Abstract
Antipsychotics share the common pharmacological feature of antagonizing the dopamine 2 receptor (D2R), which is abundant in the striatum and involved in both the therapeutic and side effects of this drug’s class. The pharmacological blockade of striatal D2R, by disinhibiting the D2R-containing medium-sized spiny neurons (MSNs), leads to a plethora of molecular, cellular and behavioral adaptations, which are central in the action of antipsychotics. Here, we focused on the cell type-specific (D2R-MSNs) regulation of some striatal immediate early genes (IEGs), such as cFos, Arc and Zif268. Taking advantage of transgenic mouse models, pharmacological approaches and immunofluorescence analyses, we found that haloperidol-induced IEGs in the striatum required the synergistic activation of A2a (adenosine) and NMDA (glutamate) receptors. At the intracellular signaling level, we found that the PKA/DARPP-32 and mTOR pathways synergistically cooperate to control the induction of IEGs by haloperidol. By confirming and further expanding previous observations, our results provide novel insights into the regulatory mechanisms underlying the molecular/cellular action of antipsychotics in the striatum.
Keywords: haloperidol, striatum, immediate early genes, dopamine, D2R, PKA, mTOR
1. Introduction
The vast majority of antipsychotics shares the common pharmacological feature of anta-gonizing the dopamine (DA) D2 receptors (D2Rs). These receptors are abundant in the striatum where they are found in half of striatal medium-sized spiny neurons (MSNs) and in cholinergic interneurons but also on terminals of projecting DA-neurons [1,2].
D2R-MSNs represent the main cell type through which antipsychotics (i.e., haloperidol, raclopride, eticlopride, sulpiride) can lead to extrapyramidal and motor side effects such as hypolocomotion, catalepsy, parkinsonism and tardive dyskinesia [3,4]. A large body of evidence indicates that D2R antagonists, by blocking/preventing the DA→D2R→Gi (inhibitory G protein-coupled receptor)-mediated tonic inhibition of D2R-MSNs, promote the activation/disinhibition of intracellular signaling events through the recruitment of multiple pathways, including the cAMP-dependent protein kinase A (PKA)/dopamine- and cAMP-regulated phosphoprotein (DARPP-32) and the mTOR cascades [5,6,7,8,9], which participate in the regulation of both transcriptional and translational modifications. However, although blockade of the endogenous action of DA onto D2R is necessary to promote the activation of signaling cascades in D2R-MSNs, several reports have also shown that D2R downstream intracellular signaling events (i.e., cAMP/PKA pathway) also depend on the dynamic orchestration of several extracellular and intracellular players whose activity may scale the modulation of D2R-containing neurons [7,8,9,10,11,12,13], thus reflecting the nature of MSNs as coincidence detectors of different neurochemical stimuli. Within the striatum, this antipsychotics-associated signaling cascade rapidly culminates in the long-term expression of immediate early genes (IEGs), such as cFos, Arc and Zif268 [14].
IEGs represent a heterogenous class of highly responsive genes that can be rapidly and transiently induced by a plethora of physiological, pharmacological and environmental stimuli. The encoded proteins of IEGs cFos, Arc and Zif268 are well known to contribute to forms of synaptic plasticity [15]. Indeed, within the striatum, the study of DA transmission, DA-mediated signaling events and IEGs has been instrumental in shedding lights on the temporal and spatial organization of striatal territories as well as on the functions of striatal cell types, circuits and neuromodulatory systems [16,17,18,19,20,21,22,23,24,25]. However, whether and how multiple (extracellular and intracellular) signaling pathways converge on the regulation of haloperidol-induced IEGs in D2R-MSNs remain to be fully understood.
Here, by using transgenic animals, pharmacological approaches and immunofluorescence analyses, we investigated whether and how (i) non-DA neurotransmitters, notably glutamate (via NMDAR) and adenosine (via A2aR), and (ii) intracellular PKA/DARPP-32 and mTOR signaling pathways contribute to the regulation of haloperidol-induced IEGs in the striatum. We observed that NMDAR and A2aR as well as PKA/DARPP-32 and mTOR pathways are distinctly required and synergistically necessary to gate haloperidol-induced activation of D2R-MSNs. Our study, by further expanding the landscape of cellular and molecular modifications elicited by antipsychotics, provide new evidence for the regulatory activity of D2R-MSNs.
2. Results
2.1. Haloperidol Induces Contrasting Cell Type-Specific Regulation of IEGs in the Dorsal Striatum
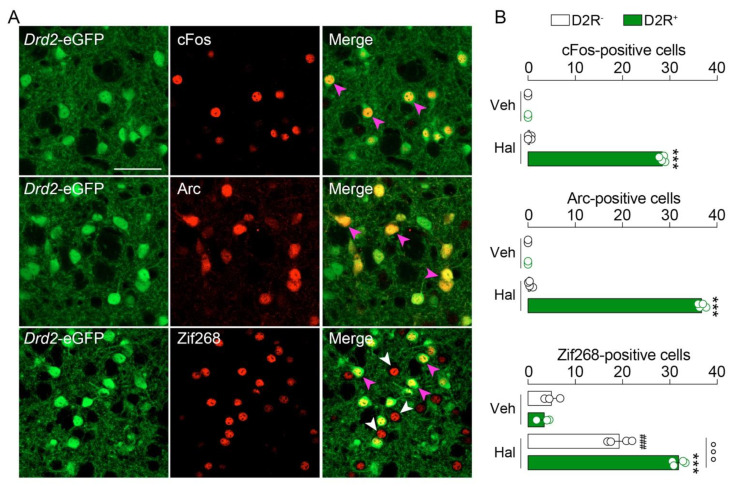
It is well established that haloperidol induces the expression of the IEGs cFos, Arc and Zif268 in the striatum [26,27,28,29,30,31]. Here, we took advantage of Drd2-eGFP mice [32] to visualize striatopallidal D2R+-neurons and revisit the cell type-specific expression patterns of cFos, Arc and Zif268 induced by haloperidol. As expected, an increase in cFos-, Arc- and Zif268-immunoreactive neurons was observed in the dorsal striatum 60 min after a single administration of haloperidol (0.5 mg/kg, ip) (Figure 1A).
Figure 1.
Haloperidol induces cFos, Arc and Zif268 in a cell type-specific manner in the mouse striatum. (A) Double immunofluorescence detection of cFos, Arc and Zif268 in the striatum of Drd2-eGFP mice 60 min after vehicle (Veh) or haloperidol (Hal) administration. Arrows in magenta indicate the expression of immediate early genes (IEGs) in D2R+-neurons, whereas arrows in white indicate the expression of IEGs in D2R--neurons. Scale bar: 50 μm. Note: given the low number of IEGs-positive neurons in Veh-treated mice, pictures are not shown. (B) Quantification of cFos, Arc and Zif268 in both D2R+- and D2R−-neurons. Statistics: *** p < 0.001 (Hal vs. Veh in D2R+-neurons), ### p < 0.001 (Hal vs. Veh in D2R−-neurons), °°° p < 0.001 (Hal in D2R+-neurons vs. Hal in D2R−-neurons for Zif268). Veh (n = 3) and Hal (n = 4). One-way ANOVA: F(3, 10) = 5301, p < 0.0001 (cFos); F(3, 10) = 5618, p < 0.0001 (Arc); F(3, 10) = 180.7, p < 0.0001 (Zif268).
Cell type-specific analysis revealed that cFos and Arc were exclusively triggered in striatopallidal D2R+-neurons (Figure 1A,B). In contrast, Zif268 was increased in both D2R--neurons (putative striatonigral neurons) and striatopallidal D2R+-neurons (Figure 1A,B), although Zif268+/D2R+-neurons outnumbered Zif268+/D2R--neurons (Figure 1A,B). This first set of results indicates that cFos and Arc, but not Zif268, can be used as bonafide markers to study long-term cellular and molecular events induced by haloperidol in striatopallidal neurons.
