Abstract
Objective
In recent years, many studies have reported good results with total hip arthroplasty (THA) for displaced femoral neck fractures (FNFs). However, no study has reported the clinical outcomes of the anterolateral modified Watson–Jones THA (MWJ-THA) for displaced FNFs. This study aimed to investigate the clinical results of THA for displaced FNFs at our hospital and to discuss the advantages of MWJ-THA over THA with other approaches for displaced FNFs.
Methods
Forty-three patients who underwent MWJ-THA for displaced FNFs were included in this study. Patient characteristics, preinjury walking ability, activities of daily living, implants used, walking ability (at 1, 3, and 6 months after surgery), cup placement angle, clinical hip score, surgical complications, revision surgery, and death within 1 year after surgery were investigated.
Results
The mean age of the 43 patients was 63.3 years, and the mean body mass index (kg/m2) was 21.1. Regarding the heads used, 28-mm heads were used in 4 patients, 32-mm heads were used in 32 patients, and 36-mm heads were used in 7 patients. The cups were placed in the Lewinnek safety zone (93.0%). Four patients had stem sinkage of a few millimeters. 6 months postoperatively, 38 patients walked unaided, and 4 patients walked with a cane. The Harris Hip Score averaged over 90 points at all time points. No postoperative dislocation was observed. Two patients died within 1 year postoperatively.
Conclusion
In this study, MWJ-THA was performed for displaced FNFs and resulted in no postoperative dislocations. Furthermore, more than 90% of the patients regained their preinjury walking ability at 6 months postoperatively. MWJ-THA has great dislocation control and is effective in treating displaced FNFs.
Keywords: clinical outcome, dislocation, femoral neck fracture, modified watson jones approach, total hip arthroplasty
Introduction
The number of femoral neck fractures (FNFs) in the elderly has been increasing in recent years and is expected to continue to increase.1 Surgical intervention, such as osteosynthesis, hemiarthroplasty (HA), and total hip arthroplasty (THA), is recommended as the treatment method. When arthroplasty is chosen, hip hemiarthroplasty is recommended for those with low physical activity due to debate over unipolar vs bipolar hemiarthroplasty. However, THA has better long-term results than HA and is often performed in highly active patients, particularly because of less cartilage damage on the postoperative acetabular side.2
In recent years, the use of THA for FNFs has been increasing because of the increase in healthy life expectancy and the number of highly active elderly patients.3 However, high postoperative dislocation rates have become a problem. The early postoperative dislocation rate of THA for FNFs was 3.4%,4 which is 2 to 4 times higher than that of THA for osteoarthritis.4,5 In particular, the posterior approach has been reported to have a dislocation rate of 3%–8%.5,6 Several studies that compared the postoperative dislocation rates of THA and HA reported dislocation rates of 4%–6% for THA and 0%–2.5% for HA.7-9
In our hospital, we chose HA for displaced FNFs in elderly patients with low activity and THA for displaced FNFs in elderly patients with high activity, patients with rheumatoid arthritis, and patients with developmental dysplasia of the hip (DDH). In most cases, we used the anterolateral modified Watson–Jones (MWJ) approach, which is a musculotendon-sparing approach described by Röttinger et al.10
In recent years, many studies have reported good results with THA for displaced FNFs, but no study has reported the clinical results of MWJ-THA for displaced FNFs. This study aimed to investigate the clinical results of THA for displaced FNFs at our hospital and to discuss the advantages of MWJ-THA over THA with other approaches for displaced FNFs.
