Abstract
The treatment of breast cancer has improved dramatically over the past century, from a strictly surgical approach to a coordinated one, including local and systemic therapies. Systemic therapies for early-stage disease were initially tested against observation or placebo only in adjuvant trials. Subsequent clinical trials focusing on treatment ‘fine-tuning’ had a marked increase in cohort size, duration and costs, leading to a growing interest in the neoadjuvant setting in the past decade. Neoadjuvant trial designs have the advantages of enabling the direct evaluation of treatment effects on tumour diameter and offer unique translational research opportunities through the comparative analysis of tumour biology before, during and after treatment. Current technologies enabling the identification of better predictive biomarkers are shaping the new era of (neo)adjuvant trials. An urgent need exists to reinforce collaboration between the pharmaceutical industry and academia to share data and thus establish large databases of biomarker data coupled with patient outcomes that are easily accessible to the scientific community. In this Review, we summarize the evolution of (neo)adjuvant trials from the pre-genomic to the post-genomic era and provide critical insights into how neoadjuvant studies are currently designed, discussing the need for better end points and treatment strategies that are more personalized, including in the post-neoadjuvant setting.
Subject terms: Breast cancer, Drug development
Systemic therapies for early-stage disease have been tested in clinical trials for decades. The authors of this Review provide an overview of the evolution of (neo)adjuvant trials from the pre-genomic to the post-genomic era, focusing on design, end points and biomarkers that, together, could enable the delivery of more personalized treatment.
Key points
Systemic therapy for patients with early-stage breast cancer has dramatically improved over the past eight decades, and the aims and designs of (neo)adjuvant clinical trials have consistently evolved.
The transition of clinical trials from the pre-genomic to the post-genomic era has been based on a deeper understanding of disease biology and a higher level of interest in the discovery of molecular markers associated with a response to treatment.
The currently adopted approach to the design of neoadjuvant trials requires a new wave of changes, with the implementation of validated end points with more robust predictive associations with survival outcomes and more personalized treatment strategies (escalation and/or de-escalation).
The evolution towards a more personalized treatment approach is leading to increasing interest in the post-neoadjuvant setting to investigate new drugs specifically in patients with high-risk disease.
Optimizing the efficiency of the search for novel biomarkers that can guide treatment tailoring requires the establishment of large, well-annotated databases of candidate biomarkers linked with clinical outcomes that are also easily accessible to the scientific community.
Early sharing of data from clinical trials should be based on joint efforts and reinforced collaboration between the pharmaceutical industry and academic entities.
Introduction
Breast cancer is the most common malignancy among women worldwide, with an estimated >290,000 new cases and 43,000 deaths in the USA in 2022 (ref.1). These numbers are likely to be biased by the COVID-19 pandemic, which has led to reduced access to care and, consequently, to delays in diagnosis. These delays translate into a short-term lower incidence, albeit with a greater number of patients having more advanced-stage disease at diagnosis and, ultimately, increased mortality2. Thus, breast cancer has long been and remains a major public health problem.
Decades of research have demonstrated that breast cancer is a complex and heterogeneous disease and have provided meaningful advances in treatment options for patients, with substantial improvements in clinical outcomes over the years3. In this Review, we summarize the steps taken in the development of systemic therapies for patients with early-stage breast cancer, from the pre-genomic to the post-genomic era and from the identification of novel active agents to a deeper understanding of disease biology and the discovery of predictive biomarkers.
We provide critical insights into the design pitfalls of studies involving patients with early-stage breast cancer, discuss the need for better end points and propose new ways of thinking in order to address these issues. Finally, we highlight the ability of new technologies to identify novel predictive markers of efficacy that are shaping the new era of early-stage breast cancer trials.
The evolution of breast cancer treatment
The treatment of patients with breast cancer has evolved dramatically over the past century, from a strictly surgical approach to a multidisciplinary one, including radiotherapy, chemotherapy, endocrine therapy, targeted therapy and immunotherapy. This evolution has arisen from a progressively deeper understanding of the disease and from the recognition of salient, peculiar features that make it different to other cancer types4. Firstly, patients with node-positive disease have a higher risk of relapse in the absence of specific therapies and derive the greatest magnitude of benefit from systemic adjuvant treatments. Secondly, two-thirds of patients with breast cancer have hormone receptor (HR)-positive disease and benefit from the inhibition of oestrogen receptor (ER) signalling, using various endocrine therapies. Thirdly, breast cancer is a tremendously heterogeneous and complex disease and genetic alterations that might occur and/or drive cancer development could be useful targets for specifically designed therapies. These achievements in understanding breast cancer have been mirrored by the successful development of drugs that have been demonstrated to reduce the risk of disease relapse and death in randomized trials.
The first large-cohort studies in the adjuvant setting involving patients with early-stage breast cancer focused on the role of adjuvant chemotherapy and were either non-randomized or compared the use of chemotherapy with observation or placebo alone5–7. The findings of these seminal studies testing the role of adjuvant chemotherapy, which started in 1957 (refs.5,7,8), were confirmed in subsequent studies conducted by the National Surgical Adjuvant Breast and Bowel Project (NSABP)8 and, ultimately, by large meta-analyses led by the Early Breast Cancer Trialists’ Collaborative Group (EBCTCG)6,9. These analyses demonstrated meaningful reductions in the annual incidence of breast cancer recurrence and mortality (28% and 16%, respectively) with adjuvant chemotherapy regimens comprising several different agents9.
A first step towards a more personalized treatment approach was the evaluation of adjuvant endocrine therapy for patients with HR-positive breast cancer. In the early 1980s, seminal studies led by the Nolvadex Adjuvant Trial Organisation (NATO)10,11 and the NSABP12 provided the first data indicating clinical benefit for patients with early-stage breast cancer receiving adjuvant tamoxifen. Some years later, the EBCTCG confirmed these improvements in survival outcomes based on the pooled data of 30,000 women coming from a worldwide collaboration, where tamoxifen was associated with a highly significant reduction in the annual incidence of both disease recurrence and mortality (25% and 17%, respectively)9.
Finally, the advent of HER2-targeted therapies for patients with HER2-positive breast cancer marked another milestone, based on fruitful cooperation between basic research scientists and clinical investigators, in the evolution towards more personalized treatment. The HERA trial13 demonstrated that 1 year of trastuzumab after adjuvant chemotherapy confers a significant survival benefit in these patients (10-year disease-free survival (DFS) benefit of 6–8% for patients receiving trastuzumab)14; this result was confirmed in similar adjuvant trials and in an EBCTCG meta-analysis published in 2021 (ref.15).
Evolution of adjuvant clinical trials
This first wave of seminal clinical trials comparing cancer therapies with observation alone or placebo was followed by a second generation of more sophisticated and refined studies comparing different interventions with each other, including different chemotherapy regimens (such as those based on anthracycline versus combinations based on anthracycline and taxane)6, different endocrine therapies (such as tamoxifen versus aromatase inhibitors)16 and different targeted treatment strategies (such as single versus dual HER2 inhibition)17. The limited differences in magnitudes of benefit associated with these treatment modalities could not always be detected in cohorts of a suboptimal sample size. Therefore, the role of the EBCTCG in conducting periodic patient-level meta-analyses became vital in demonstrating small but significant risk reductions: the addition of a taxane to an anthracycline-based regimen in patients with node-positive breast cancer was associated with a reduction in 8-year disease recurrence of 4.6%, a reduction in 8-year breast cancer mortality of 2.8% and a reduction in 8-year all-cause mortality of 3.2%, respectively6. Similarly, 10-year breast cancer mortality was found to be lower with aromatase inhibitors than with tamoxifen, albeit with a modest reduction of 2.1% (12.1% vs 14.2%; P = 0.009)6,16.
