Abstract
Background
Immigrants in Western countries have been particularly affected by the COVID-19 crisis.
Objective
We analysed excess mortality rates among the foreign-born population and changes in their distinctive mortality profiles (“migrant mortality advantage”) during the first pandemic wave in France.
Data and methods
Deaths from all causes in metropolitan France from March 18 to May 19, 2020 were used, with information on sex, age, region of residence and country of birth. Similar data from 2016 through 2019 were used for comparisons.
Results
During the pre-pandemic period (2016–2019), immigrant populations (except those from Central and Eastern Europe) had lower standardized mortality rates than the native-born population, with a particularly large advantage for immigrants from sub-Saharan Africa. In the regions most affected by COVID-19 (Grand-Est and Île-de-France), the differences in excess mortality by country of birth were large, especially in the working-age groups (40–69 years), with rates 8 to 9 times higher for immigrants from sub-Saharan Africa, and about 3 to 4 times higher for immigrants from North Africa, from the Americas and from Asia and Oceania relative to the native-born population. The relative overall mortality risk for men born in sub-Saharan Africa compared to native-born men, which was 0.8 before the pandemic, shifted to 1.8 during the first wave (0.9 to 1.5 for women). It also shifted from 0.8 to 1.1 for men from North Africa (0.9 to 1.1 for women), 0.7 to 1.0 for men from the Americas (0.9 to 1.3 for women), and 0.7 to 1.2 for men from Asia and Oceania (0.9 to 1.3 for women).
Conclusion
Our findings shed light on the disproportionate impact of the first wave of the pandemic on the mortality of populations born outside Europe, with a specific burden of excess mortality within the working-age range, and a complete reversal of their mortality advantage.
Keywords: France, Foreign-born, Immigrants, COVID-19, Mortality, Excess mortality, Migrant mortality advantage, Inequalities
1. Introduction
The specific vulnerability of immigrant communities in the context of the COVID-19 crisis has been evidenced in a number of Western countries. In Europe, large mortality disparities by country of birth have been described for Sweden (Drefahl et al., 2020; Rostila et al., 2021), Denmark and Norway (Krasnik et al., 2020), Italy (Canevelli et al., 2020), Belgium (Vanthomme et al., 2021), and France (Papon and Robert-Bobée, 2020, 2021). An OECD report on the pandemic's impact on immigrants and their children emphasizes the role of social determinants via multiple, mutually compounding mechanisms: greater risk of exposure to the virus (from overcrowded housing conditions, concentration in unstable and non-teleworkable jobs, daily commuting in public transportation and difficulties for maintaining physical distance in the workplace), greater risk of developing severe forms of the disease from comorbidities such as diabetes and obesity, and barriers in access to health care (OECD, 2020).
While the empirical findings abound, little has been done to relate them to the theoretical framework that grounds research on migrants' mortality in demography and social epidemiology. Migrants, and in particular non-Western migrants, have a distinctive mortality profile influenced by strong selective factors, be it in-migration selection (‘healthy migrant effect’) or out-migration selection (‘unhealthy return migration’ or ‘salmon bias’). Two components of this framework are likely to be affected by the COVID-19 crisis: first, the central concept of a ‘migrant mortality advantage’ (MMA), potentially threatened by the burden of deaths from COVID-19; and, second, the ‘out-migration selection’ mechanism, suspended by the closure of international borders during the first wave of the pandemic. Immigrants' mortality patterns and their changes during the pandemic can be put into perspective in light of this framework.
The French context is particularly well suited for analysing of the impact of the COVID-19 pandemic on migrant communities along these lines. First, France has a long history of immigration dating back to the middle of the nineteenth century. In 2020, more than 10% of the population was born abroad (6.8 million out of a population of 67.3 million). Immigrant origins are diverse, with 48% born in Africa and 32% in Europe. The most represented countries of birth are Algeria (13%), Morocco (12%), Portugal (9%), Tunisia (5%), Italy (4%) and Spain (4%). Half of all immigrants originate from one of these countries (INSEE, 2022).
Second, France was one of the most hardly hit European countries during the first wave of the COVID-19 pandemic, with 27% increase in deaths compared with the same period in 2019 (Desrivierre and Fabre, 2020; Le Minez and Roux, 2021). The government response was commensurate with the health threat and has been rated as one of the most stringent by the Oxford COVID-19 Government Response Tracker (Hale et al., 2021). Measures aiming to protect the population, such as lockdowns, led to a polarization in exposure to infection, with some segments of the population significantly exposed, especially health care and frontline essential workers, and others less so – those at home, teleworking, or benefiting from temporary wage subsidies. Immigrants were disproportionately represented among the first group (Gosselin et al., 2021), and, according to the national institute of statistics (INSEE), deaths among the foreign-born population increased during the first wave by 48% compared with 2019, versus 22% among the native-born population (Papon and Robert-Bobée, 2020; INSEE, 2021).
Last, the early diffusion of the pandemic around a limited number of clusters led to an uneven spread of the disease during the first wave. The lockdown, however, was implemented over the entire territory, regardless of the local situation. The temporary interruption of international migration coupled with the heterogeneity of the pandemic's spread across the territory constitutes a sort of natural experiment, providing opportunities for informative contrasts across regions and subpopulations.
For all these reasons relating to both the population composition and the circumstances of the first wave, the study of the differential impact of the pandemic between migrant and native populations is likely to be of particular interest in France. Thus far, given the unavailability of causes of death by country of birth of decedents for 2020, the amplitude of the COVID-19 burden among migrants has only been assessed in terms of proportional increases in the total number of deaths (Papon and Robert-Bobée, 2020, 2021). The purposes of this study are to explore : (a) the excess rate of mortality related to COVID-19 in the different foreign-born groups in comparison with the native-born, and ; (b) the extent to which the COVID-19 pandemic has impacted pre-existing mortality differentials between the foreign-born and the native-born. Our focus is on the first wave of the pandemic, during which the country was not yet prepared and frontline essential workers were particularly exposed.
2. Analytical approach
The analysis was designed to explore several dimensions and sources of variation in mortality during the pandemic: age, sex, place of birth, and region of residence in France. Below age 70, there was little mortality increase in the native-born population, and the increase in the foreign-born populations started at age 40 (Papon and Robert-Bobée, 2020, 2021). We have therefore bracketed ages into two groups: 40–69 (which can be considered “premature mortality”) and 70 and over. Given the considerable spatial heterogeneity of virus circulation during the period of interest (Fouillet et al., 2020), the analysis was run at two levels, that of metropolitan France (“national level”), and that of the most affected regions (which include some eastern departments (“Grand Est”), and Paris and its adjacent departments (“Île de France”)).
