Abstract
Background.
The integration of medical and dental care in the dental setting offers a unique opportunity to close medical care gaps, such as providing immunizations and laboratory-based tests, compared with traditional nonintegrated settings.
Methods.
We used a matched cohort study design among patients 65 years or older (n = 2,578) with an index dental visit to the Kaiser Permanente Northwest medical-dental integration (MDI) program from June 1, 2018, through December 31, 2019. MDI patients were matched 1:1 to non-MDI controls (n = 2,578) on 14 characteristics. The Kaiser Permanente Northwest MDI program focuses on closing 23 preventive (for example, flu vaccines) and disease management care gaps (for example, glycated hemoglobin testing) within the dental setting. The closure of all care gaps (yes versus no) was the outcome for the analysis. Multivariable logistic regression was used to evaluate the association between exposure to the MDI program and level of office integration (least, moderate, and most integration) with closure of care gaps. All data were obtained through Kaiser Permanente Northwest’s electronic health record.
Results.
MDI patients had significantly higher odds (odds ratio [OR], 1.46, 95% confidence interval [CI], 1.29 to 1.65) of closing all medical care gaps than non-MDI patients. Greater MDI integration was associated with significantly higher odds of gap closure compared with non-MDI (least integration: OR, 1.18, 95% CI, 1.02 to 1.37; moderate integration: OR, 1.70, 95% CI, 1.36 to 2.12; most integration: OR, 2.08, 95% CI, 1.73 to 2.50).
Conclusions.
Patients receiving dental care in an MDI program had higher odds of closing medical care gaps compared with similar patients receiving dental care in a non-MDI program.
Practical Implications.
MDI is effective at facilitating delivery of preventive and disease management medical services.
Keywords: Medical-dental integration (MDI), medical care gaps, Medicare
Several professional societies recommend ongoing receipt of preventive medical services for adults, such as immunizations (for example, influenza), cancer screening (for example, mammography), and disease management monitoring.1–3 The benefits of receiving these services have been well documented with reductions in morbidity and mortality. For example, regular receipt of glycated hemoglobin (HbA1c) testing for adults with diabetes mellitus (DM) has been shown to improve cardiovascular outcomes for adults with DM.4–8 The need for such services is especially important for people 65 years or older, nearly 80% of whom have 2 or more chronic conditions and require routine preventive and disease management care.9,10
The dental setting has emerged as a potentially effective venue to provide preventive and disease management services to close medical care gaps. Prior research showed that integration of medical and dental health records within the same health system and using electronic health record (EHR) alerts to inform dental providers when their patients are overdue for preventive and disease management services can reduce emergency department (ED) and hospital use.11,12 Other studies have also found that better integration between dental and medical care reduces patient barriers to care access, diabetes-specific hospital admissions, and ED use,11 as well as health care costs and hospital admissions for those with chronic conditions (for example, coronary artery disease) and those who are pregnant.13 Accordingly, the dental setting may represent a unique opportunity within the health care system for completing screening tests, including identification of cardiovascular risk factors14,15 and diabetes,16 as well as for addressing certain unmet medical care needs.
To date, however, no studies have examined the potential benefits of a comprehensive, population-based medical-dental integration (MDI) program on the closure of medical care gaps—defined as completion of recommended preventive medical services for patients who are overdue for these services.2 Kaiser Permanente Northwest (KPNW) is an ideal setting to study this because the membership, EHR, and medical and dental services are all contained within the same delivery system. Two studies within KPNW have examined the receipt of dental care (versus nonreceipt) with use11 and adherence with Healthcare Effectiveness Data Information Set outcomes,12 although these studies did not isolate the impact of MDI, specifically. Furthermore, little is known about whether the level of integration between medical and dental programs is differentially associated with closure of care gaps for patients 65 years or older who are overdue for these services.
METHODS
Population
We conducted a retrospective matched cohort analysis of KPNW medical and dental members who met all 4 inclusion criteria:
65 years or older;
had a dental visit at a KPNW dental clinic from June 1, 2018, through December 31, 2019;
had at least 1 medical care gap at the time of their first (index) dental visit during that time period;
had 12 months of continuous health plan enrollment before an index dental visit.
