Abstract
Esophagobronchial fistula (EBF) formation is a severe complication of advanced thoracic malignancies, that affects the prognosis and quality of life of patients. This study reports the case of an 80‐year‐old man with advanced esophageal cancer, complicated by EBF formation in the left main bronchus proximal to the carina following chemoradiation therapy. A fully covered stent was placed in the left main bronchus but was dislocated on the oral side. The attempt to place a partially covered self‐expandable metallic stent (SEMS) also failed due to stent dislocation on the oral side. To avoid stent dislocation, a partially covered SEMS with a length of 40 mm and a diameter of 16 mm was placed to cover the EBF in the left main bronchus. Then, a silicone Y stent (16 × 13 × 13 mm in outer diameter) was inserted to support the SEMS from the inside. After placing the SEMS and Y stent, the position of the SEMS was stabilized. The patient remained stable with adequate oral intake.
Esophagobronchial fistula (EBF) formation is a severe complication of advanced thoracic malignancies, that affects the prognosis and quality of life of patients. To avoid stent dislocation, a partially covered self‐expandable metallic stent (SEMS) with a length of 40 mm and a diameter of 16 mm was placed to cover the EBF in the left main bronchus. Then, a silicone Y stent (16 × 13 × 13 mm in outer diameter) was inserted to support the SEMS from the inside. After placing the SEMS and Y stent, the position of the SEMS was stabilized.

INTRODUCTION
The development of an esophagobronchial fistula (EBF) secondary to a thoracic malignancy causes aspiration pneumonia and is associated with a high mortality rate. A self‐expandable metallic stent (SEMS) is used to manage EBF. However, in cases involving a fistula located proximal to the carina, the SEMS is easily dislocated due to inadequate support from the proximal side. This study reports a case of EBF, located proximal to the carina, that was successfully managed by the placement of a SEMS in the left main bronchus, followed by the placement of a silicone Y stent to support the SEMS from the inside.
CASE REPORT
An 80‐year‐old man was diagnosed with advanced esophageal cancer (Mt, T4bN0M0, stage IVa). The patient was treated with chemotherapy and radiation, which achieved a partial response. Chest computed tomography (CT) revealed pneumonia in the left lung. Bronchoscopy showed an EBF at the level of the left main stem bronchus 0.5 cm from the carina (Figure 1).
FIGURE 1.
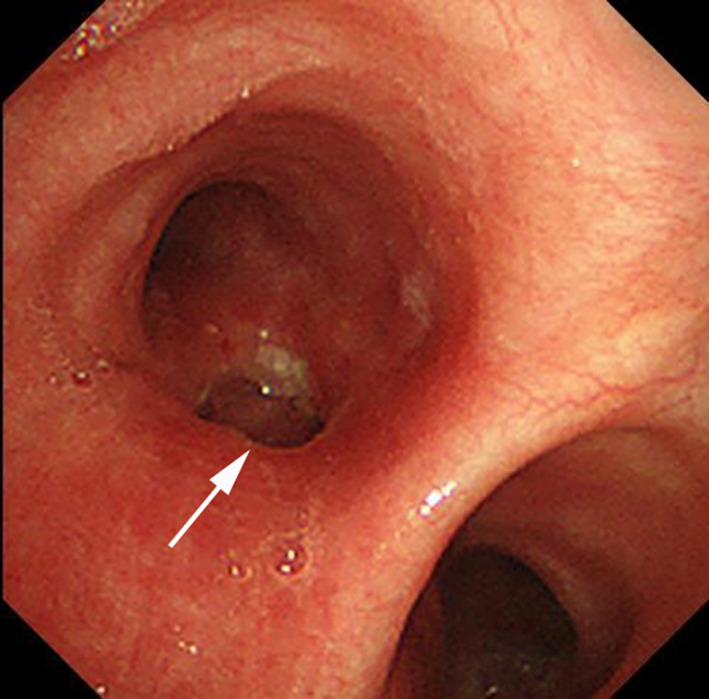
Bronchoscopy showing an esophagobronchial fistula in the left main bronchus 0.5 cm from the carina (arrow)
A covered AERO stent (Merit Medical Systems) with a length of 40 mm and a diameter of 12 mm was placed in the left main bronchus to cover the fistula. However, the stent was dislocated to the oral side after 12 days. A partially covered Ultraflex stent (Boston Scientific) with a length of 40 mm and diameter of 14 mm was placed in the same manner (Figure 2a). 6 days after insertion, the stent was dislocated proximally. This resulted in the reopening of the fistula in the left main bronchus and esophagus (Figure 2b). The dislocation was caused by the lack of contact between the proximal side of the stent and bronchial lumen. Since the fistula was located proximal to the carina, the stent was inadequately supported.
