Abstract
Introduction: TTFields plus Temozolomide (TTFields/TMZ) extended survival versus TMZ alone in newly diagnosed glioblastoma (GBM) patients in the EF-14 trial. We have reported a retrospective analysis of newly diagnosed Chinese GBM patients who received TTFields/TMZ treatment and TMZ treatment from August 2018 to May 2021 in Huashan hospital in Shanghai. Methods: Overall survival (OS) and progression-free survival (PFS) curves were constructed using the Kaplan–Meier method. A Cox proportional hazards regression model, propensity score matched data, and inverse probability of treatment weighting (IPTW) based on propensity score were used to assess the effect of TTFields and account for confounding factors. Results: In the preliminary analysis, the median PFS in TTFields/TMZ group was 16 months (95% CI, 9.6–24.6) versus 11 months (95% CI, 9–12) in TMZ group (p < 0.05). Median overall survival was 21.8 months (95% CI, 17.4-NA) with TTFields/TMZ versus 15 months (HR = 0.43; 95% CI, 13–18) with TMZ alone. The multivariate analysis identified surgery type, STUPP scheme, IDH status, and TTFields use as favorable prognostic factors. After PSM adjustment, the variate among the groups was similar, except that the methylation rate of MGMT promoter remained high in the TMZ group (12 v 32 months; p = 0.011). Upon IPTW Survival analysis, TTFields was associated with a significantly lower risk of death (HR = 0.19 in OS; 95% CI, 0.09–0.41) and progression (HR = 0.35; 95% CI 0.14–0.9) compared with TMZ group. Conclusion: In the final analysis of our single-center Chinese patients with glioblastoma, adding TTFields to temozolomide chemotherapy resulted in statistically significant improvement in PFS and OS.
Keywords: glioblastoma, tumor treating fields, chemotherapy, retrospective cohort
1. Introduction
Adult glioblastoma is one of the most fatal and challenging diseases and is associated with repeated recurrence and inferior prognosis [1,2,3]. Multimodal therapy of glioblastoma includes surgery, radiotherapy, systemic chemotherapy, and target therapy, which have been proven to result in limited improvement [4]. Most clinical trials revealed that the overall survival was around 15 months [5,6,7], and 5-year survival rate was only 5.8% [8,9,10]. Second-line therapies such as lomustine, carmustine, and temozolomide rechallenging after standard concurrent chemoradiation and adjuvant chemotherapy might only benefit a subgroup of patients with MGMT promoter methylation [11,12].
Tumor treating fields (TTFields) have changed the first-line clinical practice of glioblastoma worldwide by its promising therapeutic efficacy [13,14,15]. Delivering low-intensity, intermediate-frequency of 200 kHz alternating electric fields, TTFields present with the inhibitory effect of tumor cell proliferation by interfering with mitotic spindle formation during metaphase [16,17,18].
An EF-14 randomized trial revealed a median progression-free survival (PFS) of 6.7 months in the TTFields plus temozolomide group and PFS of 4 months in the temozolomide-alone group. The median overall survival (OS) of TTFields plus temozolomide group was 20.9 months, and OS of temozolomide-alone group was 16.0 months [14,19]. This represented the first positive outcome of all the therapies in newly diagnosed glioblastoma since Stupp protocols in 2005 [15]; however, it was devoid of clinical improvements in recurrent glioblastoma [20].
Correlations between genetic alternations and therapeutic efficacy have also been investigated in patients treated with TTFields [21]. There were undergoing trials of combinations of regiments as well, which were intended to facilitate the interaction between TTFields and other medical prescriptions [22].
This article is the first report on TTFields for the Chinese population. Our objective of this retrospective study was to evaluate the efficacy and safety of TTFields combined with TMZ during maintenance therapy versus TMZ alone in Chinese patients.
2. Methods and Materials
2.1. Patients and Tumor Samples
We included glioblastoma patients who underwent surgery followed by Stupp regimen and TTFields treatment at the Department of Neurosurgery, Huashan Hospital, Fudan University, between August 2018 and February 2021. Patients meeting the following criteria were eligible for the TTFields group: (1) age 18 or older; (2) histological diagnosis of GBM; (3) TTFields treatment for no less than 4 weeks; and (4) tumor available for genetic detection. Patients in the Non-TTFields group underwent surgery at Huashan Hospital between January 2016 and October 2017 and were required to meet all the above criteria, excluding criterion 3. The ethics committee approved this study of Huashan Hospital, Fudan University. Informed consent was obtained from all patients. Approval was granted by the Ethics Committee of Huashan Hospital, Fudan University Shanghai, China 200040 (No. KY2015-256).
Baseline characteristics included age, sex, Karnofsky performance status score (KPS), the extent of resection, tumor location, TTFields usage, progression-free survival (PFS), and overall survival (OS). The extent of resection was classified as gross total resection (GTR), partial resection, and biopsy. GTR was determined based on both surgical findings and postoperative images. Complete resection was achieved during surgery and confirmed by postoperative T1-weighted magnetic resonance imaging with contrast (no residual enhancement was observed on MR imaging). Patient compliance was assessed monthly as the average percentage of each day the TTFields treatment was conducted (out of each 24 h period).
2.2. Molecular Analysis
Glioma samples were obtained during surgical resection, snap-frozen by liquid nitrogen, and stored at −80 ℃. DNA of eligible quality and quantity was extracted from brain tumor tissue following the manufacturer’s instructions (BlackPREP FFPE kit, Analytik, Jena, Germany). The mutation status of IDH and telomerase reverse transcriptase (TERT) promoter were determined by Sanger sequencing (HITACHI 3500xL Dx Genetic Analyzer, Applied Biosystems Inc., Waltham, MA, USA). MGMT promoter methylation was detected by pyrosequencing (Pyromark Q24 instrument, Hildesheim, Germany).