We included all patients meeting these criteria whose index dental visit occurred at any of the 4 MDI clinics and identified a 1:1 matched sample of patients who met the inclusion criteria and whose index dental visit occurred at 1 of 13 non-MDI dental clinics during the same window. Patients were matched according to sex, care gap type (preventive only, disease management only, or both), age (within 5 years), and dental clinic and index visit date (± 60 days). With respect to dental clinics, the 4 MDI dental clinics were each matched to 3 to 4 non-MDI dental clinics on the basis of total volume of dental staff full-time equivalents and annual volume of dental visits.
Non-MDI patients were further propensity matched to MDI patients based on 7 characteristics: Charlson comorbidity index (0, 1, ≥ 2), smoking status (yes versus no), ED use in the previous 12 months (any versus none), hospitalization in previous 12 months (any versus none), presence of any of 5 systemic conditions (DM, rheumatoid arthritis, cardiovascular disease, coronary artery disease, hypertension; yes versus no), periodontal disease status (healthy/early, moderate, advanced), and total number of open care gaps at the index visit (continuous). Data from KPNW’s EHR were used for the analysis.
Institutional Review Board Approval
The protocol for this study was approved by the institutional review board within KPNW. The need for individual consent for data use was waived.
Setting
KPNW serves approximately 605,000 medical members and 250,000 dental members in Oregon and Washington. The KPNW MDI program includes 3 distinct model types used in 4 dental clinics. Each model is described as follows: least, moderate, or most integration. The least MDI model was implemented June 1, 2018, while the other 2 models were implemented on August 1, 2018.
Least Integration
One medical and dental office is located in the same building with no medical staff embedded in the dental office. In this model, a dental member assistant (DMA) identifies care gaps at the time of dental visit and coordinates closely with other medical departments located within the building (for example, laboratory, vision, and nurse treatment center for immunizations) to complete overdue care gaps. The DMA also arranges for on-site follow-up with primary care clinicians for care coordination regarding chronic conditions when directed.
Moderate Integration
One stand-alone dental office has embedded medical staff. A licensed practical nurse (LPN) is embedded within the stand-alone dental clinic to address care gaps. The LPN can provide immunizations, collect samples for laboratory-based tests, and provide other basic services (for example, HbA1c test, blood pressure screening, DM foot examinations) directly in the dental setting. The LPN also coordinates all other medical services that require offsite referrals (for example, mammography) or offsite follow-up with primary care (for example, follow-up regarding abnormal HbA1c results).
Most Integration
Two colocated medical and dental offices have embedded medical staff. These 2 dental offices are colocated within a medical office building, and an LPN is embedded within the dental clinic itself. The LPN provides direct services and coordinates with other colocated medical staff members to complete additional services. At both clinics following this model, a single DMA and LPN work closely to identify care gaps before dental visits. The LPN then provides services to close care gaps that can be directly addressed in the dental setting (for example, immunizations and blood pressure screening) and coordinate with other colocated medical departments to address other care gaps after the dental visit (for example, laboratory-based tests and DM retinopathy screening). The LPN also arranges follow-up care as needed with primary care for care coordination regarding chronic conditions.
Non-MDI dental offices do not include embedding of medical staff members to complete on-site care gap closure or enhanced care coordination to complete needed follow-up services. Within the non-MDI clinics, dental staff members use an EHR-based decision support tool (described below) to remind patients of being overdue for evidence-based preventive and disease management services.
Medical Care Gaps
KPNW dental and medical clinics use the Panel Support Tool (PST) to identify patient care gaps. The PST is EHR based and uses an informatics system that tracks care gaps, patient reminders, and follow-up care and has been in use since 2006.17 The PST lists care gaps for a primary care physician’s panel based on current clinical guidelines and evidence for ongoing screening tests and disease management services.1,2,18
Patients were included in the sample if they had any of 23 care gaps indicated by the PST. Care gaps are listed in the figure and include gaps in preventive care (that is, immunizations and screening tests) and disease management (that is, laboratory-based tests, screening tests, annual examinations, and smoking cessation resources) for patients with diabetes, coronary artery disease, and hypertension; patients taking certain medications; and active or occasional smokers. The primary outcome measure of this study was closure of all medical care gaps present at the index dental visit. For 18 of the 23 measures, care gap closure was assessed 30 days after the index visit; fecal immunochemical testing, mammography, annual DM examination, retinopathy examination, and smoking cessation were assessed at 60 days after the index visit.
Figure.
