Abstract
Our clinical series comprises 124 patients with movement disorders (MDs) and/or ataxia with cerebellar atrophy (CA), many of them showing signs of neurodegeneration with brain iron accumulation (NBIA). Ten NBIA genes are accepted, although isolated cases compatible with abnormal brain iron deposits are known. The patients were evaluated using standardised clinical assessments of ataxia and MDs. First, NBIA genes were analysed by Sanger sequencing and 59 patients achieved a diagnosis, including the detection of the founder mutation PANK2 p.T528M in Romani people. Then, we used a custom panel MovDisord and/or exome sequencing; 29 cases were solved with a great genetic heterogeneity (34 different mutations in 23 genes). Three patients presented brain iron deposits with Fe-sensitive MRI sequences and mutations in FBXO7, GLB1, and KIF1A, suggesting an NBIA-like phenotype. Eleven patients showed very early-onset ataxia and CA with cortical hyperintensities caused by mutations in ITPR1, KIF1A, SPTBN2, PLA2G6, PMPCA, and PRDX3. The novel variants were investigated by structural modelling, luciferase analysis, transcript/minigenes studies, or immunofluorescence assays. Our findings expand the phenotypes and the genetics of MDs and ataxias with early-onset CA and cortical hyperintensities and highlight that the abnormal brain iron accumulation or early cerebellar gliosis may resembling an NBIA phenotype.
Keywords: movement disorders, ataxia, cerebellar atrophy, neurodegeneration with brain iron accumulation (NBIA), gene panel, exome sequencing
1. Introduction
In 2015, we initiated a new research line focused on disorders associated with neurodegeneration with brain iron accumulation (NBIA). This group of syndromes is characterised by movement disorders (MDs) with the common feature of abnormal deposits of iron in the brain, although clinical and neuroimaging features are variable, reflecting the genetic heterogeneity in this group [1,2,3]. Pantothenate kinase-associated neurodegeneration (PKAN), caused by PANK2 mutations [4], is the most frequent NBIA phenotype; dystonia, parkinsonism, and cognitive decline over the years are core features. In PLA2G6-associated neurodegeneration (PLAN), the second most frequent NBIA, hypotonia, ataxia, and early progressive cerebellar atrophy (CA) are the hallmark of the disease, with brain iron deposits detected in only 50% or less of cases [5]. Different clinical characteristics are predominant in other NBIA disorders, as ataxia, spastic paraparesis, peripheral neuropathy, optic atrophy, and neuropsychiatric problems. Thus, the clinical phenotype and brain magnetic resonance imaging (MRI) patterns evolve differently in each disorder and depend on the stage of the disease and the age of the patient [3].
In clinical practice, genetic diagnosis in these phenotypes may end up being a cumbersome odyssey, due to the difficulty in making reliable genotype-phenotype correlations. Assessment of next generation sequencing (NGS) tools has been reported for cohorts with MDs [6], and more frequently for specific sets of entities such as ataxia [7,8] or hereditary spastic paraplegia (HSP) [9,10]. Targeted gene sequencing likely represents the most cost-effective option, whereas the gold standard seems to be whole exome sequencing (WES) as it covers the known coding genome.
In our cohort, the sequencing of selected NBIA genes in 114 patients provided the genetic diagnosis of 59 patients, including the detection of the founder mutation PANK2 p.T528M in the Roma population. We then studied the undiagnosed patients using a custom panel MovDisord and WES-trio, plus 10 additional cases investigated exclusively by WES-proband. Twenty-nine probands achieved a conclusive molecular diagnosis with a great genetic heterogeneity (34 different disease-causing mutations in 23 genes). Considering the whole series, the diagnostic success rate was 70.97%. We expanded MDs phenotypes with brain iron accumulation, but also ataxia phenotypes with CA and cortical hyperintensities, from classical PLAN to non-progressive congenital ataxia (NPCA) phenotypes.
2. Results
2.1. Genetics
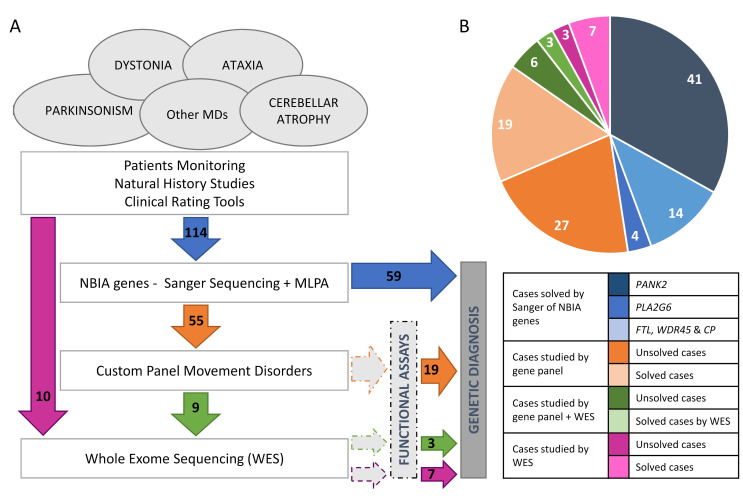
The mutational screening of the most frequent NBIA genes revealed that 41 (35.96%) and 14 (12.28%) out of 114 patients carried biallelic mutations in PANK2 or PLA2G6, respectively (Figure 1). Regarding other NBIA genes, one proband harboured a causative variant in WDR45 (c.182A>C, p.N61T); two in FTL (c.286G>A, p.A96T; c.509_*4del, p.L170_Pfs*8); and another one in CP (c.1652C>T, p.T551I/c.2684G>C, p.G895A). Taken together, the etiological diagnosis was attained in 59 (51.75%) patients. The NBIA mutations detected in our series are available at https://espinos.cipf.es (accessed on 1 August 2022).
Figure 1.
Casuistry and strategy. (A) Pipeline designed for genetic analysis of a cohort of patients with movement disorders and ataxia, which includes different approaches from candidate gene to gene panel and WES (whole exome sequencing) carried out in a cohort of 124 probands. (B) Distribution of cases studied by gene panel MovDisord. In 59 probands, a definitive diagnosis was achieved by Sanger sequencing and MLPA (in blue): 41 patients carried mutations in PANK2, 14 in PLA2G6, and 4 in other NBIA genes (http://espinos.cipf.es/index.php/en/mutations-db, accessed on 1 August 2022). Using a custom panel MovDisord, the remaining 55 probands were investigated and the causative mutations were identified in 19 cases (in orange). Finally, nine patients were further studied by WES and in three cases the clinical variant was detected (in green). To compare both approaches (gene panel versus WES), ten patients were investigated by WES only, and the disease-causing mutations were detected in seven of them (in purple). NBIA: neurodegeneration with brain iron accumulation. MD: Movement disorders. MLPA: multiplex ligation-dependent probe amplification.
The seven unrelated Roma patients from Spain (homozygous for the PANK2 c.1583C>T, p.T528M mutation), shared the same haplotype [A-268-C-T-C-G-285] that stretched from rs1078152 to D20S116, encompassing a 0.9 Mb region (Table S1). The Hungarian Roma proband had a narrower haplotype for both alleles, which included the intragenic markers (13.1 Kb) only. Two Greek heterozygous carriers of the PANK2 c.1583C>T mutation presented the same haplotype as the Spanish patients, and one Greek proband showed a finer haplotype from rs1078152 to rs7270329 (0.8 Mb). Lastly, the non-Roma Spanish proband heterozygous for the investigated variant had a different haplotype, suggesting different mutational events for PANK2 c.1583C>T.
The 55 unsolved patients were investigated by a custom panel MovDisord (Figure 1). The mean coverage among all samples was >400×, the lowest mean coverage achieved was 233×, and the highest 605× (Figure S1). In all cases, at least 99.7% of the bases were covered with >20 reads and mean gene coverage was >65× (Table S2). Panel MovDisord was robust in terms of coverage, as well as read depth for all genes and samples.
Nineteen out of fifty-five patients were genetically diagnosed (Table 1 and Figure 1). Nine unsolved patients were then investigated by WES-trio and mutations in PLEKHG2, NR4A2, and PRDX3 were identified in three probands (Table 1). None of these three genes were included in the panel. In parallel, seven out of ten patients, investigated by WES-proband only, obtained a conclusive genetic diagnosis (Table 1 and Figure 1). It is worth mentioning that the MD-319 case (LRRK2 gene) was cleared up after a reanalysis of WES data two years after the initial analysis. In total, 29 patients were diagnosed.
Table 1.
Genetic findings of the 29 solved cases.