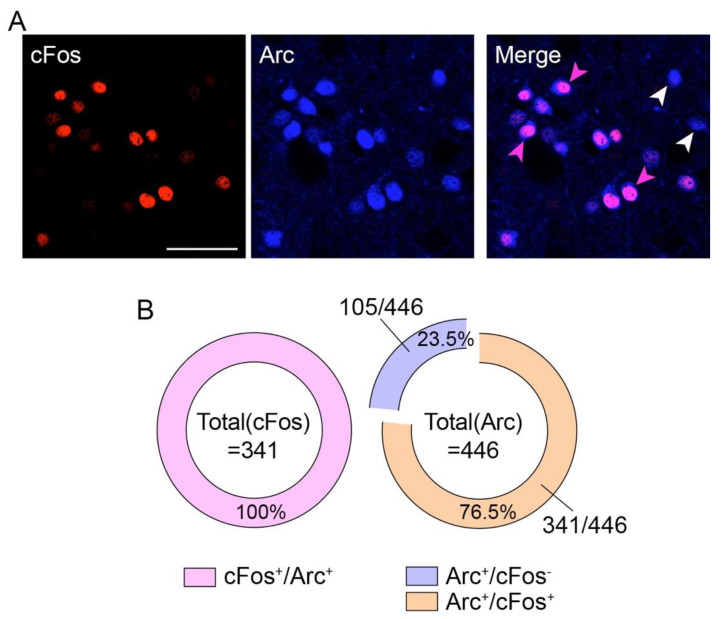
Next, we wondered whether the induction of cFos and Arc spatially occurred in the same or different subpopulations of D2R+-neurons. Thus, we performed a double immunofluorescence analysis for cFos and Arc. We observed a complete colocalization (341 out of 341 neurons, 100%) of cFos with Arc (Figure 2A,B). However, we also observed that among all Arc+-neurons, 23.5% (105 out of 446 neurons) did not express cFos (Figure 2A,B), therefore indicating that haloperidol-induced cellular modifications may occur at different spatial scales.
Figure 2.
Spatiocellular organization of haloperidol-induced cFos and Arc. (A) Double immunofluorescence detection of cFos (red) and Arc (blue) following haloperidol administration. Scale bar: 50 μm. Arrows in magenta indicate the co-expression of cFos and Arc in the same neurons, whereas arrows in white indicate the expression of Arc (no cFos co-expression). (B) Quantification of the degree of colocalization between cFos and Arc. Note that 23.5% of Arc+-neurons did not express cFos.
2.2. Haloperidol-Induced cFos and Arc Require the Activation of A2a and NMDA Receptors
Next, we investigated the contribution of non-DA receptors in the regulation of haloperidol-induced cFos and Arc (Figure 1). We focused on A2a (highly enriched in striatopallidal neurons [33]) and NMDA receptors as they strongly contribute to the regulation of the striatopallidal neurons’ activity and plasticity [34,35].
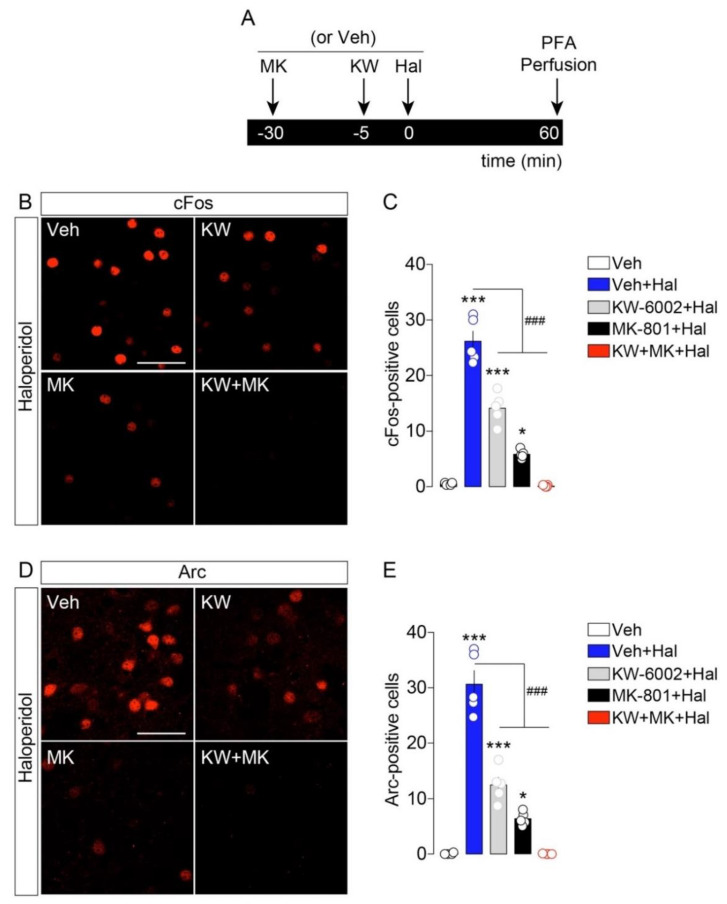
We observed that pretreatment with the specific A2aR antagonist KW-6002 (3 mg/kg [8]) significantly reduced haloperidol-induced cFos expression in the striatum (Figure 3A–C). In addition, when mice were pretreated with the NMDAR antagonist MK-801 (0.1 mg/kg), we noticed a dramatic reduction in haloperidol-induced cFos activation (Figure 3A–C). However, both A2aR and NMDAR blockades failed in fully preventing cFos expression in haloperidol-treated mice. Interestingly, the co-administration of KW-6002 and MK-801 before haloperidol injection resulted in a complete loss of cFos activation (Figure 3A–C). Similar regulatory mechanisms were observed when Arc was used as a molecular proxy of the haloperidol-induced activation of striatopallidal neurons. In fact, while KW-6002 and MK-801 distinctly reduced haloperidol-induced Arc expression (Figure 3D,E), the co-administration of both A2aR and NMDAR antagonists completely prevented the cellular/molecular response of striatopallidal neurons to haloperidol (Figure 3D,E).
Figure 3.
Haloperidol-induced cFos and Arc require the activation of A2a and NMDA receptors. (A) Temporal schedule of pharmacological treatments. (B) Immunofluorescence detection of cFos in the striatum of animals treated with vehicle + haloperidol (n = 5), KW-6002 (KW) + haloperidol (n = 5), MK-801 (MK) + haloperidol (n = 5) and KW-6002 (KW) + MK-801(MK) + haloperidol (n = 5). Note: given the low number of IEGs-positive neurons in Veh-treated mice, pictures are not shown. Scale bar: 50 μm. (C) Quantification of cFos+-neurons in all experimental groups. Statistics: * p < 0.05 and *** p < 0.001 (drugs vs. vehicle), ### p < 0.001 (KW-6002 + haloperidol and MK-801 + haloperidol vs. haloperidol). One-way ANOVA: F(4, 19) = 113.9, p < 0.0001. (D) Immunofluorescence detection of Arc in the striatum following pharmacological administrations. Scale bar: 50 μm. (E) Quantification of Arc+-neurons. Statistics: * p < 0.05 and *** p < 0.001 (drugs vs. vehicle), ### p < 0.001 (KW-6002 + haloperidol and MK-801 + haloperidol vs. haloperidol). One-way ANOVA: F(4, 19) = 90.46, p < 0.0001.
These results indicate that ambient adenosine and glutamate are necessary and act synergistically to gate the responsiveness of striatopallidal neurons to the antipsychotic haloperidol.
2.3. Haloperidol-Induced cFos and Arc Require the Involvement of PKA/DARPP-32 and mTOR Pathways
Haloperidol promotes the PKA-dependent phosphorylation of DARPP-32 on Thr34, which converts DARPP-32 into an inhibitor of protein phosphatase 1 (PP-1), thereby inhibiting the dephosphorylation of numerous cAMP/PKA-dependent molecular targets [36]. Indeed, at the intracellular level, A2aR and D2R oppositely regulate the cAMP/PKA/DARPP-32 pathway [7], and seminal reports have shown that the cellular modifications elicited by haloperidol depend on the recruitment of key intracellular signaling cascades such as the PKA/DARPP-32 and mTOR pathways [7,8,9,37]. Here, we decided to investigate whether these two pathways were, distinctly and/or synergistically, involved in the regulation of haloperidol-induced IEGs.
