Abstract
Rule-out of acute myocardial infarction (AMI) in patients presenting with acute chest pain at the emergency department (ED) is a major challenge across the globe. Patients presenting very early with chest pain may provide a diagnostic challenge even when using a cardiac necrosis specific biomarker, high sensitivity troponin (hs-Tn) as they are elevated at 3–6 h after the symptom onset. Copeptin is a marker of acute hemodynamic stress which is released within few minutes of the occurrence of MI and is elevated immediately at the presentation of patients with AMI. This indicates a complementary pathophysiology and kinetics of these two biomarkers. Hence, we evaluated whether or not a protocol with combined testing of copeptin and hs-TnI at admission in patients presenting with chest pain within 6 h in low to intermediate risk and suspected ACS leads to an earlier diagnosis of AMI and thereby, aids to prevent a higher proportion of major adverse cardiac events than the current standard protocol followed in ED. A total of 148 patients as per the inclusion criterion were recruited for the study. The dual biomarker copeptin and hs-TnI allows a rule-out of AMI at presentation with a sensitivity of 100% and NPV of 99.8%. Hence, the use of dual biomarker in conjunction with clinical assessment may obviate the need for a prolonged stay in the ED and retesting hs-TnI after 2 h (for delta check) in more than two–thirds of the patients. The inclusion of these tests could have an impact on the economic burden of the ED without jeopardizing the outcome for the patient.
Keywords: Acute coronary syndrome (ACS), Rule-out, Acute myocardial infarction (AMI), High sensitivity troponin (hs-Tn), Copeptin
Introduction
Acute Coronary Syndrome (ACS) is one of the major causes of mortality and morbidity globally and is one of the most common reasons patients present to the Emergency Department (ED). Most of the patients are subjected to 6–12 h observation in chest pain units (CPU) with a resultant excellent prognosis but at a high cost and rule-out of acute myocardial infarction (AMI) becomes a major challenge in the ED. Therefore, the critical issue is the quick and accurate identification and management of patients with the ACS, while appropriately discharging those not requiring urgent therapy and hospitalization. Hence, there is a need for the identification of a biomarker or a combination of biomarkers that can play a pivotal role in the diagnosis and rule out AMI. Over the past decades' cardiac troponins, which are very sensitive and specific indicators of myocardial damage, have emerged as key biomarkers for patients with ACS and have undoubtedly improved the rate of detection of silent ACS. ECG (Electrocardiograph) recording and cardiac troponin (Tn) measurement at presentation have been the diagnostic tools for the assessment of patients with possible ACS who present to the ED [1, 2]. A further clinically relevant increase in the sensitivity of cardiac Tn at an early diagnostic stage was achieved with the introduction of high-sensitivity cardiac troponin (hs-Tn) T and I assays [3]. Although, they are capable of detecting myocardial necrosis earlier than conventional Tn assay, still there remains a Tn-blind period very early after the onset of symptoms due to the delayed release of Tn following cardiac injury. Therefore, there is a need of a biomarker that is released instantly in the event of hemodynamic stress, as is evidenced in MI too, which would enable better risk stratification of patients with chest pain.
In such a scenario, one of the major hypothalamic stress hormones, arginine vasopressin (AVP), plays a crucial role in the regulation of the individual endogenous stress response [4]. However, due to its unstable nature and rapid clearance from plasma, the measurement of AVP is rarely reproducible [5]. Copeptin, a glycosylated peptide consisting of 39 amino acids is derived from the precursor AVP and is more stable and easier to measure. Its level adequately represents the production of AVP. Thus, copeptin is a functional mirror of AVP concentration with high prognostic accuracy [5–7]. According to recent studies and meta-analyses, copeptin measurement (along with conventional cardiacTn assays) improves the early detection of AMI, enabling the identification of patients who can be safely discharged early from the ED [6, 8, 9].
Thus, the aim of this prospective observational study was to assess the combined value of copeptin and hs-TnI for early rule-out of AMI, especially NSTEMI (non-ST segment elevation myocardial infarction), in low to intermediate-risk patients with suspected ACS presenting with chest pain in the ED, within 6 h of the onset of symptoms. Another major objective was to compare the diagnostic efficacy of this combination with the current standard protocol followed in the ED which along with clinical assessment includes the estimation of triage biomarkers (TnI, CK MB, and BNP).
Material and Methods
Patients
Over a period of one year, a total of 148 patients, more than 18 years of age who presented to the ED of our hospital with chest pain in less than six hours with low to intermediate risk of MI were recruited for the study. They were subjected to the standard ED protocol for the management of chest pain, and did not have a definitive diagnosis on basis of ECG and cardiac enzymes. All patients included in the study gave their written informed consent.