| Patient | Gene | RefSeq | Position | DNA Change |
Protein Change |
Prediction ◊ | rs number (MAF) ǂ |
References PMID § | Method |
|---|---|---|---|---|---|---|---|---|---|
| MD-208 | CASK | NM_003688.3 | X:41383202 | c.2589+2T>G | ― | P | NA | None | Gene Panel |
| MD-216 | CPLANE1 | NM_023073.3 | 5:37201821 | c.3379T>G | p.S1127A | LP | rs776423792 (1.193 × 10−5) |
None | Gene Panel |
| 5:37164372 | c.7588+3A>G | ― | P | NA | None | ||||
| MD-122 | EXOSC3 | NM_013042.3 | 9:37783990 | c.395A>C | p.D132A | P | rs141138948 (4.067 × 10−4) |
22544365, 23564332, 23564332, 23975261, 24524299, 25533962, 27777260, 28687512, 30950035, 31692161 | Gene Panel |
| HOMOZYGOSIS (No Consanguinity) |
|||||||||
| MD-012 | EXOSC3 | NM_013042.3 | 9:37783990 | c.395A>C | p.D132A | P | rs141138948 (4.067 × 10−4) |
22544365, 23564332, 23564332, 23975261, 24524299, 25533962, 27777260, 28687512, 30950035, 31692161 | Gene Panel |
| HOMOZYGOSIS (No Consanguinity) |
|||||||||
| MD-018 # | FBXO7 | NM_012179.3 | 22:32875213 | c.368C>G | p.S123 * | P | NA | 32767480 | Gene Panel |
| HOMOZYGOSIS (Consanguinity) | |||||||||
| MD-137 | FUCA1 | NM_000147.4 | 1:24194637 | c.140G>C | p.R47P | LP | NA | None | Gene Panel |
| HOMOZYGOSIS (Consanguinity) |
|||||||||
| MD-020 | GLB1 | NM_000404.3 | 3:33114105 | c.176G>A | p.R59H | P | rs72555392 (3.607 × 10−5) |
10338095, 17664528, 28939701, 31761138 | Gene Panel |
| 3:33114174 | c.107A>G | p.Y36C | P | rs748345527 (4.809 × 10−5) |
None | ||||
| MD-270 | HEXA | NM_000520.5 | 15:72646027 | c.459+5G>A | ― | P | rs762060470 (2.829 × 10−5) |
1837283, 25525159 | Gene Panel |
| 15:72638893 | c.1305C>T | ― | P | rs587779406 (8.488 × 10−5) |
20363167, 25606403 | ||||
| MD-320 | ITPR1 | NM_00116872.1 | 3:4687357 | c.800C>T | p.T267M | P | rs797044955 (NA) |
24091540, 28659154, 29878067, 29925855, 29925855, 30842224, 31632679, 32695065 | WES-proband |
| MD-106 | ITPR1 | NM_00116872.1 | 3:4687362 | c.805C>T | p.R269W | P | NA | 27062503, 25533962, 28826917, 28191890, 28135719, 28659154, 29925855 | Gene Panel |
| MD-041 | ITPR1 | NM_00116872.1 | 3:4706967 | c.1655A>G | p.Y552C | LP | NA | None | Gene Panel |
| MD-200 | KIF1A | NM_001244008.1 | 2:241725854 | c.506C>G | p.R169T | LP | NA | 34121983 | Gene Panel |
| MD-189 | KIF1A | NM_001244008.1 | 2:241715280 | c.946C>T | p.R316W | P | NA | 25265257, 26354034, 28554332 | Gene Panel |
| MD-299 | KIF1A | NM_001244008.1 | 2:241715280 | c.946C>T | p.R316W | P | NA | 25265257, 26354034, 28554332 | WES-proband |
| MD-319 | LRRK2 | NM_198578.4 | 12:40734202 | c.6055G>A | p.G2019S | P | rs34637584 (4.884 × 10−4) |
15726496, 16102999, 16333314, 16750377, 16966501, 17060589, 17116211, 17210620, 17200152, 19072560, 20008657, 19283415, 21686713, 19302196, 19741132 σ | WES-proband |
| HOMOZYGOSIS (Consanguinity) |
|||||||||
| MD-277 # | NR4A2 | NM_006186.4 | 2:157184954 | c.956G>A | p.R319Q | LP | NA | 33585677 | WES-trio |
| MD-173 | PDGFB | NM_002608.3 | 22:39621853 | c.602-1G>C | ― | P | NA | None | Gene Panel |
| MD-252 | PNKD | NM_015488.4 | 2:219187987 | c.-4C>G | ― | LP | rs1461115674 (8.152 × 10−6) |
None | Gene Panel |
| MD-341 | PLA2G6 | NM_003560 | 22:38519251 | c.1442T>A | p.L481Q | LP | rs587784330 (5.922 × 10−6) |
16783378, 24870368, 25164370 | WES-proband |
| HOMOZYGOSIS (Consanguinity) |
|||||||||
| MD-181 | PLEKHG2 | NM_022835.2 | 19:39905680 | c.158C>T | p.T53I | P | NA | None | WES-trio |
| HOMOZYGOSIS (Consanguinity) |
|||||||||
| MD-323 | PMPCA | NM_015160.2 | 9:139310844 | c.633+1G>A | --- | P | rs1442110087 (7.961 × 10−6) |
None | WES-proband |
| 9:139306513 | c.136T>C | p.S46P | LP | NA | None | ||||
| MD-174 # | PRDX3 | NM_006793.5 | 10:120931956 | c.489C>G | p.R163E | P | NA | 35766882 | WES-trio |
| HOMOZYGOSIS (Consanguinity) |
|||||||||
| MD-296 | QARS1 | NM_005051 | 3:49138870 | c.794G>A | p.R265H | LP | rs916890735 (6.575 × 10−6) |
None | WES-proband |
| HOMOZYGOSIS (Consanguinity) |
|||||||||
| MD-126 # | REEP1 | arr[hg19]2p11.2 (chr2:83,335,425-87,271,924; Hg 19) | P | ― | 22062632, 24986827 | Gene Panel | |||
| MD-307 | RPGRIP1L | NM_015272 | 16:53720424 | c.697A>T | p.K233* | P | rs121918197 (2.788 × 10−5) |
17558409, 25525159 | WES-proband |
| 16:53686828 | c.1769_1770delCT | p.S590Cfs* | P | NA | None | ||||
| MD-159 # | SPG7 | NM_003119.3 | 16:89613145 | c.1529C>T | p.A510V | LP | rs61755320 (2.899 × 10−5) |
18799786, 20981092, 20186691, 21623769, 22995991, 23269439, 22571692, 25133958, 25525159, 26626314, 29057857, 27957547, 29026558, 28362824, 28832565, 29482223, 29913018, 30369941, 31433872, 30098094, 31316545, 29915382, 30537300, 31692161 | Gene Panel |
| 16:89616953 | c.1715C>T | p.A572V | P | rs72547551 (3.537 × 10−5) |
14985266, 25681447, 29482223 | ||||
| MD-219 # | SPTBN2 | NM_006946.3 | 11:66483417 | c.193A>G | p.K65E | P | NA | 33801522 | Gene Panel |
| MD-207 # | SPTBN2 | NM_006946.3 | 11:66481110 | c.764A>G | p.D255G | P | NA | 33801522 | Gene Panel |
| MD-153 | TPP1 | NM_000391.3 | 11:6636487 | c.1340G>A | p.R447H | P | rs119455956 (7.953 × 10−5) |
10330339, 19038966, 20340139, 26143525, 29655203 | Gene Panel |
| 11:6640007 | c.229G>C | p.G77R | P | rs121908195 (7.969 × 10−5) |
26633542, 31741823 | ||||
AD, Autosomal Dominant; AR, Autosomal Recessive; LP, Likely Pathogenic; NA, Not-Available; P, Pathogenic; PMID, PubMed Identifier; RefSeq, Reference Sequence; SCA, Spinocerebellar Ataxia; SPG: Spastic Paraplegia; WES, Whole Exome Sequencing; XLD, X-linked dominant. ◊ Prediction of pathogenicity performed according to the ACMG/AMP guidelines [11]. ǂ Consulted database gnomAD v2.1.1, except for rs916890735 that is only annotated in gnomAD v3.1.1 (accessed on 1 August 2022). § References associated with each mutation in the Human Mutation Database (HGMD®) Professional 2022.2 (Qiagen, Santa Clarita, CA, USA; accessed om 1 August 2022). σ The LRRK2 p.G2019S change is reported in at least 119 articles. # Clinical features of patients MD-018, MD-277, MD-174, MD-126, MD-159, MD-219, and MD-207 were previously reported [12,13,14,15,16,17].
Two cases were familial and one case currently sporadic (MD-252), likely would be a familial one (the daughter’s proband is asymptomatic; Figure S2 and Table 2); twenty-five cases were sporadic (11 de novo cases); and one case remained unclassified due to lack of information. Most of the deleterious changes were transmitted in an AR fashion (16 cases) or in an AD manner (12 cases), and only one case presented an X-linked dominant (XLD) inheritance. Nine AR cases had mutations in homozygosis, and in seven of them, the parents were consanguineous (five patients from Morocco, one from Greece, and one from Spain). Two mutations were identified twice: EXOSC3 p.D132A in homozygosis in non-consanguineous cases, and KIF1A p.R316W with a de novo presentation (Table 1 and Table 2). As a whole, 34 mutations were detected, 17 of them not previously associated with disease, in 23 different genes, including those formerly published [12,13,14,15,16,17].
Table 2.
Clinical features of the 29 solved cases.
| Patient Sex |
Gene | Origin | Presentation Inheritance |
Disease (OMIM) |
Age of Onset Age at Testing |
Early Symptoms | Brain MRI | Additional Clinical Features |
|---|---|---|---|---|---|---|---|---|
| MD-208 Female |
CASK | Spain | de novo XLD |
Mental retardation and microcephaly with pontine and cerebellar hypoplasia (300749) |
1 mo 3 yo |
Hypotonia Microcephaly DD |
Severe PCH | Mild limb dystonia, choreoathetosis, progressive scoliosis from 3 yo |
| MD-216 Male |
CPLANE1 | Morocco | Familial AR |
Joubert syndrome 17 (614615) |
1 yo 10 yo |
DD Hypotonia, ataxia OMA |
Molar tooth sign Cerebellar hypoplasia |
ID, ataxia and OMA improve with age |
| MD-122 Female |
EXOSC3 | Spain | Sporadic AR |
Pontocerebellar hypoplasia type 1B (614678) |
3 mo 3 yo |
Hypotonia, axial hyperextension, strabismus | Progressive vermis atrophy | Spasticity progressing to flaccid paralysis from 3-yo, g-tube feeding, neurogenic EMG pattern, exitus at 4 yo |
| MD-012 Male |
EXOSC3 | Spain | Sporadic AR |
4 mo 8 yo |
Hypotonia, DD | Progressive vermis atrophy | Spasticity from 4 yo, axonal neuropathy with loss of tendon reflexes from 5 yo, g-tube feeding, limb dystonia from 6 yo | |
| MD-018 # Female |
FBXO7 | Morocco | Sporadic AR |
Parkinson disease 15 (260300) |
2 yo 21 yo |
Mild DD, infection-triggered acute ataxia at 2 yo | CA from 10 yo Brain iron deposits from 15 yo |
Absence epilepsy from 5 yo, acute encephalopathy at 12 yo, progressive deterioration, spastic paraparesis, drug-resistant seizures, optic neuropathy, parkinsonism from 15 yo |
| MD-137 Male |
FUCA1 | Greece | Sporadic AR |
Fucosidosis (230000) |
3 yo 10 yo |
Speech difficulties, gait disturbances |
GP T2 hypointensity from 10 yo |
Static encephalopathy, progression of gait disorder with dystonia, ID, dysmorphic features, ADHD symptoms, motor stereotypes |
| MD-020 Female |
GLB1 | Spain | Sporadic AR |
GM1-gangliosidosis (230500, 230600, 230650) |
3 yo 12 yo |
Speech difficulties, motor deterioration | Brain iron deposits from 10 yo |
Oromandibular dystonia, dysarthria, neuropathy, spasticity, scoliosis |
| MD-270 Female |
HEXA | Spain | NA AR |
GM2-gangliosidosis (272800) |
26 yo 23 yo |
DD, hypotonia | CA | Cerebellar syndrome, stereotyped behaviour, progressive cognitive decline |
| MD-320 Male |
ITPR1 | Senegal | de novo AD |
SCA15 (606658) SCA29 congenital nonprogressive (117360) |
3 mo 5 yo |
DD, hypotonia, gaze-evoked nystagmus | CA Cerebellar cortical hyperintensity from 3 yo (upper > lower hemispheres) |
Ataxia, NPCA, strabismus, ID, mild lower limbs spasticity |
| MD-106 Male |
ITPR1 | Morocco | de novo AD |
<1 yo 6 yo |
DD, hypotonia | CA Cerebellar cortical hyperintensity from 3 yo (upper > lower hemispheres) |
Ataxia, NPCA, strabismus, gaze-evoked nystagmus, ID, lower limbs spasticity | |
| MD-041 Male |
ITPR1 | Spain | de novo AD |
2 mo 3 yo |
Gaze-evoked nystagmus, hypotonia | CA Cerebellar cortical FLAIR hyperintensity at age of 4 (upper > lower hemispheres) |
Ataxia, NPCA, strabismus, abnormal ocular movements, ID | |
| MD-200 Male |
KIF1A | Spain | de novo AD |
NESCAV syndrome (614255) |
<1 yo 12 yo |
