Abstract
Social vulnerability refers to the attributes of society that make people and places susceptible to natural disasters, adverse health outcomes, and social inequalities. Using a social vulnerability index (SVI), we investigated social vulnerability prevalence and its relationship with food insecurity in South Africa (SA). In this nationally representative cross-sectional survey, we calculated SVI scores from 3402 respondents (median age, 35 (26–46) years) using an SVI developed by the United States (US) Centers for Disease Control and prevention (CDC) adapted for a South African context. We measured food insecurity using a modified Community Childhood Hunger Identification Project. Findings classified 20.6% and 20.4% of adults as socially vulnerable and food insecure, respectively. The risk of food insecurity was almost threefold higher in the social vulnerability group (OR 2.76, 95% CI 2.76–2.77, p < 0.001) compared to their counterparts. The SVI could be a useful tool to guide government and policymakers in the facilitation of social relief initiatives for those most vulnerable.
Keywords: Social vulnerability, Food insecurity, South Africa, Women, Men, Inequality
Key messages
South Africa’s socially vulnerable groups (those with fewer resources, unemployed, and without high school certificate) are at a greater risk of experiencing food insecurity.
The South African government needs effective and innovative policies to reform the economy and invest in a decent education system so that social inequalities such as social vulnerability and food insecurity can be reduced or eliminated.
Introduction
South Africa (SA) is now the most unequal country in the world, with a Gini coefficient of 0.63 [1, 2]. This inequality is due largely to its history of exclusion and discrimination on race and gender, and lack of economic growth in recent years [2]. The impact of the COVID-19 pandemic on the country’s economy has further exacerbated this inequality [3, 4]. In SA, Black African and Colored households typically have higher levels of poverty than White and Asian and Indian households [5]. Female-headed households experience higher levels of poverty compared to male-headed households, partly due to the higher unemployment rates for women compared to men (37.3% vs 32.9%) [5, 6]. Poverty is intricately linked to food insecurity. Accordingly, the percentage of households in SA with inadequate or severely inadequate access to food increased from 18.8% in 2019 to 20.6% in 2020 [7]. Like poverty patterns, Black Africans and Coloreds, female-headed households, and households in rural areas are more likely to experience food insecurity than their counterparts [8–10]. In South Africa, poverty and food insecurity may also predispose individuals to other inequalities including increased risk for infectious diseases, gender-based violence (GBV), and substance abuse. This may partly explain why SA has one of the highest rates of HIV and GBV against women, and why physical assaults or violent crimes are committed mostly by men [5, 11, 12]. Despite these social inequalities having been well documented in SA [5, 8, 11, 13], nationally representative studies examining social vulnerability and its association to adverse social outcomes such as food insecurity are scarce [8, 11]. This limits our understanding of underlying causes of social inequalities and their detrimental effects on human development in different contexts. A better understanding of social inequalities at a national level and of how these inequalities vary across socio-economic, demographic, and geographical factors might help government officials to implement evidence-based social relief strategies to yield optimal results in curbing social inequalities in vulnerable groups.
Researchers assess social vulnerability using multiple indices such as the social vulnerability index (SVI) which includes a series of social, economic, and environmental indicators (social attributes) that make a community or individual vulnerable to natural disasters (14, 15). Since its development, researchers have adopted the SVI to describe social vulnerability to other public health threats, including the COVID-19 pandemic [16], food insecurity [13], obesity [17], and physical fitness [18]. Recently, we showed that young Black African women from a historically disadvantaged township in SA, characterized as socially vulnerable, were almost 3 times more likely to report household food insecurity [13]. To examine if this was the case more broadly in SA, our aim was two-fold: (i) to characterize social vulnerability in the South African population using a national representative sample with a broad spectrum of socio-demographic variables; and (ii) to investigate the associations between SVI and household food insecurity.
Material and methods
Study design
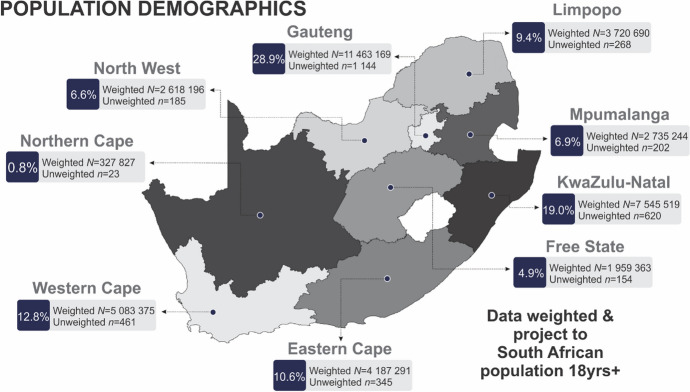
An international market research and public opinion polling company (https://www.ipsos.com) conducted this cross-sectional study in October 2021 with 3402 participants across nine provinces of SA (Fig. 1).
Fig. 1.
Population demographics outlining the nine provinces of South Africa in which the survey was conducted. The recruited sample size of 3402 corresponds to 39,640,674 weighted sample
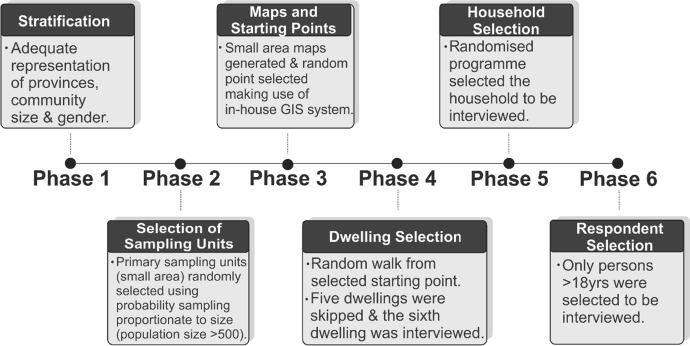
The surveyor-based participant recruitment on a six-phase stratification random probability sampling method is described in detail in Fig. 2. Ipsos used a random iterative method to weight the data to represent a South African population of 18 years and older. This technique follows a process in which researchers weight the sample iteratively to each target variable (such as age, gender, race, area, and home language), with one set of weights used as inputs for the next. The adjustments continue until every variable is consistent with the population values from which the surveyors drew the sample. For this survey, they excluded respondents younger than 18 years of age from participation.