This second wave of studies led to a recognition of the need for a marked increase in trial sample size (of several thousands of patients), despite the exponentially higher costs associated with this change in approach and the continued lack of a guarantee of success. Some examples include the D-care18, BEATRICE19 and ALTTO20 studies, all of which are randomized studies with large cohorts that nonetheless failed to demonstrate statistically significant improvements for patients receiving the experimental treatments (Supplementary Table 1). In the ALTTO trial20, investigators randomly assigned 8,381 patients to 1 year of adjuvant therapy with either trastuzumab, lapatinib (a small-molecule inhibitor of both HER2 and EGFR), or both agents either in sequence or in combination. The lapatinib arm of ALTTO was closed in 2011 owing to inferiority relative to trastuzumab and, at the protocol-specified analysis cut-off, dual inhibition of HER2 with trastuzumab plus lapatinib did not improve DFS compared with trastuzumab alone. By contrast, in the APHINITY trial, dual HER2 inhibition with trastuzumab plus pertuzumab conferred a significant improvement in invasive DFS relative to trastuzumab, albeit with an improvement in 6-year event-free survival (EFS) of only 2.8% (ref.17).
Notably, the magnitude of benefit derived from dual versus single HER2 inhibition was similar in the two studies (hazard ratio for DFS in ALTTO was 0.84, 97.5% CI 0.70–1.02; P = 0.048; in APHINITY, the hazard ratio for invasive DFS was 0.81, 95% CI 0.66–1.00; P = 0.045)20,21. The apparent failure of ALTTO and success of the same approach in APHINITY likely reflect differences in statistical assumptions22.
Increasing interest in neoadjuvant trials
Neoadjuvant approaches were initially developed for patients with locally advanced and/or inoperable cancers using radiotherapy, chemotherapy or a combination of the two in an attempt to render tumours operable and/or reduce tumour burden. However, data from preclinical models also suggested the potential for an additional therapeutic advantage for certain aggressive cancers as chemotherapy might decrease the replication rate of cancer cells23. Neoadjuvant systemic therapy was subsequently advocated as a method of increasing the feasibility of breast conservation in women considered ineligible for such an approach at diagnosis. With the landmark NSABP-B18 trial24 demonstrating equivalent DFS and overall survival (OS) with pre-surgical versus post-surgical administration of four cycles of doxorubicin plus cyclophosphamide, trust in the preoperative administration of systemic therapy grew rapidly.
Increasing interest was also motivated by other advantages of the neoadjuvant approach, including the possibility of rapid, direct evaluation of treatment effects based on measurements of tumour diameter and the research opportunities provided by comparative investigations of tumour biology before, during and after treatment25 (Table 1). Widespread adoption of the neoadjuvant approach was ultimately conferred by use of the surrogate end point of pathological complete response (pCR) as a fast and ready-to-use surrogate for long-term outcomes.
Table 1.
Evolution of neoadjuvant chemotherapy and endocrine therapy for patients with breast cancer
| Era | Major goals | Outcome achieved? |
|---|---|---|
| Neoadjuvant chemotherapy | ||
| 1980s | Improved uptake of breast-conserving surgery | Yes |
| 1990s | Improved survival outcomes owing to earlier treatment | No |
| 2000s onwards | Identification of active novel therapies | Sometimes |
| 2010s onwards | Treatment tailoring | Poor effectiveness until now |
| Neoadjuvant endocrine therapy | ||
| 1980s | Improved treatment of elderly patients (>70–75 years)a | Yes |
| 1990s | Improved uptake of breast-conserving surgery | Yes |
| 2000s onwards | Identification of active novel therapies | Sometimes |
| 2010s onwards | Treatment tailoring | Poor effectiveness until now |
aOf note, no consensus exists on the cutoff to be used, and age should be considered together with other variables, such as performance status, comorbidities, social support, and cognition and psychological status.
Interestingly, pCR has been supported by the FDA as a surrogate end point for the accelerated approval of new drugs tested in the neoadjuvant setting in randomized clinical trials26, although a ‘positive opinion’ has also been contingent on the results of clinical trials testing the same concept in another setting (such as in patients with metastatic disease). Therefore, the past 10 years have perhaps unsurprisingly witnessed exponential growth in the design and implementation of neoadjuvant trials with small cohorts that were adequately powered to detect a difference in pCR but unable to demonstrate any difference in EFS.
In 2014, a relevant association between pCR and OS was demonstrated only at the patient level in an FDA-sponsored seminal meta-analysis27 and further evidence has since confirmed a lack of surrogacy of pCR at the trial level28, which raises questions regarding the role of pCR as a primary end point in ‘pivotal’ neoadjuvant trials. Surrogate end points should only be accepted as evidence supporting drug approval when these end points have been sufficiently validated and are therefore known to accurately predict the effects of a drug over time. The role of neoadjuvant trials has also evolved over time, particularly with the transition from the pre-genomic to the post-genomic era.
Entering the post-genomic era
The Human Genome Project29 and its efforts to sequence the entire human genome were a milestone in clinical research and marked the end of the so-called pre-genomic era and the beginning of the post-genomic one. Analysis of DNA, RNA and protein sequence data is now an essential part of biomedical research30.
In breast cancer, these achievements have translated into a new way of thinking about neoadjuvant clinical trials. The key questions explored by neoadjuvant trials in the pre-genomic era mainly focused on the possibility of identifying active agents and predicting their success or on fine-tuning their administration schedules. Seminal research in this setting has led to milestones in today’s clinical practice such as the use of docetaxel in sequence with an anthracycline-based regimen instead of anthracycline-based chemotherapy alone31, the administration of weekly instead of 3-weekly paclitaxel32, and the superiority of adjuvant aromatase inhibitors compared to tamoxifen33,34.
All of these studies, conducted in the neoadjuvant setting, shared the peculiarity of being deemed ‘hypothesis generating’, with confirmatory results obtained subsequently in large adjuvant trials (Table 2). Neoadjuvant trials from the pre-genomic era had merit in that they addressed important clinical questions; however, many of these trials were characterized by disappointing results in the search for predictive biomarkers and, ultimately, a failure to identify effective biomarkers of response with the potential to enable the tailoring of treatment with taxanes35,36 and/or aromatase inhibitors33,37.
Table 2.
Examples of hypothesis-generating trials and their related hypothesis-confirming trials
| Key question | Hypothesis-generating trial | Key results | Confirmatory adjuvant study |
|---|---|---|---|
| Anthracyclines followed by taxanes versus anthracyclines alone | ABERDEEN31, in which 162 patients received neoadjuvant CVAP (four cycles), followed by randomization (1:1) to a further four cycles of CVAP versus docetaxel in the 97 patients with a PR or better on initial CVAP | Improved ORR (94% vs 64%; P = 0.001), pCR rate (34% vs 16%; P = 0.04) and 3-year OS (P = 0.05) in patients receiving sequential docetaxel | Taxanes plus anthracyclines significantly reduce the 8-year risks of disease recurrence (30.2% vs 34.8%; RR 0.84, 95% CI 0.78–0.91; P = 0.00001), disease-specific mortality (21.1% vs 23.9%; RR 0.86, 95% CI 0.79–0.93; P = 0.0005) and overall mortality (23.5% vs 26.7%; RR 0.86, 95% CI 0.79–0.93; P = 0.0002) relative to anthracyclines only in a patient-level meta-analysis of data from 11,167 patients |
| Weekly versus 3-weekly paclitaxel | Green et al. (2005)32, in which 258 patients were randomized (1:1) to receive four cycles of weekly versus 3-weekly paclitaxel followed by four cycles of 3-weekly FAC | Improved pCR rate in patients receiving weekly paclitaxel (28.2% vs 15.7%; P = 0.02) | Weekly paclitaxel led to significant improvements in DFS (HR 0.84, 95% CI 0.73–0.96; P = 0.011) and OS (HR 0.87, 95% CI 0.75–1.02; P = 0.09) in a cohort of 4,954 patients receiving either weekly or 3-weekly paclitaxel or docetaxel following four cycles of doxorubicin plus cyclophosphamide116 |
| Aromatase inhibitors versus tamoxifen | Ellis et al. (2001)33, in which 324 patients were randomized (1:1) to 4 months of neoadjuvant letrozole versus tamoxifen | Significantly improved ORR (60% vs 41%; P = 0.004) and BCS rates (48% vs 36%; P = 0.036) with aromatase inhibitors | Aromatase inhibitors significantly reduce the 10-year risk of disease recurrence (19.1% vs 22.7%, 95% CI 1.7–5.4; P < 0.00001), cancer-specific mortality (12.1% vs 14.2%, 95% CI 0.5–3.7; P = 0.009) and all-cause mortality (21.3% vs 24.0%, 95% CI 0.1–4.7; P = 0.01) in a patient-level meta-analysis of data from 31,920 patients16 |
| Dowsett et al.34,42, in which 330 patients were randomized (1:1:1) to 3 months of neoadjuvant tamoxifen, anastrozole, or tamoxifen plus anastrozole | No significant difference in ORRs between groups (ORRs 37%, 36% and 39%, respectively); significantly more patients in the anastrozole group became eligible for BCS relative to the tamoxifen group (46% vs 22%, respectively; P = 0.03) |
BCS, breast-conserving surgery; CVAP, cyclophosphamide plus vincristine, doxorubicin and prednisone; DFS, disease-free survival; FAC, fluorouracil plus doxorubicin and cyclophosphamide; ORR, overall response rate; OS, overall survival; pCR, pathological complete response; PR, partial response.