Subjects and Methods
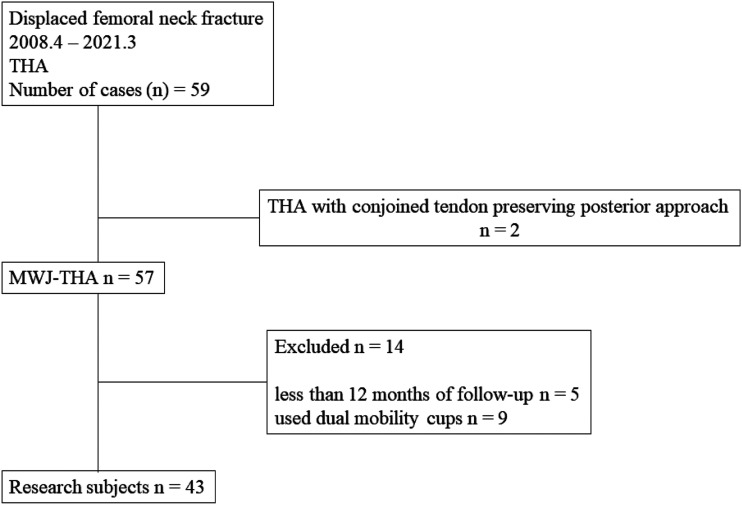
This was a retrospective analysis of 59 patients who were admitted to a single institution between April 2008 and March 2021, diagnosed with displaced FNFs, and underwent THA. Two patients underwent THA via a posterior approach were excluded from this study. 57 patients underwent THA via MWJ-THA. The exclusion criteria were having less than 12 months of follow-up (n = 5) and the use of dual mobility cups (DMCs) for comparison with previous studies which used fixed-bearing cups for displaced FNFs (n = 9). Ultimately, 43 patients were included in the study (Figure 1). The investigative protocol was approved by the Institutional Ethics Committee. All patients provided informed consent in accordance with the requirements of this review.
Figure 1.
Patient’s selection study flow chart.
Evaluation and Outcomes
We assessed patient characteristics such as age, sex, body mass index (BMI), comorbidities (other trauma, mental disorders, neuromuscular disorders, rheumatoid arthritis, and history of steroid use), pre-injury walking ability, activities of daily living (ADLs), and surgical risks determined by the anesthesiologist according to the American Society of Anesthesiologists (ASA) classification.11 Surgical information, such as the waiting period for surgery, surgical time, blood loss, use of tranexamic acid, perioperative blood transfusion, and discharge destination, was investigated. Finally, implant information was evaluated.
For the cup placement angle, the following method was used to evaluate the cups: 1 week after surgery, anteroposterior (AP) radiographs of the pelvis were obtained by focusing on the superior border of the pubic symphysis and were used to evaluate the cup alignment. One examiner (NT) measured cup alignment using Lewinnek’s method.12 Whether the cup was tilted anteriorly or posteriorly was determined using lateral radiographs of the cross table. To measure cup alignment, the method of Lewinnek et al12 (anteversion: 5°–25°; inclination: 30°–50°) was used as a safety zone.
Walking ability was assessed 1, 3, 6, and 12 months postoperatively. Walking ability was stratified into the following 5 categories: (1) use of a wheelchair or no walking, (2) use of a walker, (3) use of crutches, (4) use of a 1 stick, and (5) independent gait. The clinical hip score (Harris Hip Score [HHS]) was assessed at 3 months, 6 months, 12 months, and at the last follow-up after 12 months postoperatively. Complications from surgery (dislocation, nerve injury, intraoperative fracture, and postoperative fracture), revision surgery, and death within 1 year postoperatively were investigated. The cup placement angle and stem sinking/loosening were investigated using imaging evaluations.
Operative Procedure
MWJ-THA is a lateral supine anterolateral musculotendon-sparing procedure that was reported by Röttinger et al.10 A unique feature of this surgical entry technique is intermuscular entry, which is performed from the anterolateral side between the gluteus medius and tensor fasciae latae. Although not described in the original technique, the incised capsular ligament was preserved and repaired. The cups were set with reference to the alignment guide (operative anteversion, 20°; operative inclination, 40°). The surgery was performed or supervised by an experienced hip surgeon.
Results
Patient Characteristics, Operative Information, and Implant Information
A total of 43 patients met the inclusion criteria. Tables 1 and 2 show patient characteristics and operative information. The mean age was 63.3 years, and the mean BMI was 21.1 (kg/m2). Regarding comorbidities, 2 patients had other injuries, 4 patients had developmental hip dysplasia, and 5 patients had rheumatoid arthritis. The preinjury walking ability of most patients was unaided and their ADLs were all independent without assistance. Four patients (9.3%) were ASA class 3. The mean follow-up period was 3.1 years (minimum, 1 year; maximum, 11 years).
Table 1.
