Abstract
Objectives
Trends in the incidence of precancerous cervical lesions can be monitored to evaluate the impact of human papillomavirus (HPV) vaccination. The objective of this analysis was to determine whether declines in precancerous cervical lesions varied by area-based measures of poverty, race, and ethnicity.
Methods
We analyzed 11 years of incidence data (2008-2018) from a statewide active surveillance system of precancerous cervical lesions in Connecticut. We divided area-based measures of poverty, race, and ethnicity (percentage of the population in a census tract who were living below the federal poverty level, who were Black, and who were Hispanic) at the census-tract level into 4 groups (<5.0%, 5.0%-9.9%, 10.0%-19.9%, ≥20.0%) using recommended cut points from the Public Health Disparities Geocoding Project. We estimated incidence rates and average annual percentage changes (AAPCs) stratified by age and each area-based measure using Joinpoint regression software. We used total population and estimated screened population as denominators for each age group to calculate rates and AAPCs.
Results
During 2008-2018 in Connecticut, 18 878 women aged 21-39 were diagnosed with precancerous cervical lesions. After adjusting for screening, the largest declines occurred among women aged 21-24 (AAPC = −11.5%; 95% CI, −13.6% to −9.4%). We found significant and similar annual declines (~10%-12%) in this age group across all 4 levels of poverty, race, and ethnicity.
Conclusions
This analysis adds to the growing body of evidence demonstrating the positive impact of population-level HPV vaccination among young women that appears similar across area-based measures of sociodemographic characteristics. Monitoring is necessary to ensure the continuation of this progress in all communities.
Keywords: HPV, vaccine impact, sociodemographic, poverty, race, ethnicity, area-based measures
Monitoring trends in precancerous cervical lesions is useful for evaluating the impact of human papillomavirus (HPV) vaccination on population health. Monitoring trends is especially important in areas such as the United States that have not yet reached optimal vaccination coverage. Data from the 2019 National Health Immunization Survey–Teen showed that just 54.2% of adolescents aged 13-17 years in the United States received the recommended doses of HPV vaccine, which is well below the 2030 Healthy People goal of 80%. 1,2 In addition, monitoring trends by sociodemographic characteristics is important to detect differences in vaccination impact. Disparities in cervical cancer outcomes exist for both individual and area-level socioeconomic measures. 3 -5 Advanced-stage diagnosis of cervical cancer is associated with low socioeconomic status at the individual level and in census-tract populations with high proportions of poverty. 3,4 In addition, rates of cervical cancer, advanced-stage diagnosis, and death from cervical cancer are disproportionately higher among non-Hispanic Black and Hispanic women compared with non-Hispanic White women. 6 -8
Vaccination can lead to reductions in HPV-related disease outcomes across all levels of socioeconomic status and all racial and ethnic groups. For reductions to occur, vaccination efforts need to be widespread and may need to include special efforts to vaccinate populations most at risk for developing cervical cancer, advanced-stage diagnosis of cervical cancer, and death from cervical cancer. Analyzing trends in precancerous cervical lesions by sociodemographic characteristics can indicate whether efforts are on track to achieve equity in HPV-related disease prevention. Previous studies in many countries found significant declines in precancerous cervical lesions in young women after the introduction of HPV vaccines. 9 -12 However, few studies have examined trends by measures of socioeconomic status or race and ethnicity. 13 In a recent systematic review of HPV vaccination impact studies in the United States, 13 of the 23 included studies reported on sociodemographic data. However, only 2 studies conducted a stratified analysis to examine whether declines in HPV-related outcomes differed by sociodemographic characteristics. 13
Analyses that use census tract area–based measures are useful for identifying disparities in outcomes for various diseases. 3,14 The attributes of census tracts reflect the communities in which people live—jobs, resources, cultural norms/beliefs, access to health care services, and other living conditions. Area-based poverty, defined as the percentage of the population in a census tract living below the federal poverty level, can be used to group census tracts and evaluate socioeconomic disparities in health outcomes, including cervical cancer. 3 An analysis from the Public Health Disparities Geocoding Project found that census tracts with increasingly higher proportions of poverty were associated with increasingly poorer health outcomes in infectious disease, chronic disease, environmental exposures, and maternal–child health. 3 This information can be used by policy makers to direct funding and community outreach in places where they are needed most.
