Abstract
Background:
Telemedicine has emerged as an important tool in providing patient care during the COVID-19 pandemic. Hence, we aimed to study the clinico-epidemiological profile of patients seen in the teledermatology outpatient department (OPD) during the COVID-19 pandemic.
Material and Methods:
Retrospective data analysis of records of patients, who consulted in telemedicine OPD from 20 April 2020 to 5 Feb 2021 was done.
Results:
Out of 2524 patients registered for teledermatology consultation, 2117 completed the process of teleconsultation. The mean age of patients was 35.59 ± 15.60 years. There was a male preponderance with 1372 (64.81%) patients while females were 745 (35.19%). 1773 (83.75%) patients were managed on telemedicine alone and 344 (17.42%) patients required face to face physical consultation. The most common disorder was dermatophytosis seen in 316 (17.82%) followed by hair disorders like androgenetic alopecia and telogen effluvium in 239 (13.48%), acne in 238 (13.42%) and dermatitis in 196 (11.05%). Blood investigations were advised in 365 (17.24%) patients and skin biopsy was advised in 23 (1.09%) patients. The major causes for incomplete teleconsultation procedure were no response to telephone calls in 207 (8.2%), 76 (3.01%) patients had taken a prior consultation and 60 (2.37%) patients didn’t give consent for teleconsultation.
Conclusion:
Common dermatological diseases like tinea, acne, hair disorders and dermatitis can be managed on telemedicine alone. In India, there are fewer dermatologists per population, therefore telemedicine can be continued even after the pandemic is over in cases where diagnoses and treatment are straight forward.
Keywords: COVID-19 pandemic, teledermatology, telemedicine
Introduction
Telemedicine is a term coined in the 1970s, which means “healing at a distance”. The application of telemedicine in the context of dermatology is referred to as “teledermatology.” According to the WHO, global implementation rates of telemedicine services are highest for teleradiology (62%) followed by telepathology (41%) and teledermatology (38%).[1] Dermatology is a visual branch and hence suitable for telemedicine.[2] There is a paucity of data regarding the use of teledermatology services in India during the COVID-19 pandemic. Therefore we aim to study the clinico-epidemiological profile of patients seen in teledermatology OPD during the COVID-19 pandemic. We also wish to find how many patients we were able to manage on telemedicine alone and how many patients required face to face consultation.
Material and Methods
This was a retrospective observational study conducted at a tertiary care center in western India. Because of the nationwide lockdown announced on 25 March 2020, routine outpatient departments (OPDs) were non-functional however emergency services continued. Telemedicine OPD of the department of dermatology at our institute started w.e.f. 20 April 2020 and physical consultation started w.e.f. 15th June 2020. After clearance from the institute ethics committee (reference no. 2021/3524), retrospective data analysis of records of patients who consulted in telemedicine OPD of the department of dermatology at our institute was done w.e.f. 20 April 2020 to 5 Feb 2021.
WhatsApp, a smartphone-based application, is a popular and common mode of communication used worldwide.[3] It can send pictures, videos, text/voice messages and enables video calls, being a hybrid model of telemedicine, it was used as a mode of communication.
The patient initially takes online appointment on the institutional website. The registered patients were then telephonically called by the dermatologist and assessed whether the patient was suitable for teleconsultation or not. In 5 circumstances patients were called for physical consultation, a. uncertain diagnosis, b. dermatological disorders requiring systemic evaluation, c. dermatological emergencies, d. need of injectable drugs or e. diagnosis requiring confirmation by biopsy. The procedure used for providing telemedicine consultation has been depicted in Figure 1. Patients who completed this procedure were included in the analysis. Data regarding age, sex, a new case or follow up, patients treated on telemedicine alone, patients requiring face to face consultation, diagnoses of patients attending telemedicine OPD, blood investigations and any biopsy performed were entered in an excel sheet. Statistical analysis was performed using SPSS 21.0 software.
Figure 1.