Patient Characteristics.
| Number of Patients | 43 | |
|---|---|---|
| Age mean ± standard deviation | 63.3 | ±9.0 |
| Sex (male/female) | 15/28 | |
| BMI (kg/m2) mean ± standard deviation | 21.1 | ±3.4 |
| Comorbidities | ||
| other Trauma (%) | 2 | (4.7) |
| DDH (%) | 4 | (9.3) |
| mental Disorders (%) | 3 | (7.0) |
| neuromuscular Disorders (%) | 2 | (4.7) |
| rheumatoid Arthritis (%) | 5 | (11.6) |
| history of steroid use (%) | 1 | (2.3) |
| Pre-injury walking ability | ||
| use of a wheelchair or no walking (%) | 0 | |
| use of a walker (%) | 0 | |
| use of crutches (%) | 0 | |
| use of a 1 stick (%) | 1 | (2.3) |
| independent Gait (%) | 42 | (97.7) |
| Pre-injury activities of daily living | ||
| no Assistance | 43 | (100) |
| need Assistance | 0 | |
| American Society of Anesthesiologists classification | ||
| Class 1 (%) | 4 | (9.3) |
| Class 2 (%) | 35 | (81.4) |
| Class 3 (%) | 4 | (9.3) |
| Mean follow-up period (min/max) (year) | 3.1 | (1/11) |
Table 2.
Operative Information.
| Number of Patients | 43 | |
|---|---|---|
| Surgical time (minutes) | 93 | ±40 |
| Blood loss (ml) | 240 | ±218 |
| Use of Tranexamic Acid | ||
| Yes (%) | 34 | (79.1) |
| No (%) | 9 | (20.9) |
| Perioperative blood transfusion | ||
| Yes (%) | 2 | (4.7) |
| No (%) | 41 | (95.3) |
| Postoperative load restriction | ||
| Yes (%) | 1 | (2.3) |
| No (%) | 42 | (97.7) |
Data, mean ± standard deviation.
The mean operative time was 91 min, and the mean blood loss was 266 mL. Tranexamic acid was administered during surgery starting in September 2013, and no patient required a blood transfusion after the administration of tranexamic acid. Postoperatively, all patients were allowed to walk with full load from the day after surgery, except for 1 patient who had multiple lower extremity injuries. All patients were rehabilitated beginning from the day after surgery without any limitation of the range of motion.
Table 3 summarizes the implant information. We used basically 28 mm heads in the early days. After reports of good results with highly cross-linked polyethylene liners,13 we changed our selection a 36-mm head for a cup outer diameter (O.D.) of 54 mm or more, and a 32-mm head for a cup O.D. of 52 mm or less. As a result, we used 28-mm heads in 4 patients (7.7%), 32-mm heads in 32 patients (61.5%), and 36-mm heads in 7 patients (13.5%). Cementless stems were used in >95% of the cases.
Table 3.
Implant Information.
| Number of Patients | 43 | |
|---|---|---|
| Heads | ||
| 28 (%) | 4 | (7.7) |
| 32 (%) | 32 | (61.5) |
| 36 (%) | 7 | (13.5) |
| Stems | ||
| Cement | 1 | (2.3) |
| Cementless | 42 | (97.7) |
Outcomes
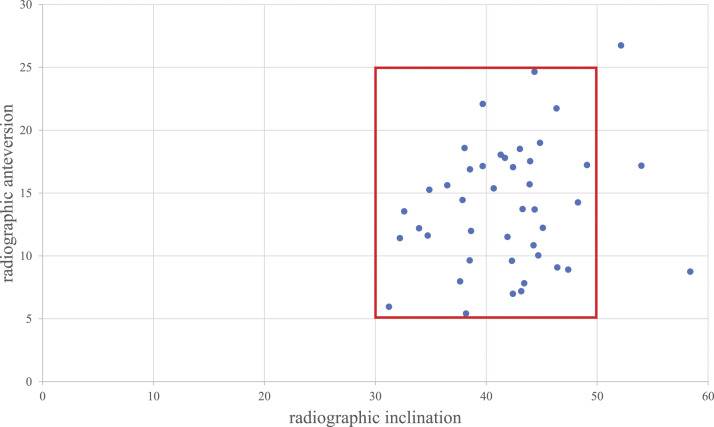
Table 4 shows walking ability at 1, 3, 6, and 12 months postoperatively by category. At 1 month post-surgery, 32 patients were able to walk unaided, and 10 were able to walk with a cane. At 6 months post-surgery, 38 patients were able to walk unaided and four were able to walk with a cane. At 6 months post-surgery, 3 patients (7.0%) had a decrease of 1 step in walking ability category compared with their conditions before the injury. Table 5 shows the HHS at 3 months, 6 months, 12 months, and at the last follow-up after 12 months postoperatively. The HHS was averaged over 90 points at all