Neoadjuvant trials from the post-genomic era have maintained an important role in identifying new active agents worthy of further investigation in the adjuvant setting. An example of this role is provided by dual inhibition of HER2 with pertuzumab plus trastuzumab, which was the first treatment to receive FDA accelerated approval based on pCR results alone from a relatively small (n = 417) neoadjuvant study (NeoSphere)38. The effectiveness of this approach was later confirmed in a larger cohort (n = 4,805) in the adjuvant setting (APHINITY)21, resulting in full approval for use in both settings in December 2017. We believe that the KEYNOTE-522 trial marks the beginning of a new era in the history of neoadjuvant trials: this large (n = 1,174), phase III study led to the approval of neoadjuvant pembrolizumab in combination with chemotherapy for patients with high-risk, early-stage triple-negative breast cancer (TNBC) in July 2021, based on significant improvements in pCR and EFS, its two co-primary end points39,40. An important lesson had been understood: a pCR improvement on its own is not a reliable surrogate of survival and should be supported by a survival end point for regulatory approval. Beyond the important role of identifying new active agents, the neoadjuvant trials of the post-genomic era have prioritized another relevant objective: the deep dissection of disease biology and the search for clinically useful molecular markers of response.
Biomarkers and disease biology
HR-positive, HER2-negative breast cancer
Since the late 1980s, a strong preclinical rationale has supported the hypothesis that a short, preoperative course of endocrine therapy could improve outcomes in HR-positive early-stage breast cancer41. However, the choice of the best end point to predict patient outcomes after such therapy has been a topic of intense academic debate. Data from two small neoadjuvant studies, IMPACT42 and Z1031 (ref.43), showed that levels of the nuclear protein Ki67, assessed 2–4 weeks after starting neoadjuvant endocrine therapy, might better predict patient outcomes than Ki67 levels at baseline. In the POETIC trial44, 4,480 postmenopausal women with HR-positive, HER2-negative early-stage breast cancer were randomly assigned to receive either aromatase inhibitors or placebo for 14 days prior to surgery. Adjuvant treatment was permitted as per standard local practice. The POETIC trial failed to show any significant differences in treatment outcomes; importantly, however, patients with a low Ki67 level at baseline (<10%) and/or after 2 weeks of treatment had a significantly lower risk of disease recurrence compared with those with a high level at 2 weeks44, suggesting that ‘dynamic’ measurements of Ki67 levels could help select patients who might not need further treatment escalation (those showing substantial Ki67 suppression). For patients without a Ki67 response, current escalated treatments (such as chemotherapy) do not provide strong evidence of benefit; for example, the Z1031 trial showed no improvements in pCR for patients without a Ki67 response to short-term neoadjuvant endocrine therapy who subsequently received chemotherapy43. Interestingly, the WSG-ADAPT run-in trial for patients with HR-positive, HER2-negative disease45 confirmed that combining assessments of static (genomic recurrence score) and dynamic (endocrine proliferation response defined as a Ki67 level of ≤10% following induction) biomarkers is feasible and could guide individualized therapy decisions in patients with early-stage breast cancer. Unfortunately, these results were not available at the time of the initiation of several very large adjuvant trials investigating the addition of CDK4/6 inhibitors to endocrine therapy, namely PALLAS46 and MonarchE47, of which only the latter had positive results albeit in a patient population defined by a high disease burden rather than by insufficient sensitivity to endocrine therapy.
The addition of CDK4/6 inhibitors to endocrine therapy has also been explored in the neoadjuvant setting for patients with HR-positive, HER2-negative early-stage breast cancer. These trials revealed a low pCR rate (0–5%) but also demonstrated that CDK4/6 inhibitors induced more profound reductions in Ki67 levels from baseline to 2 weeks and to surgery48–53.
Next to Ki67 levels, the preoperative endocrine prognostic index (PEPI) score is another tool that allows patients to be selected as candidates for treatment escalation. The PEPI score is determined by summing the partial scores corresponding to pathological tumour and nodal stages, Ki67 levels, and ER status following neoadjuvant endocrine therapy and has been shown to predict recurrence-free survival in the context of the IMPACT trial54. In the ALTERNATE study55,56, women with locally advanced luminal breast cancer were randomly assigned to receive either anastrozole, fulvestrant or a combination of the two; the primary end point was endocrine-sensitive disease rate, defined as the proportion of patients with a PEPI score of 0 among all eligible patients who started neoadjuvant endocrine therapy. Of note, patients were removed from randomization if their 2-week Ki67 levels did not decline from baseline in response to endocrine therapy. Neither fulvestrant nor fulvestrant plus anastrozole significantly improved endocrine-sensitive disease rate compared with anastrozole alone56. Relapse-free survival data remain immature.
The search for gene expression signatures that might enable patients receiving endocrine therapy to safely avoid chemotherapy has been another area of intense research interest. Owing to the more widespread use of screening, which has modified the epidemiology of breast cancers, the question of de-escalation has become crucial. The risk of disease relapse can now be characterized by transcriptomic signatures, two of which (Oncotype-DX and MammaPrint) have proven clinical utility in the selection of patients who will have excellent outcomes on adjuvant endocrine therapy alone57–59.
The intrinsic tumour subtype is also being investigated as a potential predictive biomarker. In a retrospective, exploratory analysis of data from patients with luminal metastatic breast cancer from the MONALEESA phase III studies, all PAM50 intrinsic subtypes were associated with a consistent OS benefit with the addition of ribociclib to endocrine therapy, except for the basal-like subtype60. Similar data from patients with early-stage disease are not yet available.
Further complexity exists when questioning the optimal definition of ER positivity. Although 1% of cells staining ER positive on immunohistochemistry is considered the official cut-off for ER-positive breast cancer, a cut-off of 10% is often used to guide clinical decision-making, which is supported by literature reports indicating that tumours with 1–9% ER expression (so-called ER-low tumours) have similar clinical characteristics to those classed as ER-negative (<1%)61.
HER2-positive breast cancer
The discovery that 15–20% of breast cancers have an aggressive clinical course linked to overexpression of HER2 marked the beginning of an era of steady progress, with the registration of four HER2-targeted therapies in the early-stage disease setting62. Based on a growing understanding of both the HER2 signalling pathway and the mechanism of action of HER2-targeted therapies, translational research efforts have focused on identifying predictive biomarkers of response that are both directly related to HER2 itself (such as the ratio of ERBB2 copy number to CEP17 determined using FISH, polysomy, mRNA and protein expression) and go beyond HER2, namely evaluating other receptors and/or ligands (such as HER3, EGFR, EGF, IGFR), HER2 downstream signalling pathways (such as PIK3CA/PTEN or RhoA), features associated with the tumour stroma (such as tumour-infiltrating lymphocytes (TILs) or immune-related gene signatures), and other patient-specific variables (such as the presence of HER2 and/or Fcγ receptor polymorphisms). Unfortunately, none of these putative biomarkers has thus far reached clinical utility62, although some have generated early promising results, for example, in the WSG-ADAPT trial63,64.
Stratification based on tumour-intrinsic subtypes is another attractive strategy that could be incorporated into patient selection for treatment escalation or de-escalation. The PAM50-based HER2-enriched intrinsic subtype is associated with a higher likelihood of a pCR following neoadjuvant therapy65, and tools combining traditional clinical, pathological and molecular characteristics to better predict clinical outcomes in patients with early-stage HER2-positive breast cancer are currently in development66.
