Abstract
The frequency and clinical manifestation of lung fibrosis accompanied by coronavirus disease (COVID-19) are not well-established. We aimed to identify the factors attributed to post-COVID-19 fibrosis. This single-center prospective study included patients diagnosed with COVID-19 pneumonia from 12 April to 22 October 2021 in the Republic of Korea. The primary outcome was the presence of pulmonary fibrosis on a CT scan 3 months after discharge; the fibrosis risk was estimated by a multiple logistic regression. The mean patient age was 55.03 ± 12.32 (range 27–85) years; 65 (66.3%) were men and 33 (33.7%) were women. The age, Charlson Comorbidity Index, lactate dehydrogenase level, aspartate aminotransferase level, and Krebs von den Lungen-6 level were significantly higher and the albumin level and the saturation of the peripheral oxygen/fraction of inspired oxygen (SpO2/FiO2) ratio were significantly lower in the fibrosis group than in the non-fibrosis group; the need for initial oxygen support was also greater in the fibrosis group. An older age (adjusted odds ratio (AOR) 1.12; 95% confidence interval (CI) 1.03–1.21) and a lower initial SpO2/FiO2 ratio (AOR 7.17; 95% CI 1.72–29.91) were significant independent risk factors for pulmonary fibrosis after COVID-19 pneumonia. An older age and a low initial SpO2/FiO2 ratio were crucial in predicting pulmonary fibrosis after COVID-19 pneumonia.
Keywords: pulmonary fibrosis, COVID-19, pneumonia
1. Introduction
The first case of infection due to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was reported in Wuhan, China, in December 2019. The infection was subsequently named coronavirus disease (COVID-19) by the World Health Organization (WHO). Since then, the COVID-19 pandemic has persisted as a global infection [1,2,3], with the number of confirmed cases surpassing half a billion and six million deaths to date.
Many studies have reported at least one persistent symptom in patients after their recovery from COVID-19. Post-COVID-19 symptoms range from respiratory symptoms such as exertional dyspnea, chest discomfort, and a cough to non-respiratory symptoms such as fatigue, cognitive impairments, and psychological problems such as anxiety and depression [4,5,6].
In patients hospitalized for COVID-19 pneumonia, a ground-glass opacity pattern is a typical initial radiologic finding and the pattern varies from severe acute respiratory distress syndrome to interstitial pneumonia [7,8]. Studies have reported that in moderate to severe COVID-19 pneumonia, the typical ground-glass opacification patterns turn into fibrotic changes, causing residual respiratory symptoms such as dyspnea and a cough for months [9,10]. Studies on whether the sequelae of COVID-19 pneumonia persist in certain patients, especially survivors, are in progress.
Currently, an antiviral therapy, an anti-inflammatory therapy (corticosteroids), and supportive care are the main pillars of COVID-19 pneumonia treatment; no specific preventive therapy or treatment has been officially recommended for pulmonary fibrosis. Clinical trials, including randomized controlled trials (ClinicalTrials.gov identifier: NCT04541680, NCT04619680, and NCT04607928), are investigating the possibility of applying antifibrotic agents such as pirfenidone and nintedanib, which have already been proven to be effective for treating idiopathic pulmonary fibrosis [11,12]. Due to the increasing number of cases, survivors need further attention and the long-term changes in COVID-19-infected lungs and symptoms must be studied.
Thus, we aimed to identify the factors attributed to post-COVID-19 fibrosis to provide a better understanding of the disease entity and additional treatment options for survivors of COVID-19. In this study, we analyzed 3-month follow-up CT scans to evaluate the fibrotic progression and its risk factors in patients who had been diagnosed with COVID-19.
2. Materials and Methods
2.1. Study Design and Population
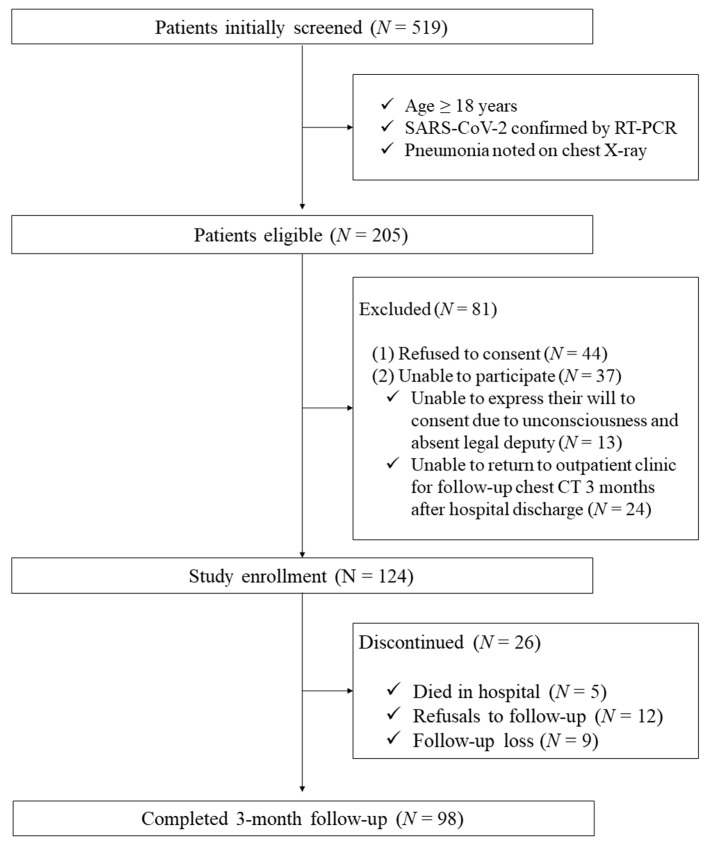
This single-center prospective study included patients who were diagnosed with COVID-19 pneumonia. The entire population of 519 patients hospitalized at the National Medical Center in the Republic of Korea from 12 April to 22 October 2021 was screened. The patient inclusion criteria were as follows: (1) age > 18 years; (2) SARS-CoV-2 infection confirmed by a positive nasopharyngeal swab reverse transcriptase-polymerase chain reaction; and (3) a diagnosis of pneumonia from an initial chest X-ray. Patients who refused to consent to this study, were unable to participate, were unable to express their will to consent due to unconsciousness and the absence of a legal deputy, or were unable to return to the outpatient clinic for a follow-up chest CT scan 3 months after the hospital discharge were excluded (Figure 1).