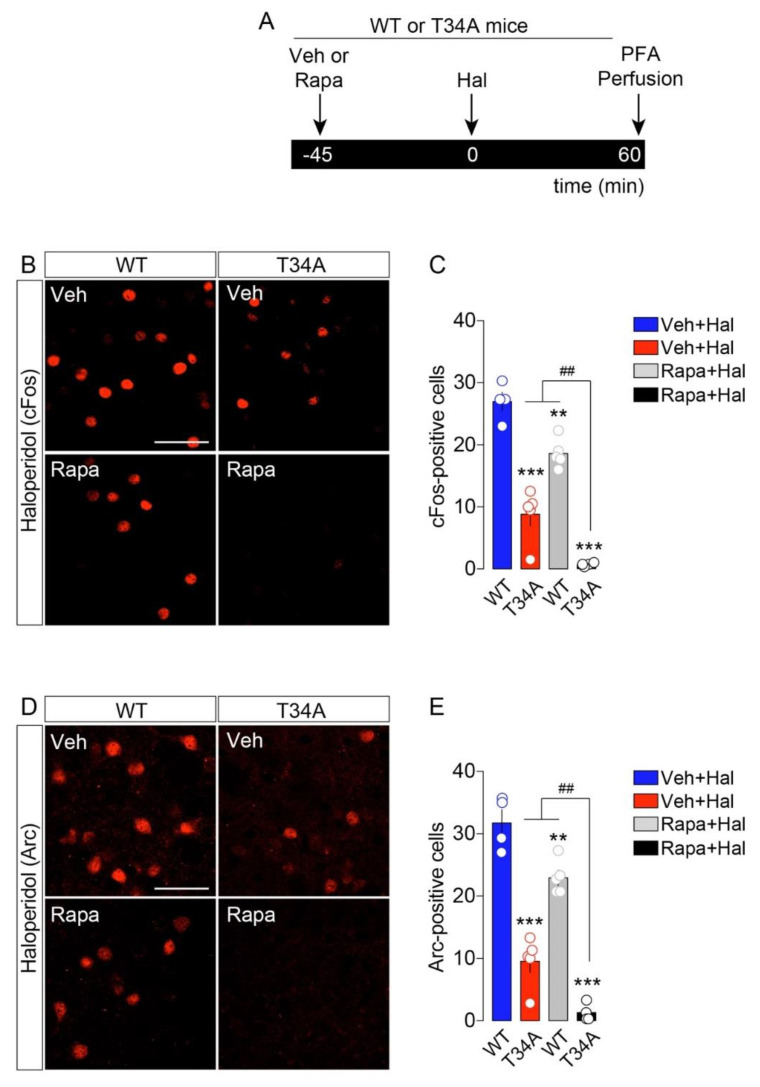
To dampen the PKA/DARPP-32 striatal path in vivo, we used DARPP-32 mutant mice in which Thr34 was replaced by Ala (T34A) [38]. Compared to WT mice, T34A mutant mice showed reduced cFos and Arc activation following haloperidol administration (Figure 4A–E). To inhibit the mTOR signaling pathway, mice were pretreated with rapamycin (5 mg/kg, [9]). As shown in Figure 4, rapamycin reduced haloperidol-induced cFos and Arc (Figure 4A–E). Interestingly, when both PKA/DARPP-32 and mTOR pathways were downregulated (rapamycin administration to T34A mutant mice), we observed a more pronounced reduction in cFos and Arc following haloperidol administration.
Figure 4.
Haloperidol-induced cFos and Arc require the intracellular activation of PKA/DARPP-32 and mTOR pathways. (A) Temporal schedule of pharmacological treatments. (B,D) Immunofluorescence detection of cFos (B) and Arc (D) in the striatum of WT and T34A animals treated with vehicle + haloperidol, or rapamycin + haloperidol. Scale bars: 50 μm. (C) Quantification of cFos+-neurons in WT and T34A mutant mice treated with vehicle + haloperidol and rapamycin + haloperidol (n = 4–5/group). Statistics: ** p < 0.01 and *** p < 0.001 (T34A + Hal, WT + Rapa + Hal, T34A + Rapa + Hal vs. WT + Hal), ## p < 0.01 (T34A + Rapa + Hal vs. T34A + Hal and WT + Rapa + Hal). One-way ANOVA: F(3, 14) = 62.67, p < 0.0001. (E) Quantification of Arc+-neurons in WT and T34A mutant mice treated with vehicle + haloperidol and rapamycin + haloperidol (n = 4–5/group). Statistics: ** p < 0.01 and *** p < 0.001 (T34A + Hal, WT + Rapa + Hal, T34A + Rapa + Hal vs. WT + Hal), ## p < 0.01 (T34A + Rapa + Hal vs. T34A + Hal and WT + Rapa + Hal). One-way ANOVA: F(3, 14) = 70.07, p < 0.0001.
These results indicate that intracellular cAMP/PKA and mTOR pathways are both synergistically mobilized and required for the full cellular/molecular action of haloperidol onto striatopallidal neurons.
3. Discussion
In this study we show that the typical antipsychotic haloperidol, which alters the activity and plasticity of D2R-MSNs [39,40], elicits cell type-specific activation of IEGs in the mouse striatum (D1R-MSNs vs. D2R-MSNs) and that this activation requires the contribution of different signaling actors. Here, we focused on cFos, Arc and Zif268 which, by representing the result of long-term cellular/molecular adaptations, are dynamically triggered by a plethora of stimuli and are also involved in the regulation of several neuronal functions [41,42,43,44]. We observed that the haloperidol-induced expression of the IEGs cFos and Arc was exclusively restricted to striatopallidal D2R+-neurons, whereas Zif268 expression was triggered in both D2R--neurons (putative striatonigral D1R-MSNs) and striatopallidal neurons (D2R-MSNs). These findings are in line with and further extend previous observations on haloperidol-regulated phospho-proteins (histone H3, ribosomal protein S6), highlighting the cell type-specific reactivity of MSNs to DA-related agents [7,8,18,19]. However, the cell type-unspecific expression of Zif268 in the striatal MSNs suggests that haloperidol, most likely through an indirect mechanism involving striatal cholinergic and/or GABAergic interneurons [45,46], may also regulate the activity of D1R-MSNs even though no major changes in the electrophysiological profile of this cell type have been observed [40]. In this study, we focused on the rostral segment of the dorsal striatum. However, the striatum extends throughout a rostro-caudal axis with major differences in the topographic and functional organization of striatal domains and cell types [17,22,24,47,48]. Indeed, it will be of high interest to explore whether and how antipsychotics impact on the regulatory functions of caudal striatal domains.
In addition to the selective induction of cFos and Arc in striatopallidal neurons following haloperidol administration, we noticed that cFos+/D2R+-neurons seemed to represent a subpopulation of Arc+/D2R+-neurons. This is of interest in light of recent reports describing that the two major striatal cell populations (D1R- and D2R-MSNs) may actually consist of different subpopulations with distinct spatiocellular and spatiomolecular features [49,50,51,52]. Indeed, the use of unbiased high-throughput technologies, either at the single cell or population level, will be instrumental to reappraise the functional heterogeneity of striatal neurons.
The therapeutic action as well as the side effects of antipsychotics strongly depend on the pharmacological blockade of D2R. However, other neurotransmitters participate in regulating the cellular activity of D2R-containing neurons and consequently scale the behavioral effects of haloperidol (i.e., catalepsy). Adenosine and glutamate represent two of the major neuromodulators/neurotransmitters able to regulate the activity of MSNs, and seminal reports have shown that their respective receptors, A2aR and NMDAR, distinctly influence haloperidol-associated effects. In fact, the pharmacological administration of A2aR antagonists and/or genetic deletion of A2aR counteract haloperidol-associated behaviors [53,54,55]. This is in line with our observation showing that the blockade of A2aR was sufficient to partially blunt haloperidol-induced cFos and Arc expression in the striatum. This action is mainly due to the opposite regulation exerted on D2R-MSNs by A2aR and D2R, which are positively (via Gs) and negatively (via Gi) coupled to the adenylyl cyclase, respectively. While the A2aR and D2R downstream signaling events may buffer the intracellular production of cAMP, several reports have also indicated that A2aR and D2R can heterodimerize (protein–protein interaction) at the membrane levels, therefore influencing the activity of each receptor [56,57,58,59,60,61].
