Abstract
Carcinoma of the axillary tail of Spence is a rare type of breast cancer that develops at a specific anatomical position in the breast, with an incidence of approximately 0.3%. It should be differentiated from axillary soft tissue tumor, axillary ectopic breast cancer, and lymph node metastases of breast and other primary cancers. Here, we report a case of carcinoma of the axillary tail of Spence in a 47-year-old patient who visited our clinic with a lower axillary mass and was diagnosed based on mammography, US, CT, and MRI findings.
Keywords: Breast Neoplasm, Axilla, Mammography, Ultrasonography, Magnetic Resonance Imaging
Abstract
유방의 겨드랑꼬리에 발생한 악성 종양은 유방의 특정 해부학적 위치에서 발생하는 유방암의 한 종류이며 발생률은 0.3% 정도로 드문 질환이다. 이는 겨드랑이에서 발생하는 연부조직 종양, 액와부 부유방에서 발생한 유방암, 유방암의 림프절 전이 또는 다른 원발암의 림프절 전이 등과 감별이 필요하다. 저자들은 겨드랑이 종물을 주소로 내원한 47세 환자에서 유방촬영술, 초음파, 전산화단층촬영, 자기공명영상을 통해 겨드랑꼬리 유방암을 진단한 증례를 경험하여 보고하고자 한다.
INTRODUCTION
Breast cancer is one of the most common malignant tumors in female. However, breast cancer that arises from the axillary tail of Spence (ATS) is rarely reported with a low incidence rate of about 0.3% among breast cancer (1). The ATS is located in specific anatomical structure, which is a narrow part of mammary gland extension to axilla along the inferolateral edge of the pectoralis major muscle. Also, it can penetrate through a defect of clavipectoral fascia, which is a deep fascia between subclavius and pectoralis minor muscle (2). The clinicopathologic, prognostic, and imaging features are scarcely studied so far. Here, we present a rare case of a carcinoma of the ATS (CATS) in the subcutaneous fat layer of the anterior axillary fossa with its imaging findings of multi-modalities including mammography, US, CT, and MRI.
CASE REPORT
A 47-year-old female came to our medical center, complaining of a left axillary mass for 2 weeks. She had no remarkable past medical history other than hysterectomy for uterine myoma. She also did not have any breast cancer family history.
Physical examination showed a superficially located soft mass in the lower axillary fossa, measuring about 2 cm, without overlying skin changes.
A mediolateral oblique digital mammography showed a well-defined hyperdense mass in the left axillary portion (Fig. 1A). For further evaluation, breast US was performed and identified a 1.2 cm sized round-shaped, partially microlobulated margin, hypoechoic mass with increased vascularity in the subcutaneous fat layer of the left lower axillary fossa (Fig. 1B). When considering the location of the lesion, primary subcutaneous soft tissue mass, axillary ectopic breast lesion, the ATS lesion, and lymphadenopathy were considered. On breast US, a 0.4 cm sized small benign looking nodule was noted in the left breast and no remarkable lesion was found in the right breast and both axillae. Based on the US findings, the axillary mass was classified as breast imaging reporting and data system (BI-RADS) category 4B. US guided core needle biopsy by 14-gauge ACECUT was performed, and the pathologic result revealed invasive carcinoma.
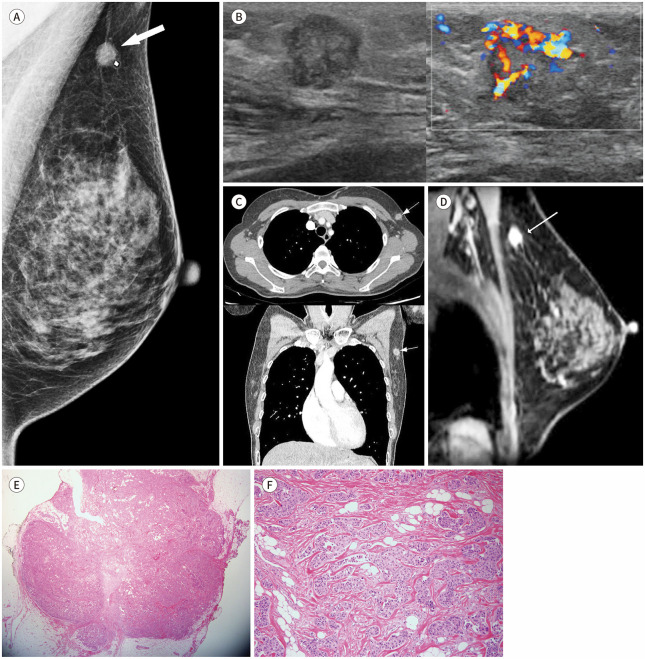
Fig. 1. Carcinoma of the axillary tail of Spence in a 47-year-old female presenting with a palpable mass in the left lower axilla.