time points. This was considered a good clinical score. Postoperatively, all patients were rehabilitated without limitation of the range of motion. Table 6 shows complications related to surgery. There were no cases of intraoperative nerve injury. No postoperative dislocation was observed. There was 1 intraoperative fracture of the greater trochanter, but no additional treatment was performed. Periprosthetic fractures due to falls were observed in 2 patients after surgery: 1 occurred at 3 weeks post-surgery, and the other occurred at 5 months post-surgery. One patient underwent stem replacement and the other underwent osteosynthesis. Table 7 shows details of patients who died within 1 year after surgery. Two patients (4.7%) died within 1 year of surgery, and both had no obvious comorbidities at the time of surgery. Both deaths were due to medical illnesses and not causally related to the surgery. With regard to the cup placement angle, the average radiographic anteversion was 13.98° ± 4.99° (range: 5.42°–26.76°), and the average radiographic inclination was 42.00° ± 5.65° (range: 31.23°–58.39°). Table 8 lists the frequency distributions for all the angles in this study. Among the 43 patients, 40 (93.0%) were in the Lewinnek safety zone (Figure 2). There were 4 cases of stem sinking, all of which sank by a few millimeters. The patients had no awareness or complaints of leg length differences. No cases of stem loosening were observed.
Table 4.
Walking Ability.
| Number of Patients | 43 | |
|---|---|---|
| 1 month after surgery | ||
| use of a wheelchair or no walking (%) | 0 | |
| use of a walker (%) | 0 | |
| use of crutches (%) | 1 | (2.3) |
| use of a 1 stick (%) | 10 | (23.3) |
| independent Gait (%) | 32 | (74.4) |
| 3 months after surgery | ||
| use of a wheelchair or no walking (%) | 0 | |
| use of a walker (%) | 0 | |
| use of crutches (%) | 0 | |
| use of a 1 stick (%) | 5 | (11.6) |
| independent Gait (%) | 38 | (88.4) |
| 6 months after surgery | ||
| use of a wheelchair or no walking (%) | 0 | |
| use of a walker (%) | 0 | |
| use of crutches (%) | 0 | |
| use of a 1 stick (%) | 4 | (9.3) |
| independent Gait (%) | 38 | (88.4) |
| Deaths (%) | 1 | (2.3) |
| 12 months after surgery | ||
| use of a wheelchair or no walking (%) | 0 | |
| use of a walker (%) | 0 | |
| use of crutches (%) | 0 | |
| use of a 1 stick (%) | 4 | (9.3) |
| independent Gait (%) | 37 | (86.0) |
| Deaths (%) | 2 | (4.7) |
| Decreased walking ability by 1 or more steps | 3 | (7.0) |
Table 5.
Clinical hip score (Harris Hip Score).
| Harris Hip Score | Average | Median |
|---|---|---|
| After 3 months | 91 | 93 |
| After 6 months | 91 | 96 |
| After 1 year | 94 | 96 |
| Final follow-up after 1 years | 91 | 96 |
Table 6.
Complications related to surgery.
| Number of Patients | 5 | |
|---|---|---|
| Dislocation | 0 | |
| Nerve injury | 0 | |
| Intraoperative fracture | 1 | (2.3) |
| Postoperative periprosthetic femoral fracture | 2 | (4.7) |
| Reoperation | 2 | (4.7) |
Table 7.
Deaths within 1 year after surgery.
| Number of Patients | 2 | |
|---|---|---|
| Age at the time of surgery | Cause of death | Time of death after surgery |
| 67 | Heart failure | 11 months postoperative |
| 71 | Electrolyte disturbance | 4 months postoperative |
Table 8.