In addition to ambient striatal adenosine, the excitatory neurotransmitter glutamate, mostly released from cortico-striatal and thalamo-striatal projections, is another key player in the regulation of MSNs. Seminal studies have shown that the pharmacological blockade of NMDAR was sufficient to blunt haloperidol-induced catalepsy [62,63,64], and our study provides further evidence that NMDARs are required for haloperidol-induced cFos [65,66] and Arc in the striatum. Indeed, NMDARs can gate the action of haloperidol (D2R) through multiple mechanisms. First, the activation of NMDAR can boost the activation of the cAMP/PKA cascade via an indirect A2aR-dependent mechanism [67]. Second, haloperidol-induced cAMP/PKA activity can lead to the PKA-dependent phosphorylation of NMDAR subunits, thus facilitating glutamatergic transmission [68]. Third, recent reports have shown that dopamine receptors can also heterodimerize with NMDARs [69,70,71]. Fourth, the blockade of NMDAR may also counteract the D2R-dependent modulation of cortico-striatal glutamate transmission [72,73]. Therefore, NMDAR antagonists may blunt haloperidol-elicited striatal IEGs through all these mechanisms.
However, our study also shows that while the blockade of A2aR or NMDAR blunted haloperidol-induced IEGs, the co-administration of A2aR and NMDAR antagonists (KW-6002 and MK-801, respectively) resulted in the full abolishment of cFos and Arc. These results indicate that to modulate striatal networks, haloperidol requires the dynamic and synergistic action of dopamine (D2R), adenosine (A2aR) and glutamate (NMDAR).
At the intracellular molecular level, haloperidol mobilizes the PKA/DARPP-32 cascade as well as the mTOR signaling pathway [7,8,9,37,74,75]. Indeed, the downregulation of the PKA/DARPP-32 [76] and mTOR [75] pathways dampened haloperidol-induced catalepsy. In line with these reports, we observed a reduction in cFos and Arc when haloperidol was administered to DARPP-32 T34A mutant mice (inhibition of PKA/DARPP-32 cascade) and also when it was preceded by the injection of rapamycin (inhibition of mTOR). However, we also noticed that when both signaling paths were downregulated (rapamycin administration to T34A mice), haloperidol completely failed to induce cFos and Arc expression in the striatum, therefore indicating that both signaling cascades are necessary and required for the full action of haloperidol. It is interesting to note that beside the antagonistic functions of A2aR and D2R on the cAMP/PKA/DARPP-32 pathway, NMDAR have also been associated to the downstream activation of the mTOR pathway [77,78,79], thus indicating that the converging contribution of these two intracellular signaling cascades may actually reflect the dynamic involvement of extracellular adenosine and glutamate in mediating the D2R-dependent action of haloperidol in striatopallidal neurons. Indeed, our results describing the dynamic regulation of striatal IEGs represent also a call for the use of modern high-throughput quantitative technologies to deeply investigate the cell type-specific adaptations elicited by antipsychotics.
In conclusion, our study, by confirming and expanding previous observations and also by providing a new synergic perspective of striatal regulatory mechanisms, highlights the heterogenous complexity of in vivo processes which may be involved in the therapeutic and adverse effects of antipsychotics.
4. Material and Methods
4.1. Animals
For all experiments, 8–12-week-old mice were used. Male C57BL/6J mice (25–30 g) were purchased from Taconic (Tornbjerg, Denmark). Bacterial artificial chromosome transgenic mice expressing eGFP under the control of the promoter for the D2R (Drd2-eGFP) were generated by the GENSAT program (Gene Expression Nervous System Atlas) at the Rockefeller University [80] and backcrossed on a C57BL/6J background. Knock-in mice expressing a mutated form of DARPP-32, in which the threonine (Thr34) is replaced by an alanine (DARPP-32 T34A mutant mice), were generated as previously described [38] and backcrossed on a C57BL/6J background. Animals were maintained in a 12 h light–dark cycle at a stable temperature of 22 °C, with food and water ad libitum. To reduce the stressogenic component of in vivo manipulations, before any pharmacological experimentation, mice were handled and injected with saline for three consecutive days. The experiments were conducted in accordance with the guidelines of the Research Ethics Committee of Karolinska Institutet, Swedish Animal Welfare Agency and the 2010/63/EU directive for the care and use of experimental animals.
4.2. Drugs
Haloperidol (0.5 mg/kg, Sigma-Aldrich, St. Louis, MO, USA) was dissolved in saline containing 0.05% (v/v) acetic acid with the pH adjusted to 6.0 with 1 M NaOH, and it was injected 60 min before perfusion. The A2aR antagonist KW-6002 (also known as istradefylline, 3 mg/kg, [8]), a gift from Dr. Edilio Borroni (Hoffmann-LaRoche, Basel, Switzerland), was suspended by sonication in a solution of 5% (v/v) Tween 80 in saline and administered 5 min before haloperidol as previously reported [8]. The NMDAR antagonist MK-801 (also known as dizocilpine, 0.1 mg/kg, Tocris, Bristol, UK) was dissolved in saline and administered 30 min before haloperidol, which is in line with previous reports [17,81,82]. Rapamycin (5 mg/kg, LC Laboratories, Woburn, MA, USA) was dissolved in a solution of 5% (v/v) dimethylsulfoxide (DMSO), 5% Tween-20 and 15% (v/v) PEG-400, and administered (once per day) starting 3 days before the experiment. On the day of the experiment, rapamycin was injected 45 min before haloperidol as previously reported [9]. All drugs were administered intraperitoneally (i.p.) in a volume of 10 mL/kg, except for rapamycin (mTOR inhibitor), which was administered in a volume of 5 mL/kg. When mice were not treated with drugs, they received an equivalent volume of the corresponding vehicle.
4.3. Tissue Preparation and Immunofluorescence
Tissues were prepared as previously described [17]. In brief, mice were rapidly anaesthetized by i.p. injection of pentobarbital (500 mg/kg, Sanofi-Aventis, Paris, France) prior to intracardiac perfusion of 4% (w/v) paraformaldehyde (PFA) in 0.1 M Na2HPO4/NaH2PO4 buffer (pH 7.5), which was delivered with a peristaltic pump at 20 mL/min over 5 min. Brains were post-fixed overnight in the same solution and stored at 4 °C.
Thirty μm thick sections were cut with a vibratome (Leica, France) and stored at −20°C in a solution containing 30% (v/v) ethylene glycol, 30% (v/v) glycerol, and 0.1 M sodium phosphate buffer until they were processed for immunofluorescence.
Sections were processed as follows: free-floating sections were rinsed three times for 10 min in Tris-buffered saline (TBS, 50 mM Tris–HCL, 150 mM NaCl, pH 7.5). After 15 min of incubation in 0.2% (v/v) Triton X-100 in TBS, sections were rinsed in TBS again and blocked for 1 h in a solution of 3% BSA in TBS. Sections were then incubated for 72 h at 4 °C in 1% BSA, 0.15% Triton X-100 with the primary antibodies. Antibodies for cFos (1∶400, #sc-52), Arc (1∶400, #sc-17839), and Zif268 (1∶400, #sc-189) were purchased from Santa Cruz Biotechnology [83]. GFP was amplified by using a chicken anti-GFP (1:1000, Invitrogen/ThermoFisher Scientific, Waltham, MA, USA). Sections were rinsed three times for 10 min in TBS and incubated for 45 min with goat Cy3-, Cy5-coupled (1:400, Jackson Immunoresearch, Cambridge House, St. Thomas’ Place, UK), and/or goat A488 (1:400, Invitrogen/ThermoFisher Scientific, Waltham, MA, USA) secondary antibodies. Sections were rinsed for 10 min twice in TBS and twice in Tris-buffer (1 M, pH 7.5) before mounting in a 1,4-diazabicyclo-[2.2.2]-octane (DABCO, Sigma-Aldrich) solution.
4.4. Confocal Microscopy and Image Analysis
Single and/or double-immunolabeled images from each region of interest (dorsal striatum) were obtained using sequential laser scanning confocal microscopy (Zeiss LSM510 META, Oberkochen, Germany). Images were acquired at the level of the dorsal striatum (rostral level). Photomicrographs were obtained with the following band-pass and long-pass filter setting: GFP (band pass filter: 505–530), Cy3 (band-pass filter: 560–615) and Cy5 (long-pass filter 650).