The body of research on trends of HPV-related disease by sociodemographic characteristics is small and somewhat dated and shows mixed results. The objective of this analysis was to examine 11 years of surveillance data in Connecticut (2008-2018) to determine whether statewide trends in overall rates of precancerous cervical lesions differ by area-based measures of poverty, race, and ethnicity.
Methods
The Centers for Disease Control and Prevention began to monitor the impact of HPV vaccination through population surveillance of cervical intraepithelial neoplasia grades 2/3 and adenocarcinoma in situ (CIN2+) in 2008. Details of these surveillance methods are available elsewhere. 15 In Connecticut, this surveillance was facilitated, beginning in January 2008, by including CIN2+ on the list of conditions required to be reported to the Connecticut Department of Public Health by all pathology laboratories that serve Connecticut residents. To maximize case finding, laboratories that report >80% of cases are routinely audited for completeness and accuracy of reporting. This project was reviewed by state and federal institutional review boards and determined exempt from human subjects review because it was deemed public health surveillance.
We restricted our analyses to female residents of Connecticut aged 21-39. We excluded women aged <21 because of changes in clinical guidelines in 2012, which recommended this age group no longer undergo cervical cancer screening. 16 To calculate incidence rates, we obtained population denominators from the 2010 US Census Bureau. 17
Because cervical cancer screening is a prerequisite for a diagnosis of CIN2+, we also conducted analyses that used population denominators adjusted for screening using data from the Behavioral Risk Factor Surveillance System (BRFSS) specific to Connecticut. 18 The BRFSS is a random-digit–dialed telephone (both landline and cell phone) survey that asks participants about various health-related risk behaviors, chronic health conditions, and use of preventive services such as cancer screenings. We calculated the proportion of women screened for cervical cancer in Connecticut for each year by age group. We estimated the population of screened women by applying these proportions to the census denominators for each age group.
We used ArcGIS version 10.8.1 (Esri) to geocode the residential addresses of women diagnosed with CIN2+ who were reported to the Connecticut surveillance system to the census-tract level. We then matched geocoded cases to the corresponding area-based measures obtained from the American Community Survey 5-year estimates provided by the US Census Bureau. 19,20 We defined the area-based measure of poverty as the percentage of the population in a census tract with an annual household income that was below the federal poverty level. We defined the area-based measures of race and ethnicity as the percentage of Black residents and the percentage of Hispanic residents, respectively, in a census tract. We divided these area-based measures into 4 groups: <5.0%, 5.0%-9.9%, 10.0%-19.9%, and ≥20.0% of the census tract. We selected these categories a priori from the cut points used in the Public Health Disparities Geocoding Project. 3
Statistical Analysis
We used Joinpoint Regression Program version 4.8.0.1 (Applications Branch, Surveillance Research Program, National Cancer Institute) to model rates of CIN2+ over time and estimate average annual percentage change (AAPC). We first ran separate models for each age group. We included the most parsimonious models (ie, models that contained either 0 or 1 joinpoint). A joinpoint is an inflection point at which a significant change in the trend has occurred. We modeled rates for the total population of Connecticut and rates that used an estimated population of screened women. We further analyzed age groups in which significant declines occurred by each area-based measure. We used t tests to determine significance at the P < .05 level. These analyses tested whether declines occurred across the 4 levels of each area-based measure in the total population and in the screened population of the corresponding age group. We generated separate models for each area-based measure. We generated rates, AAPCs, and 95% CIs for each of the 4 levels of each area-based measure.