Fig. 2.
A six-phase stratification random probability sampling method used for sample selection. GIS geographic information system
Materials
We administered a national demographic questionnaire through Ipsos, written in English, in the participant’s language of choice (English, IsiXhosa, IsiZulu) and included measures of socio-economic status (SES) such as household asset index, employment, and education. We measured household food insecurity using the adapted Community Childhood Hunger Identification Project (CCHIP) [19, 20]. We used only the following three CCHIP questions to compute a food insecurity score (score of 1 was given for each “Yes” response) [20]: (1) ‘Does your household ever run out of money to buy food?’; (2) ‘Do you ever cut the size of meals or skip meals because there is not enough money for food?’ or; (3) ‘Do you or any of your children ever go to bed hungry because there is not enough money to buy food?’. We classified those who responded with “No” to all three questions (score = 0) or “Yes” to only one of the three questions (score = 1) as “Food secure.” In contrast, we classified respondents who answered “Yes” to two or three questions (score = 2 or 3) as “Food Insecure.” Because the study design called for interviewing an adult household member, we focused on household food insecurity and did not specifically investigate child malnutrition. The adult being interviewed may not have had sufficient information about household children, given multiple family and non-family members living together.
The Human Research Ethics Committee (Medical) of the University of the Witwatersrand (H21/06/36) approved the study. They study team fully informed participants about the objectives of the survey and provided written informed consent before their inclusion in the study.
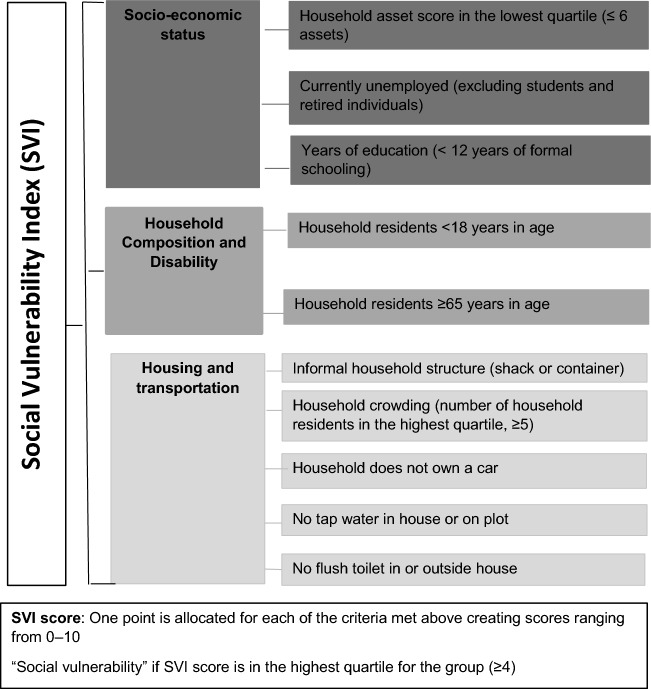
Social vulnerability index (SVI)
We adapted the SVI score previously used by the United States Centers of Disease Control and Prevention (CDC) [15, 21] and calculated SVI score values for each respondent across three domains: SES, household composition and disability, and housing and transportation (Fig. 3). We did not include the minority and language domain as SA is predominately Black African (80.9%) and has 11 official languages [22]. Previous studies have provided detailed descriptions of the domains [15, 21]. Briefly, SES includes factors that affect an individual or community’s ability to respond to hazards including resources (poverty or wealth), employment, and education. We used a household asset score from a list of 21 assets (including refrigerator, stove, washing machine, TV, and telephone) as an indicator of resource level. We based this score on standard measures used in the Demographic and Health Surveys household questionnaire (www.measuredhs.com) extensively used in this setting [23, 24]. We defined a household with an asset score in the lowest quartile (≤ 6) as socially vulnerable. We recorded unemployment for participants not currently working and excluded those who were studying or retired. We also classified those with less than 12 years of formal education (no high school certificate) as more vulnerable. The household composition and disability domain refers to household residents most likely to need assistance in the event of a disaster, including individuals in vulnerable age groups (< 18 or ≥ 65 years). This survey did not include disability or government disability support. For the housing and transportation domain, we characterized as more vulnerable the households with informal housing structures (shacks or containers), crowded (number of household residents in the highest quartile, ≥ 5), lacking sanitation facilities (no tap water and flush toilet in the house or yard), and without vehicle access. We measured household crowding using only the number of residents in the household because the survey included no data on number of rooms for sleeping.
Fig. 3.
Social vulnerability domains and indicators used in this study
Statistical analysis
Where applicable, we tested data for normality using distribution plots. We conducted all descriptive and logistic regression analyses using weighted data to represent a South African population of 18 years and older. We present results as frequencies (%) or non-parametric statistics, such as median and interquartile range (IQR). We performed in separate univariate models, logistic regression analyses to determine whether SVI indicators (all dichotomous exposures), SVI (a continuous exposure), and “social vulnerability” (SVI score ≥ 4) (a dichotomous exposure) predicted the likelihood of being food insecure compared with remaining food secure group as a reference. We included all ten SVI indicators in one multivariate regression model to test the predictive effect of each social vulnerability indicator while adjusting for the other nine indicators. We conducted all data analyses using Stata® (Version 17.0, StataCorp, College Station, TX, USA).
Results
Social vulnerability and food insecurity in the South African population
Table 1 reports descriptive statistics of the South African population according to social vulnerability characteristics and food insecurity status. About 31.3% of the respondents had a vulnerable household asset score (≤ 6 assets), 27.6% were unemployed, and 23.5% had less than 12 years of formal schooling (did not complete high school). Approximately, 44.2% of the households included residents less than 18 years of age, and only 8.8% had residents 65 years and older. Only 5.3% and 15.6% of the respondents lived in informal housing structures and crowded households, respectively. About 34.8% of the households did not own a vehicle and 38.9% of the households did not have sanitation facilities (tap water or toilet).
