Abstract
Objective
The global shift of trends to minimally invasive spine (MIS) surgery for lumbar degenerative diseases has become prominent in India for few decades. We aimed to assess the current status of MIS techniques for lumbar interbody fusion and their surgical outcomes in the Indian population.
Materials and Methods:
A systematic review (following Preferred Reporting Items for Systematic Reviews and Meta-Analysis guidelines) was performed using PubMed and Google Scholar till November 2020. The primary (visual analog scale [VAS] and oswestry disability index [ODI] scores; intraoperative blood loss; duration of surgery; duration of hospital stay, and fusion rate) and secondary (wound-associated complications and dural tear/cerebrospinal fluid (CSF) leak) outcomes were analyzed using Review Manager 5.4 software.
Results:
A total of 15 studies comprising a total of 1318 patients were included for analysis. The pooled mean of follow-up duration was 26.64 ± 8.43 months (range 5.7–36.5 months). Degenerative spondylolisthesis of Myerding grade I/II was the most common indication, followed by lytic listhesis, herniated prolapsed disc, and lumbar canal stenosis. The calculated pooled standard mean difference (SMD) suggested a significant decrease in postoperative ODI scores (SMD = 5.53, 95% confidence interval [CI] = 3.77–7.29; P < 0.01) and VAS scores (SMD = 6.50, 95% CI = 4.6–8.4; P < 0.01). The pooled mean blood loss, duration of postoperative hospital stay, duration of surgery, and fusion rate were 127.75 ± 52.79 mL, 4.78 ± 3.88 days, 178.59 ± 38.69 min, and 97.53% ± 2.69%, respectively. A total of 334 adverse events were recorded in 1318 patients, giving a complication rate of 25.34%.
Conclusions:
Minimally invasive transforaminal lumbar interbody fusion (TLIF) is the most common minimally invasive technique employed for lumbar interbody fusion in India, while oblique lumbar interbody fusion is in the initial stages. The surgical and outcome-related factors improved significantly after MIS LIF in the Indian population.
Keywords: Lumbar degenerative disease, lumbar interbody fusion, meta-analysis, minimally invasive spine surgery, minimally invasive transforaminal lumbar interbody fusion, spondylolisthesis, systematic review
INTRODUCTION
The basic principle of the evolution of new surgical techniques is to make them simpler and faster with the preservation of the normal anatomical structures. The recent minimally invasive techniques for lumbar inter-body fusion are the foremost steps in this process. In the spine, the major injury to the normal adjacent anatomical structures responsible for the preservation of functional spine unit is grossly affected in the open techniques during the exposure. As the minimally invasive techniques avoid such damage by modifying the access, they are also known as minimal access spine techniques. A major indication of these surgeries is degenerative lumbar spondylosis. It also includes degenerative spondylolisthesis (DS), disc generation, and canal stenosis. With almost 266 million (3.63%) cases per year worldwide, this is a major cause of morbidity.[1] In low- to middle-income countries like India, the incidence is up to four times higher than the high-income countries/developed countries.[1] Although a very small percentage of these patients needs surgical intervention, the overall number of such patients is soaring due to the enormous expanding Indian population. In such circumstances, the use of minimally invasive spine (MIS) techniques would not only reduce patient morbidity but will also improve productivity by the early resumption of work. There has been a major stride in this direction in western countries. We aimed to assess the present status of MIS techniques for lumbar interbody fusion and their outcome in the Indian population. We systematically reviewed the literature published on the MIS techniques used in the Indian population to date to assess the trends and did a meta-analysis to evaluate their surgical and clinical outcome concerning open techniques and the results reported worldwide.
MATERIALS AND METHODS
Research protocol
This study is a systematic review and meta-analysis to assess the role of minimally invasive lumbar interbody fusion techniques in India. It was performed as per Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines.[2] The study aimed to assess the clinical and surgical outcome of minimally invasive lumbar interbody fusion in the Indian population. Extracted data were analyzed in terms of primary and secondary outcomes.
Search strategy and eligibility criteria
A comprehensive literature search was performed using PubMed (Medline database) and Google Scholar till November 2020. The inclusion criteria for the studies were original articles reporting the clinical outcome of lumbar interbody fusion using minimally invasive techniques including anterior lumbar interbody fusion (ALIF), lateral lumbar interbody fusion (LLIF), oblique lumbar interbody fusion (OLIF), and MIS-transforaminal lumbar interbody fusion (MIS-TLIF) in Indian patients. The exclusion criteria were articles with less than 10 reported cases reported in a language other than English, duplicate publications, and studies with no clinical data. An initial search was done on PubMed using the query “posterior lumbar interbody fusion (PLIF) OR TLIF OR OLIF OR LLIF OR lateral lumbar interbody fusion ORALIF OR ALIF OR lumbar interbody fusion AND India OR Indian” with no limits used. There were 109 results. Totally 63 studies were excluded based on the title and the abstract. The full text was reviewed of the 46 remaining articles. Eleven studies were identified as eligible studies. Google scholar was searched separately for each keyword. The duplicates to the PubMed search were excluded, and three more studies were identified. The search procedure and the data extraction were performed by two authors independently. All the prominent MIS surgeons were communicated for any more publications that were not included. The last search was performed on December 4, 2020. A total of 15 studies were finally included for data extraction and analysis.[3,4,5,6,7,8,9,10,11,12,13,14,15,16,17] The detailed search methodology is summarized in [Figure 1] (PRISMA flowchart). The study design, demographics, and features of the included studies are summarized in [Table 1]. The primary outcomes of the study were (1) postoperative improvement in functional scores (visual analog scale [VAS] and Oswestry Disability Index [ODI]), (2) intraoperative blood loss, (3) duration of surgery, (4) duration of hospital stay, and (5) fusion rate. The secondary outcome included (1) wound-associated complications and (2) dural tear/CSF leak.