Quantifications were performed in 325.75 µm × 325.75 µm confocal images. Immunofluorescent striatal cells (expressing IEGs and/or eGFP) were counted (absolute number) blindly of the treatment/group by using the cell counter plugin of the ImageJ software taking as standard reference a fixed threshold of fluorescence. Of note, the distinction between striatal cell types (Figure 1) was performed using Drd2-eGFP mice (positive vs. negative neurons) [32,80].
4.5. Statistical Analysis
All statistical comparisons were performed with two-sided tests in Prism 6 (GraphPad Software, La Jolla, CA, USA). The distribution of data was determined with a Shapiro–Wilk normality test. No sample size calculations were performed. To determine outliers in every experimental group, we performed the Grubbs’ test in Prism. No outliers were identified. All the data were analyzed using either Student’s t-test with equal variances or one-way ANOVA. In all cases, the significance threshold was automatically set at p < 0.05. The one-way ANOVA analysis, where treatment was the independent variable, was followed by a Bonferroni post hoc test for specific comparisons only when the overall ANOVA revealed a significant difference (at least p < 0.05) among groups. All the values and statistical analyses are reported in the figure legends.
Author Contributions
Conceptualization, E.V., G.F. and G.G.; Data curation, O.O.; Formal analysis, O.O. and G.G.; Funding acquisition, E.V., G.F. and G.G.; Investigation, O.O., E.V., G.F. and G.G.; Methodology, O.O. and G.G.; Project administration, G.G.; Resources, E.V., G.F. and G.G.; Supervision, G.G.; Writing—original draft, G.G.; Writing—review & editing, O.O., E.V., G.F. and G.G. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the guidelines of the Research Ethics Committee of the Karolinska Institutet, Swedish Animal Welfare Agency and the 2010/63/EU directive for the care and use of experimental animals.
Informed Consent Statement
Not Applicable.
Data availability Statement
The data presented in this study are available in the Figures and Results sections.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This work was supported by Agence Nationale de la Recherche (HERO, ANR-21-CE14-0021-01, G.G.), Fédération pour la Recherche sur le Cerveau and Association France Parkinson (G.G.), Université Paris Cité (G.G.), Inserm (E.V.), Fondation pour la Recherche Médicale (EQU202203014705, E.V.), Agence Nationale de la Recherche (DISCOMMODE, ANR-21-CE37-0013 and SubDOPA, ANR-21-CE16-0028, E.V.). Swedish Research Council (Grant 2019-01170, G.F.). O.O. was supported by a doctoral fellowship from the Fondation pour la Recherche Médicale.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Gallo E.F. Disentangling the Diverse Roles of Dopamine D2 Receptors in Striatal Function and Behavior. Neurochem. Int. 2019;125:35–46. doi: 10.1016/j.neuint.2019.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gerfen C.R., Surmeier D.J. Modulation of Striatal Projection Systems by Dopamine. Annu. Rev. Neurosci. 2011;34:441–466. doi: 10.1146/annurev-neuro-061010-113641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sykes D.A., Moore H., Stott L., Holliday N., Javitch J.A., Lane J.R., Charlton S.J. Extrapyramidal Side Effects of Antipsychotics Are Linked to Their Association Kinetics at Dopamine D2 Receptors. Nat. Commun. 2017;8:763. doi: 10.1038/s41467-017-00716-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Factor S.A., Burkhard P.R., Caroff S., Friedman J.H., Marras C., Tinazzi M., Comella C.L. Recent Developments in Drug-Induced Movement Disorders: A Mixed Picture. Lancet Neurol. 2019;18:880–890. doi: 10.1016/S1474-4422(19)30152-8. [DOI] [PubMed] [Google Scholar]
- 5.Konradi C., Heckers S. Haloperidol-Induced Fos Expression in Striatum Is Dependent upon Transcription Factor Cyclic AMP Response Element Binding Protein. Neuroscience. 1995;65:1051–1061. doi: 10.1016/0306-4522(94)00546-H. [DOI] [PubMed] [Google Scholar]
- 6.Li J., Guo Y., Schroeder F.A., Youngs R.M., Schmidt T.W., Ferris C., Konradi C., Akbarian S. Dopamine D2-like Antagonists Induce Chromatin Remodeling in Striatal Neurons through Cyclic AMP-Protein Kinase A and NMDA Receptor Signaling. J. Neurochem. 2004;90:1117–1131. doi: 10.1111/j.1471-4159.2004.02569.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bertran-Gonzalez J., Håkansson K., Borgkvist A., Irinopoulou T., Brami-Cherrier K., Usiello A., Greengard P., Hervé D., Girault J.-A., Valjent E., et al. Histone H3 Phosphorylation Is under the Opposite Tonic Control of Dopamine D2 and Adenosine A2A Receptors in Striatopallidal Neurons. Neuropsychopharmacology. 2009;34:1710–1720. doi: 10.1038/npp.2008.228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Valjent E., Bertran-Gonzalez J., Bowling H., Lopez S., Santini E., Matamales M., Bonito-Oliva A., Hervé D., Hoeffer C., Klann E., et al. Haloperidol Regulates the State of Phosphorylation of Ribosomal Protein S6 via Activation of PKA and Phosphorylation of DARPP-32. Neuropsychopharmacology. 2011;36:2561–2570. doi: 10.1038/npp.2011.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bonito-Oliva A., Pallottino S., Bertran-Gonzalez J., Girault J.-A., Valjent E., Fisone G. Haloperidol Promotes MTORC1-Dependent Phosphorylation of Ribosomal Protein S6 via Dopamine- and CAMP-Regulated Phosphoprotein of 32 KDa and Inhibition of Protein Phosphatase-1. Neuropharmacology. 2013;72:197–203. doi: 10.1016/j.neuropharm.2013.04.043. [DOI] [PubMed] [Google Scholar]
- 10.Yamaguchi T., Goto A., Nakahara I., Yawata S., Hikida T., Matsuda M., Funabiki K., Nakanishi S. Role of PKA Signaling in D2 Receptor-Expressing Neurons in the Core of the Nucleus Accumbens in Aversive Learning. Proc. Natl. Acad. Sci. USA. 2015;112:11383–11388. doi: 10.1073/pnas.1514731112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhang X., Nagai T., Ahammad R.U., Kuroda K., Nakamuta S., Nakano T., Yukinawa N., Funahashi Y., Yamahashi Y., Amano M., et al. Balance between Dopamine and Adenosine Signals Regulates the PKA/Rap1 Pathway in Striatal Medium Spiny Neurons. Neurochem. Int. 2019;122:8–18. doi: 10.1016/j.neuint.2018.10.008. [DOI] [PubMed] [Google Scholar]
- 12.Ghiglieri V., Napolitano F., Pelosi B., Schepisi C., Migliarini S., Di Maio A., Pendolino V., Mancini M., Sciamanna G., Vitucci D., et al. Rhes Influences Striatal CAMP/PKA-Dependent Signaling and Synaptic Plasticity in a Gender-Sensitive Fashion. Sci. Rep. 2015;5:10933. doi: 10.1038/srep10933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Beggiato S., Tomasini M.C., Borelli A.C., Borroto-Escuela D.O., Fuxe K., Antonelli T., Tanganelli S., Ferraro L. Functional Role of Striatal A2A, D2, and MGlu5 Receptor Interactions in Regulating Striatopallidal GABA Neuronal Transmission. J. Neurochem. 2016;138:254–264. doi: 10.1111/jnc.13652. [DOI] [PubMed] [Google Scholar]