Those patients with a definitive diagnosis of MI or those who required hospital admission become necessary due to any other reason/co-morbidity were excluded from the study. Diagnoses were adjudicated by consensus of cardiology and emergency consultants on basis of standard ED protocol and the fourth universal definition of MI (UDMI) [10].
ED Protocol/Standard Care
The standard protocol for the management of a patient presenting to our ED within 6 h of chest pain is routine clinical examinations, including ECG, blood pressure measurement, pulse oximetry monitoring, and triage biomarkers (TnI, CK MB, and BNP) at presentation, and then at 6–9 h after admission, according to the clinical situation.
Additional Tests As Per the Hypothesis
Additionally for all recruited patients hs-TnI and copeptin were measured at the time of presentation.
Diagnosis of MI
In the present study, the diagnosis of MI was based on the fourth UDMI, which defines that “myocardial injury is based on the elevation of cardiac Tn concentration, with at least one measurement exceeding the 99th percentile upper reference limit derived from a normal reference population. The myocardial injury is considered acute if there is a rise and/or fall of cardiac Tn values” [10].
Sampling and Laboratory Investigations
At the time of admission in ED two samples were drawn from each patient, one for the standard care process and the other for the study protocol. Standard care included estimation of TnI, CK-MB, and BNP, measured using the Cardio 3 Panel of Triage [11].
The study protocol included estimation of hs-TnI and copeptin, estimated by chemiluminescent microparticle immunoassay (CMIA) and time-resolved amplification of cryptate emission (TRACE) respectively, Fig. 1.
Fig. 1.
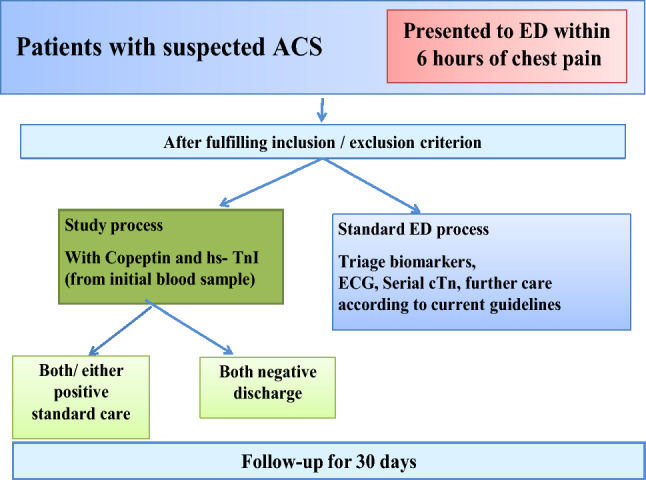
Study design
Follow Up
Patients were followed up for 30 days after first presentation in ED and were assessed for survival/AMI / sudden cardiac death, and all incidents recorded.
Data and Statistical Analysis
All data generated (standard protocol and study protocol) were tabulated and subjected to statistical analysis which was performed using the 20th version of SPSS (Chicago, IL, USA). Data was presented as mean, standard deviation (SD), and standard error of the mean (SEM). Student t-test was employed to compare the mean between two groups. During the evaluation of results, a p-value of < 0.05 was considered significant. ROC curve was used to compare the diagnostic performance of study tests. It was also used to determine the diagnostic cut-offs (for MI) of the study parameters with maximum sensitivity and specificity, along with positive predictive value (PPV) and negative predictive value (NPV).
Results
In a duration of one year, a total of 1796 patients presented with chest pain in the ED, and all of them were screened. Of them 148 patients fulfilled the inclusion criteria. The major reason for exclusion was the late presentation, more than 6 h from the chest pain onset. The demographic and other details are reported in Table 1. Mean age of patients was 59.4 years and 23.07% of them were women. Of these 148 patients, 52 (35.13.%) were admitted for further evaluation on basis of standard protocol, based on clinical examination and complete medical charts i.e. ECG, clinical notes, and all biomarker reports. After complete workup made after admission and requisite investigations (rise/fall of biomarkers, ECG changes, imaging evidence of new loss of viable myocardium, and/or new regional wall motion abnormality, only 32 (21.6.%) were finally diagnosed with AMI. This was in agreement with the data derived from study protocol which was on the basis of both hs-TnI and copeptin being higher than the cut-offs derived. Of the screened patients, the two groups were made (patients with MI and patients without MI),Table 1 depicts demographic details of all the patients included in the study. Table 2 shows that the mean hs-TnI and copeptin concentrations were higher in cases of MI in comparison to cases without MI and hs-TnI was found to be statistically significant. SEM = Standard Error of Mean. *p-value < 0.05 was considered as statistically significant.
Table 1.