DECRESCENDO (NCT04675827) is an ongoing, single-arm, prospective trial testing de-escalation of chemotherapy for patients with HER2-positive, HR-negative and node-negative early-stage breast cancer. After neoadjuvant taxane-based chemotherapy and dual HER2 blockade, patients with a pCR will receive an additional 14 cycles of adjuvant pertuzumab plus trastuzumab but no further chemotherapy. This approach is based on the hypothesis that the HER2-enriched subtype (roughly 65–70% of the trial population) has ‘HER2-addicted’ tumours that are therefore good candidates for anthracycline omission. Nonetheless, an ambitious 3-year invasive recurrence-free survival of at least 94% will have to be demonstrated in this molecularly defined subpopulation for this trial to meet the primary end point.
Triple-negative breast cancer
TNBC has been traditionally considered a ‘targetless’ breast cancer subtype, for which chemotherapy has long been the only effective and available treatment strategy67. Nevertheless, advances in clinical research in the past decades have been changing the treatment landscape of TNBC, both in terms of chemotherapy options (such as the introduction of dose-dense regimens and platinum-based therapies in the neoadjuvant setting) and in terms of other therapies that are now available for patients with this tumour type, including PARP inhibitors, immune-checkpoint inhibitors and antibody–drug conjugates. Immune-checkpoint inhibitors, in particular, have revolutionized the treatment and clinical trajectory of several cancer types, and relevant efforts are being made to identify predictive biomarkers of response, including in breast cancer. PD-L1 (ref.68), TILs68, a high tumour mutational burden (typically ≥10 mutations per megabase)69, mismatch repair deficiency70, immune gene signatures71 and intrinsic molecular subtypes71 are under investigation, but, so far, no biomarkers have been proven to have a clear role in predicting response to immune-checkpoint inhibitors in early-stage TNBC. A further level of complexity derives from the existence of several different diagnostic assays, scoring algorithms, intersample and intrasample heterogeneity, and differences according to the site of evaluation (metastatic versus primary lesions)72. Furthermore, beyond tumour characteristics, several additional factors could affect the outcomes of patients receiving immune-checkpoint inhibitors73, including the general characteristics of the patient (including immune function74, obesity75 and/or the microbiota76). Thus, the search for biomarkers capable of predicting a response to immune-checkpoint inhibitors in patients with early-stage TNBC remains a huge challenge.
A portion of the tumours that were traditionally considered to be TNBCs match the definition of the so-called HER2-low category (namely those with a HER2 immunohistochemistry score of 1+ or 2+ without detectable amplification on FISH)77. Robust evidence so far supports the use of the HER2-targeted antibody–drug conjugate trastuzumab deruxtecan in these patients78, thus underlining that the traditional distinction between these three breast cancer subtypes might be too simplistic and unhelpful in certain scenarios given that the level of expression of both HER2 and hormone receptors is not binary but rather a continuous spectrum of expression, which intrinsically limits most attempts at classification.
Time to re-think trial design?
Improving the end points of neoadjuvant trials
The establishment of an accelerated approval pathway for drugs designed to treat serious diseases that are also unmet medical needs dates back to the early 1990s and clearly addressed the need to expedite the entire process in the best interest of patients79,80. Such pathways typically rely on improvements on one or more surrogate end points to provide an early indication of efficacy. However, considerable academic debate exists on how and when a surrogate end point can truly be considered as ‘validated’. According to certain international guidelines81,82, surrogate validation should be based on robust correlation with survival end points, both at the study level and at an individual patient level.
As explained previously, pCR is only weakly correlated with OS at the study level28, thus questioning the role of pCR as a valid surrogate end point. Moreover, pCR appears to lose some of its prognostic power when used to assess the efficacy of drugs that are not chemotherapies. This limitation applies to immune-checkpoint inhibitors. For example, the GeparNUEVO study69,83 was a randomized, phase II study testing the addition of durvalumab to neoadjuvant chemotherapy for patients with early-stage TNBC. No significant improvement in pCR rate was observed69; however, after a median follow-up duration of 43.7 months, durvalumab was associated with a significant improvement in survival outcomes (3-year OS 95.1% vs 83.1%, hazard ratio 0.26, 95% CI 0.09–0.79; P = 0.0076)83. This observation might reflect that immune-checkpoint inhibitors have a different mechanism of action to that of cytotoxic agents, and, by activating an immune response against cancer cells instead of acting directly against them, they are able to produce more durable and, in some cases, delayed responses84–86. Furthermore, pCR might also not be the best end point for the evaluation of responses to neoadjuvant endocrine therapy. Compared with other breast cancer subtypes, HR-positive, HER2-negative tumours are characterized by lower pCR rates than neoadjuvant therapies and a simple distinction between pCR versus non-pCR might be not useful because few patients reach a pCR. Compared with other breast cancer subtypes, HR-positive, HER2-negative tumours are traditionally characterized by lower pCR rates than neoadjuvant therapies87. Thus, a dichotomous distinction between pCR and non-pCR could be an overly simplistic and inaccurate indicator of patient outcome, while the extent of residual disease could provide important additional information.
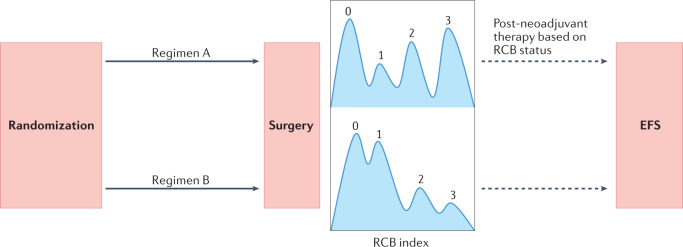
The issues with pCR justify a renewed interest in residual cancer burden (RCB). RCB is a continuous index based on the assessment of pathological measurements of the primary tumour (dimensions and cellularity fraction) and nodal metastases (number and size). Based on these parameters, the RCB index can be divided into one of four categories: RCB 0 (pCR), RCB 1, RCB 2 and RCB 3 (Fig. 1). The association between RCB and long-term outcomes has been robustly demonstrated in all breast cancer subtypes (HR-positive and HER2-negative, HER2-positive, and TNBC) independently of other clinical and/or pathological characteristics88. Evaluations of the RCB index should increasingly be adopted as a clinical end point in neoadjuvant trials involving patients with early-stage breast cancer.
Fig. 1. Residual cancer burden as an end point for neoadjuvant clinical trials.
Replacing pathological complete response (pCR) with a residual cancer burden (RCB) profile and event-free survival (EFS) is likely to improve the accuracy of data from neoadjuvant clinical trials as an early indicator of clinical benefit. RCB is a validated surrogate88,117 of longer-term survival outcomes (such as EFS) that is also more granular than dichotomous comparisons of pCR versus non-pCR, with improved survival durations often seen for patients with more limited residual disease. Thus, post-neoadjuvant trials should increasingly explore treatment strategies directed at addressing the residual disease profile.
Considerable debate currently exists regarding the role of survival end points. In the list of surrogate end points to be used for regulatory approval purposes released by the FDA in 2018, beyond pCR, DFS, EFS, objective response rate and PFS are all permitted89. The initial justification for this approach comes from the desire to expedite the approval process owing to the shorter time required for assessments based on these end points compared with OS, thus allowing patients with unmet medical needs earlier access to drugs that might be effective. However, the strength of the associations of these surrogate end points with OS is not well documented. In 2020, Gyawali et al. explored the underlying evidence for these surrogate end points90, showing that considerable variability exists and that, in some scenarios, the association with OS is either weak or absent.
With the exponential increase in cancer drug costs in the past years, agreeing on a ‘prioritization’ list based on the real added value of such drugs is a legitimate response. This much-needed but difficult exercise has been conducted by ASCO, with the development of the ASCO Value Framework91, and by ESMO with the development of the ESMO Magnitude of Clinical Benefit Scale (MCBS)92, which values improvements in OS and/or quality of life far more heavily than improvements in ORR or extension of PFS. Interestingly, DFS has been the subject of an intense debate, leading to a reasonable consensus: living additional months or years without detectable disease has greater value than living somewhat longer with stable, non-progressive disease; thus, improvements in median DFS of sufficient magnitude are credited with high scores on the ESMO-MCBS until OS data become available, at which point a lack of OS benefit induces a one-point downgrade (ESMO-MCBS version 2.0 will soon be published93). Although the scale does not include a dimension of ‘cost’, its application might help health authorities to prioritize drugs that more strongly warrant financial investment.
