Abstract
Background:
Arthroscopic microfracture for osteochondral lesion of the talus (OLT) has shown good functional outcomes in the short and long term.
Purpose:
To investigate 5-year radiographic and clinical outcomes after arthroscopic microfracture in treatment of OLT and the effectiveness of adjunct therapies including platelet-rich plasma (PRP) and hyaluronic acid (HA).
Study Design:
Cohort study; Level of evidence, 2.
Methods:
We prospectively enrolled 432 patients who underwent arthroscopic microfracture for OLT from May 1, 2011, to May 31, 2015. Magnetic resonance imaging (MRI) and weightbearing radiographs were performed annually after the initial surgery. The MOCART (magnetic resonance observation of cartilage repair tissue) score was used to evaluate the structure of the repaired cartilage on MRI, and patient-reported outcomes (American Orthopaedic Foot and Ankle Society ankle-hindfoot scale [AOFAS] and the Foot and Ankle Outcome Score) were collected annually. The primary outcome measure was 5-year AOFAS score. We recorded baseline characteristics including age, body mass index (BMI), and lesion size, and other potentially related factors including number of PRP/HA injection and change in BMI from baseline.
Results:
Included were 355 patients, all with minimum 5-year follow-up data. The overall reoperation rate was 9.0% (32 of 355). According to multivariable analysis, 5-year AOFAS scores were associated with number of PRP injections (correlation coefficient, 3.12 [95% CI, 2.36 to 3.89]; P < .001), BMI at baseline (correlation coefficient, -0.222 [95% CI, -0.363 to -0.082]; P = .002), and mean BMI change from baseline (correlation coefficient, -1.15 [95% CI, -1.32 to -0.98]; P < .001). When comparing number of PRP injections (0, 1-2, or ≥3), we found that patients who had serial PRP injection (≥3 with at least a 3-month interval between injections) had diminished functional and radiographic deterioration over time.
Conclusion:
Arthroscopic microfracture improved patient-reported and structural outcomes for patients with OLT at 5 years after surgery. Serial PRP injections and reduction in BMI from baseline were able to slow radiographic and functional deterioration. Future trials regarding the combination of microfracture and PRP in treatment of OLT should focus on the efficacy of longer term, intra-articular, serial injections of PRP instead of single injections.
Keywords: BMI, microfracture, osteochondral lesion, platelet-rich plasma
Osteochondral lesion of the talus (OLT) is characterized by talar cartilage detachment with or without subchondral involvement and commonly affects physically active persons. 51 Arthroscopic microfracture aimed to induce the formation of regenerative fibrous cartilage for repairing OLT can reliably achieve good functional outcomes in the short term, especially for small-size defects. 10,21 Functional outcomes are expected to deteriorate over time after surgery because of the weaker structure of fibrous cartilage compared with hyaline cartilage, 29,35 with a reoperation rate ranging from 5% to 20%. 4,10,14,15,32
Many prognostic factors including age, 8 body mass index (BMI), 13 preoperative joint range of motion, 2 cystic OLT, 17 and weightbearing timing have been investigated extensively by previous studies. 45 Previous outcomes of arthroscopic microfracture for OLT have been reported based on retrospective data with a small to medium sample sizes (<200 patients). 13,23,31,41 For instance, a case series with 165 consecutive ankles failed to observe any clinically important prognostic factors on functional outcomes of arthroscopic microfracture but indicated trends toward significance for several factors including BMI and symptom duration at baseline. 10 A larger sample size might overcome this problem and further elucidate this issue.
In addition, many adjunct therapies, including platelet-rich plasma (PRP) and hyaluronic acid (HA), 19,33,43 have been recommended in combination with surgery based on functional benefits in the short term after arthroscopic microfracture. In fact, a substantial number of patients could receive these therapies repeatedly after surgery. For the retrospective data mentioned above, 13,23,31,41 the information on adjunct treatments after surgery was generally unavailable. Thus, the impact of serial and longer term application of these therapies after arthroscopic microfracture remains unknown based on currently available literature.
In this study, we aimed to determine both preoperative and postoperative prognostic factors of arthroscopic microfracture for OLT with the largest sample size to date with 5-year follow-up. In addition, consecutive radiographic data could give a meaningful insight into OLT and arthroscopic microfracture.