Figure 1.
Enrollment flowchart. SARS-CoV-2: severe acute respiratory syndrome coronavirus 2; RT-PCR: reverse transcriptase-polymerase chain reaction; CT: computed tomography.
2.2. Study Variables
All information was collected from electronic medical records. Demographic characteristics, including age, sex, body mass index (BMI), smoking history, and underlying comorbidities, were included in the analysis. For the clinical status at admission, the vital signs, oxygen support, laboratory results, and Eastern Cooperative Oncology Group performance status were reviewed. During hospitalization, the variables related to the hospital course such as the length of hospital stay, intensive care unit admission, maximum oxygen support, and medication were also collected. Medications included antiviral agents (remdesivir), monoclonal antibodies (regdanvimab and tocilizumab), steroids, and antibacterial agents. Antifibrotic agents that did not have clear evidence [13] of use and were not approved by the Korean Food and Drug Administration (FDA) were not applied to the study population.
Among laboratory findings, Krebs von den Lungen-6 (KL-6), a serological biomarker for interstitial lung disease, has the potential to predict fibrosis in patients with COVID-19 pneumonia [14,15]. In our study, however, we started to collect KL-6 from the middle of the study period; thus, data were only available for 79 patients. We referred to multiple studies published in 2021 that reported a correlation between KL-6 and post-COVID-19 fibrosis [14,16].
2.3. Study Outcome
The primary outcome of this study was the presence of pulmonary fibrosis on CT scans 3 months after discharge. Two independent radiologists specializing in pulmonology radiologic imaging were fully blinded to any other clinical findings and evaluated the CT scans for the presence of fibrosis. Pulmonary fibrosis was defined when any of the following radiologic features were present: (1) parenchymal bands; (2) traction bronchiectasis with or without volume loss; (3) reticulation; and (4) honeycombing [17,18,19]. In the case of a discrepancy between the assessments of the two radiologists, a final consensus was reached after a discussion. The inter-rater reliability between the radiologists was substantial, with a Cohen’s kappa of 0.938.
The study protocol was approved by the Institutional Review Board of the National Medical Center (NMC-2021-04-032). The present study was registered with the Clinical Research Information Service (No. KCT0006312). Written informed consent was provided by individual patients or their caregivers with a legal deputy.
2.4. Statistical Analyses
The descriptive statistics were presented as numbers (percentages) for the categorical variables and as the mean ± standard deviation for the continuous variables. We compared the two groups using the χ2 or Fisher’s exact test for the categorical variables, as appropriate, and the Student’s t-test for the continuous variables. The risk of post-COVID-19 pulmonary fibrosis was estimated for each potential risk factor (age, sex, BMI, and smoking status) and the variables having p-values < 0.10 were included in the multiple logistic regression models. Adjusted odds ratios (ORs) and 95% confidence intervals (CIs) were calculated and a p-value < 0.05 was considered to be statistically significant. All statistical analyses were performed using the SAS statistical package (version 9.4; SAS Institute Inc., Cary, NC, USA).
3. Results
3.1. Baseline Characteristics
Among the 124 patients initially enrolled in this study, 5 died during admission, 12 refused follow-up visits, and 9 were lost to follow-up (Figure 1). A total of 98 patients who underwent a CT scan follow-up 3 months after discharge were included. Pulmonary fibrosis was observed in 43 (43.9%) patients.
Table 1 shows the clinical characteristics of the study population. The mean age was 55.03 ± 12.32 (range 27–85) years; 65 (66.3%) of the patients were men and 33 (33.7%) were women. The age, Charlson Comorbidity Index, lactate dehydrogenase (LDH) level, aspartate aminotransferase (AST) level, and KL-6 level were significantly higher and the albumin level and the saturation of the peripheral oxygen/fraction of inspired oxygen (SpO2/FiO2) ratio were significantly lower in the fibrosis than in the non-fibrosis group; the need for initial oxygen support was also greater in the fibrosis group.