DD, microcephaly, nystagmus | CA | Ataxia, NPCA, lower limbs spasticity, seizures (4 yo), dysphagia, intellectual disability, axonal neuropathy, optic atrophy (9 yo) |
| MD-189 Male |
KIF1A | Portugal | de novo AD |
SPG30 (610357) | 12 mo 22 yo |
DD, visual deficit | CA Brain iron deposits from 17 yo |
Ataxia, NPCA, optic atrophy, stuttering (2 yo), lower limbs spasticity (3 yo), cognitive regression (4 yo), peripheral neuropathy, seizures (14 yo) |
| MD-299 Male |
KIF1A | Spain | de novo AD |
SPG30 (610357) | 11 mo 9 yo |
DD, hypotonia | CA Cerebellar cortical and deep WM FLAIR hyperintensity |
Ataxia (2 yo), NPCA, acquired microcephaly, lower limbs spasticity (3 yo), cognitive impairment, no regression |
| MD-319 Male |
LRRK2 | Morocco | Sporadic AR |
Parkinson disease (607060) |
5 yo 14 yo |
Tremor | Normal | Hands tremor, cervical tremor, mild bradykinesia, hoarseness voice (13 yo) |
| MD-277 # Male |
NR4A2 | Spain | de novo AD |
AD early-onset dystonia-parkinsonism with intellectual disability (601828) |
12 yo 29 yo |
Mild DD from 1 yo | Normal | Borderline IQ (77; 7 yo), motor tics from 16-yo, dystonia and parkinsonism from 28 yo |
| MD-173 Female |
PDGFB | Spain | Familial AD |
Basal ganglia calcification idiopathic 5 (615483) |
19 yo 19 yo |
Postural and intentional tremor | Calcifications | Tremor |
| MD-252 Male |
PNKD | Spain | Familial? AD |
Paroxysmal nonkinesigenic dyskinesia 1 (118800) |
49 yo 49 yo |
Paroxysmal dystonia | Normal | Dystonia, parkinsonism |
| MD-341 Female |
PLA2G6 | Morocco | Sporadic AR |
Infantile neuroaxonal dystrophy 1 (256600) NBIA2B (610217) Parkinson disease 14 (612953) |
12 mo 5 yo |
Ataxic gait, DD | CA Cerebellar cortical FLAIR hyperintensity |
Ataxia, dysmetria, hypotonia, spasticity, axonal motor impairment, optic atrophy, intellectual disability |
| MD-181 Male |
PLEKHG2 | Spain | Sporadic AR |
Leukodystrophy and acquired microcephaly with or without dystonia (616763) | 1 mo 6 yo |
Hypotonia, DD | Thalamic lesions CA |
Spastic-dystonic tetraparesia from 6 mo, bilateral cataracts, OMA, neuropathy |
| MD-323 Male |
PMPCA | Spain | Sporadic AR |
SCAR2 (213200) |
21 mo 9 yo |
Motor development delay, ataxia, nystagmus | CA Cerebellar cortical hyperintensity |
Ataxia, NPCA, mild cognitive impairment |
| MD-174 # Male |
PRDX3 | Morocco | Sporadic AR |
NA | 2 yo 3 yo |
Non-triggered acute cerebellar syndrome | Rapid progression of CA | Ataxia, chronic cerebellar syndrome following acute onset, demyelinating neuropathy from 5 yo |
| MD-296 Male |
QARS1 | Morocco | Sporadic AR |
Microcephaly, progressive seizures, and cerebral and cerebellar atrophy (615760) |
18 mo 13 yo |
Febrile seizures, DD, atypical absences | CA | ID, language impairment, drug-resistant epilepsy with non-motor and motor seizures |
| MD-126 # Female |
REEP1 | Spain | de novo AD |
SPG31 (610250) |
33 yo 35 yo |
Parkinsonism | Calcifications | Parkinsonism, tremor, spasticity, dystonia, slow saccades, dysarthria |
| MD-307 Male |
RPGRIP1L | Spain | Sporadic AR |
COACH syndrome (216360) Joubert syndrome 7 (611560) Meckel syndrome 5 (611561) |
1 mo 1 yo |
Hypotonia, nystagmus, strabismus | PCH | Profound DD, g-tube feeding, awake apneas, seizures, dyskinesia, exitus at 24 mo |
| MD-159 # Male |
SPG7 | Spain | Sporadic AR |
SPG7 (607259) | 17 yo 26 yo |
Dystonia, postural instability, dysarthria | CA | Mild dystonic gait with mild spastic-ataxia gait, dysmetric saccades, gaze-evoked nystagmus, intention tremor |
| MD-219 # Male |
SPTBN2 | Spain | de novo AD |
SCA5 (600224) | 4 mo 11 yo |
Hypotonia, transient upgaze deviation | Severe CA Cerebellar cortical hyperintensity |
Ataxia, NPCA, moderate ID |
| MD-207 # Male |
SPTBN2 | Spain | de novo AD |
SCA5 (600224) | 12 mo 8 yo |
Motor delay, DD | Severe CA Cerebellar cortical hyperintensity |
Ataxia, NPCA, ADHD, borderline IQ |
| MD-153 Male |
TPP1 | Cuba | Sporadic AR |
Ceroid lipofuscinosis neuronal 2 (204500) SCA7 (609270) |
5 yo 13 yo |
Speech delay, stuttering, motor clumsiness | GP FLAIR low signal, cerebral and CA, white matter T2-high signal | Limb and orofacial dystonia from 11 yo, spasticity, cognitive decline, no seizures |
AD, Autosomal Dominant; ADHD, Attention-Deficit Hyperactivity Disorder; AR, Autosomal Recessive; CA, Cerebellar Atrophy established in consecutive neuroimaging; COACH, Cerebellar vermis hypo/aplasia, Oligophrenia, Congenital ataxia, Ocular coloboma, and Hepatic fibrosis; FLAIR, fluid attenuated inversion recovery; GP, Globus pallidus; DD, Developmental Delay; EMG, Electromyogram; ID, Intellectual Disability; IQ, Intelligence Quotient; mo, months old; MRI, Magnetic Resonance Imaging; NA, Not-available; NBIA, Neurodegeneration with Brain Iron Accumulation; NESCAV, Neurodegeneration and Spasticity with or without Cerebellar Atrophy or Cortical Visual impairment; NPCA, Non-Progressive Congenital Ataxia; OMA, Oculomotor Apraxia; OMIM, Online Mendelian Inheritance in Men; PCH, Ponto-Cerebellar Hypoplasia; SCA, Spinocerebellar Ataxia; SCAR, SCA Autosomal Recessive; SPG, Spastic Paraplegia; WM, White Matter; XLD, X-Linked Dominant; yo, years old. # Clinical features of patients MD-018, MD-277, MD-174, MD-126, MD-159, MD-219 and MD-207 were previously reported [12,13,14,15,16,17].
2.2. Genotype-Phenotype Correlation
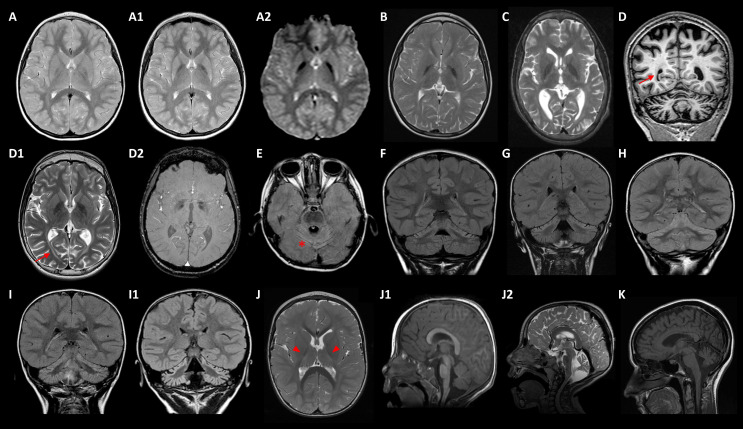
Five cases with T2W MRI showing bilateral GP hypointensities carried disease-causing mutations in FBXO7, GLB1, FUCA1, TPP1, and KIF1A (Table 1 and Table 2) MD-018 (homozygous FBXO7 p.S123*) was previously described [14]. MD-020 (GLB1 p.R59H/p.Y36C) suffers from a GM1-gangliosidosis type II, with an onset at age 3 with dysphemia. The patient showed a slow progression of the motor disorder, with generalized dystonia at age 12, associated with bulbar dysfunction (dysphagia, dysarthria, dysphonia), and mild flattening of vertebral bodies with scoliosis; iron-sensitive MRI sequences showed brain iron deposits from 10 years old (Figure 2A–A2). MD-137 (homozygous FUCA1 p.R47P) with a history of static encephalopathy, had a dystonic gait from 3 years old and presented GP T2W hypointensities from 10 years old (Figure 2B). MD-153 (TPP1 p.R447H/p.G77R) suffered from a progressive spastic-dystonic gait and also, showed T2W GP hypointensities, together with CA and deep white matter subtle demyelination, at the age of 14 (Figure 2C). Finally, MD-189 (KIF1A p.R316W) presented with an ataxic-spastic gait with early-onset CA, but iron deposits ascertained by SWI sequences from 17 years old (Figure 2D–D2).
Figure 2.
Main neuroimaging features. (A–A2) MD-020/GLB1: axial TSE (turbo spin echo) T2 weighted image at ages 6 (A) and 11 (A1) showing progression of globus pallidus (GP) hypointensities, demonstrating iron deposition in axial T2* GRE (gradient echo) image (A2) at 11 years old. (B) MD-137/FUCA1 and (C) MD-153/TPP1 revealing T2-weighted images (T2WI) GP hypointensities at ages 10 and 14, respectively. (D–D2) MD-189/KIF1A at 17 years old: coronal T1-weighted image showing cerebral and cerebellar atrophy (D), axial T2WI revealing GP hypointensity (D1) and SWI, susceptibility weighted imaging (D2) showing iron deposition; the patient also presented periventricular and deep white matter abnormal signal (arrows). (E) MD-200/KIF1A at age of 4: axial FLAIR (fluid attenuated inversion recovery) image revealing global cerebellar atrophy with cortical hyperintensity (* tram-track sign). (F–H) Coronal FLAIR images uncover predominantly upper cerebellar cortical hyperintensity in patients MD-106 at age of 3 (F), MD-041 of 4 (G), and MD-320 of 4 (H), with ITPR1 variants. (I–I1) MD-323/PMPCA: Coronal FLAIR images at 2 years old (I), and at 8 years old (I1) demonstrating progression of cerebellar atrophy with cortical hyperintensities. (J–J2) MD-181/PLEKHG2 from 2 (J,J1) to 5 years old (J2): T2WI (J) showing thalamic and posterior internal capsule hyperintensities (head arrows), and mild deep white matter hyperintensity; mid-sagittal T1 weighted image (J1) and midsagittal T2WI (J2) demonstrating progression of cerebellar atrophy. (K) MD-270/HEXA: mid-sagittal T2WI revealing cerebellar atrophy at disease onset (23 years old).
Eleven diagnosed patients manifested very early-onset ataxia and CA associated with mutations in ITPR1 (3), KIF1A (3), PLA2G6, PMPCA, SPTBN2 (2), and PRDX3 (Table 1 and Table 2). The patients with mutations in SPTBN2 or PRDX3 were previously reported [13,17]. Interestingly, nine subjects evolved to an NPCA phenotype [18]; they harboured mutations in ITPR1, KIF1A, PMPCA, and SPTBN2. Additionally, five patients with ITPR1 (2) or KIF1A (3) variants developed lower limbs spasticity over time; two children with KIF1A mutations additionally associated optic atrophy, and one of them showed the early appearance of iron deposits demonstrated by iron-sensitive sequences (Figure 2D2).
In the reported PLAN series [5], CA is universal and one-third of the patients showed cerebellar cortical hyperintensities, discovered by axial or coronal FLAIR (fluid attenuated inversion recovery) MRI sequences. Remarkably, this neuroimaging finding was also observed in seven out of nine NPCA patients (Figure 2E–I1), related to deleterious variants in KIF1A (1), ITPR1 (3), PMPCA (1), and SPTBN2 (2) [13]. MD-181 (homozygous PLEKHG2 p.T53I) showed very early-onset hypotonia, and developmental delay rapidly evolved into spastic-dystonic tetraparesis from 6 months old (Table 1 and Table 2), when subtle symmetrical T2 hyperintensities on thalami and deep white matter were detected (Figure 2J). The clinical course showed a significant deterioration with the appearance of oculomotor apraxia, peripheral neuropathy, and CA from 2 to 5 years old (Figure 2J1–J2). MD-159 (SPG7 p.A510V/p.A572V), previously reported [15,19], presented early onset multifocal dystonia with severe cranio-cervical involvement and mild CA on brain MRI. MD-270 (HEXA c.459+5G>A/c.1305C>T) started with a cerebellar syndrome at 23 years old with cognitive decline and CA (Figure 2K). MD-296 (homozygous QARS1 p.R265H) suffered from a developmental delay and seizures from the second year of age, associated with mild CA without ataxia.