Figure 1.

Preferred Reporting Items for Systematic Reviews and Meta-Analysis flowchart of the selection process to identify studies eligible for pooling
Table 1.
Study design, demographics, and features of the included studies
| Study | Design | Sample size (n) | Age (years) | Gender (male: female) | Grades of listhesis | Level | Procedure type | Follow-up duration (months) |
|---|---|---|---|---|---|---|---|---|
| Jhala et al. 2014 | Prospective Observational | 23 | 55.45 (24-78) | 1:2.8 | I, II | L4-L5 (14) L5-S1 (7) | MI-TLIF | 16 (12-60) |
| Hari et al. 2016 | Retrospective Observational | 300 | 49.2 (22-81) | 1.3:1 | NA | NA | MI-TLIF | 12 |
| Kulkarni et al. 2016 | Prospective cohort study | 36 | 51.55 | 1:2.6 | NA | L2-L3 (20) L3-L4 (16) | MI-TLIF | 36.5 (18-54) |
| Rajakumar et al. 2017 | Prospective cohort study | 36 | 51.7 (24-80) | 1:1.6 | II, III | L3-L4 (4) L4-L5 (19) L5-S1 (13) | MI-TLIF | 30.4 (24-60) |
| Ganesan et al. 2017 | Prospective cohort study | 24 | 54.63 | NA | I, II | NA | MI-TLIF | 25.6 |
| Chandra Vemula et al. 2018 | Prospective Observational | 25 | 61.05 (54-65) | 1:4 | I, II | L3-L4 (1) L4-L5 (14) L5-S1 (9) | MI-TLIF | 18 (6-25) |
| Krishnan et al. 2018 | Retrospective Observational | 13 | 55.23±7.29 | 1:1.6 | NA | L4-L5 (9) L5-S1 (4) | MI-TLIF | 39±6.36 (25-47) |
| Singh et al. 2019 | Retrospective Observational | 30 | 42.55 (14-65) | 1:1.3 | I, II, III | NA | MI-TLIF | 12.4 (7-39) |
| Patel et al. 2020 | Prospective Observational | 560 | 61.8±12.7 | 1:1.2 | NA | L1-L2 (11) L2-L3 (17) L3-L4 (72) L4-L5 (256) L5-S1 (204) | MI-TLIF | 29.1±4.8 |
| Balasubramanian et al. 2020 | Prospective cohort study | 40 | 48.4±11.4 | 1:1 | I, II | NA | MI-TLIF | 6 |
| Subramaniam et al. 2020 | Retrospective Cohort study | 31 | 51.8 | 1:2.9 | I, II, III | L3-L4 (3) L4-L5 (23) L5-S1 (17) | MI-TLIF | 9 |
| Mehta et al. 2020 | Retrospective Observational | 100 | 60.89 (37-77) | 1:1.7 | I, II | L3-L4 (7) L4-L5 (79) L5-S1 (14) | MI-TLIF | 25.25±2.55 |
| Modi et al. 2020 | Retrospective Observational | 40 | 49.6±10.4 | 1:1.86 | NA | NA | MI-TLIF | 24 |
| Parikh et al. 2019 | Retrospective Observational | 45 | 63 (40-80) | 1:2 | I, II, III | L1-L2 (3) L2-L3 (4) L3-L4 (16) L4-L5 (36) L5-S1 (1) | OLIF | 11 (1-18) |
| Sardhara et al. 2019 | Retrospective Observational | 15 | 52.5±9.69 | 1.1:1 | I, II | L3-L4 (1) L4-L5 (14) L5-S1 (1) | OLIF | 5.7±3.3 |
MI-TLIF - Minimally invasive transforaminal lumbar interbody fusion, OLIF - Oblique lumbar interbody fusion, NA - Not available
Statistical analysis
Meta-analysis was performed using Review Manager 5.4 software (Cochrane Collaboration, Oxford, UK). Standard mean difference (SMD) was calculated for continuous outcomes (ODI, VAS-B, and VAS Score) along with 95% confidence intervals (CIs). Similarly, mean (95% CI) was calculated for the blood loss, duration of hospital stay, and duration of surgery whereas pooled frequency (%) was calculated for complications. The level of significance was set at P < 0.05. The statistic of I2 was used to efficiently test for the heterogeneity, where I2 <25%, I2 = 25%–50%, and I2 > 50% indicates low, moderate, and a high degree of heterogeneity, respectively. A random-effect model was used to estimate pooled effects as I2 >50. When only range was reported for a continuous variable in an included study, the Standard deviation (SD) was estimated according to the method described in the Cochrane Handbook for Systematic Reviews.[18]
RESULTS
Demographics
A total of 15 studies comprising a total of 1318 patients were included for analysis. These are summarized in [Table 1]. The pooled mean age of the patients was 56.77 ± 14.1 years, with more females than males (M: F = 1:1.24). The sample size of the studies ranges from 13 to 560 patients. These studies were published between 2014 and 2020. The pooled mean of follow-up duration was 26.64 ± 8.43 months (range 5.7–36.5 months).