Demographic details of the study population
| Patients’ characteristics | Patients with MI (n = 52) | Patients without MI (n = 96) |
|---|---|---|
| Age (Years) | 55.4 ± 15 | 62.4 ± 8.7 |
| Sex (Male/Female) | 32/20 | 29/67 |
| Smoking (Yes/No) | 38/14 | 67/29 |
| Exercise (Yes/No) | 37/15 | 58/28 |
| Alcohol consumption (Yes/No) | 30/22 | 59/37 |
| Hypertension (Yes/No) | 26/26 | 53/43 |
| On Antihypertensive drugs (Yes/No) | 19/33 | 17/79 |
| Platelet inhibitors (Yes/No) | 17/35 | 11/85 |
| Central Obesity (Yes/No) | 39/13 | 45/41 |
| Dyslipidemia (Yes/No) | 25/27 | 47/39 |
| On lipid lowering drugs (Yes/No) | 28/24 | 39/59 |
| Diabetes mellitus (Yes/No) | 29/23 | 37/61 |
| Past history of any CV event (Yes/No) | 27/25 | 18/78 |
| Family history of CVD (Yes/No) | 17/35 | 27/69 |
Table 2.
Mean level of study variables in study population
| Parameters | Patients with MI (n = 52) (mean ± SEM) |
Patients without MI (n = 96) ( mean ± SEM) |
p value |
|---|---|---|---|
| Copeptin (pmol/L) | 87 ± 37 | 12 ± 7.4 | 0.184 |
| hs-TnI ( pg/mL) | 498 ± 415 | 32 ± 17 | 0.01* |
| Triage Markers | |||
| TnI ( ng/mL) | 7.2 ± 0.62 | 2.5 ± 1.3 | 0.04* |
| CKMB (ng/mL) | 27.7 ± 7 | 5.5 ± 1 | 0.03* |
| BNP (pg/mL) | 1149 ± 470 | 227 ± 49.7 | 0.098 |
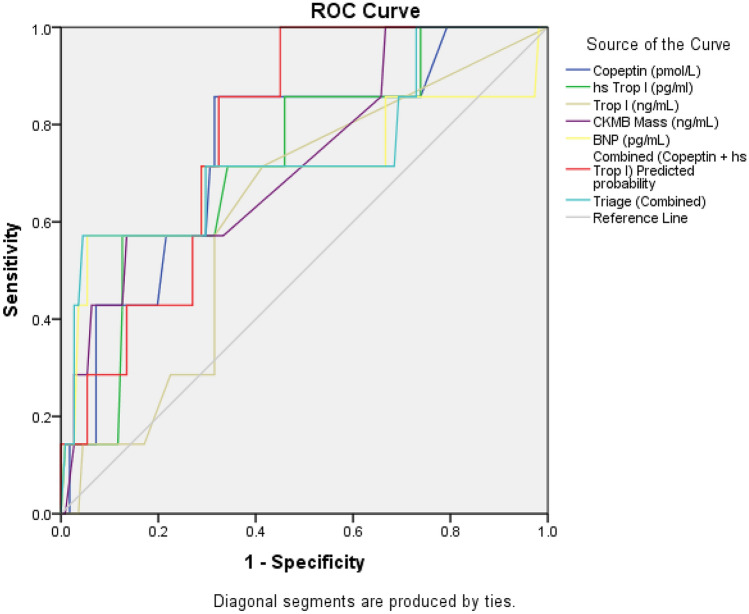
Overall diagnostic values were quantified by calculating the area under the receiver operating characteristic (ROC) curve as seen in Fig. 2. ROC curve was plotted for all the biochemical parameters individually and in appropriate combinations (TnI, CKMB, BNP, copeptin, hs-TnI, combined triage markers, and combination of copeptin and hs -TnI). Table 3 shows the ROC curve analysis of the same. A comparison between AUCs was performed. Optimal hs-TnI and copeptin thresholds were determined.
Fig. 2.
ROC curve of study variables
Table 3.
Characteristics of ROC curve of study variables
| Test Variable | Area Under Curve (AUC) | P Value | 95% Confidence Interval | |
|---|---|---|---|---|
| Lower Bound | Upper Bound | |||
| Combined Copeptin + hs-TnI | 0.89 | 0.012 | 0.658 | 0.907 |
| Copeptin | 0.750 | 0.043 | 0.567 | 0.932 |
| hs-TnI | 0.728 | 0.027 | 0.545 | 0.912 |
| TnI | 0.622 | 0.042 | 0.428 | 0.815 |
| CKMB | 0.730 | 0.041 | 0.534 | 0.926 |
| BNP | 0.707 | 0.067 | 0.441 | 0.972 |
| Triage (combined) | 0.713 | 0.052 | 0.515 | 0.943 |
On basis of AUC the cut off levels, sensitivity, specificity, PPV, and NPV of each study variable as well as the relevant combinations were calculated along with 95% confidence intervals, as shown in Table 4. The cut-offs derived for copeptin and hs-TnI were 17.8 pmol/L, 47.5 pg/mL, respectively. Combined Copeptin + hs-TnI had 100% sensitivity, 59% specificity 33% PPV and 99.8% NPV. After evaluating the performance characteristics of all the biomarkers in the study patients, it was found that combining copeptin with hs TnI resulted in an improved ROC AUC of 0.89 (95% CI, 0.658–0.907), with a significant difference compared with that of hs TnI alone (p = 0.012).