Five patients developed a severe encephalopathy with a pontocerebellar hypoplasia (PCH) pattern (Table 1 and Table 2). MD-208 (heterozygous CASK c.2589+2T>G), a 5-year-old girl, also had congenital microcephaly with PCH and generalised CA. MD-307 (RPGR1P1L p.K233*/p.S590Cfs*), an 11-month boy, developed progressive encephalopathy with respiratory complications and early death. MD-307 and MD-216 (CPLANE1 p.S1127A/c.7588+3A>G) presented the characteristic molar tooth sign on brain MRI associated with Joubert syndrome. Lastly, two patients, MD-122 and MD-012 (homozygous EXOSC3 p.D132A), suffered from progressive encephalopathy with spasticity, muscular weakness, and early and rapid vermis atrophy.
Only one case showed an MRI with calcium depositions: MD-173 (PDGFB c.602-1G>C) and her affected mother, who presented a mild phenotype with postural and intention tremors. The remaining four patients did not show any remarkable findings in brain MRI (Table 1 and Table 2). MD-126 (REEP1 arr[hg19]2p11.2 (chr2:83,335,425-87,271,924)) and MD-277 (NR4A2 p.R319Q) were previously reported [12,16]. MD-252 (PNKD c.-4C > G), presented at the age of 49 with paroxysmal episodes of lingual dystonia and blepharospasm. The attacks lasted for a few minutes and were usually precipitated after prolonged speaking. Further, mild upper limb dystonic postures were evident on examination. An extensive study including MRI and magnetic resonance angiography, electroencephalogram, dopamine transporter single photon emission CT (DaT-SPECT) and a thorough laboratory investigation, was performed without findings. Segregation analysis revealed that his healthy daughter, 25 years old, heterozygous for the PNKD c.-4C>G, remained asymptomatic (Figure S2). MD-319 (LRRK2 p.G2019S) started with tremors at age 5; by 14 years old, he presented bradykinesia and a hoarse voice.
A whole deletion of NIPA1 was observed in heterozygosis in two patients, which was a heterozygous 15q11.2 BP1-BP2 microdeletion (Table 3) whose implications in disease are controversial [20]. Thus, MD-168 and MD-143 presented with disparate symptoms, and therefore, it is not possible to conclude that the 15q11.2 BP1-BP2 microdeletion is the only molecular cause underlying illness in our probands.
Table 3.
Genetics and main clinical features of controversial cases.
| Patient Sex |
Gene | Candidate Mutation rs Number (MAF) § |
Onset Status Inheritance |
Disease (OMIM) Inheritance |
Main Clinical Features | References PMID § | Observations |
|---|---|---|---|---|---|---|---|
| MD-168 Male |
NIPA1 | arr[hg19] 15q11.2(22,770,421–23,277,436)×1 507 Kb deletion that includes seven genes: TUBGCP5, CYFIP1, NIPA2, NIPA1, LOC283683, WHAMMP3, GOLGA8I |
2 yo Sporadic case Heterozygosis AD |
The 15q11.2 BP1-BP2 microdeletion syndrome (615656) AD |
Autism, obsessive phobic disorder, language delay, dysarthria, severe hypermetropia, generalised dystonia | 31451536, 25689425, 30909440, 30542208, 19328872, 21359847, 28387067, 32117010 | The 15q11.2 BP1-BP2, although associated with neurodevelopmental disorders in multiple papers, should not be considered as a disease causing mutation, since this microdeletion or reported microduplication may explain only a small fraction of the clinical phenotype |
| MD-143 Male |
NIPA1 | arr[hg19] 15q11.2(22,770,421–23,214,655)×1 444 Kb deletion that includes six genes: TUBGCP5, CYFIP1, NIPA2, NIPA1, LOC283683, WHAMMP3 |
73 yo Sporadic case Heterozygosis AD |
Chorea, parkinsonism | |||
| MD-232 Male |
NIPA1 | c.272G>C (p.P91R) novel |
12 yo Sporadic case Heterozygosis AD |
Spastic paraplegia 6 (600363) AD |
GP T2 hypointensity, lower limb spasticity-dystonia, intellectual disability, sensorineural deafness | novel | The proband also had a 18p duplication and a 18q deletion with unclear clinical implications. |
| MD-179 Female |
GCH1 | c.671A>G (p.K224R) rs41298442(MAF: 3.709 × 10−4) |
20 yo Sporadic case Heterozygosis AD |
Dystonia DOPA-responsive (128230) AD |
GP T2 hypointensity, dystonia, dysarthria, upper limbs tremor | 8852666, 12391354, 15303002, 25497597, 30314816 | Her two asymptomatic children carried the mutation in heterozygosis |
| MD-342 Female |
PARK2
PRKN |
c.220_221dupTG (p.W74Cfs*) rs746646126(MAF: 3.191 × 10−5) |
9 yo Sporadic case Homozygosis AR |
Parkinson disease juvenile type 2 (600116) AR |
Ataxia, motor delay, intention tremor, dysarthria, hypotonia, spasticity | 10072423 | The proband’s phenotype does not fit with the PARK2-associated parkinsonism |
| MD-347 Female |
SACS | c.4016C>A (p.Q1143K) rs144267558(MAF: 1.066 × 10−3) |
2 mo Sporadic case Compound Heterozygosis AR |
ARSACS (270550) AR |
Cerebellar vermis hypoplasia, oculomotor apraxia, improving with age | 29915382 | MD-347 seems to be a carrier of a deleterious mutation (p.Q1143K), whereas p.N4573H (VUS) likely does not contribute to the clinical outcome. |
| c.14306A>C (p.N4573H) rs34382952(MAF: 3.124 × 10−3) |
None |
AD, Autosomal Dominant; AR, Autosomal Recessive; ARSACS, Autosomal Recessive Spastic Ataxia type Charlevoix Saguenay; GP: Globus pallidus; MAF, Minor Allele Frequency; NBIA, Neurodegeneration with Brain Iron Accumulation; mo, months old; OMIM: Online Mendelian Inheritance in Men; PMID, PubMed Identifier; yo, years old; VUS: Variant of Uncertain Significance; XLD: X-Linked Dominant. Consulted database gnomAD v2.1.1. § References associated with each mutation in the Human Mutation Database (HGMD®) Professional 2022.2 (Qiagen, Santa Clarita, CA, USA; accessed on 1 August 2022).
MD-232 (heterozygous NIPA1 p.P91R) carried a duplication on chromosome 18 and a deletion on chromosome 18q 46,XY, der(18)del(18)(q22-qter)invdup(18)(p11.1-pter) (Table 3), with unclear clinical consequences. The patient showed T2W GP hypointensities, although the MRI sequences were not conclusive at age 11. Strikingly, the immunofluorescence assay displayed that NIPA1 p.P91R may alter the intracellular transport (Figure S3), but how it contributes to the final clinical outcome remains elusive.
MD-179 (heterozygous GCH1 p.K224R), MD-342 (homozygous PARK2 p.W74Cfs*), and MD-347 (SACS p.Q1143K/p.N4573H) carried interesting variants as candidates to be the disease-causing mutations (Table 3 and Figure S2). Nonetheless, the segregation analyses and/or the clinical picture made us discard them as causative mutations in these probands.
2.3. Studies to Investigate the Pathogenicity of the Novel Variants
In the 65 patients studied by gene panel MovDisord and/or WES, 17 novel causative variants were identified (Table 1). We performed additional studies to obtain evidence of pathogenicity. We previously reported the analyses of four novel mutations located in FBXO7, SPTBN2, and PRDX3 [13,14,17]. GLB1 p.Y36C must be damaging because the affected girl showed an extremely low blood β-galactosidase activity (4 nmol/h per mg protein), which supports a defective GLB1 protein. RPGR1P1L p.S590Cfs* change is expected to be detrimental as it is a premature stop codon. Thus, we describe studies for nine novel variants, including a new change (NIPA1 p.P91R) detected in a patient with a controversial diagnosis (Table 3), which was studied to ascertain if it may contribute to the clinical outcome.
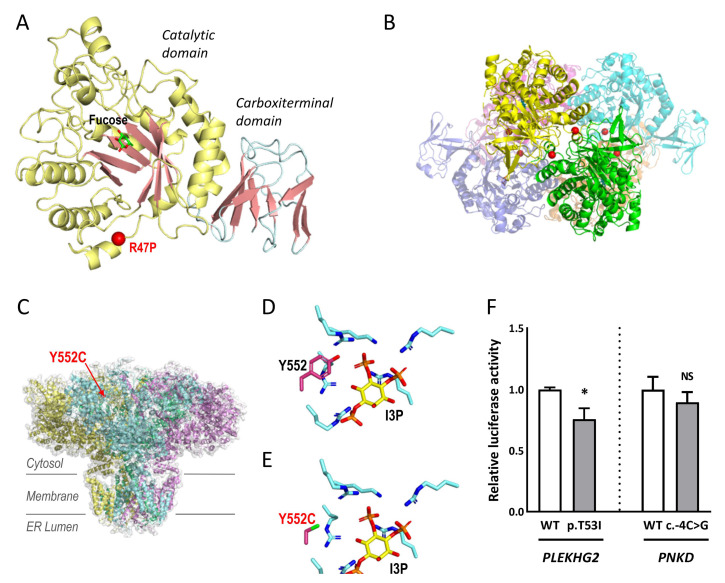
FUCA1 p.R47P, and ITPR1 p.Y552C were explored by structural modelling. Importantly, the proband MD-137 showed a complete absence of α-fucosidase activity (0.00 nmol/h per mg protein), supporting that the patient suffered from a α-fucosidase deficiency. Tissue α-L-fucosidase (FUCA1) is a lysosomal enzyme responsible for hydrolysing the α-1,6-linked fucose of fucose-containing glycoproteins and glycolipids. Despite its clinical importance, the three-dimensional structure of human or other animal FUCA1 is not known. However, the high percentage of sequence identity (35%) with FUCA1 from Thermotoga maritima (TmFUCA1) [21] allows reliable modelling of human FUCA1 (HuFUCA1; Figure 3A), which is practically identical to the model generated by AlphaFold (rmsd 0.932 Å/298 Cα) [22]. R47 is localised at the catalytic domain of HuFUCA1, away from the active site, in the N-terminal α-helix, that in TmFUCA1 mediates the interactions between subunits of the molecular hexamer (Figure 3B). Sequence conservation between TmFUCA and HuFUCA1 sequences does not imply that they have equivalent architectures. Therefore, we cannot anticipate whether or not R47 will play a key role in maintaining the stability of the oligomer. What is certain is that the R47P mutation is not compatible with maintaining the amino-terminal helix of FUCA1. It is therefore predictable that the mutation may disrupt the helix, probably affecting the correct folding of the subunit, and consequently its stability, which may support the absence of α-fucosidase activity in the patient.
Figure 3.
Structural modelling and luciferase assays. (A,B) FUCA1 p.R47P. (A) Structural modelling on HuFUCA1 subunit. The catalytic and carboxy terminal domains are coloured differently. Localization of R47P is mapped with a red sphere. A molecule of fucose bound to the active site is shown in sticks representation. (B) Hexamer of TmFUCA1 (PDB 1ODU). Each subunit is shown with a different colour. The equivalent residue to R47 from HuFUCA1 is indicated by red spheres, to show its participation in the intersubunit surface. (C–E) ITPR1 p.Y552C: (C) The cryo-EM structure of ITPR1 tetramer (PDB 7LHE) is represented in an orientation along the membrane plane. Each subunit is shown with a different colour. Y552 is mapped in one of the subunits with a red sphere and labelled. (D,E) Detail of the IP3 binding site (D), PDB 1N4K, and modelling of the Y5552C variant (E). The side chain of tyrosine or cytosine at position 552 as well as those from the lysine/arginine cluster coordinating the phosphoryl groups of I3P are shown in stick representation. I3P is also shown in stick representation with carbon atoms coloured in yellow. Oxygen, nitrogen, phosphorus, and sulphur atoms are coloured red, blue, orange, and green respectively. (F) Luciferase assays to assess PLEKHG2 p.T53I and PNKD c.-4C>G variants in transfected HEK293T with expression constructs for wild-type (WT) and mutants. The luciferase activity was normalised to the WT. Data represent the mean ± SEM of three independent experiments performed in triplicate. * p < 0.05; n.s., not significant.
