2DM [164].
Table 1.
A summary showing the clinical trial data of glycyrrhizic acid (GL) and its derivatives for the management of type 2 diabetes mellitus (T2DM) and its comorbidities.
| Drug Name | Trial Design | Trial Length | Sample Size | Patients Recruited |
Dosage | Clinical Outcome | Ref. |
|---|---|---|---|---|---|---|---|
| Diammonium glycyrrhizinate enteric-coated capsule (DGEC) | Randomized controlled trial | 24 weeks | 146 | Patients with T2DM and non-alcoholic fatty liver disease (NAFLD) | Group 1, Metformin alone (500 mg, 3 times daily); Group 2, DGEC alone (450 mg, 3 times daily); Group 3, Metformin (500 mg, 3 times daily) plus DGEC (450 mg, 3 times daily) | Enhanced hypoglycemic action of metformin, including lowering metabolic parameters, the levels of liver enzymes, and lipid levels. Ameliorated hepatic fibrosis. |
[163] |
| DGEC | Randomized uncontrolled trial | 6 months | 76 | Patients with T2DM and NAFLD | Group 1, Acarbose (50–100 mg, 3 times daily) plus Simvastatin (10 mg, once daily); Group 2, Metformin (0.5–1 g, 2 times daily) plus DGEC (50–150 mg, 3 times daily) | Improved metabolic parameters, hepatic function, and lipid profile. | [164] |
| GL tablets | Single-patient trial | 2 months | 1 | Patients with T2DM and acquired reactive perforating collagenosis | Topical application of corticosteroids (2 times daily), oral anti-histamine drug (once daily), GL tablets (3 times daily) | Blood glucose level was controlled, and skin was improved. | [165] |
| GL | Randomized controlled trial | >1 year | 39 | Patients with T2DM and chronic hepatitis | GL (240–525 mg, once weekly) | Decreased serum testosterone concentrations. | [166] |
Reactive perforating collagenosis is a rare skin disorder of transepidermal elimination. A study reported on a 73-year-old T2DM female patient with acquired reactive perforating collagenosis. This patient had itchy papules on her back and lower limbs for 3 months and has been diagnosed as a T2DM patient for 15 years. Her blood glucose level was controlled, and improvement was achieved after treatment with topical application of corticosteroids and oral anti-histamine drug along with GL tablets, suggesting that this might be a good therapy to treat acquired reactive perforating collagenosis [165]. In addition, testosterone deficiency is prevalent in T2DM male patients with metabolic syndrome [167]. A clinical study was conducted to investigate the effects of GL on serum testosterone concentrations in T2DM male patients with chronic hepatitis. Thirty-nine male patients were randomized into two groups, without GL treatment (21 patients), and with GL treatment (18 patients). GL was treated for more than 1 year, which decreased serum testosterone concentrations, and they pointed out that the reduction in serum testosterone concentrations might cause insulin resistance [166]. To date, there are limited clinical trials studying the role of GL or derivatives in T2DM and its comorbidities, and these results reveal that GL and its derivatives might have potential therapeutic effects for T2DM due to its anti-hyperglycemic property and improvement in metabolic syndromes. However, there is still a lack of solid clinical evidence to support the safety and effectiveness of GL and its derivatives in T2DM treatment; therefore, this highlights the urgent need for more clinical trials for the treatment of T2DM and its complications.
6. Conclusions and Future Perspectives
Over the past decades, the incidence rate of T2DM is increasing rapidly, and T2DM is causing a serious burden to individuals and society worldwide. Traditional Chinese medicine is increasingly attracting the attention, interests, and acceptance of pharmaceutical companies due to low toxicity and high efficacy. GL and its derivatives are major bioactive compounds derived from licorice. They have potent anti-diabetic effects on T2DM and its complications, including lowering blood glucose and insulin levels, improving insulin resistance and glucose tolerance, regulating lipid metabolism, and enhancing insulin secretion. Due to the poor bioavailability of GL, it has been formulated as nanoparticles or conjugated with various metals. Moreover, GL-loaded nanoparticles can reduce blood glucose levels and improve lipid profile, and the dosages used in nanoparticles are only one-quarter of the pure GL form; therefore, the nanoparticles are more potent than the pure compound of GL. Furthermore, GL and DGEC have been studied in clinical trials for the treatment of diabetic comorbidities, indicating their potential use as therapeutic drugs. However, there are limited clinical trials for the treatment of T2DM. Therefore, future direction should be focused on the safety evaluation studies and phase II clinical trials for the development of GL and its derivatives as potential drugs of T2DM and its complications.
Author Contributions
Conceptualization, D.T., Y.W. and C.T.V.; formal Analysis, D.T. and C.T.V.; funding acquisition, Y.W.; investigation, D.T., H.H.L.T., Y.W. and C.T.V.; supervision, Y.W. and C.T.V.; writing—original draft, D.T.; writing—review and editing, H.H.L.T., Z.Z., S.W., C.T.V. and Y.W. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This work was funded by the Science and Technology Development Fund of Macau (FDCT/0006/2020/AKP; FDCT/007/2020/ALC), Major Basic and Applied Basic Research Projects of Guangdong Province of China (2019B030302005), and Key-Area Research and Development Program of Guangdong Province, China (2020B1111110003; EF013/ICMS-WYT/2020/GDSTC).
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization (WHO) Diabetes. [(accessed on 12 May 2022)]. Available online: https://www.who.int/news-room/fact-sheets/detail/diabetes.
- 2.American Diabetes Association Diagnosis and classification of diabetes mellitus. Diabetes Care. 2014;37((Suppl. 1)):S81–S90. doi: 10.2337/dc14-S081. [DOI] [PubMed] [Google Scholar]
- 3.International Diabetes Federation (IDF) Diabetes Facts & Figures. [(accessed on 12 May 2022)]. Available online: https://idf.org/aboutdiabetes/what-is-diabetes/facts-figures.html.
- 4.Galicia-Garcia U., Benito-Vicente A., Jebari S., Larrea-Sebal A., Siddiqi H., Uribe K.B., Ostolaza H., Martin C. Pathophysiology of type 2 diabetes mellitus. Int. J. Mol. Sci. 2020;21:6275. doi: 10.3390/ijms21176275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liao S. Side Effects and Interactions of Diabetes Drugs. [(accessed on 12 May 2022)]. Available online: https://www.webmd.com/diabetes/diabetes-drugs-side-effects-interactions.
- 6.Healthline A Complete List of Diabetes Medications. [(accessed on 12 August 2022)]. Available online: https://www.healthline.com/health/diabetes/medications-list#takeaway.