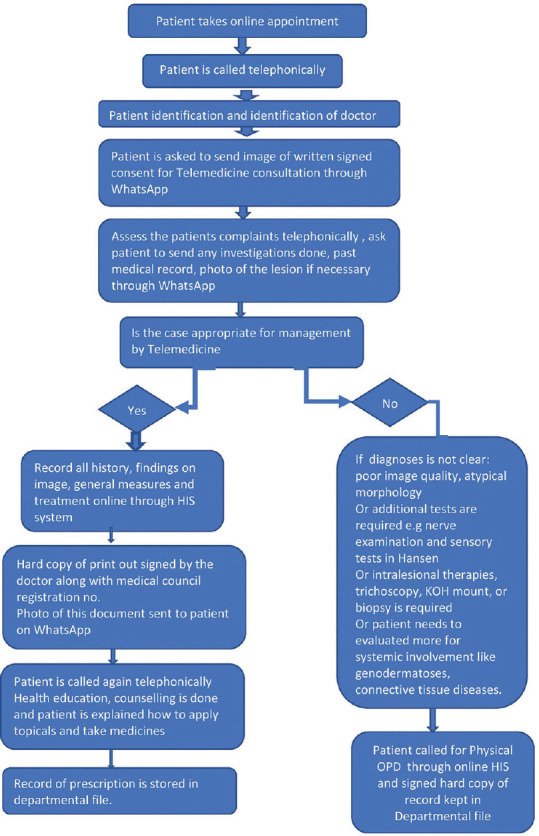
Flowchart showing the procedure of teledermatology consultation
Results
A total of 2524 patients were registered for teledermatology consultation, out of which 2117 patients completed the process of teleconsultation and were included in the analysis. The main reasons for not completing the teleconsultation procedure were not responding to telephone calls in 207 (8.2%), 76 (3.01%) patients had taken a prior consultation and 60 (2.37%) didn’t give consent for teleconsultation. Other reasons were patient’s phone was not reachable, patient doesn’t have WhatsApp, the patient was busy, has provided the wrong phone no. at the time of appointment etc. The remaining 2117 patients were then analyzed.
The mean age of patients was 35.59 ± 15.60 years (range - 2 months to 81 years). Most of the patients 655 (30.94%) were in the age group of 21-30 years followed by 51-60 years 589 (27.82%) [Figure 2]. The majority of patients were males i.e., 1372 (64.81%) while females were 745 (35.19%). Most of the patients were new cases i.e., 1420 (67.08%) and 697 (32.92%) were follow up cases. 1773 (83.75%) patients were managed on telemedicine alone and 344 (17.42%) required face to face physical consultation. Demographic details of the patients have been shown in Table 1.
Figure 2.
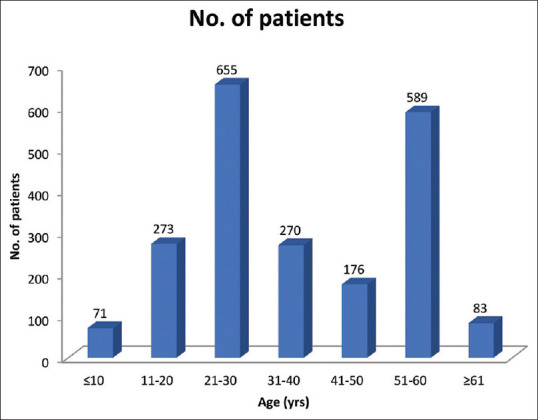
Age distribution of patients seen in teledermatology OPD
Table 1.
Demographic details of the study population
| Parameter | Values |
|---|---|
| Mean age (years) | 35.59±15.60 years (2 months to 81 years) |
| Males, n (%) | 1372 (64.81%) |
| Females, n (%) | 745 (35.19%) |
| New cases, n (%) | 1420 (67.08%) |
| Follow up cases, n (%) | 697 (32.92%) |
| Managed on telemedicine alone, n (%) | 1773 (83.75%) |
| Called for Physical OPD/Face to face consultation, n (%) | 344 (17.42%)* |
*Denominator is 1975 (2117-142); 142 patients were excluded for calculating percentage for this parameter because Physical OPD started after 15th June 2020. Because of lockdown restrictions, there was no facility for physical consultation between 20th April and 14th June 2020.