Table 1.
Social vulnerability and food insecurity characteristics in the South African population
| Domains | Social vulnerability indicators | Median (IQR) | National prevalence (%) |
|---|---|---|---|
| Socio-economic status | Household asset scorea in the lowest quartile (≤ 6 assets) | 4 (3–5) | 31.3 |
| Currently unemployed (excluding students and retired individuals) | 27.6 | ||
| Years of education (< 12 years of formal schooling) | 23.5 | ||
| Household composition and disability | Vulnerable ages (household residents < 18 years in age) | 44.2 | |
| Vulnerable ages (household residents ≥ 65 years in age) | 8.8 | ||
| Housing and transportation | Informal household structure (shack or container) | 5.3 | |
| Household crowdingb (number of household residents in the highest quartile, ≥ 5) | 5 (5–6) | 15.6 | |
| Household does not own a car | 34.8 | ||
| No tap water in house or on plot | 13.5 | ||
| No flush toilet in the house or outside | 25.4 | ||
| Total SVI score and SVI groups | |||
| Total SVI score | 2 (1–3) | ||
| SVI score ≥ 4 (Socially vulnerable group) | 4 (4–5) | 20.6 | |
| SVI score < 4 | 2 (1–2) | 79.4 | |
| Food insecurity groups | |||
| Food secure | 79.6 | ||
| Food insecure | 20.4 | ||
| Social vulnerability prevalence by food insecurity groups | |||
| Food secure | 16.7 | ||
| Food insecure | 35.6 |
aThe median (IQR) of the household asset score for the entire population is 9 (6–12)
bThe median (IQR) of the household crowding score for the sample is 3 (2–4)
The prevalence of social vulnerability (SVI score ≥ 4, 20.6%) and food insecurity (20.4%) in Table 1 was comparable. Respondents who were food insecure (35.6%) had higher social vulnerability prevalence than those who were not food insecure (14.1%) (Table 1).
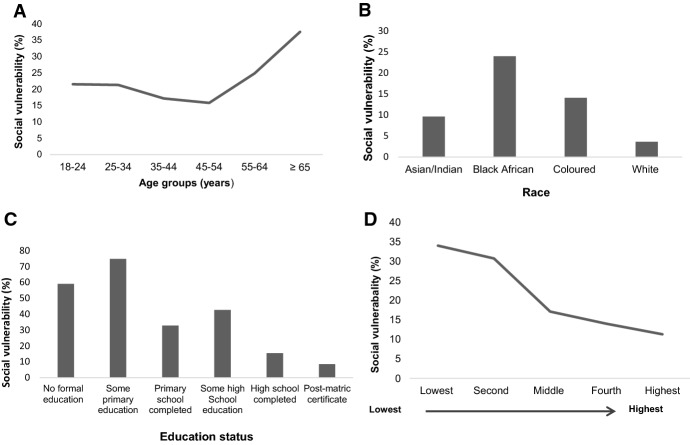
The prevalence of social vulnerability by province, community size, age groups, race, education attainment, and household monthly income appear in Figs. 4 and 5. Social vulnerability was more prevalent in Mpumalanga (41.4%) and KwaZulu-Natal (31.1%); the Northern Cape (0.0%) and North West (1.9%) provinces had the lowest rates (Fig. 4A). Social vulnerability prevalence was highest in rural areas (36.8%) (Fig. 4B).
Fig. 4.
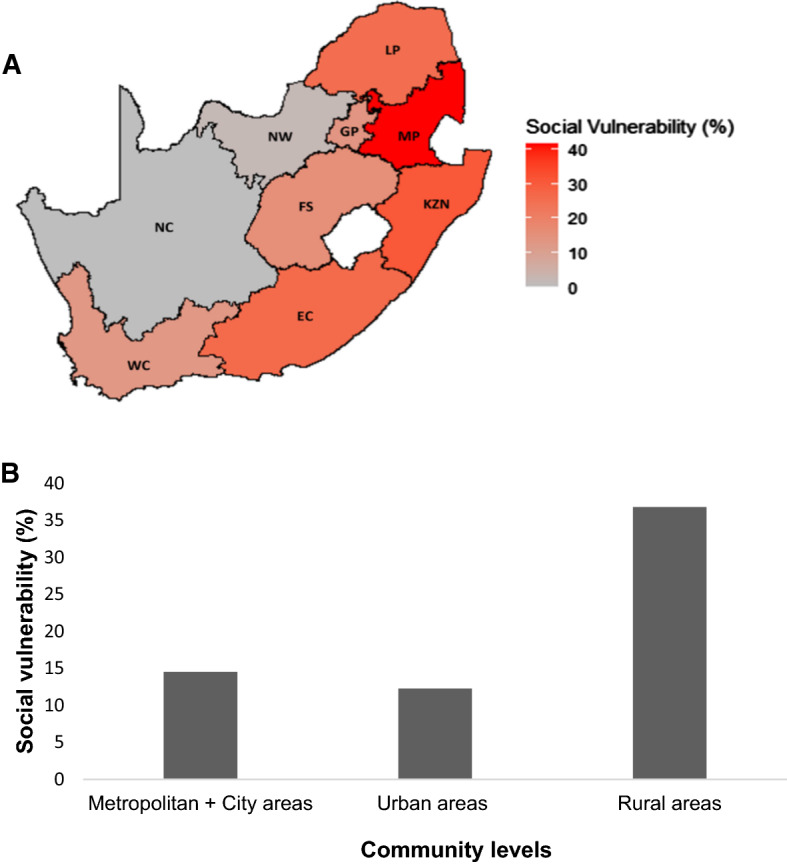
Distribution of social vulnerability (%) at provincial (A) and community (B) level. EC Eastern Cape, FS Free State, GP Gauteng Province, KZN KwaZulu-Natal, LP Limpopo Province, MP Mpumalanga, NW North West, NC Northern Cape, WC Western Cape
Fig. 5.