Methods
Patients
From May 1, 2011, to May 31, 2015, a total of 432 patients who underwent arthroscopic microfracture for OLT were prospectively enrolled into this study. Patients were eligible if they were 18 to 45 years old, had a score of ≥40 for ankle pain on a 100-point visual analog scale (higher scores indicate worse pain) during daily activities after nonoperative treatment, and had a lesion size <150 mm2 on preoperative magnetic resonance imaging (MRI). Patients were excluded from enrollment if they had bilateral OLT, a previous ankle operation for osteochondral defects, history of malignancy, or any concomitant conditions in addition to OLT that impaired their daily activity level. The protocol for this study was approved by the ethics committee of our institution, and written consent was obtained from all participants. This study complied with the code of ethics of the World Medical Association (Declaration of Helsinki) and was conducted according to The Strengthening the Reporting of Observational Studies in Epidemiology guidelines. 46
Surgical Treatment
Microfracture was performed at the time of arthroscopic surgery strictly according to the technique described in previous studies. 25,30 Briefly, all unstable and unhealthy cartilaginous and fibrous tissues were debrided to achieve a sharp perpendicular articular margin. After debridement, multiple holes (centers 3-4 mm apart and 4 mm deep) were created in the subchondral bone with a sharp surgical awl. Because of the lack of strong clinical evidence, adjunct therapies including PRP and HA were used according to the preference of the treating surgeons and patients.
Patients received intraoperative or postoperative injection of PRP or HA based on their preference after consulting with the treating surgeons. PRP was prepared using a commercially available product (WEGO Platelet-Rich Plasma Preparation Kits; WEGO), which commonly yielded a platelet concentration factor of more than 6 times over whole blood and with a platelet recovery rate of approximately 80%. The leukocytes in this PRP are no more than 4 times the concentration in whole blood. For each patient, 40 ml whole blood was collected into blood collection tubes with anticoagulant. A nurse used WEGO PRP kits used 2-time spins to collect 3 to 4 ml PRP (first time: 800g for 10 minutes; second time: 1100g for 10 minutes) at room temperature. Immediately after PRP preparation, intra-articular injection of PRP was performed. The HA used in this study was manufactured by Bausch & Lomb.
Postoperative Management
For the rehabilitation period, after immobilization with a posterior plaster splint for the initial week, partial weightbearing in a walking boot was allowed during the following 2 weeks; then, full weightbearing was encouraged as tolerated. The walking boot was removed at 8 weeks. Avoiding impact sports activities (eg, running, basketball, skiing) was recommended to all patients for 4 to 6 months. Return to sports was encouraged after 6 months. Patients were asked to report any adjunct therapies after surgery. Avoiding gaining bodyweight was regularly recommended to all patients.
Baseline and Outcome Data Collection
Baseline characteristics including age, sex, education level, BMI, and symptom duration before surgery were self-reported by patients. Patients received MRI scanning and standard weightbearing anteroposterior (AP) radiographs and lateral plain radiographs of the ankle at baseline and annually after surgery. The MOCART (magnetic resonance observation of cartilage repair tissue) score was used to evaluate the structure of repaired cartilage on MRI, 28,44 and the Kellgren-Lawrence (K-L) scoring system was used to grade radiographic osteoarthritis (ROA). 40 The MOCART scores and K-L grades were reviewed and rated by K.Y., G.M., and Y.S., who specialized in musculoskeletal radiology. A consensus on scoring was achieved after discussion.
Although lesion-size measurement under direct arthroscopic visualization has recently been recommended, 49 at the start of this study, lesion-size measurement was more commonly performed on MRI scans. 39 The size of the OLT was measured on MRI scans from the following formula 12 : lesion size = coronal maximum length × sagittal maximum length × 0.79.
For patient-reported outcomes, we adopted well-validated, self-report instruments, including the American Orthopaedic Foot and Ankle Society ankle-hindfoot scale (AOFAS) and the Foot and Ankle Outcome Score (FAOS). 27,42 These outcomes were collected annually. The AOFAS is a validated, 9-item scale and the primary patient-reported outcome of this study (range, 0-100 points; higher scores indicate less pain and better function) with 3 subscales (pain, function and alignment). 18,22 FAOS consists of 5 subscales: pain, other symptoms, activities of daily living, sport and recreation function, and foot- and ankle-related quality of life.
Because there are no well-established diagnosis criteria for ankle osteoarthritis (OA) to date, the diagnosis ankle OA in this study was determined clinically by J.Zh., J.Zo., and Z.S. on the basis of history, physical examination, and laboratory and radiographic findings. 3,37 ROA of K-L grade ≥2 was the prerequisite for clinical diagnosis of ankle OA.
Statistical Analysis
All statistical tests are 2-sided and at the .05 level of significance. All statistical analysis in this study was conducted using SPSS (Version 24.0, Chicago, IL, USA);. Continuous variables are represented as means and standard deviations, and categorical variables are represented as number (percentage). For univariable analysis, 5-year AOFAS with continuous and categorical variables were compared using the Kruskal-Wallis test and linear regression, respectively. When the yielded P value was <.2 in the univariable analysis, that variable was included in the multivariable analysis. We then constructed multivariable linear models for the association of these variables with 5-year AOFAS.
Results
Of the initial 432 included patients, there were 57 losses to follow-up within 5 years, 1 unforeseen death, and 19 consent withdrawals. Ultimately, 355 patients completed a minimum 5-year follow-up and were included for analysis. The overall reoperation rate was 9.0% (32 of 355). Notably, for patients who received revision surgery within 5 years, the outcome of the final follow-up was carried forward for the final analysis.