Cup placement angle.
| Angle Ranges | Number of Patients (n = 43) | Percentage of Total |
|---|---|---|
| Inclination (°) | ||
| 25-30 | 0 | 0 |
| 30-35 | 6 | 14.0 |
| 35-40 | 10 | 23.2 |
| 40-45 | 18 | 41.8 |
| 45-50 | 6 | 14.0 |
| >50 | 3 | 7.0 |
| Anteversion (°) | ||
| 0-5 | 0 | 0 |
| 5-10 | 11 | 25.6 |
| 10-15 | 13 | 30.2 |
| 15-20 | 15 | 34.9 |
| 20-25 | 3 | 7.0 |
| 25-30 | 1 | 2.3 |
Figure 2.
Scatter diagram of cup orientation. The y-axis shows radiographic inclination and the x-axis shows radiographic anteversion. The red box shows the Lewinnek safe zone.
Discussion
We studied the clinical outcomes of 43 patients who underwent MWJ-THA with fixed-bearing cups for displaced FNFs. There were no postoperative dislocations, and the mean HHS score was more than 90 points at 3 months postoperatively. In terms of walking ability, 90.5% of patients were able to walk independently at 6 months postoperatively, and 92.9% of patients regained their preinjury walking ability.
THA for FNFs is known to have a higher postoperative dislocation rate than THA for osteoarthritis4,5 and is associated with higher dislocation rates than HAs.7-9,14 There are several reasons for this finding. First, the soft tissues and muscles around the hip play an important role in joint stability; however, displaced fractures of the femoral neck are considered acute trauma, and damage to this area can lead to postoperative instability.15-17 Second, a good preoperative range of motion was maintained postoperatively with THA.7-9,14 Third, THA is more prone to dislocations than HA because the former uses a smaller head than the latter.7-9,14
Dislocation rates differ depending on the surgical approach used. The anterior approach has been reported to have a lower dislocation rate than the posterior approach.18 Noticewala et al19 studied 66 patients who underwent THA with a posterior approach for FNFs. Four cases (6.1%) of dislocations occurred within 6 months postoperatively. The head size was similar to that of the current study.19 Patient age and BMI were higher than those in the current study, but previous large-scale studies have shown that age and BMI are not risk factors for dislocation.20,21
Compared to previous reports of THA with fixed-bearing cups for FNFs, the current study had the lowest dislocation rate.19,22-25 Furthermore, the mortality rate within 1 year in our study was 4.7%, which is lower than that in the control study (Table 9). As there were no cases of THA via the posterior approach during the observation period of this study, we compared MWJ-THA and HA via the posterior approach for displaced FNFs at our hospital. So far, 295 cases of HA have been performed using the posterior approach. Of these, there were 8 cases of postoperative dislocation, with a dislocation rate of 2.7%.26 Although THA for FNF is known to have a higher dislocation rate than HA,7-9,14 the dislocation rate in our study was lower than that in our HA via the posterior approach.
Table 9.
Summary of the Literature on the Mortality and Dislocation Rates in Different Approaches.
| Studies | Year | Approach | Age | BMI (kg/m2) | Head (mm) | Dislocation Rate (%) | 12-mo Motality Rate (%) |
|---|---|---|---|---|---|---|---|
| Present study | MWJ | 63.3 | 21.1 | 28,32,36 | 0 | 4.7 | |
| Baker et al21 | 2006 | Lateral | 74.2 | N/A | 28 | 7.5 | N/A |
| Tarasevicius et al22 | 2010 | Posterior | 74 | N/A | 28,32 | 6.9 | 19.0 |
| Lim et al23 | 2016 | Anterolateral/posterior | 70 | 25.1 | N/A | 7.0 | 6.0 |
| Thurig et al24 | 2016 | DAA | 75 | N/A | 28,32 | 2.3 | 16.7 |
| Noticewala et al20 | 2018 | Posterior | 73.3 | 25.1 | 22,28,32,36 | 6.7 | N/A |
BMI, Body Mass Index; MWJ, Modified Watson–Jones approach; DAA, Direct Anterior Approach
MWJ-THA has the potential to solve these problems. We believe that it offers good protection against posterior dislocation because it preserves the posterior muscle groups, and impingement in the extended position can be checked intraoperatively because the surgery is performed in the lateral supine position.