Social vulnerability prevalence (%) by age groups (A), race (B), education (C), and household monthly income quintiles (D)
Those 65 years and older were more socially vulnerable (37.6%) than their younger counterparts (Fig. 5A). By race, Black Africans had the highest level of social vulnerability (24.0%); only 3.6% of White South Africans were characterized as socially vulnerable (Fig. 5B). Respondents with 12 or more years of schooling had low levels of social vulnerability (15.6% and 8.6%) (Fig. 5C). Social vulnerability decreased with increasing household monthly income. Social vulnerability prevalence was highest in households with the lowest (34.0%) and second lowest (30.7%) income quintiles (Fig. 5D). Unemployed respondents (42.8%) had higher social vulnerability prevalence than their employed counterparts (10.1%) (data not presented). Compared to males, females had higher levels of social vulnerability (23.5% vs. 17.4%) (data not shown).
Logistic regression for the prediction of food insecurity
The estimated odds ratios (ORs) of social vulnerability indicators (assessed in ten univariate analyses and one multivariate analysis), SVI score and social vulnerability (SVI score ≥ 4) in predicting food insecurity appear in Table 2. The majority of social vulnerability indicators were significantly associated with increased risk for food insecurity. Households without a vehicle, however, were associated with a 79% (univariate analysis) and 69% (multivariate analysis) decrease in the relative log odds of being food insecure compared to households that owned a vehicle. In contrast, households without a flush toilet were 45% more likely to be food insecure. However, after adjusting for another nine indicators (multivariate analysis), households without a flush toilet were 40% less likely to experience food insecurity. SES indicators proved most salient as predictors of food insecurity. Overall, a one-unit change in social vulnerability was associated with a 39% increase in the relative log odds of being food insecure compared to food secure. Those who were socially vulnerable were 2.76 times at greater risk of food insecurity than those who were not socially vulnerable (Table 2).
Table 2.
Logistic regression predicting likelihood of food insecurity based on social vulnerability characteristics
| Univariate models | Multivariate model | |
|---|---|---|
| OR (95% CI)* | OR (95% CI)* | |
| Social vulnerability indicators | ||
| Socio-economic status | ||
| Household asset score in the lowest quartile (≤ 6 assets) | 2.62 (2.61–2.62) | 2.14 (2.13–2.14) |
| Currently unemployed (excluding students and retired individuals) | 3.43 (3.43–3.44) | 2.53 (2.53–2.53) |
| Years of education (< 12 years of formal schooling) | 2.97 (2.97–2.98) | 1.99 (1.99–1.99) |
| Household composition and disability | ||
| Vulnerable ages (Household residents < 18 years in age) | 1.55 (1.55–1.56) | 1.31 (1.31–1.31) |
| Vulnerable ages (Household residents ≥ 65 years in age) | 1.21 (1.21–1.21) | 1.20 (1.20–1.20) |
| Housing and transportation | ||
| Informal household structure (shack or container) | 2.10 (2.09–2.10) | 1.24 (1.24–1.24) |
| Household crowding (Number of household residents in the highest quartile, ≥ 5) | 1.51 (1.51–1.51) | 1.23 (1.23–1.23) |
| Household does not own a car | 0.21 (0.21–0.21) | 0.31 (0.31–0.31) |
| No tap water in house or on plot | 1.70 (1.70–1.70) | 1.05 (1.05–1.05) |
| No flush toilet in the house or outside | 1.45 (1.44–1.45) | 0.60 (0.60–0.60) |
| Social vulnerability | ||
| Total SVI score | 1.39 (1.39–1.39) | |
| Social vulnerability (SVI score ≥ 4) | 2.76 (2.76–2.77) |
SVI - social vulnerability index
*p < 0.001 for all the models
Discussion
We aimed to investigate the prevalence of social vulnerability and its association with food insecurity in SA. To our knowledge, this is the first study to measure social vulnerability using SVI in a nationally representative sample (weighted data representing approximately 39.6 million households) with key socio-economic, demographic, and geographical factors; and to compare social vulnerability prevalence among these factors. Our main findings identified 20.6% of the South African population as socially vulnerable and 20.4% of households as having experienced food insecurity in October 2021 during level 1 COVID-19 lockdown (lowest enforced level of infection control restrictions). We showed that SVI was associated with a 40.0% increased risk for food insecurity and the risk of food insecurity was almost threefold higher in the socially vulnerable group compared to their counterparts.
The finding that the prevalence of social vulnerability was higher in vulnerable groups (rural areas, older persons, Black African, without high school certificate, and low income, and female) corresponds with the vulnerable groups typically identified in existing literature [8, 10, 25]. We did, however, find some notable differences from previously reported regions of vulnerability [8, 10, 25]. Our data suggest that Mpumalanga was the most vulnerable province even though Eastern Cape, KwaZulu-Natal, and Limpopo are the three provinces with the largest rural populations, many of whom are unemployed, living in poverty, and experiencing chronic food insecurity [8, 10, 25]. These discrepancies might be explained by the dynamic nature of social vulnerability, that is susceptible to changes during and following a public health threat such as COVID-19. As observed in most countries, the pandemic also led to an economic decline and higher unemployment rates in SA [3, 26, 27]. This exacerbated poverty and subsequently widened the gap in social inequalities [3, 26, 27]. Therefore, it is possible that Mpumalanga might have been disproportionately affected by the pandemic. To our knowledge, there are no studies to substantiate these claims.