Indications for fusion
Degenerative listhesis of Myerding's Grade I or II was the most common indication, followed by lytic listhesis, herniated prolapsed disc, and lumbar canal stenosis. Post-discectomy pain failed back syndrome and degenerative scoliosis were indications for MIS-LIF in less than ten patients each. L4/L5 (n = 464, 51%) was the most common level operated, followed by L5/S1 (30%), L3/L4 (13%), L2/L3 (4%), and L1/L2 (2%). Single-level fusion was done in most cases. Few studies reported multilevel fusion to a maximum of 3 levels.
Primary outcomes
Most authors reported the clinical outcome in terms of ODI and VAS scores. Two authors used the MacNab score. The primary and secondary outcomes of the included studies are summarized in [Table 2].
Table 2.
Operative outcomes of the included studies
| Author | VAS-pre (L) | VAS-post (L) | VAS-pre (B) | VAS-post (B) | ODI-pre | ODI-post (latest follow-up) | Surgery duration (min) | Blood loss | Fluoroscopic exposure | Conversion to open | Mobilisation within days | Duration of hospital stay (days) | Fusion rate |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Jhala et al. 2014 | MacNab criteria Excellent-14 Good-5 Fair-2 Poor-2 | 180 (150-330) | NA | NA | 1 | 2 | NA | 95.6% | |||||
| Hari et al. 2016 | NA | NA | 6.74±1.34 | 1.34±1.37 | 58.23±12.25 | 14.60±8.89 | 115 | 60 | NA | Nil | 1 | 8.4 (3-23) | 96% |
| Kulkarni et al. 2016 | Percentage change=70.12±39.19 | Percentage change=50.17±38.39 | Percentage change=61.79±33.4 | 204±32.4 | 111.81 | 57.77 (44-96) | Nil | 1 | 3±2 | 100% | |||
| Rajakumar et al. 2017 | NA | NA | 6.5±1.5 | 1.6±1.3 | 53.7±13.1 | 22.5±15.5 | 146.7 | 90 | NA | Nil | 1 | 2.5 | 97% |
| Ganesan et al. 2017 | 8 | 2 | 7 | 2 | 57.8 | 19.9 | NA | 63±21.565 | NA | Nil | NA | 3±0.68 | 91.7% |
| Chandra Vemula et al. 2018 | NA | NA | 7.33 (6-8) | 2.66 (2-4) | 41.66 (32-47) | 18.16 (15-21) | NA | NA | NA | Nil | NA | NA | 100% |
| Krishnan et al. 2018 | 8.84±0.90 | 0.92±1.04 | 8.39±1.04 | 0.77±0.83 | 75.97±12.78 | 34.19±8.91 | 250.23±52.9 | 47.70±12.35 | NA | Nil | 1 | 29.92±4.94 h (24-39) | 100% |
| Singh et al. 2019 | NA | NA | NA | NA | 61.87±16.65 | 24.23±13.85 | NA | NA | 48.5±20.5 (first 10 cases) 18±7.25 (next 20 cases) | Nil | 2 | 5.2 | BFG 62%-II 31%-III |
| Patel et al. 2020 | NA | NA | 7.9±1.13 | 3.01±1.18 | 73.13±6.32 | 18.89±6.12 | 173±39 | 110±15 | NA | Nil | 1 day | 3.3±1.76 | 98.0% (n=549) |
| Balasubramanian et al. 2020 | NA | NA | 7.18±0.91 | 2.06±0.57 | 54.63±4.89 | 19±3.79 | 171±46.2 | 250±63.24 | 33±12 | 1 | NA | 3±2 | 100 |
| Subramaniam et al. 2020 | 6.52 | 1.79 | 5.97 | 1.8 | NA | NA | NA | 100 (50-250) | NA | Nil | NA | 5 | NA |
| Mehta et al. 2020 | 7.36±1.11 | 1.48±0.89 | 6.1±1.13 | 1.95±1.1 | 63.2±6.47 | 23.92±2.41 | 186.25 | 215 | 3.1 Gy cm2 | Nil | NA | NA | 97% |
| Modi et al. 2020 | NA | NA | 8.4±0.7 | 2.1±0.9 | 62.1±5.1 | 21.3±7.2 | 191.8±33.8 | 109.9±23.5 | NA | Nil | NA | 5±1.1 | NA |
| Parikh et al. 2019 | MacNab criteria Excellent-33 (73.3%) Good-11 (24.44%) Fair-1 (2.22%) Poor-0 | 40 | NA | NA | Nil | NA | 2 | NA | |||||
| Sardhara et al. 2019 | NA | NA | 7±0.7 | 3.3±0.4 | 35±6.1 | 14.6±4.1 | 191.4±25.6 | NA | NA | Nil | 2 | 8±3.7 | BFG 2-I 7-II 3-III |
VAS - Visual Analog Scale, ODI - Oswestry disability score, B - Backache, L - Limb pain, NA - Not available, BFG - Bridewell interbody fusion grade
Oswestry Disability Index score
The preoperative and postoperative ODI scores were reported in 11 studies. Ten studies were analyzed as data in one study was inadequate. The ODI scores of 1159 patients were evaluated [Figure 2]. The effect size was measured in terms of the standardized mean difference (SMD). The line of null effect was not crossed by the 95% CI line for the standardized mean difference for any of the included studies. The pooled SMD was suggestive of a significantly strong correlation of a decrease in ODI scores following surgery (SMD = 5.53, 95% CI = 3.77–7.29; P < 0.01). The overall percentage change in the ODI score at the last follow-up was 63.1%.