Although there is an official WHO definition of COVID-19 deaths (WHO, 2020), counts of such deaths are subject to a large amount of uncertainty. To quantify the burden, we used excess mortality, defined as the difference between all-cause mortality during the pandemic and the all-cause mortality that would be expected during the same period based on trends in the recent past. Excess mortality has long been used to assess the impact of pandemics, and is considered the most objective indicator of the COVID-19 death toll (Karlinsky and Kobak, 2021; COVID-19 Excess Mortality Collaborators, 2022) and a reliable metric for comparing countries (Beaney et al., 2020). Additionally, excess mortality is particularly relevant for COVID-19, as it represents the net impact on mortality from direct and indirect effects of the pandemic and associated governmental restrictions and measures. We estimate the mortality burden from COVID-19 in terms of excess mortality rate rather than percent increase in death counts, as the former is related to pre-pandemic levels of mortality, that differ across subpopulations.
To assess the pandemic's impact on pre-existing mortality differences between the foreign- and native-born populations, we compared the difference in overall mortality between these two groups during the study period (March 18 to May 19, 2020) to the difference over the same period during the previous years (2016–2019). This comparison yielded information on the extent to which the migrant mortality advantage still held, disappeared or reversed as a result of the pandemic, separately for males and females.
Lastly, in order to explore the possible role of the interruption of return migration in explaining mortality increases among migrant groups, we investigated mortality patterns in the regions least affected by the pandemic. The rationale was that a very limited change could be interpreted as return migration dynamics during this short period of time having no impact, whereas a sizeable change could be interpreted as an indication of its role.
3. Methods
3.1. Mortality data
All deaths in metropolitan France (i.e., excluding overseas territories) during the first wave of the COVID-19 pandemic (March 18 to May 19, 2020) were covered, with information on sex, age, municipality of residence and country of birth. Provisional death data from death certificates are transmitted monthly by the National Institute of Statistics and Economic Studies (INSEE) to the Epidemiological Centre for Medical Causes of Death (CépiDc-Inserm), which matches the administrative and medical parts of the certificates. To evaluate the quality of the provisional dataset, counts of deaths by age, sex, municipality of residence and country of birth were then compared with the existing official finalized counts for 2016–2019. We found very little differences in death counts across geo-demographic cells between the sources, except for deaths of individuals born in Algeria, a country considered part of the French territory until its independence in 1962. The absence of a final dataset thus led us to exclude these individuals, who represent about 10,000 deaths per year.
3.2. Population data by country of birth
INSEE census data used for calculating the person-year denominators included in our mortality indicators and statistical modelling are derived from the Annual Census Surveys (Enquêtes Annuelles de Recensement), which is a rolling annual census designed to cover the entire population over a 5-year cycle. As the latest available data are for 2018, we extrapolated populations until 2020 using a model which best predicts the 2017 and 2018 populations. This led to the estimation of the populations for the years 2019 and 2020 using separate linear projections of the 2017–2018 populations for each crossed category of sex, age, country of birth and region of residence. In line with the data quality issue concerning Algerian-born population reported earlier (see above section), we excluded this population from our analysis (about 1,383,000 individuals per year).
3.3. Country of birth classification
Countries of birth were grouped into seven broad regions: Northern and Western Europe, Central and Eastern Europe (including all Balkans countries, except Greece), Southern Europe, North Africa (excluding Algeria), sub-Saharan Africa, Asia and Oceania, and the Americas. The France-born population (native-born) was taken as the reference group in statistical models.
3.4. French administrative regions grouping by degree of intensity of the COVID-19 first-wave
The 13 administrative regions of metropolitan France were grouped by intensity of the first COVID-19 wave (weeks 12–20), based on the Eurosurveillance report (Fouillet et al., 2020) which combines incidence, hospitalization and mortality. Following this classification, the regions of Île-de-France and Grand-Est were grouped as the most affected, Auvergne-Rhône-Alpes, Hauts-de-France and Bourgogne-Franche-Comté as intermediately affected, and the remaining regions as least affected.
3.5. Mortality indicators
To account for the different age compositions of the subpopulations, annual direct standardized mortality rates for ages 40 and over were calculated from 2016 to 2019 for each country-of-birth group. The figures provided background knowledge and were compared to update the MMA patterns. Direct standardization was used, applying as reference the age-specific population counts of the European Standard Population of 2013 (Eurostat, 2013) to the observed age-specific death rates.
To assess the sudden rise of mortality during the first wave relative to comparable periods in previous years, standardized mortality rates were also calculated for weeks 12–20 from 2016 to 2020. For annual indicators, the population denominators were the average of the population on January 1st of a given year and on January 1st of the following year. Then, the annual and the subannual indicators were compared in order to check whether the period was representative of the general mortality in terms of level and temporal stability and whether it preserved the MMA hierarchy. In order to allow comparability with annual indicators, the infra-annual (9-week) denominators considered were the annual denominators multiplied by the proportion of exposure time in 1 year (9 × 7/365.25 days). Those denominators were therefore expressed in person-years, and 95% confidence intervals were estimated. For the two age groups (40–69 and 70+), death counts and standardized mortality rates during weeks 12–20 were estimated for 2020 and for the 2016–2019 period. Differences in standardized rates between 2020 and the 2016–2019 period were also calculated. The variance of this difference of standardized rates was estimated as the sum of the two variances (independence hypothesis). All results were stratified by sex and country-of-birth group.
3.6. Modelling excess mortality
To estimate excess mortality in 2020 by sex, age and country of birth during the first COVID-19 wave (weeks 12–20), overdispersed Poisson models of death counts from year 2016 to year 2020 with log-link function were built, with population denominators as offsets. In all these models, we introduced : (a) a linear annual mortality trend effect to adjust for mortality time course ; (b) a categorical country-of-birth effect to adjust the average MMA, and ; (c) an interaction term between a dummy variable taking value 1 for year 2020 and the country of birth, to estimate the mortality excess in 2020 relative to expected mortality in 2020 in the absence of pandemic by country of birth.
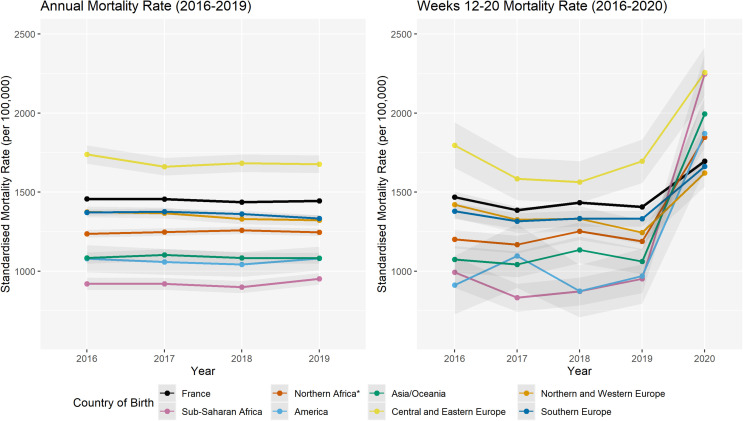
Other models were also tested separately to consider a quadratic mortality trend and a specific mortality trend by country of birth, but they led to little gain in explained deviance and to non-significant differences compared with the native-born population's mortality trend. Finally, the common mortality linear trend was selected for being the most parsimonious model while at the same time for smoothing the potentially artefactual variations or the variations resulting from the timing and strength of the seasonal flu (see Fig. 1 ).