Table 4.
Cut off levels, Sensitivity, Specificity, Positive Predictive Value (PPV) and Negative Predictive Value (NPV) of various study variables
| Biomarkers | Cut off levels | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) |
|---|---|---|---|---|---|
| Copeptin (pmol/L) | 17.8* | 57 | 87.4 | 22 | 97 |
| hs-TnI (pg/mL) | 47.5* | 85.7 | 68.5 | 95.6 | 98.2 |
| Combined Copeptin & hs-TnI | Same as above* | 100 | 59 | 33 | 99.8 |
| Tn I | 0.015** | 71.4 | 58.6 | 28 | 89 |
| CKMB (IU/L) | 22.5** | 43 | 92 | 25 | 86 |
| BNP | 1245** | 57 | 95 | 10 | 88 |
| Triage (combined) | Same as above** | 67 | 49 | 46 | 62 |
* Copeptin + hsTropI - the combination being proposed
** the conventional triage in use
Combination of Biomarkers Hs-TnI and Copeptin for Early Exclusion of Acute MI
As evident from Table 4, a value of < 47.5 pg/mL for hs-TnI could be used for rapid exclusion of AMI with a sensitivity of 85.7%, specificity of 68.5%, PPV of 95.6%, and NPV of 98.2%. The corresponding values for the biomarker copeptin were 87.4%, 57.1%, 22.5%, and 97.1%, respectively at a cut-off of 17.8 pmol/L. An hs-TnI level of < 47.5 pg/mL in combination with a copeptin value of < 17.8 pmol/L at initial presentation excluded acute MI with a sensitivity of 100%, specificity of 59%, PPV of 33%, and NPV of 99.8%, indicating that this combination has an even higher diagnostic accuracy than that of either hs-TnI or copeptin alone.
Discussion
Chest pain is one of the most common complaints leading to ED visits and subsequent admission. The vast majority of these patients (approximately 87%) are ultimately found not to have ACS [12]. Therefore, identification of patients and their rapid rule-out at the presentation in ED, who are highly unlikely to have ACS, is of paramount importance. Not only medical but it has economic importance also as it will reduce the unnecessary utilization of healthcare facilities. After the first Tn measurement, there remains a diagnostic uncertainty which leads to a series of tests in ED, and the additional costs associated with it exceed cost spent in ED each year [13–15]. Recent advances in cardiac Tn assays to hs-Tn assays allow for sensitive detection of myocardial injury [16]. A shorter, 1 h or 3 h, protocol can be used with high sensitivity assays, but the biomarker release is substantially dependent on blood flow, due to significant variability in the time to peak value i.e. the time when a normal value may become greater than 99th percentile URL, which again leads to increase in length of stay in the ED and delay in ruling out of AMI [17, 18]. Thus the need of the hour is the expeditious evaluation of such patients with the help of a biomarker which is released early in the event of hemodynamic stress.
Arginine vasopressin (AVP), also known as antidiuretic hormone, is one of the key hormones of the hypothalamic–pituitary–adrenal (HPA) axis and is responsible for a variety of hemodynamic functions. Despite a theoretical diagnostic role in cardiovascular disease, its clinical application as an aid in diagnosis has been limited by its short half-life in circulation. Copeptin is the C-terminal part of pro-AVP and is released together with AVP during the processing of the precursor peptide from the neurohypophysis upon hemodynamic or osmotic stimuli [19]. Contrary to AVP, copeptin is stable both in serum and plasma at room temperature and can be easily measured as a 'shadow' fragment of AVP in the circulation. Also, the results are available within one hour, which makes the biomarker useful in the emergency department (ED). Khan et al. (2007), first reported, an increase in copeptin concentrations after AMI, with the highest values reported on day 1 and a subsequent decline over the next 2 to 5 days [20]. Keller et al. 2010, measured copeptin for rapid exclusion of AMI in patients presenting with suspected ACS and found it to be elevated (> 14 pmol/l) within 4 h of symptom onset, while levels of cardiac TnT (> 99th percentile of the upper reference range) were undetectable [5]. Hence, it was suggested by them that the addition of copeptin may be useful to rule out AMI in such patients. Bolignano et al., 2014, had a similar observation about the use of the additive value of copeptin in ruling out MI early, even before Tn has begun to rise [21].