Compared to their urban counterparts, rural areas are disproportionally less developed with poorly maintained infrastructure that deprives people of employment opportunities, basic services, and good quality education [8, 10, 25]. Although poverty is lower in urban areas than in rural areas [10], the rapid increase in urban population growth coupled with overcrowding caused by unplanned and informal built environments [28], and poor sanitation facilities increase vulnerability to multiple hazards. These hazards can cause serious public health threats (including infectious diseases, food insecurity, and pollution). Indeed, households without sanitation facilities are at greater risk of developing infectious diseases [29], that might result in medical expenses. Paying for medical care could decrease household food expenditure and dietary diversity. Accordingly, we showed an association between households without sanitation facilities and increased exposure to food insecurity. The unexpected change of direction in the association between a lack of toilet facility and food insecurity after adjusting for other social vulnerability indicators requires further investigation. The inverse association between lack of vehicle access and food insecurity might be indirectly linked to costs associated with vehicle ownership (such as monthly installments to purchase or lease, maintenance, and fuel), rather than the use of vehicle to access food as previously reported [30]. Within South Africa, these costs might reduce food quality and quantity. Future studies are needed to test these claims.
The gender differences in social vulnerability could be attributed to employment disparities [6], family care responsibilities (it is females who often have to care for the sick and elderly), and due to female-headed households usually having more dependents or vulnerable groups (such as children and adult females), or both [8, 9, 25]. This may partly explain why females or female-headed households with fewer resources are at higher risk of food insecurity compared to their counterparts [8, 9, 13, 25]. Social vulnerability was highest in those 65 years and older. The finding that social vulnerability increases exponentially from 45 to 54 years of age corroborates previous reports in U.S [31] and European [32] populations. Although the exact mechanisms underlying this phenomenon are not fully understood, these findings have policy implications in SA (described below).
The 20.4% prevalence of food insecurity reported in the current study corresponds to the 20.6% prevalence previously reported during the 2020 General Household Survey [7]. However, it differs from the 35.0% household food insecurity prevalence reported by National Income Dynamics Study (NIDS)-Coronavirus Rapid Mobile Survey (CRAM) during the 5th wave of the COVID-19 pandemic (April–May 2021) [9]. Even when we used the same question used by NIDS-CRAM (proportion of households who had run out of money to buy food in the previous 30 days) and compared our results again, the prevalence of food insecurity in our study remained lower (18%) [9]. Therefore, we postulate that the dynamic nature of food insecurity might be a key contributing factor for the discrepancies in food insecurity rates. Findings from the NIDS-CRAM showed that food insecurity declined from 47.0% in wave 1 to 38.0% in wave 2, but, increased again during wave 3 (41%), and remained consistent during wave 4 (39.0%) and wave 5 (35.0%) [9]. Also, variations in food insecurity, dietary patterns or eating behaviors, might also be attributed to environmental and societal changes associated with development or lack of supportive policies from various sectors of the food system (such as agriculture, urban planning, and food industries).
South Africa has implemented several policies addressing production, access, and use of food, including nutritional content, to ease poverty and food insecurity [33]. Boatemma et al. review these policies in detail [33]. Some of the major policies on food availability include the “Zero Vat Rating of Basic Foodstuffs” (1994 and reviewed in 2018) [34], in which nineteen staple food items (such as brown bread, rice, and fruit and vegetables) are exempted from taxation. In 2004, the Department of Social Development (DSD) implemented the “Social Assistance Act” to provide social assistance and cash payments as social grants to vulnerable groups [35]. There are four main types of grants: family and children, old age, social protection (social relief of distress grants, SRDG), and a disability grant. The social grant system remains the largest source of support for many vulnerable groups and the government’s primary response to poverty and food insecurity in SA [36]. It is well established with a wide reach of 18.4 million beneficiaries [36].
Undoubtedly, the social grants provide vulnerable households with means to purchase food and prevent them from experiencing severe hunger, especially during emergencies such as COVID-19. In response to the pandemic, the government issued the SRDG (“COVID-19 grant”) to vulnerable groups. To date, more than 10 million people have received the SRDG. The government has re-extended until March 2023 [26]. Without such efforts, poverty and household income inequality would have been higher in vulnerable households [37]. Despite all these efforts, food insecurity has remained high in SA. This is largely driven by a series of complex factors including failure of social grants to keep up with inflation of food prices, and use of these funds for many non-food necessities [38]. Vulnerable households tend to have greater numbers of residents than others, a factor linked to households that compromise food quantity and quality to cater for the entire household [9, 38, 39]. Accordingly, we showed household crowding to be associated with a 23.0% increase in food insecurity, even after adjusting for other social vulnerability indicators. Collectively, these factors might explain why grant recipient households still display higher levels of social vulnerability and food insecurity compared to their non-recipient households [8, 9, 39].
The findings that SES indicators were major determinants of food insecurity align with the previous reports [10, 25, 33]. The government developed various initiatives such as the recent National Development Plan 2030: Our Future-Make it Work (2012). This plan aims to eliminate poverty and reduce inequalities by 2030 [40]. Economic development and job creation, however, have been major challenges for the government, partly due to corruption and political instability that has caused a decline in long-term investments [2, 26]. Other contributing factors are gaps in the formulation and implementation of policies to address food insecurity and a lack collaboration from different stakeholders in the food system [33]. Researchers often view food insecurity as a rural issue and a majority of initiatives addressing food insecurity focus on solutions related to production [33, 41, 42]. Urban areas are also vulnerable to food insecurity as they depend more on the cash economy than their rural counterparts [41]. With more people residing in urban areas (64%) [28], the labor market will become extremely competitive, and subsequently lead to higher poverty rates in vulnerable groups (those without education and older adults). Poverty and food insecurity are already shifting towards urban areas [10, 43], thus need to be addressed urgently.