Fig. 1.
Age and sex-standardized overall mortality rates at ages 40 years and over. Calendar years 2016–2019 (left) and weeks 12–20 of years 2016–2020 (right), by country-of-birth group. France (all regions).
All models were adjusted for age (5-year groups), stratified by age group (40–69 and 70+), by sex and by French regions grouped by intensity of the first wave of COVID-19:
where was the observed number of deaths, was the population denominator taken as offset, i the age and sex group, j the country-of-birth group, k the year from 2016 to 2020, measured the temporal mortality trend, adjusted on mortality by country of birth (taking native-born as the reference group), while the interaction effects estimated the excess mortality in 2020 in immigrant groups against the excess mortality in the native-born populations.
3.7. Estimating excess mortality
For excess mortality, the difference between the observed mortality level during weeks 12–20 in 2020 and the mortality level which would be expected during the same period, had the COVID-19 outbreak not occurred, were first calculated for each country of birth. Secondly, we calculated the ratio of the excess mortality among immigrants to the excess mortality among natives for each group of countries of birth. Using results from our model, we then estimated the mortality rate in 2020 and the expected mortality rate without the COVID-19 outbreak for each 5-year age group, sex and country-of-birth group with the following equations:
Then, the standardized mortality rates were calculated as follows:
where the subscript a could be either working-age, older adults or the whole population, and W the population weight in the reference population.
Finally, the excess mortality indicator for age-sex i and country of birth j was calculated as the ratio of the difference between the standardized rate and the standardized expected rate against the excess mortality estimated identically for the native population:
The delta-method (Oehlert, 1992) was used to approximate the variances used to test the significance.
3.8. Relative risk by country of birth before and during the pandemic
To compare the average of the overall (all-cause) mortality differentials between the foreign and the native-born populations (aged 40 and over) during the years preceding the pandemic and in 2020, the following Poisson models were regressed separately for 2016–2019 and 2020:
The reported measure for region of birth group j was then the relative overall risk of mortality .
4. Results
Hereafter, France refers to metropolitan France and the terms foreign-born and immigrants are used interchangeably. Death counts and person-years denominators in the study period (weeks 12–20, 2020) and on the average in the same period for years 2016–2019 are provided in the Appendix (Table 1 ).
The standardized mortality rate (ages 40+) of the French-born population for years 2016–2019 averaged 1450 deaths per 100,000 person-years (Fig. 1, left). The foreign-born groups experienced lower levels consistently throughout this period, except immigrants from Central and Eastern Europe, whose rate was about 10–15% higher. The group from sub-Saharan Africa had the lowest mortality levels of all (about 35% lower than the native-born), followed by the groups from Asia and Oceania and the Americas (−25%), North Africa (less than −15%), and finally the three groups from Europe (less than −5%). In all groups, a higher level of excess mortality was observed among men than among women, and the gender gap was particularly large among those born in Central and Eastern Europe, with a male-to-female ratio exceeding 6.
During the short period of the first wave of the pandemic (Fig. 1, right), mortality spiked in all groups, but to a much greater extent for non-European born populations. The relative increase ranged from an average of +10–15% for French-born and European-born populations to as high as +250% for the group from sub-Saharan Africa.
The statistical modelling of the excess mortality in the first wave reveals a definite age pattern across country-of-birth groups (Table 1), with sharper rises among migrants relative to native-born in the populations aged 40–69 versus 70 and over. The differences between men and women, visible within both age groups, did not reach significance. A much greater ratio of excess mortality was visible for non-European-born than for European-born groups of migrants, irrespective of sex and age. At working ages, the ratios were particularly large in the group from sub-Saharan Africa (ratio of 16 in women, 19 in men), and lower but still very large in the other non-European groups, ranging around 6 to 8 in the group from the Americas and in the group from Asia and Oceania and around 4 in the group from North Africa.
Table 1.
Age-standardized excess mortality during weeks 12–20, 2020, and migrant vs. native-born mortality ratiosa by sex and country-of-birth group, for ages 40–69 and 70 and over. France (all regions).
| Sex |
Country-of-birth group |
Ages 40-69 |
Ages 70 and over |
||
|---|---|---|---|---|---|
| Age-standardized excess mortality rate (per 100,000) |
Ratio | Age-standardized excess mortality rate (per 100,000) |
Ratio | ||
| Women | France (ref) | 25 | 1.00 | 782 | 1.00 |
| North Africa | 106 | 4.24* | 1424 | 1.82** | |
| Sub-Saharan Africa | 404 | 16.16*** | 1740 | 2.23* | |
| The Americas | 160 | 6.40 | 2487 | 3.18* | |
| Asia & Oceania | 145 | 5.80** | 2269 | 2.90*** | |
| Central & Eastern Europe | 47 | 1.88 | 2125 | 2.72 | |
| Northern & Western Europe | 33 | 1.32 | 800 | 1.02 | |
| Southern Europe | 52 | 2.08 | 1010 | 1.29 | |
| Men | France (ref) | 51 | 1.00 | 1340 | 1.00 |
| North Africa | 196 | 3.84*** | 2719 | 2.03*** | |
| Sub-Saharan Africa | 960 | 18.82** | 5908 | 4.41*** | |
| The Americas | 353 | 6.92* | 2683 | 2.00 | |
| Asia & Oceania | 428 | 8.39*** | 3400 | 2.54* | |
| Central & Eastern Europe | 286 | 5.61 | 1834 | 1.37 | |
| Northern & Western Europe | 63 | 1.47 | 1167 | 0.87 | |
| Southern Europe | 75 | 1.47 | 1380 | 1.03 | |
*: p < 0.05; **: p < 0.01; ***: p < 0.001.
Estimates based on Poisson regression model. See text for details.
Part of the differences by birth group is attributable to place-of-residence effects, as there is a concentration of foreign-born in the Île-de-France region, which belonged to the most hard hit group. At ages 40 and over, 23% of the native-born population resides in the most affected regions, as opposed to 43% of the foreign-born population as a whole, and as high as 57% of immigrants from sub-Saharan Africa (see Table 1 in the Appendix). Focusing on this specific group of the most affected regions, we find narrower differences across regions of birth (Table 2 ). Almost none of the ratios for the European groups were significant in this stratified analysis, while those for the non-European birth groups, although much reduced, remained large and retained significance. In the working-age population, the excess mortality ratios were around 8–9 for the group from sub-Saharan Africa, and around 3–4 for the groups from North Africa, Asia and Oceania and America, while most estimates for the non-European older adults were quite lower (<2). In the least affected regions, the mortality levels in 2020 remained aligned with the yearly fluctuations observed during the pre-pandemic period, which suggests that the interruption of migration had little role in the disproportionate increase found for the foreign-born in the most affected regions (see Graph 1 in the Appendix).
Table 2.