The post-neoadjuvant setting: a promising scenario gaining in popularity
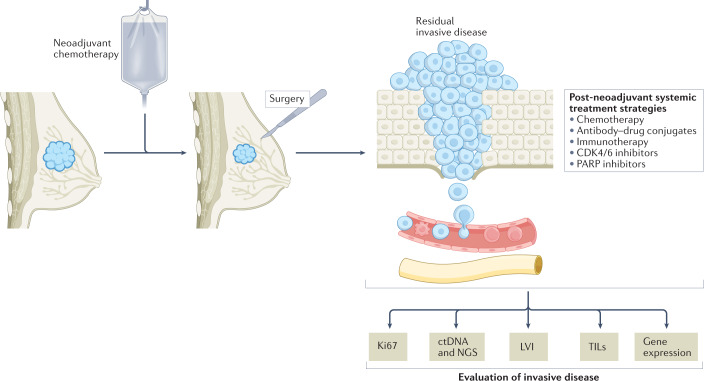
Among the several advantages provided by the neoadjuvant approach is the possibility of selecting patients for treatment escalation or de-escalation based on their response to neoadjuvant therapy. Despite imperfect surrogacy, patients who do not have a pCR generally have worse long-term survival outcomes than those with a pCR after the completion of neoadjuvant therapy27. Hence, the post-neoadjuvant setting is an attractive scenario for the design of pivotal clinical trials as it involves selecting patients with high-risk residual invasive disease at surgery who might be candidates for treatment escalation. Furthermore, compared to the traditional adjuvant setting, such trials are less likely to enrol patients already cured by standard therapy (Fig. 2). Two systemic post-neoadjuvant treatments for patients with residual invasive disease at surgery are already approved for use in clinical practice: capecitabine for patients with TNBC, based on the results of the CREATE-X trial94, and trastuzumab emtansine (T-DM1) for patients with HER2-positive disease, based on the results of KATHERINE95.
Fig. 2. The post-neoadjuvant setting: an attractive scenario for future clinical trials.
The post-neoadjuvant setting offers the possibility of selecting patients with residual invasive disease at surgery who might benefit from additional adjuvant treatments (white text box) and also the avoidance of enrolling patients who are not likely to benefit from further therapy owing to a complete response to neoadjuvant therapy. Moreover, this approach allows translational analyses to be performed on the residual tumour material, thus enabling potential biomarkers to be identified (such as Ki67, tumour-infiltrating lymphocytes (TILs), circulating tumour DNA (ctDNA), and/or genetic and genomic alterations) (sepia text boxes), which could subsequently be validated prospectively. LVI, lymphovascular invasion; NGS, next-generation sequencing.
In the CREATE-X trial, 910 patients with early-stage, HER2-negative (HR-positive or HR-negative) breast cancer and residual disease after the completion of neoadjuvant chemotherapy were randomly assigned to either 6–8 cycles of capecitabine or to no treatment. In the overall population, post-neoadjuvant capecitabine resulted in significant improvements in invasive DFS (hazard ratio 0.70, 95% CI 0.53–0.92; P = 0.01) and OS (hazard ratio 0.59, 95% CI 0.39–0.90; P = 0.01), respectively, with a greater magnitude of benefit in the TNBC subgroup (n = 286) (hazard ratio 0.58, 95% CI 0.39–0.87 for invasive DFS, and hazard ratio 0.52, 95% CI 0.30–0.90 for OS, respectively)94. In the KATHERINE trial, 1,486 patients with early-stage, HER2-positive breast cancer and residual disease at surgery, after neoadjuvant chemotherapy and HER2-targeted therapy, were randomly assigned to receive either T-DM1 or trastuzumab for 14 cycles. T-DM1 was associated with a significant improvement in invasive DFS (hazard ratio 0.50, 95% CI 0.39–0.64)95.
In 2021, another study, OLYMPIA96, demonstrated a significant improvement in 3-year invasive DFS (85.9% vs 77.1%, hazard ratio 0.58, 99.5% CI 0.41–0.82; P < 0.001) and OS (59 vs 86 events, hazard ratio 0.68, 99% CI 0.44–1.05; P = 0.02) with olaparib in patients with high-risk, BRCA-mutated, HER2-negative early-stage breast cancer, including those previously treated in the neoadjuvant setting and who presented with residual disease at surgery.
Another attractive feature of the post-neoadjuvant setting is the possibility to perform translational analyses on residual disease and thus tailor post-surgical systemic therapy accordingly (Fig. 2). In other words, the evaluation of residual disease could reveal potential biomarkers (such as Ki67, TILs, RCB, and/or changes in gene expression and genetic alterations) for risk assessment and enable further fine-tuning of subsequent tailored treatments.
The post-neoadjuvant setting also features several promising treatment de-escalation scenarios. The most prominent considerations involve omitting breast and/or axillary surgery for patients without residual disease. Ongoing studies are investigating the omission of breast and/or axillary surgery after neoadjuvant systemic therapy in patients with a complete response97,98, some of them with encouraging results99,100, although this approach is currently not considered to be the standard of care.
The new era: future directions
The application of emerging technologies, including genomics, proteomics, metabolomics, pharmacogenetics and functional imaging, to the development of predictive biomarkers of efficacy is beginning to shape the new era of (neo)adjuvant clinical trials in patients with early-stage breast cancer.
Liquid biopsy
Liquid biopsy is a non-invasive method of obtaining information on tumour characteristics and thus informing on prognosis through the analysis of circulating material present in blood, including circulating tumour DNA (ctDNA) and circulating tumour cells101. In particular, findings from the past 10 years support the use of ctDNA sequencing as a feasible technique for use in patients with early-stage breast cancer101,102 and an increasing amount of emerging data are now suggesting its clinical utility in this setting103,104. Thus, as liquid biopsy has shown promise to predict early disease relapse before imaging103,104, it could become an important tool to be implemented in study designs, to select patients requiring additional treatments and, ultimately, to guide treatment escalation or de-escalation in the post-neoadjuvant setting.
The ongoing phase II c-TRAK (NCT03145961) trial is using ctDNA mutation tracking to detect minimal residual disease and guide the use of pembrolizumab in patients with high-risk early-stage TNBC. Despite the inconclusive preliminary results presented at the San Antonio Breast Cancer Symposium 2021, c-TRAK has undoubted merit in the potential to provide proof of initial clinical utility of a ctDNA assay to guide the selective use of a systemic treatment (that is, pembrolizumab) in patients with TNBC105.
At the 2022 ASCO Annual Meeting, data on the role of ctDNA in the detection of late disease recurrence (>5 years from diagnosis) in women with high-risk HR-positive breast cancer were presented106. Of 83 evaluable patients, 10% had minimal residual disease identified via ctDNA. ctDNA was detected in all patients who had distant disease relapse within the study follow-up period (n = 5), with a lead time (the time from first positive ctDNA sample to clinical recurrence) of up to 37.6 months (median 12.4 months)106,107. Results from additional ongoing studies are needed to determine whether therapeutic intervention immediately after ctDNA detection can improve the clinical outcomes of these patients (such as ASPRIA (NCT04434040), PERSEVERE (NCT04849364), DARE (NCT04567420) and LEADER (NCT03285412)).
Functional imaging
Early changes in 18F-labelled fluorodeoxyglucose (18FDG) uptake observed using PET-CT during neoadjuvant therapy have been correlated with the presence or absence of pCR in several trials involving patients with early-stage breast cancer108,109. Unfortunately, none of these studies has explored the feasibility of using suboptimal standardized uptake values (SUVs) after 2–3 cycles of neoadjuvant therapy to adapt the treatment scheme and thus improve outcomes. The clinical utility of treatment de-escalation in patients with an excellent response on 18FDG-PET appears more promising.