2.3. Statistical Analysis
Continuous variables with normal distribution were presented as the mean followed by standard deviation. The abnormal distribution of continuous variables was introduced as the median, followed by the interquartile range from the first quartile to the third quartile (Q1–Q3). Student’s t-test and Wilcoxon rank-sum test were used for normally and abnormally distributed quantitative data at baseline. Categorical variables at baseline were analyzed by chi-squared or Fisher’s exact test.
Propensity score matching (PSM) was performed to match patients of the TTFields group with the Non-TTFields group. The propensity score data set was constructed using the multivariable logistic regression model, including age, sex, baseline KPS, the extent of resection, tumor location, IDH mutation status, MGMT promoter methylation, TERT promoter mutation status, and Stupp regimen. We used caliper matching with the caliper 0.2 of the pooled standard deviation of the logit of the propensity score. Patients in the TTFields group were matched 1:2 to patients in the Non-TTFields group.
The propensity data set generated the inverse probability of treatment weighting (IPTW) dataset. To balance those observable characteristics, each patient was weighted by the inverse probability of being in the TTFields group to compare to the Non-TTFields group.
For the primary endpoint, multivariate Cox regression assessed the association between overall survival and the two treatment groups. The model was adjusted by those variates whose p-value was no more than 0.10. Those variates with clinical meanings related to the primary endpoint were adjusted, ignoring the p-value. We analyzed the PSM dataset and the IPTW dataset with Cox regression for sensitivity analysis. The results were expressed as adjusted hazard ratios (HRs) with 95% confidence intervals (95% CIs). For the median time comparison, log-rank tests were used between the two groups. All hypothesis tests were two-sided, and values of <0.05 were considered statistically significant.
Stata SE 13 (Serial number 401306302851), R software version 4.2.0 (http://cran.r-project.org, accessed on 1 May 2022, and easy-R (www.empowerstats.com, accessed on 1 May 2022) were used for statistical analysis. GraphPad was used to generate figures.
3. Results
3.1. Study Population
Two hundred and sixty-seven patients were enrolled from 2019 to 2021 in our studies, and sixty-three patients received TTFields. The median age of the TTFields group was 51 and for Non-TTFields, 54. Around 48% were male patients, and 65% were in the non-TTFields group; the mean Karnofsky performance status scale score for each group was 80 and 90, respectively. In the TTFields group, 70% of gross total resection operations were achieved, versus 79% for Non-TTFields.
Tumor locations were classified into three categories: frontal lobe, superficial surface excluding frontal lobe, and midline/deep structure/infratentorial. The distribution of tumor location is shown in Table 1. All histological tissue slides were available, and an experienced pathologist confirmed the diagnosis of glioblastoma. MGMT methylation, TERT promoter, and IDH mutant status were tested in our studies. Standard Stupp protocol was performed in all patients in the TTFields group and reached 83% in the non-TTFields group.
Table 1.
Patient characteristics.
| TTF (n = 63) | N-TTF (n = 204) | ||
|---|---|---|---|
| Age | Mean ± SD | 49.98 ± 13.40 | 51.72 ± 14.43 |
| Median | 51 | 54 | |
| Sex | Male | 30 (48%) | 132 (65%) |
| Female | 33 (52%) | 72 (35%) | |
| Baseline KPS | Mean ± SD | 80.00 ± 12.05 | 82.70 ± 14.59 |
| Median | 80.00 | 90.00 | |
| Surgery extension | Gross total resection | 44 (70%) | 161 (79%) |
| Partial resection | 10 (16%) | 43 (21%) | |
| Biopsy | 9 (14%) | 0 (0.00%) | |
| Tumor location | Frontal lobe | 18 (29%) | 86 (42%) |
| Superficial hemisphere | 26 (41%) | 96 (47%) | |
| midline/deep structure/infratentorial | 19 (30%) | 22 (11%) | |
| IDH1-R132H status | Wild type | 56 (89%) | 180 (88%) |
| Mutated | 5 (8%) | 20 (10%) | |
| Invalid | 2 (3%) | 4 (2%) | |
| MGMT promoter region methylation | Methylated | 20 (32%) | 43 (21%) |
| Unmethylated | 38 (60%) | 66 (32%) | |
| Invalid | 5 (8%) | 95 (47%) | |
| TERT promoter mutation status | Unmethylated | 23 (37%) | 57 (28%) |
| Methylated | 28 (44%) | 52 (25%) | |
| Invalid | 12 (19%) | 95 (47%) | |
| Median compliance of TTFields | Mean ± SD | 0.85 ± 0.10 | |
| Median | 0.87 | ||
| Completed standard Stupp protocol | Yes | 63 (100%) | 170 (83%) |
| No | 0 (0%) | 34 (17%) |
Lastly, median compliance in the TTFields group was 87% during the recommended therapy period.