Age-standardized excess mortality during weeks 12–20, 2020, and migrant vs. native-born mortality ratiosa by sex and country-of-birth group, for ages 40–69 and 70 and over. Most affected regions in France (Île-de-France and Grand-Est).
| Sex |
Country-of-birth group |
Ages 40-69 |
Ages 70 and over |
||
|---|---|---|---|---|---|
| Age-standardized excess mortality rate (per 100,000) |
Ratio | Age-standardized excess mortality rates (per 100,000) |
Ratio | ||
| Women | France (ref) | 70 | 1.00 | 2314 | 1.00 |
| North Africa | 228 | 3.26* | 3298 | 1.43* | |
| Sub-Saharan Africa | 634 | 9.06*** | 3552 | 1.54 | |
| The Americas | 242 | 3.46 | 4450 | 1.92 | |
| Asia & Oceania | 217 | 3.10* | 4359 | 1.88*** | |
| Central & Eastern Europe | 187 | 2.67 | 3211 | 1.39 | |
| Northern & Western Europe | 75 | 1.07 | 2081 | 0.90 | |
| Southern Europe | 179 | 2.56* | 2410 | 1.04 | |
| Men | France (ref) | 196 | 1.00 | 3888 | 1.00 |
| North Africa | 493 | 2.52*** | 6186 | 1.59*** | |
| Sub-Saharan Africa | 1519 | 7.75*** | 10,085 | 2.59*** | |
| The Americas | 721 | 3.68** | 7226 | 1.86 | |
| Asia & Oceania | 592 | 3.02*** | 5472 | 1.41* | |
| Central & Eastern Europe | 492 | 2.51 | 3536 | 0.91 | |
| Northern & Western Europe | 67 | 0.34 | 4876 | 1.25 | |
| Southern Europe | 191 | 0.97 | 2791 | 0.72** | |
*: p < 0.05; **: p < 0.01; ***: p < 0.001.
Estimates based on Poisson regression model. See text for details.
Table 3 presents overall mortality differentials between the foreign and native-born populations at ages 40 and over, with age-adjustment within the broad age groups. During weeks 12–20 of years 2016–2019, there was a difference in favour of foreign-born groups (except for men and women from Central and Eastern Europe and for women from Northern and Western Europe), with relative risks ranging from 0.68 (p < 0.05) for American-born men to 0.97 (p < 0.05) for Southern European-born women, and a stronger advantage for non-European-born populations. In 2020, there was a loss of this advantage for all foreign-born groups, in both the working-age and older-adult populations. Moreover, there was a reversal of the mortality for men and women from sub-Saharan Africa (0.8 to 1.8 and 0.9 to 1.5), Asia and Oceania (0.7 to 1.2 and 0.9 to 1.3), and North Africa (0.8 to 1.1 (NS) and 0.9 to 1.1).
Table 3.
Relative risks of mortalitya in migrants relative to native-born. Ages 40 years and over, weeks 12–20 of 2016–2019 and of 2020. France (all regions).
| Country-of-birth group | Men | Women | ||
|---|---|---|---|---|
| 2016–2019 | 2020 | 2016–2019 | 2020 | |
| France (ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| North Africa | 0.79* | 1.05 | 0.92* | 1.12* |
| Sub-Saharan Africa | 0.75* | 1.81* | 0.88* | 1.5* |
| The Americas | 0.68* | 1.02 | 0.70* | 1.15 |
| Asia & Oceania | 0.70* | 1.17* | 0.85* | 1.26* |
| Central & Eastern Europe | 1.18* | 1.31* | 1.20* | 1.46* |
| Northern & Western Europe | 0.87* | 0.89 | 1.04 | 1.05 |
| Southern Europe | 0.95* | 0.97 | 0.97* | 1.04 |
*: p < 0.05; **: p < 0.01; ***: p < 0.001.
Estimates based on Poisson regression model. See text for details.
5. Discussion
In France, as in other Western countries, migrants have experienced a disproportionate impact of the COVID-19 pandemic, particularly during the first wave (Papon and Robert-Bobée, 2021). Over and above the relative mortality increase, we provide estimates of the excess mortality rate, which is more relevant as a measure of the COVID-19 burden when comparing groups whose pre-pandemic levels are very different. Based on this indicator and considering the uneven geographical spread of the pandemic in France, we shed new light on the considerable mortality burden for non-Western migrants and particularly those from sub-Saharan and North Africa, and on their distinctive vulnerability at working ages. Considering temporal trends, we examine the consequences of the mortality crisis on the distinctive foreign-born mortality profiles, with a reversal of what is called the “migrant mortality advantage”.
5.1. Immigrant versus native-born mortality levels before the pandemic
Looking at standardized mortality rates from all causes we found that, during the 4 years preceding the pandemic, the mortality levels of migrant groups were lower than that of the native-born. The only exception was for the group originating from Central and Eastern Europe, whose level was consistently higher throughout the pre-pandemic years. The migrant mortality advantage is a classic feature of migrants’ mortality throughout the world, and it has been shown to vary by age in a U-shape pattern (Guillot et al., 2018). In many countries, migrants only experience excess mortality at young ages, and their advantage, very large at adult ages, tapers progressively, as mortality tends to converge at older ages with that of natives. This variation, which is very consistent across countries, seems to be best explained by in-migration selection effects, coupled with progressive deterioration over the life course in the host country (Wallace et al., 2019).
The findings for Eastern Europeans are consistent with those of two previous studies on immigrant mortality in France, covering respectively the mid-1970s (Brahimi, 1980) and the mid-2000s (Boulogne et al., 2012). In both studies, migrants from Eastern Europe were the only group at a disadvantage. In the earlier study (Brahimi, 1980), Polish men had an excess mortality from respiratory diseases, related to their occupational history as workers in coal mines, and from liver cirrhosis, related to their higher level of alcohol use compared to natives. In the later study, Eastern European migrants were shown to have higher mortality than the native-born, particularly from diabetes, cardiovascular and cerebrovascular diseases, and from infectious diseases (Boulogne et al., 2012).
5.2. Excess mortality burden during the first wave of the COVID-19 pandemic
During the first wave, the pandemic had such a disproportionate impact on migrants that it led to a crossing of the curves of the native-born for groups from sub-Saharan Africa, Asia and Oceania, the Americas and North Africa. There was a strong gender pattern, with greater levels of excess mortality for males, as observed in many contexts (Pison and Meslé, 2022). Our analysis of the excess mortality uncovered considerable differentials in the working age range, with particularly heavy burdens for non-Western migrants.
The highest ratio estimates relative to the native-born were for those born in sub-Saharan Africa (about 16 in females, 19 in males), and the figures were around 4 for North Africa and around 6 to 8 for the Americas and Asia and Oceania. Lower estimates were found at ages 70 years and over, still ranging around 2 to 4. The groups from Europe had elevated estimates, but much less so, and not reaching significance. Restricting the analysis to the most affected regions (Île-de-France and Grand-Est) led to a substantial decline of the ratios, particularly for those born in sub-Saharan Africa. However, the figures remained in the very high range of 8–9 for the latter group, with migrants from North Africa, from the Americas and from Asia and Oceania also still having significant excess mortality, to a greater extent in the active age range (around 3), than at older ages (around 1.5).