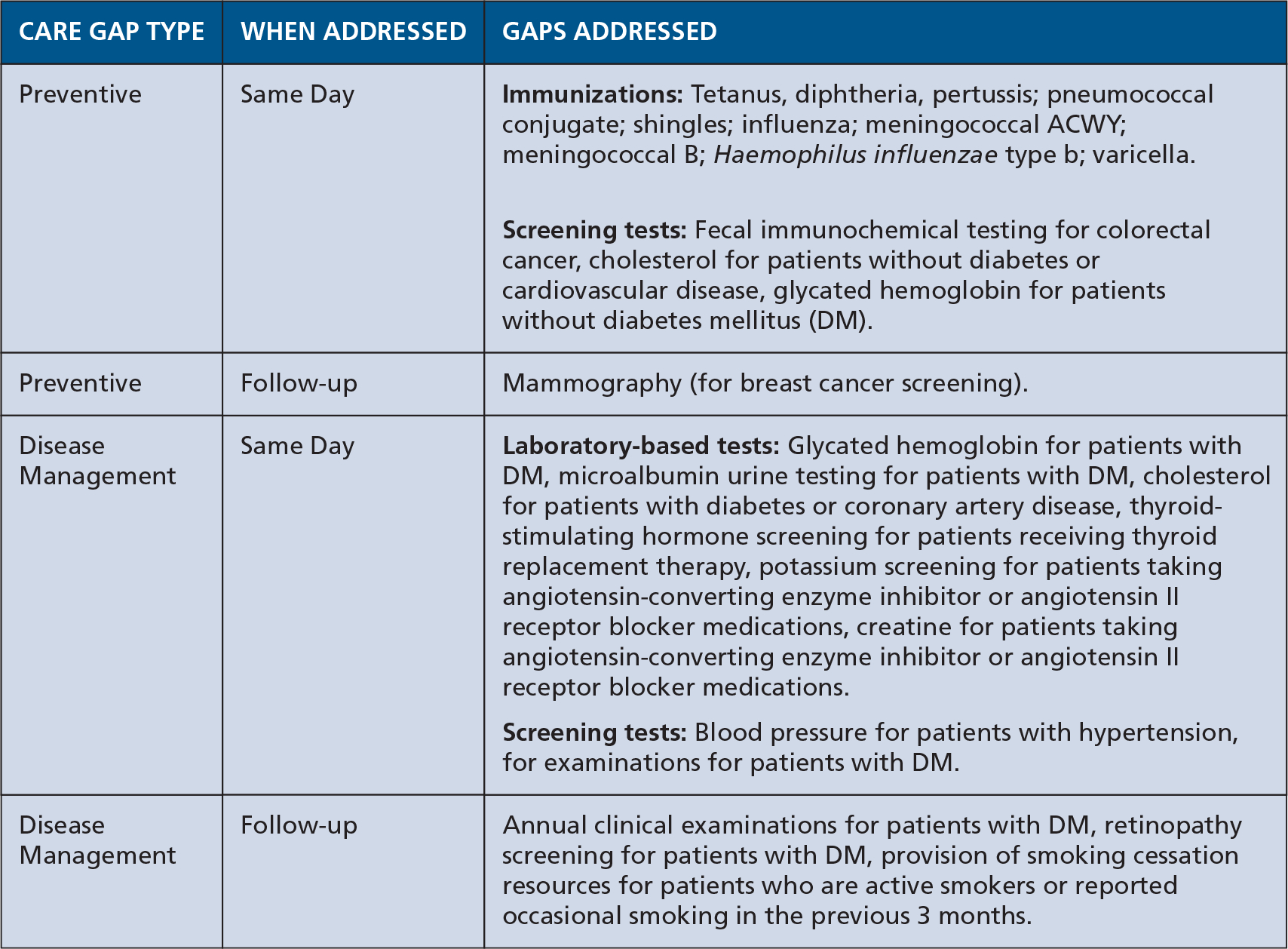
Description of care gaps.