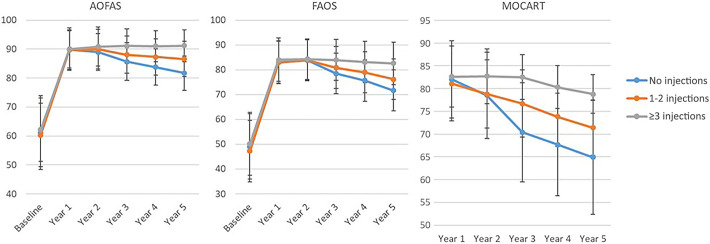
Five-Year Clinical and Radiographic Outcomes After Microfracture
The 5-year clinical and radiographic scores after microfracture are shown in Figure 1. Regarding structural outcomes on MRI scans, there was a marked improvement in MOCART scores from baseline to year 1, followed by a gradual decrease in scores over time (year 1, 81.7 ± 8.1; year 2, 79.3 ± 8.4; year 3, 74.8 ± 9.8; year 4, 72.0 ± 9.8; year 5, 69.6 ± 10.5). Regarding patient-reported outcomes, we observed a trend that the functional deterioration on the AOFAS and FAOS lagged behind the structural deterioration on MRI. Scores on the AOFAS (year 1, 89.9 ± 6.7; year 2, 89.7 ± 6.6; year 3, 87.5 ± 6.7; year 4, 86.3 ± 6.6; year 5, 85.1 ± 6.8) and FAOS (year 1, 83.1 ± 8.5; year 2, 84.0 ± 8.3; year 3, 80.3 ± 8.5; year 4, 78.1 ± 8.7; year 5, 75.1 ± 9.0) were both generally stable in the initial 2 years after surgery. Regarding radiographic outcomes, incident progression of ROA in years 1 through 5 was observed in 5 (1.4%), 15 (4.2%), 33 (9.3%), 55 (15.5%), and 71 (20.0%) patients.
Figure 1.
MRI and clinical outcomes from baseline to 5 years after microfracture for osteochondral lesion of the talus. AOFAS, American Orthopaedic Foot and Ankle Society ankle-hindfoot scale; FAOS, Foot and Ankle Outcome Score; MOCART, magnetic resonance observation of cartilage repair tissue; MRI, magnetic resonance imaging.
Univariable Analysis of Prognostic Factors
Table 1 presents demographic and clinical characteristics and evaluation using univariable analyses. The univariable analysis yielded P values <0.2 for the following variables: age at baseline, BMI at baseline, mean BMI change from baseline, lesion size, and number of PRP injection. These variables were then included into the multivariable analysis.
Table 1.
Univariable Correlation Between Demographic/Clinical Characteristics and 5-Year AOFAS a
| Categorical Variables | AOFAS Score (Mean ± SD) | Pb | |
|---|---|---|---|
| Sex | .329 | ||
| Male (n = 269) | 85.2 ± 6.8 | ||
| Female (n = 86) | 84.7 ± 7.0 | ||
| Number of PRP injections c | <.001 | ||
| 0 (n = 156) | 81.7 ± 5.9 | ||
| 1-2 (n = 148) | 86.6 ± 6.1 | ||
| ≥3 (n = 51) | 91.2 ± 5.5 | ||
| Intraoperative PRP injection | .189 | ||
| No (n = 260) | 84.8 ± 7.1 | ||
| Yes (n = 95) | 85.9 ± 5.7 | ||
| Number of HA injections c | .530 | ||
| 0 (n = 88) | 84.4 ± 8.0 | ||
| 1-2 (n = 163) | 85.4 ± 6.6 | ||
| ≥3 (n = 104) | 85.2 ± 6.1 | ||
| Intraoperative HA injection | .893 | ||
| No (n = 223) | 85.1 ± 7.0 | ||
| Yes (n = 132) | 85.2 ± 6.5 | ||
| Ankle instability at baseline d | .449 | ||
| Yes (n = 86) | 83.9 ± 6.7 | ||
| No (n = 269) | 85.4 ± 6.8 | ||
| Subchondral cyst at baseline | .869 | ||
| Yes (n = 61) | 85.6 ± 7.0 | ||
| No (n = 294) | 85.0 ± 6.8 | ||
| Continuous variables | Mean ± SD | Correlation Coefficient | Pe |
| Age at baseline, years | 28.4 ± 6.3 | −0.123 | .033 |
| BMI at baseline | 25.4 ± 3.6 | −0.172 | .084 |
| Mean BMI change from baseline f | 0.548 ± 3.11 | −1.354 | <.001 |
| Lesion size, mm2 | 95.3 ± 32.5 | 0.014 | .197 |
| Symptom duration before surgery, months | 12.3 ± 4.2 | 0.003 | .970 |
| Preoperative AOFAS score | 61.0 ± 11.8 | 0.004 | .906 |
| Preoperative FAOS score | 48.5 ± 12.8 | 0.018 | .523 |
a AOFAS, American Orthopaedic Foot and Ankle Society ankle-hindfoot scale; BMI, body mass index; FAOS, Foot and Ankle Outcome Score; HA, hyaluronic acid; PRP, platelet-rich plasma. Boldface P values indicate variables included in the multivariable analysis (P < .2).
b Kruskal-Wallis test.
c Number of injections during the study period (intraoperatively and postoperatively).
d Ankle instability was a clinical diagnosis made by the treating surgeons.
e Univariable linear regression.
f Mean BMI change from baseline = Mean BMI from years 1 through 5 minus BMI at baseline.
