Introduction
Here, we describe a case of erythroderma in an immunocompetent patient. Erythroderma is commonly associated with psoriasis (20%), drug reactions (19%), atopic dermatitis (9%), cutaneous T-cell lymphoma (CTCL) (8%), contact dermatitis (6%), and seborrheic dermatitis (4%).1 Scabies infestation, caused by the Sarcoptes scabiei mite, is a common dermatologic condition with an estimated number of 100 million cases annually.2 However, very few individuals with scabies present with erythroderma. This represents a fulminant infestation, termed crusted (Norwegian) scabies, usually seen in immunocompromised or debilitated patients with impaired sensory response.2 Scabies is generally transmitted by prolonged skin-to-skin contact with an infected person. It can also spread by contact with items such as the clothing or bedding of an infected individual. Both modes of transmission are more likely with crusted scabies. Treatment of crusted scabies requires special consideration, frequently with combined systemic and topical agents. With this case description, we aim to aid in the early recognition and management of erythrodermic crusted scabies.
Case report
An 80-year-old woman with a history of ulcerative colitis, hypothyroidism, and atopy was referred to our practice for an erythematous rash and pruritus lasting 1 year. She was previously treated with topical and systemic corticosteroids, broadband UV-B, and empiric topical permethrin without improvement. Four doses of dupilumab 300 mg were also administered; however, her rash had been expanding, and the pruritus was worsening and causing sleep disturbance. She reported no other medication changes and had not used new soaps, lotions, or detergents. There was no fever, chills, joint pain, lymph node swelling, cough, or other infectious symptoms and no record of a previous skin biopsy. Distributed on the scalp, face, trunk, extremities, and periungual areas were thick crusted erythematous plaques with fissures and focal powdery scale (Fig 1). There was no nail dystrophy, scleral involvement, or mucosal involvement. Palms and soles were clear, Nikolsky sign was negative, and there were no pustules. She had no history of psoriasis or lymphoproliferative disorder and did not take any over-the-counter medications or herbal supplements. The patient had never received hematopoietic cell transplantation or blood products. Complete blood count revealed mild leukocytosis of 11,700 white blood cells/uL (210 eosinophils/uL) and platelets and hematocrit within normal limits. Serum creatinine, serum electrolytes, and kidney function studies were within normal limits. Two skin biopsies and flow cytometry of peripheral blood were performed. Diagnoses considered included atopic dermatitis, CTCL, psoriasis, crusted (Norwegian) scabies, and an autoimmune connective tissue disease. Flow cytometry did not show clonal a T cell population or otherwise demonstrate evidence of lymphoproliferative disease. Histopathology (Fig 2) showed spongiosis, parakeratosis, and acanthosis as well as a perivascular and interstitial mixed inflammatory infiltrate including lymphocytes and eosinophils. In both biopsy samples, in the stratum corneum, there were multiple organisms morphologically compatible with scabies. A diagnosis of crusted scabies was established. Systemic therapy with 2 courses of 200 μg/kg of ivermectin, separated by 10 days, was instituted in addition to topical 5% permethrin. The patient was advised to decontaminate bedding, clothes, and towels and dispose of items that cannot be sanitized. One week later, the patient reported improvement of pruritus and clearing of her rash. At a follow-up visit 2 weeks after therapy initiation, her disseminated erythematous plaques had resolved, pruritus ceased, and sleep was restored.
Fig 1.
Erythroderma. Representative clinical image (A) trunk and (B) face.
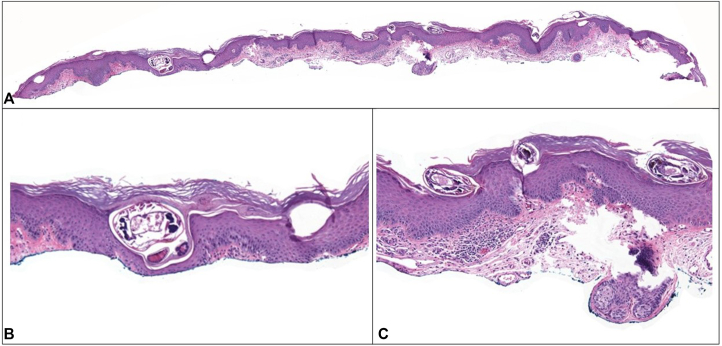
Fig 2.
Histopathology of the biopsy site on the trunk. Low magnification (A) and high magnification (B and C) representative images showing multiple Sarcoptes scabiei mites in epidermis.