The COVID-19 pandemic provoked collaboration between government and various external partners, such as corporate and faith-based organizations and NGOs that worked together to provide goods and financial assistance to vulnerable individuals and communities [9]. This partnership can be retained in the fight against food insecurity. Through this partnership, relevant organizations can use the COVID-19 pandemic as a reference to learn from the mistakes (such as mismanagement of funds and other resources) [9, 44]. They can identify areas of improvement and make use of a new database of social relief recipients to effectively direct efforts (such as social assistance initiatives and job opportunities) to those most vulnerable. Because social vulnerability and food insecurity are interlinked, and both dynamic in nature, we propose monitoring their patterns over time. This can guide government and affiliated partners to re-evaluate and develop new policies to combat current and future food insecurity. In rural areas, social relief initiatives need to change from solutions based on production to economic reform initiatives such as the development and maintenance of infrastructure. This should include provision of efficient service delivery, job creation opportunities, and improved education facilities. Such reforms can enable rural households to have multiple incomes and a surplus to afford non-food necessities [8]. Policy and social development initiatives addressing urban food insecurity must focus on urban food systems (both formal and informal markets) to ensure that food is affordable, easily accessible, and of good quality and diversity [41]. Currently, those who qualify for the old-age grant are 60 years and older, but our findings suggest that social vulnerability increases exponentially from 45 to 54 years of age. Fortunately, the DSD has already developed a proposal to introduce a “Basic Income Grant” [36], that is currently under discussion. Consideration about its implementation is urgent—to provide income support for unemployed individuals from 18 to 59 years of age, and to those who are currently not receiving a social grant. Until this policy is implemented, we call on the government to increase all social grants and to make temporary relief measures such as SRDG and food parcels or vouchers permanent for vulnerable groups until they reach a low vulnerability state or are no longer vulnerable or qualify for the old-age grant. We also call government to strengthen and support gender-based socio-economic initiatives such as “The women empowerment and gender quality Bill” (2013) [45] and prevent social vulnerabilities in women, especially in Black African women.
Our findings have policy implications for other vulnerable regions, especially those in Sub-Saharan Africa and South Asia [46]. Although vulnerable groups tend to be similar across socio-economic groups (such as children, women, rural areas), we also recommend countries use social vulnerability indices to describe and continuously update their vulnerable groups so that social relief efforts can be directed consistently to the relevant people.
Strengths and limitations
Strengths of our study include use of large-scale nationally representative data to measure the prevalence and distribution of social vulnerability across multiple socio-economic, demographic, and geographical factors. This detailed analysis allowed us to discern a better profile of the vulnerable groups in SA. There are also limitations. This was a cross-sectional study; thus, our results do not imply causality. Although we calculated the SVI using several indicators, these do not amount to a complete list of all indicators of social vulnerability. There are many other important indicators of social vulnerability we did not capture in our SVI, including disability and health status. We only used three questions to determine food insecurity, which might not have captured dimensions of food insecurity such as food expenditure, quality of food, and food behaviors (eating bigger porting sizes). We could not specifically classify child hunger in our study. Overall, however, household food insecurity is inherently associated with malnutrition in both children and adults [47–49]. Therefore, poverty and food insecurity might partly explain why SA has one of the highest levels of child malnutrition (persisting undernutrition, obesity, and micronutrient deficiencies) [49, 50].
Conclusions
Government requires an urgent and innovative framework to grow a stable economy, create jobs, improve the education system, and develop new and effective food insecurity policies that will make food easily accessible and affordable while considering nutritional factors. Policy or social development initiatives need to prioritize vulnerable groups, including Black Africans, women, rural areas, those residing in Mpumalanga and KwaZulu-Natal. In the absence of aggressive economic reforms and an adequate education system, vulnerable groups in SA and other LMICs will continue to suffer from the burden of high social and economic inequalities.
Acknowledgements
SAN, LJW, and this research are supported by the DSI-NRF Centre of Excellence (CoE) in Human Development at the University of the Witwatersrand, Johannesburg, South Africa. The content is solely the responsibility of the authors and does not reflect the views of the DSI-NRF CoE in Human Development.
Biographies
Asanda Mtintsilana
is a Postdoctoral Researcher at SA MRC/Wits Developmental Pathways for Health Research Unit, Department of Paediatrics, Faculty of Health Sciences, School of Clinical Medicine, University of the Witwatersrand, Johannesburg, South Africa.
Siphiwe N. Dlamini
is a Postdoctoral Researcher at SA MRC/Wits Developmental Pathways for Health Research Unit, Department of Paediatrics, Faculty of Health Sciences, School of Clinical Medicine, University of the Witwatersrand, Johannesburg, South Africa.
Witness Mapanga
is a Postdoctoral Researcher at SA MRC/Wits Developmental Pathways for Health Research Unit, Department of Paediatrics, Faculty of Health Sciences, School of Clinical Medicine, University of the Witwatersrand, Johannesburg, South Africa and Postdoctoral Researcher at the Noncommunicable Diseases Research Division, Wits Health Consortium (PTY) Ltd, Johannesburg, South Africa.
Ashleigh Craig
is a Postdoctoral Researcher at SA MRC/Wits Developmental Pathways for Health Research Unit, Department of Paediatrics, Faculty of Health Sciences, School of Clinical Medicine, University of the Witwatersrand, Johannesburg, South Africa.
Justin Du Toit
is a Centre and Research Manager at the DSI-NRF Centre of Excellence in Human Development, University of the Witwatersrand, Johannesburg, Gauteng, South Africa.
Lisa J. Ware
is an Associate Director at SA MRC/Wits Developmental Pathways for Health Research Unit, Department of Paediatrics, Faculty of Health Sciences, School of Clinical Medicine, University of the Witwatersrand, Johannesburg, South Africa and a Senior Researcher at the DSI-NRF Centre of Excellence in Human Development, University of the Witwatersrand, Johannesburg, Gauteng, South Africa.
Shane A. Norris
is a Professor and Director at SA MRC/Wits Developmental Pathways for Health Research Unit, Department of Paediatrics, Faculty of Health Sciences, School of Clinical Medicine at University of the Witwatersrand, Johannesburg, South Africa; Director at the DSI-NRF Centre of Excellence in Human Development, University of the Witwatersrand, Johannesburg, Gauteng, South Africa, and Professorial Fellow at the Global Health Research Institute, School of Human Development and Health, University of Southampton, United Kingdom.
Declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Asanda Mtintsilana, Email: Asanda.Mtintsilana@wits.ac.za.
Siphiwe N. Dlamini, Email: siphiwe.dlamini2@wits.ac.za
Witness Mapanga, Email: wmapanga@witshealth.co.za.