TBCRC026 was a phase II trial designed to investigate the correlation between 18FDG-PET SUV corrected for lean body mass (SULmax) and pCR rate on neoadjuvant pertuzumab plus trastuzumab (without chemotherapy) in patients with ER-negative, HER2-positive early-stage breast cancer110. The primary objective was to demonstrate a correlation between early changes in SULmax, assessed at baseline and 15 days after the start of neoadjuvant therapy, and pCR. The primary objective of the study was not met according to the predefined statistical boundaries, although early changes in SULmax were found to predict the likelihood of a pCR, thus providing a promising strategy to guide the de-escalation of neoadjuvant therapy based on early functional imaging findings110 in patients with tumours that appear to be highly sensitive to HER2-targeted therapy alone.
PHERGain111 (NCT03161353) is a randomized, phase II study designed to assess early metabolic responses to neoadjuvant trastuzumab plus pertuzumab using 18FDG-PET. In PHERGain, 18FDG-PET is used to identify patients with HER2-positive breast cancer who are more likely to benefit from neoadjuvant dual HER2 inhibition, without chemotherapy. Interestingly, at a primary analysis, 18FDG-PET responders (defined as a reduction of at least 40% of the maximum SUV after two cycles of treatment) had a pCR rate of 37.9% (95% CI 31.6–44.5; P < 0.0001 compared with the historical rate)111. Follow-up for the survival end point (DFS) is ongoing and will ultimately provide data on the possibility of selecting patients who might be able to avoid chemotherapy.
Spatial transcriptomics and single-cell RNA sequencing
All organs of the human body, including breast tissues, are comprised of different subpopulations of cells with strictly interconnected functions. By characterizing the transcriptome of each individual cell, single-cell RNA sequencing can identify distinct subgroups of cells within the same tissue. However, this information is obtained through the isolation of cells and therefore the destruction of information regarding their spatial localization within the tissue. Spatial information is essential to understanding the interconnections existing among different cells. Hence, increasing efforts are being made to merge information coming from single-cell RNA sequencing together with spatial transcriptomics112. The integration of such data can further help to identify both differences and similarities between malignant and non-malignant breast tissues but also enable the dissection of intertumour and intratumour heterogeneity.
Integration and collaboration
Clinical and translational early-stage breast cancer research remains highly fragmented despite the existence of several unique initiatives such as the EBCTCG, which started in 1985, the Breast International Group founded in 1999, and the National Clinical Trial Network launched in 2014 (formerly the North America Breast Cancer Group).
The process of biomarker discovery and validation likely requires access to very large, well-annotated databases of ‘candidate biomarkers’ linked with clinical outcomes; nonetheless, no clinical trial on its own is able to achieve such a goal. For this and other reasons, the International Committee of Medical Journal Editors issued an important statement in 2016, namely that sharing data from interventional clinical trials is an ethical obligation113. The time has come to go one step further: after a protected period of time to enable sponsors to exploit their intellectual property rights, biomarker data collected in trials with sufficient quality control procedures should become freely accessible to the broader scientific community. The costs linked to this process will not be negligible but will be much lower than those associated with thousands of additional and increasingly sophisticated independent translational research efforts. Additionally, an increasingly active role for patient advocates in the design of future trials is sought, both as a fundamental part of academic research and to provide a ‘counterweight’ to industry-led research114,115.
The future landscape of clinical trials
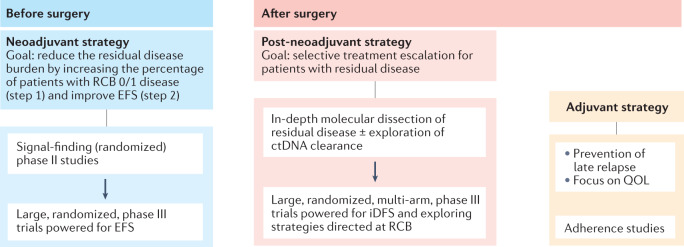
Neoadjuvant and post-neoadjuvant trials are expected to have an increasing role in the evaluation of systemic therapies for patients with early-stage breast cancer (Fig. 3). Nonetheless, a number of methodological improvements in trial design and implementation are required. Those designing neoadjuvant strategies should aim to implement end points with more robust associations with survival outcomes and, thus far, RCB is the best candidate to replace pCR given the higher level of granularity for assessments of the extent of residual disease it provides. To optimize resources, increase efficiency and minimize the risks of exposing patients to suboptimal and sometimes toxic therapies, neoadjuvant trials should first focus on ‘signal-finding’, randomized, phase II designs involving limited numbers of patients. Results from these studies can subsequently be confirmed in larger-cohort, randomized phase III studies that are powered to demonstrate improvements in EFS. In this regard, I-SPY (NCT01042379), a US initiative, embraced this strategy many years ago by testing neoadjuvant and personalized adaptive novel agents in patients with early-stage breast cancer to determine which new drugs are most effective in particular breast cancer subtypes and to identify early predictors of treatment success. At enrolment, each new patient is included in one of the ten specific molecular subtypes; then, the I-SPY 2 randomization engine assigns each participant to a study arm, giving more weight to treatments that have proved to be more successful in that specific tumour subtype. When the predictive probabilities for an experimental agent reach a pre-specified level of either efficacy or futility, the treatment is then either declared to be successful or administration is stopped. Not surprisingly, RCB 0 (implying pCR) has been chosen as the primary end point because it enables fast turnaround and thus the rapid evaluation of new drugs. However, this design also probably explains, for reasons outlined previously, the relatively limited number of drugs declared as being ‘successful’ that have ultimately entered clinical practice in patients with early-stage disease.
Fig. 3. Proposed landscape of future post-(neo)adjuvant clinical trials in early-stage breast cancer.
Neoadjuvant trials are increasingly adopting residual cancer burden (RCB) as a surrogate end point for survival and should aim to be large (n = ~1,000–1,500), randomized, adequately powered for survival end points (such as event-free survival; EFS) and designed following successful phase II, ‘signal-finding’ studies. Interest in such trials is currently increasing, especially those designed to identify patients with residual disease at surgery who might benefit from treatment escalation strategies based on in-depth molecular dissection of residual invasive disease and/or the exploration of circulating tumour DNA (ctDNA) detection. Interest in traditional adjuvant strategies (without neoadjuvant treatment) is likely to decline, although such studies remain relevant to the assessment of quality-of-life (QOL) outcomes, adherence to study treatment and exploration of ‘delayed strategies’ designed to reduce the risk of late relapse (>5–10 years), especially in patients with hormone receptor-positive disease. iDFS, invasive disease-free survival.
The post-neoadjuvant setting will likely gain further popularity owing to the possibility of treatment escalation for patients with residual disease after the completion of neoadjuvant therapy. An in-depth molecular dissection of residual disease, with or without systematic screening for ctDNA detection, will help in the design of large-cohort, randomized, multi-arm, phase III trials powered to demonstrate potential improvements in invasive DFS. The pure adjuvant setting (that is, the administration of systemic treatment after surgery without patient selection based on response to a prior treatment) is expected to have a more marginal role, focusing on ways to improve treatment adherence and/or quality of life, although this approach will continue to be important for investigating ‘delayed’ treatment strategies designed to tackle the problems of tumour dormancy and/or late disease relapse in patients with HR-positive disease.
Conclusions
Breast cancer investigators have paved the way towards reinforced collaboration on two fronts: conducting pooled analyses of individual patient data from completed trials, and reducing duplication of effort in their design and implementation. After two decades of substantial research interest in small-cohort neoadjuvant trials thought to be the ideal replacement for expensive and risky adjuvant trials with larger cohorts that are ‘contaminated’ by patients with low-risk disease, a better understanding of the limitations of pCR as a surrogate end point for DFS is emerging. This observation has led to a willingness to improve the design of neoadjuvant trials, together with a growing interest in exploiting the post-neoadjuvant setting as a way to ameliorate the prognosis of patients at the highest risk. Nonetheless, the weakest aspect of this new approach remains biomarker research for improved treatment tailoring: more powerful and expensive technologies are emerging that enable the more detailed dissection of both the biology of tumours and their microenvironments; however, their use within trials with moderate cohort sizes is unlikely to provide data that support clinical utility. An accelerated, responsible, and user-friendly biomarker and clinical data-sharing process must become a high priority for the next generation of trials.