The contribution of population density to those large differences has to be considered, as the virus is expected to spread faster in dense areas with more contacts among residents. At the national level, the relative increase in deaths during the period March 2-April 19, 2020 was greatest in the most densely populated municipalities (+49%, in comparison with +26% for the country) (Gascard et al., 2020). This is relevant to our findings, as 35% of the persons born in France reside in the most densely populated municipalities, as opposed to 65% of those born in North Africa, and more than 70% of those born in sub-Saharan Africa or Asia. At the regional level, the Île-de-France has by far the greatest density and has also the larger share of foreign-born population. Within the very dense municipalities, significant disparities were found according to birthplace, with deaths increasing by 39% compared to 2019 for those born in France, by 76% for those born in North Africa and by 158% for those born in sub-Saharan Africa. The figures were respectively 95%, 191% and 368% in Seine-Saint-Denis, the départment (territorial collectivity) of Île-de-France with the greatest proportion of foreign-born (Papon and Robert-Bobée, 2021). All in all, the large mortality excess observed for populations born in Africa in those early stages of the pandemic may be related to a compounding of the effects of density and of residence in seeding regions of the epidemic, in addition to other factors (see below).
The levels of burden are difficult to relate precisely to findings from other countries, where neither the epidemic and lockdown contexts, nor the birthplace groupings were similar, but rough comparisons can be made. For the neighbouring country of Belgium, estimates of the all-cause mortality differences between 2020 and 2019 were provided (Vanthomme et al., 2021), and, dividing the excess mortality in the different groups by the excess mortality among those born in Belgium, we find for males from sub-Saharan Africa aged between 40 and 64 years about the same ratio as in our study (i.e. around 19). Smaller gaps were reported in Sweden, as the hazard ratios for mortality from COVID-19 ranged around 2 to 3 for migrants from low- and middle-income countries of the Middle East and North Africa, and around 1.5 to 2 for those from other low- and middle-income countries, as compared to the populations born in Sweden (Drefahl et al., 2020).
5.3. Age pattern of excess mortality and roles of occupational factors and living conditions
In our study, a striking feature of the mortality impact on migrant groups was the disproportionate toll paid by non-Western migrants at middle ages, compared with the native-born for whom the burden was concentrated at older ages. Earlier ages at death translate into more years of life lost and to dramatic consequences on close family members, particularly children. Given their occupational profiles in essential sectors (Gosselin et al., 2021), migrants in these groups were frequently unable to work remotely during the pandemic, had jobs that often exposed them to infection without providing adequate protection, and relied on public transportation for commuting (Gosselin et al., 2022). Moreover, they tended to live in crowded households and neighbourhoods as pointed out above, all factors that increase the risk of infection. In France in November 2020, as many as 15.4% of immigrants from Africa and 14.6% of their descendants had developed antibodies against the SARS-CoV-2 virus, as opposed to 5.2% of the native-born (Warszawski et al., 2020).
Additionally, migrants of all ages may have faced barriers in access to coronavirus tests and treatment in hospitals, leading to worse prognosis once infected, and the issue was likely compounded by their higher prevalence of comorbidities. The coexistence of comorbidites with the mortality advantage is a complex phenomenon which has been observed in studies of gender and health, as there is a similar male-female health-survival paradox, with women experiencing more medical conditions and disability, while living longer than men (Oksuzyan et al., 2008). Regarding the spread and impact of the pandemic, the joint influence of socioeconomic, sociodemographic and cultural factors on COVID-19 risks has been theorized through the concept of syndemic pandemic, which exacerbates existing inequalities in health and exposures within populations (Marmot and Allen, 2020; Bambra et al., 2020). The substantial mortality disadvantage for migrants, which we have highlighted here, illustrates this phenomenon.
5.4. Reversal of differential overall mortality
Our statistical analyses uncover a complete reversal of the differential mortality for most of the migrant groups, as a consequence of their much greater excess mortality. We provide evidence for a reversal of the mortality advantage for migrants from sub-Saharan Africa (from 0.80* to 1.7*), North Africa (from 0.84* to 1.08*) and Asia and Oceania (from 0.76* to 1.21*). The same phenomenon was reported in Belgium (Vanthomme et al., 2021). However, in that case, the crossing of the curves was only apparent for those from sub-Saharan Africa, standing out as the only migrant group with significantly higher mortality than native Belgians during the first wave. Additionally, in the age range of 40–64 years, their mortality rate ratios of 1.79 [1.34–2.38] for men and 1.85 [1.29–2.65] for women were almost entirely explained by socioeconomic and sociodemographic characteristics. Unlike in our study, migrants from North Africa in Belgium remained at an advantage during the crisis, with mortality rate ratios of 0.66 [0.49–0.88] for men and of 0.62 [0.42–0.94] for females, which the authors attributed to their language proficiency that allowed them to follow recommended prevention measures.
Such a rapid shift in differential mortality has been reported in other contexts. In the United States, one study found that the Hispanic advantage for general mortality narrowed but persisted during the pandemic (Saenz and Garcia, 2021). This finding has been questioned recently by authors using a different estimation approach, yielding age-and-place adjusted COVID-19 death rates on a national level that were 80% higher for Blacks and more than 50% higher for Hispanics, relative to Whites, with almost no difference for Asians (Goldstein and Atherwood, 2020). The role played by exposure at work, in transportation and at home, and that of barriers to health care were pinpointed in the latter study, as they have in the French context (Brun and Simon, 2020; Cognet, 2021).
5.5. Risk of infectious diseases among migrants in different contexts
The disproportionate COVID-19 burden in migrants can be understood as an amplification of a more general pattern of vulnerability to infectious diseases. In the French study by Boulogne et al. (2012), the two groups born in Africa had respectively a twofold and more than threefold higher mortality from these diseases relative to the native-born, explained in large part by their six-to nine-fold greater mortality due to AIDS. In non-epidemic times, as infectious diseases represent a small fraction of the total burden of disease, this excess risk does not compromise the migrants mortality advantage.
It has long been considered that the infectious risk of migrants was related to ‘imported’ diseases requiring strict control by official authorities. AIDS in particular is often considered as having been acquired by Africans in their country of origin, prior to migration. And yet, Desgrées-du-Loû et al. (2015) have demonstrated high levels of HIV acquisition after migration among African migrants in France, questioning the widespread view of HIV as a mainly imported epidemic. Although AIDS and COVID-19 have completely different modes of transmission, the COVID-19 burden in migrants provides further support for the hypothesis of a specific vulnerability of migrants to infectious diseases post-migration, in large part attributable to their material disadvantage and to their working and living conditions. Paradoxically, this vulnerability coexists with their relative protection from Western chronic diseases, which in itself is the main explanation for the migrant mortality advantage.