3.2. Prognostic Factors and Survival Rate
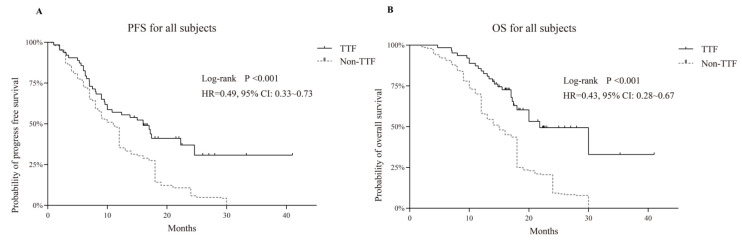
The median overall survival (OS) of the TTFields and non-TTFields group was 21.8 (95% CI 17.4–NA) versus 15 months (95% CI 13–18), for a proportional hazard ratio (HR) of 0.43 (95% CI 0.38–0.67, p < 0.001). The median progression-free survival of both groups was 16 (95% CI 9.6–24.6) versus 11 months (95% CI 9–12) with a proportional HR of 0.49 (95% CI 0.33–0.73, p < 0.001), as shown in Figure 1.
Figure 1.
Kaplan–Meier survival analysis in comparing tumor treating fields (TTF) versus non-TTF group; progression-free survival (PFS) is shown in (A) and overall survival in (B), revealing the prognostic advantages of TTF.
According to the univariate analysis of PFS and OS, as revealed in Table 2 and Table 3, administration of TTFields was a crucial prognostic factor in PFS and OS. The proportional HR was 0.53 (95% CI 0.37–0.75, p < 0.001) for PFS and was 0.40 (95% CI 0.27–0.60, p < 0.001) for OS.
Table 2.
Univariate and multivariate analyses of progression-free survival (PFS) in GBM patients.
| Univariate Analysis | Multivariate Analysis | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| n (%) | HR | 95% CI | Crude p-Value | HR | 95% CI | Adjusted p-Value | |||
| Lower | Upper | Lower | Upper | ||||||
| Age | |||||||||
| <65 | 215 (81%) | 1 | |||||||
| ≥65 | 52 (19%) | 1.27 | 0.93 | 1.73 | 0.130 | ||||
| Sex | |||||||||
| Male | 162 (61%) | 1 | |||||||
| Female | 105 (39%) | 0.71 | 0.55 | 0.93 | 0.013 | 0.84 | 0.64 | 1.11 | 0.219 |
| TTFields usage * | |||||||||
| N-TTF | 204 (76%) | 1 | |||||||
| TTF | 63 (24%) | 0.53 | 0.37 | 0.75 | <0.001 | 0.49 | 0.33 | 0.73 | 0.001 |
| Baseline KPS | |||||||||
| ≤80 | 82 (31%) | 1 | |||||||
| >80 | 185 (69%) | 0.96 | 0.73 | 1.27 | 0.793 | ||||
| Surgery extension * | |||||||||
| Gross total resection | 205 (77%) | 1 | |||||||
| Partial resection | 53 (20%) | 2.17 | 1.58 | 2.99 | <0.001 | ||||
| Biopsy | 9 (3%) | 1.66 | 0.82 | 3.39 | 0.162 | 2.03 | 1.56 | 2.64 | <0.001 |
| Tumor location | |||||||||
| Frontal lobe | 104 (39%) | 1 | |||||||
| Superficial hemisphere a | 122 (46%) | 1.09 | 0.83 | 1.44 | 0.533 | ||||
| Midline/deep structure/infratentorial | 41 (15%) | 1.35 | 0.92 | 1.97 | 0.127 | ||||
| IDH1-R132H status * | |||||||||
| Wild-type | 236 (88%) | 1 | |||||||
| Mutated | 25 (9%) | 0.58 | 0.37 | 0.92 | 0.019 | ||||
| Invalid | 6 (3%) | 0.6 | 0.22 | 1.61 | 0.310 | 0.63 | 0.44 | 0.92 | 0.016 |
| MGMT promoter region methylation | |||||||||
| Methylated | 63 (24%) | 1 | |||||||
| Unmethylated | 104 (39%) | 1.54 | 1.09 | 2.18 | 0.014 | ||||
| Invalid | 100 (37%) | 1.49 | 1.06 | 2.1 | 0.021 | 1.09 | 0.88 | 1.35 | 0.443 |
| TERT promoter mutation status | |||||||||
| Unmethylated | 80 (30%) | 1 | |||||||
| Methylated | 80 (30%) | 1.58 | 1.13 | 2.21 | 0.007 | ||||
| Invalid | 107 (40%) | 1.34 | 0.99 | 1.82 | 0.062 | 1.03 | 0.85 | 1.25 | 0.786 |
| Completed standard Stupp protocol * | |||||||||
| Yes | 233 (87%) | 1 | |||||||
| No | 34 (13%) | 2.19 | 1.51 | 3.17 | <0.001 | 1.78 | 1.21 | 2.61 | 0.003 |
a Frontal lobe was not included. * Demonstrates statistically significance at p < 0.05, both univariate and multivariate analyses.
Table 3.
Univariate and multivariate analyses of overall survival (OS) in GBM patients.