A. The left mediolateral oblique mammogram shows a small isodense mass (arrow) in the palpable area of the left lower axilla region.
B. The US shows a 1.2-cm, round, heterogeneously hypoechoic mass with a microlobulated margin in the subcutaneous fat layer of the left lower axillary fossa (left). The color Doppler scan reveals increased vascularity within the mass (right).
C. Axial and coronal reconstructed views of the chest CT scan with contrast enhancement shows a round solid nodular lesion density in the left lower axilla in the anterolateral aspect of the pectoralis major with continuous breast tissue (arrows). The mass is homogeneously hypodense to skeletal muscles in the precontrast image (46 Hounsfield units) with significant enhancement (104 Hounsfield units).
D. The sagittal oblique reconstructed breast MR image with contrast enhancement shows a well-defined solid mass in the left lower axilla (arrow) and continuous enhancing breast tissue extending to the axilla.
E. The tumor shows a round outline with a small daughter-nodule-like protrusion (hematoxylin & eosin stain, × 10).
F. Trabecular arrangements with the desmoplastic stroma, consistent with invasive carcinoma of no special type, are noted (hematoxylin & eosin stain, × 100).
The patient underwent chest CT with contrast enhancement to figure out further metastatic lesion. There was no detectable metastatic lesion in both lungs and mediastinum (Fig. 1C).
Breast MRI with contrast enhancement was performed to determine if there were additional lesions that were not revealed by mammography or US. The malignant mass confirmed by biopsy was seen in the left lower axillary portion, indicating continuity with normal breast tissue in the upper outer quadrant (UOQ) (Fig. 1D). A small enhancing mass was observed in the left UOQ area. However, by second look US, it was identified as a probably benign mass. Also, a prominent lymph node with eccentric cortical thickening was noted in the left axilla. Fine needle aspiration was done, and no malignant cells were found.
The surgeon performed a partial mastectomy with sentinel lymph node dissection. No lymph node metastasis was proven. Microscopically the axillary tumor showed trabecular arrangements with the desmoplastic stroma, which are typical histological features of invasive carcinoma, no special type (Fig. 1E, F). In immunohistochemical study, estrogen, and progesterone receptor were negative, human epidermal growth factor receptor 2 was positive and Ki-67 labelling index was 20%.
The patient underwent adjuvant chemotherapy in the form of docetaxel and cyclophosphamide, followed by Trastuzumab and radiotherapy as well. No recurrence was observed for 19 months until the last follow-up.
This study was approved by the Institutional Review Board of our institution and the requirement for informed consent was waived (IRB No. 2021-11-031).
DISCUSSION
The CATS is a rare disease entity to date, and only few papers have studied the characteristics of the disease. According to the previous literature by Gou et al. (3), who performed the largest research about the clinicopathological characteristics and prognostic features of CATS, the prognosis is worse for the CATS than for the UOQ cancer, since CATS has a higher grade, higher negative hormone receptor rate and more positive nodal metastasis than UOQ breast cancer. The CATS can be easily understaged because it may be hidden under the pectoralis muscle or plastic reconstruction, and potentially positive nodes in ATS may be missed, which can lead to undertreatment of CATS (3). There are a few case reports of the CATS, and most of them also reported the advanced stage of the CATS, unlike our case of the early stage.
The ATS is a different structure from axillary ectopic breast tissue (4). The axillary ectopic breast tissue is a residual breast tissue that persists from normal embryologic development, and it is a result of mammary ridge development failure, so it does not show continuity with the main breast parenchyma (5). On the other hand, the ATS is a normal breast structure that extends along the inferolateral edge of the pectoralis major muscle and can enter the axilla through a defect of the clavipectoral fascia, which is known as a foramen of Langer (2). Therefore, the ATS is characterized by showing a continuous relationship with UOQ breast tissue and can be distinguished from ectopic breast tissue (6).
MRI plays an important role in the localization of the ATS (2). Since it is difficult to identify detailed structures such as clavipectoral fascia by CT or MRI, it is not easy to define the exact ATS boundaries. However, when continuous breast tissue from the main breast parenchyma is seen in the MRI, we can confirm that the lesion arises from the ATS. In our case, a sagittal oblique reconstructed MRI showed continuous mammary tissue from UOQ breast to axilla. Therefore, we could identify that the lesion was from the ATS, rather than the axillary ectopic breast tissue.