Results
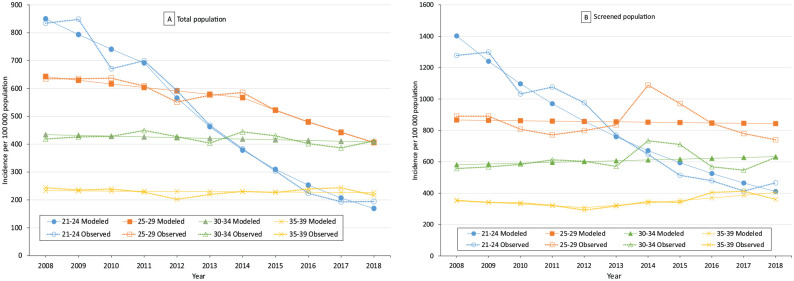
During 2008-2018 in Connecticut, 18 878 women aged 21-39 were diagnosed with CIN2+; we successfully geocoded 98% of reported cases. The number of reported cases of CIN2+ in the total population declined from 2117 in 2008 to 1276 in 2018 among women aged 21-39. Models for age groups 21-24 and 25-29 were best fit with 1 joinpoint each, in years 2011 and 2014, respectively (Figure A). Age groups 30-34 and 35-39 were best fit with no joinpoints. We observed significant declines in the incidence of reported cases of CIN2+ in young women during the study period. The AAPC was −14.9% (95% CI, −17.9% to −11.8%) among women aged 21-24 and −4.5% (95% CI, −5.8% to −3.1%) among women aged 25-29. We observed no significant declines in CIN2+ among women aged 30-34 or 35-39.
Figure.
Modeled estimates of the incidence and observed incidence of precancerous cervical lesions per 100 000 population, by age group and year of diagnosis, among women aged 21-39, Connecticut, 2008-2018. (A) Total population. (B) Screened population. Data source: HPV-IMPACT Program, Connecticut Emerging Infections Program.
When we evaluated the incidence rates among women screened for cervical cancer, we found significant declines among women aged 21-24 (AAPC = −11.5%; 95% CI, −13.6% to −9.4%) but not among women in other age groups. The best fit model for this age group had no joinpoints. The incidence rate per 100 000 population among women aged 21-24 screened for cervical cancer dropped from 1277 in 2008 to 466 in 2018 (Figure B). For women aged 25-29 screened for cervical cancer, the incidence rate dropped from 890 in 2008 to 740 in 2018.
When we examined trends among women aged 21-24 by area-based measures in the total population of women aged 21-24, we observed significant declines in CIN2+ across all 4 levels of poverty. The magnitudes of these declines were similar to one another, with AAPCs ranging from −13.3% to −15.2% among the 4 levels. We found similar results for area-based measures of race and ethnicity. AAPCs ranged from −13.2% to −16.1% across all 4 levels of percentage Black and from −13.3% to −15.7% across all 4 levels of percentage Hispanic (Table 1).
Table 1.
