Abstract
Background
Gallbladder cancer is a rare type of malignancy with overall poor prognosis. It represents the most common type of biliary tract cancer. Surgical resection can provide cure for those presenting in early stages. However, patients presenting with locally advanced or metastatic disease are considered unresectable and the first line of management in such cases is chemotherapy.
Case presentation
60 years old Saudi female with no previous medical background who was diagnosed at local hospital to have unresectable metastatic gallbladder cancer to the liver. She received 6 cycles of neoadjuvant chemotherapy as the standard protocol (Gemcitabin + Cisplatin). She showed a good response and after a multidisciplinary tumor board decision was then taken for a successful curative surgical resection (R0). Post operatively, she had another 4 cycles adjuvant chemotherapy of the same regimen. She is still on active surveillance, alive in a good condition with no local recurrence or distant metastasis after 42 months post operatively.
Discussion
Patients with gallbladder cancer are often diagnosed at late stages and those with locally advanced or metastatic gallbladder cancer are not candidates for surgical resection, even though it is a principal part of management to achieve cure. A conversion surgical resection is yet possible in selected patients initially labeled as having unresectable gallbladder cancer following neoadjuvant chemotherapy.
Conclusion
A conversion surgical resection can achieve cure in appropriately selected candidates initially labeled as unresectable gallbladder cancer following good response to neoadjuvant chemotherapy. Careful patient selection and multidisciplinary team management is recommended. Further studies are needed to standardized the management approach regarding criteria for eligible candidates, timing before considering conversion, and extent of resection.
Keywords: Conversion surgery, Curative surgical resection, Unresectable gallbladder cancer, Gemcitabin plus cisplatin
Highlights
-
•
Patients with gallbladder cancer are often diagnosed at late stages and those with locally advanced or metastatic gallbladder cancer are not candidates for surgical resection, even though it is a principal part of management to achieve cure.
-
•
The management approach for such tumor stages is a palliative systemic chemotherapy using the standard protocols of Gemcitabin + Cisplatin or clinical trial along with supportive care. Palliative radiotherapy may also play a role
-
•
The limit of surgical resection can be variable depending on the pre- and intra- operative findings ranging from only radical cholecystectomy to more aggressive procedures including major hepatic resection, extra-hepatic biliary duct resection, or adjacent organs resection depending on the tumor extensions aiming to achieve R0 resection.
-
•
Surgical resection for gallbladder cancer can be potentially curative, is not always feasible especially in locally advanced or metastatic cases. However, it should be considered whenever possible following good response to neoadjuvant chemotherapy in appropriate candidates.
1. Introduction
Among biliary tract cancer, gallbladder cancer represents the most common type. However, it is either an incidental post-operative histopathological finding in patients undergoing surgery for benign disease or is frequently diagnosed in advanced stages resulting in poor prognosis and long term survival.
Surgical resection for gallbladder cancer, although can be potentially curative, is not always feasible especially in locally advanced or metastatic cases. However, it should be considered whenever possible following good response to neoadjuvant chemotherapy in appropriate candidates after a multidisciplinary team decision.
A few conversion cases have been reported in the literature with no standardized criteria regarding patient selection, extent of resection, appropriate timing of surgical intervention for initially unresectable gallbladder cancer.
2. Case report
60 years old Saudi female not known to have any chronic medical illnesses before, complained of recurrent attacks of abdominal pain mainly over the epigastric region for 1 month duration with no other associated symptoms. She had no known family history of gallbladder cancer or other malignancies. She denied any previous genetic screening. She is married and living with her family in a good socioeconomic status.
She was worked up and fully investigated at another local hospital and then referred to our facility on March 2018 as case of advanced gall bladder cancer with liver metastasis.
Her clinical examination was unremarkable and no masses could be palpated in the abdomen. The laboratory investigations showed normal levels of the tumor markers as the following: carbohydrate antigen 19-9 (CA 19-9): 15.6, carcinoembryonic antigen (CEA): 3.7, alpha-fetoprotein (AFP): 7.23.