Discussion
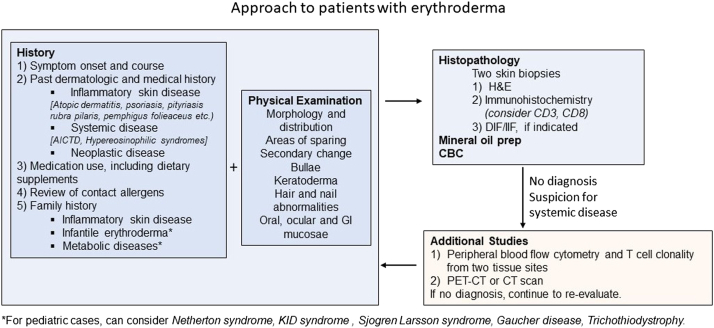
A case of erythroderma caused by crusted scabies in an immunocompetent individual is described. Erythroderma, defined as generalized redness and scaling of the skin, is a nonspecific clinical presentation with multiple etiologies. In adults, common causes include psoriasis (20%), drug reactions (19%), atopic dermatitis (9%), CTCL (8%), and contact dermatitis (6%). In neonates, ichthyoses, staphylococcal scalded skin syndrome, and immunodeficiency are common. For individuals our patient’s age, it is also imperative to consider HIV, syphilis, and other sexually transmitted diseases, since they are at higher risk of contracting these conditions. Scabies is a comparatively rare cause of erythroderma, accounting for less than 0.5% of cases.3 An erythroderma diagnostic algorithm is depicted in Fig 3.
Fig 3.
Diagnostic algorithm for patients with erythroderma.
Review of literature identified previous reports of erythroderma in the setting of scabies infestation in immunocompromised4 or individuals with defective sensory response,5 which are risk factors for crusted scabies. In contrast, our report describes an immunocompetent and physically active patient who was previously treated with permethrin. Although limited evidence exists regarding type 2 immune responses against scabies, it is possible that dupilumab exacerbated scabies here. Therefore, when eczematous eruptions worsen on dupilumab, scabies should be considered in addition to allergic contact dermatitis and CTCL.
A summary of treatments for scabies is shown in Table I. Topical permethrin failure has been reported in up to 10% of cases in meta-analyses.6 This can occur due to (1) reinfestation with scabies from a family member or contaminated clothing, (2) inappropriate treatment or secondary failure due to poor penetration into thick scaly skin containing large numbers of mites, or (3) permethrin resistance, which has been described but may be increasing and underreported.7,9 After establishing the diagnosis, the patient volunteered that she performed a single application of permethrin and did not decontaminate her belongings prior to referral to our practice.
Table I.
| Treatment | Application | Side effects | Notes |
|---|---|---|---|
| Scabies | |||
| Permethrin 5% cream OR | Apply for 8-14 h, repeat in 7 days | Nausea, dizziness, pruritus abdominal pain, and fever | Pregnancy category B |
| Ivermectin 200 μg/kg OR | Take on days 1 and 8 | Neck dystonia, pruritus, burning, and stinging | Contraindicated in children <15 kg |
| Lindane 1% lotion OR | Apply for 8 h, repeat in 7 d | Neurotoxicity and seizures (black box warning) | Contraindicated in seizure disorder |
| Spinosad 0.9% topical suspension OR | Apply for 6 h | Burning, erythema, and xeroderma | |
| Crotamiton 10% cream OR | Apply for 8 h on days 1, 2, 3, and 8 | Pruritus | Limited efficacy data |
| Precipitated sulfur 5% to 10% | Apply for 8 h on days 1, 2, and 3 | Pruritus, burning, and stinging | Limited efficacy data |
| Crusted scabies | |||
| Permethrin 5% cream AND | Apply daily for 7 d then twice weekly | ||
| Ivermectin 200 μg/kg | Take on days 1, 2, 8, 9, and 15 |
Two meta-analyses6,10 found comparable clearance rates of scabies with oral ivermectin and topical permethrin. Two recent phase 3, placebo-controlled randomized controlled trials also showed that topical spinosad is an effective scabies treatment.8 Its efficacy compared to oral ivermectin and topical permethrin remains unclear, however, and it has not been tested in crusted scabies. For crusted scabies, the Center for Disease Control currently recommends treating with combined oral ivermectin (200 ug/kg on days 1, 2, 8, 9, and 15) and topically with 5% permethrin or 25% benzoyl benzoate (daily for 7 days, then twice weekly until cure).2 This case demonstrates the importance of considering crusted scabies as a cause of erythroderma and the importance of proper treatment application by (1) treating patients and contacts at the same time, (2) ensuring re-treatment 1 week apart, and (3) ensuring decontamination. A straightforward method to ensure decontamination is high temperature treatment in a clothes dryer, as Sarcoptes scabiei mites are destroyed by exposure to 122 °F for 10 minutes.