| Univariate Analysis | Multivariate Analysis | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| n (%) | HR | 95% CI | Crude p-Value | HR | 95% CI | Adjusted p-Value | |||
| Lower | Upper | Lower | Lower | ||||||
| Age | |||||||||
| <65 | 215 (81%) | 1 | |||||||
| ≥65 | 52 (19%) | 1.32 | 0.96 | 1.81 | 0.087 | ||||
| Sex | |||||||||
| Male | 162 (61%) | 1 | |||||||
| Female | 105 (39%) | 0.75 | 0.57 | 0.98 | 0.034 | 0.82 | 0.63 | 1.08 | 0.154 |
| TTFields usage * | |||||||||
| N-TTF | 204 (76%) | 1 | |||||||
| TTF | 63 (24%) | 0.40 | 0.27 | 0.60 | <0.001 | 0.43 | 0.28 | 0.67 | <0.001 |
| Baseline KPS | |||||||||
| ≤80 | 82 (31%) | 1 | |||||||
| >80 | 185 (69%) | 1.01 | 0.76 | 1.34 | 0.952 | ||||
| Surgery extension * | |||||||||
| Gross total resection | 205 (77%) | 1 | |||||||
| Partial resection | 53 (20%) | 1.61 | 1.17 | 2.22 | 0.003 | ||||
| Biopsy | 9 (3%) | 0.74 | 0.33 | 1.68 | 0.473 | 1.46 | 1.12 | 1.91 | 0.006 |
| Tumor location | |||||||||
| Frontal lobe | 104 (39%) | 1 | |||||||
| Superficial hemisphere a | 122 (46%) | 0.99 | 0.75 | 1.31 | 0.953 | ||||
| Midline/deep structure/infratentorial | 41 (15%) | 1.18 | 0.79 | 1.75 | 0.425 | ||||
| IDH1-R132H status | |||||||||
| Wild-type | 236 (88%) | 1 | |||||||
| Mutated | 25 (9%) | 0.81 | 0.52 | 1.28 | 0.373 | ||||
| Invalid | 6 (3%) | 0.77 | 0.29 | 2.09 | 0.612 | ||||
| MGMT promoter region methylation | |||||||||
| Methylated | 63 (24%) | 1 | |||||||
| Unmethylated | 104 (39%) | 1.46 | 1.02 | 2.08 | 0.036 | ||||
| Invalid | 100 (37%) | 1.57 | 1.11 | 2.22 | 0.010 | 1.10 | 0.89 | 1.35 | 0.381 |
| TERT promoter mutation status | |||||||||
| Unmethylated | 80 (30%) | 1 | |||||||
| Methylated | 80 (30%) | 1.65 | 1.17 | 2.32 | 0.005 | ||||
| Invalid | 107 (40%) | 1.57 | 1.15 | 2.15 | 0.005 | 1.09 | 0.90 | 1.32 | 0.387 |
| Completed standard Stupp protocol * | |||||||||
| Yes | 233 (87%) | 1 | |||||||
| No | 34 (13%) | 3.08 | 2.12 | 4.47 | <0.001 | 2.53 | 1.71 | 3.73 | <0.001 |
a Frontal lobe was not included. * Demonstrates statistically significance at p < 0.05, both univariate and multivariate analyses.
Furthermore, clinical significances were discovered in the following indicators. Females demonstrated longer PFS and OS (HR = 0.71; 95% CI, 0.55–093; p = 0.013 and HR = 0.75; 95% CI, 0.57–0.98; p = 0.034, respectively). Gross total resection revealed superior prognosis than subtotal resection (HR = 2.17; 95% CI, 1.58–2.99; p < 0.001 and HR = 1.61; 95% CI, 1.17–2.22; p = 0.003, in PFS and OS, respectively). Biomarker such as IDH mutant status was only positive in PFS (HR = 0.58; 95% CI, 0.37–092; p = 0.013), as MGMT methylation status (HR = 1.54; 95% CI, 1.09–2.18; p = 0.014 and HR = 1.46; 95% CI, 1.02–2.08; p = 0.036, in PFS and OS, respectively) and TERT promoter status (HR = 1.58; 95% CI, 1.13–2.21; p = 0.007 and HR =1.65; 95% CI, 1.17–2.32; p = 0.006, in PFS and OS, respectively) were both related to outcome with significance. Lastly, accomplishment of Stupp protocol was also an impact factor (HR = 2.19; 95% CI, 1.51–3.17; p < 0.001 and HR =3.08; 95% CI, 2.21–4.47; p < 0.001, in PFS and OS, respectively).
3.3. Multivariate Analysis
Multivariate analysis by Cox regression (Table 2 and Table 3) demonstrated that the usage of TTFields prolonged the survival time (HR = 0.49; 95% CI, 0.33–0.73; p < 0.001 and HR = 0.43; 95% CI, 0.28–0.67; p < 0.001, in PFS and OS, respectively). A similar result was also discovered in the Stupp protocol accomplished subgroup (HR = 2.19; 95% CI, 1.51–3.17; p < 0.001 and HR = 3.08; 95% CI, 2.12–4.47; p < 0.001, in PFS and OS, respectively).
3.4. Propensity Score-Matching and Inverse Probability Treatment Weighting Analysis
Propensity score-matching (PSM) was used in our studies to reduce the influence of selection bias between the TTFields and non-TTFields groups. The validated cohort is shown in Table 4. The survival risk of the TTFields group was significantly lower than the Non-TTFields group (HR = 0.60; 95% CI, 0.39–0.92; p < 0.001 and HR = 0.54; 95% CI, 0.33–0.89; p < 0.001, in PFS and OS, respectively) in the propensity score-matching analysis, as shown in Figure 2.
Table 4.