- 7.Nash R.J., Kato A., Yu C.Y., Fleet G.W. Iminosugars as therapeutic agents: Recent advances and promising trends. Future Med. Chem. 2011;3:1513–1521. doi: 10.4155/fmc.11.117. [DOI] [PubMed] [Google Scholar]
- 8.Horne G., Wilson F.X., Tinsley J., Williams D.H., Storer R. Iminosugars past, present and future: Medicines for tomorrow. Drug Discov. Today. 2011;16:107–118. doi: 10.1016/j.drudis.2010.08.017. [DOI] [PubMed] [Google Scholar]
- 9.Verma A.K., Dubbu S., Chennaiah A., Vankar Y.D. Synthesis of di- and trihydroxy proline derivatives from D-glycals: Application in the synthesis of polysubstituted pyrrolizidines and bioactive 1C-aryl/alkyl pyrrolidines. Carbohydr. Res. 2019;475:48–55. doi: 10.1016/j.carres.2019.02.004. [DOI] [PubMed] [Google Scholar]
- 10.Chennaiah A., Bhowmick S., Vankar Y.D. Conversion of glycals into vicinal-1, 2-diazides and 1, 2-(or 2, 1)-azidoacetates using hypervalent iodine reagents and Me 3 SiN 3. Application in the synthesis of N-glycopeptides, pseudo-trisaccharides and an iminosugar. RSC Adv. 2017;7:41755–41762. doi: 10.1039/C7RA08637G. [DOI] [Google Scholar]
- 11.Chennaiah A., Dahiya A., Dubbu S., Vankar Y.D. A Stereoselective Synthesis of an Imino Glycal: Application in the Synthesis of (-)-1-epi-Adenophorine and a Homoimindosugar. Eur. J. Org. Chem. 2018;2018:6574–6581. doi: 10.1002/ejoc.201801241. [DOI] [Google Scholar]
- 12.Wang X., Zhang H., Chen L., Shan L., Fan G., Gao X. Liquorice, a unique "guide drug" of traditional Chinese medicine: A review of its role in drug interactions. J. Ethnopharmacol. 2013;150:781–790. doi: 10.1016/j.jep.2013.09.055. [DOI] [PubMed] [Google Scholar]
- 13.Fiore C., Eisenhut M., Ragazzi E., Zanchin G., Armanini D. A history of the therapeutic use of liquorice in Europe. J. Ethnopharmacol. 2005;99:317–324. doi: 10.1016/j.jep.2005.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang H., Ding X., Tai K.B., Yu A.W. Alternative Medicine and Chinese Herbs and the Kidney. In: Ronco C., Bellomo R., Kellum J.A., Ricci Z., editors. Critical Care Nephrology. 3rd ed. Elsevier; Philadelphia, PA, USA: 2019. pp. 1313–1319.e1. [Google Scholar]
- 15.Xu R., Xiao Q., Cao Y., Yang J. Comparison of the exposure of glycyrrhizin and its metabolites and the pseudoaldosteronism after intravenous administration of alpha- and beta-glycyrrhizin in rat. Drug Res. 2013;63:620–624. doi: 10.1055/s-0033-1349837. [DOI] [PubMed] [Google Scholar]
- 16.Choi M., Thuy L.T., Lee Y., Piao C., Choi J.S., Lee M. Dual-functional dendrimer micelles with glycyrrhizic acid for anti-inflammatory therapy of acute lung injury. ACS Appl. Mater. Interfaces. 2021;13:47313–47326. doi: 10.1021/acsami.1c08107. [DOI] [PubMed] [Google Scholar]
- 17.Wu Z., Wang Z., Xie Z., Zhu H., Li C., Xie S., Zhou W., Zhang Z., Li M. Glycyrrhizic acid attenuates the inflammatory response after spinal cord injury by inhibiting high mobility group box-1 protein through the p38/Jun N-terminal kinase signaling pathway. World Neurosurg. 2021;158:e856–e864. doi: 10.1016/j.wneu.2021.11.085. [DOI] [PubMed] [Google Scholar]
- 18.Sathyamoorthy Y., Kaliappan K., Nambi P., Radhakrishnan R. Glycyrrhizic acid renders robust neuroprotection in rodent model of vascular dementia by controlling oxidative stress and curtailing cytochrome-c release. Nutr. Neurosci. 2020;23:955–970. doi: 10.1080/1028415X.2019.1580935. [DOI] [PubMed] [Google Scholar]
- 19.Elsherbini A.M., Maysarah N.M., El-Sherbiny M., Al-Gayyar M.M., Elsherbiny N.M. Glycyrrhizic acid ameliorates sodium nitrite-induced lung and salivary gland toxicity: Impact on oxidative stress, inflammation and fibrosis. Hum. Exp. Toxicol. 2021;40:707–721. doi: 10.1177/0960327120964555. [DOI] [PubMed] [Google Scholar]
- 20.Zheng W., Huang X., Lai Y., Liu X., Jiang Y., Zhan S. Glycyrrhizic acid for COVID-19: Findings of targeting pivotal inflammatory pathways triggered by SARS-CoV-2. Front. Pharmacol. 2021;12:631206. doi: 10.3389/fphar.2021.631206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bentz G.L., Lowrey A.J., Horne D.C., Nguyen V., Satterfield A.R., Ross T.D., Harrod A.E., Uchakina O.N., McKallip R.J. Using glycyrrhizic acid to target sumoylation processes during Epstein-Barr virus latency. PLoS ONE. 2019;14:e0217578. doi: 10.1371/journal.pone.0217578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sheikhi S., Khamesipour A., Radjabian T., Ghazanfari T., Miramin Mohammadi A. Immunotherapeutic effects of Glycyrrhiza glabra and glycyrrhizic acid on Leishmania major-infection BALB/C mice. Parasite Immunol. 2022;44:e12879. doi: 10.1111/pim.12879. [DOI] [PubMed] [Google Scholar]
- 23.Qian Y., Zheng Y., Jin J., Wu X., Xu K., Dai M., Niu Q., Zheng H., He X., Shen J. Immunoregulation in diabetic wound repair with a photoenhanced glycyrrhizic acid hydrogel scaffold. Adv. Mater. 2022;34:e2200521. doi: 10.1002/adma.202200521. [DOI] [PubMed] [Google Scholar]
- 24.Wang H., Ge X., Qu H., Wang N., Zhou J., Xu W., Xie J., Zhou Y., Shi L., Qin Z., et al. Glycyrrhizic acid inhibits proliferation of gastric cancer cells by inducing cell cycle arrest and apoptosis. Cancer Manag. Res. 2020;12:2853–2861. doi: 10.2147/CMAR.S244481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cai S., Bi Z., Bai Y., Zhang H., Zhai D., Xiao C., Tang Y., Yang L., Zhang X., Li K., et al. Glycyrrhizic acid-induced differentiation repressed stemness in hepatocellular carcinoma by targeting c-Jun N-terminal kinase 1. Front. Oncol. 2019;9:1431. doi: 10.3389/fonc.2019.01431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Akutagawa K., Fujita T., Ouhara K., Takemura T., Tari M., Kajiya M., Matsuda S., Kuramitsu S., Mizuno N., Shiba H., et al. Glycyrrhizic acid suppresses inflammation and reduces the increased glucose levels induced by the combination of Porphyromonas gulae and ligature placement in diabetic model mice. Int. Immunopharmacol. 2019;68:30–38. doi: 10.1016/j.intimp.2018.12.045. [DOI] [PubMed] [Google Scholar]
- 27.Zhang W., Li T., Zhang X.J., Zhu Z.Y. Hypoglycemic effect of glycyrrhizic acid, a natural non-carbohydrate sweetener, on streptozotocin-induced diabetic mice. Food Funct. 2020;11:4160–4170. doi: 10.1039/C9FO02114K. [DOI] [PubMed] [Google Scholar]
- 28.Sil R., Ray D., Chakraborti A.S. Glycyrrhizin ameliorates insulin resistance, hyperglycemia, dyslipidemia and oxidative stress in fructose-induced metabolic syndrome-X in rat model. Indian J. Exp. Biol. 2013;51:129–138. [PubMed] [Google Scholar]
- 29.Ali N.M., Mahmoud A.A.A., Mahmoud M.F., El Fayoumi H.M. Glycyrrhizic acid and silymarin alleviate the neurotoxic effects of aluminum in rats challenged with fructose-induced insulin resistance: Possible role of toll-like receptor 4 pathway. Drug Chem. Toxicol. 2019;42:210–219. doi: 10.1080/01480545.2018.1544984. [DOI] [PubMed] [Google Scholar]
- 30.Abo El-Magd N.F., El-Mesery M., El-Karef A., El-Shishtawy M.M. Glycyrrhizin ameliorates high fat diet-induced obesity in rats by activating NrF2 pathway. Life Sci. 2018;193:159–170. doi: 10.1016/j.lfs.2017.11.005. [DOI] [PubMed] [Google Scholar]