Table 1.
Clinical characteristics of the study population.
| Fibrosis | Non-Fibrosis | p-Value € | |
|---|---|---|---|
| (N = 43) | (N = 55) | ||
| Age, years (mean ± SD) | 60.7 ± 11.0 | 50.6 ± 11.5 | <0.001 |
| Male (N, %) | 29 (67.4) | 36 (65.5) | 0.836 |
| BMI (kg/m2) (mean ± SD) | 24.5 ± 3.9 | 26.4 ± 5.2 | 0.056 |
| Current or ex-smoker (N, %) | 24 (55.8%) | 26 (47.3%) | 0.401 |
| Underlying diseases, yes (N, %) | |||
| Hypertension | 18 (41.9%) | 16 (29.1%) | 0.188 |
| Diabetes mellitus | 10 (23.3%) | 12 (21.8%) | 0.866 |
| Chronic lung disease * | 1 (2.3%) | 2 (3.6%) | 1.000 |
| Heart disease * | 3 (7.0%) | 2 (3.6%) | 0.651 |
| Stroke * | 3 (7.0%) | 1 (1.8%) | 0.316 |
| Chronic kidney disease * | 2 (4.7%) | 2 (3.6%) | 1.000 |
| Malignancy * | 3 (7.0%) | 2 (3.6%) | 0.651 |
| Charlson Comorbidity Index (mean ± SD) | 2.2 ± 1.7 | 1.2 ± 1.6 | 0.004 |
| ECOG at admission (mean ± SD) | 1.7 ± 1.3 | 1.3 ± 1.2 | 0.109 |
| Laboratory finding (mean ± SD) | |||
| CRP (mg/L) | 94.9 ± 70.6 | 75.4 ± 66.4 | 0.164 |
| LDH (U/L) | 465.3 ± 147.0 | 378.0 ± 188.3 | 0.016 |
| Albumin (g/dL) | 3.6 ± 0.4 | 4.0 ± 0.4 | <0.001 |
| D-dimer (μg/mL FEU) | 2.2 ± 4.2 | 1.2 ± 2.7 | 0.180 |
| AST (U/L) | 65.4 ± 51.1 | 42.67 ± 23.80 | 0.009 |
| ALT (U/L) | 54.6 ± 54.1 | 39.7 ± 32.1 | 0.116 |
| KL-6 (U/mL) | 584.9 ± 441.3 | 345.3 ± 165.0 | 0.008 |
| BUN (mg/dL) | 15.8 ± 8.9 | 13.9 ± 12.4 | 0.412 |
| Creatinine (mg/dL) | 0.8 ± 0.5 | 0.8 ± 0.6 | 0.652 |
| Vital signs (mean ± SD) | |||
| Systolic BP (mmHg) | 128.1 ± 21.8 | 124.9 ± 24.9 | 0.501 |
| Pulse rate (per minute) | 86.5 ± 12.5 | 88.0 ± 14.4 | 0.580 |
| Respiratory rate (per minute) | 21.7 ± 3.9 | 21.2 ± 3.5 | 0.481 |
| Body temperature (Celsius) | 37.1 ± 2.8 | 37.7 ± 0.9 | 0.104 |
| SpO2/FiO2, initial | 296.0 ± 141.3 | 390.5 ± 110.3 | 0.001 |
| Oxygen support, initial, yes (N, %) * | 0.004 | ||
| Support was not needed | 14 (32.6) | 36 (65.5) | |
| NP or simple mask | 17 (39.5) | 15 (27.3) | |
| Reservoir bag or HFNC | 11 (25.6) | 3 (5.5) | |
| Mechanical ventilation | 1 (2.3) | 1 (1.8) |
HFNC: high-flow nasal cannula; ECMO: extracorporeal membrane oxygenation; KL-6: Krebs von den Lungen-6; BMI: body mass index; CRP: C-reactive protein; LDH: lactate dehydrogenase; AST: aspartate aminotransferase; ALT: alanine aminotransferase; BUN: blood urea nitrogen; ECOG: Eastern Cooperative Oncology Group. Chronic lung diseases include asthma, chronic obstructive pulmonary disease, interstitial lung disease, bronchiectasis, TB-destroyed lung, sarcoidosis, and emphysema. Values are presented as a number (%), mean (standard deviation (SD)), or median (interquartile range). € Tested by chi-squared test for categorical variables and by t-test for continuous ones. * Tested by Fisher’s exact test.
The clinical courses of these patients are summarized in Table 2. More patients in the fibrosis group (N = 19, 44.2%) were admitted to the intensive care unit compared with the non-fibrosis group (N = 10, 18.2%) (p = 0.005). A higher proportion of patients in the fibrosis group than in the non-fibrosis group required an oxygen supply during the entire hospital stay and at a higher concentration of oxygen (p = 0.009). The rate of antiviral agent and steroid use was also higher in the fibrosis group (N = 37, 86.0% for the antiviral agent and N = 41, 95.3% for the steroids) compared with the non-fibrosis group (N = 33, 60.0% for the antiviral agent and N = 37, 69.8% for steroids).
Table 2.