- 14.de Bartolomeis A., Marmo F., Buonaguro E.F., Rossi R., Tomasetti C., Iasevoli F. Imaging Brain Gene Expression Profiles by Antipsychotics: Region-Specific Action of Amisulpride on Postsynaptic Density Transcripts Compared to Haloperidol. Eur. Neuropsychopharmacol. 2013;23:1516–1529. doi: 10.1016/j.euroneuro.2012.11.014. [DOI] [PubMed] [Google Scholar]
- 15.Minatohara K., Akiyoshi M., Okuno H. Role of Immediate-Early Genes in Synaptic Plasticity and Neuronal Ensembles Underlying the Memory Trace. Front. Mol. Neurosci. 2015;8:78. doi: 10.3389/fnmol.2015.00078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gonzales B.J., Mukherjee D., Ashwal-Fluss R., Loewenstein Y., Citri A. Subregion-Specific Rules Govern the Distribution of Neuronal Immediate-Early Gene Induction. Proc. Natl. Acad. Sci. USA. 2020;117:23304–23310. doi: 10.1073/pnas.1913658116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gangarossa G., Castell L., Castro L., Tarot P., Veyrunes F., Vincent P., Bertaso F., Valjent E. Contrasting Patterns of ERK Activation in the Tail of the Striatum in Response to Aversive and Rewarding Signals. J. Neurochem. 2019;151:204–226. doi: 10.1111/jnc.14804. [DOI] [PubMed] [Google Scholar]
- 18.Gangarossa G., Perroy J., Valjent E. Combinatorial Topography and Cell-Type Specific Regulation of the ERK Pathway by Dopaminergic Agonists in the Mouse Striatum. Brain Struct. Funct. 2013;218:405–419. doi: 10.1007/s00429-012-0405-6. [DOI] [PubMed] [Google Scholar]
- 19.Bertran-Gonzalez J., Bosch C., Maroteaux M., Matamales M., Hervé D., Valjent E., Girault J.-A. Opposing Patterns of Signaling Activation in Dopamine D1 and D2 Receptor-Expressing Striatal Neurons in Response to Cocaine and Haloperidol. J. Neurosci. 2008;28:5671–5685. doi: 10.1523/JNEUROSCI.1039-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Savell K.E., Tuscher J.J., Zipperly M.E., Duke C.G., Phillips R.A., Bauman A.J., Thukral S., Sultan F.A., Goska N.A., Ianov L., et al. A Dopamine-Induced Gene Expression Signature Regulates Neuronal Function and Cocaine Response. Sci. Adv. 2020;6:eaba4221. doi: 10.1126/sciadv.aba4221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.van Elzelingen W., Goedhoop J., Warnaar P., Denys D., Arbab T., Willuhn I. A Unidirectional but Not Uniform Striatal Landscape of Dopamine Signaling for Motivational Stimuli. Proc. Natl. Acad. Sci. USA. 2022;119:e2117270119. doi: 10.1073/pnas.2117270119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gangarossa G., Espallergues J., Mailly P., De Bundel D., de Kerchove d’Exaerde A., Hervé D., Girault J.-A., Valjent E., Krieger P. Spatial Distribution of D1R- and D2R-Expressing Medium-Sized Spiny Neurons Differs along the Rostro-Caudal Axis of the Mouse Dorsal Striatum. Front. Neural Circuits. 2013;7:124. doi: 10.3389/fncir.2013.00124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Surmeier D.J., Plotkin J., Shen W. Dopamine and Synaptic Plasticity in Dorsal Striatal Circuits Controlling Action Selection. Curr. Opin. Neurobiol. 2009;19:621–628. doi: 10.1016/j.conb.2009.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Valjent E., Gangarossa G. The Tail of the Striatum: From Anatomy to Connectivity and Function. Trends Neurosci. 2021;44:203–214. doi: 10.1016/j.tins.2020.10.016. [DOI] [PubMed] [Google Scholar]
- 25.Gangarossa G., Espallergues J., de Kerchove d’Exaerde A., El Mestikawy S., Gerfen C.R., Hervé D., Girault J.-A., Valjent E. Distribution and Compartmental Organization of GABAergic Medium-Sized Spiny Neurons in the Mouse Nucleus Accumbens. Front. Neural Circuits. 2013;7:22. doi: 10.3389/fncir.2013.00022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nguyen T.V., Kosofsky B.E., Birnbaum R., Cohen B.M., Hyman S.E. Differential Expression of C-Fos and Zif268 in Rat Striatum after Haloperidol, Clozapine, and Amphetamine. Proc. Natl. Acad. Sci. USA. 1992;89:4270–4274. doi: 10.1073/pnas.89.10.4270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Robertson G.S., Matsumura H., Fibiger H.C. Induction Patterns of Fos-like Immunoreactivity in the Forebrain as Predictors of Atypical Antipsychotic Activity. J. Pharmacol. Exp. Ther. 1994;271:1058–1066. [PubMed] [Google Scholar]
- 28.Polese D., de Serpis A.A., Ambesi-Impiombato A., Muscettola G., de Bartolomeis A. Homer 1a Gene Expression Modulation by Antipsychotic Drugs: Involvement of the Glutamate Metabotropic System and Effects of D-Cycloserine. Neuropsychopharmacology. 2002;27:906–913. doi: 10.1016/S0893-133X(02)00371-8. [DOI] [PubMed] [Google Scholar]
- 29.de Bartolomeis A., Iasevoli F., Marmo F., Buonaguro E.F., Eramo A., Rossi R., Avvisati L., Latte G., Tomasetti C. Progressive Recruitment of Cortical and Striatal Regions by Inducible Postsynaptic Density Transcripts after Increasing Doses of Antipsychotics with Different Receptor Profiles: Insights for Psychosis Treatment. Eur. Neuropsychopharmacol. 2015;25:566–582. doi: 10.1016/j.euroneuro.2015.01.003. [DOI] [PubMed] [Google Scholar]
- 30.Samaha A.-N., Reckless G.E., Seeman P., Diwan M., Nobrega J.N., Kapur S. Less Is More: Antipsychotic Drug Effects Are Greater with Transient Rather than Continuous Delivery. Biol. Psychiatry. 2008;64:145–152. doi: 10.1016/j.biopsych.2008.01.010. [DOI] [PubMed] [Google Scholar]
- 31.Fumagalli F., Frasca A., Racagni G., Riva M.A. Antipsychotic Drugs Modulate Arc Expression in the Rat Brain. Eur. Neuropsychopharmacol. 2009;19:109–115. doi: 10.1016/j.euroneuro.2008.09.001. [DOI] [PubMed] [Google Scholar]
- 32.Valjent E., Bertran-Gonzalez J., Hervé D., Fisone G., Girault J.-A. Looking BAC at Striatal Signaling: Cell-Specific Analysis in New Transgenic Mice. Trends Neurosci. 2009;32:538–547. doi: 10.1016/j.tins.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 33.Schiffmann S.N., Fisone G., Moresco R., Cunha R.A., Ferré S. Adenosine A2A Receptors and Basal Ganglia Physiology. Prog. Neurobiol. 2007;83:277–292. doi: 10.1016/j.pneurobio.2007.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Azdad K., Gall D., Woods A.S., Ledent C., Ferré S., Schiffmann S.N. Dopamine D2 and Adenosine A2A Receptors Regulate NMDA-Mediated Excitation in Accumbens Neurons through A2A-D2 Receptor Heteromerization. Neuropsychopharmacology. 2009;34:972–986. doi: 10.1038/npp.2008.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lambot L., Chaves Rodriguez E., Houtteman D., Li Y., Schiffmann S.N., Gall D., de Kerchove d’Exaerde A. Striatopallidal Neuron NMDA Receptors Control Synaptic Connectivity, Locomotor, and Goal-Directed Behaviors. J. Neurosci. 2016;36:4976–4992. doi: 10.1523/JNEUROSCI.2717-15.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Girault J.-A., Nairn A.C. DARPP-32 40 Years Later. Adv. Pharmacol. 2021;90:67–87. doi: 10.1016/bs.apha.2020.09.004. [DOI] [PubMed] [Google Scholar]
- 37.Bateup H.S., Svenningsson P., Kuroiwa M., Gong S., Nishi A., Heintz N., Greengard P. Cell Type-Specific Regulation of DARPP-32 Phosphorylation by Psychostimulant and Antipsychotic Drugs. Nat. Neurosci. 2008;11:932–939. doi: 10.1038/nn.2153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Svenningsson P., Tzavara E.T., Carruthers R., Rachleff I., Wattler S., Nehls M., McKinzie D.L., Fienberg A.A., Nomikos G.G., Greengard P. Diverse Psychotomimetics Act through a Common Signaling Pathway. Science. 2003;302:1412–1415. doi: 10.1126/science.1089681. [DOI] [PubMed] [Google Scholar]