Figure 2.
Forrest plot comparing the functional outcome of minimally invasive spine surgery for lumbar interbody fusion, in terms of preoperative versus postoperative ODI. ODI: Oswestry Disability Score
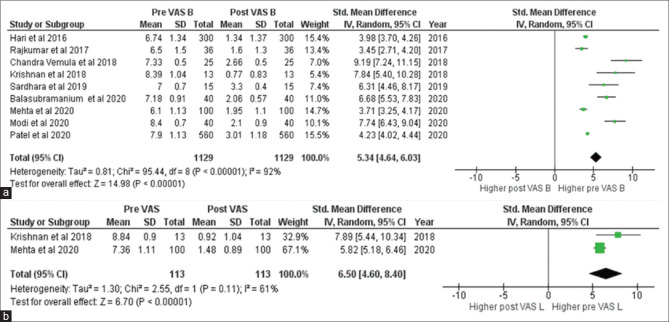
Visual analog scale score
The VAS score for backache was reported in eleven studies and adequate data for analysis were available in nine studies. One thousand one hundred and twenty-nine patients were assessed. The calculated SMD in each study showed a significant change in the VAS-B scores following surgery (SMD = 5.34, 95% CI = 4.06–6.03; P < 0.01) [Figure 3a].
Figure 3.
Forrest plot comparing the pain outcome of minimally invasive spine surgery for lumbar interbody fusion, in terms of preoperative versus postoperative. (a) VAS-B. (b) VAS-L. VAS-B: Visual analog score for backache, VAS-L: Visual analog score for lower limb pain
VAS score for pain radiating to the lower limb was reported by four studies and could be analyzed in two studies only. There was a statistically significant change in the VAS-L scores post-surgery (SMD = 6.50, 95% CI = 4.6–8.4; P < 0.01) [Figure 3b].
Intraoperative blood loss
Ten studies reported intraoperative blood loss during MIS-LIF. Most had reported mean blood loss only. The pooled blood loss during the procedure was found to be 127.75 ± 52.79 mL (mean ± SD) in 808 reported cases [Figure 4].
Figure 4.

Intraoperative blood loss in included studies and pooled mean
Duration of hospital stay
Data of 1028 patients from eight studies suggested a mean (±SD) duration of postoperative hospital stay of 4.78 ± 3.88 days. Most of the authors reported discharge between the 3rd and 5th postoperative days [Figure 5].
Figure 5.
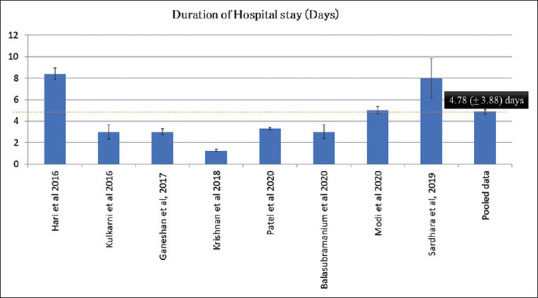
Duration of hospital stay in included studies and pooled mean
Surgery duration
Only 8 out of 15 studies, with 827 patients, had mentioned data adequate to calculate an overall time required for surgery. The mean ± SD duration of surgery was 178.59 ± 38.69 min [Figure 6].
Figure 6.

Duration surgery in included studies and pooled mean
Fusion rates
The reported fusion rates were between 91.7% and 100% by ten authors. The mean ± SD fusion rate was 97.53% ± 2.69. Two authors had reported fusion in terms of Bridwell Fusion Grades. Most patients had grade II or III fusion at the last follow-up.
Secondary outcome
Complications rates
The complications were reported as the number of events. Radiculopathy was the most common postoperative complication (n = 76, 5.8%), followed by CSF leak or dural tear (n = 60, 4.5%) and operative site infections (n = 52, 3.9%). Hardware-associated problems, screw misplacement needing revision, nonunion or persistent instability, and bladder/bowel impairment were other significant postoperative complications [Figure 7]. A total of 334 events were recorded in 1318 patients, giving a complication rate of 25.34%. Data were inadequate to calculate overall complications per case. Psoas spasms, peritoneal breach, vascular injury, and gastroparesis were the complications specific to OLIF.
Figure 7.

Complications reported in the included studies
DISCUSSION
The minimally invasive techniques for lumbar interbody fusion are aimed at minimal or no interruption of the posterior tension band helps in the preservation of normal biomechanics and thus yields rapid recovery. It includes ALIF, OLIF, LLIF, and minimally invasive TLIF (MI-TLIF) techniques. The interbody fusion through these approaches is augmented with either lateral interbody fusion with plates or percutaneous posterolateral pedicle screw fixation. The ALIF and PLIF were succeeded by the TLIF and LLIF, while OLIF has evolved recently. In our systematic review, we found that Indian authors have published work comprising MI-TLIF and OLIF only. There was no case series of anterior or lateral lumbar interbody fusion. The reports of MIS-TLIF were from 2016 to 2021. While there were only two series of OLIF reported. This is the first meta-analysis of Indian data to assess the pooled outcome of minimally invasive techniques for lumbar interbody fusion.