Statistical analyses
We first conducted descriptive analyses of analytic variables to confirm assumptions and as a quality assurance process. To assess the performance of our matching algorithm, we calculated standardized differences of demographic and clinical characteristics between MDI and non-MDI patients. To assess the association between MDI and closure of all care gaps, we used logistic regression models comparing care gap closure between MDI and non-MDI patients. We used the standardized difference as a measure of whether key variables were balanced between groups or should be added to the regression model to control for potential confounding. Larger standardized differences indicate larger differences between groups. Variables with a standardized difference (≥ 0.2 after matching) were considered to be meaningfully different between groups19 and were adjusted for in our models. The threshold of 0.2 has been used previously in observational studies.20,21
However, because no differences of 0.2 or higher were found after matching, we did not conduct further adjustment. To assess the association between level of MDI integration and closure of all care gaps, we conducted a separate analysis with logistic regression and a categorical independent variable consisting of non-MDI population (reference group) and the 3 levels of MDI integration: least integration, moderate integration, and most integration.
RESULTS
Population characteristics
The patients in the MDI and non-MDI groups were well-balanced for gap type, age, sex, and most clinical and demographic variables after matching (Table 1). In both groups, average age was 70.9 years, 40.3% of patients were male, and the mean total number of open care gaps at the index visit was 1.8. Groups differed significantly in comorbidities at baseline (patients in MDI clinics were more likely to have no comorbidities at baseline) and previous hospitalizations (MDI clinic patients were less likely to have been hospitalized in the past 12 months). However, no standardized differences greater than 0.2 between the MDI and non-MDI groups were found.
Table 1.
Population characteristics.*
| CHARACTERISTICS | MDI† CLINICS (N = 2,578), NO. (%) | NON-MDI CLINICS (N = 2,578), NO. (%) | P VALUE | STANDARD DIFFERENCE |
|---|---|---|---|---|
| Exact-Matched Variables | ||||
| Baseline gap type | Not applicable | |||
| Preventive alone | 1,611 (62.5%) | 1,611 (62.5%) | 0.00 | |
| Disease management alone | 538 (20.9%) | 538 (20.9%) | 0.00 | |
| Both types | 429 (16.6%) | 429 (16.6%) | 0.00 | |
| Age, mean (SD‡) matched within 5 years | 70.9 (5.0) | 71.1 (5.1) | .13 | 0.04 |
| Sex (exact match) | ||||
| Male (versus female) | 1,040 (40.3%) | 1,040 (40.3%) | Not applicable | 0.00 |
| Propensity-Matched Variables | .02 | |||
| CCI§ 0 | 1,351 (52.4%) | 1,268 (49.2%) | 0.04 | |
| CCI 1 | 450 (17.5%) | 517 (20.1%) | 0.04 | |
| CCI ≥ 2 | 777 (30.1%) | 793 (30.8%) | 0.01 | |
| Current smoker | ||||
| Yes (versus no) | 158 (6.1%) | 151 (5.9%) | .68 | 0.01 |
| Emergency department use in previous 12 months | ||||
| Yes (versus no) | 398 (15.4%) | 434 (16.8%) | .17 | 0.03 |
| Hospitalization in previous 12 months | ||||
| Yes (versus no) | 166 (6.4%) | 202 (7.8%) | .05 | 0.04 |
| Systemic conditions (% yes) | ||||
| Diabetes mellitus | 707 (27.4%) | 719 (27.9%) | .71 | 0.01 |
| Rheumatoid arthritis | 37 (1.4%) | 37 (1.4%) | Not applicable | 0.00 |
| Cardiovascular disease | 263 (10.2%) | 304(11.8%) | .07 | 0.03 |
| Cardiovascular disease | 309 (12.0%) | 327 (12.7%) | .45 | 0.01 |
| Hypertension | 1,365 (52.9%) | 1,385 (53.7%) | .58 | 0.01 |
| Periodontal disease status | .84 | |||
| Healthy/early | 1,917 (74.4%) | 1,936 (75.1%) | 0.01 | |
| Moderate | 451 (17.5%) | 430 (16.7%) | 0.01 | |
| Advanced | 82 (3.2%) | 78 (3.0%) | 0.01 | |
| Missing | 128 (5.0%) | 134 (5.2%) | 0.01 | |
| Total open gaps at index visit, mean (SD) | 1.8 (1.2) | 1.8 (1.2) | .84 | 0.01 |
| Non – Propensity-Matched Variables | ||||
| Socioeconomic Status: Area Deprivation Index, mean (SD) | 4.6 (2.4) | 4.5 (2.6) | .36 | 0.03 |
Population includes population of Medicare patients 65 years or older with 1 or more care gaps at baseline. P value from t test for age, count of open gaps at baseline, and Area Deprivation Index state rank; P value from χ2 for all other variables.
MDI: Medical-dental integration.