Examining the pandemic situation in the regions of origin adds further insights. Although reliable statistics are lacking, it is generally agreed that apart from South Africa, the pandemic has had a later onset and slower spread and that the disease has been less severe and lethal in countries of sub-Saharan Africa than in other continents (Bamgboye et al., 2021). For instance, in the Democratic Republic of the Congo, a much higher prevalence of SARS-CoV-2 than the number of COVID-19 cases was reported (Nkuba et al., 2022). The authors interpreted this gap as a reflection of the youthfulness of the population resulting in greater numbers of asymptomatic cases, and possibly of protection resulting from past exposure to similar coronaviruses conferring relative immunity in the continent. Under the latter hypothesis, migrants might lose this type of protection over time in a different environment abroad. This scenario is a promising research avenue to investigate.
5.6. Exploring the hypothetical excess mortality in migrants from suspension of return migration
Taking into account both the geographical heterogeneity of diffusion of the pandemic's spread and the lockdown circumstances allowed us to better characterize patterns of excess mortality for migrants. In the early stage of the pandemic, there was a concentration of the disease around the main seeding centers of the virus in the population, i.e. the Île-de-France and Grand-Est regions. At the other extreme, there was a group of regions which were hardly affected. We expected the forced immobilization of migrants imposed by the lockdown to be largely responsible for any excess mortality among them in the regions with the lowest disease incidence.
Our analysis does not provide evidence for any significantly increased mortality during the lockdown for the different foreign-born groups in those parts of the country. We may therefore consider that the interruption of return migration, and particularly of ‘unhealthy remigration’ have not resulted in either visible or significant excess mortality. This implies that the disproportionate mortality increases for immigrants that we observe in the most affected regions are real and not the product of a bias arising from the sudden disruption of their usual mobility patterns. The manifestation of the ‘salmon bias’, especially if its amplitude is very limited, may need a longer period, as the migrants with severe disease and unable to return would not have died within this limited time, but later. There could still be a bias operating from returns prior to the lockdown, and this check was useful in that it allowed us to verify that the excess mortality of migrants in the most affected regions could legitimately be attributed to the pandemic.
5.7. Limitations
One limitation of this study is the absence of reliable individual socioeconomic measure to be adjusted for in the analysis. On death certificates, the information on occupation is indicated post-mortem by the family or health professionals, and therefore often missing or unreliable (Rey et al., 2013). Yet, the socio-economic dimension is paramount for explaining migrants’ vulnerability to infection, and should therefore be incorporated in future studies, possibly through area deprivation indices. These inequalities are important for understanding preventive measures and health care information accessibility, in particular for publics facing language barriers. The influence of social deprivation at the area level on the risk of infection was documented in a previous publication (Vandentorren et al., 2022).
Due to country's colonial past, INSEE defines an immigrant as a person born abroad with a foreign nationality at birth. In our study, immigrant groups comprise French nationals born abroad, whose mortality patterns may be close to those of French nationals born in France (Kerjosse and Lé, 2020). This is mainly relevant to Algeria, whose ‘repatriates’ left in the early 1960s, but this country of birth which provisional death data are not reliable was not included in order to obtain comparable population estimates over time.
The annual population data we used were smoothed estimates produced annually by INSEE from census data and obtained from a 5-year wave. The 2-year trend model of 2017 and 2018 used for projection also resulted in smoothed population counts for 2019 and 2020. The model also includes a common temporal mortality trend for all countries of birth and the native-born population, producing smoothed expected mortality estimates for 2020 as summaries of the past trend.
We also expect immigrant populations for certain countries of birth to be underestimated due to illegal immigration. This could result in numerator-denominator bias, as the deaths of illegal immigrants would be part of the numerator, not of the denominator. To assess the potential impact of this type of bias, we ran a sensitivity analysis with a foreign-born population increased by 20%, and found that both the strength of the associations and the significance held. Additionally, it has to be pointed out that the relative risks used to estimate the excess mortality rates were large and significant (results not shown).
5.8. Policy and research implications
We provide evidence for considerable inequalities, which raise pressing questions for both health researchers and public health policy makers. Our comprehensive approach to the analysis of migrants’ mortality profiles has provided strong estimates of mortality in relation with the COVID-19 pandemic, shedding light on the considerable burden carried by non-Western migrant communities in France and their specific vulnerability at adult ages in the context of this crisis. Those inequalities call for action in a context of concern over future pandemic threats. In Scandinavian countries, it has been contended that action targeting migrant groups was taken only in reaction to media alerting to the danger for public health constituted by an excess burden in migrants (Krasnik et al., 2020). This was very late, and it should be emphasized that early action is needed at different levels to protect migrant communities.
Further work should include cause-of-death data to estimate the potential role of comorbidities. This should also allow one to measure the indirect impact of the pandemic and lockdown context on mortality by diseases which must be expected to increase due to the congestion of health care facilities (e.g. a disease with a poor prognosis in the absence of medical treatment) and reduced reactivity (e.g. an acute health event).
Several implications may be inferred. First, structural barriers need to be addressed, as migrants’ material living and working conditions favour disease transmission and complicate the application of appropriate measures. Second, it has to be recognized that issues of access to health care may be compounded by discrimination in the health care system, which has to be brought into the open and tackled (Melchior et al., 2021). Lastly, communication barriers have to be mitigated by crafting messages and recommendations that are culturally appropriate, adapted to the public, and delivered through appropriate information channels.
In terms of research, there are concerns regarding the sequelae of the COVID-19 crisis in migrant populations and its mortality impact on the long-term, and those have to be addressed considering the two opposed facets of their health, both robust and vulnerable. More theoretically, the ‘migrant mortality advantage’ paradigm could be questioned and contextualized by relating it to the evolving epidemiological situation and health transition in origin and host countries.
Authors’ contributions
Funding acquisition and project coordination: S. Vandentorren. Conceptualization and methodology: M. Khlat, M. Guillot, W. Ghosn, S. Vandentorren. Formal analyses: W. Ghosn, M. Khlat, M. Guillot, Software: W. Ghosn. Writing – Original draft: M. Khlat, W. Ghosn. Writing – Review & Editing: C. Delpierre, A. Desgrées du Loû, A. Fouillet, W. Ghosn, M. Guillot, T. Lefèvre, M. Khlat, S. Rican, S. Vandentorren.
Acknowledgments
This work was supported in part by REACTing-Inserm [Grant CM/YY/JS/2020/02] and by Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) of the National Institutes of Health (NIH) (Award number R01HD079475). We thank Dr. Grégoire Rey, director of the Centre d’Epidémiologie sur les Causes Médicales de Décès (CépiDc) at Inserm, Dr. Maria Melchior, director of the Equipe de Recherche en Epidémiologie Sociale (ERES) at Inserm and Dr. Carole Dufouil from Bordeaux Population Health for their support of the DcCOV project. We also thank Mr. Christopher Leichtnam, Translations coordinator and editor at Ined for his editorial work on the paper.
Contributor Information
DcCOVMIG Research Team:
Cyrille Delpierre, Annabel Desgrées du Loû, Anne Fouillet, Walid Ghosn, Michel Guillot, Thomas Lefèvre, Myriam Khlat, Stéphane Rican, and Stéphanie Vandentorren
APPENDIX.