- 31.Liu L., Jiang Y., Steinle J.J. Inhibition of HMGB1 protects the retina from ischemia-reperfusion, as well as reduces insulin resistance proteins. PLoS ONE. 2017;12:e0178236. doi: 10.1371/journal.pone.0178236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Alberts P., Nilsson C., Selen G., Engblom L.O., Edling N.H., Norling S., Klingstrom G., Larsson C., Forsgren M., Ashkzari M., et al. Selective inhibition of 11 beta-hydroxysteroid dehydrogenase type 1 improves hepatic insulin sensitivity in hyperglycemic mice strains. Endocrinology. 2003;144:4755–4762. doi: 10.1210/en.2003-0344. [DOI] [PubMed] [Google Scholar]
- 33.Sun X., Duan X., Wang C., Liu Z., Sun P., Huo X., Ma X., Sun H., Liu K., Meng Q. Protective effects of glycyrrhizic acid against non-alcoholic fatty liver disease in mice. Eur. J. Pharmacol. 2017;806:75–82. doi: 10.1016/j.ejphar.2017.04.021. [DOI] [PubMed] [Google Scholar]
- 34.Huo X., Meng X., Zhang J., Zhao Y. Hepatoprotective effect of different combinations of 18alpha-and 18beta-glycyrrhizic acid against CCl4-induced liver injury in rats. Biomed. Pharmacother. 2020;122:109354. doi: 10.1016/j.biopha.2019.109354. [DOI] [PubMed] [Google Scholar]
- 35.Moon M.H., Jeong J.K., Lee Y.J., Seol J.W., Ahn D.C., Kim I.S., Park S.Y. 18beta-Glycyrrhetinic acid inhibits adipogenic differentiation and stimulates lipolysis. Biochem. Biophys. Res. Commun. 2012;420:805–810. doi: 10.1016/j.bbrc.2012.03.078. [DOI] [PubMed] [Google Scholar]
- 36.Thakur V., Alcoreza N., Delgado M., Joddar B., Chattopadhyay M. Cardioprotective effect of glycyrrhizin on myocardial remodeling in diabetic rats. Biomolecules. 2021;11:569. doi: 10.3390/biom11040569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yu M., Huang H., Dong S., Sha H., Wei W., Liu C. High mobility group box-1 mediates hippocampal inflammation and contributes to cognitive deficits in high-fat high-fructose diet-induced obese rats. Brain Behav. Immun. 2019;82:167–177. doi: 10.1016/j.bbi.2019.08.007. [DOI] [PubMed] [Google Scholar]
- 38.Li Y., Yao N., Zhang T., Guo F., Niu X., Wu Z., Hou S. Ability of post-treatment glycyrrhizic acid to mitigate cerebral ischemia/reperfusion injury in diabetic mice. Med. Sci. Monit. 2020;26:e926551. doi: 10.12659/MSM.926551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hou S., Zhang T., Li Y., Guo F., Jin X. Glycyrrhizic acid prevents diabetic nephropathy by activating AMPK/SIRT1/PGC-1alpha signaling in db/db mice. J. Diabetes Res. 2017;2017:2865912. doi: 10.1155/2017/2865912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Thakur V., Nargis S., Gonzalez M., Pradhan S., Terreros D., Chattopadhyay M. Role of glycyrrhizin in the reduction of inflammation in diabetic kidney disease. Nephron. 2017;137:137–147. doi: 10.1159/000477820. [DOI] [PubMed] [Google Scholar]
- 41.Thakur V., Sadanandan J., Chattopadhyay M. High-mobility group box 1 protein signaling in painful diabetic neuropathy. Int. J. Mol. Sci. 2020;21:881. doi: 10.3390/ijms21030881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Liu L., Jiang Y., Steinle J.J. Epac1 and glycyrrhizin both inhibit HMGB1 levels to reduce diabetes-induced neuronal and vascular damage in the mouse retina. J. Clin. Med. 2019;8:772. doi: 10.3390/jcm8060772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mohammad G., Abdelaziz G.M., Siddiquei M.M., Ahmad A., De Hertogh G., Abu El-Asrar A.M. Cross-talk between sirtuin 1 and the proinflammatory mediator high-mobility group box-1 in the regulation of blood-retinal barrier breakdown in diabetic retinopathy. Curr. Eye Res. 2019;44:1133–1143. doi: 10.1080/02713683.2019.1625406. [DOI] [PubMed] [Google Scholar]
- 44.Pastorino G., Cornara L., Soares S., Rodrigues F., Oliveira M.B.P.P. Liquorice (Glycyrrhiza glabra): A phytochemical and pharmacological review. Phytother. Res. 2018;32:2323–2339. doi: 10.1002/ptr.6178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Newell-Price J.D.C. Cushing Disease. In: Melmed S., editor. The Pituitary. 4th ed. Academic Press; Cambridge, MA, USA: 2017. pp. 515–571. [Google Scholar]
- 46.Sabbioni C., Mandrioli R., Ferranti A., Bugamelli F., Saracino M.A., Forti G.C., Fanali S., Raggi M.A. Separation and analysis of glycyrrhizin, 18beta-glycyrrhetic acid and 18alpha-glycyrrhetic acid in liquorice roots by means of capillary zone electrophoresis. J. Chromatogr. A. 2005;1081:65–71. doi: 10.1016/j.chroma.2005.03.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Graebin C.S. The Pharmacological Activities of Glycyrrhizinic Acid (“Glycyrrhizin”) and Glycyrrhetinic Acid. In: Merillon J.-M., Ramawat K.G., editors. Sweeteners: Pharmacology, Biotechnology, and Applications. 1st ed. Springer International Publishing; New York, NY, USA: 2017. pp. 245–261. [Google Scholar]
- 48.Yang L., Jiang Y., Zhang Z., Hou J., Tian S., Liu Y. The anti-diabetic activity of licorice, a widely used Chinese herb. J. Ethnopharmacol. 2020;263:113216. doi: 10.1016/j.jep.2020.113216. [DOI] [PubMed] [Google Scholar]
- 49.Takeda S., Ishthara K., Wakui Y., Amagaya S., Maruno M., Akao T., Kobashi K. Bioavailability study of glycyrrhetic acid after oral administration of glycyrrhizin in rats; relevance to the intestinal bacterial hydrolysis. J. Pharm. Pharmacol. 1996;48:902–905. doi: 10.1111/j.2042-7158.1996.tb05998.x. [DOI] [PubMed] [Google Scholar]
- 50.Akao T., Hayashi T., Kobashi K., Kanaoka M., Kato H., Kobayashi M., Takeda S., Oyama T. Intestinal bacterial hydrolysis is indispensable to absorption of 18 beta-glycyrrhetic acid after oral administration of glycyrrhizin in rats. J. Pharm. Pharmacol. 1994;46:135–137. doi: 10.1111/j.2042-7158.1994.tb03756.x. [DOI] [PubMed] [Google Scholar]
- 51.Yang J., Zhou L., Wang J., Wang G., Davey A.K. The disposition of diammonium glycyrrhizinate and glycyrrhetinic acid in the isolated perfused rat intestine and liver. Planta Med. 2008;74:1351–1356. doi: 10.1055/s-2008-1081328. [DOI] [PubMed] [Google Scholar]
- 52.Jin S., Fu S., Han J., Jin S., Lv Q., Lu Y., Qi J., Wu W., Yuan H. Improvement of oral bioavailability of glycyrrhizin by sodium deoxycholate/phospholipid-mixed nanomicelles. J. Drug Target. 2012;20:615–622. doi: 10.3109/1061186X.2012.702770. [DOI] [PubMed] [Google Scholar]
- 53.Fry J.C. Natural low-calorie sweeteners. In: Baines D., Seal R., editors. Natural Food Additives, Ingredients and Flavourings. 1st ed. Woodhead Publishing; Sawston, UK: 2012. pp. 41–75. [Google Scholar]
- 54.Cheng H.S., Yaw H.P., Ton S.H., Choy S.M., Kong J.M., Abdul Kadir K. Glycyrrhizic acid prevents high calorie diet-induced metabolic aberrations despite the suppression of peroxisome proliferator-activated receptor gamma expression. Nutrition. 2016;32:995–1001. doi: 10.1016/j.nut.2016.02.002. [DOI] [PubMed] [Google Scholar]
- 55.Ko B.S., Jang J.S., Hong S.M., Sung S.R., Lee J.E., Lee M.Y., Jeon W.K., Park S. Changes in components, glycyrrhizin and glycyrrhetinic acid, in raw Glycyrrhiza uralensis Fisch, modify insulin sensitizing and insulinotropic actions. Biosci. Biotechnol. Biochem. 2007;71:1452–1461. doi: 10.1271/bbb.60533. [DOI] [PubMed] [Google Scholar]
- 56.Boucher J., Kleinridders A., Kahn C.R. Insulin receptor signaling in normal and insulin-resistant states. Cold Spring Harb. Perspect. Biol. 2014;6:a009191. doi: 10.1101/cshperspect.a009191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) Insulin Resistance & Prediabetes. [(accessed on 12 June 2022)]; Available online: https://www.niddk.nih.gov/health-information/diabetes/overview/what-is-diabetes/prediabetes-insulin-resistance.