Various dermatoses which were managed on telemedicine alone were shown in Table 2. Out of 1773 patients who were managed on telemedicine alone, the most common disorder was dermatophytosis seen in 316 (17.82%) followed by hair disorders like androgenetic alopecia and telogen effluvium which were seen in 239 (13.48%), acne in 238 (13.42%) and dermatitis in 196 (11.05%). Clinical images of a few such patients who were managed on telemedicine alone were shown in Figure 3. Out of 2117 patients seen in telemedicine OPD, blood investigations were advised in 365 (17.24%) patients and skin biopsy was advised in 23 (1.09%) patients. Skin biopsies were performed after physical consultation. Various diseases for which biopsy was advised were pemphigus vulgaris, erosive lichen planus, cutaneous leishmaniasis, eumycetoma, panniculitis, bullous lupus erythematosus, urticarial vasculitis etc.
Table 2.
Pattern of dermatological diseases which were managed on telemedicine alone
| DIAGNOSES | No. of patients | Percentage (%) |
|---|---|---|
| Tinea | 316 | 17.82 |
| Hair disorders | 239 | 13.48 |
| Acne and acne scars | 238 | 13.42 |
| Dermatitis | 196 | 11.05 |
| Pruritus or Urticaria | 125 | 7.05 |
| Papulosquamous disorders | 114 | 6.43 |
| Vitiligo | 72 | 4.06 |
| Pigmentary disorders other than vitiligo | 70 | 3.95 |
| Scabies | 59 | 3.33 |
| Immunobullous diseases | 38 | 2.14 |
| Fungal infections other than Tinea | 37 | 2.09 |
| Bacterial infection | 32 | 1.80 |
| Viral infection | 29 | 1.64 |
| Genital diseases | 23 | 1.30 |
| Connective tissue disease | 11 | 0.62 |
| Benign nodules | 8 | 0.45 |
| Hansen’s disease | 4 | 0.23 |
| Pediculosis capitis | 1 | 0.05 |
| Miscellaneous | 140 | 7.90 |
| Doubtful (only symptomatic treatment given) | 17 | 0.96 |
| Not mentioned | 4 | 0.23 |
| TOTAL | 1773 | 100 |
Figure 3.

Clinical photographs of patients seen in teledermatology OPD: (a) Tinea corporis, (b) Scabietic nodule, (c) Polymorphic light eruption, (d) Psoriasis vulgaris
Discussion
Teledermatology was initially started to address the need of shortage of dermatologists, however during the current pandemic it has become a necessity in providing patient care as it ensures social distancing. Several studies have shown teledermatology good in terms of diagnosis, treatment accuracy as well as cost-effectiveness.[4] Teledermatology helps us in overcoming the barriers of lockdown, distance and also helps in follow up of patients with chronic skin diseases by improving adherence to treatment and improving quality of life.[5,6,7]
Krueger et al.[8] retrospectively compared the trends seen in teledermatology and in-person visits. They found that patients in the teledermatology cohort were younger with a mean age of 41 years. In a study from Spain mean age of patients was 42 years, and 62% were women.[9] In the present study too the mean age was 35 years. However, males were more than females, accounting for 64.81% of patients. The predominance of males may be due to increased access to mobiles and the internet to males in comparison to females. Additionally, there may be an inherent hesitation in taking and sending photographs of diseased skin or seeking help in doing so in females.
In a study from India, there was a three-fold increase in teledermatology consultations during the pandemic when compared to before the pandemic. In their study before the pandemic, most of the patients seen in teldermatology were follow-up cases while now during the pandemic it was both new and follow up cases (63.2%).[10] Similar observation was made in our study where the majority of cases were new cases (67.08%) and follow up cases were 32.92%. This shows how the teledermatology has emerged during the COVID-19 pandemic as an important mode for delivery of dermatology related health care services.
In a study from Spain, which used a hybrid model of teledermatology, a diagnosis could be made in 87.1% of patients. In contrast, the diagnosis was not possible in 12.8% of cases for the following reasons: the image was not consistent with the consultation, image quality was poor, and requirement of additional testing.[9] Similar observations were noted in our study where we were able to manage 83.75% of patients on telemedicine alone and only 17.42% of patients required in-person visits.