Appendix Table 1.
Deaths at ages at ages 40 and over and population denominators. Weeks 12–20 of years 2020 and 2016–2019. National and subnational levels.
| Country-of-birth group | France (all regions) (100%) |
Most affected regions | Intermediate regions | Least affected regions |
|---|---|---|---|---|
| Death counts, Weeks 12-20, 2020 | ||||
| France | 107,853 | 29,628 | 29,129 | 49,096 |
| North Africa | 5,957 | 2,621 | 956 | 2,380 |
| Sub-Saharan Africa | 1,739 | 1,313 | 113 | 313 |
| The Americas | 310 | 225 | 22 | 63 |
| Asia & Oceania | 1,567 | 1,081 | 203 | 283 |
| Central & Eastern Europe | 1,011 | 568 | 222 | 221 |
| Northern & Western Europe | 1,528 | 569 | 348 | 611 |
| Southern Europe | 4,335 | 1,558 | 1,073 | 1,704 |
| Total | 124,300 | 37,563 | 32,066 | 54,671 |
| Average death counts, Weeks 12-20, 2016-2019 | ||||
| France | 85,820 | 17,286 | 23,077 | 45,457 |
| North Africa | 4,874 | 1,354 | 876 | 2,644 |
| Sub-Saharan Africa | 599 | 317 | 69 | 213 |
| The Americas | 142 | 65 | 16 | 62 |
| Asia & Oceania | 780 | 410 | 142 | 228 |
| Central & Eastern Europe | 741 | 346 | 194 | 201 |
| Northern & Western Europe | 1,230 | 340 | 290 | 599 |
| Southern Europe | 3,380 | 884 | 838 | 1,658 |
| Total | 97,566 | 21,002 | 25,502 | 51,062 |
| Population, Weeks 12-20, 2020 (person-years) | ||||
| France | 29,463,497 | 6,645,235 | 7,850,761 | 14,967,501 |
| North Africa | 1,023,472 | 378,166 | 190,753 | 454,552 |
| Sub-Saharan Africa | 653,238 | 372,294 | 83,404 | 197,540 |
| The Americas | 156,985 | 84,489 | 21,139 | 51,357 |
| Asia & Oceania | 643,180 | 371,715 | 111,251 | 160,213 |
| Central & Eastern Europe | 280,831 | 137,333 | 58,932 | 84,565 |
| Northern & Western Europe | 495,395 | 138,539 | 112,924 | 243,933 |
| Southern Europe | 971,365 | 352,192 | 229,069 | 390,104 |
| Total | 33,687,963 | 8,479,963 | 8,658,233 | 16,549,765 |
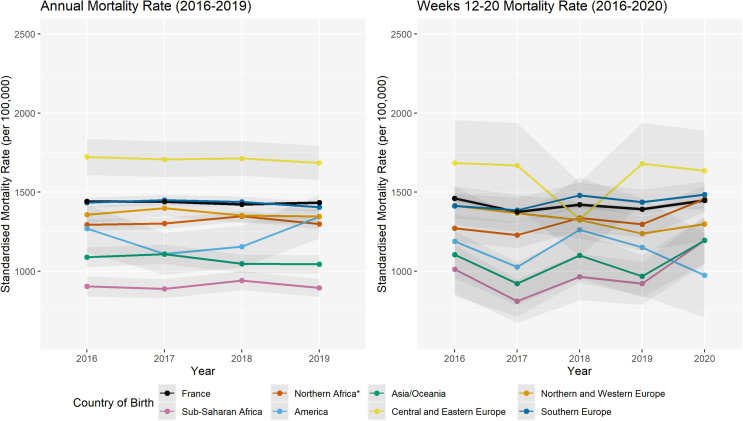
Appendix Fig. 1.
Age and sex-standardized overall mortality rates at ages 40 years and over. Calendar years 2016–2019 (left) and weeks 12–20 of years 2016–2020 (right), by country-of-birth group. France, least affected regions
References
- Bambra C., Riordan R., Ford J., Matthews F. The COVID-19 pandemic and health inequalities. 2020;74:964–968. doi: 10.1136/jech-2020-214401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bamgboye E.L., Omiye J.A., Afolaranmi O.J., Davids M.R., Tannor E.K., Wadee S., et al. COVID-19 pandemic: is Africa different? J. Natl. Med. Assoc. 2021;113:324–335. doi: 10.1016/j.jnma.2020.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beaney T., Clarke J.M., Jain V., Golestaneh A.K., Lyons G., Salman D., et al. Excess mortality: the gold standard in measuring the impact of COVID-19 worldwide? J. R. Soc. Med. 2020;113:239–334. doi: 10.1177/0141076820956802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boulogne R., Jougla E., Breem Y., Kunst A.E., Rey G. Mortality differences between the foreign-born and locally-born population in France (2004-2007) Soc. Sci. Med. 2012:1213–1223. doi: 10.1016/j.socscimed.2012.01.002. [DOI] [PubMed] [Google Scholar]
- Brahimi M. La mortalité des étrangers. Population. 1980:603–622. [Google Scholar]
- Brun S., Simon P.L. De facto; 2020. 'invisibilité des minorités dans les chiffres du Coronavirus: le détour par la Seine-Saint-Denis; pp. 68–78. Mai 2020. [Google Scholar]
- Canevelli M., Palmieri L., Raparelli V., Punzo O., Donfrancesco C., La Noce C.L., et al. COVID-19 mortality among migrants living in Italy. Ann. Ist. Super Sanita. 2020;56:373–377. doi: 10.4415/ANN_20_03_16. [DOI] [PubMed] [Google Scholar]
- Cognet M. La fabrique des inégalités de santé, une réalité sociale trop souvent tue. Rev. Fr. Des. Aff. Soc. 2021;3:117–123. [Google Scholar]
- COVID-19 Excess Mortality Collaborators . Vol. 399. The Lancet; 2022. pp. 1513–1536. (Estimating Excess Mortality Due to the COVID-19 Pandemic: a Systematic Analysis of COVID-19-Related Mortality, 2020-21). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desgrées-du-Loû A., Pannetier J., Ravalihasy A., Gosselin A., Supervie V., Panjo H., et al. Sub-Saharan African migrants living with HIV acquired after migration, France, ANRS PARCOURS Study. 2012 to 2013, Euro Surveillance. 2015;20:pii=30065. doi: 10.2807/1560-7917.ES.2015.20.46.30065. [DOI] [PubMed] [Google Scholar]
- Desrivierre D., Fabre J. Plus de décès pendant l’épisode de Covid-19 du printemps 2020 qu’au cours de la canicule de 2003. INSEE Première. 2020:1–4. [Google Scholar]
- Drefahl S., Wallace M., Mussino E., Aradhya S., Kolk M., Brandén M., et al. A population-based cohort study of socio-demographic risk factors for COVID-19 deaths in Sweden. Nat. Commun. 2020;11:5097. doi: 10.1038/s41467-020-18926-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eurostat . Revision of the European Standard Population. Report of Eurostat’s task force. European Commission; 2013. pp. 1–128. In press. [DOI] [Google Scholar]
- Fouillet A., Pontais I., Caserio-Schönemann C. C. C.-S. Excess all-cause mortality during the first wave of the COVID-19 epidemic in France, March to May 2020. Euro Surveill. 2020;25 doi: 10.2807/1560-7917.ES.2020.25.34.2001485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gascard N., Kauffmann B., Labosse A. 26% de décès supplémentaires entre début mars et mi-avril 2020: les communes denses sont les plus touchées. INSEE Focus. 2020:191. [Google Scholar]
- Goldstein J.R., Atherwood S. 2020. Improved Measurement of Racial/ethnic Disparities in COVID-19 Mortality in the United States, medRxiv. [Google Scholar]
- Gosselin A., Melchior M., Desprat D., Devetter F.-X., Pannetier J., Valat E., et al. Were immigrants on the frontline during the lockdown? Evidence from France. Eur. J. Publ. Health. 2021;31:1278–1281. doi: 10.1093/eurpub/ckab094. [DOI] [PubMed] [Google Scholar]