Conflicts of interest
RT and GM have no conflicts of interest to declare. WD has research funding from Pfizer, is a consultant for Eli Lilly and Twi Biotechnology, and receives licensing fees from EMD/Sigma/Millipore in unrelated work. BK has served on advisory boards and/or is a consultant and/or is a clinical trial investigator for Abbvie, Aclaris Therapeutics Inc, AltruBio Inc, Almirall, Arena Pharmaceuticals, Bioniz Therapeutics, Bristol-Meyers Squibb, Concert Pharmaceuticals Inc, Dermavant Sciences Inc, Eli Lilly and Company, Incyte Corp, LEO Pharma, Otsuka/Visterra Inc, Pfizer Inc, Regeneron, Sanofi Genzyme, TWi Biotechnology Inc, and Viela Bio. BK is on speaker bureaus for Eli Lilly, Incyte, Pfizer, Regeneron, and Sanofi Genzyme.
Footnotes
Funding sources: There were no funding sources for this work. RT is supported by NIH F30CA254246-01. WD is supported by a Career Development Award from NIAMS (K08AI159229-01). GM is supported by a NIAID-funded fellowship T32AR007016-47 to Yale Department of Dermatology. GM has been supported by the Dermatology Foundation and American Skin Association.
IRB approval status: Not applicable.
Consent information: The patient consented to the publication of their photographs and medical information for the purpose of this report, and consent forms are on the file.
References
- 1.Rothe M.J., Bernstein M.L., Grant-Kels J.M. Life-threatening erythroderma: diagnosing and treating the “red man”. Clin Dermatol. 2005;23(2):206–217. doi: 10.1016/j.clindermatol.2004.06.018. [DOI] [PubMed] [Google Scholar]
- 2.Chandler D.J., Fuller L.C. A review of scabies: an infestation more than skin deep. Dermatology. 2019;235:79–90. doi: 10.1159/000495290. [DOI] [PubMed] [Google Scholar]
- 3.Das A., Bar C., Patra A. Norwegian scabies: rare cause of erythroderma. Indian Dermatol Online J. 2015;6(1):52. doi: 10.4103/2229-5178.148951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Quay E.R., Lam C. An important cause of erythroderma. BMJ. 2017;357:j1205. doi: 10.1136/bmj.j1205. [DOI] [PubMed] [Google Scholar]
- 5.Mehta V., Balachandran C., Monga P., Rao R., Rao L. Images in clinical practice. Norwegian scabies presenting as erythroderma. Indian J Dermatol Venereol Leprol. 2009;75(6):609–610. doi: 10.4103/0378-6323.57726. [DOI] [PubMed] [Google Scholar]
- 6.Dhana A., Yen H., Okhovat J.P., et al. Ivermectin versus permethrin in the treatment of scabies: a systematic review and meta-analysis of randomized controlled trials. J Am Acad Dermatol. 2018;78(1):194–198. doi: 10.1016/j.jaad.2017.09.006. [DOI] [PubMed] [Google Scholar]
- 7.Akaslan T., Mert Ö., Küçük Ö.S. Scabies increase during the COVID-19 pandemic: should we change our treatment strategy during the pandemic? Ann Parisitol. 2022;68(1):35–38. doi: 10.17420/ap6801.405. [DOI] [PubMed] [Google Scholar]
- 8.Seiler J.C., Keech R.C., Aker J.L., et al. Spinosad at 0.9% in the treatment of scabies: efficacy results from 2 multicenter, randomized, double-blind, vehicle-controlled studies. J Am Acad Dermatol. 2022;86(1):97–103. doi: 10.1016/j.jaad.2021.07.074. [DOI] [PubMed] [Google Scholar]
- 9.Sunderkötter C., Aebischer A., Neufeld M., et al. Increase of scabies in Germany and development of resistant mites? Evidence and consequences. J Dtsch Dermatol Ges. 2019;17(1):15–23. doi: 10.1111/ddg.13706. [DOI] [PubMed] [Google Scholar]
- 10.Rosumeck S., Nast A., Dressler C. Evaluation of ivermectin vs permethrin for treating scabies-summary of a Cochrane review. JAMA Dermatol. 2019;155(6):730–732. doi: 10.1001/jamadermatol.2019.0279. [DOI] [PubMed] [Google Scholar]