Advantage of minimally invasive spine surgery (MISS) for degenerative spine disease in Indian patients
In degenerative spine disease (DSD), surgical intervention has shown greater improvement in pain and functional status as compared to nonsurgical treatment.[19] According to the North American Spine Society guidelines for DS, surgical decompression with fusion was suggested for the treatment of patients with symptomatic spinal stenosis and DS.[20] The minimally invasive techniques provide adequate decompression, both direct and indirect. They have similar fusion rates as open techniques while keeping the posterior tension band intact.[21,22] In the meta-analysis also, we found that the DSD, including grade I to III DS, was the most common indication for intervention by Indian surgeons. All the included studies confirmed marked improvement in pain and functional status postoperatively, as a significant change in the VAS and ODI scores by MIS TLIF. Minimum exposure requirement significantly reduces the exposure and closure time. The overall duration of surgery was only 178.59 ± 38.69 min. Short operative time and minimal blood loss (pooled mean 127.75 ± 52.79 mL) confers rapid postoperative recovery. This was reflected in a short postoperative hospital stay (4.78 ± 3.88 days). The reported fusion rates were also good, ranging from 91.7% to 100%.
Lu et al. had published a systematic review and meta-analysis of minimally invasive versus open spinal fusion for spondylolisthesis for non-Indian patients in 2017.[22] [Table 3] shows a comparison between the primary outcomes of the present study and the outcomes reported by Lu et al.[22] The pooled duration of surgery for the Indian literature was less than the open and MIS cohorts of Lu et al. The blood loss and duration of hospital stay were comparable to the MIS cohort, while it was less as compared to the open surgery group. The fusion rates achieved as reported by the Indian literature were the same as that reported by the open and MIS cohorts both.[22] All the primary and secondary outcomes of MIS-LIF in the Indian population reported by Indian authors were comparable to world standards for MIS and better than the open techniques of LIF.
Table 3.
Summary of pooled outcome of minimally invasive lumbar interbody fusion in Indian population, and comparision with outcome reported by Lu et al. for minimally invasive and open spine surgeries (review and meta-analysis of literature comparing minimally invasive spine vs. open lumbar interbody fusion)
| Variable | Results of present study (pooled data) | Overall outcome of MIS-LIF (Lu et al. MIS cohort) | Overall outcome of open LIF (Lu et al. open cohort) |
|---|---|---|---|
| Number of studies included | 15 | 10 | |
| Number of patients | 1318 | 602 (MIS=328, open=274) | |
| Males:females | 1:1.24 | 1:2.58 | 1:2.24 |
| Age (years), mean (range) | 56.77±14.1 | 58.1 (49.67-67) | 59.4 (52.6-69.1) |
| Indication for LIF | Isthmic and DS Lumbar canal stenosis Failed back syndrome | Isthmic and DS | |
| Meyerding's grades included | Grade I, II, III | Grade I and II | |
| Percentage change in ODI scores | 63.1 (%) | NA | NA |
| Duration of surgery | 178.59±38.69 | 213 | 191 |
| Blood loss | 127.75±52.79 mL | 199 | 514 |
| Duration of hospital stay (days) | 4.78±3.88 | 5.3 | 8.0 |
| Fusion rate | 97.53% (±2.69) | 96.8 | 97.2 |
| Complications (events per cent) | 25.34 | 11.2 | 16.1 |
MIS - Minimally invasive spine, MIS-LIF - MIS-lumbar interbody fusion, ODI - Oswestry disability index, DS - Degenerative spondylolisthesis, NA - Not available
Minimally invasive transforaminal lumbar interbody fusion versus oblique lumbar interbody fusion
With growing evidence of the superiority of minimally invasive techniques for lumbar interbody fusion over open techniques, the search has extended to find the superior among the MIS techniques.[21,22,23,24] MI-TLIF was first introduced in 2003, while OLIF was introduced in 2012.[25,26] Both these techniques provide a similar improvement in ODI and VAS scores.[27] While OLIF depends primarily on indirect decompression to relieve the neural compression, MI-TLIF provides added direct decompression also.[28] Lin et al. reported better intraoperative and postoperative parameters such as less intraoperative blood loss, less operative time, and shorter duration of hospital stay, with OLIF as compared to MI-TLIF. They attributed it to the non-violation of the posterior elements in OLIF, as against MI-TLIF. OLIF confers better sagittal and coronal balance due to large, anteriorly placed cage as against MI-TLIF, wherein smaller bullet-shaped cages are placed in the middle of the endplate. It provides a theoretical benefit to OLIF of fewer chances of cage subsidence.[27] Although OLIF has a superior clinical and radiological outcome, it is a relatively recent technique with a significantly steep learning curve. The lateral retroperitoneal corridor, which accounts for most of its benefits, also places one at high risk for major vascular and bowel injury. There is little literature comparing OLIF with MI-TLIF. Only two case series have been reported on OLIF involving Indian patients, as against 13 studies on MI-TLIF.[16,17] Excellent clinical improvement was reported in both OLIF and MI-TLIF cohorts included in this study. However, longer operative time and hospital stay reported by our series on OLIF highlight the steep learning curve for the technique.[17] Due to the limited sample size and significant difference in the outcomes reported by the two studies of OLIF, we could not perform a statistical comparison with the MI-TLIF cohort.