Average annual percentage change (AAPC) in precancerous cervical lesions among total population of women aged 21-24 and 25-29, by area-based measures of poverty, a Black race, and Hispanic ethnicity, Connecticut, 2008-2018 b
| Percentage of population of area-based measure b | Poverty c | Black race | Hispanic ethnicity | |||
|---|---|---|---|---|---|---|
| No. | AAPC (95% CI) | No. | AAPC (95% CI) | No. | AAPC (95% CI) | |
| Aged 21-24 | ||||||
| <5.0 | 1686 | −15.1 (−17.7 to −12.5) | 2068 | −16.1 (−19.7 to −12.4) | 1542 | −14.2 (–17.3 to –11.0) |
| 5.0-9.9 | 1067 | −15.2 (−17.8 to −12.6) | 733 | −14.2 (−16.5 to −11.8) | 1064 | −15.7 (–17.1 to –14.3) |
| 10.0-19.9 | 984 | −13.3 (−16.3 to −10.2) | 764 | −13.2 (−17.0 to −9.2) | 758 | −15.4 (−18.1 to −12.6) |
| ≥20.0 | 997 | −15.1 (−19.0 to −11.1) | 1169 | −14.7 (−18.6 to −10.5) | 1370 | −13.3 (−17.4 to −9.0) |
| Aged 25-29 | ||||||
| <5.0 | 1945 | −4.1 (−5.5 to −2.6) | 2438 | −4.1 (−6.1 to −2.2) | 1662 | −4.4 (−5.8 to −2.9) |
| 5.0-9.9 | 1437 | −3.9 (−6.3 to −1.5) | 1025 | −4.2 (−6.3 to −2.0) | 1433 | −3.7 (−5.9 to −1.3) |
| 10.0-19.9 | 1580 | −5.1 (−7.5 to −2.7) | 1225 | −5.0 (−7.2 to −2.6) | 253 | −5.0 (−7.1 to −2.9) |
| ≥20.0 | 1489 | −2.9 (−5.3 to −0.4) | 1763 | −3.5 (−6.1 to −0.8) | 2103 | −3.1 (−5.5 to −0.7) |
aArea-based measures of poverty, race, and ethnicity (percentage of the population in a census tract who were living below the federal poverty level, who were Black, and who were Hispanic) at the census-tract level divided into 4 groups using recommended cut points from the Public Health Disparities Geocoding Project. 3
bData source: HPV-IMPACT Program, Connecticut Emerging Infections Program.
cDefined as living below the federal poverty level.
When we examined trends in the incidence of CIN2+ among screened women aged 21-24, declines were slightly smaller than the declines among the total population of women aged 21-24, but overall, results were similar. Declines were significant across all 4 levels of poverty, with AAPCs ranging from −10.0% to −12.2% (Table 2). We found similar results for area-based measures of race and ethnicity. AAPCs ranged from −9.8% to −12.1% across all 4 levels of percentage Black and −10.1% to −12.3% across all 4 levels of percentage Hispanic (Table 2).
Table 2.
Average annual percentage change (AAPC) in precancerous cervical lesions among screened women aged 21-24 and 25-29, by area-based measures of poverty, Black race, and Hispanic ethnicity, Connecticut, 2008-2018 a
| Percentage of population | Poverty c | Black race | Hispanic ethnicity | |||
|---|---|---|---|---|---|---|
| No. of reported cases | AAPC (95% CI) | No. of reported cases | AAPC (95% CI) | No. of reported cases | AAPC (95% CI) | |
| Aged 21-24 | ||||||
| <5.0 | 1686 | −11.6 (−14.4 to −8.7) | 2068 | −12.1 (−14.4 to −9.8) | 1542 | −11.2 (−14.1 to −8.3) |
| 5.0-9.9 | 1067 | −12.2 (−14.2 to −10.1) | 733 | −11.1 (−14.0 to −8.0) | 1064 | −12.2 (−14.6 to −9.8) |
| 10.0-19.9 | 984 | −10.0 (−13.1 to −6.8) | 764 | −9.8 (−13.6 to −5.8) | 758 | −12.3 (−14.8 to −9.8) |
| ≥20.0 | 997 | −11.7 (−14.6 to −8.8) | 1169 | −11.4 (−14.0 to 8.8) | 1370 | −10.1 (−12.7 to −7.4) |
| Aged 25-29 | ||||||
| <5.0 | 1945 | −0.3 (−2.0 to 1.3) | 2438 | −0.2 (−2.2 to 1.9) | 1662 | −0.7 (−2.8 to −1.5) |
| 5.0-9.9 | 1437 | −0.1 (−2.6 to 2.8) | 1025 | −0.3 (−2.4 to 1.8) | 1433 | −1.3 (−3.2 to 0.6) |
| 10.0-19.9 | 1580 | −1.4 (−5.2 to 2.6) | 1225 | −1.2 (−4.7 to 2.4) | 1253 | −1.2 (−4.4 to 2.1) |
| ≥20.0 | 1489 | 1.0 (−2.7 to 4.9) | 1763 | 0.4 (−3.8 to 4.7) | 2103 | 0.7 (−3.3 to 4.9) |
aData source: HPV-IMPACT Program, Connecticut Emerging Infections Program.