Multivariable Analysis of Prognostic Factors
In the multivariable analysis (Table 2), the 5-year AOFAS was associated with number of PRP injection (correlation coefficient, 3.12 [95% CI, 2.36 to 3.89]; P < .001), BMI at baseline (95% CI, -0.222 [-0.363 to -0.082]; P = .002), and mean BMI change from baseline (95% CI, -1.15 [-1.32 to -0.98]; P < .001).
Table 2.
Multivariable Linear Regression Analysis on 5-Year AOFAS a
| Correlation Coefficient (95% CI) | P | |
|---|---|---|
| Age at baseline | -0.044 (-0.125 to 0.038) | .293 |
| BMI at baseline | -0.222 (-0.363 to -0.082) | .002 |
| Mean BMI change from baseline | -1.15 (-1.32 to -0.98) | <.001 |
| Lesion size | 0.010 (-0.006 to 0.026) | .212 |
| Number of PRP injections | 3.12 (2.36 to 3.89) | <.001 |
a Boldface P values indicate significant association with 5-year AOFAS score (P < .05). AOFAS, American Orthopaedic Foot and Ankle Society ankle-hindfoot scale; BMI, body mass index, PRP, platelet-rich plasma.
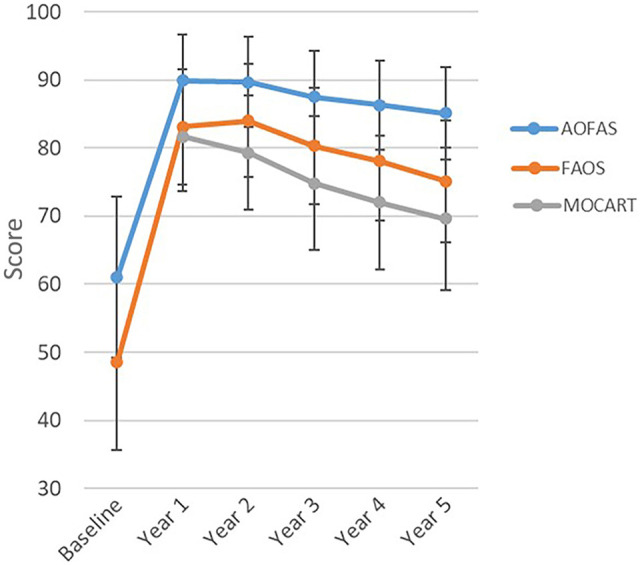
Comparison of Functional and Radiographic Outcomes by Number of PRP Injections
We further explored the role of intra-articular PRP injection by comparing functional and radiographic outcomes by number of PRP injections. In this study, 156 patients did not receive any intra-articular injection of PRP, 148 patients received single/double injection of PRP, and 51 patients received serial (≥3, range 3-9) PRP injections. We observed clear and consistent trends that the functional and radiographic deterioration could be diminished by intra-articular injection of PRP (Figure 2). The incidence of ROA progression (defined as ≥1-grade increase in K-L classification) at 5 years was significantly lower for serial PRP group (no injections: 40/156, 25.6%; 1-2 injections: 29/148, 19.6%; ≥3 injections: 2/51, 3.9%) (P < .001).
Figure 2.
Five-year radiographic and clinical outcomes according to number of PRP injections. AOFAS, American Orthopaedic Foot and Ankle Society ankle-hindfoot scale; FAOS, Foot and Ankle Outcome Score; MOCART, magnetic resonance observation of cartilage repair tissue; PRP, platelet-rich plasma.
Discussion
The current study is the largest prospective study with at least 5-year follow-up regarding the arthroscopic microfracture in treatment of OLT. In addition, an important strength of the current study was that the radiographic evaluation was performed on an annual basis, demonstrating both clinical and radiographic courses for the initial 5 years after arthroscopic microfracture for OLT. In addition, because of the prospective design, we were able to record adjunct therapies in the postoperative period more precisely than in retrospective studies. The most important finding of this study was that we observed 2 modifiable factors (number of intra-articular PRP injection and weight control after surgery) with potential to improve the prognosis of arthroscopic microfracture.