- 58.Fonseca V.A. Defining and characterizing the progression of type 2 diabetes. Diabetes Care. 2009;32((Suppl. 2)):S151–S156. doi: 10.2337/dc09-S301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Chia Y.Y., Ton S.H., Kadir A.K. Effects of glycyrrhizic acid on peroxisome proliferator-activated receptor gamma (PPARgamma), lipoprotein lipase (LPL), serum lipid and HOMA-IR in rats. PPAR Res. 2010;2010:530265. doi: 10.1155/2010/530265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Cheng H.S., Kong J.M., Ng A.X., Chan W.K., Ton S.H., Abdul Kadir K. Novel inhibitory effects of glycyrrhizic acid on the accumulation of advanced glycation end product and its receptor expression. Nat. Prod. Bioprospect. 2014;4:325–333. doi: 10.1007/s13659-014-0044-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Li Y., Hou H., Wang X., Dai X., Zhang W., Tang Q., Dong Y., Yan C., Wang B., Li Z., et al. Diammonium glycyrrhizinate ameliorates obesity through modulation of gut microbiota-conjugated BAs-FXR signaling. Front. Pharmacol. 2021;12:796590. doi: 10.3389/fphar.2021.796590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Zhang Y., Yang S., Zhang M., Wang Z., He X., Hou Y., Bai G. Glycyrrhetinic acid improves insulin-response pathway by regulating the balance between the Ras/MAPK and PI3K/Akt pathways. Nutrients. 2019;11:604. doi: 10.3390/nu11030604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Fatimah M., Malik M., Mushtaq S., Sarfraz J., Mushtaq Z., Chiragh S. Dose dependent effect of glycyrrhizin on glycaemic control of type 2 diabetic rats. Khyber Med. Univ. J. 2020;12:121–125. [Google Scholar]
- 64.Chia Y.Y., Ton S.H., Kadir K.B. Effects of glycyrrhizic acid on 11 beta-hydroxysteroid dehydrogenase (11 betaHSD1 and 2) activities and HOMA-IR in rats at different treatment periods. Exp. Clin. Endocrinol. Diabetes. 2010;118:617–624. doi: 10.1055/s-0029-1237703. [DOI] [PubMed] [Google Scholar]
- 65.Chia Y.Y., Liong S.Y., Ton S.H., Kadir K.B. Amelioration of glucose homeostasis by glycyrrhizic acid through gluconeogenesis rate-limiting enzymes. Eur. J. Pharmacol. 2012;677:197–202. doi: 10.1016/j.ejphar.2011.12.037. [DOI] [PubMed] [Google Scholar]
- 66.Chandramouli C., Ting Y.S., Lyn L.Y., Ha T.S., Kadir K.A. Glycyrrhizic acid improves lipid and glucose metabolism in high-sucrose-fed rats. J. Endocrinol. Metab. 2011;1:125–141. doi: 10.4021/jem39w. [DOI] [Google Scholar]
- 67.Takii H., Kometani T., Nishimura T., Nakae T., Okada S., Fushiki T. Antidiabetic effect of glycyrrhizin in genetically diabetic KK-Ay mice. Biol. Pharm. Bull. 2001;24:484–487. doi: 10.1248/bpb.24.484. [DOI] [PubMed] [Google Scholar]
- 68.Lim W.Y., Chia Y.Y., Liong S.Y., Ton S.H., Kadir K.A., Husain S.N. Lipoprotein lipase expression, serum lipid and tissue lipid deposition in orally-administered glycyrrhizic acid-treated rats. Lipids Health Dis. 2009;8:31. doi: 10.1186/1476-511X-8-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Muniyappa R., Madan R., Varghese R.T. Assessing Insulin Sensitivity and Resistance in Humans. In: Feingold K.R., Anawalt B., Boyce A., Chrousos G., de Herder W.W., Dhatariya K., Dungan K., Hershman J.M., Hofland J., Kalra S., et al., editors. Endotext. MD Text; South Dartmouth, MA, USA: 2021. [Google Scholar]
- 70.Matthews D.R., Hosker J.P., Rudenski A.S., Naylor B.A., Treacher D.F., Turner R.C. Homeostasis model assessment: Insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–419. doi: 10.1007/BF00280883. [DOI] [PubMed] [Google Scholar]
- 71.Katsuki A., Sumida Y., Gabazza E.C., Murashima S., Urakawa H., Morioka K., Kitagawa N., Tanaka T., Araki-Sasaki R., Hori Y., et al. QUICKI is useful for following improvements in insulin sensitivity after therapy in patients with type 2 diabetes mellitus. J. Clin. Endocrinol. Metab. 2002;87:2906–2908. doi: 10.1210/jcem.87.6.8592. [DOI] [PubMed] [Google Scholar]
- 72.Sasaki N., Ozono R., Higashi Y., Maeda R., Kihara Y. Association of insulin resistance, plasma glucose level, and serum insulin level with hypertension in a population with different stages of impaired glucose metabolism. J. Am. Heart Assoc. 2020;9:e015546. doi: 10.1161/JAHA.119.015546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Chaour M., Theroux P., Gilfix B.M., Campeau L., Lesperance J., Ghitescu M., Gelinas F., Solymoss B.C. ‘True’ fasting serum insulin level, insulin resistance syndrome and coronary artery disease. Coron. Artery Dis. 1997;8:683–688. doi: 10.1097/00019501-199711000-00002. [DOI] [PubMed] [Google Scholar]
- 74.Zhang H., Zhang C. Adipose “talks” to distant organs to regulate insulin sensitivity and vascular function. Obesity. 2010;18:2071–2076. doi: 10.1038/oby.2010.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hoffstedt J., Arner E., Wahrenberg H., Andersson D.P., Qvisth V., Lofgren P., Ryden M., Thorne A., Wiren M., Palmer M., et al. Regional impact of adipose tissue morphology on the metabolic profile in morbid obesity. Diabetologia. 2010;53:2496–2503. doi: 10.1007/s00125-010-1889-3. [DOI] [PubMed] [Google Scholar]
- 76.Vidal-Puig A.J., Considine R.V., Jimenez-Linan M., Werman A., Pories W.J., Caro J.F., Flier J.S. Peroxisome proliferator-activated receptor gene expression in human tissues. Effects of obesity, weight loss, and regulation by insulin and glucocorticoids. J. Clin. Investig. 1997;99:2416–2422. doi: 10.1172/JCI119424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Leonardini A., Laviola L., Perrini S., Natalicchio A., Giorgino F. Cross-talk between PPARgamma and insulin signaling and modulation of insulin sensitivity. PPAR Res. 2009;2009:818945. doi: 10.1155/2009/818945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Santoleri D., Titchenell P.M. Resolving the paradox of hepatic insulin resistance. Cell. Mol. Gastroenterol. Hepatol. 2019;7:447–456. doi: 10.1016/j.jcmgh.2018.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Sesti G., Federici M., Hribal M.L., Lauro D., Sbraccia P., Lauro R. Defects of the insulin receptor substrate (IRS) system in human metabolic disorders. FASEB J. 2001;15:2099–2111. doi: 10.1096/fj.01-0009rev. [DOI] [PubMed] [Google Scholar]