Clinical courses.
| Fibrosis | Non-Fibrosis | p-Value € | |
|---|---|---|---|
| (N = 43) | (N = 55) | ||
| Length of hospital stay, days (mean ± SD) | 15.1 ± 8.3 | 12.7 ± 16.0 | 0.372 |
| ICU admission, yes (N, %) | 19 (44.2%) | 10 (18.2%) | 0.005 |
| Oxygen support, max (N, %) * | 0.009 | ||
| Support was not needed | 4 (9.3) | 13 (23.6) | |
| NP or simple mask | 15 (34.9) | 29 (52.7) | |
| Reservoir bag or HFNC | 22 (51.2) | 11 (20.0) | |
| Mechanical ventilation | 2 (4.7) | 2 (3.7) | |
| Medication, yes (N, %) | |||
| Antiviral agents | 37 (86.0) | 33 (60.0) | 0.005 |
| Monoclonal antibodies | 9 (20.9) | 8 (14.5) | 0.407 |
| Steroids | 41 (95.3) | 37 (69.8) | 0.001 |
| Antibacterial agents | 31 (73.8) | 32 (60.4) | 0.169 |
HFNC: high-flow nasal cannula; ECMO: extracorporeal membrane oxygenation; KL-6: Krebs von den Lungen-6; NP: nasal prong. Values are presented as a number (%), mean (standard deviation (SD)), or median (interquartile range). € Tested by chi-squared test for categorical variables and by t-test for continuous ones. * Tested by Fisher’s exact test.
3.2. Risk Factors for Post-COVID-19 Pulmonary Fibrosis
In the multivariate regression analysis, an older age (adjusted odds ratio (AOR) 1.12; 95% CI 1.03–1.21) and a lower initial SpO2/FiO2 ratio (AOR 7.17; 95% CI 1.72–29.91) were found to be significant independent risk factors for pulmonary fibrosis after COVID-19 pneumonia (Table 3).
Table 3.
Multivariate regression analysis for independent risk factors for post-COVID-19 fibrosis.
| Variable | Crude OR (95% CI) |
p-Value | Adjusted OR €
(95% CI) |
p-Value |
|---|---|---|---|---|
| Age (years) | 1.08 (1.04–1.13) | <0.001 | 1.12 (1.03–1.21) | <0.001 |
| Sex (male) | 0.92 (0.39–2.13) | 0.842 | 1.19 (0.30–4.75) | 0.804 |
| BMI (kg/m2) | ||||
| 18.0–22.9 | 1.00 (ref) | 0.465 * | 1.00 (ref) | 0.355 * |
| 23.0–24.9 | 0.81 (0.28–2.34) | 0.694 | 1.85 (0.40–8.53) | 0.428 |
| ≥25.0 | 0.55 (0.20–1.49) | 0.237 | 0.67 (0.15–3.02) | 0.604 |
| Ex-smoker or current smoker | 1.41 (0.63–3.14) | 0.402 | 2.38 (0.66–8.59) | 0.185 |
| Charlson Comorbidity Index | ||||
| 0–1 | 1.00 (ref) | 1.00 (ref) | ||
| ≥2 | 5.05 (2.13–11.97) | <0.001 | 0.79 (0.15–4.28) | 0.782 |
| KL-6 (U/mL) | ||||
| <450 | 1.00 (ref) | 0.055 * | 1.00 (ref) | 0.208 * |
| ≥450 | 3.55 (1.26–10.04) | 0.017 | 3.09 (0.76–12.52) | 0.115 |
| Unavailable | 1.44 (0.55–3.77) | 0.453 | 0.91 (0.24–3.43) | 0.885 |
| LDH (U/L) | ||||
| <400 | 1.00 (ref) | 0.043 * | 1.00 (ref) | 0.620 * |
| ≥400 | 2.96 (1.26–6.92) | 0.013 | 1.03 (0.23–4.58) | 0.975 |
| Unavailable | 2.06 (0.27–15.80) | 0.489 | 3.94 (0.25–61.84) | 0.329 |
| AST (U/L) | ||||
| <50 | 1.00 (ref) | 1.00 (ref) | ||
| ≥50 | 3.12 (1.30–7.49) | 0.011 | 3.04 (0.71–13.07) | 0.134 |
| Albumin (g/dL) | ||||
| ≥3.8 | 1.00 (ref) | 1.00 (ref) | ||
| <3.8 | 3.14 (1.37–7.22) | 0.007 | 2.96 (0.83–10.52) | 0.094 |
| SpO2/FiO2 ratio | ||||
| ≥300 | 1.00 (ref) | 1.00 (ref) | ||
| <300 | 4.60 (1.89–11.22) | 0.001 | 7.17 (1.72–29.91) | 0.007 |
BMI: body mass index; KL-6: Krebs von den Lungen-6; ICU: intensive care unit; OR: odds ratio; CI: confidence interval. * p for trend. € Adjusted for all variables listed on the tables.