Ashleigh Craig, Email: Ashleigh.Craig@wits.ac.za.
Justin Du Toit, Email: justin.dutoit@wits.ac.za.
Lisa J. Ware, Email: lisa.ware@wits.ac.za
Shane A. Norris, Email: Shane.Norris@wits.ac.za
References
- 1.World Bank. Gini index (World Bank estimate) -South Africa [Internet]. Vol. 7. [cited 2022 Mar 22]. Available from: https://data.worldbank.org/indicator/SI.POV.GINI?locations=ZA
- 2.Purfield CM, Im F, Inchauste G. South Africa economic update: Fiscal Policy and Redistribution in an Unequal Society. World bank [Internet]. 2014;(November):51. Available from: http://www-wds.worldbank.org/external/default/WDSContentServer/WDSP/IB/2014/10/30/000470435_20141030130616/Rendered/PDF/921670WP0P131400SAEU60for0web01029b.pdf
- 3.World Bank Group. Building back better from COVID-19, with a special focus on jobs (English) [Internet]. South Africa Economic Update Edition 13. South Africa; 2021. Available from: https://openknowledge.worldbank.org/handle/10986/35987
- 4.Chitiga M, Henseler M, Mabugu RE, Maisonnave H. How COVID-19 pandemic worsens the economic situation of women in South Africa. Eur J Dev Res. 2021;34:1627. doi: 10.1057/s41287-021-00441-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.National Department of Health (NDoH). South African Demographic and Health Survey (SADHS) 2016. Pretoria, South Africa; 2019.
- 6.Statistics South Africa (Statssa). Quarterly Labour Force Survey: Quarter 3: 2021. Pretoria, South Africa; 2021.
- 7.Statistics South Africa. General Household Survey 2020 [Internet]. Pretoria, South Africa; 2021. Available from: http://www.statssa.gov.za/publications/P0318/P03182020.pdf
- 8.Mthethwa S, Wale E. Household vulnerability to food insecurity in rural south africa: evidence from a nationally representative survey data. Int J Environ Res Public Health. 2021;18(4):1–17. doi: 10.3390/ijerph18041917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.van der Berg S, Patel L, Bridgman G. Food insecurity in South Africa: Evidence from NIDS-CRAM Wave 5. 2021.
- 10.World Bank. Overcoming Poverty and Inequality in South Africa: An Assessment of Drivers, Constraints and Opportunities [Internet]. Washington; 2018. Available from: www.worldbank.org
- 11.UNAIDS. UNAIDS. Country factsheets South Africa 2020. 2021;1–12.
- 12.Dunkle KL, Jewkes RK, Brown HC, Yoshihama M, Gray GE, McIntyre JA, et al. Prevalence and patterns of gender-based violence and revictimization among women attending antenatal clinics in Soweto, South Africa. Am J Epidemiol. 2004;160(3):230–239. doi: 10.1093/aje/kwh194. [DOI] [PubMed] [Google Scholar]
- 13.Ware LJ, Kim AW, Prioreschi A, Nyati LH, Taljaard W, Draper CE, et al. Social vulnerability, parity and food insecurity in urban South African young women: the healthy life trajectories initiative (HeLTI) study. J Public Health Policy. 2021;42(3):373–389. doi: 10.1057/s41271-021-00289-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cutter SL, Boruff BJ, Shirley LW. Social vulnerability to environmental hazards. Soc Sci Q. 2003;84(June):242–261. doi: 10.1111/1540-6237.8402002. [DOI] [Google Scholar]
- 15.Flanagan BE, Gregory EW, Hallisey EJ, Heitgerd JL, Lewis B. A social vulnerability index for disaster management. J Homel Secur Emerg Manag. 2011;8(1):1–22. [Google Scholar]
- 16.Snyder BF, Parks V. Spatial variation in socio-ecological vulnerability to Covid-19 in the contiguous United States. Health Place. 2020;66(April):102471. doi: 10.1016/j.healthplace.2020.102471. [DOI] [PubMed] [Google Scholar]
- 17.An R, Xiang X. Social vulnerability and obesity among US adults. Int J Health Sci. 2015;3(3):7–21. [Google Scholar]
- 18.Gay JL, Robb SW, Benson KM, White A. Can the Social Vulnerability Index be used for more than emergency preparedness? An examination using youth physical fitness data. J Phys Act Health. 2016;13(2):121–130. doi: 10.1123/jpah.2015-0042. [DOI] [PubMed] [Google Scholar]
- 19.Wehler CA, Scott RI, Anderson JJ. The community childhood hunger identification project: a model of domestic hunger—demonstration project in Seattle, Washington. J Nutr Educ. 1992;24(1):29S–35S. doi: 10.1016/S0022-3182(12)80135-X. [DOI] [Google Scholar]
- 20.Kehoe SH, Wrottesley S, Ware L, Prioreschi A, Draper C, Ward K, et al. Food insecurity, diet quality and body composition: data from the Healthy Life Trajectories Initiative (HeLTI) pilot survey in urban Soweto, South Africa. Public Health Nutr. 2021;24(7):1629–1637. doi: 10.1017/S136898002100046X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Flanagan BE, Hallisey EJ, Adams E, Lavery A. Measuring community vulnerability to natural and anthropogenic hazards: The Centers for Disease Control and Prevention’s Social Vulnerability Index. J Environ Health. 2018;80(10):34–36. [PMC free article] [PubMed] [Google Scholar]
- 22.Statistics South Africa (Stats SA). Mid-Year population estimates 2021 [Internet]. Pretoria, South Africa; 2021. Available from: www.statssa.gov.za/?page_id=1854&PPN=P0302&SCH=72983
- 23.Griffiths PL, Johnson W, Cameron N, Pettifor JM, Norris SA. In urban South Africa, 16 year old adolescents experience greater health equality than children. Econ Hum Biol. 2013;11(4):502–514. doi: 10.1016/j.ehb.2013.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kagura J, Adair LS, Pisa PT, Griffiths PL, Pettifor JM, Norris SA. Association of socioeconomic status change between infancy and adolescence, and blood pressure, in South African young adults: birth to Twenty cohort. BMJ Open. 2016;6(3):e008805. doi: 10.1136/bmjopen-2015-008805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ngumbela XG, Khalema EN, Nzimakwe TI. Local worlds: vulnerability and food insecurity in the Eastern Cape province of South Africa. Jàmbá. 2020;12(1):1–10. doi: 10.4102/jamba.v12i1.830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.The South African Government. President Cyril Ramaphosa: 2022 State of the Nation Address. Pretoria; 2022.