- 80.Goldstein B.J. Protein-tyrosine phosphatase 1B (PTP1B): A novel therapeutic target for type 2 diabetes mellitus, obesity and related states of insulin resistance. Curr. Drug Targets Immune Endocr. Metabol. Disord. 2001;1:265–275. doi: 10.2174/1568008013341163. [DOI] [PubMed] [Google Scholar]
- 81.Combs A.P. Recent advances in the discovery of competitive protein tyrosine phosphatase 1B inhibitors for the treatment of diabetes, obesity, and cancer. J. Med. Chem. 2010;53:2333–2344. doi: 10.1021/jm901090b. [DOI] [PubMed] [Google Scholar]
- 82.Seong S.H., Nguyen D.H., Wagle A., Woo M.H., Jung H.A., Choi J.S. Experimental and computational study to reveal the potential of non-polar constituents from Hizikia fusiformis as dual protein tyrosine phosphatase 1B and alpha-glucosidase inhibitors. Mar. Drugs. 2019;17:302. doi: 10.3390/md17050302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Na M., Cui L., Min B.S., Bae K., Yoo J.K., Kim B.Y., Oh W.K., Ahn J.S. Protein tyrosine phosphatase 1B inhibitory activity of triterpenes isolated from Astilbe oreana. Bioorg. Med. Chem. Lett. 2006;16:3273–3276. doi: 10.1016/j.bmcl.2006.03.036. [DOI] [PubMed] [Google Scholar]
- 84.De-la-Cruz-Martinez L., Duran-Becerra C., Gonzalez-Andrade M., Paez-Franco J.C., German-Acacio J.M., Espinosa-Chavez J., Torres-Valencia J.M., Perez-Villanueva J., Palacios-Espinosa J.F., Soria-Arteche O., et al. Indole- and pyrazole-glycyrrhetinic acid derivatives as PTP1B inhibitors: Synthesis, in vitro and in silico studies. Molecules. 2021;26:4375. doi: 10.3390/molecules26144375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Moller N., Jorgensen J.O. Effects of growth hormone on glucose, lipid, and protein metabolism in human subjects. Endocr. Rev. 2009;30:152–177. doi: 10.1210/er.2008-0027. [DOI] [PubMed] [Google Scholar]
- 86.Kalupahana N.S., Moustaid-Moussa N. The renin-angiotensin system: A link between obesity, inflammation and insulin resistance. Obes. Rev. 2012;13:136–149. doi: 10.1111/j.1467-789X.2011.00942.x. [DOI] [PubMed] [Google Scholar]
- 87.Nandipati K.C., Subramanian S., Agrawal D.K. Protein kinases: Mechanisms and downstream targets in inflammation-mediated obesity and insulin resistance. Mol. Cell. Biochem. 2017;426:27–45. doi: 10.1007/s11010-016-2878-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Walke P.B., Bansode S.B., More N.P., Chaurasiya A.H., Joshi R.S., Kulkarni M.J. Molecular investigation of glycated insulin-induced insulin resistance via insulin signaling and AGE-RAGE axis. Biochim. Biophys. Acta Mol. Basis Dis. 2021;1867:166029. doi: 10.1016/j.bbadis.2020.166029. [DOI] [PubMed] [Google Scholar]
- 89.Parwani K., Mandal P. Role of advanced glycation end products and insulin resistance in diabetic nephropathy. Arch. Physiol. Biochem. 2020:1–13. doi: 10.1080/13813455.2020.1797106. [DOI] [PubMed] [Google Scholar]
- 90.Jiang Y., Wang Z., Ma B., Fan L., Yi N., Lu B., Wang Q., Liu R. GLP-1 improves adipocyte insulin sensitivity following induction of endoplasmic reticulum stress. Front. Pharmacol. 2018;9:1168. doi: 10.3389/fphar.2018.01168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Sun L., Xie C., Wang G., Wu Y., Wu Q., Wang X., Liu J., Deng Y., Xia J., Chen B., et al. Gut microbiota and intestinal FXR mediate the clinical benefits of metformin. Nat. Med. 2018;24:1919–1929. doi: 10.1038/s41591-018-0222-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Olefsky J.M., Glass C.K. Macrophages, inflammation, and insulin resistance. Annu. Rev. Physiol. 2010;72:219–246. doi: 10.1146/annurev-physiol-021909-135846. [DOI] [PubMed] [Google Scholar]
- 93.Daniele G., Guardado Mendoza R., Winnier D., Fiorentino T.V., Pengou Z., Cornell J., Andreozzi F., Jenkinson C., Cersosimo E., Federici M., et al. The inflammatory status score including IL-6, TNF-alpha, osteopontin, fractalkine, MCP-1 and adiponectin underlies whole-body insulin resistance and hyperglycemia in type 2 diabetes mellitus. Acta Diabetol. 2014;51:123–131. doi: 10.1007/s00592-013-0543-1. [DOI] [PubMed] [Google Scholar]
- 94.Palacios-Ortega S., Varela-Guruceaga M., Algarabel M., Ignacio Milagro F., Alfredo Martinez J., de Miguel C. Effect of TNF-alpha on caveolin-1 expression and insulin signaling during adipocyte differentiation and in mature adipocytes. Cell. Physiol. Biochem. 2015;36:1499–1516. doi: 10.1159/000430314. [DOI] [PubMed] [Google Scholar]
- 95.Hotamisligil G.S., Peraldi P., Budavari A., Ellis R., White M.F., Spiegelman B.M. IRS-1-mediated inhibition of insulin receptor tyrosine kinase activity in TNF-alpha- and obesity-induced insulin resistance. Science. 1996;271:665–668. doi: 10.1126/science.271.5249.665. [DOI] [PubMed] [Google Scholar]
- 96.Akash M.S., Shen Q., Rehman K., Chen S. Interleukin-1 receptor antagonist: A new therapy for type 2 diabetes mellitus. J. Pharm. Sci. 2012;101:1647–1658. doi: 10.1002/jps.23057. [DOI] [PubMed] [Google Scholar]
- 97.Wiegand S., Dannemann A., Krude H., Gruters A. Impaired glucose tolerance and type 2 diabetes mellitus: A new field for pediatrics in Europe. Int. J. Obes. 2005;29((Suppl. 2)):S136–S142. doi: 10.1038/sj.ijo.0803081. [DOI] [PubMed] [Google Scholar]
- 98.Bano G. Glucose homeostasis, obesity and diabetes. Best Pract. Res. Clin. Obstet. Gynaecol. 2013;27:715–726. doi: 10.1016/j.bpobgyn.2013.02.007. [DOI] [PubMed] [Google Scholar]
- 99.Sharma R., Tiwari S. Renal gluconeogenesis in insulin resistance: A culprit for hyperglycemia in diabetes. World J. Diabetes. 2021;12:556–568. doi: 10.4239/wjd.v12.i5.556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Islam R., Kim J.G., Park Y., Cho J.Y., Cap K.C., Kho A.R., Chung W.S., Suh S.W., Park J.B. Insulin induces phosphorylation of pyruvate dehydrogenase through RhoA activation pathway in HepG2 cells. FASEB J. 2019;33:2072–2083. doi: 10.1096/fj.201800917R. [DOI] [PubMed] [Google Scholar]
- 101.Seckl J.R., Walker B.R. Minireview: 11beta-hydroxysteroid dehydrogenase type 1- a tissue-specific amplifier of glucocorticoid action. Endocrinology. 2001;142:1371–1376. doi: 10.1210/endo.142.4.8114. [DOI] [PubMed] [Google Scholar]