3.3. Characteristics of Radiological Findings in the Fibrosis Group
The detailed radiologic features of the 43 follow-up chest CT scans from the fibrosis group 3 months after discharge are summarized in Table 4. Parenchymal bands were present in all CT scans, with evidence of pulmonary fibrosis this accounted for 43.88% of the total study population. Other fibrotic features were also observed in relatively small populations; traction bronchiectasis with or without volume loss was present in eight (8.16%), reticulation in one (1.02%), and honeycombing in two (2.04%) follow-up CT scans.
Table 4.
Characteristic radiological findings according to the component of pulmonary fibrosis in chest CT scans.
| Image Findings, Yes (N, % of Fibrosis Group) | |
|---|---|
| Parenchymal bands | 43 (100%) |
| Traction bronchiectasis ± volume loss | 8 (18.6%) |
| Reticulation | 1 (2.3%) |
| Honeycombing | 2 (4.7%) |
4. Discussion
This study was conducted in a single national hospital to identify the clinical courses and prognostic factors of pulmonary fibrosis after COVID-19 pneumonia by investigating patients who developed fibrotic sequelae in the 3-month follow-up CT scans. A total of 43 (43.9%) out of 98 patients presented with a fibrotic change. An older age and a low initial SpO2/FiO2 ratio were significant risk factors for pulmonary fibrosis after COVID-19. In the chest CT findings, parenchymal bands were the dominant feature in the fibrosis group; traction bronchiectasis with/without volume loss, reticulation, or honeycombing appeared in less than one-tenth of the population.
The significant prognostic factors identified in our study were consistent with the findings of other studies. An older age is a widely acknowledged risk factor for pulmonary fibrosis after COVID-19 in many multivariate analyses [20,21,22]. In a Chinese study, although 61% of the study population presented a complete radiological resolution after seven months, older patients were more likely to develop fibrosis [23]. In previous outbreaks of coronaviruses such as severe acute respiratory syndrome and Middle East respiratory syndrome coronavirus, an older age has also been suggested to be a risk factor for pulmonary fibrosis [24,25]. Fibrotic changes after a respiratory viral infection could be explained by the increasing disease severity in older patients or physiological susceptibility of the aged lung [26].
A lower initial SpO2/FiO2 ratio represented a higher initial disease severity. This finding was in line with the WHO guidelines, in which the extent of the oxygen demand is one of the major criteria for the classification of the disease severity [27]. Nabahati et al. [10] adapted this definition and reported that patients with severe pneumonia (oxygen saturation < 94%, PaO2/FiO2 < 300, respiratory rate > 30, or lung filtrates > 50%) had a higher risk of pulmonary fibrosis. In a large Chinese cohort study, patients with a high disease severity (high-flow nasal cannula, non-invasive ventilation, or invasive mechanical ventilation) in the acute phase were likely to have a decreased diffusion capacity and CT abnormalities after discharge [28]. This suggests that an excessive viral activity is correlated with a fibroproliferative response and an impairment in the gas exchange.
In previous studies, laboratory findings (including interleukin-6 (IL-6), LDH, interferon-gamma, and KL-6 levels) have been suggested to be prognostic factors for pulmonary fibrosis [9,14,15,29,30]. Our study also attempted to identify the clinically significant laboratory indicators. High LDH (≥400 U/L), AST (≥50 U/L), KL-6 (≥450 U/mL), and low albumin (<3.8 g/dL) levels appeared to be significant in the univariate analysis (p < 0.05); however, their predictive values were not proven in our multivariate model. Earlier studies have suggested that high KL-6 is a predictive indicator of pulmonary fibrosis in COVID-19 [14,15]. Although not statistically significant, our results in the multivariate analysis were similar to those of recent studies. Considering that our collection of KL-6 data was incomplete, its predictive power could be promising in future studies.
The percentage of fibrotic change and its components have varied in previous studies exploring the pulmonary consequence of patients with COVID-19 pneumonia, ranging from approximately 20% to 70% [20,31,32,33]. This variance might be derived from the lack of an established clear definition and the occurrence of pulmonary fibrosis following COVID-19. Our study findings were consistent with those of an Egyptian study in which 90 (52.0%) of 173 patients with moderate to severe COVID-19 pneumonia presented with pulmonary fibrosis at a 3-month follow-up. Of the 90 patients, parenchymal bands were observed in 58 (64.4%), bronchiectasis in 11 (12.2%), and honeycombing in 4 (4.4%) [10]. Similarly, in a Chinese study, 141 (68.12%) of 207 patients showed pulmonary fibrosis 91–120 days after the onset [22]. In an Italian study, 72% of 118 patients showed fibrosis-like changes at a 6-month follow-up [31] whereas in another Italian study with 220 patients, radiological sequelae were observed in 45 (20%) patients 3–6 months after discharge [34].
In most studies, patients with more than a moderate disease severity were selected for the study population [10,22,31,34]. Our study also included patients with moderate to severe COVID-19 pneumonia. However, marked differences between the results may have occurred due to varying study designs such as the clinical characteristics of the populations, definitions of fibrosis, and study durations. In real-world clinical practice, it is important to identify patients who are likely to develop fibrotic changes and who require long-term management.