Postoperative surgical and clinical outcome
LIF aims to restore the intervertebral space and stabilize the segments with proper height and lordosis.[28,29] Restoration of the disc height and foraminal height by the insertion of an interbody cage causes indirect decompression. The thick and lax hypertrophied ligamentum flavum, anterior longitudinal ligament, and posterior longitudinal ligament are stretched to allow space in the spinal canal. Extra space is created between the boney boundaries of the neural foramina counters the boney osteophytes within. Resection of the bony spur, the medial part of the facet, lamina, hypertrophied ligamentum flavum, and the herniated disc provide direct decompression of the spinal canal and the neural foramina. Fusion induced by the interbody cage with lateral vertebral body screws or posterolateral pedicle screws corrects the instability at the spinal motion segment. These mechanisms, along with restoration of the coronal and sagittal balance, are responsible for the significant postoperative improvement in ODI and VAS scores with interbody fusion. The height and alignment correction were evaluated in only 2 Indian studies on MISS for lumbar interbody fusion. Parikh et al. studied these effects in OLIF. They reported significant improvement in the foraminal height (26.27%), disc height (92.1%), segmental lordosis (3.4°), listhesis reduction (6.8°), and spinal canal area (42.7%).[16] Rajakumar et al. in their study on MIS-TLIF found that there was a significant decrease in the sacral slope (SS) and an increase in the pelvic tilt following interbody fusion. There was a significant increase in the disc space angle and a decrease in the lumbar lordosis. Complete reduction of all grades of spondylolisthesis (grades II–III) was achieved.[6]
Complication
Radiculopathy in the form of paresthesia involving the dermatome of the affected nerve was the most common postoperative complication reported. Patel et al. had reported an extensive study of 560 patients of MIS-TLIF over 10 years.[11] It was focused on perioperative complications. They reported an overall complication rate of 25.5%. Transient paresthesia and superficial wound infections were reported as the most common complications. Overall, most of the complications were reversible and improved in 4–6 weeks.[11,16] CSF leak and dural tear were the second-most common complication encountered. Most of the authors reported the use of fibrin glue to seal the rent with no postoperative CSF leaks.[11] Screw misplacement and revision were reported in 2.5% (n = 34/1318) patients. Lu et al. reported lower complication rates in MIS (11.2%) and open LIF cohorts (16.1%) as compared to our results of pooled complication rates of Indian literature (25.34%).[22] This could be because most Indian surgeons are in the early phase of their learning curve. Eight studies had a sample size of more than 30 and only three studies had more than 50. Complications are more common during the early part of the learning curve of MISS. Most authors concluded that the asymptote is achieved by the 30th case based on the technique, and significantly improved outcomes are observed afterward.[14,15,30,31] It also explains the variability in the reported complication rates within the Indian literature.
Impediments to universal acceptance of MISS over open techniques for lumbar interbody fusion
The minimally invasive techniques have proved to be more effective, but every bean has its black. Most authors have highlighted the steep learning curve, increased expenses, and radiation exposure as major hurdles. Patel et al. reported significantly higher complication rates during the first 3 years of experience of MI-TLIF as compared to the past 7 years in 10 years of their experience (44.3% vs. 16.75%, respectively).[11] Mehta et al. did a retrospective analysis of MIS-TLIF cases to assess the learning curve in DS. They concluded that the learning curve is achieved between 25th and 50th cases.[14] Modi et al. also reported that the operative time reached a plateau by the 50th case.[15] Singh et al. reported a significant reduction in the need of the number of C-arm shots after 10 cases.[10]
A significantly larger exposure to radiation was reported by most of the authors. Singh et al. assessed the psychological stress among the residents, nursing staff, and technicians.[10] They noted higher stress levels among the staff involved in MIS surgery due to increased risk of radiation exposure. Kulkarni et al. reported that 57.7 (44–96) [mean (range)] X-ray shots were taken per case during MIS-TLIF. It was found to be significantly higher than the X-ray exposure in open techniques.[5] Balasubramanium et al. reported it to be 33 ± 12 shots per case.[12] Other studies also concluded increased radiation exposure with minimally invasive techniques.[32,33]
The cost of treatment is a major factor in deciding the surgical approach/technique. Due to the requirement of specialized instruments, minimally invasive techniques are invariably costly as compared to their open counterparts. Kulkarni et al. gave an estimate of 1.25–1.5 lakhs additional cost of performing MIS-TLIF. This is a major reason for the lag in MIS techniques acceptance in many centers of India. However, at government-aided setups, MISS could be cost-effective as the duration of hospital stay is considerably less as compared to open techniques. It would also increase the turnover rate and aid in shortening the wait list. Furthermore, MISS has a lower tendency for the occurrence of adjacent segment disease as compared to open techniques.[34] This would reduce the readmission rates. However, there is still no sufficient evidence to confirm the cost-effectiveness of MISS over open surgical treatments.[20]
Limitations
Our search was restricted to PubMed and Google Scholar. There may be few eligible studies that may have been on other databases and not included in the study. However, communication with eminent spine surgeons makes it less likely and adds strength to the search methodology. Most of the included studies were retrospective and were of low level of evidence. There could be significant bias in these studies. Although this study represents the highest level of evidence regarding the outcome of MIS-LIF in India, a confirmation with a large multicenter randomized control trial is imperative. There was a lack of data, especially regarding the variance in most of the studies. Mathematical tools had to be used for their calculation. It was then used to calculate the pooled means. Another limitation of the study was considerable heterogeneity between the studies. The application of random effect model allowed equal distribution of the effect across the studies.