FIGURE 2.
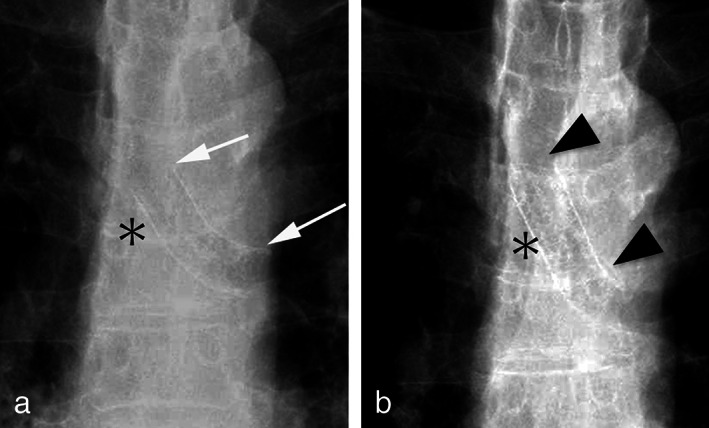
(a) Chest radiograph showing the self‐expandable metallic stent placed in the left main bronchus (arrows). (b) Chest radiograph showing the dislocation of a self‐expandable stent to the oral side (arrowheads). The location of the carina is shown by an asterisk.
To avoid recurrent SEMS dislocation, a covered Ultraflex, 40 mm in length with a diameter of 16 mm as well as a 25‐mm covered central area and 7.5‐mm uncovered mesh on both ends, was inserted to cover the EBF in the left main bronchus. Then, a silicone Y stent (16–13‐13 mm in outer diameter, Novatech) was placed via rigid bronchoscopy under general anesthesia to support the SEMS from the inside (Figure 3). After the placement of the SEMS and silicone Y stent, the patient's aspiration pneumonia showed improvement. The patient was able to take oral intake 7 days after stent placement. However, the patient died due to the progression of primary esophageal cancer 5 months after stent replacement. The SEMS and silicone Y‐stents remained in position with no noted migration.
FIGURE 3.
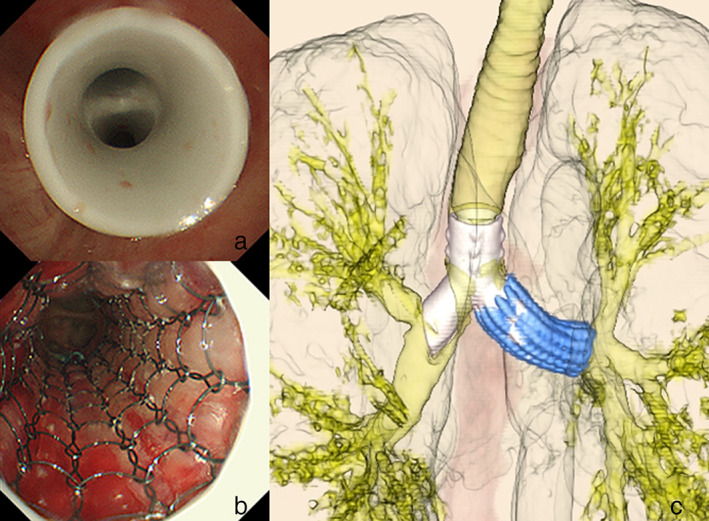
(a) Silicone Y stent is placed in the carina. (b) A silicone Y stent is placed inside a self‐expanding metallic stent (SEMS) to support the SEMS. (c) Three‐dimensional computed tomography image showing the silicone Y‐stent supporting the SEMS from the inside.