In CHOPIN (copeptin helps in early detection of patients with MI), one of the largest multicenter studies on consecutive patients with chest pain also concluded that adding copeptin to cardiac TnI allowed safe rule out of AMI in patients presenting with suspected ACS. For the cardiac TnI values in the 99th percentile ( 40 ng/L) was used as cut off at a copeptin level of < 14 pmol/L. This combination has the potential to rule out AMI in 58% of patients without serial blood draws, which is logistically challenging and also a financial burden for already overcrowded EDs and hospitals [22].
Möckel et al., 2015, in a randomized-controlled trial showed the safety of early discharge using a single combination of copeptin with cardiac Tn (conventional and sensitive assay) at presentation. Notably, 68% of patients could be discharged by the combined use of copeptin and cardiac Tn versus 12% with cardiac Tn analysis alone [13].
Ideally, diagnosis of AMI with hs -TnI alone requires a delta check of two values, at least 2 to 3 h apart. In the course of MI, copeptin is secreted very early whereas Tn rises later. Thus, they are complementary biomarkers that, when used together, can help rule out MI with a single blood draw [23]. Hence, copeptin along with hs -TnI might assist with risk stratification, resource allocation, and rule out decisions [24]. In this prospective study, the significance of dual biomarker strategy that combines hs-TnI (cardiac necrosis biomarker) and copeptin (a biomarker for endogenous stress) was examined and its significance with the standard protocol was compared. To the best of our knowledge, this is the first study in the Indian population to assess the combination of hs-TnI and copeptin as a rule-out marker for AMI patients presenting with chest pain in the ED in less than 6 h. In the present study, it was observed that the sensitivity and the NPV of the combined biomarker was significantly better than the NPV of hs-TnI (Table 4). Using a combination of hs-TnI and copeptin no delta check is required and the diagnosis can be immediately confirmed. Our results suggest that based on the combination of hs-TnI and copeptin, AMI can be ruled with a sensitivity of 100% and a NPV of 99.8%. As per the recommendation of 4th UDMI, Cardiac Tn is required to be measured at presentation and after 6 –9 h, for the diagnosis of AMI. Hence this combination might obviate admission for almost 80% of the patients in the ED. Also, this dual biomarker strategy is significantly better than triage biomarkers currently used in ED along with clinical assessment. The results showed that continuous ECG monitoring and serial blood sampling done in all patients to rule out AMI as per the standard protocol could be limited to the patients positive for either hs-TnI (> 47.5 pg/mL) or copeptin (> 17.8 pmol/l), whereas these resources would not be required for patients negative for both markers.
Reichlin et al., 2009, was the first one who did a study on this concept. The initial observation of elevated copeptin levels in the vast majority of AMI patients led to design this first pilot study to test and confirm the hypothesis for the feasibility and safety of a dual-marker strategy (6, 20, 25).
Reichlin et. al., reported that the combination of two markers significantly increased the diagnostic accuracy provided by hs-TnT alone, with an AUC of 0.97 (p < 0.001) for the combination of hs-TnT and copeptin. Another group of co-workers had similar results for copeptin and they found that the combination of the copeptin and TnT concentration at admission showed an NPV of 92.4%. They also demonstrated that when STEMI diagnoses are excluded, an added benefit for the rapid rule-out of NSTEMI is seen only when the copeptin and hs-TnT concentrations were used at pre-specified cut-offs (Keller et al., 2010). Several diagnostic studies, randomized management trials and meta-analyses support the fact of dual marker strategy where at pre specified cut offs copeptin and hs-TnT improve in ruling out of NSTEMI [25–29]
The overall diagnostic performance of dual biomarker reflected by ROC analysis was higher than hs-TnI alone. The high NPV (99.8%) of this combination might enable NSTEMI to be ruled out in most of the patients with NSTEMI. Rapid and safe rule-out of low to intermediate-risk patients presenting to ED is important because approximately 80% of them do not have NSTEMI. Rapid discharge of these patients will decrease ED crowding and costs and improve the quality of care. ED crowding is related to an increased risk of in-hospital mortality and adverse cardiovascular outcomes. It results in a longer treatment time for patients with acute pain, and a greater probability of leaving the ED against medical advice or without being seen. Copeptin has also been recommended in the ESC 2015 guidelines in combination with either Tn or hs-Tn [30].
The dual biomarker strategy combining hs-TnI and copeptin benefits from the integration of complementary information provided by pathophysiologically different processes. It is important to note that despite extensive research with markers representing various pathophysiological pathways including inflammation, platelet activation, and ischemia, none of the markers previously assessed have been able to show any diagnostic benefit, alone or in combination with Tns. Therefore, further studies need to be done to evaluate the impact of a combined biomarker approach integrating copeptin in the initial evaluation of patients with chest pain in the actual ED setting.