As many patients have reported persistent symptoms after COVID-19, the concept of long COVID has been suggested. Osikomaiya et al. [35] reported that a moderate disease severity had significantly higher odds of persistent COVID-19-like symptoms after discharge than a mild severity. In a systematic review, the most frequent symptom was a shortness of breath or dyspnea, with a median frequency of 36.0% in 26 studies [6]. In clinical settings, respiratory symptoms are often observed in patients post-COVID-19, ranging from minor discomfort to recurrent hospitalization or even death due to an unresolved respiratory failure.
Fibrotic changes in the lungs have been proposed as the main cause of a reduced pulmonary function. In a 3-month follow-up study conducted by Cocconcelli et al. [34], patients with pulmonary fibrosis were more likely to present with dyspnea with modified Medical Research Council scale scores of 1 and 2. However, a gradual recovery from fibrotic changes and the related symptoms has been observed in long-term studies [22,36]. Moreover, in a British study, an early treatment with corticosteroids was proven to be effective in improving persistent dyspnea and a decreased pulmonary function [37]. Therefore, it is important to understand the progression of pulmonary fibrosis in COVID-19 and identify its prognostic factors from the initial stage of treatment.
The strength of our study was the prospective follow-up of patients with moderate to severe COVID-19. We were able to evaluate the radiological proportion and clinical features of pulmonary fibrosis in patients with a severity requiring hospitalization. In addition, our study identified the clinical risk factors for fibrotic changes, which can be used to predict the disease progression and provide personalized treatment plans.
This study had several limitations. First, the follow-up CT was conducted only once, and 3 months was a relatively short period for evaluating the long-term sequelae of COVID-19. Follow-up CTs for longer period might be needed to provide more evidence for the disease progression and reversibility. Second, this study was conducted at a single center. However, the National Medical Center functioned as a tertiary referral hospital during the COVID-19 outbreak; therefore, our study population may have represented the disease severity and progression of the general population. Third, our study design did not include CT findings at admission. As a result, a quantitative radiologic evaluation of the initial disease severity was absent in the study. Finally, the study design only included patients who successfully recovered and were discharged; those who died during hospitalization were excluded from the study population. Even though our institution was one of the main referral hospitals providing treatment to patients with severe COVID-19, our study population included a small number of patients who required mechanical ventilation or extracorporeal membrane oxygenation. As these populations are expected to present the most severe disease progression, the fibrotic changes in COVID-19 could have been underestimated in this study. Future studies on a large scale with a longitudinal design and a longer follow-up are needed to investigate fibrosis occurring consequently in patients with pneumonia.
5. Conclusions
This study revealed that an older age and a low initial SpO2/FiO2 ratio were crucial in predicting pulmonary fibrosis after COVID-19 pneumonia. Further studies are needed to evaluate the long-term prognosis of fibrotic sequelae and the possible treatment options.
Acknowledgments
The authors would like to thank to respiratory coordinator nurses, Yun-sun Kim and Myeong ju Seok, for their contribution toward this study.
Author Contributions
I.L., J.K. (Joohae Kim), Y.Y. (Yohwan Yeo) and J.K. (Junghyun Kim): study conception and design, data analysis and interpretation, manuscript drafting, and revision; J.Y.L., I.J., J.-S.J., G.K., B.S.C., Y.K., M.-K.K. and J.J.: data collection, data interpretation, and critical review of manuscript; Y.Y. (Yup Yoon) and S.C.J.: data analysis and interpretation. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study protocol was approved by the Institutional Review Board of the National Medical Center (NMC-2021-04-032). The present study was registered with the Clinical Research Information Service (No. KCT0006312).
Informed Consent Statement
Written informed consent was provided by the individual patients or their caregivers with a legal deputy.
Data Availability Statement
De-identified participant data are available upon reasonable request to the corresponding author (Junghyun Kim) by e-mail for the study protocols with the approval of the institutional review board.
Conflicts of Interest
The authors declare that there are no conflicts of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Funding Statement
This research was supported by a grant from the National Medical Center of the Republic of Korea (grant number NMC2021-General Research Program-04).