SD: Standard deviation.
CCI: Charlson comorbidity index.
Care gap closure
Patients treated at MDI clinics had significantly higher odds (odds ratio [OR], 1.46, 95% confidence interval [CI], 1.29 to 1.65) of closing all medical care gaps than the non-MDI population. Each integration model was associated with significantly higher levels of care gap closure than the non-MDI population, with ORs increasing as level of embedding increased (Table 2); least integration (OR, 1.18, 95% CI, 1.02 to 1.37), more integration (OR, 1.70, 95% CI, 1.36 to 2.12), and most integration (OR, 2.08, 95% CI, 1.73 to 2.50).
Table 2.
Logistic regression analysis of medical care gap closure,* by total MDI† population and MDI model type.
| MDI POPULATION CHARACTERISTICS | ODDS RATIO | 95% CONFIDENCE INTERVAL | p VALUE |
|---|---|---|---|
| Total MDI Population | |||
| MDI population | 1.46 | 1.29–1.65 | < .0001 |
| Non-MDI population | 1.00 | NA‡ | NA |
| MDI Model Type, Dental Clinic | |||
| Least integration: Colocated medical and dental office, nonembedded medical staff. Salmon Creek | 1.18 | 1.02–1.37 | < .0007 |
| Moderate integration: Stand-alone dental office, embedded medical staff. Glisan | 1.70 | 1.36–2.12 | < .0346 |
| Most integration: Colocated medical and dental office, embedded medical staff. Beaverton, Cedar Hills | 2.08 | 1.73–2.50 | < .0001 |
| Non-MDI population | 1.00 | NA | NA |
Population includes patients enrolled in Medicare who were patients 65 years or older with 1 or more care gaps at baseline. All care gap closure assessed at 30 days after index visit, except for fecal immunochemical testing, mammography, annual diabetes mellitus examination, retinopathy examination, and smoking cessation, which was assessed at 60 days after index visit. P value from logistic regression analysis.
MDI: Medical-dental integration.
NA: Not applicable.
DISCUSSION
Patients 65 years or older who received dental care at an MDI clinic were nearly 1.5 times as likely to close all care gaps than patients who received dental care at a usual care clinic. The care gap closure effect was significant for dental clinics at all 3 levels of integration. We also found that higher levels of MDI were associated with higher levels of care gaps closures. These findings suggest that MDI is an effective way to facilitate use of preventive and disease management health services.
To our knowledge, these results are the first of which we are aware to evaluate the independent effect of MDI with higher care gap closure among patients 65 years or older. Moreover, this study is the first of which we are aware to examine the “dose response” of higher levels of MDI with care gap closure. These findings were consistent with previous research conducted within KPNW, which found that the receipt of dental care was associated with higher use of Healthcare Effectiveness Data Information Set–level preventive services12 and lower DM-specific use.11 Similarly, other research outside of KPNW found the dental setting could promote preventive health. Greenberg and colleagues14 found that by screening patients at an academic dental clinic, previously unidentified cardiovascular risk factors could be identified. In addition, Jontell and Glick15 found that oral health care professionals can screen and identify patients not aware of their risk of developing serious complications from cardiovascular disease and advise these patients to seek medical care. Similarly, a 2014 systematic review22 found that screening for dysglycemia in dental offices effectively identified high-risk patients who required triage for glycemic management. However, our study is the first to isolate the association of MDI with outcomes, using rigorous study methods.
The observation that all 3 integration models improved rates of care gap closure is encouraging, as it suggests that relatively small changes, such as colocating a dental office within a medical building or embedding a single medical staff member within a dental office, can have a real impact on care gap closure when coupled with EHR tools integrating medical and dental records. A key challenge in extending this model to other systems is the typical nonintegration of medical and health care in distinct insurance plans and service networks. However, our study findings do have broad applicability to general dentistry within the United States. In particular, many federally qualified health centers (FQHCs) have care delivery systems that are organized similarly to Kaiser Permanente; dental care is provided at FQHCs with colocated medical staff. Thus, FQHCs could be early adopters of this model. Indeed, some dental FQHCs have already developed similar programs focused on early child medical and dental examinations. Furthermore, our finding of care gap closure with MDI in stand-alone dental offices (the moderate integration group) suggests this model could be implemented in stand-alone dental care delivery settings, where most dental care is provided in the United States. Although barriers persist in implementing this model in solo and small group dental practices, the evidence from this study of the effectiveness in closing medical care gaps in the dental setting suggests that changes in billing and coding of medical and dental procedures to make integration more feasible could lead to long-term cost savings.