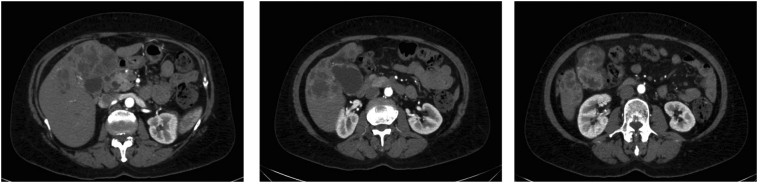
Staging computed tomography of chest, abdomen and pelvis (CT CAP) was requested for her and was suggestive for gallbladder cancer with liver invasion/metastasis. It showed a lobulated segmental soft tissue thickening involving the gallbladder wall measuring 4.1 × 1.8 cm associated with exophytic lobulated cystic component of the gallbladder fundus and multiple cystic lesion involving the surrounding liver in segment IV, V and VIII measuring 12.2 × 6 cm in its maximum widest dimension. Mildly dilated intrahepatic biliary ducts at both lobes and prominent common bile duct (CBD) with maximum caliber 1 cm. No definite obstructing lesions at the distal common bile duct and no significant enlarged abdominal or pelvic lymph nodes present (Fig. 1).
Fig. 1.
Initial CT.
An image-guided tru-cut biopsy was taken from the lesion in the left liver lobe which was positive for metastatic moderately differentiated adenocarcinoma most consistent with primary biliary or gallbladder origin.
Patient was labeled initially unresectable due to the presence of distant metastasis to the liver and the multidisciplinary tumor board decision was to start palliative chemotherapy. With an informed patient consent, she was then started on the standard protocol chemotherapy. She completed 6 cycles of Gemcitabine - Cisplatin (May 2018 till November 2018). She showed a good response to the chemotherapy and her repeated laboratory investigations was still showing normal levels of the tumor markers as the following: CA 19-9: 3.11, and CEA: 1.3.
The re-staging magnetic resonance imaging (MRI) of liver, fluorodeoxyglucose positron emissions tomography (FDG-PET) scan, and CT CAP all showed interval decrease of the gallbladder mass and adjacent liver invasion/metastasis, indicating good response to chemotherapy. There was a significant regression of previously detected exophytic soft tissue mass related to the fundus of the gallbladder currently measures 2.3 × 2 cm, residual nodularity was noted at the gallbladder wall as well as interval regression of previously detected multiple hypodense focal lesions seen involving the liver parenchyma predominantly segment IV and segment V. CBD was significantly dilated reaching up to 1.5 cm diameter with mild intrahepatic biliary dilatation but no detectable obstructing stones or lesions. No significant retroperitoneal lymph nodes with interval regression of previously detected peripancreatic lymph node currently measures 1.4 cm compared to 1.6 cm diameters. A few tiny small nodules were seen at the omentum likely representing the mesenteric lymph nodes. No peritoneal nodules or omental deposits. No ascites (Fig. 2).
Fig. 2.
Post chemotherapy.
The multidisciplinary tumor board decision was to go for a conversion surgery with an intent to cure. After obtaining an informed consent from the patient and explaining the risks versus the benefits of the surgical intervention, patient was operated on by an oncology and transplant hepatobiliary surgeon. On December 2018 she underwent open radical cholecystectomy including resection of hepatic segments IVb and V, and regional (porta hepatis) lymphadenectomy. Intra- operative ultrasonography showed no definite metastatic hepatic lesions with intra- operative frozen section confirming negative resection margins of the cystic duct.
The procedure went smoothly as planned pre operatively, no unexpected difficulties were encountered. The procedure lasted approximately 14 h with moderate amount of blood loss, however, no blood transfusion was required.
Post operatively, patient was extubated and shifted to high dependency unit (HDU) for 24 h observation uneventfully. She was then shifted to the regular surgical ward next day and had smooth post-operative period. However, on post-operative day 4, she developed pulmonary embolism (PE) confirmed on Chest CT (PE protocol) and for that was started on therapeutic anticoagulants. She was discharged home on post-operative day 11 in a stable condition.
The final histopathological examination showed: gallbladder residual moderately differentiated adenocarcinoma (tumor size of 2 cm in maximum diameter), with evidence of chemotherapy effects in both gallbladder and liver, extensive calcifications within the gallbladder, and no viable residual tumor in the liver. All surgical margins were negative for malignancy. Five excised porta hepatis lymph nodes were negative for malignancy. Final pathological stage: ypT1b, pN0, pM0 (AJCC 8th edition, 2017).