Krueger et al.[8] found that in the teledermatology group inflammatory dermatoses (49%) like acne, rosacea, eczemas, psoriasis etc., and hair disorders (4.8%) were the main group of disorders whereas skin cancer and other neoplastic disorders (21%) were less frequently encountered. Su et al.[11] and Asabor et al.[12] observed that dermatologists were easily comfortable in managing common dermatoses like acne, rosacea, psoriasis, atopic dermatitis, and eczema via teledermatology even when the in-person evaluation was an option. In a survey done in India, disorders that were easily diagnosed in teledermatology included acne, followed closely by tinea, alopecia, bacterial infections, eczema, viral infections and pigmentary disorders.[13] Similar findings were noted in the present study where the most common disorder was dermatophytosis followed by hair disorders like androgenetic alopecia and telogen effluvium, acne and dermatitis.
Skin biopsy was advised in 1.09% of patients. In a web-based global survey, one-quarter of participants were performing procedures among which biopsy was the most common procedure.[14]
In a study from northern India, different barriers to a successful teleconsultation were duplicate entries (3.01%), incorrect contact details (2.91%), connectivity issues (7.06%) and technological inability of the patient to send pictures (5.79%).[15] However in the present study main reasons for not completing the teleconsultation procedure were patients not responding to telephone calls in 8.2%, the patient had taken a prior consultation (3.01%) and 2.37% didn’t give consent for teleconsultation which could likely be due to hesitation in sending photographs or poor understanding of the hybrid model.
The different problems faced during telemedicine consultation along with their possible solutions have been depicted in Table 3.
Table 3.
Problems encountered during Teleconsultation and possible solutions
| Problem | Solution |
|---|---|
| Image quality is poor | Instruction leaflet can be provided at the time of booking for online appointment for capturing good quality images. |
| Image should be clicked parallel to the skin lesion; background should be clear to avoid any distractions. | |
| Image should be clicked at a distance first so that anatomical area can be recognized followed by close up photo without blurring the image. | |
| Patient don't pick up the call | Reminder through message can be given one day before specifying the timing of scheduled appointment |
| Difficulty in clicking the image as patient is outdoors while teleconsultation | At the time of online booking of appointment instruction leaflet can be provided to click the images one day before the scheduled date of appointment. |
| Privacy and security issue | Using reliable platforms with end.to.end encryption. |
| Confirming identity of both patient and doctor. | |
| Hesitancy in sending images of genital lesions | Patient can be called for face.to.face consultation. |
| Some care cannot be provided remotely such as full body examinations, procedures/Sometimes images may be inadequate for teledermatology evaluations | Instruction leaflet should contain a disclaimer that patient may be needed to be seen physically in case necessary. |
| Illiterate patients and patients not having multimedia cell phones | During the time of telemedicine booking patient must be advised that images will be required and patient may be required to make arrangements for the same. |
| Patients having hesitancy to reveal sexual history and contacts due to privacy in telemedicine | Such patients should be counselled and a rapport must be established among the patients and if necessary, should be called for history taking and physical evaluation. |
| Few patients are not satisfied and urge on physical appointment. | Proper counselling is required for the patient and patient must be given each and every information required and must be asked for any questions from their side. If the patient isn't satisfied then the patient can be called for a physical appointment. |
| Hesitancy of females in sending images due to improper information about who has access to the photos. | Patients should be properly informed that who will have access, and how the information will be stored. |
| Overdiagnosis/Underdiagnosis | Image quality should be improved, in case of any doubt in diagnosis proper detailed history should be taken and patient can be called physically |
| Internet connectivity | Connectivity should be improved on both sides i.e., patient as well as provider for faster and smoother communication |
| Patients not understanding treatment advices | Each and every drug should be explained in detail and the duration up to which the drug has to be applied should be informed. Special care should be taken for immunosuppressives. |
Even though there are certain drawbacks, teledermatology served as a useful tool in patient management during this pandemic. We propose an algorithm for telemedicine consultation which can help dermatologists in routine practice [Figure 4].