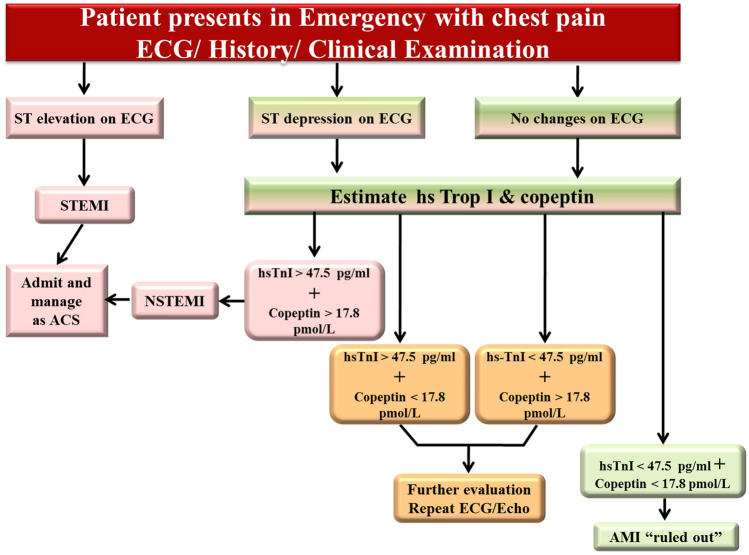
In summary, our results show that negative results to both copeptin and hs-TnI testing on admission could potentially allow safe and early rule-out of AMI without the need for further serial Tn testing. Also, the estimation of copeptin on ED admission added incremental value to initial hs-TnI in patients with chest pain presenting to the ED within 6 h of the onset of symptom. This combined biomarker approach resulted in high sensitivity and NPV for ruling out NSTEMI in patients with chest pain. Hence, the use of a combined biomarker approach with an estimation of copeptin and hs-TnI at presentation can support a safe discharge process in low to intermediate-risk patients presenting with suspected ACS. Therefore, copeptin is not able to replace cardiac Tn or hs-TnI but helps in earlier decision making. This strategy will help to optimize resource allocation and processes and also optimize the patients’ turnaround time in the ED while reducing the need of subsequent diagnostic tests. Faster diagnosis can increase patient well-being, since unnecessary patient stress, anxiety, and other risks associated with hospitalization can be avoided. Towards the above, an algorithm is suggested as given in Fig. 3, which could help in early ‘rule-in’ or ‘rule-out’ of AMI in a patient with acute chest pain.
Fig. 3.
Algorithm of management in emergency department of patient with chest pain
However, the concept of combined biomarker strategy, which can lead to improved rule out accuracy is an alluring prospect but studies on a larger number of patients are needed to evaluate the use of copeptin along with hs-TnI levels in NSTEMI patients in the ED. This will help in the improvement of patient care and to establish “ Is copeptin that biomarker, which perhaps can distinguish between the AMI and Non-AMI?
Limitations
This was a single-centre study, conducted on prospective patients admitted to ED of SGRH with acute chest pain. However, to confirm the results of this study, further interventional multicentric trials with more subjects are needed to ensure the effectiveness and patient benefit of the new strategy.
Conflicts
Conflicts of interest: All authors declare that they have no conflict of interest.
Ethics Approval: All procedures performed in studies were in accordance with the ethical standards of our institutional ethics committee; approved under number EC/02/16/961.
Informed Consent: All patients were included in the study after procuring their written informed consent.
Acknowledgements
We are grateful to Thermofischer Scientific and Abbott Diagnostics for supporting our study with the requisite reagents.
Authors Contributions:
In Study design, review of Literature and preparation of manuscript.