Supplementary information
Author contributions
E.A. and M.P. researched data for this manuscript, J.G. and M.P. discussed manuscript content, and all authors wrote and reviewed and/or edited this manuscript prior to submission.
Peer review
Peer review information
Nature Reviews Clinical Oncology thanks J. Heil, who co-reviewed with A. Pfob; and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Competing interests
E.A. has received fees or honoraria for consultant roles for Eli Lilly and Sandoz and support for attending medical conferences from Eli Lilly, Genetic, Istituto Gentili, Novartis and Roche, all unrelated to the submitted work. J.G. has received fees or honoraria for consultant roles for Daiichi, Eisai, Exact Science, Gilead, Lilly, Merck, Novartis, Onxeo, Pfizer, Roche Genentech and Seattle Genetics, and works in an institution that receives research grants from Eisai, Exact Science and Roche Genentech, all unrelated to the submitted work. M.P. has received fees or honoraria for consultant roles for AstraZeneca, Camel-IDS/Precirix, Frame Therapeutics, Gilead, Immunomedics, Immutep, Lilly, Menarini, MSD, NBE Therapeutics, Novartis, Odonate, Pfizer, Roche Genentech, Seagen and Seattle Genetics, is part of the scientific board at Oncolytics, and works in an institution that receives research grants from AstraZeneca, Immunomedics, Lilly, Menarini, MSD, Novartis, Pfizer, Radius, Roche Genentech, Servier and Synthon, all unrelated to the submitted work.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
ClinicalTrials.gov: https://clinicaltrials.gov/
Supplementary information
The online version contains supplementary material available at 10.1038/s41571-022-00687-1.
References
- 1.Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J. Clin. 2022;72:7–33. doi: 10.3322/caac.21708. [DOI] [PubMed] [Google Scholar]
- 2.Yabroff KR, et al. Association of the COVID-19 pandemic with patterns of statewide cancer services. J. Natl Cancer Inst. 2021;114:907–909. doi: 10.1093/jnci/djab122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Smith BD, et al. Improvement in breast cancer outcomes over time: are older women missing out? J. Clin. Oncol. 2011;29:4647–4653. doi: 10.1200/JCO.2011.35.8408. [DOI] [PubMed] [Google Scholar]
- 4.Polyak K. Breast cancer: origins and evolution. J. Clin. Invest. 2007;117:3155–3163. doi: 10.1172/JCI33295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bonadonna G, et al. Combination chemotherapy as an adjuvant treatment in operable breast cancer. N. Engl. J. Med. 1976;294:405–410. doi: 10.1056/NEJM197602192940801. [DOI] [PubMed] [Google Scholar]
- 6.Early Breast Cancer Trialists' Collaborative Group (EBCTCG) et al. Comparisons between different polychemotherapy regimens for early breast cancer: meta-analyses of long-term outcome among 100,000 women in 123 randomised trials. Lancet. 2012;379:432–444. doi: 10.1016/S0140-6736(11)61625-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fisher B, et al. 1-Phenylalanine mustard (L-PAM) in the management of primary breast cancer. a report of early findings. N. Engl. J. Med. 1975;292:117–122. doi: 10.1056/NEJM197501162920301. [DOI] [PubMed] [Google Scholar]
- 8.Fisher B, Redmond C, Fisher ER, Wolmark N. Systemic adjuvant therapy in treatment of primary operable breast cancer: National Surgical Adjuvant Breast and Bowel Project experience. NCI Monogr. 1986;1:35–43. [PubMed] [Google Scholar]
- 9.Early Breast Cancer Trialists’ Collaborative Group Systemic treatment of early breast cancer by hormonal, cytotoxic, or immune therapy. 133 randomised trials involving 31,000 recurrences and 24,000 deaths among 75,000 women. Lancet. 1992;339:71–85. doi: 10.1016/0140-6736(92)90997-H. [DOI] [PubMed] [Google Scholar]
- 10.No authors listed. Controlled trial of tamoxifen as adjuvant agent in management of early breast cancer. Interim analysis at four years by Nolvadex Adjuvant Trial Organisation. Lancet. 1983;1:257–261. [PubMed] [Google Scholar]
- 11.Nolvadex & Adjuvant Trial Organisation Controlled trial of tamoxifen as a single adjuvant agent in the management of early breast cancer. Br. J. Cancer. 1988;57:608–611. doi: 10.1038/bjc.1988.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fisher B, et al. Treatment of primary breast cancer with chemotherapy and tamoxifen. N. Engl. J. Med. 1981;305:1–6. doi: 10.1056/NEJM198107023050101. [DOI] [PubMed] [Google Scholar]
- 13.Piccart-Gebhart MJ, et al. Trastuzumab after adjuvant chemotherapy in HER2-positive breast cancer. N. Engl. J. Med. 2005;353:1659–1672. doi: 10.1056/NEJMoa052306. [DOI] [PubMed] [Google Scholar]
- 14.Cameron D, et al. 11 years’ follow-up of trastuzumab after adjuvant chemotherapy in HER2-positive early breast cancer: final analysis of the herceptin adjuvant (HERA) trial. Lancet. 2017;389:1195–1205. doi: 10.1016/S0140-6736(16)32616-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bradley R, et al. Trastuzumab for early-stage, HER2-positive breast cancer: a meta-analysis of 13,864 women in seven randomised trials. Lancet Oncol. 2021;22:1139–1150. doi: 10.1016/S1470-2045(21)00288-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Early Breast Cancer Trialists’ Collaborative Group (EBCTCG). Aromatase inhibitors versus tamoxifen in early breast cancer: patient-level meta-analysis of the randomised trials. Lancet. 2015;386:1341–1352. doi: 10.1016/S0140-6736(15)61074-1. [DOI] [PubMed] [Google Scholar]
- 17.Piccart M, et al. Adjuvant pertuzumab and trastuzumab in early HER2-positive breast cancer in the APHINITY trial: 6 years’ follow-up. J. Clin. Oncol. 2021;39:1448–1457. doi: 10.1200/JCO.20.01204. [DOI] [PubMed] [Google Scholar]
- 18.Coleman R, et al. Adjuvant denosumab in early breast cancer (D-CARE): an international, multicentre, randomised, controlled, phase 3 trial. Lancet Oncol. 2020;21:60–72. doi: 10.1016/S1470-2045(19)30687-4. [DOI] [PubMed] [Google Scholar]
- 19.Cameron D, et al. Adjuvant bevacizumab-containing therapy in triple-negative breast cancer (BEATRICE): primary results of a randomised, phase 3 trial. Lancet Oncol. 2013;14:933–942. doi: 10.1016/S1470-2045(13)70335-8. [DOI] [PubMed] [Google Scholar]
- 20.Piccart-Gebhart M, et al. Adjuvant lapatinib and trastuzumab for early human epidermal growth factor receptor 2-positive breast cancer: results from the randomized phase III adjuvant lapatinib and/or trastuzumab treatment optimization trial. J. Clin. Oncol. 2016;34:1034–1042. doi: 10.1200/JCO.2015.62.1797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.von Minckwitz G, et al. Adjuvant pertuzumab and trastuzumab in early HER2-positive breast cancer. N. Engl. J. Med. 2017;377:122–131. doi: 10.1056/NEJMoa1703643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Holmes EM, et al. Are we assuming too much with our statistical assumptions? Lessons learned from the ALTTO trial. Ann. Oncol. 2019;30:1507–1513. doi: 10.1093/annonc/mdz195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ragaz J, et al. Preoperative adjuvant chemotherapy (neoadjuvant) for carcinoma of the breast: rationale and safety report. Recent. Results Cancer Res. 1985;98:99–105. doi: 10.1007/978-3-642-82432-6_11. [DOI] [PubMed] [Google Scholar]
- 24.Wolmark N, Wang J, Mamounas E, Bryant J, Fisher B. Preoperative chemotherapy in patients with operable breast cancer: nine-year results from National Surgical Adjuvant Breast and Bowel Project B-18. J. Natl Cancer Inst. Monogr. 2001 doi: 10.1093/oxfordjournals.jncimonographs.a003469. [DOI] [PubMed] [Google Scholar]
- 25.Fumagalli D, et al. A common language in neoadjuvant breast cancer clinical trials: proposals for standard definitions and endpoints. Lancet Oncol. 2012;13:e240–e248. doi: 10.1016/S1470-2045(11)70378-3. [DOI] [PubMed] [Google Scholar]
- 26.FDA. Pathological Complete Response in Neoadjuvant Treatment of High-Risk Early-Stage Breast Cancer: Use as an Endpoint to Support Accelerated Approval. https://www.fda.gov/drugs/guidance-compliance-regulatory-information/guidances-drugs (2022).