It has been well-established that the MRI findings correlate with clinical outcomes after cartilage repair surgery in the knee. 6 However, substantial controversy existed regarding the correlation between functional outcomes and MRI findings after repair for OLT. 34 A case series with 1-year follow-up found no correlation between MOCART score and patient-reported outcomes after repair of OLT. 1 In contrast, a previous study revealed that the MOCART score was in moderate association with functional outcomes at a mean of 3.6 years (range, 2.2-8.1 years) after microfracture. 47 For longer follow-up, MRI scan findings were increasingly associated with the functional prognosis over 10 years and at a level comparable with that of knee function. 24 Our data might partially explain the divergence on this issue. The structural deterioration on MRI occurred before that of functional outcomes according to our observations. Thus, any observation at a single time point might find more or less inconsistency between MRI and functional outcomes.
PRP is derived from autologous peripheral blood by a centrifugation system to obtain various type of growth factors originally stored in the α-granules in platelets. 9 Early clinical trials and meta-analysis of clinical trials recommended PRP for treating intra-articular diseases including OA and osteochondral lesion by enhancing cartilage regeneration and modulating the intra-articular environment. 16,26,38,50 Therefore, the global commercial market for PRP has increased rapidly in recent years and is projected to exceed $400 million before 2024 and $1.2 billion before 2028. 37 However, the Platelet-Rich Plasma Injections for the Management of Ankle Osteoarthritis (PRIMA) and RESTORE (a 2-group, multisite, superiority randomized clinical trial) studies, 2 high-quality, recently published, multicenter, randomized trials 5,37 have concluded decisively that PRP has no benefits in addition to placebo effects in treatment of knee and ankle OA. To the best of our knowledge, for osteochondral lesion, there remains no such decisive evidence to elucidate the efficacy of PRP, especially in the long term. A meta-analysis concluded that PRP provided a statistically significant but clinically unimportant improvement in combination with microfracture in ankles at short-term follow-up. 7 Here, we demonstrated that PRP could diminish functional and structural deterioration over time for at least 5 years after arthroscopic microfracture for OLT and there appeared to be a benefit to performing multiple PRP injections during the follow-up period.
Functional outcomes after microfracture deteriorate over time because of the weaker structure of fibrous cartilage when compared with hyaline cartilage. 4,5 Thus, many alternative and adjunct techniques, including matrix-induced autologous chondrocytes implantation technique, 31 autologous matrix-induced chondrogenesis, 7 bone marrow concentrate, 1 PRP, 32 and HA, 16 have been developed and recommended to achieve more “hyaline” repair.
We showed that both baseline BMI and change from baseline during follow-up were substantially associated with functional outcomes and structural findings on MRI scans. Increased BMI at baseline is a well-established risk factor for poor outcomes after microfracture in ankle, knee, and hip. 13,20,36,48 Likewise, we also observed an association between baseline BMI and functional/structural outcomes. The repaired tissue is fibrous cartilage with a weaker mechanical strength compared with hyaline cartilage. 29,35 Thus, the repaired cartilage is expected be more susceptible to increased bone weight. 11 In addition, all previous studies, to the best of our knowledge, did not involve BMI change from baseline. Clearly, BMI after surgery might be more important and straightforward a parameter to measure than baseline BMI.
Limitations
There are some limitations to this study. First, although we had more 300 participants who contributed data, the stratified analyses on PRP injection we conducted were still limited by inadequate power. Ideally, we should treat the number of PRP injections as a continuous variable. However, because of the limited sample size, we turned this variable into a categorical variable. The optimal number of PRP injections per year after arthroscopic microfracture for OLT remains uncertain. Since this is an ongoing study, we will hopefully be able to answer this question in the foreseeable future. Second, because this is an observational study, the decision on whether to undergo PRP injections was based on patient willingness and recommendations from the treating surgeons. It is conceivable that those patients who had a good response to the first PRP injection might be more amenable to receiving subsequent PRP injections. It is more likely that PRP did modify disease progression because PRP injection was also associated with better structural outcomes. A future confirmative randomized trial is needed to elucidate this question. Finally, it is reasonable to speculate that PRP injections are interrelated with BMI change from baseline. Conceivably, patients who had better functional outcomes were more likely to participate in physical activity. Increased physical activity could subsequently reduce BMI gain after surgery. However, the cohort was insufficiently powered to elucidate this point.
Conclusion
Arthroscopic microfracture improved patient-reported and structural outcomes for patients with OLT at 5 years after surgery. Over time, however, deterioration was seen in structural outcomes (MOCART scores), followed by deterioration in patient-reported outcomes. Serial PRP injections and a reduction in BMI from baseline could slow down the radiographic and functional deterioration. Future trials regarding the combination of microfracture and PRP in treatment of OLT should focus on efficacy of longer term, intra-articular, serial injection of PRP instead of single injections.
Footnotes
Final revision submitted July 26, 2022; accepted August 2, 2022.
One or more of the authors has declared the following potential conflict of interest or source of funding: This study was funded by Ningxia Hui Autonomous Region Key R&D Program (2020BCH01001), Shanghai Science and Technology Innovation Action Plan (20025800200), and Shanghai Municipal Technical and Scientific Commission (19441902400). AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Shanghai Sixth People’s Hospital (ref No. 2010-136).