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Lu H., Stratton C.W., Tang Y.W. Outbreak of pneumonia of unknown etiology in Wuhan, China: The mystery and the miracle. J. Med. Virol. 2020;92:401–402. doi: 10.1002/jmv.25678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wu J.T., Leung K., Leung G.M. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: A modelling study. Lancet. 2020;395:689–697. doi: 10.1016/S0140-6736(20)30260-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhu N., Zhang D., Wang W., Li X., Yang B., Song J., Zhao X., Huang B., Shi W., Lu R., et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N. Engl. J. Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Seessle J., Waterboer T., Hippchen T., Simon J., Kirchner M., Lim A., Muller B., Merle U. Persistent Symptoms in Adult Patients 1 Year After Coronavirus Disease 2019 (COVID-19): A Prospective Cohort Study. Clin. Infect. Dis. 2022;74:1191–1198. doi: 10.1093/cid/ciab611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sykes D.L., Holdsworth L., Jawad N., Gunasekera P., Morice A.H., Crooks M.G. Post-COVID-19 Symptom Burden: What is Long-COVID and How Should We Manage It? Lung. 2021;199:113–119. doi: 10.1007/s00408-021-00423-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nasserie T., Hittle M., Goodman S.N. Assessment of the Frequency and Variety of Persistent Symptoms Among Patients With COVID-19: A Systematic Review. JAMA Netw. Open. 2021;4:e2111417. doi: 10.1001/jamanetworkopen.2021.11417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Guan C.S., Lv Z.B., Yan S., Du Y.N., Chen H., Wei L.G., Xie R.M., Chen B.D. Imaging Features of Coronavirus disease 2019 (COVID-19): Evaluation on Thin-Section CT. Acad. Radiol. 2020;27:609–613. doi: 10.1016/j.acra.2020.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shi H., Han X., Jiang N., Cao Y., Alwalid O., Gu J., Fan Y., Zheng C. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: A descriptive study. Lancet Infect. Dis. 2020;20:425–434. doi: 10.1016/S1473-3099(20)30086-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zou J.N., Sun L., Wang B.R., Zou Y., Xu S., Ding Y.J., Shen L.J., Huang W.C., Jiang X.J., Chen S.M. The characteristics and evolution of pulmonary fibrosis in COVID-19 patients as assessed by AI-assisted chest HRCT. PLoS ONE. 2021;16:e0248957. doi: 10.1371/journal.pone.0248957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nabahati M., Ebrahimpour S., Khaleghnejad Tabari R., Mehraeen R. Post-COVID-19 pulmonary fibrosis and its predictive factors: A prospective study. Egypt. J. Radiol. Nucl. Med. 2021;52:248. doi: 10.1186/s43055-021-00632-9. [DOI] [Google Scholar]
- 11.Gentile F., Aimo A., Forfori F., Catapano G., Clemente A., Cademartiri F., Emdin M., Giannoni A. COVID-19 and risk of pulmonary fibrosis: The importance of planning ahead. Eur. J. Prev. Cardiol. 2020;27:1442–1446. doi: 10.1177/2047487320932695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Collins B.F., Raghu G. Antifibrotic therapy for fibrotic lung disease beyond idiopathic pulmonary fibrosis. Eur. Respir. Rev. 2019;28:190022. doi: 10.1183/16000617.0022-2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bazdyrev E., Rusina P., Panova M., Novikov F., Grishagin I., Nebolsin V. Lung Fibrosis after COVID-19: Treatment Prospects. Pharmaceuticals. 2021;14:807. doi: 10.3390/ph14080807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Xue M., Zhang T., Chen H., Zeng Y., Lin R., Zhen Y., Li N., Huang Z., Hu H., Zhou L. Krebs Von den Lungen-6 as a predictive indicator for the risk of secondary pulmonary fibrosis and its reversibility in COVID-19 patients. Int. J. Biol. Sci. 2021;17:1565–1573. doi: 10.7150/ijbs.58825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Naderi N., Rahimzadeh M. Krebs von den Lungen-6 (KL-6) as a clinical marker for severe COVID-19: A systematic review and meta-analyses. Virology. 2022;566:106–113. doi: 10.1016/j.virol.2021.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yamaya T., Hagiwara E., Baba T., Kitayama T., Murohashi K., Higa K., Sato Y., Otoshi R., Tabata E., Shintani R. Serum Krebs von den Lungen-6 levels are associated with mortality and severity in patients with coronavirus disease 2019. Respir. Investig. 2021;59:596–601. doi: 10.1016/j.resinv.2021.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hansell D.M., Bankier A.A., MacMahon H., McLoud T.C., Müller N.L., Remy J. Fleischner Society: Glossary of terms for thoracic imaging. Radiology. 2008;246:697–722. doi: 10.1148/radiol.2462070712. [DOI] [PubMed] [Google Scholar]
- 18.Hansell D.M., Goldin J.G., King T.E., Lynch D.A., Richeldi L., Wells A.U. CT staging and monitoring of fibrotic interstitial lung diseases in clinical practice and treatment trials: A Position Paper from the Fleischner society. Lancet Respir. Med. 2015;3:483–496. doi: 10.1016/S2213-2600(15)00096-X. [DOI] [PubMed] [Google Scholar]