CONCLUSIONS
MI-TLIF is the most common minimally invasive technique employed for lumbar interbody fusion in India. The inception of OLIF is in the initial stages. There was a significant improvement in clinical status postoperatively. The complication rate was 25.34% (events per case). The surgical and outcome-related factors such as operative time, intraoperative blood loss, duration of hospital stay, and fusion rates of Indian surgeons were comparable to the world standards. This study represents the first systematic review and meta-analysis of Indian data of minimally invasive techniques for lumbar interbody fusion.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Ravindra VM, Senglaub SS, Rattani A, Dewan MC, Härtl R, Bisson E, et al. Degenerative lumbar spine disease: Estimating global incidence and worldwide volume. Global Spine J. 2018;8:784–94. doi: 10.1177/2192568218770769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Moher D, Liberati A, Tetzlaff J, Altman DG PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jhala A, Singh D, Mistry M. Minimally invasive transforaminal lumbar interbody fusion: Results of 23 consecutive cases. Indian J Orthop. 2014;48:562–7. doi: 10.4103/0019-5413.144217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hari A, Krishna M, Rajagandhi S, Rajakumar DV. Minimally invasive transforaminal lumbar interbody fusion-indications and clinical experience. Neurol India. 2016;64:444–54. doi: 10.4103/0028-3886.181536. [DOI] [PubMed] [Google Scholar]
- 5.Kulkarni AG, Bohra H, Dhruv A, Sarraf A, Bassi A, Patil VM. Minimal invasive transforaminal lumbar interbody fusion versus open transforaminal lumbar interbody fusion. Indian J Orthop. 2016;50:464–72. doi: 10.4103/0019-5413.189607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rajakumar DV, Hari A, Krishna M, Sharma A, Reddy M. Complete anatomic reduction and monosegmental fusion for lumbar spondylolisthesis of Grade II and higher: Use of the minimally invasive “rocking” technique. Neurosurg Focus. 2017;43:E12. doi: 10.3171/2017.5.FOCUS17199. [DOI] [PubMed] [Google Scholar]
- 7.Ganesan S, Jayabalan V, Kumar V, Kailash K. Clinical and radiological outcomes of modified mini-open and open transforaminal lumbar interbody fusion: A comparative study. Asian Spine J. 2018;12:544–50. doi: 10.4184/asj.2018.12.3.544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chandra Vemula VR, Prasad BC, Jagadeesh MA, Vuttarkar J, Akula SK. Minimally invasive transforaminal lumbar interbody fusion using bone cement-augmented pedicle screws for lumbar spondylolisthesis in patients with osteoporosis. Case series and review of literature. Neurol India. 2018;66:118–25. doi: 10.4103/0028-3886.222826. [DOI] [PubMed] [Google Scholar]
- 9.Krishnan A, Barot M, Dave B, Bang P, Devanand D, Patel D, et al. Percutaneous transforaminal endoscopic decompression and cageless percutaneous bone graft transforaminal lumbar interbody fusion: A feasibility study. J Orthop Allied Sci. 2018;6:21–7. [Google Scholar]
- 10.Suyash S, Jayesh S, Kamlesh S, Arun K, Sanjay B. Reverberations from our initial cases of MIS TLIF: Perilous fear of radiation exposure and recollection of our cuts and bruises. IP Indian J Neurosci. 2019;5:81–6. [Google Scholar]
- 11.Patel J, Kundnani V, Raut S, Meena M, Ruparel S. Perioperative complications of minimally invasive transforaminal lumbar interbody fusion (MI-TLIF): 10 years of experience with MI-TLIF. Global Spine J. 2021;11:733–9. doi: 10.1177/2192568220941460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Balasubramanian S, Sonone S, Dahapute A, Muni S, Gala R, Marathe N, et al. A comparative prospective study of clinical and radiological outcomes between open and minimally invasive transforaminal lumbar interbody fusion. Indian Spine J. 2019;2:138–45. [Google Scholar]
- 13.Subramanian N, Srikantha U, Sitabkhan M, Jagannatha AT, Khanapure K, Varma RG, et al. Minimally invasive vs. open transforaminal lumbar interbody fusion: Early outcome observations. J Spinal Surg. 2015;2:1–7. [Google Scholar]
- 14.Mehta RP, Patel AS, Jain S, Ruparel S, Kire N, Upadhyaya M, et al. Learning curve of MIS-TLIF using 22 mm-tubular retractor in degenerative spondylolisthesis (Grade 1-2) – A review over 100 cases. J Minim Invasive Spine Surg Tech. 2020;5:20–5. [Google Scholar]
- 15.Modi HN. Learning curve for minimally invasive spine surgeries: A review of initial 162 patients in five years of implementing MISS technique. J Minim Invasive Spine Surg Tech. 2020;5:43–50. [Google Scholar]
- 16.Parikh NP, Mistry M, Jhala AC. Effect of indirect neural decompression by minimally invasive oblique lumbar interbody fusion in adult degenerative lumbar spine disease and its limitations. J Minim Invasive Spine Surg Tech. 2019;4:5–13. [Google Scholar]