- 39.Centonze D., Usiello A., Costa C., Picconi B., Erbs E., Bernardi G., Borrelli E., Calabresi P. Chronic Haloperidol Promotes Corticostriatal Long-Term Potentiation by Targeting Dopamine D2L Receptors. J. Neurosci. 2004;24:8214–8222. doi: 10.1523/JNEUROSCI.1274-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sebel L.E., Graves S.M., Chan C.S., Surmeier D.J. Haloperidol Selectively Remodels Striatal Indirect Pathway Circuits. Neuropsychopharmacology. 2017;42:963–973. doi: 10.1038/npp.2016.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.de Bartolomeis A., Buonaguro E.F., Latte G., Rossi R., Marmo F., Iasevoli F., Tomasetti C. Immediate-Early Genes Modulation by Antipsychotics: Translational Implications for a Putative Gateway to Drug-Induced Long-Term Brain Changes. Front. Behav. Neurosci. 2017;11:240. doi: 10.3389/fnbeh.2017.00240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Peebles C.L., Yoo J., Thwin M.T., Palop J.J., Noebels J.L., Finkbeiner S. Arc Regulates Spine Morphology and Maintains Network Stability in Vivo. Proc. Natl. Acad. Sci. USA. 2010;107:18173–18178. doi: 10.1073/pnas.1006546107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Grueter B.A., Robison A.J., Neve R.L., Nestler E.J., Malenka R.C. ∆FosB Differentially Modulates Nucleus Accumbens Direct and Indirect Pathway Function. Proc. Natl. Acad. Sci. USA. 2013;110:1923–1928. doi: 10.1073/pnas.1221742110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhang J., Zhang L., Jiao H., Zhang Q., Zhang D., Lou D., Katz J.L., Xu M. C-Fos Facilitates the Acquisition and Extinction of Cocaine-Induced Persistent Changes. J. Neurosci. 2006;26:13287–13296. doi: 10.1523/JNEUROSCI.3795-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yael D., Zeef D.H., Sand D., Moran A., Katz D.B., Cohen D., Temel Y., Bar-Gad I. Haloperidol-Induced Changes in Neuronal Activity in the Striatum of the Freely Moving Rat. Front. Syst. Neurosci. 2013;7:110. doi: 10.3389/fnsys.2013.00110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wiltschko A.B., Pettibone J.R., Berke J.D. Opposite Effects of Stimulant and Antipsychotic Drugs on Striatal Fast-Spiking Interneurons. Neuropsychopharmacology. 2010;35:1261–1270. doi: 10.1038/npp.2009.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Menegas W., Bergan J.F., Ogawa S.K., Isogai Y., Umadevi Venkataraju K., Osten P., Uchida N., Watabe-Uchida M. Dopamine Neurons Projecting to the Posterior Striatum Form an Anatomically Distinct Subclass. eLife. 2015;4:e10032. doi: 10.7554/eLife.10032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Menegas W., Akiti K., Amo R., Uchida N., Watabe-Uchida M. Dopamine Neurons Projecting to the Posterior Striatum Reinforce Avoidance of Threatening Stimuli. Nat. Neurosci. 2018;21:1421–1430. doi: 10.1038/s41593-018-0222-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tran M.N., Maynard K.R., Spangler A., Huuki L.A., Montgomery K.D., Sadashivaiah V., Tippani M., Barry B.K., Hancock D.B., Hicks S.C., et al. Single-Nucleus Transcriptome Analysis Reveals Cell-Type-Specific Molecular Signatures across Reward Circuitry in the Human Brain. Neuron. 2021;109:3088–3103.e5. doi: 10.1016/j.neuron.2021.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Puighermanal E., Castell L., Esteve-Codina A., Melser S., Kaganovsky K., Zussy C., Boubaker-Vitre J., Gut M., Rialle S., Kellendonk C., et al. Functional and Molecular Heterogeneity of D2R Neurons along Dorsal Ventral Axis in the Striatum. Nat. Commun. 2020;11:1957. doi: 10.1038/s41467-020-15716-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Märtin A., Calvigioni D., Tzortzi O., Fuzik J., Wärnberg E., Meletis K. A Spatiomolecular Map of the Striatum. Cell Rep. 2019;29:4320–4333.e5. doi: 10.1016/j.celrep.2019.11.096. [DOI] [PubMed] [Google Scholar]
- 52.Chen R., Blosser T.R., Djekidel M.N., Hao J., Bhattacherjee A., Chen W., Tuesta L.M., Zhuang X., Zhang Y. Decoding Molecular and Cellular Heterogeneity of Mouse Nucleus Accumbens. Nat. Neurosci. 2021;24:1757–1771. doi: 10.1038/s41593-021-00938-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Pardo M., Lopez-Cruz L., Valverde O., Ledent C., Baqi Y., Müller C.E., Salamone J.D., Correa M. Adenosine A2A Receptor Antagonism and Genetic Deletion Attenuate the Effects of Dopamine D2 Antagonism on Effort-Based Decision Making in Mice. Neuropharmacology. 2012;62:2068–2077. doi: 10.1016/j.neuropharm.2011.12.033. [DOI] [PubMed] [Google Scholar]
- 54.Varty G.B., Hodgson R.A., Pond A.J., Grzelak M.E., Parker E.M., Hunter J.C. The Effects of Adenosine A2A Receptor Antagonists on Haloperidol-Induced Movement Disorders in Primates. Psychopharmacology. 2008;200:393–401. doi: 10.1007/s00213-008-1214-8. [DOI] [PubMed] [Google Scholar]
- 55.Mott A.M., Nunes E.J., Collins L.E., Port R.G., Sink K.S., Hockemeyer J., Müller C.E., Salamone J.D. The Adenosine A2A Antagonist MSX-3 Reverses the Effects of the Dopamine Antagonist Haloperidol on Effort-Related Decision Making in a T-Maze Cost/Benefit Procedure. Psychopharmacology. 2009;204:103–112. doi: 10.1007/s00213-008-1441-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ferre S., von Euler G., Johansson B., Fredholm B.B., Fuxe K. Stimulation of High-Affinity Adenosine A2 Receptors Decreases the Affinity of Dopamine D2 Receptors in Rat Striatal Membranes. Proc. Natl. Acad. Sci. USA. 1991;88:7238–7241. doi: 10.1073/pnas.88.16.7238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Fuxe K., Ferré S., Zoli M., Agnati L.F. Integrated Events in Central Dopamine Transmission as Analyzed at Multiple Levels. Evidence for Intramembrane Adenosine A2A/Dopamine D2 and Adenosine A1/Dopamine D1 Receptor Interactions in the Basal Ganglia. Brain Res. Brain Res. Rev. 1998;26:258–273. doi: 10.1016/S0165-0173(97)00049-0. [DOI] [PubMed] [Google Scholar]
- 58.Prasad K., de Vries E.F.J., Elsinga P.H., Dierckx R.A.J.O., van Waarde A. Allosteric Interactions between Adenosine A2A and Dopamine D2 Receptors in Heteromeric Complexes: Biochemical and Pharmacological Characteristics, and Opportunities for PET Imaging. Int. J. Mol. Sci. 2021;22:1719. doi: 10.3390/ijms22041719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bonaventura J., Rico A.J., Moreno E., Sierra S., Sánchez M., Luquin N., Farré D., Müller C.E., Martínez-Pinilla E., Cortés A., et al. L-DOPA-Treatment in Primates Disrupts the Expression of A(2A) Adenosine-CB(1) Cannabinoid-D(2) Dopamine Receptor Heteromers in the Caudate Nucleus. Neuropharmacology. 2014;79:90–100. doi: 10.1016/j.neuropharm.2013.10.036. [DOI] [PubMed] [Google Scholar]