bArea-based measures of poverty, race, and ethnicity (percentage of the population in a census tract who were living below the federal poverty level, who were Black, and who were Hispanic) at the census-tract level divided into 4 groups using recommended cut points from the Public Health Disparities Geocoding Project. 3
cDefined as living below the federal poverty level.
When we examined trends in the incidence of CIN2+ in the total population of women aged 25-29 by area-based measures, we observed significant declines across all levels of area-based poverty, race, and ethnicity (Table 1). As we found for women aged 21-24, the magnitudes of decline were similar to one another, with AAPCs ranging from −2.9% to −5.1% (Table 1). However, when we examined trends in this age group among screened women, declines were smaller, and none were significant in any of the area-based measures or across any of the levels (Table 2).
Discussion
Our analysis contributes to the growing body of evidence that demonstrates the population-level impact of HPV vaccination. Our results demonstrated large, significant declines in the incidence of CIN2+ among women aged 21-24 and 25-29, who were more likely than older women to have been vaccinated before exposure. We did not observe significant declines among women aged 30-34 and 35-39, who were less likely than women aged 21-24 or 25-29 to be vaccinated before exposure (if at all). During the study period, the vaccination rate for adolescent girls aged 13-17 years in Connecticut increased from 45.0% in 2008 to 69.1% in 2019. 21 These results are consistent with other studies in the United States and internationally that demonstrate the impact of HPV vaccination on young women since vaccine introduction. 11,12
Our study demonstrated similar declines in the incidence of CIN2+ among young women across all levels of area-based measures of poverty, race, and ethnicity, indicating a significant and equitable impact of vaccination on all groups. Few studies have examined the differences in trends of HPV-related disease by sociodemographic characteristics, which limits the ability to detect differences in vaccination impact and determine whether disparities in cervical cancer may be reduced or exacerbated by vaccination. Previous studies have found mixed results. 10,22 -24 Perkins et al 22 found equitable declines in rates of genital warts among racial groups over time, even though initial rates were disparate. In contrast, a study by Niccolai et al 10 found that declines in cervical lesions were smaller among women residing in areas with large proportions of residents living in poverty and racial and ethnic minority groups than among women living in areas with lower proportions of residents living in poverty and racial and ethnic minority groups.
More recently, a study from the HPV Vaccine Impact Monitoring Project, a 5-site surveillance system funded by the Centers for Disease Control and Prevention, found significant declines in HPV 16/18–associated lesions from 2008 to 2014 among non-Hispanic Black and non-Hispanic White women but not Hispanic and Asian women. 23 However, that analysis did not consider age in these racial and ethnic groups. Because the impact of vaccination is most likely to be seen among younger women, who were eligible for vaccination, the results of that study have limited implications. Another study, which examined data from Connecticut in the HPV Vaccine Impact Monitoring Project, showed that decreases in the proportion of HPV 16/18–associated lesions in young women were smaller and occurred later in areas of concentrated poverty and areas with larger proportions of Black residents when compared with areas with lower poverty and fewer Black residents. 24 It is encouraging that our analysis indicated that the impact of vaccination among young women was similar across all levels of area-based poverty, race, and ethnicity in Connecticut. Our results may be in part due to the Vaccines for Children (VFC) program. The HPV vaccine has been available in Connecticut through the VFC program since it became available in 2006. The VFC program provides vaccines at no cost for children who could not otherwise afford them, creating access for all populations.