Patient characteristics before and after propensity score-matching (PSM).
| Unmatched Data | Matched Data | |||||
|---|---|---|---|---|---|---|
| TTF (n = 63) | N-TTF (n = 204) | p-Value | TTF (n = 49) | N-TTF (n = 87) | p-Value | |
| Age | 0.398 | 0.962 | ||||
| Mean ± SD | 49.98 ± 13.40 | 51.72 ± 14.43 | 49.41 ± 13.26 | 49.29 ±14.58 | ||
| Sex | 0.015 | 0.445 | ||||
| Male | 30 (48%) | 132 (64%) | 22 (45%) | 45 (52%) | ||
| Female | 33 (52%) | 72 (35%) | 27 (55%) | 42 (48%) | ||
| Baseline KPS | 0.184 | 0.891 | ||||
| Mean ± SD | 80.00 ± 12.05 | 82.70 ± 14.59 | 81.84 ± 11.85 | 82.18 ± 15.21 | ||
| Surgery extension | <0.001 | 0.436 | ||||
| Gross total resection | 44 (70%) | 161 (79%) | 40 (82%) | 66 (76%) | ||
| Partial resection | 10 (16%) | 43 (21%) | 9 (18%) | 21 (24%) | ||
| Biopsy | 9 (14%) | 0 (0%) | ||||
| Tumor location | <0.001 | 0.809 | ||||
| Frontal lobe | 18 (29%) | 86 (42%) | 16 (33%) | 31 (36%) | ||
| Superficial hemisphere | 26 (41%) | 96 (47%) | 23 (47%) | 42 (48%) | ||
| Midline/deep structure/infratentorial | 19 (30%) | 22 (11%) | 10 (20%) | 14 (16%) | ||
| IDH1-R132H status | 0.780 | 0.714 * | ||||
| Wild-type | 56 (89%) | 180 (88%) | 0.744 | 42 (86%) | 73 (84%) | |
| Mutated | 5 (8%) | 20 (10%) | 5 (10%) | 12 (14%) | ||
| Invalid | 2 (3%) | 4 (2%) | 2 (4%) | 2 (2%) | ||
| MGMT promoter region methylation | <0.001 | 0.011 | ||||
| Methylated | 20 (32%) | 43 (21%) | 12 (24%) | 32 (37%) | ||
| Unmethylated | 38 (60%) | 66 (32%) | 33 (67%) | 36 (41%) | ||
| Invalid | 5 (8%) | 95 (47%) | 4 (9%) | 19 (22%) | ||
| TERT promoter mutation status | <0.001 | 0.43 | ||||
| Unmethylated | 23 (37%) | 57 (28%) | 18 (37%) | 38 (44%) | ||
| Methylated | 28 (44%) | 52 (25%) | 23 (47%) | 31 (36%) | ||
| Invalid | 12 (19%) | 95 (47%) | 8 (16%) | 18 (20%) | ||
| Completed standard Stupp protocol | <0.001 | NA | ||||
| Yes | 63 (100.00%) | 170 (83%) | 49(100%) | 87(100%) | ||
| No | 0 (0.00%) | 34 (17%) | 0 | 0 | ||
* Fisher chi-squared test.
Figure 2.
Kaplan–Meier survival analysis after propensity score-matching (PSM) in comparing TTF versus Non-TTF group; progression-free survival (PFS) is shown in (A) and overall survival in (B).
MGMT methylation status impacted the outcomes between the two groups, with elevated risk of non-methylation group (HR = 1.13; 95% CI, 0.39–0.92; p < 0.001 and HR = 0.54; 95% CI, 0.33–0.89; p < 0.001, in PFS and OS, respectively).
After inverse probability treatment weighting (IPTW), the baseline features of the two groups were balanced, and the significance remained (Table 5).
Table 5.
PFS and OS analysis after inverse probability treatment weighting (IPTW).
| PFS | |||||
|---|---|---|---|---|---|
| HR | Std. Err. | p-Value | 95% CI | ||
| Lower | Upper | ||||
| TTF | 0.35 | 0.17 | 0.031 | 0.14 | 0.91 |
| OS | |||||
| HR | Std. Err. | p-Value | 95% CI | ||
| Lower | Upper | ||||
| TTF | 0.19 | 0.08 | <0.001 | 0.09 | 0.41 |
4. Discussion
The phase 3 EF-14 international trial demonstrated the efficacy of TTFields plus TMZ versus TMZ alone as maintenance therapy in patients with newly diagnosed GBM [19]. This led to the approval of TTFields in combination with TMZ for the treatment of newly diagnosed GBM in October 2015. In China, the joint guideline committee of the Chinese Glioma Cooperative Group (CGCG) recently published a guideline and recommended TTFields for the treatment of GBM [23]. While the results of these studies led to approval of FDA and C-FDA for GBM populations, a portion of the neuro-oncology and neurosurgery community remains skeptical of TTFields therapy. The skepticism is due to incoherent results, with certain clinicians taking a wait-it-out approach [24,25]. Here, we retrospectively analyzed the effect of TTFields plus TMZ in newly diagnosed GBM in our center. After observing from 267 GBM patients, TTFields plus TMZ therapy (63 patients) resulted in extended progression-free survival and overall survival compared with temozolomide therapy (204 patients). These findings are consistent with the EF-14 results.
In our current study, the patients of TTFields/TMZ treatment were extracted from the post-marketing registry of newly diagnosed patients in our hospital. The clinical data of TMZ treatment patients were collected from the follow-up library of glioma in Huashan Hospital [26]. There are some apparent differences between the two groups. The TTFields/TMZ group displayed a relatively higher female-to-male ratio, more STUPP scheme, and less MGMT methylation. This reflects the probability that some of the Chinese female patients tended to accept TTFields to prolong survival and agree to shave their heads regardless of aesthetic purposes. In contrast, some Chinese male patients do not want to shave their heads and wear transducer arrays for social reasons. A strength of our study is that measures were taken to reduce those potential biases. We performed a propensity score based on IPTW adjustment, which significantly reduces confounding bias and imbalance in co-variates and thus potentially offers an estimate of treatment effect similar to randomized trials [27,28]. In our preliminary analysis, the median progression-free survival (PFS) in the TTFields/TMZ arm was 16 months (95% CI 9.6–24.6) versus 11 months (95% CI 9–12) with TMZ alone (p < 0.05). Median overall survival was 21.8 months (95% CI 17.4-NA) with TTFields/TMZ versus 15 months (95% CI 13–18; HR 0.43, p < 0.01) with TMZ group. After adjustment, the arms were well-balanced regarding sex, resection, STUPP scheme, and MGMT promoter methylation. Upon IPTW survival analysis, TTFields/TMZ was associated with a significantly lower risk of death (hazard ratio (HR), 0.19 in OS (95% CI 0.09–0.41) and progression (HR, 0.35 (95% CI 0.14–0.91)) compared with TMZ, which was consistent with preliminary analysis.