References
- 1. Albano D, Martinelli N, Bianchi A, Giacalone A, Sconfienza LM. Evaluation of reproducibility of the MOCART score in patients with osteochondral lesions of the talus repaired using the autologous matrix-induced chondrogenesis technique. Radiol Med. 2017;122(12):909–917. [DOI] [PubMed] [Google Scholar]
- 2. Amouyel T, Barbier O, De L’Escalopier N, et al. Higher preoperative range of motion is predictive of good mid-term results in the surgical management of osteochondral lesions of the talus: a prospective multicentric study. Published online January 30, 2022. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-022-06876-w [DOI] [PubMed] [Google Scholar]
- 3. Arnold JB, Bowen CJ, Chapman LS, et al. International Foot and Ankle Osteoarthritis Consortium review and research agenda for diagnosis, epidemiology, burden, outcome assessment and treatments. Osteoarthritis Cartilage. 2022;30(7):945–955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Becher C, Malahias MA, Ali MM, Maffulli N, Thermann H. Arthroscopic microfracture vs. arthroscopic autologous matrix-induced chondrogenesis for the treatment of articular cartilage defects of the talus. Knee Surg Sports Traumatol Arthrosc. 2019;27(9):2731–2736. [DOI] [PubMed] [Google Scholar]
- 5. Bennell KL, Paterson KL, Metcalf BR, et al. Effect of intra-articular platelet-rich plasma vs placebo injection on pain and medial tibial cartilage volume in patients with knee osteoarthritis: the RESTORE randomized clinical trial. JAMA. 2021;326(20):2021–2030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Blackman AJ, Smith MV, Flanigan DC, Matava MJ, Wright RW, Brophy RH. Correlation between magnetic resonance imaging and clinical outcomes after cartilage repair surgery in the knee: a systematic review and meta-analysis. Am J Sports Med. 2013;41(6):1426–1434. [DOI] [PubMed] [Google Scholar]
- 7. Boffa A, Previtali D, Altamura SA, Zaffagnini S, Candrian C, Filardo G. Platelet-rich plasma augmentation to microfracture provides a limited benefit for the treatment of cartilage lesions: a meta-analysis. Orthop J Sports Med. 2020;8(4):2325967120910504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Brulc U, Drobnič M, Kolar M, Stražar K. A prospective, single-center study following operative treatment for osteochondral lesions of the talus. Foot Ankle Surg. 2022;28(6):714–719. [DOI] [PubMed] [Google Scholar]
- 9. Chahla J, Cinque ME, Piuzzi NS, et al. A call for standardization in platelet-rich plasma preparation protocols and composition reporting: a systematic review of the clinical orthopaedic literature. J Bone Joint Surg Am. 2017;99(20):1769–1779. [DOI] [PubMed] [Google Scholar]
- 10. Choi SW, Lee GW, Lee KB. Arthroscopic microfracture for osteochondral lesions of the talus: functional outcomes at a mean of 6.7 years in 165 consecutive ankles. Am J Sports Med. 2020;48(1):153–158. [DOI] [PubMed] [Google Scholar]
- 11. Choi WJ, Jo J, Lee JW. Osteochondral lesion of the talus: prognostic factors affecting the clinical outcome after arthroscopic marrow stimulation technique. Foot Ankle Clin. 2013;18(1):67–78. [DOI] [PubMed] [Google Scholar]
- 12. Choi WJ, Park KK, Kim BS, Lee JW. Osteochondral lesion of the talus: is there a critical defect size for poor outcome? Am J Sports Med. 2009;37(10):1974–1980. [DOI] [PubMed] [Google Scholar]
- 13. Chuckpaiwong B, Berkson EM, Theodore GH. Microfracture for osteochondral lesions of the ankle: outcome analysis and outcome predictors of 105 cases. Arthroscopy. 2008;24(1):106–112. [DOI] [PubMed] [Google Scholar]
- 14. Cogan CJ, Friedman J, You J, et al. Prior bone marrow stimulation surgery influences outcomes after cell-based cartilage restoration: a systematic review and meta-analysis. Orthop J Sports Med. 2021;9(9):23259671211035384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Dahmen J, Hurley ET, Shimozono Y, et al. Evidence-based treatment of failed primary osteochondral lesions of the talus: a systematic review on clinical outcomes of bone marrow stimulation. Cartilage. 2021;13(1)(suppl):1411S–1421S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Dai WL, Zhou AG, Zhang H, Zhang J. Efficacy of platelet-rich plasma in the treatment of knee osteoarthritis: a meta-analysis of randomized controlled trials. Arthroscopy. 2017;33(3):659–670.e651. [DOI] [PubMed] [Google Scholar]