- 19.Hatabu H., Hunninghake G.M., Richeldi L., Brown K.K., Wells A.U., Remy-Jardin M., Verschakelen J., Nicholson A.G., Beasley M.B., Christiani D.C., et al. Interstitial lung abnormalities detected incidentally on CT: A Position Paper from the Fleischner Society. Lancet Respir. Med. 2020;8:726–737. doi: 10.1016/S2213-2600(20)30168-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Han X., Fan Y., Alwalid O., Li N., Jia X., Yuan M., Li Y., Cao Y., Gu J., Wu H. Six-month follow-up chest CT findings after severe COVID-19 pneumonia. Radiology. 2021;299:E177–E186. doi: 10.1148/radiol.2021203153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yasin R., Gomaa A.A.K., Ghazy T., Hassanein S.A., latif Ibrahem R.A., Khalifa M.H. Predicting lung fibrosis in post-COVID-19 patients after discharge with follow-up chest CT findings. Egypt. J. Radiol. Nucl. Med. 2021;52:118. doi: 10.1186/s43055-021-00495-0. [DOI] [Google Scholar]
- 22.Li X., Shen C., Wang L., Majumder S., Zhang D., Deen M.J., Li Y., Qing L., Zhang Y., Chen C. Pulmonary fibrosis and its related factors in discharged patients with new corona virus pneumonia: A cohort study. Respir. Res. 2021;22:203. doi: 10.1186/s12931-021-01798-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liu M., Lv F., Huang Y., Xiao K. Follow-Up Study of the Chest CT Characteristics of COVID-19 Survivors Seven Months After Recovery. Front. Med. 2021;8:636298. doi: 10.3389/fmed.2021.636298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Das K.M., Lee E.Y., Singh R., Enani M.A., Al Dossari K., Van Gorkom K., Larsson S.G., Langer R.D. Follow-up chest radiographic findings in patients with MERS-CoV after recovery. Indian J. Radiol. Imaging. 2017;27:342–349. doi: 10.4103/ijri.IJRI_469_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Antonio G.E., Wong K., Hui D.S., Wu A., Lee N., Yuen E.H., Leung C., Rainer T.H., Cameron P., Chung S.S. Thin-section CT in patients with severe acute respiratory syndrome following hospital discharge: Preliminary experience. Radiology. 2003;228:810–815. doi: 10.1148/radiol.2283030726. [DOI] [PubMed] [Google Scholar]
- 26.Naik P.K., Moore B.B. Viral infection and aging as cofactors for the development of pulmonary fibrosis. Expert Rev. Respir. Med. 2010;4:759–771. doi: 10.1586/ers.10.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.World Health Organization . Living Guidance for Clinical Management of COVID-19: Living Guidance. World Health Organization; Geneva, Switzerland: 2021. [Google Scholar]
- 28.Huang C., Huang L., Wang Y., Li X., Ren L., Gu X., Kang L., Guo L., Liu M., Zhou X. 6-month consequences of COVID-19 in patients discharged from hospital: A cohort study. Lancet. 2021;397:220–232. doi: 10.1016/S0140-6736(20)32656-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wallis T.J., Heiden E., Horno J., Welham B., Burke H., Freeman A., Dexter L., Fazleen A., Kong A., McQuitty C. Risk factors for persistent abnormality on chest radiographs at 12-weeks post hospitalisation with PCR confirmed COVID-19. Respir. Res. 2021;22:157. doi: 10.1186/s12931-021-01750-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hu Z.J., Xu J., Yin J.M., Li L., Hou W., Zhang L.L., Zhou Z., Yu Y.Z., Li H.J., Feng Y.M., et al. Lower Circulating Interferon-Gamma Is a Risk Factor for Lung Fibrosis in COVID-19 Patients. Front. Immunol. 2020;11:585647. doi: 10.3389/fimmu.2020.585647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Caruso D., Guido G., Zerunian M., Polidori T., Lucertini E., Pucciarelli F., Polici M., Rucci C., Bracci B., Nicolai M. Post-Acute sequelae of COVID-19 pneumonia: Six-month Chest CT follow-up. Radiology. 2021;301:E396–E405. doi: 10.1148/radiol.2021210834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gulati A., Lakhani P. Interstitial lung abnormalities and pulmonary fibrosis in COVID-19 patients: A short-term follow-up case series. Clin. Imaging. 2021;77:180–186. doi: 10.1016/j.clinimag.2021.03.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Huang W., Wu Q., Chen Z., Xiong Z., Wang K., Tian J., Zhang S. The potential indicators for pulmonary fibrosis in survivors of severe COVID-19. J. Infect. 2021;82:e5–e7. doi: 10.1016/j.jinf.2020.09.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cocconcelli E., Bernardinello N., Giraudo C., Castelli G., Giorgino A., Leoni D., Petrarulo S., Ferrari A., Saetta M., Cattelan A. Characteristics and prognostic factors of pulmonary fibrosis after COVID-19 pneumonia. Front. Med. 2021;8:3085. doi: 10.3389/fmed.2021.823600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Osikomaiya B., Erinoso O., Wright K.O., Odusola A.O., Thomas B., Adeyemi O., Bowale A., Adejumo O., Falana A., Abdus-Salam I., et al. ‘Long COVID’: Persistent COVID-19 symptoms in survivors managed in Lagos State, Nigeria. BMC Infect. Dis. 2021;21:304. doi: 10.1186/s12879-020-05716-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Farghaly S., Badedi M., Ibrahim R., Sadhan M.H., Alamoudi A., Alnami A., Muhajir A. Clinical characteristics and outcomes of post-COVID-19 pulmonary fibrosis: A case-control study. Medicine. 2022;101:e28639. doi: 10.1097/MD.0000000000028639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Myall K.J., Mukherjee B., Castanheira A.M., Lam J.L., Benedetti G., Mak S.M., Preston R., Thillai M., Dewar A., Molyneaux P.L. Persistent post–COVID-19 interstitial lung disease. An observational study of corticosteroid treatment. Ann. Am. Thorac. Soc. 2021;18:799–806. doi: 10.1513/AnnalsATS.202008-1002OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
De-identified participant data are available upon reasonable request to the corresponding author (Junghyun Kim) by e-mail for the study protocols with the approval of the institutional review board.