- 27.Jain R, Bassier I, Budlender J, Zizzamia R. The labour market and poverty impacts of covid-19 in South Africa: an update with NIDS-CRAM Wave 2 [Internet]. Available from: www.opensaldru.uct.ac.za.
- 28.van Niekerk W, le Roux A. Chapter 10: Human settlements. In: Climate risk and vulnerability: a handbook for Southern Africa. 2nd ed. 2017.
- 29.Freeman MC, Garn JV, Sclar GD, Boisson S, Medlicott K, Alexander KT, et al. The impact of sanitation on infectious disease and nutritional status: a systematic review and meta-analysis. Int J Hyg Environ Health. 2017;220:928–949. doi: 10.1016/j.ijheh.2017.05.007. [DOI] [PubMed] [Google Scholar]
- 30.Martinez JC, Clark JM, Gudzune KA. Association of personal vehicle access with lifestyle habits and food insecurity among public housing residents. Prev Med Rep. 2019;13:341–345. doi: 10.1016/j.pmedr.2019.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Abeliansky AL, Erel D, Strulik H. Social vulnerability and aging of elderly people in the United States. SSM - Population Health. 2021;16. [DOI] [PMC free article] [PubMed]
- 32.Wallace LMK, Theou O, Pena F, Rockwood K, Andrew MK. Social vulnerability as a predictor of mortality and disability: cross-country differences in the survey of health, aging, and retirement in Europe (SHARE) Aging Clin Exp Res. 2015;27(3):365–372. doi: 10.1007/s40520-014-0271-6. [DOI] [PubMed] [Google Scholar]
- 33.Boatemaa S, Drimie S, Pereira L. Addressing food and nutrition security in South Africa: a review of policy responses since. Afr J Agric Resour Econ. 2002;13:264–279. [Google Scholar]
- 34.Department of National Treasury. Recommendations on Zero Ratings in the Value-Added Tax System. Pretoria: National Treasury; 2018.
- 35.Department of Social Development. Social Assistance Act. Social Assistance Act Pretoria: Department of Social Development; 2004.
- 36.Department of Social Development. Department of Social Development: Annual Report 2020|21 [Internet]. Pretoria; 2021. Available from: www.sassa.gov.za.
- 37.Bhorat H, Köhler T. Social assistance during South Africa’s national lockdown examining the COVID-19 grant, changes to the child support grant, and post-October policy options.
- 38.Devereux S, Waidler J. Food Security SA Working Paper Series: Why does malnutrition persist in South Africa despite social grants? [Internet]. Cape Town; 2017. (001). Available from: www.foodsecurity.ac.za.
- 39.Chakona G, Shackleton CM. Food insecurity in South Africa: To what extent can social grants and consumption of wild foods eradicate hunger? World Dev Perspect. 2019;13:87–94. doi: 10.1016/j.wdp.2019.02.001. [DOI] [Google Scholar]
- 40.South Africa. National Planning Commission. Our future: make it work: national development plan, 2030. National Planning Commission; 2012.
- 41.Battersby J. Urban food insecurity in Cape town, South Africa: An alternative approach to food access. Dev South Afr. 2011;28(4):545–561. doi: 10.1080/0376835X.2011.605572. [DOI] [Google Scholar]
- 42.Battersby J, Haysom G. Linking urban food security, urban food systems, poverty, and urbanisation. In: Battersby J, Watson V, editors. Urban food systems govervenance and poverty in African cities. 1. London: Routledge; 2018. pp. 1–290. [Google Scholar]
- 43.Walsh CM, van Rooyen FC. Household food security and hunger in rural and urban communities in the free state province, South Africa. Ecol Food Nutr. 2015;54(2):118–137. doi: 10.1080/03670244.2014.964230. [DOI] [PubMed] [Google Scholar]
- 44.Felix J. Covid-19 relief: Government squandered R177m on “damaged, poorly packaged” food parcels-AG. 2021; Available from: https://www.news24.com/news24/southafrica/news/covid-19-relief-government-squandered-r177m-on.
- 45.The South African Government. Women Empowerment and Gender Equality Bill. Pretoria: Minister of Women, Children and People with Disabilities; 2013.
- 46.Alkire S, Assa J, Calderón C, Casarini A, Conceição P, Dirksen J, et al. Global Multidimensional Poverty Index 2021: unmasking disparities by ethnicity, caste and gender [Internet]. 2021. Available from: http://hdr.undp.organd, https://ophi.org.uk/multidimensional-poverty-index/
- 47.Pan L, Sherry B, Njai R, Blanck HM. Food insecurity is associated with obesity among US adults in 12 states. J Acad Nutr Diet. 2012;112(9):1403–1409. doi: 10.1016/j.jand.2012.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tester JM, Rosas LG, Leung CW. Food insecurity and pediatric obesity: a double whammy in the era of COVID-19. Curr Obes Rep. 2020;9:442–450. doi: 10.1007/s13679-020-00413-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mbhenyane X, Labuschagne I. South Africa’s twin malnutrition challenges: hunger and obesity. The Conversation. 2017.
- 50.Popkin BM, Corvalan C, Grummer-Strawn LM. Dynamics of the double burden of malnutrition and the changing nutrition reality. The Lancet. 2020;395:65–74. doi: 10.1016/S0140-6736(19)32497-3. [DOI] [PMC free article] [PubMed] [Google Scholar]