- 102.Edwards C.R., Stewart P.M., Burt D., Brett L., McIntyre M.A., Sutanto W.S., de Kloet E.R., Monder C. Localisation of 11 beta-hydroxysteroid dehydrogenase--tissue specific protector of the mineralocorticoid receptor. Lancet. 1988;2:986–989. doi: 10.1016/S0140-6736(88)90742-8. [DOI] [PubMed] [Google Scholar]
- 103.Yu S., Meng S., Xiang M., Ma H. Phosphoenolpyruvate carboxykinase in cell metabolism: Roles and mechanisms beyond gluconeogenesis. Mol. Metab. 2021;53:101257. doi: 10.1016/j.molmet.2021.101257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Liu L., Wang Y., Wang J., Dong Y., Chang S., Liu X., Lutfy K., Chen H., Friedman T.C., Jiang M., et al. Enhanced hexose-6-phosphate dehydrogenase expression in adipose tissue may contribute to diet-induced visceral adiposity. Int. J. Obes. 2018;42:1999–2011. doi: 10.1038/s41366-018-0041-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Atanasov A.G., Odermatt A. Readjusting the glucocorticoid balance: An opportunity for modulators of 11beta-hydroxysteroid dehydrogenase type 1 activity? Endocr. Metab. Immune Disord. Drug Targets. 2007;7:125–140. doi: 10.2174/187153007780832082. [DOI] [PubMed] [Google Scholar]
- 106.Classen-Houben D., Schuster D., Da Cunha T., Odermatt A., Wolber G., Jordis U., Kueenburg B. Selective inhibition of 11beta-hydroxysteroid dehydrogenase 1 by 18alpha-glycyrrhetinic acid but not 18beta-glycyrrhetinic acid. J. Steroid Biochem. Mol. Biol. 2009;113:248–252. doi: 10.1016/j.jsbmb.2009.01.009. [DOI] [PubMed] [Google Scholar]
- 107.Duan C., Liu M., Xu H., Tang W., Liu J., Hou L., Li L. Decreased expression of GLUT4 in male CG-IUGR rats may play a vital role in their increased susceptibility to diabetes mellitus in adulthood. Acta Biochim. Biophys. Sin. 2016;48:872–882. doi: 10.1093/abbs/gmw088. [DOI] [PubMed] [Google Scholar]
- 108.Alam F., Islam M.A., Khalil M.I., Gan S.H. Metabolic control of type 2 diabetes by targeting the GLUT4 glucose transporter: Intervention approaches. Curr. Pharm. Des. 2016;22:3034–3049. doi: 10.2174/1381612822666160307145801. [DOI] [PubMed] [Google Scholar]
- 109.Wang T., Wang J., Hu X., Huang X.J., Chen G.X. Current understanding of glucose transporter 4 expression and functional mechanisms. World J. Biol. Chem. 2020;11:76–98. doi: 10.4331/wjbc.v11.i3.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Rani R., Dahiya S., Dhingra D., Dilbaghi N., Kim K.H., Kumar S. Evaluation of anti-diabetic activity of glycyrrhizin-loaded nanoparticles in nicotinamide-streptozotocin-induced diabetic rats. Eur. J. Pharm. Sci. 2017;106:220–230. doi: 10.1016/j.ejps.2017.05.068. [DOI] [PubMed] [Google Scholar]
- 111.Rani R., Dahiya S., Dhingra D., Dilbaghi N., Kaushik A., Kim K.H., Kumar S. Antidiabetic activity enhancement in streptozotocin + nicotinamide-induced diabetic rats through combinational polymeric nanoformulation. Int. J. Nanomed. 2019;14:4383–4395. doi: 10.2147/IJN.S205319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Sherwani S.I., Khan H.A., Ekhzaimy A., Masood A., Sakharkar M.K. Significance of HbA1c test in diagnosis and prognosis of diabetic patients. Biomark. Insights. 2016;11:95–104. doi: 10.4137/BMI.S38440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Negishi M., Irie A., Nagata N., Ichikawa A. Specific binding of glycyrrhetinic acid to the rat liver membrane. Biochim. Biophys. Acta. 1991;1066:77–82. doi: 10.1016/0005-2736(91)90253-5. [DOI] [PubMed] [Google Scholar]
- 114.Rastegari A., Mottaghitalab F., Dinarvand R., Amini M., Arefian E., Gholami M., Atyabi F. Inhibiting hepatic gluconeogenesis by chitosan lactate nanoparticles containing CRTC2 siRNA targeted by poly(ethylene glycol)-glycyrrhetinic acid. Drug Deliv. Transl. Res. 2019;9:694–706. doi: 10.1007/s13346-019-00618-1. [DOI] [PubMed] [Google Scholar]
- 115.Adiels M., Olofsson S.O., Taskinen M.R., Boren J. Overproduction of very low-density lipoproteins is the hallmark of the dyslipidemia in the metabolic syndrome. Arterioscler. Thromb. Vasc. Biol. 2008;28:1225–1236. doi: 10.1161/ATVBAHA.107.160192. [DOI] [PubMed] [Google Scholar]
- 116.Savage D.B., Petersen K.F., Shulman G.I. Disordered lipid metabolism and the pathogenesis of insulin resistance. Physiol. Rev. 2007;87:507–520. doi: 10.1152/physrev.00024.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Eu C.H., Lim W.Y., Ton S.H., bin Abdul Kadir K. Glycyrrhizic acid improved lipoprotein lipase expression, insulin sensitivity, serum lipid and lipid deposition in high-fat diet-induced obese rats. Lipids Health Dis. 2010;9:81. doi: 10.1186/1476-511X-9-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Sil R., Ray D., Chakraborti A.S. Glycyrrhizin ameliorates metabolic syndrome-induced liver damage in experimental rat model. Mol. Cell. Biochem. 2015;409:177–189. doi: 10.1007/s11010-015-2523-y. [DOI] [PubMed] [Google Scholar]
- 119.Palacio Rojas M., Prieto C., Bermudez V., Garicano C., Nunez Nava T., Martinez M.S., Salazar J., Rojas E., Perez A., Marca Vicuna P., et al. Dyslipidemia: Genetics, lipoprotein lipase and HindIII polymorphism. F1000Research. 2017;6:2073. doi: 10.12688/f1000research.12938.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Wung S.F., Kulkarni M.V., Pullinger C.R., Malloy M.J., Kane J.P., Aouizerat B.E. The lipoprotein lipase gene in combined hyperlipidemia: Evidence of a protective allele depletion. Lipids Health Dis. 2006;5:19. doi: 10.1186/1476-511X-5-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Goldberg I.J., Eckel R.H., Abumrad N.A. Regulation of fatty acid uptake into tissues: Lipoprotein lipase- and CD36-mediated pathways. J. Lipid Res. 2009;50:S86–S90. doi: 10.1194/jlr.R800085-JLR200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Park S.S., Seo Y.K. Excess accumulation of lipid impairs insulin sensitivity in skeletal muscle. Int. J. Mol. Sci. 2020;21:1949. doi: 10.3390/ijms21061949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Ferre P., Foufelle F. SREBP-1c transcription factor and lipid homeostasis: Clinical perspective. Horm. Res. 2007;68:72–82. doi: 10.1159/000100426. [DOI] [PubMed] [Google Scholar]