In addition, proper cup placement is essential to prevent dislocation. In this study, it was placed in 93.0% accuracy within the Lewinnek safety zone.12 Cup placement with an alignment guide in the lateral supine position is inferior to that in the supine position. However, in our previous report, the accuracy of freehand cup placement in the MWJ approach was 92.8% in the Lewinnek safe zone and 74% in the Callanan safe zone. This indicates that our cup installation was sufficiently accurate.27 A similar result was observed in the present study. Also, through this approach there were no cups placed in retroversion, which is likely approach-related and contributes to the lack of dislocations.
The HHS in this study averaged >90 points at all time points. In a study comparing the anterior approach with other approaches, no significant differences were found; however, the median HHS score was higher in the anterior approach (94 points). The length of hospital stay was significantly shorter with the anterior approach than with the posterior approach, and better results were attributed to earlier ambulation and rehabilitation.28
In this study, periprosthetic fractures due to falls were observed in 2 patients after surgery: 1 occurred at 3 weeks post-surgery, and the other occurred at 5 months post-surgery. These patients required reoperation. Patients with proximal femoral fractures have a higher risk of falling within the first month after surgery29 and that a second fracture at the same site is more likely to occur within 48 months after injury.30 Patients who sustain proximal femoral fractures should be cautious about postoperative falls and fractures.
This study had several limitations. First, this was a retrospective cohort study, and it is possible that some information was incomplete. However, because patient data were recorded and available in the electronic medical records used in our hospital, there were no significant differences and the overall outcome was not affected. Second, this study did not include a control group that received other treatments. Considering that the posterior approach has been reported to have a high dislocation rate, we could not use such a technique in the control group because of ethical issues. Therefore, we compared MWJ THA and HA using the posterior approach performed at our hospital. Third, the follow-up period in this study was relatively short. However, given that most complications in trauma patients occur in the early postoperative period, the present results may have been sufficient to examine the clinical outcomes of MWJ-THA for FNFs. Fourth, we cannot rule out the possibility of patient selection bias. At our institution, THA for displaced FNFs is limited to highly active patients and those with rheumatoid arthritis and DDH. The mean and median patient ages in our study were 63.3 and 65 years, respectively, which are lower than those reported in other studies. The relatively low age may have affected the results because older patients tend to have more comorbidities and higher mortality rates than younger patients.
Conclusion
We investigated the clinical outcomes of MWJ-THA for displaced FNFs at our institution. There were no cases of postoperative dislocation. Furthermore, more than 80% of the patients regained their preinjury walking ability and had good clinical scores. We will continue to follow-up patients and compare their results with those of other approaches and implants.
Acknowledgments
We thank to Department of General Affairs in Toyama Prefectural Central Hospital for data organization.
Footnotes
Authors contribution: All authors listed meet the authorship criteria according to the latest guidelines of the International Committee of Medical Journal Editors. All authors are in agreement with the manuscript.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD
Naoki Takemoto https://orcid.org/0000-0002-1518-1428
References