Funding
Funding: No funding was received for the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bassand JP, Hamm CW, Ardissino D, Boersma E, Budaj A, Fernández-Avilés F, et al. Task force for diagnosis and treatment of non-ST-segment elevation acute coronary syndromes of European society of cardiology. Guidelines for the diagnosis and treatment of non-ST-segment elevation acute coronary syndromes. Eur Heart J. 2007;28:1598–1660. doi: 10.1093/eurheartj/ehm161. [DOI] [PubMed] [Google Scholar]
- 2.Chen Y, Tao Y, Zhang L, Zhu W, Zhou X. Diagnostic and prognostic value of Biomarkers in acute Myocardial Infarction. BMJ 2019; 210–16. [DOI] [PubMed]
- 3.Reichlin T, Hochholzer W, Bassetti S, Steuer S, Stelzig C, Hartwiger S, et al. Early diagnosis of myocardial infarction with sensitive cardiac troponin assays. N Engl J Med. 2009;361(9):858–867. doi: 10.1056/NEJMoa0900428. [DOI] [PubMed] [Google Scholar]
- 4.Itoi K, Jiang YQ, Iwasaki Y, Watson SJ. Regulatory mechanisms of corticotropin-releasing hormone and vasopressin gene expression in the hypothalamus. J Neuroendocrinol. 2004;16:348–355. doi: 10.1111/j.0953-8194.2004.01172.x. [DOI] [PubMed] [Google Scholar]
- 5.Keller T, Tzikas S, Zeller T, Czyz E, Lillpopp L, Ojeda FM, et al. Copeptin improves early diagnosis of acute myocardial infarction. J Am Coll Cardiol. 2010;55:2096–2106. doi: 10.1016/j.jacc.2010.01.029. [DOI] [PubMed] [Google Scholar]
- 6.Reichlin T, Hochholzer W, Stelzig C, Laule K, Freidank H, Morgenthaler NG, et al. Incremental value of copeptin for rapid rule out of acute myocardial infarction. J Am Coll Cardiol. 2009;54:60–68. doi: 10.1016/j.jacc.2009.01.076. [DOI] [PubMed] [Google Scholar]
- 7.Balanescu S, Kopp P, Gaskill MB, Morgenthaler NG, Schindler C, Rutishauser J. Correlation of plasma copeptin and vasopressin concentrations in hypo, iso-, and hyperosmolar states. J Clin Endocrinol Metab. 2011;96:1046–1052. doi: 10.1210/jc.2010-2499. [DOI] [PubMed] [Google Scholar]
- 8.Lipinski MJ, Escárcega RO, D’Ascenzo F, Magalhães MA, Baker NC, Torguson R, et al. A systematic review and collaborative meta-analysis to determine the incremental value of copeptin for rapid rule-out of acute myocardial infarction. Am J Cardiol. 2014;113:1581–1591. doi: 10.1016/j.amjcard.2014.01.436. [DOI] [PubMed] [Google Scholar]
- 9.Raskovalova T, Twerenbold R, Collinson PO, Keller T, Bouvaist H, Folli C, et al. Diagnostic accuracy of combined cardiac troponin and copeptin assessment for early rule-out of myocardial infarction: a systematic review and meta-analysis. Eur Heart J Acute Cardiovasc Care. 2014;3:18–27. doi: 10.1177/2048872613514015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thygesen K, Alpert J S, Jaffe A S, Chaitman B R, Bax J J, Morrow D A, et al. and The Executive Group on behalf of the Joint European Society of Cardiology (ESC)/American College of Cardiology (ACC)/American Heart Association (AHA)/World Heart Federation (WHF) Task Force for the Universal Definition of Myocardial Infarction. Fourth Universal Definition of Myocardial Infarction. Eur Heart J. 2019;40 :237–69.
- 11.Galvani M, Ferrini D, Ghezzi F, Ottani F. Cardiac markers and risk stratification: an integrated approach. Clin Chim Acta. 2001;311:9–17. doi: 10.1016/S0009-8981(01)00552-6. [DOI] [PubMed] [Google Scholar]
- 12.Bhuiya FA, Pitts SR , Mc Caig LF. Emergency department visits for chest pain and abdominal pain: United States, 1999–2008. NCHS Data Brief 2010;1–8. [PubMed]
- 13.Möckel M, Searle J, Hamm C, Slagman A, Blankenberg S, Huber K, et al. Early discharge using single cardiac troponin and copeptin testing in patients with suspected acute coronary syndrome (ACS): a randomized, controlled clinical process study. Eur Heart J. 2015;36(6):369–376. doi: 10.1093/eurheartj/ehu178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wildi K, Zellweger C, Twerenbold R, Jaeger C, Reichlin T, Haaf P, et al. Incremental value of copeptin to highly sensitive cardiac Troponin I for rapid rule-out of myocardial infarction. Int J Cardiol. 2015;190:170–176. doi: 10.1016/j.ijcard.2015.04.133. [DOI] [PubMed] [Google Scholar]
- 15.Stallone F, Schoenenberger AW, Puelacher C, Gimenez MR, Walz B, Devasia AN, et al. Incremental value of copeptin in suspected acute myocardial infarction very early after symptom onset. Eur Heart J Acute Cardiovasc Care. 2016;5:407–415. doi: 10.1177/2048872616641289. [DOI] [PubMed] [Google Scholar]