- 17. Dankert J, Kennedy JG, Shimozono Y, Deyer T, Mercer NP. Predictors of outcomes of microfracture for osteochondral lesions of the talus. Foot Ankle Orthop. 2022;7(1):2473011421s2473000014. [Google Scholar]
- 18. De Boer AS, Meuffels DE, Van der Vlies CH, et al. Validation of the American Orthopaedic Foot and Ankle Society Ankle-Hindfoot Scale Dutch language version in patients with hindfoot fractures. BMJ Open. 2017;7(11):e018314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Doar F, Uzun E, Gürbüz K, et al. Comparison of arthroscopic treatment methods in talar osteochondral lesions: a multicenter, prospective, randomized clinical trial. J Am Podiatr Med Assoc. 2021;111(4):10.7547/20-218 [DOI] [PubMed] [Google Scholar]
- 20. Domb BG, Chen SL, Go CC, et al. Predictors of clinical outcomes after hip arthroscopy: 5-year follow-up analysis of 1038 patients. Am J Sports Med. 2021;49(1):112–120. [DOI] [PubMed] [Google Scholar]
- 21. Drakos MC, Eble SK, Cabe TN, et al. Comparison of functional and radiographic outcomes of talar osteochondral lesions repaired with micronized allogenic cartilage extracellular matrix and bone marrow aspirate concentrate vs microfracture. Foot Ankle Int. 2021;42(7):841–850. [DOI] [PubMed] [Google Scholar]
- 22. Erichsen J, Froberg L, Viberg B, Damborg F, Jensen C. Danish language version of the American Orthopedic Foot and Ankle Society Ankle-Hindfoot Scale (AOFAS-AHS) in patients with ankle-related fractures. J Foot Ankle Surg. 2020;59(4):657–663. [DOI] [PubMed] [Google Scholar]
- 23. Ferkel RD, Zanotti RM, Komenda GA, et al. Arthroscopic treatment of chronic osteochondral lesions of the talus: long-term results. Am J Sports Med. 2008;36(9):1750–1762. [DOI] [PubMed] [Google Scholar]
- 24. Giannini S, Battaglia M, Buda R, Cavallo M, Ruffilli A, Vannini F. Surgical treatment of osteochondral lesions of the talus by open-field autologous chondrocyte implantation: a 10-year follow-up clinical and magnetic resonance imaging T2-mapping evaluation. Am J Sports Med. 2009;37(suppl 1):112S–118S. [DOI] [PubMed] [Google Scholar]
- 25. Gobbi A, Francisco RA, Lubowitz JH, Allegra F, Canata G. Osteochondral lesions of the talus: randomized controlled trial comparing chondroplasty, 23 microfracture, and osteochondral autograft transplantation. Arthroscopy. 2006;22(10):1085–1092. [DOI] [PubMed] [Google Scholar]
- 26. Görmeli G, Karakaplan M, Görmeli CA, Sarikaya B, Elmali N, Ersoy Y. Clinical effects of platelet-rich plasma and hyaluronic acid as an additional therapy for talar osteochondral lesions treated with microfracture surgery: a prospective randomized clinical trial. Foot Ankle Int. 2015;36(8):891–900. [DOI] [PubMed] [Google Scholar]
- 27. Goulart Neto AM, Maffulli N, Migliorini F, de Menezes FS, Okubo R. Validation of Foot and Ankle Ability Measure (FAAM) and the Foot and Ankle Outcome Score (FAOS) in individuals with chronic ankle instability: a cross-sectional observational study. J Orthop Surg Res. 2022;17(1):38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Haleem AM, Ross KA, Smyth NA, et al. Double-plug autologous osteochondral transplantation shows equal functional outcomes compared with single-plug procedures in lesions of the talar dome: a minimum 5-year clinical follow-up. Am J Sports Med. 2014;42(8):1888–1895. [DOI] [PubMed] [Google Scholar]
- 29. Hannon CP, Smyth NA, Murawski CD, et al. Osteochondral lesions of the talus: aspects of current management. Bone Joint J. 2014;96-b(2):164–171. [DOI] [PubMed] [Google Scholar]
- 30. Jung HG, Carag JA, Park JY, Kim TH, Moon SG. Role of arthroscopic microfracture for cystic type osteochondral lesions of the talus with radiographic enhanced MRI support. Knee Surg Sports Traumatol Arthrosc. 2011;19(5):858–862. [DOI] [PubMed] [Google Scholar]
- 31. Krych AJ, Pareek A, King AH, Johnson NR, Stuart MJ, Williams RJ III. Return to sport after the surgical management of articular cartilage lesions in 24 the knee: a meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2017;25(10):3186–3196. [DOI] [PubMed] [Google Scholar]
- 32. Lambers KTA, Dahmen J, Altink JN, Reilingh ML, van Bergen CJA, Kerkhoffs G. Bone marrow stimulation for talar osteochondral lesions at long-term follow-up shows a high sports participation though a decrease in clinical outcomes over time. Knee Surg Sports Traumatol Arthrosc. 2021;29(5):1562–1569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Mei-Dan O, Carmont MR, Laver L, Mann G, Maffulli N, Nyska M. Platelet-rich plasma or hyaluronate in the management of osteochondral lesions of the talus. Am J Sports Med. 2012;40(3):534–541. [DOI] [PubMed] [Google Scholar]