- 1.Cooper C, Cole ZA, Holroyd CR, Earl SC, Harvey NC, Dennison EM, et al. Secular trends in the incidence of hip and other osteoporotic fractures. Osteoporos Int. 2011;22:1277-1288. doi: 10.1007/s00198-011-1601-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Migliorin F, Trivellas A, Driessen A, Quack V, El Mansy Y, Schenker H, et al. Hemiarthroplasty versus total arthroplasty for displaced femoral neck fractures in the elderly: meta-analysis of randomized clinical trials. Arch Orthop Trauma Surg. 2020;140:1695-1704. doi: 10.1007/s00402-020-03409-3. [DOI] [PubMed] [Google Scholar]
- 3.Ju DG, Rajaee SS, Mirocha J, Lin CA, Moon CN. Nationwide Analysis of Femoral Neck Fractures in Elderly Patients: A Receding Tide. J Bone Joint Surg Am. 2017;99:1932-1940. doi: 10.2106/JBJS.16.01247. [DOI] [PubMed] [Google Scholar]
- 4.Meek RMD, Allan DB, McPhillips G, Kerr L, Howie CR. Epidemiology of dislocation after total hip arthroplasty. Clin Orthop Relat Res. 2006;447:9-18. doi: 10.1097/01.blo.0000218754.12311.4a. [DOI] [PubMed] [Google Scholar]
- 5.Hailer NP, Weiss RJ, Stark A, Karrholm J. The risk of revision due to dislocation after total hip arthroplasty depends on surgical approach, femoral head size, sex, and primary diagnosis. An analysis of 78, 098 operations in the Swedish Hip Arthroplasty Register. Acta Orthop. 2012;83:442-448. doi: 10.3109/17453674.2012.733919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Prigent F. Incidence of capsular closure and piriformis pre- servation on the prevention of dislocation after total hip arthroplasty through the minimal posterior approach: Comparative series of 196 patients. Eur J Orthop Surg Traumatol. 2008;18:333-337. doi: 10.1007/s00590-008-0295-8. [DOI] [Google Scholar]
- 7.Keating JF, Grant A, Masson M, Scott N, Forbes J. Randomized comparison of reduction and fixation, bipolar hemiarthroplasty, and total hip arthroplasty. Treatment of displaced intracapsular hip fractures in healthy older patients. J Bone Joint Surg Am. 2006;88:249-260. doi: 10.2106/JBJS.E.00215. [DOI] [PubMed] [Google Scholar]
- 8.Macaulay W, Yoon RS, Parsley B, Nellans KW, Teeny SM. Displaced femoral neck fractures: is there a standard of care? Orthopedics. 2007;30:748-749. doi: 10.3928/01477447-20070901-08. [DOI] [PubMed] [Google Scholar]
- 9.Investigators H, Bhandari M, Einhorn TA, et al. Total hip arthroplasty or hemiarthroplasty for hip fracture. N Engl J Med. 2019;381:2199-2208. doi: 10.1056/NEJMoa1906190. [DOI] [PubMed] [Google Scholar]
- 10.Bertin KC, Röttinger H. Anterolateral mini-incision hip replacement surgery: a modified Watson-Jones approach. Clin Orthop Relat Res. 2004;429:248-255. doi: 10.1097/01.blo.0000150294.81825.8c. [DOI] [PubMed] [Google Scholar]
- 11.Owens WD, Felts JA, Spitznagel EL, Jr. ASA physical status classifications: a study of consistency of ratings. Anesthesiology. 1978;49:239-243. doi: 10.1097/00000542-197810000-00003. [DOI] [PubMed] [Google Scholar]
- 12.Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60:217-220. [PubMed] [Google Scholar]
- 13.Devane PA, Horne JG, Ashmore A, Mutimer J, Kim W, Stanley J. Highly Cross-Linked Polyethylene Reduces Wear and Revision Rates in Total Hip Arthroplasty: A 10-Year Double-Blinded Randomized Controlled Trial. J Bone Joint Surg Am. 2017;99(20):1703-1714. doi: 10.2106/JBJS.16.00878. [DOI] [PubMed] [Google Scholar]
- 14.Yu L, Wang Y, Chen J. Total hip arthroplasty versus hemiarthroplasty for displaced femoral neck fractures: meta-analysis of randomized trials. Clin Orthop Relat Res. 2012;470:2235-2243. doi: 10.1007/s11999-012-2293-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Guyen O, Pibarot V, Vas G, Chevillotte C, Carret JP, Bejui-Hugues J. Unconstrained tripolar implants for primary total hip arthroplasty in patients at risk for dislocation. J Arthroplasty. 2007;22:849-858. doi: 10.1016/j.arth.2006.11.014. [DOI] [PubMed] [Google Scholar]
- 16.Tarasevičius S, Robertsson O, Dobozinskas P, Wingstrand H. A comparison of outcomes and dislocation rates using dual articulation cups and THA for intracapsular femoral neck fractures. Hip Int. 2013;23:22-26. doi: 10.5301/HIP.2013.10632. [DOI] [PubMed] [Google Scholar]