The inositol 1,4,5-trisphosphate (IP3) receptor (ITPR1), a tetrameric transmembrane channel located in the endoplasmic reticulum membrane (Figure 3C–E) [23], releases Ca2+ to the cytosol in response to IP3. The highly conserved Y552 is involved in I3P binding, and in fact, Y552A is known to reduce the binding of this ligand [24]. The considerable difference in size due to the change in Y552C places the reactive sulfhydryl group of the cysteine too far from the ligand to participate in its binding (Figure 3C). Thus, Y552C may affect the binding of I3P and consequently, may interfere with calcium release to the cytoplasm. This finding may indicate that the mutated protein would not work properly, although this cannot be established with certainty.
To investigate PLEKHG2 p.T53I and PNKD c.-4C>G, luciferase analyses were performed. PLEKHG2 is a RhoGTPase that catalyses the hydrolysis of guanosine triphosphate (GTP) to guanosine diphosphate (GDP), activated by heterotrimeric G protein βγ (Gβγ) subunits [25]. To assess whether the p.T53I mutation affects the activation of the PLEKHG2 downstream signalling pathway, we used a luciferase reporter assay in HEK293 cells under the control of the SRE promoter, whose transcription activity is known to be regulated by Rho GTPases. The transcriptional activation capacity expression of the mutated gene was significantly reduced by 25% compared to the control (Figure 3F). PNKD shares a high percentage of sequence identity (43%) with human hydroxyacylglutathione hydrolase (HAGH). The transcriptional activity of PNKD c.-4C>G resulted in a decrease to ~11% compared to the control (Figure 3F). For both variants, we detected altered luciferase activities. These in vitro findings do not guarantee with absolute certainty that the mutated protein has an abnormal activity.
Four novel mutations, located on the consensus sequence at splice sites, causing the loss of at least one exon were detected (Figure 4): CASK c.2589+2T>G led to the skipping of exon 26 (84 bp); PDGFB c.602-1G>C to exon 6 plus part of the 3′UTR (untranslated region; 153 bp); CPLANE1 c.7588+3A>G to exon 37 (55 bp); and PMPCA c.633+1G>A to exon 6 (101 bp).
Figure 4.
Impact on transcript processing of splicing mutations. Exons are indicated by boxes and introns are represented by horizontal bars (not to scale). Location of specific primers used in RT-PCR is indicated by arrows. Dotted lines represent the anomalous splicing outcome and sequences of the abnormal products are shown (electropherogram). Genomic mutations (in red) are harboured in a heterozygous state and the consensus transcript was also detected in patients’ samples further confirmed by specific band sequencing. (A–C) Reverse transcription-polymerase chain reaction (RT-PCR) products obtained from RNA of control and patients’ blood samples (agarose electrophoretic results) and schematic representation of the aberrant splicing events. (A) CASK c.2589+2T>G (MD-208) induces the complete skipping of exon 26, corresponding to the lower 402 bp band. (B) PDGFB c.602-1G>C (MD-173) causes the loss of the last exon of the gene plus 28 bp of the contiguous 3′ untranslated region (3′UTR) region presenting a 367 bp aberrant product absent in the healthy control. (C) CPLANE1 c.7588+3G>A (MD-216) resulted in single exon 37 skipping leading to an alternative transcript 55 bp shorter than the expected. (D) PMPCA exon 6 minigene assay. Agarose gel shows the band pattern of transcripts obtained after overexpression of pSPL3-derived constructs: wild-type (WT) allele, mutant allele c.633+1G>A and empty vector ø. SD6 and SA2 are the resident exons of the pSPL3 reporting vector. In the absence of an inserted fragment, a product of 263 bp is obtained. The analysed variant causes the skipping of exon 6. bp, base pair; Ct, control; FW, forward primer; RV, reverse primer.
We performed immunofluorescence assays to determine the subcellular localization of NIPA1 p.P91R (Table 3), using p.G106R as pathogenic control associated with aberrant protein subcellular distribution [26]. The immunofluorescence assays performed with several cell markers (M6PR, GRP94, and EEA1) revealed partial colocalisation with these markers, although no differences were observed compared to WT (data not shown). Notwithstanding, the expression pattern using Na+, K+ ATPase showed that the mutated NIPA1 protein was concentrated in a perinuclear distribution, whereas the WT protein was distributed throughout the cytoplasm (Figure S3), suggesting an abnormal trafficking of mutated proteins as was established for the NIPA1-associated HSP phenotype [26,27].
3. Discussion
Our clinical series comprised 124 patients with MDs and/or CA. Genes related to NBIA disorders were initially studied in cases with brain iron deposits and/or a complex MDs phenotype that included ataxia, spasticity, and/or peripheral neuropathy. This first approach yielded a conclusive diagnosis for 59 patients. Most patients were PKAN (35.96%) or PLAN (12.28%), which represent the two major NBIA types [1]. Only four patients suffered from other NBIA disorders (mutations in WDR45, FTL or CP). Another PLAN subject (MD-341) who was directly studied by WES-proband, was later diagnosed. Strikingly, no mutations in the remaining NBIA genes were identified in subsequent analyses, which highlights that the abnormal accumulation of brain iron can be due to a primary mutation, but also to the neurodegenerative process that accompanies the disease.
The haplotype for the PANK2 locus in Roma patients confirmed that p.T528M was a founder mutation in Spain, just as other mutations have been previously reported for several Mendelian diseases [28,29,30]. The Roma population makes up around 1.5% of the total Spanish population, thus representing one of the largest Roma communities in the world (http://www.unioromani.org). PANK2 p.T528M likely represents an ancestral mutational event, since Roma PKAN patients from Spain and from Hungary shared the haplotype. The PANK2 p.T528M-associated haplotype was also constructed in the non-Roma Greek heterozygous patients, which may be the outcome of mixing with neighbouring populations. Ultimately, the different haplotypes obtained for the non-Roma Spanish proband heterozygous for PANK2 p.T528M showed that the mutation has arisen in different occasions throughout history. In fact, this has been reported in non-Roma PKAN-affected subjects [31,32,33,34]. PANK2 p.T528M seems to be relatively frequent, likely because homozygous individuals present with a milder clinical picture [35], which may have made its transmission easier through generations in the Roma population.
MDs and ataxias are related to hundreds of genes with high phenotypic overlap. We developed a targeted method that tested between 498 genes in its first version [14] and 517 in its last version, as new genes of interest were reported. Our custom panel MovDisord displayed a capture with uniform coverage and high read depths in all samples, providing a cost-effective alternative, with a diagnosis success rate of 34.54% (19/55 patients). Nowadays, WES is probably the best strategy; WES-trio may yield ~40% of solved cases versus WES-proband with ~28% [36]. Nonetheless, we achieved a success rate of 70.0% (7/10 patients) and of 33.33% (3/9 patients) using WES-proband or WES-trio, respectively. It is worth mentioning that in the patients investigated by WES-trio, the most common genes were ruled out by the gene panel MovDisord. Altogether, we obtained a success rate of 52.63% (10/19 cases) using WES. In fact, WES-based strategies seem to display a diagnostic ceiling of ~50% [37], to a certain extent, due to the difficulty of interpreting new variants, hence the relevance of developing additional studies that help to understand their pathological nature.
In the sixty-five patients investigated by panel MovDisord and/or WES, seventeen novel variants were identified, one of them a premature stop codon that was assumed to be detrimental. Together with the cases previously reported [12,13,14,15,16,17], we achieved experimental evidence of damage for 14 of these new genetic changes. Unfortunately, for some mutations, the possible ad hoc analyses were beyond our possibilities. The studies performed for PNKD c.-4C>G and NIPA1 p.P91R deserve a special mention. The luciferase assay revealed that PNKD c.-4C>G, detected in an affected man and in his asymptomatic daughter, may have a decreased transcriptional activity, supporting that the proper activity of the enzyme may be altered. Although we cannot categorically establish the causality of PNKD c.-4C>G, individuals carrying PNKD mutations who remain apparently unaffected have been reported, and in fact, incomplete penetrance seems to be relatively common in paroxysmal nonkinesigenic dyskinesia [38,39]. This phenomenon may explain the absence of clinical signs in the proband’s daughter, although it is also possible that she presents the first symptoms in her forties like her father.
NIPA1 p.P91R was analysed by immunofluorescence and we concluded that intracellular trafficking would be impaired, as previously reported for other NIPA1 mutations causing HSP [26,27]. NIPA1 p.P91R was detected in a patient with a complex phenotype, who also suffered from a partial trisomy 18p and a partial monosomy 18q. Known syndromes due to a similar chromosomal alteration have nothing to do with MDs [40,41]. A patient with a partial deletion of the chromosome 18q was reported with a complex phenotype, which shared some neurological findings with our proband: intellectual disability, sensorineural hearing loss and dystonia [42]. It is not possible to establish the contribution of NIPA1 p.P91R to the clinical outcome with the available data.
In this cohort, 29 patients with phenotypes of MDs, spasticity, or ataxia were diagnosed with 23 distinct genetic conditions. Of those, five patients presented MDs such as dystonia or parkinsonism, spasticity, and suspicion of brain iron deposits or GP hypointensities; they were associated with variants in FBXO7, FUCA1, GLB1, TPP1, and KIF1A. In fact, isolated cases with GP hypointensities consistent with iron excess are known in at least 17 distinct genes [1], including AP4M1 and AP4S1, which, like FUCA1, GLB1, and TPP1, are involved in lysosomal disorders. Lysosomes are implicated in the recycling of membranes, autophagy and even iron metabolism. It is tempting to speculate that abnormal iron accumulation may result from a defect in intralysosomal recycling. Patients with NBIA phenotype on MRI and mutations in FUCA1 (1 case) or in GLB1 (4 cases) have been previously described [43,44,45,46,47]. To our knowledge, our proband MD-153 is the first case with the early appearance of GP hypointensities and TPP1 mutations. The three patients here described, MD-137 (FUCA1), MD-020 (GLB1), and MD-153 (TPP1), suffered from lysosomal diseases. Additionally, a subject with α-mannosidosis, also a lysosomal storage disease, who presented hypointensity signals in the GP was published [48]. Taken together, NBIA on MRI seems not to be so rare in some lysosomal disorders, especially in GM1-gangliosidosis, since so far, five unrelated cases are known (including our proband). Thus, GLB1 has been suggested as an NBIA gene [49], although this depends on the authors. Single cases with NBIA phenotype have been reported for several genes such as REPS1 or CRAT [50], and in occasions, they are described as NBIA genes [51], or as genes to be considered NBIA genes if additional cases are reported [52].