DISCUSSION
EBF formation is a negative predictor of prognosis, and patients with EBF develop aspiration pneumonia, resulting in a poor quality of life. SEMS placement is included in the standard treatment for malignant EBF. Silicone Y stents are useful for managing malignant stenosis of the carina. However, they are less suitable for EBF due to the gap between the stent and bronchial lumen, which maintains the communication between the bronchus and esophagus. Because of the negative pressure in the bronchus, even a small gap would allow fluid to flow into the bronchus from the esophagus. Therefore, it is necessary to eliminate the gap between the stent and the bronchus SEMS.
One major complication of SEMS is dislocation, which occurs in 5%–10% of cases. 1 It more commonly affects tracheal and carinal lesions than bronchial lesions. When the EBF of the left main bronchus is located proximal to the carina, keeping the SEMS intact is difficult because it is not in contact with the bronchial lumen on the oral side. Several fixation methods have been reported. Fibrin glue was used to fix the SEMS in the left main bronchus, 2 but this procedure was a temporary treatment. Internal fixation by suturing through the proximal end of the stent and the bronchial wall using rigid bronchoscopy has also been reported. 3 However, this method is difficult due to the inadequate space for suturing on the proximal side of the stent. External fixation of stents, using anchoring devices, has also been reported. 4 This procedure is applicable for cases involving the upper trachea only, and it is technically difficult.
There have been few reports on the simultaneous use of SEMS and a silicone stent in the management of EBF. 5 However, the fixation of SEMS via the placement of an overlapping silicone stent has not been reported.
This report documents a simple and straightforward method, that utilized the SEMS and a silicone Y stent to prevent SEMS migration. First, the method is technically easy to perform, and it only requires a rigid bronchoscope. Second, the silicone Y‐stent remains intact for a prolonged duration of time, and it is easily removable. Third and most importantly, this method is useful for cases of EBF, located proximal to the carina with inadequate lumen to support the proximal side of the SEMS.
To the best of our knowledge, this is the first report of a patient with EBF, successfully managed by a SEMS, followed by fixation with a silicone Y stent inside the metallic stent.
CONFLICT OF INTEREST
The authors have no conflict of interests to declare.
Ohtsuka T, Kato D, Tsukamoto Y, Shibazaki T, Nakada T, Yabe M, et al. Esophagobronchial fistula successfully managed with a self‐expandable metallic stent followed by fixation using a silicon Y stent. Thorac Cancer. 2022;13(20):2908–2910. 10.1111/1759-7714.14625
REFERENCES
- 1. Marchese R, Poidomani G, Paglino G, Crimi C, Lo Nigro C, Argano V. Fully covered self‐expandable metal stent in tracheobronchial disorders: clinical experience. Respiration. 2015;89(1):49–56. [DOI] [PubMed] [Google Scholar]
- 2. Fiorelli A, Messina G, Santoriello C, Liguori G, Arrigo E, Caronia FP, et al. Fibrin glue to fix metallic airway stent. J Thorac Dis. 2019;11(1):E4–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ehab A, Hagemann M. Internal fixation of the proximal tracheal self‐expandable metallic stent (SEMS): migration prevention in high risk patients. J Thorac Dis. 2020;12(6):3211–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Majid A, Fernandez‐Bussy S, Kent M, Folch E, Fernandez L, Cheng G, et al. External fixation of proximal tracheal airway stents: a modified technique. Ann Thorac Surg. 2012;93(6):e167–9. [DOI] [PubMed] [Google Scholar]
- 5. Chen Y, Zhou ZQ, Feng JX, Su ZQ, Zhong CH, Lu LY, et al. Hybrid stenting with silicone Y stents and metallic stents in the management of severe malignant airway stenosis and fistulas. Transl Lung Cancer Res. 2021;10(5):2218–28. [DOI] [PMC free article] [PubMed] [Google Scholar]