She followed up in the surgical clinic for routine post-operative care. She continued her therapeutic anticoagulants with appropriate hematology assessment and monitoring in the clinic. She was referred back to her medical oncologist one month post operatively to continue her treatment.
During her regular follow up with medical oncologist, she received another 4 cycle of Gemctabine – Cisplatin as adjuvant chemotherapy (January 2019 till May 2019).
Patient is still alive in a good condition. She is following up regularly on active surveillance with medical oncology every 6 months with repeated imaging as appropriate. Her last CT CAP done recently showed no local recurrence or distant metastasis after 3 and 1/2 years from the surgery.
3. Discussion
Gallbladder cancer, although rare, is the most common biliary tract cancer with the majority being adenocarcinomas. It is an aggressive rapidly spreading type of cancer with short-term overall survival.
Even though the tumor stage is an important prognostic indicator for gallbladder cancer, however, it is rarely detected in early stages owing to its vague nonspecific symptoms, if any. It is usually an incidental finding in patient undergoing routine cholecystectomy for presumed benign etiologies [1].
Those patients presenting with “tumor distant lymph node metastases in the celiac axis or aortocaval groove” or presenting with “metastatic disease that includes distant metastases, nodal metastases beyond the porta hepatis, and extensive involvement of the porta hepatis causing jaundice or vascular encasement” are considered unresectable [1].
Although complete surgical resection is the only potential management approach to achieve cure, it is not the standard of care for locally advanced or metastatic gallbladder cancers. The management approach for such tumor stages is a palliative systemic chemotherapy using the standard protocols of Gemcitabin + Cisplatin or clinical trial along with supportive care. Palliative radiotherapy may also play a role [1].
However, with the advancement in the chemotherapeutic agents, conversion cases have been reported in the literature for the initially unresectable gallbladder cancer that after a good response to neoadjuvant chemotherapy underwent a successful surgical resection (Table 1) [2], [3], [4], [5], [6], [7], [8], [9], [10], [11], [12], [13].
Table 1.
Cases of initially unresectable gallbladder cancer underwent conversion surgery.
| Author (year of publication) | Initial cancer status | Neoadjuvant chemotherapy | Surgical intervention |
|---|---|---|---|
|
Primary gallbladder cancer with hepatic metastasis. | Gemcitabine. | Cholecystectomy, resection of liver bed, D2 lymph node dissection, partial resection of the duodenum and transverse colon, excision of induration in hepatic segment 8 (metastasis in imaging). |
|
Primary gallbladder cancer with hepatic, colonic and duodenal invasion and para-aortic lymph node metastasis. | Gemcitabine + S-1. | Cholecystectomy, resection of liver bed, lymphadenoectomy. |
|
Primary gallbladder cancer with arterial invasion. | Gemcitabine. | Cholecystectomy, resection of liver bed, extrahepatic bile duct resection, right hemihepatectomy with caudate lobectomy. |
|
Primary gallbladder cancer with arterial invasion. | Gemcitabine. | Cholecystectomy, resection of liver bed, extrahepatic bile duct resection, right hemihepatectomy with caudate lobectomy and portal vein resection. |
|
Primary gallbladder cancer with arterial invasion. | Gemcitabine. | Cholecystectomy, resection of liver bed, extrahepatic bile duct resection, Central inferior hepatectomy (segment IVa + V), portal vein and right hepatic artery resection. |
|
Primary gallbladder cancer with arterial invasion. | Gemcitabine. | Cholecystectomy, resection of liver bed, extrahepatic bile duct resection, Central inferior hepatectomy (degment IVa + V). |
|
Primary gallbladder cancer with liver invasion, lymph nodes metastasis, perineural invasion of the common hepatic and celiac arteries. | S-1. | Cholecystectomy, resection of liver bed, right lobectomy with extrabiliary duct resection and lymphadenectomy. |
|
Primary gallbladder cancer wit para- aortic lymph nodes metastasis. | Gemcitabin + Cisplatin. | Cholecystectomy, resection of liver bed, extrahepatic biliary duct resection and lymphadenectomy. |
|
Primary gallbladder cancer with hepatic metastasis. | Gemcitabine + S-1. | Cholecystectomy, Central bisegmentectomy of liver and D2 lymph node dissection. |
|