In 22 out of 29 solved patients, the phenotype was associated with CA, but only one was diagnosed with PLAN (MD-341). It is worth mentioning the early appearance of cerebellar cortical hyperintensities in seven patients with a non-progressive phenotype associated to variants in ITPR1 (3), SPTBN2 (2), PMPCA, and KIF1A genes, resembling the neuroimaging pattern recognised in neurodegenerative disorders such as PLAN, mitochondrial disorders, late onset GM2 gangliosidosis, and recently in our patient with PRDX3-associated neurodegeneration (PRAN) [17]. This paradox has already been described in other patients with ataxia and mutations in KIF1A, ITPR1, and PMPCA but also in KCNC3, and CACNA1A genes [53,54,55]. It has been presumed that the bright cortex in the cerebellum is a reactive gliosis to the neuronal cell loss and axonal swelling, but different hypotheses are pending to explain how diverse genetic disorders affecting predominantly the cerebellum early in life can present a neurodegenerative sign on neuroimaging, but stable or even improving neurodevelopment over the years. In addition, the three patients with ITPR1 mutations also had a superior CA, a pattern very recently proposed to be related to ITPR1 in 83% of a cohort that included carriers of the p.T267M and p.R269W variants like two of our patients [51].
Globally, our cohort presented a high phenotypic overlap as reported in MDs, ataxias, and NBIA disorders [1,2], with non-classical NBIA genes involved. Interestingly, two probands presented MDs, CA, and brain iron deposits or GP hypointensities, carrying mutations in FBXO7 and TPP1, respectively. Spasticity and CA were a common combination in 10 patients with variants in FBXO7, PLEKHG2, TPP1, ITPR1, KIF1A, and SPG7 genes; ataxia was also present in those with ITPR1, KIF1A, and SPG7 mutations; two probands with mutations in EXOSC3 suffered from early severe encephalopathy and CA, with progressive motor neuron signs after the first years of life.
4. Material and Methods
4.1. Patients
The study was conducted in accordance with the Declaration of Helsinki, and was approved by the Ethic Committees at Hospital Sant Joan de Déu in Barcelona (protocol code PIC-27-15 dated 12 March 2015) and Hospital Universitari i Politècnic La Fe in València (protocol codes: 2019/0052 dated 22 May 2019, and 2021/65/1 dated 22 September 2021).
Our cohort comprised 124 paediatric and adult patients with MDs and/or CA. PLAN and PKAN cohorts were previously described [5,35]. Acquired aetiologies were fully excluded in all of them. Demographic and familial history was systematically collected. Phenotyping included standardised assessments of ataxia, MDs, and other neurological symptoms such as spasticity, muscle weakness, or signs of peripheral neuropathy. Based on the phenotypic traits, we classified the patients according to two clinical presentations: (1) MDs such as dystonia, parkinsonism or tremor; spasticity; with or without brain iron deposits; (2) Early-onset ataxia or encephalopathy and CA, with or without brain iron deposits.
4.2. Neuroimaging Approaches
Brain MRI studies were performed in 1.5- and 3-T scanners, depending on the referral hospitals. The identification of iron deposit signs in basal ganglia, particularly in globus pallidus (GP) and substantia nigra (SN), was ascertained by iron-sensitive sequences, especially susceptibility weighted imaging (SWI) and T2-weighted imaging (T2WI). In MRI studies without these specific sequences, T2-weighted (T2W) hypointensities in basal ganglia were considered only suspicious with regard to iron deposits, according to normal age-dependent signals [3]. CA was ascertained by loss of cerebellar volume in at least two consecutive cerebral MRI studies. To assess the progression of CA, a quantitative analysis by mid-sagittal vermis relative diameter (MVRD) was performed in cerebral MRIs [5,13]. Additionally, cerebellar cortical hyperintensities were ascertained on T2-weighted or FLAIR MRI sequences, since they are associated with neurodegenerative phenotypes as PLAN [5].
4.3. Genetic and Genomic Studies
4.3.1. Genetic Analysis of NBIA Genes
In the first phase, the study was conducted based on the patients’ clinical findings. In 114 patients, the main NBIA genes, PANK2, PLA2G6, WDR45, FTL, and CP, were screened by Sanger sequencing as previously described [5,35], including the analysis of large deletions and/or duplications in PANK2 and PLA2G6 by Multiplex Ligation-dependent Probe Amplification (SALSA MLPA probemix P120, MRC Holland, Amsterdam, The Netherlands) (Figure 1).
To investigate if the PANK2 c.1583C>T (rs137852967) detected in homozygosis in Roma patients was a founder mutation, we constructed the haplotype for the PANK2 locus. We included eight homozygous Roma probands from Spain (7) and from Hungary (1), and four heterozygous non-Roma probands from Greece (3) and from Spain (1). We selected five extragenic markers (3 microsatellites and 2 SNPs) and three intragenic SNPs from the UCSC Genome Browser (https://genome.ucsc.edu/, accessed on 4 November 2021), the GeneLoc (https://genecards.weizmann.ac.il/geneloc/index.shtml, accessed on 4 November 2021) or the dbSNP (https://www.ncbi.nlm.nih.gov/snp/, accessed on 4 November 2021), which spanned a 1.06 Mb region flanking the PANK2 gene: cen_rs1078152-D20S867-rs6084513-rs137852967-rs6037695-rs7270329-D20S889-D20S116-rs1628323_tel. Protocol has been described previously [56]. Forward PCR primers (available upon request) were labelled with FAM fluorescent dyes (Sigma Aldrich, St. Louis, MO, USA). Amplicons were electrophoresed using an ABI3730xl (Applied Biosystems, Foster City, CA, USA) and analysed with the Peak Scanner Software v2.0, at the Service of Genomics and Translational Genetics (CIPF, Valencia, Spain).
4.3.2. Gene Panel, WES and Chromosomal Microarray Analysis
The 55 remaining patients without a conclusive result after the analysis of the NBIA genes were investigated using a custom panel MovDisord (Figure 1). The Table S1 shows the 517 genes involved in MDs and ataxia included in the last version of the panel MovDisord, which was reported in its first version [14].
Later, nine remaining patients without genetic diagnoses were investigated by WES-trio, and to compare panel genes versus WES, 10 additional patients were directly investigated by WES-proband as previously reported [17], except for patient MD-277, which was investigated as previously reported [12].
Bioinformatics analyses (filtering data, study of the novelty of the candidate variants and CNVs, copy number variants) were carried out as previously described [17]. WES data from unsolved patients were recently reanalysed using the platform RD Connect Genome-Phenome Analysis Platform (https://platform.rd-connect.eu/, accessed on 4 November 2021).
Molecular karyotype was performed using genomic DNA from peripheral blood leukocytes and the CytoScan 750 K Array platform (Affymetrix Inc., Santa Clara, CA, USA) according to the manufacturer’s protocol. Hybridised arrays were scanned on an Affymetrix GeneChip Scanner 3000 and the resulting files were analysed with Chromosome Analysis Suite (ChAS) (Affymetrix Inc., Santa Clara, CA, USA) software v3.1, based on the reference genome sequence of the UCSC Genome Browser hg19. DGV (http://dgv.tcag.ca/dgv/app/home, accessed on 16 July 2021) and DECIPHER (https://decipher.sanger.ac.uk/, accessed on 16 July 2021) were used for the interpretation of CNVs.
4.4. Studies to Investigate the Pathogenicity of Novel Variants
4.4.1. Structural Modelling: ITPR1 and FUCA1
Figure 3 was prepared using PYMOL Molecular Graphics System, v2.0 Schrödinger, LLC (https://pymol.org, accessed on 15 September 2021). ITPR1 p.Y552C was modelled in the crystal structure of the IP3 binding domain of ITPR1 (residues 236-602, PDB entry 1N4K) [24]. FUCA1 p.R47P was modelled by SWISS-MODEL [57], from the crystal structure of TmFUCA1 (PDB entries 1HL8, 1HL9 and 1ODU) [21].
4.4.2. Luciferase Reporter Assays: PLEKHG2 and PNKD
The reporter vector pGL4.33[luc2P/SRE/Hygro] (Promega, Madison, WI, USA) and PLEKHG2 (NM_022835.3) cloned into the pcDNA3.1:myc (N-ter) vector, kindly ceded by Dr. Chen Songhai [25], were employed in PLEKHG2 assays. For PNKD, a fragment of 933 bp of the 5’ upstream sequence of the gene was amplified by PCR from a healthy control using the Herculase II Fusion DNA Polymerase (Agilent Technologies, Foster City, CA, USA) and cloned into the pGL4.24[luc2P/minP] reporter vector (Promega, Madison, WI, USA) between XhoI/HindIII restriction sites. The mutants (PLEKHG2 p.T53I and PNKD c.-4C>G) were obtained using the aforementioned technique. Primers are available upon request. HEK293T cells were cultured with complete DMEM (supplemented with 10% heat-inactivated FBS, 5 g/L D-glucose, 1% P/S and 1% L-glutamine) in 24-well plates. The following day, cells were transiently transfected using FuGENE HD Transfection Reagent (Promega, Madison, WI, USA) with the pertinent pGL4 constructs, and renilla luciferase normalisation vector (pRL-TK) with different p.GL4: pRL-TK ratio for each experiment, being 30:1 for PNKD and 3:1 for PLEKHG2. Furthermore, in the case of PLEKHG2, the pGL4.33[luc2P/SRE/Hygro] vector was co-transfected with wild type or mutated PLEKHG2 and after six hours the cell medium was changed to complete DMEM without FBS, as previously described [25,58]. For both assays, after 24 h, luciferase activity was assessed using the Dual-Luciferase® Reporter Assay System (Promega, Madison, WI, USA). Three independent experiments were carried out for statistical analysis by unpaired two-sample t test.
4.4.3. Transcript Analysis and Minigenes: CASK, PDGFB, CPLANE1/C5orf42 and PMPCA
Protocols for both approaches are described in Sánchez-Monteagudo et al. [59]. Primers are available upon request.
4.4.4. NIPA1 Subcellular Location
The NIPA1 (NM_144599.4) tagged with FLAG in C-ter and cloned in pcDNA3.1 vector was acquired from GenEZ™ ORF cDNA Clones (GenScript, Piscataway, NJ, USA). The NIPA1 p.P91R and p.G106R missense mutations were introduced using a Site-Directed Mutagenesis kit (Agilent, Santa Clara, CA, USA) using specific primers for each mutation (available upon request). HeLa cells were grown in complete DMEM and transiently transfected with 2 µg of NIPA1 wild-type (WT), p.P91R, or p.G106R with FuGENE HD Transfection Reagent (Promega, Madison, WI, USA). After 24 h, the cells were fixed, permeabilised and blocked as previously described [13]. The samples were incubated with the primary antibodies anti-FLAG (Sigma-Aldrich, Saint Louis, MO, USA) and anti-Na+/K+-ATPase, anti-mannose-6-phosphate receptor (M6PR), anti-glucose-regulated protein 94 KDa (GRP94), or anti-early endosome antigen 1 (EEA1; Abcam, Cambridge, UK). The following day, they were exposed to the appropriate secondary antibodies conjugated with fluorophores (Invitrogen, Carlsbad, CA, USA) and examined using the SP2-Leica confocal microscope (Leica, Wetzlar, Germany).
5. Conclusions
The NGS technology has made it possible to accelerate the diagnosis of Mendelian MDs, but the number of unsolved cases is still too high. The interpretation of the genetic variants and their phenotypic consequences is a challenge. The low prevalence of each clinical form, the great genetic heterogeneity, and the notable variable expressivity complicate the diagnosis. This report adds new genetic and clinical pieces to the puzzle of MDs and/or ataxias, and contributes to improving the genetic counselling and care of these patients with rare diseases. We have to work hard in order to “enable all people living with a rare disease to receive an accurate diagnosis, care and available therapy within one year of coming to medical attention” [60].
Acknowledgments
We are in debt with the patients and their families for agreeing to participate in this study. We thank Maria Judit Molnar and Renáta Bencsi who kindly provided a sample of a Hungarian patient carrier of the PANK2 p.T528M.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijms231911847/s1.