- Gosselin A., Warszawski J., Bajos N. Higher risk, higher protection: COVID-19 risk among immigrants in France-results from the population-based EpiCov survey. Eur. J. Publ. Health. 2022:1–9. doi: 10.1093/eurpub/ckac046. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guillot M., Khlat M., Elo I., Solignac M., Wallace M. Understanding age variations in the migrant mortality advantage: an international comparative perspective. PLoS One. 2018;13 doi: 10.1371/journal.pone.0199669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hale T., Angrist N., Goldszmidt R., Kira B., Petherick A., Phillips T., et al. A global panel database of pandemic policies. Nat. Human Behav. 2021;5:529–538. doi: 10.1038/s41562-021-01079-8. [DOI] [PubMed] [Google Scholar]
- INSEE . INSEE Références; 2021. France, portrait social. Edition 2021. [Google Scholar]
- INSEE . Chiffres-clés; 2022. L’essentiel sur … les immigrés et les étrangers.https://www.insee.fr/fr/statistiques/3633212 [Google Scholar]
- Karlinsky A., Kobak D. Tracking excess mortality across countries during the COVID-19 pandemic with the World Mortality Dataset. Elife. 2021:10. doi: 10.7554/eLife.69336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerjosse R., Lé J. Les personnes nées françaises à l'étranger ont un profil plus proche des natifs que des immigrés. INSEE Première. 2020:1829. [Google Scholar]
- Krasnik A., Norredam M., Diaz E., Aradhya S., Benfield T., Madar A.A., et al. Situational brief: migration and COVID-19 in scandinavian countries. Lancet Policy Briefs. 2020:1–10. [Google Scholar]
- Le Minez S., Roux V. INSEE PREMIERE; 2021. 2020 : une hausse inédite des décès depuis 70 ans. No. 1847. [Google Scholar]
- Marmot M., Allen J. Exposing and amplifying health inequalities. J. Epidemiol. Community Health. 2020;74:681–682. doi: 10.1136/jech-2020-214720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melchior M., Desgrées du Loû A., Gosselin A.D.G.D., Carabali M., Merckx J., et al. Migrant status, ethnicity and COVID-19: more accurate European data are greatly needed. Clin. Microbiol. Infect. 2021;27:160–162. doi: 10.1016/j.cmi.2020.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nkuba A., Makiala S.M., Guichet E., Tshiminyi P.M., Bazitama Y.M., Yambayamba M.K., et al. High prevalence of anti-SARS-CoV-2 antibodies after the first wave of COVID-19 in Kinshasa, Democratic Republic of the Congo: results of a cross-sectional household-based survey. Clin. Infect. Dis. 2022;74(5):882–890. doi: 10.1093/cid/ciab515. Jun 5:ciab515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- OECD . 2020. What Is the Impact of the COVID-19 Pandemic on Immigrants and Their Children? [Google Scholar]
- Oehlert G. A note on the delta method. Am. Statistician. 1992;46:27–29. [Google Scholar]
- Oksuzyan A., Juel K., Vaupel J., Christensen K. Men: good health and high mortality. Sex differences in health and aging. Aging Clin. Exp. Res. 2008;20:91–102. doi: 10.1007/bf03324754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papon S., Robert-Bobée I. INSEE FOCUS; 2020. The number of deaths rose twice as high for people born abroad as for those born in France during the Covid-19 health crisis. No. 198. [Google Scholar]
- Papon S., Robert-Bobée I. INSEE FOCUS; 2021. Deaths in 2020 : greater increase for people born abroad than for those born in France, especially in March-April. No. 231. [Google Scholar]
- Pison G., Meslé F. COVID-19 is more deadly for men than for women. Population & Societies. 2022;598:1–4. [Google Scholar]
- Rey G., Rican S., Luce D., Menvielle G., Jougla E. Measuring social inequalities in cause-specific mortality in France: comparison between linked and unlinked approaches. Epidemiol. Public Health/Rev. Epidémiol. Santé Publique. 2013;61:221–231. doi: 10.1016/j.respe.2012.11.004. [DOI] [PubMed] [Google Scholar]
- Rostila M., Cederström A., Wallace M., Brandén M., Malmberg B., Andersson G. Disparities in COVID-19 deaths by country of birth in Stockholm, Sweden: a total population based cohort study. Am. J. Epidemiol. 2021;190:1510–1518. doi: 10.1093/aje/kwab057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saenz R., Garcia M.A. The disproportionate impact of COVID-19 on older Latino mortality: the rapidly diminishing Latino paradox. J Gerontol B Psychol Soc Sci. 2021;76:e81–e87. doi: 10.1093/geronb/gbaa158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vandentorren s., DSmaïli S., Chatignoux E., Maurel M., Alleaume C., Neufcourt L., et al. The effect of social deprivation on the dynamic of SARS-CoV-2 infection in France: a population-based analysis. Lancet. 2022;7:e240–e249. doi: 10.1016/S2468-2667(22)00007-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vanthomme K., Gadeyne S., Lusyne P., Vandenheede H. A population-based study on mortality among Belgian immigrants during the first COVID-19 wave in Belgium. Can demographic and socioeconomic indicators explain differential mortality? SSM - Population Health. 2021 doi: 10.1016/j.ssmph.2021.100797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallace M., Khlat M., Guillot M. Mortality advantage among migrants according to duration of stay in France, 2004-2014. BMC Publ. Health. 2019:19. doi: 10.1186/s12889-019-6652-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warszawski J., Bajos N., Costemalle V., Leblanc S., Epicov E. vol. 2021. Etudes & Résultats; 2020. p. 1202. (4 % de la population a développé des anticorps contre le SARS-CoV-2 entre mai et novembre). [Google Scholar]
- WHO . WHO; 2020. International Guidelines for Certification and Classification (Coding) of COVID-19 as Cause of Death. [Google Scholar]