- 124.Yamamoto M., Nagasawa Y., Fujimori K. Glycyrrhizic acid suppresses early stage of adipogenesis through repression of MEK/ERK-mediated C/EBPbeta and C/EBPdelta expression in 3T3-L1 cells. Chem.-Biol. Interact. 2021;346:109595. doi: 10.1016/j.cbi.2021.109595. [DOI] [PubMed] [Google Scholar]
- 125.Fu Z., Gilbert E.R., Liu D. Regulation of insulin synthesis and secretion and pancreatic beta-cell dysfunction in diabetes. Curr. Diabetes Rev. 2013;9:25–53. doi: 10.2174/157339913804143225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Butler A.E., Janson J., Bonner-Weir S., Ritzel R., Rizza R.A., Butler P.C. Beta-cell deficit and increased beta-cell apoptosis in humans with type 2 diabetes. Diabetes. 2003;52:102–110. doi: 10.2337/diabetes.52.1.102. [DOI] [PubMed] [Google Scholar]
- 127.Kubota N., Terauchi Y., Tobe K., Yano W., Suzuki R., Ueki K., Takamoto I., Satoh H., Maki T., Kubota T., et al. Insulin receptor substrate 2 plays a crucial role in beta cells and the hypothalamus. J. Clin. Investig. 2004;114:917–927. doi: 10.1172/JCI21484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Fujimoto K., Polonsky K.S. Pdx1 and other factors that regulate pancreatic beta-cell survival. Diabetes Obes. Metab. 2009;11((Suppl. 4)):30–37. doi: 10.1111/j.1463-1326.2009.01121.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Matschinsky F., Liang Y., Kesavan P., Wang L., Froguel P., Velho G., Cohen D., Permutt M.A., Tanizawa Y., Jetton T.L., et al. Glucokinase as pancreatic beta cell glucose sensor and diabetes gene. J. Clin. Investig. 1993;92:2092–2098. doi: 10.1172/JCI116809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Forbes J.M., Cooper M.E. Mechanisms of diabetic complications. Physiol. Rev. 2013;93:137–188. doi: 10.1152/physrev.00045.2011. [DOI] [PubMed] [Google Scholar]
- 131.National Health Service (NHS) Diabetic Retinopathy. [(accessed on 12 June 2022)]; Available online: https://www.nhs.uk/conditions/diabetic-retinopathy/
- 132.Forrester J.V., Kuffova L., Delibegovic M. The role of inflammation in diabetic retinopathy. Front. Immunol. 2020;11:583687. doi: 10.3389/fimmu.2020.583687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Wang F.C., Pei J.X., Zhu J., Zhou N.J., Liu D.S., Xiong H.F., Liu X.Q., Lin D.J., Xie Y. Overexpression of HMGB1 A-box reduced lipopolysaccharide-induced intestinal inflammation via HMGB1/TLR4 signaling in vitro. World J. Gastroenterol. 2015;21:7764–7776. doi: 10.3748/wjg.v21.i25.7764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Wang Y., Zhong J., Zhang X., Liu Z., Yang Y., Gong Q., Ren B. The role of HMGB1 in the pathogenesis of type 2 diabetes. J. Diabetes Res. 2016;2016:2543268. doi: 10.1155/2016/2543268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Guzman-Ruiz R., Ortega F., Rodriguez A., Vazquez-Martinez R., Diaz-Ruiz A., Garcia-Navarro S., Giralt M., Garcia-Rios A., Cobo-Padilla D., Tinahones F.J., et al. Alarmin high-mobility group B1 (HMGB1) is regulated in human adipocytes in insulin resistance and influences insulin secretion in beta-cells. Int. J. Obes. 2014;38:1545–1554. doi: 10.1038/ijo.2014.36. [DOI] [PubMed] [Google Scholar]
- 136.Biscetti F., Gentileschi S., Bertucci F., Servillo M., Arena V., Angelini F., Stigliano E., Bonanno G., Scambia G., Sacchetti B., et al. The angiogenic properties of human adipose-derived stem cells (HASCs) are modulated by the high mobility group box protein 1 (HMGB1) Int. J. Cardiol. 2017;249:349–356. doi: 10.1016/j.ijcard.2017.09.165. [DOI] [PubMed] [Google Scholar]
- 137.Mohammad G., Siddiquei M.M., Alam K., Nawaz M.I., Mousa A., Opdenakker G., Abu El-Asrar A.M. High-mobility group box-1 regulates the expression of matrix metalloproteinase-9 in diabetic retina. Int. J. Clin. Exp. Pathol. 2016;9:828–840. [Google Scholar]
- 138.Mollica L., De Marchis F., Spitaleri A., Dallacosta C., Pennacchini D., Zamai M., Agresti A., Trisciuoglio L., Musco G., Bianchi M.E. Glycyrrhizin binds to high-mobility group box 1 protein and inhibits its cytokine activities. Chem. Biol. 2007;14:431–441. doi: 10.1016/j.chembiol.2007.03.007. [DOI] [PubMed] [Google Scholar]
- 139.Mohammad G., Jomar D., Siddiquei M.M., Alam K., Abu El-Asrar A.M. High-mobility group box-1 protein mediates the regulation of signal transducer and activator of transcription-3 in the diabetic retina and in human retinal muller cells. Ophthalmic Res. 2017;57:150–160. doi: 10.1159/000448115. [DOI] [PubMed] [Google Scholar]
- 140.Samsu N. Diabetic nephropathy: Challenges in pathogenesis, diagnosis, and treatment. BioMed Res. Int. 2021;2021:1497449. doi: 10.1155/2021/1497449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Cheng X., Qiu L., Wang F. 18alpha-Glycyrrhetinic acid (GA) ameliorates fructose-induced nephropathy in mice by suppressing oxidative stress, dyslipidemia and inflammation. Biomed. Pharmacother. 2020;125:109702. doi: 10.1016/j.biopha.2019.109702. [DOI] [PubMed] [Google Scholar]
- 142.Hou S., Zheng F., Li Y., Gao L., Zhang J. The protective effect of glycyrrhizic acid on renal tubular epithelial cell injury induced by high glucose. Int. J. Mol. Sci. 2014;15:15026–15043. doi: 10.3390/ijms150915026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Li J., Lee Y.S., Choi J.S., Sung H.Y., Kim J.K., Lim S.S., Kang Y.H. Roasted licorice extracts dampen high glucose-induced mesangial hyperplasia and matrix deposition through blocking Akt activation and TGF-beta signaling. Phytomedicine. 2010;17:800–810. doi: 10.1016/j.phymed.2010.02.004. [DOI] [PubMed] [Google Scholar]
- 144.Shrikanth C.B., Nandini C.D. AMPK in microvascular complications of diabetes and the beneficial effects of AMPK activators from plants. Phytomedicine. 2020;73:152808. doi: 10.1016/j.phymed.2018.12.031. [DOI] [PubMed] [Google Scholar]