- 34. Migliorini F, Maffulli N, Eschweiler J, Driessen A, Tingart M, Baroncini A. Reliability of the MOCART score: a systematic review. J Orthop Traumatol. 2021;22(1):39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Murawski CD, Kennedy JG. Operative treatment of osteochondral lesions of the talus. J Bone Joint Surg Am. 2013;95(11):1045–1054. [DOI] [PubMed] [Google Scholar]
- 36. Neri T, Dehon M, Klasan A, Putnis SE, Farizon F, Philippot R. Predictors of functional outcome after microfracture treatment of cartilage defects of the knee. Surg Technol Int. 2020;37:341–347. [PubMed] [Google Scholar]
- 37. Paget LDA, Reurink G, de Vos RJ, et al. Effect of platelet-rich plasma injections vs placebo on ankle symptoms and function in patients with ankle osteoarthritis: a randomized clinical trial. JAMA. 2021;326(16):1595–1605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Patel S, Dhillon MS, Aggarwal S, Marwaha N, Jain A. Treatment with platelet-rich plasma is more effective than placebo for knee osteoarthritis: a prospective, double-blind, randomized trial. Am J Sports Med. 2013;41(2):356–364. [DOI] [PubMed] [Google Scholar]
- 39. Ramponi L, Yasui Y, Murawski CD, et al. Lesion size is a predictor of clinical outcomes after bone marrow stimulation for osteochondral lesions of the talus: a systematic review. Am J Sports Med. 2017;45(7):1698–1705. [DOI] [PubMed] [Google Scholar]
- 40. Reijman M, Hazes JM, Koes BW, Verhagen AP, Bierma-Zeinstra SM. Validity, reliability, and applicability of seven definitions of hip osteoarthritis used in epidemiological studies: a systematic appraisal. Ann Rheum Dis. 2004;63(3):226–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Schwartz AM, Niu S, Mirza FA, Thomas AR, Labib SA. Surgical treatment of talus OCL: mid- to long-term clinical outcome with detailed analyses of return to sport. J Foot Ankle Surg. 2021;60(6):1188–1192. [DOI] [PubMed] [Google Scholar]
- 42. Seo SG, Kim JS, Seo DK, Kim YK, Lee SH, Lee HS. Osteochondral lesions of the talus. Acta Orthop. 2018;89(4):462–467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Shang XL, Tao HY, Chen SY, Li YX, Hua YH. Clinical and MRI outcomes of HA injection following arthroscopic microfracture for osteochondral lesions of the talus. Knee Surg Sports Traumatol Arthrosc. 2016;24(4):1243–1249. [DOI] [PubMed] [Google Scholar]
- 44. Shi W, Yang S, Xiong S, et al. Comparison of autologous osteoperiosteal and osteochondral transplantation for the treatment of large, medial cystic osteochondral lesions of the talus. Am J Sports Med. 2022;50(3):769–777. [DOI] [PubMed] [Google Scholar]
- 45. Song M, Li S, Yang S, Dong Q, Lu M. Is early or delayed weightbearing the better choice after microfracture for osteochondral lesions of the talus? A meta-analysis and systematic review. J Foot Ankle Surg. 2021;60(6):1232–1240. [DOI] [PubMed] [Google Scholar]
- 46. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495–1499. [DOI] [PubMed] [Google Scholar]
- 47. Yang HY, Lee KB. Arthroscopic microfracture for osteochondral lesions of the talus: second-look arthroscopic and magnetic resonance analysis of cartilage repair tissue outcomes. J Bone Joint Surg Am. 2020;102(1):10–20. [DOI] [PubMed] [Google Scholar]
- 48. Yanke AB, Wuerz T, Saltzman BM, Butty D, Cole BJ. Management of patellofemoral chondral injuries. Clin Sports Med. 2014;33(3):477–500. [DOI] [PubMed] [Google Scholar]
- 49. Yasui Y, Hannon CP, Fraser EJ, et al. Lesion size measured on MRI does not accurately reflect arthroscopic measurement in talar osteochondral lesions. Orthop J Sports Med. 2019;7(2):2325967118825261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Yausep OE, Madhi I, Trigkilidas D. Platelet rich plasma for treatment of osteochondral lesions of the talus: a systematic review of clinical trials. J Orthop. 2020;18:218–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. You JY, Lee GY, Lee JW, Lee E, Kang HS. An osteochondral lesion of the distal tibia and fibula in patients with an osteochondral lesion of the talus on MRI: prevalence, location, and concomitant ligament and tendon injuries. AJR Am J Roentgenol. 2016;206(2):366–372. [DOI] [PubMed] [Google Scholar]