In this study, the surgery extension, complete standard Stupp protocol, and TTFields were significantly associated in both univariate and multivariate analyses. In addition, MGMT promoter unmethylation and TERT mutation showed worse survival on univariate analysis. Surgery extension [29], complete standard Stupp protocol [29], and TTFields [29] were previously reported as predictors of improved survival of patients with GBM, consistent with the results of the present study.
Treatment adherence and electric field duration time have emerged as important factors for TTFields efficacy [30,31,32,33]. Patients are recommended to wear the device for at least 18 h per day, with a corresponding adherence rate of ≥75%. While adherence rates were high in both EF-11 and EF-14, the median adherence rate was below the recommended 75% in PRiDe [29]. In our study, median adherence rate was 85%. The median duration of tumor treating fields therapy was longer in our group (10.6 months) compared with that of EF-14 (8.2 months). These findings suggest that high adherence rate and long electric field duration may ensure the effectiveness of electric field therapy in GBM.
Based on the results of our study, it can be reasonably argued that TTFields should be discussed with Chinese patients who are newly diagnosed with GBM as part of initial therapy. Further studies would be needed to refine the population most likely to benefit, and more importantly, identify subsets where the benefit is minuscule or not present. Future analysis of prolonged and short survival to NovoTTField Therapy will need to include multi-omics analysis of the tumor (exon sequencing, methylation, RNA sequencing, advanced liquid biopsy capacities). We find that there has been important progress in understanding the molecular determinants of glioma invasion and migration, such as growth factors, intracellular signaling cascade, cell–ECM, and cell–cell receptors [29]. Along with ever-improving molecular technologies and their sensitivities, we are hopeful that specific biomarkers involved in glioma invasion and migration will soon be found in tissue, blood, or CSF [34].
In conclusion, our data represent the largest group of patients with newly diagnosed GBM in China, containing 267 patients in total, 63 of whom were treated with NovoTTFields. The results, individually and collectively, demonstrate that adding TTFields to temozolomide chemotherapy can result in statistically significant improvement in progression-free survival and overall survival in Chinese GBM patients.
Author Contributions
Conceptualization, L.C.; Data curation, J.Z.; Formal analysis, L.C. and Z.Q.; Funding acquisition, H.X.; Investigation, C.C., H.X., K.S., Y.Z. and Z.Q.; Methodology, J.Z.; Resources, Y.W. and X.S.; Supervision, Z.Q.; Writing—original draft, C.C. and H.X.; Writing—review & editing, L.C. and Z.Q. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Huashan Hospital, Fudan University Shanghai, China 200040 (No.KY2015-256).
Informed Consent Statement
Informed consent was obtained from all individual participants included in the study. The authors affirm that human research participants provided informed consent for publication of the clinical data.
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors have no relevant financial or non-financial interests to disclose.
Funding Statement
This work was supported by the National Natural Science Foundation of China (No. 82103376). CSCO treatment and Research Fund Project Y-zai2021/ms-0270, Y-zai2021/qn-0204.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Tan A.C., Ashley D.M., López G.Y., Malinzak M., Friedman H.S., Khasraw M. Management of glioblastoma: State of the art and future directions. CA Cancer J. Clin. 2020;70:299–312. doi: 10.3322/caac.21613. [DOI] [PubMed] [Google Scholar]
- 2.Alexander B.M., Cloughesy T.F. Adult glioblastoma. J. Clin. Oncol. 2017;35:2402–2409. doi: 10.1200/JCO.2017.73.0119. [DOI] [PubMed] [Google Scholar]
- 3.Weller M., van den Bent M., Preusser M., Le Rhun E., Tonn J.C., Minniti G., Bendszus M., Balana C., Chinot O., Dirven L., et al. EANO guidelines on the diagnosis and treatment of diffuse gliomas of adulthood. Nat. Rev. Clin. Oncol. 2020;18:170–186. doi: 10.1038/s41571-020-00447-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McNamara M.G., Lwin Z., Jiang H., Templeton A.J., Zadeh G., Bernstein M., Chung C., Millar B.-A., Laperriere N., Mason W.P. Factors impacting survival following second surgery in patients with glioblastoma in the temozolomide treatment era, incorporating neutrophil/lymphocyte ratio and time to first progression. J. Neuro-Oncol. 2014;117:147–152. doi: 10.1007/s11060-014-1366-9. [DOI] [PubMed] [Google Scholar]