Figure 4.
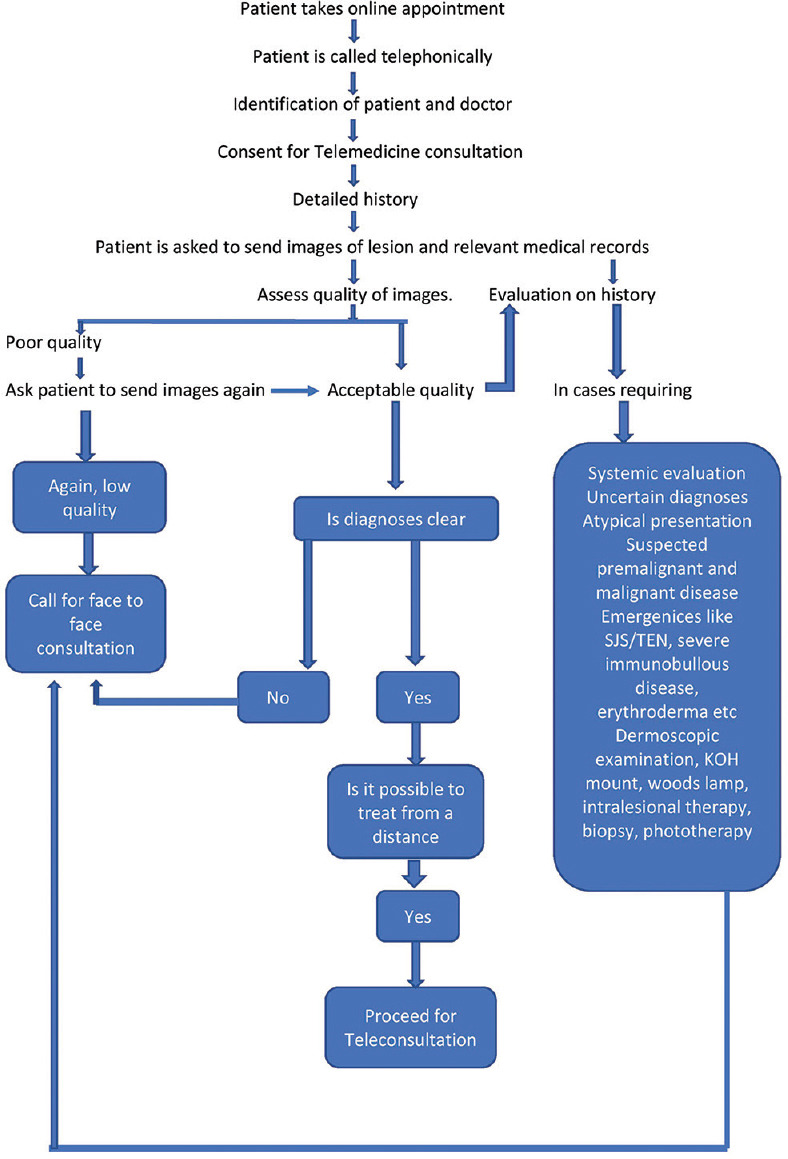
Proposed algorithm for teledermatology consultation (Hybrid model)
Conclusion
Dermatology being a visual branch helps in managing the majority of patients on telemedicine alone. Common dermatological diseases like tinea, acne, hair disorders and dermatitis can be managed on telemedicine alone. In India, there are fewer dermatologists per population, this emphasizes the importance of teledermatology especially for remote areas. Telemedicine can be continued even after the pandemic is over in cases where diagnoses and treatment are easy.
Limitation
The limitation of the study is retrospective study design. Diagnoses of patients who were called for physical consultation were not recorded. The level of satisfaction for teledermatology services among dermatologists and patients was not assessed.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Telemedicine:Opportunities and developments in member states:Report on the second Global survey on eHealth, World Health Organization 2010. [[Last accessed on 2022 Jan 24]]. Available from: https://www.who.int/goe/publications/goe_telemedicine_2010.pdf .