- 17.Rowan FE, Salvatore AJ, Lange JK, Westrich GH. Dual-mobility vs fixed-bearing total hip arthroplasty in patients under 55 years of age: a single-institution, matched-cohort analysis. J Arthroplasty. 2017;32:3076-3081. doi: 10.1016/j.arth.2017.05.004. [DOI] [PubMed] [Google Scholar]
- 18.Zijlstra WP, De Hartog B, Van Steenbergen LN, Scheurs BW, Nelissen RGHH. Effect of femoral head size and surgical approach on risk of revision for dislocation after total hip arthroplasty. Acta Orthop. 2017;88:395-401. doi: 10.1080/17453674.2017.1317515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Noticewala M, Murtaugh TS, Danoff J, Cunn GJ, Shah RP, Geller J. Has the risk of dislocation after total hip arthroplasty performed for displaced femoral neck fracture improved with modern implants? J Clin Orthop Trauma. 2018;9:281-284. doi: 10.1016/j.jcot.2017.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Enocson A, Hedbeck CJ, Tidermark J, Pettersson H, Ponzer S, Lapidus LJ. Dislocation of total hip replacement in patients with fractures of the femoral neck. Acta Orthop. 2009;80:184-189. doi: 10.3109/17453670902930024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Abdulla I, Mahdavi S, Khong H, Gill R, Powell J, Johnston KD, et al. Does body mass index affect the rate of adverse outcomes in total hip and knee arthroplasty? A retrospective review of a total joint replacement database. Can J Surg. 2020;63:E142-E149. doi: 10.1503/cjs.006719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Baker RP, Squires B, Gargan MF, Bannister G. Total hip arthroplasty and hemiarthroplasty in mobile, independent patients with a displaced intracapsular fracture of the femoral neck. A randomized, controlled trial. J Bone Joint Surg Am. 2006;88:2583-2589. doi: 10.2106/JBJS.E.01373. [DOI] [PubMed] [Google Scholar]
- 23.Tarasevicius S, Busevicius M, Robertsson O, Wingstrand H. Dual mobility cup reduces dislocation rate after arthroplasty for femoral neck fracture. BMC Muscoskel Disord. 2010;11:175. doi: 10.1186/1471-2474-11-175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lim JW, Ng GS, Jenkins RC, Ridley D, Jariwala A, Sripada S. Total hip replacement for neck of femur fracture: comparing outcomes with matched elective cohort. Injury. 2016;47:2144-2148. doi: 10.1016/j.injury.2016.07.019. [DOI] [PubMed] [Google Scholar]
- 25.Thurig G, Schmitt JW, Slankamenac K, Werner CML. Safety of total hip arthroplasty for femoral neck fractures using the direct anterior approach: a retrospective observational study in 86 elderly patients. Patient Saf Surg. 2016;10:12. doi: 10.1186/s13037-016-0100-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nakamura T, Yamakawa T, Hori J, Goto H, Nakagawa A, Takatsu T, et al. Conjoined tendon preserving posterior approach in hemiarthroplasty for femoral neck fractures: A prospective multicenter clinical study of 322 patients. J Orthop Surg. 2021;29(3):1-8. doi: 10.1177/23094990211063963. [DOI] [PubMed] [Google Scholar]
- 27.Yoshitani J, Nakamura T, Maruhashi Y, Hashimoto N, Sasagawa T, Ueshima K, et al. Is the alignment guide technique in total hip arthroplasty sufficient for accurate cup positioning with a modified Watson Jones approach? J Orthop Surg. 2018;26:230949901880664. doi: 10.1177/2309499018806645. [DOI] [PubMed] [Google Scholar]
- 28.Elstad ZM, Buckner JF, Taunton MJ, Sherman CE, Ledford CK, Wilke BK. Outcomes of Total Hip Arthroplasty Via the Direct Anterior vs Alternative Approaches for Acute Femoral Neck Fractures. Arthroplasty Today. 2021;8:92-95. doi: 10.1016/j.artd.2021.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pils K, Neumann F, Meisner W, Schano W, Vavrovsky G, Van der Cammen TJM. Predictors of falls in elderly people during rehabilitation after hip fracture–who is at risk of a second one? Z Gerontol Geriatr. 2003;36:16-22. doi: 10.1007/s00391-003-0142-9. [DOI] [PubMed] [Google Scholar]
- 30.Nymark T, Lauritsen JM, Ovesen O, Rock ND, Jeune B. Short time-frame from first to second hip fracture in the Funen County Hip Fracture Study. Osteoporos Int. 2006;17:1353-1357. doi: 10.1007/s00198-006-0125-y. [DOI] [PubMed] [Google Scholar]