- 5.Stupp R., Mason W.P., van den Bent M.J., Weller M., Fisher B., Taphoorn M.J.B., Belanger K., Brandes A.A., Marosi C., Bogdahn U., et al. Radiotherapy plus Concomitant and Adjuvant Temozolomide for Glioblastoma. N. Engl. J. Med. 2005;352:987–996. doi: 10.1056/NEJMoa043330. [DOI] [PubMed] [Google Scholar]
- 6.Gilbert M.R., Wang M., Aldape K.D., Stupp R., Hegi M.E., Jaeckle K.A., Armstrong T.S., Wefel J.S., Won M., Blumenthal D.T., et al. Dose-Dense Temozolomide for Newly Diagnosed Glioblastoma: A Randomized Phase III Clinical Trial. J. Clin. Oncol. 2013;31:4085–4091. doi: 10.1200/JCO.2013.49.6968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Han S.J., Rolston J.D., Molinaro A.M., Clarke J.L., Prados M.D., Chang S.M., Berger M.S., DeSilva A., Butowski N.A. Phase II trial of 7 days on/7 days off temozolmide for recurrent high-grade glioma. Neuro-Oncology. 2014;16:1255–1262. doi: 10.1093/neuonc/nou044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stupp R., Hegi M.E., Mason W.P., van den Bent M.J., Taphoorn M.J.B., Janzer R.C., Ludwin S.K., Allgeier A., Fisher B., Belanger K., et al. Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phase III study: 5-year analysis of the EORTC-NCIC trial. Lancet Oncol. 2009;10:459–466. doi: 10.1016/S1470-2045(09)70025-7. [DOI] [PubMed] [Google Scholar]
- 9.Ostrom Q.T., Gittleman H., Truitt G., Boscia A., Kruchko C., Barnholtz-Sloan J.S. CBTRUS Statistical Report: Primary Brain and Other Central Nervous System Tumors Diagnosed in the United States in 2011–2015. Neuro-Oncology. 2018;20:iv1–iv86. doi: 10.1093/neuonc/noy131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ostrom Q.T., Cote D.J., Ascha M., Kruchko C., Barnholtz-Sloan J.S. Adult Glioma Incidence and Survival by Race or Ethnicity in the United States From 2000 to 2014. JAMA Oncol. 2018;4:1254–1262. doi: 10.1001/jamaoncol.2018.1789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wick W., Puduvalli V.K., Chamberlain M.C., Bent M.V.D., Carpentier A.F., Cher L.M., Mason W., Weller M., Hong S., Musib L., et al. Phase III Study of Enzastaurin Compared With Lomustine in the Treatment of Recurrent Intracranial Glioblastoma. J. Clin. Oncol. 2010;28:1168–1174. doi: 10.1200/JCO.2009.23.2595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Herrlinger U., Tzaridis T., Mack F., Steinbach J.P., Schlegel U., Sabel M., Hau P., Kortmann R.-D., Krex D., Grauer O., et al. Lomustine-temozolomide combination therapy versus standard temozolomide therapy in patients with newly diagnosed glioblastoma with methylated MGMT promoter (CeTeG/NOA–09): A randomised, open-label, phase 3 trial. Lancet (London, UK) 2019;393:678–688. doi: 10.1016/S0140-6736(18)31791-4. [DOI] [PubMed] [Google Scholar]
- 13.Weller M., dan der Bent M., Tonn J.C., Stupp R., Preusser M., Cohen-Jonathan-Moyal E., Henriksson R., Le Rhun E., Balana C., Chinot O., et al. European Association for Neuro-Oncology (EANO) guideline on the diagnosis and treatment of adult astrocytic and oligodendroglial gliomas. Lancet Oncol. 2017;18:e315–e329. doi: 10.1016/S1470-2045(17)30194-8. [DOI] [PubMed] [Google Scholar]
- 14.Stupp R., Taillibert S., Kanner A.A., Kesari S., Steinberg D.M., Toms S.A., Taylor L.P., Lieberman F., Silvani A., Fink K.L., et al. Maintenance Therapy With Tumor-Treating Fields Plus Temozolomide vs Temozolomide Alone for Glioblastoma: A Randomized Clinical Trial. JAMA. 2015;314:2535–2543. doi: 10.1001/jama.2015.16669. [DOI] [PubMed] [Google Scholar]
- 15.Weller M. Tumor-treating fields: Time for demystification. Ann. Oncol. 2018;29:1628–1630. doi: 10.1093/annonc/mdy220. [DOI] [PubMed] [Google Scholar]
- 16.Kirson E.D., Gurvich Z., Schneiderman R., Dekel E., Itzhaki A., Wasserman Y., Schatzberger R., Palti Y. Disruption of Cancer Cell Replication by Alternating Electric Fields. Cancer Res. 2004;64:3288–3295. doi: 10.1158/0008-5472.CAN-04-0083. [DOI] [PubMed] [Google Scholar]
- 17.Giladi M., Schneiderman R.S., Voloshin T., Porat Y., Munster M., Blat R., Sherbo S., Bomzon Z., Urman N., Itzhaki A., et al. Mitotic Spindle Disruption by Alternating Electric Fields Leads to Improper Chromosome Segregation and Mitotic Catastrophe in Cancer Cells. Sci. Rep. 2015;5:18046. doi: 10.1038/srep18046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mun E.J., Babiker H.M., Weinberg U., Kirson E.D., Von Hoff D.D. Tumor-Treating Fields: A Fourth Modality in Cancer Treatment. Clin. Cancer Res. 2018;24:266–275. doi: 10.1158/1078-0432.CCR-17-1117. [DOI] [PubMed] [Google Scholar]