Primary gallbladder cancer with arterial invasion, | Gemcitabin + Cisplatin. | Cholecystectomy, resection of liver bed, extrahepatic bile duct resection, right hepatic trisectionectomy, caudal lobectomy, lymphadenectomy. |
|
Primary gallbladder cancer wit para- aortic lymph nodes metastasis. | Gemcitabin + Cisplatin. | Cholecystectomy, resection of liver bed, lymphadenectomy. |
|
Primary gallbladder cancer with liver invasion, duodenum invasion, transverse colon invasion, and surrounding lymphatic metastasis. | Gemcitabin + Cisplatin. | Cholecystectomy, resection of liver bed, lymphadenectomy. |
|
Primary gallbladder cancer with para- aortic lymph nodes metastasis. | Gemcitabin + Cisplatin. | Cholecystectomy, resection of liver bed, extrahepatic bile duct resection, lymphadenectomy. |
|
Primary gallbladder cancer with invasion of liver and right hepatic artery. | Gemcitabin + Cisplatin. | Cholecystectomy, right and segment 4a liver resection, extrahepatic duct resection and cholangiojejunostomy. |
|
Primary gallbladder cancer with liver infiltration, lymph nodes metastasis on the posterior surface of pancreatic head infiltrating CBD, para- aortic lymph nodes metastasis. | Gemcitabin + Cisplatin. | Cholecystectomy, resection of liver bed, lymphadenectomy. |
The limit of surgical resection can be variable depending on the pre- and intra- operative findings ranging from only radical cholecystectomy to more aggressive procedures including major hepatic resection, extra-hepatic biliary duct resection, or adjacent organs resection depending on the tumor extensions aiming to achieve R0 resection [1].
Our patient was labeled initially unresectable due to the presence of liver metastasis; stage IVB as per AJCC (8th edition, 2017) [1].
However, after 6 cycles of neoadjuvant chemotherapy (Gemcitabin + Cisplatin), she showed a good response and a multidisciplinary tumor board recommended for a conversion surgery with curative intent. A radical surgical resection including cholecystectomy, hepatic resection of segments IVb and V (gallbladder bed) and regional (porta hepatis) lymphadenectomy was carried on. No further liver resection was needed as no definite metastatic lesions identified on intra-operative ultrasonography.
The final histopathological examination showed residual tumor of the gallbladder that is a moderately differentiated adenocarcinoma with maximum tumor size of 2 cm, evidence of chemotherapy effects in both gallbladder and liver was noted, no viable residual tumor in the liver, and the excised regional lymph nodes were all negative for metastasis, which confirms a good response to neoadjuvant chemotherapy that eventually resulted in R0 resection.
Our patient also received another 4 cycles of adjuvant chemotherapy (Gemcitabin + Cisplatin) due to the presence of residual tumor on the final histopathological examination post operatively.
She is still on active surveillance with no evidence of local recurrence or distant metastasis after 42 months from the surgery.
In conclusion, we re- emphasize on the previously elaborated importance for considering conversion surgical intervention following good response to neoadjuvant chemotherapy in those labeled initially unresectable in order to achieve cure and hence improve the long-term and cancer-free survival.
Accumulation of further cases is still needed in order to improve the current guidelines. To the date, no standardized criteria to select candidates for conversion surgery in those with initially unresectable gallbladder cancer, the duration of neoadjuvant chemotherapy before considering surgery, and the aggressiveness of the surgical intervention needed to achieve cure.
Funding
None.
Ethical approval
Not applicable.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
-
-
FA, study concept and design, data collection, data analysis and interpretation, writing the paper, artwork editing, bibliographic research
-
-
EA, data collection, data analysis and interpretation, writing the paper, bibliographic research.
-
-
RA, data collection, data analysis and interpretation, grammar correction.
-
-
MM, data analysis and interpretation, writing the paper, artwork editing. -MA, data collection, data analysis and interpretation.
Registration of research studies
Not applicable.
Guarantor
DR. Mohammed AlQahtani.
Declaration of competing interest
None.
Contributor Information
Eman Almaher, Email: emanalmaher@gmail.com.
Mohammed AlQahtani, Email: mohammedsaad.qahtani@kfsh.med.sa.
References
- 1.NCCN © 2022 National Comprehensive Cancer Network® Version 1.2022, 03/29/22.