Author Contributions
Funding acquisition, B.P.-D. and C.E.; investigation, D.M.-R., I.H., P.S., N.G.-R., R.B.-F., C.T., C.M.-M., I.M.-C., M.J.M.-G., A.G.-R., R.B.-M., I.S.-B., I.M.-T., A.D.-R., P.J., E.M. (Esther Moreno), L.P.-P., M.O.G., Á.R.-G., E.M. (Esteban Muñoz), M.J.M., A.S.-M., C.F., A.A.-B., R.M.P., S.J.-M., P.M., V.L., B.P.-D., A.D., S.A.-A. and C.E.; writing—original draft, S.A.-A. and C.E.; writing—review and editing, S.A.-A. and C.E. All authors have read and agreed to the published version of the manuscript.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information.
Conflicts of Interest
The authors declare that they have no competing interests.
Funding Statement
This work was supported by the Instituto de Salud Carlos III (ISCIII)—Subdirección General de Evaluación y Fomento de la Investigación within the framework of the National R + D+I Plan co-funded with European Regional Development Funds (ERDF) [Grants PI18/00147 and PI21/00103 to CE]; the Fundació La Marató TV3 [Grants 20143130 and 20143131 to BPD and CE]; and by the Generalitat Valenciana [Grant PROMETEO/2018/135 to CE]. Part of the equipment employed in this work was funded by Generalitat Valenciana and co-financed with ERDF (OP ERDF of Comunitat Valenciana 2014–2020). PS had an FPU-PhD fellowship funded by the Spanish Ministry of Education, Culture and Sport [FPU15/00964]. IH has a PFIS-PhD fellowship [FI19/00072]. ASM has a contract funded by the Spanish Foundation Per Amor a l’Art (FPAA).
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hinarejos I., Machuca-Arellano C., Sancho P., Espinos C. Mitochondrial Dysfunction, Oxidative Stress and Neuroinflammation in Neurodegeneration with Brain Iron Accumulation (NBIA) Antioxidants. 2020;9:1020. doi: 10.3390/antiox9101020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tello C., Darling A., Lupo V., Pérez-Dueñas B., Espinós C. On the complexity of clinical and molecular bases of neurodegeneration with brain iron accumulation. Clin. Genet. 2018;93:731–740. doi: 10.1111/cge.13057. [DOI] [PubMed] [Google Scholar]
- 3.Lee J.H., Yun J.Y., Gregory A., Hogarth P., Hayflick S.J. Brain MRI Pattern Recognition in Neurodegeneration with Brain Iron Accumulation. Front. Neurol. 2020;11:1024. doi: 10.3389/fneur.2020.01024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhou B., Westaway S.K., Levinson B., Johnson M.A., Gitschier J., Hayflick S.J. A novel pantothenate kinase gene (PANK2) is defective in Hallervorden-Spatz syndrome. Nat. Genet. 2001;28:345–349. doi: 10.1038/ng572. [DOI] [PubMed] [Google Scholar]
- 5.Darling A., Aguilera-Albesa S., Tello C.A., Serrano M., Tomas M., Camino-Leon R., Fernandez-Ramos J., Jimenez-Escrig A., Poo P., O’Callaghan M., et al. PLA2G6-associated neurodegeneration: New insights into brain abnormalities and disease progression. Park. Relat. Disord. 2019;61:179–186. doi: 10.1016/j.parkreldis.2018.10.013. [DOI] [PubMed] [Google Scholar]
- 6.Montaut S., Tranchant C., Drouot N., Rudolf G., Guissart C., Tarabeux J., Stemmelen T., Velt A., Fourrage C., Nitschke P., et al. Assessment of a Targeted Gene Panel for Identification of Genes Associated with Movement Disorders. JAMA Neurol. 2018;75:1234–1245. doi: 10.1001/jamaneurol.2018.1478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sun M., Johnson A.K., Nelakuditi V., Guidugli L., Fischer D., Arndt K., Ma L., Sandford E., Shakkottai V., Boycott K., et al. Targeted exome analysis identifies the genetic basis of disease in over 50% of patients with a wide range of ataxia-related phenotypes. Genet. Med. 2018;21:195–206. doi: 10.1038/s41436-018-0007-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Coutelier M., Hammer M.B., Stevanin G., Monin M.L., Davoine C.S., Mochel F., Labauge P., Ewenczyk C., Ding J., Gibbs J.R., et al. Efficacy of Exome-Targeted Capture Sequencing to Detect Mutations in Known Cerebellar Ataxia Genes. JAMA Neurol. 2018;75:591–599. doi: 10.1001/jamaneurol.2017.5121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Elert-Dobkowska E., Stepniak I., Krysa W., Ziora-Jakutowicz K., Rakowicz M., Sobanska A., Pilch J., Antczak-Marach D., Zaremba J., Sulek A. Next-generation sequencing study reveals the broader variant spectrum of hereditary spastic paraplegia and related phenotypes. Neurogenetics. 2019;20:27–38. doi: 10.1007/s10048-019-00565-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.D’Amore A., Tessa A., Casali C., Dotti M.T., Filla A., Silvestri G., Antenora A., Astrea G., Barghigiani M., Battini R., et al. Next Generation Molecular Diagnosis of Hereditary Spastic Paraplegias: An Italian Cross-Sectional Study. Front. Neurol. 2018;9:981. doi: 10.3389/fneur.2018.00981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Richards S., Aziz N., Bale S., Bick D., Das S., Gastier-Foster J., Grody W.W., Hegde M., Lyon E., Spector E., et al. Standards and guidelines for the interpretation of sequence variants: A joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet. Med. 2015;17:405–424. doi: 10.1038/gim.2015.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jesús S., Hinarejos I., Carrillo F., Martínez-Rubio M.D., Macías-García D., Sánchez-Monteagudo A., Adarmes A., Lupo V., Pérez-Dueñas B., Mir P., et al. NR4A2 is involved in dystonia-parkinsonism with intellectual disability, language impairment and motor tics. Neurol. Genet. 2021;7:e543. doi: 10.1212/NXG.0000000000000543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sancho P., Andrés-Bordería A., Gorría-Redondo N., Llano K., Martínez-Rubio D., Yoldi-Petri M.E., Blumkin L., Rodríguez de la Fuente P., Gil-Ortiz F., Fernández-Murga L., et al. Expanding the β-III spectrin-associated phenotypes toward non-progressive congenital ataxias with neurodegeneration. Int. J. Mol. Sci. 2021;22:2505. doi: 10.3390/ijms22052505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Correa-Vela M., Lupo V., Montpeyo M., Sancho P., Marce-Grau A., Hernandez-Vara J., Darling A., Jenkins A., Fernandez-Rodriguez S., Tello C., et al. Impaired proteasome activity and neurodegeneration with brain iron accumulation in FBXO7 defect. Ann. Clin. Transl. Neurol. 2020;7:1436–1442. doi: 10.1002/acn3.51095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Campins-Romeu M., Baviera-Munoz R., Sastre-Bataller I., Bataller L., Jaijo T., Martinez-Torres I. Hereditary Spastic Paraplegia 7 Presenting as Multifocal Dystonia with Prominent Cranio-Cervical Involvement. Mov. Disord. Clin. Pract. 2021;8:966–968. doi: 10.1002/mdc3.13257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Baviera-Munoz R., Martinez-Rubio D., Sastre-Bataller I., Campins-Romeu M., Losada-Lopez M., Perez-Garcia J., Novella-Maestre E., Martinez-Torres I., Espinos C. A 3.9-Mb Deletion on 2p11.2 Comprising the REEP1 Gene Causes Early-Onset Atypical Parkinsonism. Neurol. Genet. 2021;7:e642. doi: 10.1212/NXG.0000000000000642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Martinez-Rubio D., Rodriguez-Prieto A., Sancho P., Navarro-Gonzalez C., Gorria-Redondo N., Miquel-Leal J., Marco-Marin C., Jenkins A., Soriano-Navarro M., Hernandez A., et al. Protein misfolding and clearance in the pathogenesis of a new infantile onset ataxia caused by mutations in PRDX3. Hum. Mol. Genet. 2022:ddac146. doi: 10.1093/hmg/ddac146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bertini E., Zanni G., Boltshauser E. Nonprogressive congenital ataxias. Handb Clin. Neurol. 2018;155:91–103. doi: 10.1016/B978-0-444-64189-2.00006-8. [DOI] [PubMed] [Google Scholar]
- 19.Baviera-Munoz R., Campins-Romeu M., Carretero-Vilarroig L., Sastre-Bataller I., Martinez-Torres I., Vazquez-Costa J.F., Muelas N., Sevilla T., Vilchez J.J., Aller E., et al. Clinical and genetic characteristics of 21 Spanish patients with biallelic pathogenic SPG7 mutations. J. Neurol. Sci. 2021;429:118062. doi: 10.1016/j.jns.2021.118062. [DOI] [PubMed] [Google Scholar]
- 20.Jonch A.E., Douard E., Moreau C., Van Dijck A., Passeggeri M., Kooy F., Puechberty J., Campbell C., Sanlaville D., Lefroy H., et al. Estimating the effect size of the 15q11.2 BP1-BP2 deletion and its contribution to neurodevelopmental symptoms: Recommendations for practice. J. Med. Genet. 2019;56:701–710. doi: 10.1136/jmedgenet-2018-105879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sulzenbacher G., Bignon C., Nishimura T., Tarling C.A., Withers S.G., Henrissat B., Bourne Y. Crystal structure of Thermotoga maritima alpha-L-fucosidase. Insights into the catalytic mechanism and the molecular basis for fucosidosis. J. Biol. Chem. 2004;279:13119–13128. doi: 10.1074/jbc.M313783200. [DOI] [PubMed] [Google Scholar]
- 22.Jumper J., Evans R., Pritzel A., Green T., Figurnov M., Ronneberger O., Tunyasuvunakool K., Bates R., Zidek A., Potapenko A., et al. Highly accurate protein structure prediction with AlphaFold. Nature. 2021;596:583–589. doi: 10.1038/s41586-021-03819-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fan G., Baker M.L., Wang Z., Baker M.R., Sinyagovskiy P.A., Chiu W., Ludtke S.J., Serysheva I.I. Gating machinery of InsP3R channels revealed by electron cryomicroscopy. Nature. 2015;527:336–341. doi: 10.1038/nature15249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bosanac I., Alattia J.R., Mal T.K., Chan J., Talarico S., Tong F.K., Tong K.I., Yoshikawa F., Furuichi T., Iwai M., et al. Structure of the inositol 1,4,5-trisphosphate receptor binding core in complex with its ligand. Nature. 2002;420:696–700. doi: 10.1038/nature01268. [DOI] [PubMed] [Google Scholar]
- 25.Edvardson S., Wang H., Dor T., Atawneh O., Yaacov B., Gartner J., Cinnamon Y., Chen S., Elpeleg O. Microcephaly-dystonia due to mutated PLEKHG2 with impaired actin polymerization. Neurogenetics. 2016;17:25–30. doi: 10.1007/s10048-015-0464-y. [DOI] [PubMed] [Google Scholar]