- 19.Stupp R., Taillibert S., Kanner A.A., Read W., Steinberg D.M., Lhermitte B., Toms S., Idbaih A., Ahluwalia M.S., Fink K., et al. Effect of Tumor-Treating Fields Plus Maintenance Temozolomide vs Maintenance Temozolomide Alone on Survival in Patients With Glioblastoma: A Randomized Clinical Trial. JAMA. 2017;318:2306–2316. doi: 10.1001/jama.2017.18718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stupp R., Wong E.T., Kanner A.A., Steinberg D., Engelhard H., Heidecke V., Kirson E.D., Taillibert S., Liebermann F., Dbalý V., et al. NovoTTF-100A versus physician’s choice chemotherapy in recurrent glioblastoma: A randomised phase III trial of a novel treatment modality. Eur. J. Cancer. 2012;48:2192–2202. doi: 10.1016/j.ejca.2012.04.011. [DOI] [PubMed] [Google Scholar]
- 21.Dono A., Mitra S., Shah M., Takayasu T., Zhu J.-J., Tandon N., Patel C.B., Esquenazi Y., Ballester L.Y. PTEN mutations predict benefit from tumor treating fields (TTFields) therapy in patients with recurrent glioblastoma. J. Neuro-Oncol. 2021;153:153–160. doi: 10.1007/s11060-021-03755-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shah P.P., White T., Khalafallah A., Romo C.G., Price C., Mukherjee D. A systematic review of tumor treating fields therapy for high-grade gliomas. J. Neuro-Oncol. 2020;148:433–443. doi: 10.1007/s11060-020-03563-z. [DOI] [PubMed] [Google Scholar]
- 23.Jiang T., Nam D.-H., Ram Z., Poon W.-S., Wang J., Boldbaatar D., Mao Y., Ma W., Mao Q., You Y., et al. Clinical practice guidelines for the management of adult diffuse gliomas. Cancer Lett. 2021;499:60–72. doi: 10.1016/j.canlet.2020.10.050. [DOI] [PubMed] [Google Scholar]
- 24.Printz C. Electrical device for patients with glioblastoma met with support, skepticism: Some question the device’s efficacy, others tout it as a new standard of care. Cancer. 2015;121:969–970. doi: 10.1002/cncr.28991. [DOI] [PubMed] [Google Scholar]
- 25.Wick W. TTFields: Where does all the skepticism come from? Neuro-Oncology. 2016;18:303–305. doi: 10.1093/neuonc/now012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Aibaidula A., Lu J.-F., Wu J.-S., Zou H.-J., Chen H., Wang Y.-Q., Qin Z.-Y., Yao Y., Gong Y., Che X.-M., et al. Establishment and maintenance of a standardized glioma tissue bank: Huashan experience. Cell Tissue Bank. 2015;16:271–281. doi: 10.1007/s10561-014-9459-4. [DOI] [PubMed] [Google Scholar]
- 27.Choi J., Kim H.J., Lee J., Cho S., Ko M.J., Lim Y.-S. Risk of Hepatocellular Carcinoma in Patients Treated With Entecavir vs Tenofovir for Chronic Hepatitis B: A Korean Nationwide Cohort Study. JAMA Oncol. 2019;5:30–36. doi: 10.1001/jamaoncol.2018.4070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bonnot P.-E., Piessen G., Kepenekian V., Decullier E., Pocard M., Meunier B., Bereder J.-M., Abboud K., Marchal F., Quenet F., et al. Cytoreductive Surgery With or Without Hyperthermic Intraperitoneal Chemotherapy for Gastric Cancer With Peritoneal Metastases (CYTO-CHIP study): A Propensity Score Analysis. J. Clin. Oncol. 2019;37:2028–2040. doi: 10.1200/JCO.18.01688. [DOI] [PubMed] [Google Scholar]
- 29.Mrugala M.M., Engelhard H., Tran D.D., Kew Y., Cavaliere R., Villano J.L., Bota D.A., Rudnick J., Sumrall A.L., Zhu J.-J., et al. Clinical Practice Experience With NovoTTF-100A™ System for Glioblastoma: The Patient Registry Dataset (PRiDe) Semin. Oncol. 2014;41((Suppl. 6)):S4–S13. doi: 10.1053/j.seminoncol.2014.09.010. [DOI] [PubMed] [Google Scholar]
- 30.Burri S.H., Gondi V., Brown P.D., Mehta M.P. The Evolving Role of Tumor Treating Fields in Managing Glioblastoma. Am. J. Clin. Oncol. 2018;41:191–196. doi: 10.1097/COC.0000000000000395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Onken J., Staub-Bartelt F., Vajkoczy P., Misch M. Acceptance and compliance of TTFields treatment among high grade glioma patients. J. Neuro-Oncol. 2018;139:177–184. doi: 10.1007/s11060-018-2858-9. [DOI] [PubMed] [Google Scholar]
- 32.Benson L. Tumor Treating Fields Technology: Alternating Electric Field Therapy for the Treatment of Solid Tumors. Semin. Oncol. Nurs. 2018;34:137–150. doi: 10.1016/j.soncn.2018.03.005. [DOI] [PubMed] [Google Scholar]
- 33.Lacouture M.E., Davis M.E., Elzinga G., Butowski N., Tran D., Villano J.L., DiMeglio L., Davies A.M., Wong E.T. Characterization and Management of Dermatologic Adverse Events With the NovoTTF-100A System, a Novel Anti-mitotic Electric Field Device for the Treatment of Recurrent Glioblastoma. Semin. Oncol. 2014;41((Suppl. 4)):S1–S14. doi: 10.1053/j.seminoncol.2014.03.011. [DOI] [PubMed] [Google Scholar]
- 34.Drappatz J., Norden A.D., Wen P.Y. Therapeutic strategies for inhibiting invasion in glioblastoma. Expert Rev. Neurother. 2009;9:519–534. doi: 10.1586/ern.09.10. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.