The overall declines in the incidence of CIN2+ observed in our study are encouraging, especially in the context of moderate rates of vaccine uptake in Connecticut. The most recent estimate of vaccination coverage, in 2019, among adolescent girls and boys aged 13-17 years in Connecticut was 70.6% for 1 dose. 1 Although the rate of vaccine uptake has been slowly and steadily increasing over time, it is still well behind coverage for other adolescent vaccines such as tetanus, diphtheria, and pertussis (96.5%) and meningococcal conjugate vaccine (93.7%). 1 Documented strategies for improving vaccine uptake, such as increasing health care provider recommendations for the vaccine, improving training for medical providers on communication strategies for HPV vaccination, and community-based interventions, should be implemented across all areas to improve vaccine uptake and strengthen herd immunity. 25
Limitations and Strengths
Our study had some limitations. First, it was an ecologic analysis of cases of CIN2+ over time. We did not know the vaccination status for cases, so we cannot decisively conclude that the decrease in cases was solely due to vaccination. Other factors that may have influenced rates of cervical lesions include changes in screening practices and changes in patterns of sexual behavior, such as increased condom use and/or increased abstinence. Second, screening guidelines changed in 2009 and 2012 with the initiation of screening changing from 18 years to 21 years and the interval between screenings getting larger over time. We addressed this problem by excluding adult women aged 18-20 from the analysis and by performing a separate analysis using the screened population as the denominator to account for decreases in incidence that may have been due to the changes in screening guidelines. Third, when adjusting for screening, we produced ecologic population-level estimates by age groups. We could not geocode screening data; therefore, we could not estimate screening by area-based measures. Screening rates may have differed across levels of area-based measures. These differences could have limited the ability to detect changes across groups. Lastly, results from our analysis may not be generalizable outside Connecticut.
Our study also had several strengths. First, it was based on a robust population-based statewide surveillance system with high levels of case ascertainment. Second, it extended our previous analysis, which was conducted in a limited catchment area and used data from the same surveillance system, by including additional years of data. 24 Our current study, which examined trends in a broader catchment area of the entire state and examined overall trends, suggests that over time, the differences detected in the previous study may have diminished. 24 Finally, it builds on the analysis from the HPV Vaccine Impact Monitoring Project, which examined individual-level measures of race and ethnicity by age and provides additional evidence of vaccination impact. 23 We focused on area-based measures that are important for detecting disparities, or lack thereof, in the impact of vaccination among various populations, which can be used to design targeted interventions.
Conclusion
The declines in the incidence of CIN2+ demonstrated in our analysis are encouraging. Future cervical cancer prevention efforts should continue to focus on increasing vaccination in all populations, with a particular focus on children and adolescents aged 11-12 years to reach optimal levels of vaccination coverage to protect people, strengthen herd immunity, and maximize the impact of vaccination. Continued monitoring of vaccination impact by sociodemographic characteristics is needed to ensure widespread and equitable impact. Future studies incorporating trend analysis of vaccine uptake and cervical cancer screening by individual sociodemographic characteristics and area-based measures could detect and further inform differences identified in vaccination impact.
Acknowledgments
The Connecticut Emerging Infections Program (EIP) acknowledges James Hadler, MD, MPH, of the Connecticut EIP for his consultation on this article. In addition, we acknowledge the data collection efforts of the many students in the Yale School of Public Health over the years who have contributed to the surveillance system that provided data for this analysis. The authors also thank Lauri Markowitz, MD, Julia Gargano, PhD, and Angela Cleveland, MPH, at the Centers for Disease Control and Prevention for contributions to the surveillance project.
Footnotes
The authors declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: D.M.W. has received consulting fees from Pfizer Inc; Merck & Co, Inc; GlaxoSmithKline; and Affinivax, Inc, for work unrelated to this article and is principal investigator on research grants from Pfizer, Inc, and Merck & Co, Inc, to Yale University, which are unrelated to this article. L.M.N. has served as scientific advisor to Merck & Co, Inc.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was funded by the Centers for Disease Control and Prevention cooperative grant NU50CK000488.