The findings from our research have clear policy significance. Medicare does not pay for dental services, except if the care is related to hospitalization. Because of the clear benefit in promoting use of preventive and disease management services among the Medicare population, our results suggest there may be benefits in the Medicare program offering dental insurance coverage to recipients 65 years or older.
We recognize several potential limitations associated with this study. First, use of data from 1 health care system may limit generalizability to other more diverse populations. However, the KPNW membership reflects the underlying population of the area.23,24 Compared with the US population, the total KPNW membership is slightly less white and has a higher proportion of members older than 65 years.25 Another limitation is that the retrospective cohort design uses information from the EHR, which does not enable us to assess causality. However, we think this limitation is reduced owing to a strong retrospective, propensity-score matched design reducing the affect of confounders on the proposed analysis. Lastly, the study did not address the cost-effectiveness of closing care gaps.
Future research should examine the use of LPNs and other medical staff members in smaller, more traditional stand-alone dental offices to understand whether adding such staff members is cost-effective, owing to increasing use of preventive and disease management services. Such studies could inform whether further expansion of MDI services in more traditional dental offices is feasible and effective. Second, future research is needed to evaluate the long-term impact of ongoing use in the MDI program with improvements in long-term health outcomes, reductions in health care use, and potential reductions in health care costs. However, further research is needed to test this specifically. The long-term effects of these MDI programs are a vital question for future study. Given the high level of care gaps among older people and the critical need for screening and disease management among this population, our study focused on patients 65 years or older. However, future research should identify the effectiveness of MDI on younger age groups as well.
CONCLUSIONS
Our data indicate that integrating medical and dental care can effectively close care gaps among older adults and may be an effective, relatively low-cost way to improve health outcomes for this population. More research is needed regarding the long-term health effects of these programs, as well as potential cost and health care use reductions and how such programs can be applied to other dental and health care settings.
Acknowledgments
The study was funded by grant 1R21DE029026-01 from the National Institute of Dental and Craniofacial Research.
ABBREVIATION KEY
- DM
Diabetes mellitus
- DMA
Dental member assistant
- ED
Emergency department
- EHR
Electronic health record
- KPNW
Kaiser Permanente Northwest
- FQHC
Federally qualified heath center
- HbA1c
Glycated hemoglobin
- LPN
Licensed practical nurse
- MDI
Medical-dental integration
- PST
Panel Support Tool
Footnotes
Disclosure. None of the authors reported any disclosures.
Contributor Information
David M. Mosen, Center for Health Research, Kaiser Permanente Northwest, Portland, OR 3800 N Interstate Ave, Portland, OR 97227-1110.
Matthew P. Banegas, Center for Health Research, Kaiser Permanente Northwest, Portland, OR..
John F. Dickerson, Center for Health Research, Kaiser Permanente Northwest, Portland, OR..
Jeffrey L. Fellows, Center for Health Research, Kaiser Permanente Northwest, Portland, OR..
Neon B. Brooks, Center for Health Research, Kaiser Permanente Northwest, Portland, OR..
Daniel J. Pihlstrom, Evidence-based Practice, Permanente Dental Associates, Portland, OR..
Hala M. Kershah, Medical Dental Integration, Dental Administration, Kaiser Permanente Northwest, Portland, OR..
Jason L. Scott, Center for Health Research, Kaiser Permanente Northwest, Portland, OR..
Erin M. Keast, Center for Health Research, Kaiser Permanente Northwest, Portland, OR..