- 16.Twerenbold R, Jaffe A, Reichlin T, Reiter M, Mueller C. High-sensitive troponin T measurements: what do we gain and what are the challenges? Eur Heart J. 2012;33(5):579–586. doi: 10.1093/eurheartj/ehr492. [DOI] [PubMed] [Google Scholar]
- 17.Thygesen K, Mair J, Giannitsis E, Mueller C, Lindahl B, Blankenberg S, et al. Study group on biomarkers in cardiology of ESC working group on acute cardiac care. How to use high sensitivity cardiac troponins in acute cardiac care. Eur Heart J. 2012;33:2252–2257. doi: 10.1093/eurheartj/ehs154. [DOI] [PubMed] [Google Scholar]
- 18.Mueller C, Giannitsis E, Möckel M, Huber K, Mair J, Plebani M, et al. And biomarker study group of the ESC acute cardiovascular care association. Rapid rule out of acute myocardial infarction: novel biomarker-based strategies. Eur Heart J Acute Cardiovasc Care. 2017;6(3):218–222. doi: 10.1177/2048872616653229. [DOI] [PubMed] [Google Scholar]
- 19.McCann CJ, Glover BM, Menown IB, Moore MJ, McEneny J, Owens CG, et al. Novel biomarkers in early diagnosis of acute myocardial infarction compared with cardiac troponinT. Eur Heart J. 2008;29:2843–2850. doi: 10.1093/eurheartj/ehn363. [DOI] [PubMed] [Google Scholar]
- 20.Khan SQ, Dhillon OS, O’Brien RJ, Struck J, Quinn PA, Morgenthaler NG, et al. C-terminal provasopressin (copeptin) as a novel and prognostic marker in acute myocardial infarction: Leicester Acute Myocardial Infarction Peptide (LAMP) study. Circulation. 2007;115:2103–2110. doi: 10.1161/CIRCULATIONAHA.106.685503. [DOI] [PubMed] [Google Scholar]
- 21.Bolignano D, Cabassi A, Fiaccadori E, Ghigo E, Pasquali R, Peracino A, et al. Copeptin (CTproAVP), a new tool for understanding the role of vasopressin in pathophysiology. Clin Chem Lab Med. 2014;52:1447–1456. doi: 10.1515/cclm-2014-0379. [DOI] [PubMed] [Google Scholar]
- 22.Maisel A, Mueller C, Neath SX, Christenson RH, Morgenthaler NG, McCord J, et al. Copeptin helps in the early detection of patients with acute myocardial infarction: primary results of the CHOPIN trial (Copeptin Helps in the early detection Of Patients with acute myocardial INfarction) J Am Coll Cardiol. 2013;62(2):150–160. doi: 10.1016/j.jacc.2013.04.011. [DOI] [PubMed] [Google Scholar]
- 23.Beri N, Daniels LB, Jaffe A, Mueller C, Anand I, Peacock WF, et al. Copeptin to rule out myocardial infarction in Blacks versus Caucasians. Eur Heart J Acute Cardiovasc Care. 2019;8(5):395–403. doi: 10.1177/2048872618772500. [DOI] [PubMed] [Google Scholar]
- 24.Morgenthaler NG, Struck J, Alonso C, Bergmann A. Assay for the measurement of copeptin, a stable peptide derived from the precursor of vasopressin. Clin Chem. 2006;52:112–119. doi: 10.1373/clinchem.2005.060038. [DOI] [PubMed] [Google Scholar]
- 25.Giannitsis E, Kehayova T, Vafaie M, Katus HA. Combined testing of high-sensitivity troponin T and copeptin on presentation at prespecified cutoffs improves rapid rule-out of non–ST-segment elevation myocardial infarction. Clin Chem. 2011;57:1452–1455. doi: 10.1373/clinchem.2010.161265. [DOI] [PubMed] [Google Scholar]
- 26.Giavarina D, Carta M, Fortunato A, Wratten ML, Hartmann O, Soffiati G. Copeptin and high sensitive troponin for a rapid rule out of acute myocardial infarction? Clin Lab. 2011;57(9–10):725–730. [PubMed] [Google Scholar]
- 27.Westwood M, van Asselt T, Ramaekers B, Whiting P, Thokala P, Joore M, et al. High-sensitivity troponin assays for the early rule-out or diagnosis of acute myocardial infarction in people with acute chest pain: a systematic review and cost-effectiveness analysis. Health Technol Assess. 2015;19(44):1–234. doi: 10.3310/hta19440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stallone F, Schoenenberger AW, Puelacher C, Rubini GM, Walz B, Naduvilekoot A, et al. Incremental value of copeptin in suspected acute myocardial infarction very early after symptom onset. Eur Heart J Acute Cardiovasc Care. 2016;5(5):407–415. doi: 10.1177/2048872616641289. [DOI] [PubMed] [Google Scholar]
- 29.Stengaard C, Sørensen JT, Ladefoged SA, Lassen JF, Rasmussen MB, Pedersen CK, et al. The potential of optimizing prehospital triage of patients with suspected acute myocardial infarction using high-sensitivity cardiac troponin T and copeptin. Biomarkers. 2017;22(3–4):351–360. doi: 10.1080/1354750X.2016.1265008. [DOI] [PubMed] [Google Scholar]
- 30.Hamm CW, Bassand JP, Agewall S, Bax J, Boersma E, Bueno H, et al. ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: the Task Force for the management of acute coronary syndromes (ACS) in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC) Eur Heart J. 2011;32:2999–3054. doi: 10.1093/eurheartj/ehr236. [DOI] [PubMed] [Google Scholar]