- 60.Bonaventura J., Navarro G., Casadó-Anguera V., Azdad K., Rea W., Moreno E., Brugarolas M., Mallol J., Canela E.I., Lluís C., et al. Allosteric Interactions between Agonists and Antagonists within the Adenosine A2A Receptor-Dopamine D2 Receptor Heterotetramer. Proc. Natl. Acad. Sci. USA. 2015;112:E3609–E3618. doi: 10.1073/pnas.1507704112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Agnati L.F., Ferré S., Lluis C., Franco R., Fuxe K. Molecular Mechanisms and Therapeutical Implications of Intramembrane Receptor/Receptor Interactions among Heptahelical Receptors with Examples from the Striatopallidal GABA Neurons. Pharmacol. Rev. 2003;55:509–550. doi: 10.1124/pr.55.3.2. [DOI] [PubMed] [Google Scholar]
- 62.Yoshida Y., Ono T., Kizu A., Fukushima R., Miyagishi T. Striatal N-Methyl-D-Aspartate Receptors in Haloperidol-Induced Catalepsy. Eur. J. Pharmacol. 1991;203:173–180. doi: 10.1016/0014-2999(91)90712-y. [DOI] [PubMed] [Google Scholar]
- 63.Moore N.A., Blackman A., Awere S., Leander J.D. NMDA Receptor Antagonists Inhibit Catalepsy Induced by Either Dopamine D1 or D2 Receptor Antagonists. Eur. J. Pharmacol. 1993;237:1–7. doi: 10.1016/0014-2999(93)90085-V. [DOI] [PubMed] [Google Scholar]
- 64.Kaur S., Ozer H., Starr M. MK 801 Reverses Haloperidol-Induced Catalepsy from Both Striatal and Extrastriatal Sites in the Rat Brain. Eur. J. Pharmacol. 1997;332:153–160. doi: 10.1016/S0014-2999(97)01078-9. [DOI] [PubMed] [Google Scholar]
- 65.de Souza I.E., Meredith G.E. NMDA Receptor Blockade Attenuates the Haloperidol Induction of Fos Protein in the Dorsal but Not the Ventral Striatum. Synapse. 1999;32:243–253. doi: 10.1002/(SICI)1098-2396(19990615)32:4<243::AID-SYN1>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- 66.Hussain N., Flumerfelt B.A., Rajakumar N. Glutamatergic Regulation of Haloperidol-Induced c-Fos Expression in the Rat Striatum and Nucleus Accumbens. Neuroscience. 2001;102:391–399. doi: 10.1016/S0306-4522(00)00487-5. [DOI] [PubMed] [Google Scholar]
- 67.Nash J.E., Brotchie J.M. A Common Signaling Pathway for Striatal NMDA and Adenosine A2a Receptors: Implications for the Treatment of Parkinson’s Disease. J. Neurosci. 2000;20:7782–7789. doi: 10.1523/JNEUROSCI.20-20-07782.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Leveque J.C., Macías W., Rajadhyaksha A., Carlson R.R., Barczak A., Kang S., Li X.M., Coyle J.T., Huganir R.L., Heckers S., et al. Intracellular Modulation of NMDA Receptor Function by Antipsychotic Drugs. J. Neurosci. 2000;20:4011–4020. doi: 10.1523/JNEUROSCI.20-11-04011.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Liu X.-Y., Chu X.-P., Mao L.-M., Wang M., Lan H.-X., Li M.-H., Zhang G.-C., Parelkar N.K., Fibuch E.E., Haines M., et al. Modulation of D2R-NR2B Interactions in Response to Cocaine. Neuron. 2006;52:897–909. doi: 10.1016/j.neuron.2006.10.011. [DOI] [PubMed] [Google Scholar]
- 70.Perreault M.L., Hasbi A., O’Dowd B.F., George S.R. Heteromeric Dopamine Receptor Signaling Complexes: Emerging Neurobiology and Disease Relevance. Neuropsychopharmacology. 2014;39:156–168. doi: 10.1038/npp.2013.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Andrianarivelo A., Saint-Jour E., Pousinha P., Fernandez S.P., Petitbon A., De Smedt-Peyrusse V., Heck N., Ortiz V., Allichon M.-C., Kappès V., et al. Disrupting D1-NMDA or D2-NMDA Receptor Heteromerization Prevents Cocaine’s Rewarding Effects but Preserves Natural Reward Processing. Sci. Adv. 2021;7:eabg5970. doi: 10.1126/sciadv.abg5970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Yin H.H., Lovinger D.M. Frequency-Specific and D2 Receptor-Mediated Inhibition of Glutamate Release by Retrograde Endocannabinoid Signaling. Proc. Natl. Acad. Sci. USA. 2006;103:8251–8256. doi: 10.1073/pnas.0510797103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Bamford N.S., Zhang H., Schmitz Y., Wu N.-P., Cepeda C., Levine M.S., Schmauss C., Zakharenko S.S., Zablow L., Sulzer D. Heterosynaptic Dopamine Neurotransmission Selects Sets of Corticostriatal Terminals. Neuron. 2004;42:653–663. doi: 10.1016/S0896-6273(04)00265-X. [DOI] [PubMed] [Google Scholar]
- 74.Bonito-Oliva A., Södersten E., Spigolon G., Hu X., Hellysaz A., Falconi A., Gomes A.-L., Broberger C., Hansen K., Fisone G. Differential Regulation of the Phosphorylation of Trimethyl-Lysine27 Histone H3 at Serine 28 in Distinct Populations of Striatal Projection Neurons. Neuropharmacology. 2016;107:89–99. doi: 10.1016/j.neuropharm.2016.02.037. [DOI] [PubMed] [Google Scholar]
- 75.Ramírez-Jarquín U.N., Shahani N., Pryor W., Usiello A., Subramaniam S. The Mammalian Target of Rapamycin (MTOR) Kinase Mediates Haloperidol-Induced Cataleptic Behavior. Transl. Psychiatry. 2020;10:336. doi: 10.1038/s41398-020-01014-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Bateup H.S., Santini E., Shen W., Birnbaum S., Valjent E., Surmeier D.J., Fisone G., Nestler E.J., Greengard P. Distinct Subclasses of Medium Spiny Neurons Differentially Regulate Striatal Motor Behaviors. Proc. Natl. Acad. Sci. USA. 2010;107:14845–14850. doi: 10.1073/pnas.1009874107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Li Y., Li B., Wan X., Zhang W., Zhong L., Tang S.-J. NMDA Receptor Activation Stimulates Transcription-Independent Rapid Wnt5a Protein Synthesis via the MAPK Signaling Pathway. Mol. Brain. 2012;5:1. doi: 10.1186/1756-6606-5-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Gong R., Park C.S., Abbassi N.R., Tang S.-J. Roles of Glutamate Receptors and the Mammalian Target of Rapamycin (MTOR) Signaling Pathway in Activity-Dependent Dendritic Protein Synthesis in Hippocampal Neurons. J. Biol. Chem. 2006;281:18802–18815. doi: 10.1074/jbc.M512524200. [DOI] [PubMed] [Google Scholar]
- 79.Wang X., Luo Y., He Y., Li F., Shi H., Xue L., Xue Y., Lu L. Nucleus Accumbens Core Mammalian Target of Rapamycin Signaling Pathway Is Critical for Cue-Induced Reinstatement of Cocaine Seeking in Rats. J. Neurosci. 2010;30:12632–12641. doi: 10.1523/JNEUROSCI.1264-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Gong S., Zheng C., Doughty M.L., Losos K., Didkovsky N., Schambra U.B., Nowak N.J., Joyner A., Leblanc G., Hatten M.E., et al. A Gene Expression Atlas of the Central Nervous System Based on Bacterial Artificial Chromosomes. Nature. 2003;425:917–925. doi: 10.1038/nature02033. [DOI] [PubMed] [Google Scholar]
- 81.Valjent E., Corvol J.C., Pages C., Besson M.J., Maldonado R., Caboche J. Involvement of the Extracellular Signal-Regulated Kinase Cascade for Cocaine-Rewarding Properties. J. Neurosci. 2000;20:8701–8709. doi: 10.1523/JNEUROSCI.20-23-08701.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Gainetdinov R.R., Mohn A.R., Bohn L.M., Caron M.G. Glutamatergic Modulation of Hyperactivity in Mice Lacking the Dopamine Transporter. Proc. Natl. Acad. Sci. USA. 2001;98:11047–11054. doi: 10.1073/pnas.191353298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Gangarossa G., Di Benedetto M., O’Sullivan G.J., Dunleavy M., Alcacer C., Bonito-Oliva A., Henshall D.C., Waddington J.L., Valjent E., Fisone G. Convulsant Doses of a Dopamine D1 Receptor Agonist Result in Erk-Dependent Increases in Zif268 and Arc/Arg3.1 Expression in Mouse Dentate Gyrus. PLoS ONE. 2011;6:e19415. doi: 10.1371/journal.pone.0019415. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in this study are available in the Figures and Results sections.