- 26.Zhao J., Matthies D.S., Botzolakis E.J., Macdonald R.L., Blakely R.D., Hedera P. Hereditary spastic paraplegia-associated mutations in the NIPA1 gene and its Caenorhabditis elegans homolog trigger neural degeneration in vitro and in vivo through a gain-of-function mechanism. J. Neurosci. 2008;28:13938–13951. doi: 10.1523/JNEUROSCI.4668-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Goytain A., Hines R.M., El-Husseini A., Quamme G.A. NIPA1(SPG6), the basis for autosomal dominant form of hereditary spastic paraplegia, encodes a functional Mg2+ transporter. J. Biol. Chem. 2007;282:8060–8088. doi: 10.1074/jbc.M610314200. [DOI] [PubMed] [Google Scholar]
- 28.Sevilla T., Martinez-Rubio D., Marquez C., Paradas C., Colomer J., Jaijo T., Millan J.M., Palau F., Espinos C. Genetics of the Charcot-Marie-Tooth disease in the Spanish Gypsy population: The hereditary motor and sensory neuropathy-Russe in depth. Clin. Genet. 2013;83:565–570. doi: 10.1111/cge.12015. [DOI] [PubMed] [Google Scholar]
- 29.Casana P., Martinez F., Haya S., Lorenzo J.I., Espinos C., Aznar J.A. Q1311X: A novel nonsense mutation of putative ancient origin in the von Willebrand factor gene. Br. J. Haematol. 2000;111:552–555. doi: 10.1046/j.1365-2141.2000.02410.x. [DOI] [PubMed] [Google Scholar]
- 30.Gil-Pena H., Coto E., Santos F., Espino M., Cea Crespo J.M., Chantzopoulos G., Komianou F., Gomez J., Alonso B., Iglesias S., et al. A new SLC12A3 founder mutation (p.Val647Met) in Gitelman’s syndrome patients of Roma ancestry. Nefrologia. 2017;37:423–428. doi: 10.1016/j.nefro.2017.01.007. [DOI] [PubMed] [Google Scholar]
- 31.Wu Y.W., Hess C.P., Singhal N.S., Groden C., Toro C. Idiopathic basal ganglia calcifications: An atypical presentation of PKAN. Pediatr. Neurol. 2013;49:351–354. doi: 10.1016/j.pediatrneurol.2013.06.021. [DOI] [PubMed] [Google Scholar]
- 32.Dusek P., Tovar Martinez E.M., Madai V.I., Jech R., Sobesky J., Paul F., Niendorf T., Wuerfel J., Schneider S.A. 7-Tesla Magnetic Resonance Imaging for Brain Iron Quantification in Homozygous and Heterozygous PANK2 Mutation Carriers. Mov. Disord. Clin. Pract. 2014;1:329–335. doi: 10.1002/mdc3.12080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Akcakaya N.H., Iseri S.U., Bilir B., Battaloglu E., Tekturk P., Gultekin M., Akar G., Yigiter R., Hanagasi H., Alp R., et al. Clinical and genetic features of PKAN patients in a tertiary centre in Turkey. Clin. Neurol. Neurosurg. 2017;154:34–42. doi: 10.1016/j.clineuro.2017.01.011. [DOI] [PubMed] [Google Scholar]
- 34.Yapici Z., Akcakaya N.H., Tekturk P., Iseri S.A., Ozbek U. A novel gene mutation in PANK2 in a patient with severe jaw-opening dystonia. Brain Dev. 2016;38:755–758. doi: 10.1016/j.braindev.2016.02.010. [DOI] [PubMed] [Google Scholar]
- 35.Darling A., Tello C., Martí M.J., Garrido C., Aguilera-Albesa S., Tomás Vila M., Gastón I., Madruga M., González Gutiérrez L., Ramos Lizana J., et al. Clinical rating scale for pantothenate kinase-associated neurodegeneration: A pilot study. Mov. Disord. 2017;32:1620–1630. doi: 10.1002/mds.27129. [DOI] [PubMed] [Google Scholar]
- 36.Wright C.F., FitzPatrick D.R., Firth H.V. Paediatric genomics: Diagnosing rare disease in children. Nat. Rev. Genet. 2018;19:325. doi: 10.1038/nrg.2018.12. [DOI] [PubMed] [Google Scholar]
- 37.Ngo K.J., Rexach J.E., Lee H., Petty L.E., Perlman S., Valera J.M., Deignan J.L., Mao Y., Aker M., Posey J.E., et al. A diagnostic ceiling for exome sequencing in cerebellar ataxia and related neurological disorders. Hum. Mutat. 2020;41:487–501. doi: 10.1002/humu.23946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Djarmati A., Svetel M., Momcilovic D., Kostic V., Klein C. Significance of recurrent mutations in the myofibrillogenesis regulator 1 gene. Arch. Neurol. 2005;62:1641. doi: 10.1001/archneur.62.10.1641-a. [DOI] [PubMed] [Google Scholar]
- 39.Panedey S., Ramkumarsingh L., Mahadevan L. Progressive nonparoxysmal chorea and dystonia due to myofibrillogenesis regulator-1 gene mutation. Park. Relat. Disord. 2019;60:186–187. doi: 10.1016/j.parkreldis.2018.08.019. [DOI] [PubMed] [Google Scholar]
- 40.Bartels E., Draaken B., Kazmierczak B., Spranger S., Schramm C., Baudisch F., Nöthen M.M., Schmiedeke E., Ludwig M., Reutter H. De novo partial trisomy 18p and partial monosomy 18q in a patient with anorectal malformation. Cytogenet. Genome Res. 2011;134:243–248. doi: 10.1159/000328833. [DOI] [PubMed] [Google Scholar]
- 41.Hu H., Hao J., Yao H., Chang Q., Li R., Zhang X., Liang Z. Prenatal diagnosis of de novo partial trisomy 18p and partial monosomy 18q recurrent in a family with fatal aortic coarctation. Gene. 2013;517:132–136. doi: 10.1016/j.gene.2012.12.001. [DOI] [PubMed] [Google Scholar]
- 42.Gordon M.F., Bressman S., Brin M.F., de Leon D., Warburton D., Yeboa K., Fahn S. Dystonia in a patient with deletion of 18q. Mov. Disord. 1995;10:496–499. doi: 10.1002/mds.870100415. [DOI] [PubMed] [Google Scholar]
- 43.Gautschi M., Merlini L., Calza A.M., Hayflick S., Nuoffer J.M., Fluss J. Late diagnosis of fucosidosis in a child with progressive fixed dystonia, bilateral pallidal lesions and red spots on the skin. Eur. J. Paediatr. Neurol. 2014;18:516–519. doi: 10.1016/j.ejpn.2014.02.005. [DOI] [PubMed] [Google Scholar]
- 44.Tanaka R., Momoi T., Yoshida A., Okumura M., Yamakura S., Takasaki Y., Kiyomasu T., Yamanaka C. Type 3 GM1 gangliosidosis: Clinical and neuroradiological findings in an 11-year-old girl. J. Neurol. 1995;242:299–303. doi: 10.1007/BF00878872. [DOI] [PubMed] [Google Scholar]
- 45.De Grandis E., Di Rocco M., Pessagno A., Veneselli E., Rossi A. MR imaging findings in 2 cases of late infantile GM1 gangliosidosis. AJNR Am. J. Neuroradiol. 2009;30:1325–1327. doi: 10.3174/ajnr.A1508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Vieira J.P., Conceicao C., Scortenschi E. GM1 gangliosidosis, late infantile onset dystonia, and T2 Hypointensity in the globus pallidus and substantia Nigra. Pediatr. Neurol. 2013;49:195–197. doi: 10.1016/j.pediatrneurol.2013.02.003. [DOI] [PubMed] [Google Scholar]
- 47.Takenouchi T., Kosaki R., Nakabayashi K., Hata K., Takahashi T., Kosaki K. Paramagnetic signals in the globus pallidus as late radiographic sign of juvenile-onset GM1 gangliosidosis. Pediatr. Neurol. 2015;52:226–229. doi: 10.1016/j.pediatrneurol.2014.09.022. [DOI] [PubMed] [Google Scholar]
- 48.Zoons E., de Koning T.J., Abeling N.G., Tijssen M.A. Neurodegeneration with Brain Iron Accumulation on MRI: An Adult Case of alpha-Mannosidosis. JIMD Rep. 2012;4:99–102. doi: 10.1007/8904_2011_78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hajirnis O., Udwadia-Hegde A. Chronic GM1 gangliosidosis with characteristic “wish bone sign” on brain MRI. Another type of neurodegeneration with brain iron accumulation? Mov. Disord.Clin. Pract. 2015;2:323–325. doi: 10.1002/mdc3.12197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Drecourt A., Babdor J., Dussiot M., Petit F., Goudin N., Garfa-Traoré M., Habarou F., Bole-Feysot C., Nitschke P., Ottolenghi C., et al. Impaired transferrin receptor palmitoylation and recycling in neurodegeneration with brain iron accumulation. Am. J. Hum. Genet. 2018;102:266–277. doi: 10.1016/j.ajhg.2018.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kolarova H., Tan J., Strom T.M., Meitinger T., Wagner M., Klopstock T. Lifetime risk of autosomal recessive neurodegeneration with brain iron accumulation (NBIA) disorders calculated from genetic databases. EBioMedicine. 2022;77:103869. doi: 10.1016/j.ebiom.2022.103869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Dusek P., Hofer T., Alexander J., Roos P.M., Aaseth J.O. Cerebral iron deposition in neurodegeneration. Biomolecules. 2022;12:714. doi: 10.3390/biom12050714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bolthauser E., Schmahmann J. Clinics in Developmental Medicine. 1st ed. Volume 191–192. John Wiley & Sons, I.; Hoboken, NJ, USA: 2012. Cerebellar Disorders in Children; p. 415. [Google Scholar]
- 54.Jobling R.K., Assoum M., Gakh O., Blaser S., Raiman J.A., Mignot C., Roze E., Durr A., Brice A., Levy N., et al. PMPCA mutations cause abnormal mitochondrial protein processing in patients with non-progressive cerebellar ataxia. Brain. 2015;138:1505–1517. doi: 10.1093/brain/awv057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Romaniello R., Pasca L., Panzeri E., D’Abrusco F., Travaglini L., Serpieri V., Signorini S., Aiello C., Bertini E., Bassi M.T., et al. Superior Cerebellar Atrophy: An Imaging Clue to Diagnose ITPR1-Related Disorders. Int. J. Mol. Sci. 2022;23:6723. doi: 10.3390/ijms23126723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Vanegas M.I., Marce-Grau A., Marti-Sanchez L., Mellid S., Baide-Mairena H., Correa-Vela M., Cazurro A., Rodriguez C., Toledo L., Fernandez-Ramos J.A., et al. Delineating the motor phenotype of SGCE-myoclonus dystonia syndrome. Park. Relat. Disord. 2020;80:165–174. doi: 10.1016/j.parkreldis.2020.09.023. [DOI] [PubMed] [Google Scholar]
- 57.Bienert S., Waterhouse A., de Beer T.A., Tauriello G., Studer G., Bordoli L., Schwede T. The SWISS-MODEL Repository-new features and functionality. Nucleic Acids Res. 2017;45:D313–D319. doi: 10.1093/nar/gkw1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Runne C., Chen S. PLEKHG2 promotes heterotrimeric G protein beta gamma-stimulated lymphocyte migration via Rac and Cdc42 activation and actin polymerization. Mol. Cell. Biol. 2013;33:4294–4307. doi: 10.1128/MCB.00879-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sanchez-Monteagudo A., Alvarez-Sauco M., Sastre I., Martinez-Torres I., Lupo V., Berenguer M., Espinós C. Genetics of Wilson disease and Wilson-like phenotype in a clinical series from eastern Spain. Clin. Genet. 2020;97:758–763. doi: 10.1111/cge.13719. [DOI] [PubMed] [Google Scholar]
- 60.Austin C.P., Cutillo C.M., Lau L.P.L., Jonker A.H., Rath A., Julkowska D., Thomson D., Terry S.F., de Montleau B., Ardigo D., et al. International Rare Diseases Research, C. Future of Rare Diseases Research 2017–2027: An IRDiRC Perspective. Clin. Transl. Sci. 2018;11:21–27. doi: 10.1111/cts.12500. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information.