ORCID iD
Monica M. Brackney, MS https://orcid.org/0000-0001-7925-8503
References
- 1. Elam-Evans LD., Yankey D., Singleton JA. et al. National, regional, state, and selected local area vaccination coverage among adolescents aged 13-17 years—United States, 2019. MMWR Morb Mortal Wkly Rep. 2020;69(33):1109-1116. 10.15585/mmwr.mm6933a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. US Department of Health and Human Services . Healthy People 2030. Accessed September 1, 2021. https://health.gov/healthypeople/objectives-and-data/browse-objectives/vaccination/increase-proportion-adolescents-who-get-recommended-doses-hpv-vaccine-iid-08
- 3. Krieger N., Chen JT., Waterman PD., Rehkopf DH., Subramanian SV. Painting a truer picture of US socioeconomic and racial/ethnic health inequalities: the Public Health Disparities Geocoding Project. Am J Public Health. 2005;95(2):312-323. 10.2105/AJPH.2003.032482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Zhan FB., Lin Y. Racial/ethnic, socioeconomic, and geographic disparities of cervical cancer advanced-stage diagnosis in Texas. Womens Health Issues. 2014;24(5):519-527. 10.1016/j.whi.2014.06.009 [DOI] [PubMed] [Google Scholar]
- 5. Clegg LX., Reichman ME., Miller BA. et al. Impact of socioeconomic status on cancer incidence and stage at diagnosis: selected findings from the Surveillance, Epidemiology, and End Results: National Longitudinal Mortality Study. Cancer Causes Control. 2009;20(4):417-435. 10.1007/s10552-008-9256-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Tabatabai MA., Kengwoung-Keumo JJ., Eby WM. et al. Disparities in cervical cancer mortality rates as determined by the longitudinal hyperbolastic mixed-effects type II model. PLoS One. 2014;9(9): 10.1371/journal.pone.0107242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Eng TY., Chen T., Vincent J., Patel AJ., Clyburn V., Ha CS. Persistent disparities in Hispanics with cervical cancer in a major city. J Racial Ethn Health Disparities. 2017;4(2):165-168. 10.1007/s40615-016-0214-3 [DOI] [PubMed] [Google Scholar]
- 8. Yoo W., Kim S., Huh WK. et al. Recent trends in racial and regional disparities in cervical cancer incidence and mortality in United States. PLoS One. 2017;12(2): 10.1371/journal.pone.0172548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Niccolai LM., Meek JI., Brackney M., Hadler JL., Sosa LE., Weinberger DM. Declines in human papillomavirus (HPV)–associated high-grade cervical lesions after introduction of HPV vaccines in Connecticut, United States, 2008-2015. Clin Infect Dis. 2017;65(6):884-889. 10.1093/cid/cix455 [DOI] [PubMed] [Google Scholar]
- 10. Niccolai LM., Julian PJ., Meek JI., McBride V., Hadler JL., Sosa LE. Declining rates of high-grade cervical lesions in young women in Connecticut, 2008-2011. Cancer Epidemiol Biomarkers Prev. 2013;22(8):1446-1450. 10.1158/1055-9965.EPI-13-0272 [DOI] [PubMed] [Google Scholar]
- 11. Gargano JW., Park IU., Griffin MR. et al. Trends in high-grade cervical lesions and cervical cancer screening in 5 states, 2008-2015. Clin Infect Dis. 2019;68(8):1282-1291. 10.1093/cid/ciy707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Drolet M, Bénard É, Pérez N, Brisson M, HPV Vaccination Impact Study Group . Population-level impact and herd effects following the introduction of human papillomavirus vaccination programmes: updated systematic review and meta-analysis. Lancet. 2019;394(10197):497-509. 10.1016/S0140-6736(19)30298-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Avni-Singer LR., Yakely A., Sheth SS., Shapiro ED., Niccolai LM., Oliveira CR. Assessing sociodemographic differences in human papillomavirus vaccine impact studies in the United States: a systematic review using narrative synthesis. Public Health. 