- 145.Hwang J.W., Yao H., Caito S., Sundar I.K., Rahman I. Redox regulation of SIRT1 in inflammation and cellular senescence. Free Radic. Biol. Med. 2013;61:95–110. doi: 10.1016/j.freeradbiomed.2013.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Morigi M., Perico L., Benigni A. Sirtuins in renal health and disease. J. Am. Soc. Nephrol. 2018;29:1799–1809. doi: 10.1681/ASN.2017111218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Frangogiannis N. Transforming growth factor-beta in tissue fibrosis. J. Exp. Med. 2020;217:e20190103. doi: 10.1084/jem.20190103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Sun K.H., Chang Y., Reed N.I., Sheppard D. Alpha-Smooth muscle actin is an inconsistent marker of fibroblasts responsible for force-dependent TGFbeta activation or collagen production across multiple models of organ fibrosis. Am. J. Physiol. Lung Cell Mol. Physiol. 2016;310:L824–L836. doi: 10.1152/ajplung.00350.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Vinik A.I., Nevoret M.L., Casellini C., Parson H. Diabetic neuropathy. Endocrinol. Metab. Clin. N. Am. 2013;42:747–787. doi: 10.1016/j.ecl.2013.06.001. [DOI] [PubMed] [Google Scholar]
- 150.Feldman E.L., Callaghan B.C., Pop-Busui R., Zochodne D.W., Wright D.E., Bennett D.L., Bril V., Russell J.W., Viswanathan V. Diabetic neuropathy. Nat. Rev. Dis. Primers. 2019;5:42. doi: 10.1038/s41572-019-0092-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Ciarlo L., Marzoli F., Minosi P., Matarrese P., Pieretti S. Ammonium glycyrrhizinate prevents apoptosis and mitochondrial dysfunction induced by high glucose in SH-SY5Y cell line and counteracts neuropathic pain in streptozotocin-induced diabetic mice. Biomedicines. 2021;9:608. doi: 10.3390/biomedicines9060608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Emara N.A., Mahmoud M.F., El Fayoumi H.M., Mahmoud A.A.A. The renoprotective effect of glycyrrhizic acid in insulin-resistant rats exposed to aluminum involves the inhibition of TLR4/NF-kappaB signaling pathway. Naunyn-Schmiedeberg’s Arch. Pharmacol. 2021;394:863–872. doi: 10.1007/s00210-020-02012-y. [DOI] [PubMed] [Google Scholar]
- 153.Nanayakkara N., Curtis A.J., Heritier S., Gadowski A.M., Pavkov M.E., Kenealy T., Owens D.R., Thomas R.L., Song S., Wong J., et al. Impact of age at type 2 diabetes mellitus diagnosis on mortality and vascular complications: Systematic review and meta-analyses. Diabetologia. 2021;64:275–287. doi: 10.1007/s00125-020-05319-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Leon B.M., Maddox T.M. Diabetes and cardiovascular disease: Epidemiology, biological mechanisms, treatment recommendations and future research. World J. Diabetes. 2015;6:1246–1258. doi: 10.4239/wjd.v6.i13.1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Martin-Timon I., Sevillano-Collantes C., Segura-Galindo A., Del Canizo-Gomez F.J. Type 2 diabetes and cardiovascular disease: Have all risk factors the same strength? World J. Diabetes. 2014;5:444–470. doi: 10.4239/wjd.v5.i4.444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Feng L., Zhu M.M., Zhang M.H., Wang R.S., Tan X.B., Song J., Ding S.M., Jia X.B., Hu S.Y. Protection of glycyrrhizic acid against AGEs-induced endothelial dysfunction through inhibiting RAGE/NF-kappaB pathway activation in human umbilical vein endothelial cells. J. Ethnopharmacol. 2013;148:27–36. doi: 10.1016/j.jep.2013.03.035. [DOI] [PubMed] [Google Scholar]
- 157.Zhu Z., Peng X., Li X., Tu T., Yang H., Teng S., Zhang W., Xing Z., Tang J., Hu X., et al. HMGB1 impairs endothelium-dependent relaxation in diabetes through TLR4/eNOS pathway. FASEB J. 2020;34:8641–8652. doi: 10.1096/fj.202000242R. [DOI] [PubMed] [Google Scholar]
- 158.Chen F., Song J. Cardioprotective action of glycyrrhizin on diabetic rats with myocardial remodeling. J. Healthc. Eng. 2021;2021:6343677. doi: 10.1155/2021/6343677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Yang P., Feng J., Peng Q., Liu X., Fan Z. Advanced glycation end products: Potential mechanism and therapeutic target in cardiovascular complications under diabetes. Oxid. Med. Cell. Longev. 2019;2019:9570616. doi: 10.1155/2019/9570616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Matsumoto T., Kobayashi T., Kamata K. Mechanisms underlying the impaired EDHF-type relaxation response in mesenteric arteries from Otsuka Long-Evans Tokushima Fatty (OLETF) rats. Eur. J. Pharmacol. 2006;538:132–140. doi: 10.1016/j.ejphar.2006.04.006. [DOI] [PubMed] [Google Scholar]
- 161.Zhou H., Zhang X., Lu J. Progress on diabetic cerebrovascular diseases. Bosn. J. Basic Med. Sci. 2014;14:185–190. doi: 10.17305/bjbms.2014.4.203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Shukla V., Shakya A.K., Perez-Pinzon M.A., Dave K.R. Cerebral ischemic damage in diabetes: An inflammatory perspective. J. Neuroinflamm. 2017;14:21. doi: 10.1186/s12974-016-0774-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Zhang R., Cheng K., Xu S., Li S., Zhou Y., Zhou S., Kong R., Li L., Li J., Feng J., et al. Metformin and diammonium glycyrrhizinate enteric-coated capsule versus metformin alone versus diammonium glycyrrhizinate enteric-coated capsule alone in patients with nonalcoholic fatty liver disease and type 2 diabetes mellitus. Gastroenterol. Res. Pract. 2017;2017:8491742. doi: 10.1155/2017/8491742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Xi W., Han X. Clinical study of metformin combined with diammonium glycyrrhizinate in the treatment of type 2 diabetes mellitus with non-alcoholic fatty liver disease. Chin. Hepatol. 2017;22:558–560. [Google Scholar]
- 165.Fei C., Wang Y., Gong Y., Xu H., Yu Q., Shi Y. Acquired reactive perforating collagenosis: A report of a typical case. Medicine. 2016;95:e4305. doi: 10.1097/MD.0000000000004305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Fukui M., Kitagawa Y., Nakamura N., Yoshikawa T. Glycyrrhizin and serum testosterone concentrations in male patients with type 2 diabetes. Diabetes Care. 2003;26:2962. doi: 10.2337/diacare.26.10.2962. [DOI] [PubMed] [Google Scholar]
- 167.Rao P.M., Kelly D.M., Jones T.H. Testosterone and insulin resistance in the metabolic syndrome and T2DM in men. Nat. Rev. Endocrinol. 2013;9:479–493. doi: 10.1038/nrendo.2013.122. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.