- 2.Ashique KT, Kaliyadan F. Teledermatology in the wake of COVID-19 Scenario:An Indian perspective. Indian Dermatol Online J. 2020;11:301–6. doi: 10.4103/idoj.IDOJ_260_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jakhar D, Kaul S, Kaur I. WhatsApp messenger as a teledermatology tool during coronavirus disease (COVID-19):From bedside to phone-side. Clin Exp Dermatol. 2020;45:739–40. doi: 10.1111/ced.14227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee JJ, English JC., 3rd Teledermatology:A review and update. Am J Clin Dermatol. 2018;19:253–60. doi: 10.1007/s40257-017-0317-6. [DOI] [PubMed] [Google Scholar]
- 5.Brunasso AMG, Massone C. Teledermatologic monitoring for chronic cutaneous autoimmune diseases with smartworking during COVID-19 emergency in a tertiary center in Italy. Dermatol Ther. 2020;33:e13495. doi: 10.1111/dth.13695. doi:10.1111/dth. 13695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Villani A, Megna M, Scalvenzi M, Fabbrocini G, Ruggiero A. Teledermatology and chronic skin diseases:Real life experience in a Southern Italian Dermatologic Centre. Dermatol Ther. 2020;33:e13839. doi: 10.1111/dth.13839. doi:10.1111/dth. 13839. [DOI] [PubMed] [Google Scholar]
- 7.Marasca C, Ruggiero A, Fontanella G, Ferrillo M, Fabbrocini G, Villani A. Telemedicine and support groups could be used to improve adherence to treatment and health-related quality of life in patients affected by inflammatory skin conditions during the COVID-19 pandemic. Clin Exp Dermatol. 2020;45:749. doi: 10.1111/ced.14245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Krueger S, Leonard N, Modest N, Flahive J, Guilarte-Walker Y, Rashighi M, et al. Identifying trends in patient characteristics and visit details during the transition to teledermatology:Experience at a single tertiary referral center. J Am Acad Dermatol. 2021;85:1592–4. doi: 10.1016/j.jaad.2020.11.040. [DOI] [PubMed] [Google Scholar]
- 9.Sendagorta E, Servera G, Nuno A, Gil R, Perez-Espana L, Herranz P. Direct-to-patient teledermatology during COVID-19 lockdown in a health District in Madrid, Spain:The EVIDE-19 pilot study. Actas Dermosifiliogr (Engl Ed) 2021;112:345–53. doi: 10.1016/j.ad.2020.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bhargava S, Sarkar R. Impact of COVID-19 pandemic on dermatology practice in India. Indian Dermatol Online J. 2020;11:712–9. doi: 10.4103/idoj.IDOJ_240_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Su MY, Smith GP, Das S. Trends in teledermatology use during clinic reopening after COVID-19 closures. J Am Acad Dermatol. 2021;84:e213–4. doi: 10.1016/j.jaad.2020.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Asabor EN, Bunick CG, Cohen JM, Perkins SH. Patient and physician perspectives on teledermatology at an academic dermatology department amid the COVID-19 pandemic. J Am Acad Dermatol. 2021;84:158–61. doi: 10.1016/j.jaad.2020.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sharma A, Jindal V, Singla P, Goldust M, Mhatre M. Will teledermatology be the silver lining during and after COVID-19? Dermatol Ther. 2020;33:e13643. doi: 10.1111/dth.13643. doi:10.1111/dth. 13643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bhargava S, McKeever C, Kroumpouzos G. Impact of COVID-19 pandemic on dermatology practices:Results of a web-based, global survey. Int J Womens Dermatol. 2021;7:217–23. doi: 10.1016/j.ijwd.2020.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Handa S, Mehta H, Bishnoi A, Vinay K, Mahajan R, Narang T, et al. Teledermatology during the COVID-19 pandemic:Experience at a tertiary care centre in North India. Dermatol Ther. 2021;34:e15022. doi: 10.1111/dth.15022. doi:10.1111/dth. 15022. [DOI] [PMC free article] [PubMed] [Google Scholar]