2020;178:137-150. 10.1016/j.puhe.2019.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Krieger N., Waterman PD., Chen JT., Soobader MJ., Subramanian SV. Monitoring socioeconomic inequalities in sexually transmitted infections, tuberculosis, and violence: geocoding and choice of area-based socioeconomic measures—the Public Health Disparities Geocoding Project (US). Public Health Rep. 2003;118(3):240-260. 10.1093/phr/118.3.240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hariri S., Unger ER., Powell SE. et al. The HPV Vaccine Impact Monitoring Project (HPV-IMPACT): assessing early evidence of vaccination impact on HPV-associated cervical cancer precursor lesions. Cancer Causes Control. 2012;23(2):281-288. 10.1007/s10552-011-9877-6 [DOI] [PubMed] [Google Scholar]
- 16. Saslow D., Solomon D., Lawson HW. et al. American Cancer Society, American Society for Colposcopy and Cervical Pathology, and American Society for Clinical Pathology screening guidelines for the prevention and early detection of cervical cancer. CA Cancer J Clin. 2012;62(3):147-172. 10.3322/caac.21139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. US Census Bureau . 2010 Decennial Census. Accessed September 17, 2017. https://www.census.gov/programs-surveys/decennial-census/data/tables.2010.html
- 18. Centers for Disease Control and Prevention . Behavioral Risk Factor Surveillance System survey data. US Department of Health and Human Services, Centers for Disease Control and Prevention, 2008-2018. Accessed September 18, 2021. https://www.cdc.gov/brfss
- 19. US Census Bureau . 2010-2014 American Community Survey 5-year estimates, demographic and housing estimates. 2014. Accessed May 24, 2018. https://data.census.gov/cedsci/table?q=DP05&tid=ACSDP5Y2016.DP05
- 20. US Census Bureau . 2010-2014 American Community Survey 5-year estimates, poverty status in the past 12 months. 2014. Accessed May 24, 2018. https://data.census.gov/cedsci/table?q=S1701&tid=ACSST5Y2016.S1701
- 21. Centers for Disease Control and Prevention . Vaccination coverage among adolescents (13-17 years). Accessed September 10, 2021. https://www.cdc.gov/vaccines/imz-managers/coverage/teenvaxview/data-reports/index.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fvaccines%2Fimz-managers%2Fcoverage%2Fteenvaxview%2Fdata-reports%2Fhpv%2Fdashboard%2F2019.html
- 22. Perkins RB., Legler A., Hanchate A. Trends in male and female genital warts among adolescents in a safety-net health care system 2004-2013: correlation with introduction of female and male human papillomavirus vaccination. Sex Transm Dis. 2015;42(12):665-668. 10.1097/OLQ.0000000000000369 [DOI] [PubMed] [Google Scholar]
- 23. McClung NM., Gargano JW., Bennett NM. et al. Trends in human papillomavirus vaccine types 16 and 18 in cervical precancers, 2008-2014. Cancer Epidemiol Biomarkers Prev. 2019;28(3):602-609. 10.1158/1055-9965.EPI-18-0885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Brackney MM., Gargano JW., Hannagan SE., Meek J., Querec TD., Niccolai LM. Human papillomavirus 16/18–associated cervical lesions: differences by area-based measures of race and poverty. Am J Prev Med. 2020;58(5):e149-e157. 10.1016/j.amepre.2019.12.003 [DOI] [PubMed] [Google Scholar]
- 25. Niccolai LM., Hansen CE. Practice- and community-based interventions to increase human papillomavirus vaccine coverage: a systematic review. JAMA Pediatr. 2015;169(7):686-692. 10.1001/jamapediatrics.2015.0310 [DOI] [PMC free article] [PubMed] [Google Scholar]