- 17.Sardhara J, Singh S, Mehrotra A, Bhaisora KS, Das KK, Srivastava AK, et al. Neuro-navigation assisted pre-psoas minimally invasive oblique lumbar interbody fusion (MI-OLIF): New roads and impediments. Neurol India. 2019;67:803–12. doi: 10.4103/0028-3886.263262. [DOI] [PubMed] [Google Scholar]
- 18.Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. United Kingdom (UK): John Wiley & Sons; 2019. Cochrane Handbook for Systematic Reviews of Interventions. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Weinstein JN, Lurie JD, Tosteson TD, Hanscom B, Tosteson AN, Blood EA, et al. Surgical versus nonsurgical treatment for lumbar degenerative spondylolisthesis. N Engl J Med. 2007;356:2257–70. doi: 10.1056/NEJMoa070302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Matz PG, Meagher RJ, Lamer T, Tontz WL Jr., Annaswamy TM, Cassidy RC, et al. Guideline summary review: An evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spondylolisthesis. Spine J. 2016;16:439–48. doi: 10.1016/j.spinee.2015.11.055. [DOI] [PubMed] [Google Scholar]
- 21.Chen YC, Zhang L, Li EN, Ding LX, Zhang GA, Hou Y, et al. An updated meta-analysis of clinical outcomes comparing minimally invasive with open transforaminal lumbar interbody fusion in patients with degenerative lumbar diseases. Medicine (Baltimore) 2019;98:e17420. doi: 10.1097/MD.0000000000017420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lu VM, Kerezoudis P, Gilder HE, McCutcheon BA, Phan K, Bydon M. Minimally invasive surgery versus open surgery spinal fusion for spondylolisthesis: A systematic review and meta-analysis. Spine (Phila Pa 1976) 2017;42:E177–85. doi: 10.1097/BRS.0000000000001731. [DOI] [PubMed] [Google Scholar]
- 23.Khan NR, Clark AJ, Lee SL, Venable GT, Rossi NB, Foley KT. Surgical outcomes for minimally invasive vs. open transforaminal lumbar interbody fusion: An updated systematic review and meta-analysis. Neurosurgery. 2015;77:847–74. doi: 10.1227/NEU.0000000000000913. [DOI] [PubMed] [Google Scholar]
- 24.Hammad A, Wirries A, Ardeshiri A, Nikiforov O, Geiger F. Open versus minimally invasive TLIF: Literature review and meta-analysis. J Orthop Surg Res. 2019;14:229. doi: 10.1186/s13018-019-1266-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Foley KT, Holly LT, Schwender JD. Minimally invasive lumbar fusion. Spine (Phila Pa 1976) 2003;28:S26–35. doi: 10.1097/01.BRS.0000076895.52418.5E. [DOI] [PubMed] [Google Scholar]
- 26.Silvestre C, Mac-Thiong JM, Hilmi R, Roussouly P. Complications and morbidities of mini-open anterior retroperitoneal lumbar interbody fusion: Oblique lumbar interbody fusion in 179 patients. Asian Spine J. 2012;6:89–97. doi: 10.4184/asj.2012.6.2.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lin GX, Akbary K, Kotheeranurak V, Quillo-Olvera J, Jo HJ, Yang XW, et al. clinical and radiologic outcomes of direct versus indirect decompression with lumbar interbody fusion: A matched-pair comparison analysis. World Neurosurg. 2018;119:e898–909. doi: 10.1016/j.wneu.2018.08.003. [DOI] [PubMed] [Google Scholar]
- 28.Mobbs RJ, Phan K, Malham G, Seex K, Rao PJ. Lumbar interbody fusion: Techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg. 2015;1:2–18. doi: 10.3978/j.issn.2414-469X.2015.10.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kim YH, Ha KY, Rhyu KW, Park HY, Cho CH, Kim HC, et al. Lumbar interbody fusion: Techniques, pearls and pitfalls. Asian Spine J. 2020;14:730–41. doi: 10.31616/asj.2020.0485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sharif S, Afsar A. Learning curve and minimally invasive spine surgery. World Neurosurg. 2018;119:472–8. doi: 10.1016/j.wneu.2018.06.094. [DOI] [PubMed] [Google Scholar]
- 31.Sclafani JA, Kim CW. Complications associated with the initial learning curve of minimally invasive spine surgery: A systematic review. Clin Orthop Relat Res. 2014;472:1711–7. doi: 10.1007/s11999-014-3495-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wang J, Zhou Y, Zhang ZF, Li CQ, Zheng WJ, Liu J. Comparison of one-level minimally invasive and open transforaminal lumbar interbody fusion in degenerative and isthmic spondylolisthesis grades 1 and 2. Eur Spine J. 2010;19:1780–4. doi: 10.1007/s00586-010-1404-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yu E, Khan SN. Does less invasive spine surgery result in increased radiation exposure? A systematic review. Clin Orthop Relat Res. 2014;472:1738–48. doi: 10.1007/s11999-014-3503-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Timothy J, Hanna SJ, Furtado N, Shanmuganathan M, Tyagi A. The use of titanium non-penetrating clips to close the spinal dura. Br J Neurosurg. 2007;21:268–71. doi: 10.1080/02688690701246210. [DOI] [PubMed] [Google Scholar]