- 2.Morimoto H., Ajiki T., Takase S., Fujita T., Matsumoto T., Mita Y., et al. Resection of gallbladder cancer with hepatic metastasis after chemotherapy with gemcitabine. J. Hepato-Biliary-Pancreat. Surg. 2008;15:655–658. doi: 10.1007/s00534-007-1311-9. [DOI] [PubMed] [Google Scholar]
- 3.Takita M., Iwasaki E., Hatogai K., Kishino R., Seki E., Izumiya M., et al. Advanced gallbladder cancer that showed complete response to gemcitabine plus S-1 chemotherapy. Nihon Shokakibyo Gakkai Zasshi. 2011;108:1263–1270. [PubMed] [Google Scholar]
- 4.Kato A., Shimizu H., Ohtsuka M., Yoshidome H., Yoshitomi H., Furukawa K., et al. Surgical resection after downsizing chemotherapy for initially unresectable locally advanced biliary tract cancer: a retrospective single center study. Ann. Surg. Oncol. 2013;20:318–324. doi: 10.1245/s10434-012-2312-8. [DOI] [PubMed] [Google Scholar]
- 5.Einama T., Uchida K., Taniguchi M., Ota Y., Watanabe K., Imai K., et al. Successful curative resection of gallbladder cancer following S-1 chemotherapy: a case report and review of the literature. Oncol. Lett. 2014;8:2443–2447. doi: 10.3892/ol.2014.2565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Adikrisna R., Nakamura N., Irie T., Matsumura S., Tanaka S., Arii S. Curative resection of stage IV advanced gallbladder cancer following combined treatment with gemcitabine and CDDP. Gan To Kagaku Ryoho. 2014;41:117–120. [PubMed] [Google Scholar]
- 7.Okumura T., Nakamura J., Kai K., Ide Y., Nakamura H., Koga H., Ide T., Miyoshi A., Kitahara K., Noshiro H. Curative resection of gallbladder cancer with liver invasion and hepatic metastasis after chemotherapy with gemcitabine plus S-1: report of a case. World J. Surg. Oncol. 2014 Nov;4(12):326. doi: 10.1186/1477-7819-12-326. PMID: 25367161; PMCID: PMC4226861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kato A., Shimizu H., Ohtsuka M., Yoshitomi H., Furukawa K., Takayashiki T., et al. Downsizing chemotherapy for initially unresectable locally advanced biliary tract cancer patients treated with gemcitabine plus cisplatin combination therapy followed by radical surgery. Ann. Surg. Oncol. 2015;22(Suppl 3):S1093–S1099. doi: 10.1245/s10434-015-4768-9. [DOI] [PubMed] [Google Scholar]
- 9.Tsuyuki H., Maruo H., Shimizu Y., Shibasaki Y., Nakamura K., Higashi Y., et al. A case of advanced gallbladder cancer with paraaortic lymph node metastases successfully treated by chemotherapy and conversion surgery. Gan To Kagaku Ryoho. 2018;45:2117–2119. [PubMed] [Google Scholar]
- 10.Hashimoto Y., Ueno K., Akita M., Tsugawa D., Awazu M., Mukubou H., et al. A case of conversion surgery following chemotherapy in initially unresectable locally advanced gallbladder carcinoma. Gan To Kagaku Ryoho. 2019;46:775–777. [PubMed] [Google Scholar]
- 11.Kato T., Matsuo Y., Ueda G., Aoyama Y., Omi K., Hayashi Y., et al. A case of gallbladder cancer with para-aortic lymph node metastasis successfully treated by gemcitabine plus cisplatin combination chemotherapy and conversion surgery. Gan To Kagaku Ryoho. 2020;47:2204–2206. [PubMed] [Google Scholar]
- 12.Inoue M., Hakoda K., Sawada H., Hotta R., Ohmori I., Miyamoto K., Toyota K., Sadamoto S., Takahashi T. Locally advanced gallbladder cancer treated with effective chemotherapy and subsequent curative resection: a case report. J. Med. Case Rep. 2022 Jan 17;16(1):30. doi: 10.1186/s13256-021-03248-9. PMID: 35039070; PMCID: PMC8764831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Miura Y., Ashida R., Sugiura T., et al. Pathological complete response achieved by gemcitabine plus cisplatin therapy for initially unresectable advanced gallbladder cancer: a case report. Surg. Case Rep. 2022;8(20) doi: 10.1186/s40792-022-01375-z. [DOI] [PMC free article] [PubMed] [Google Scholar]