References
- 1.American Diabetes Association. Standards of medical care in diabetes: 2014. Diabetes Care. 2014;37(suppl 1):S14–S80. [DOI] [PubMed] [Google Scholar]
- 2.US Preventive Services Task Force Guides to Clinical Preventive Services. The Guide to Clinical Preventive Services 2014: Recommendations of the U.S. Preventive Services Task Force. Rockville, MD: Agency for Healthcare Research and Quality (US); 2014. [Google Scholar]
- 3.Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019;74(10):e177–e232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nathan DM. The diabetes control and complications trial/epidemiology of diabetes interventions and complications study at 30 years: overview. Diabetes Care. 2014;37(1):9–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tricco AC, Ivers NM, Grimshaw JM, et al. Effectiveness of quality improvement strategies on the management of diabetes: a systematic review and meta-analysis. Lancet. 2012;379(9833):2252–2261. [DOI] [PubMed] [Google Scholar]
- 6.Bierman AS, Lurie N, Collins KS, Eisenberg JM. Addressing racial and ethnic barriers to effective health care: the need for better data. Health Aff (Millwood). 2002;21(3):91–102. [DOI] [PubMed] [Google Scholar]
- 7.Khaw KT, Wareham N, Bingham S, Luben R, Welch A, Day N. Association of hemoglobin A1c with cardiovascular disease and mortality in adults: the European prospective investigation into cancer in Norfolk. Ann Intern Med. 2004;141(6):413–420. [DOI] [PubMed] [Google Scholar]
- 8.National Committee on Quality Assurance (NCQA). Comprehensive Diabetes Care. Available at: https://www.ncqa.org/hedis/measures/comprehensive-diabetes-care/. Accessed February 5, 2021.
- 9.Lochner KA, Cox CS. Prevalence of multiple chronic conditions among Medicare beneficiaries, United States, 2010. Prev Chronic Dis. 2013;10:E61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Buttorff C, Ruder T, Bauman M. Multiple chronic conditions in the United States. Santa Monica, CA: Rand; 2017. [Google Scholar]
- 11.Mosen DM, Pihlstrom DJ, Snyder JJ, Shuster E. Assessing the association between receipt of dental care, diabetes control measures and health care utilization. JADA. 2012;143(1):20–30. [DOI] [PubMed] [Google Scholar]
- 12.Mosen D, Pihlstrom D, Snyder J, Smith N, Shuster E, Rust K. Association of dental care with adherence to HEDIS measures. Perm J. 2016;20(1):33–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jeffcoat MK, Jeffcoat RL, Gladowski PA, Bramson JB, Blum JJ. Impact of periodontal therapy on general health: evidence from insurance data for five systemic conditions. Am J Prev Med. 2014;47(2):166–174. [DOI] [PubMed] [Google Scholar]
- 14.Greenberg BL, Glick M, Goodchild J, Duda PW, Conte NR, Conte M. Screening for cardiovascular risk factors in a dental setting. JADA. 2007;138(6):798–804. [DOI] [PubMed] [Google Scholar]
- 15.Jontell M, Glick M. Oral health care professionals’ identification of cardiovascular disease risk among patients in private dental offices in Sweden. JADA. 2009;140(11):1385–1391. [DOI] [PubMed] [Google Scholar]
- 16.Glurich I, Bartkowiak B, Berg RL, Acharya A. Screening for dysglycaemia in dental primary care practice settings: systematic review of the evidence. Int Dent J. 2018;68(6):369–377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Livaudais G, Unitan R, Post J. Total panel ownership and the panel support tool: “it’s all about the relationship.” Perm J. 2006;10(2):72–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Smith SC Jr., Allen J, Blair SN, et al. AHA/ACC guidelines for secondary prevention for patients with coronary and other atherosclerotic vascular disease: 2006 update: endorsed by the National Heart, Lung, and Blood Institute. Circulation. 2006;113(19):2363–2372. [DOI] [PubMed] [Google Scholar]
- 19.Cohen J Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- 20.Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 2009;28(25):3083–3107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Johnson ES, Dickerson JF, Vollmer WM, et al. The feasibility of matching on a propensity score for acupuncture in a prospective cohort study of patients with chronic pain. BMC Med Res Methodol. 2017;17(1):42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Genco RJ, Genco FD. Common risk factors in the management of periodontal and associated systemic diseases: the dental setting and interprofessional collaboration. J Evid Based Dent Pract. 2014;14(suppl):4–16. [DOI] [PubMed] [Google Scholar]
- 23.Roblin DW. Validation of a neighborhood SES index in a managed care organization. Med Care. 2013;51(1):e1–e8. [DOI] [PubMed] [Google Scholar]
- 24.Koebnick C, Langer-Gould AM, Gould MK, et al. Sociodemographic characteristics of members of a large, integrated health care system: comparison with US Census Bureau data. Perm J. 2012;16(3):37–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vespa J, Armstrong DM, Medina L. Demographic Turning Points for the United States: Population Projections for 2020 to 2060. Washington, DC: United States Census Bureau; 2018. [Google Scholar]