There are several other possible differential diagnoses of an axillary lesion; subcutaneous soft tissue tumor, benign breast tumor of the ATS, CATS, and metastatic lymph nodes from occult breast cancer or other hidden malignancy. In our case, we confirmed that the location of the lesion was ATS, and after confirming with pathology as invasive carcinoma, only two differential diagnoses remained, whether it is a CATS or a complete infiltration of metastatic lymph nodes. According to the case of Patrinos et al. (7), the axillary lesion was observed in the surgical site at a position superficial than that of clavipectoral fascia, confirming that the lesion was CATS rather than metastatic lymphadenopathy. In our case, we could not confirm clavipectoral fascia by MRI, but since the axillary mass was observed at a position even superficial than pectoralis major in MRI, it was more likely to be CATS than metastatic lymphadenopathy. Since malignancy was not observed in other breast tissue or other organs in chest/abdominal CT, the possibility of metastatic lymphadenopathy could be ruled out.
Currently, the importance of the ATS is receiving more attention due to the increasing number of trials of prophylactic mastectomy due to BRCA genes. Both radiologists and surgeons can easily overlook the ATS, and the patient can eventually end in the CATS (8). Therefore, it is crucial to keep the ATS and the CATS in mind when dealing with patients with axillary mass and even in screening studies.
In conclusion, the CATS is an exceedingly rare disease, but it is a disease that must be considered for differentiation when there are patients with axillary mass. In addition, preoperative MRI can play a key role in differential diagnosis. Further studies may be necessary to better understand this rare disease entity and determine a better diagnosis and treatment direction.
Footnotes
- Conceptualization, L.J.Y.
- investigation, all authors.
- methodology, L.J.Y.
- project administration, all authors.
- supervision, L.J.Y., P.J.Y.
- validation, L.J.Y.
- visualization, P.S.Y., L.J.Y.
- writing—original draft, P.S.Y.
- writing—review & editing, L.J.Y.
Conflicts of Interest: The authors have no potential conflicts of interest to disclose.
Funding: None
References
- 1.Siotos C, McColl M, Psoter K, Gilmore RC, Sebai ME, Broderick KP, et al. Tumor site and breast cancer prognosis. Clin Breast Cancer. 2018;18:e1045–e1052. doi: 10.1016/j.clbc.2018.05.007. [DOI] [PubMed] [Google Scholar]
- 2.Okubo M, Tada K, Niwa T, Nishioka K, Tsuji E, Ogawa T, et al. A case of breast cancer in the axillary tail of Spence - enhanced magnetic resonance imaging and positron emission tomography for diagnostic differentiation and preoperative treatment decision. World J Surg Oncol. 2013;11:217. doi: 10.1186/1477-7819-11-217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gou ZC, Liu XY, Xiao Y, Zhao S, Jiang YZ, Shao ZM. Decreased survival in patients with carcinoma of axillary tail versus upper outer quadrant breast cancers: a SEER population-based study. Cancer Manag Res. 2018;14:1133–1141. doi: 10.2147/CMAR.S165291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ampil F, Caldito G, Henderson B, Li B, Kim RH, Burton G, et al. Carcinoma of the axillary tail of Spence: a case series. Anticancer Res. 2012;32:4057–4059. [PubMed] [Google Scholar]
- 5.DeFilippis EM, Arleo EK. The ABCs of accessory breast tissue: basic information every radiologist should know. AJR Am J Roentgenol. 2014;202:1157–1162. doi: 10.2214/AJR.13.10930. [DOI] [PubMed] [Google Scholar]
- 6.Adler DD, Rebner M, Pennes DR. Accessory breast tissue in the axilla: mammographic appearance. Radiology. 1987;163:709–711. doi: 10.1148/radiology.163.3.3575719. [DOI] [PubMed] [Google Scholar]
- 7.Patrinos A, Zarokosta M, Tsiaoussis J, Noussios G, Piperos Τ, Zoulamoglou M, et al. The clavipectoral fascia as the unique anatomical criteria for distinguishing breast parenchymal lesions from axillary lymph node metastasis. J Surg Case Rep. 2019;5:rjz135. doi: 10.1093/jscr/rjz135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Memon S, Emanuel JC. The axillary tail--an important caveat in prophylactic mastectomy. Breast J. 2008;14:313–314. doi: 10.1111/j.1524-4741.2008.00585.x. [DOI] [PubMed] [Google Scholar]