- 27.Cortazar P, et al. Pathological complete response and long-term clinical benefit in breast cancer: the CTNeoBC pooled analysis. Lancet. 2014;384:164–172. doi: 10.1016/S0140-6736(13)62422-8. [DOI] [PubMed] [Google Scholar]
- 28.Conforti F, et al. Evaluation of pathological complete response as surrogate endpoint in neoadjuvant randomised clinical trials of early stage breast cancer: systematic review and meta-analysis. BMJ. 2021;375:e066381. doi: 10.1136/bmj-2021-066381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Collins FS, Morgan M, Patrinos A. The human genome project: lessons from large-scale biology. Science. 2003;300:286–290. doi: 10.1126/science.1084564. [DOI] [PubMed] [Google Scholar]
- 30.Meystre, S. M., Narus, S. P. & Mitchell, J. A. In: Clinical Research Informatics (eds Richesson, R. L. & Andrews, J. E.). 113–131. (Springer, 2012).
- 31.Heys SD, et al. Neoadjuvant docetaxel in breast cancer: 3-year survival results from the Aberdeen trial. Clin. Breast Cancer. 2002;3:S69–S74. doi: 10.3816/CBC.2002.s.015. [DOI] [PubMed] [Google Scholar]
- 32.Green MC, et al. Weekly paclitaxel improves pathologic complete remission in operable breast cancer when compared with paclitaxel once every 3 weeks. J. Clin. Oncol. 2005;23:5983–5992. doi: 10.1200/JCO.2005.06.232. [DOI] [PubMed] [Google Scholar]
- 33.Ellis MJ, et al. Letrozole is more effective neoadjuvant endocrine therapy than tamoxifen for ErbB-1– and/or ErbB-2–positive, estrogen receptor–positive primary breast cancer: evidence from a phase III randomized trial. J. Clin. Oncol. 2001;19:3808–3816. doi: 10.1200/JCO.2001.19.18.3808. [DOI] [PubMed] [Google Scholar]
- 34.Dowsett M, et al. Short-term changes in Ki-67 during neoadjuvant treatment of primary breast cancer with anastrozole or tamoxifen alone or combined correlate with recurrence-free survival. Clin. Cancer Res. 2009;11:951s–958s. doi: 10.1158/1078-0432.951s.11.2. [DOI] [PubMed] [Google Scholar]
- 35.Pusztai L, et al. Evaluation of microtubule-associated protein-Tau expression as a prognostic and predictive marker in the NSABP-B 28 randomized clinical trial. J. Clin. Oncol. 2009;27:4287–4292. doi: 10.1200/JCO.2008.21.6887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bonneau C, Gurard-Levin ZA, Andre F, Pusztai L, Rouzier R. Predictive and prognostic value of the tauprotein in breast cancer. Anticancer. Res. 2015;35:5179–5184. [PubMed] [Google Scholar]
- 37.Bartlett JMS, et al. HER2 status predicts for upfront AI benefit: a TRANS-AIOG meta-analysis of 12,129 patients from ATAC, BIG 1-98 and TEAM with centrally determined HER2. Eur. J. Cancer. 2017;79:129–138. doi: 10.1016/j.ejca.2017.03.033. [DOI] [PubMed] [Google Scholar]
- 38.Gianni L, et al. Efficacy and safety of neoadjuvant pertuzumab and trastuzumab in women with locally advanced, inflammatory, or early HER2-positive breast cancer (NeoSphere): a randomised multicentre, open-label, phase 2 trial. Lancet Oncol. 2012;13:25–32. doi: 10.1016/S1470-2045(11)70336-9. [DOI] [PubMed] [Google Scholar]
- 39.Schmid P, et al. Pembrolizumab for early triple-negative breast cancer. N. Engl. J. Med. 2020;382:810–821. doi: 10.1056/NEJMoa1910549. [DOI] [PubMed] [Google Scholar]
- 40.Schmid P, et al. Event-free survival with pembrolizumab in early triple-negative breast cancer. N. Engl. J. Med. 2022;386:556–567. doi: 10.1056/NEJMoa2112651. [DOI] [PubMed] [Google Scholar]
- 41.Fisher B, Saffer E, Rudock C, Coyle J, Gunduz N. Effect of local or systemic treatment prior to primary tumor removal on the production and response to a serum growth-stimulating factor in mice. Cancer Res. 1989;49:2002–2004. [PubMed] [Google Scholar]
- 42.Smith IE, et al. Neoadjuvant treatment of postmenopausal breast cancer with anastrozole, tamoxifen, or both in combination: the Immediate Preoperative Anastrozole, Tamoxifen, or Combined with Tamoxifen (IMPACT) multicenter double-blind randomized trial. J. Clin. Oncol. 2005;23:5108–5116. doi: 10.1200/JCO.2005.04.005. [DOI] [PubMed] [Google Scholar]
- 43.Ellis MJ, et al. Ki67 proliferation index as a tool for chemotherapy decisions during and after neoadjuvant aromatase inhibitor treatment of breast cancer: results from the American College of Surgeons Oncology Group Z1031 trial (Alliance) J. Clin. Oncol. 2017;35:1061–1069. doi: 10.1200/JCO.2016.69.4406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Smith I, et al. Long-term outcome and prognostic value of Ki67 after perioperative endocrine therapy in postmenopausal women with hormone-sensitive early breast cancer (POETIC): an open-label, multicentre, parallel-group, randomised, phase 3 trial. Lancet Oncol. 2020;21:1443–1454. doi: 10.1016/S1470-2045(20)30458-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Nitz U, et al. The run-in phase of the prospective WSG-ADAPT HR+/HER2- trial demonstrates the feasibility of a study design combining static and dynamic biomarker assessments for individualized therapy in early breast cancer. Ther. Adv. Med. Oncol. 2020;12:1758835920973130. doi: 10.1177/1758835920973130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gnant M, et al. Adjuvant palbociclib for early breast cancer: the PALLAS trial results (ABCSG-42/AFT-05/BIG-14-03) J. Clin. Oncol. 2022;40:282–293. doi: 10.1200/JCO.21.02554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Johnston SRD, et al. Abemaciclib combined with endocrine therapy for the adjuvant treatment of HR+, HER2-, node-positive, high-risk, early breast cancer (monarchE). J. Clin. Oncol. 2020;38:3987–3998. doi: 10.1200/JCO.20.02514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cottu P, et al. Letrozole and palbociclib versus chemotherapy as neoadjuvant therapy of high-risk luminal breast cancer. Ann. Oncol. 2018;29:2334–2340. doi: 10.1093/annonc/mdy448. [DOI] [PubMed] [Google Scholar]
- 49.Johnston S, et al. Randomized phase II study evaluating palbociclib in addition to letrozole as neoadjuvant therapy in estrogen receptor-positive early breast cancer: PALLET trial. J. Clin. Oncol. 2019;37:178–189. doi: 10.1200/JCO.18.01624. [DOI] [PubMed] [Google Scholar]
- 50.Ma CX, et al. NeoPalAna: neoadjuvant palbociclib, a cyclin-dependent kinase 4/6 inhibitor, and anastrozole for clinical stage 2 or 3 estrogen receptor-positive breast cancer. Clin. Cancer Res. 2017;23:4055–4065. doi: 10.1158/1078-0432.CCR-16-3206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hurvitz SA, et al. Potent cell-cycle inhibition and upregulation of immune response with abemaciclib and anastrozole in neoMONARCH, phase II neoadjuvant study in HR+/HER2− breast cancer. Clin. Cancer Res. 2020;26:566–580. doi: 10.1158/1078-0432.CCR-19-1425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Chow LWC, Morita S, Chow CYC, Ng W-K, Toi M. Neoadjuvant palbociclib on ER+ breast cancer (N007): clinical response and EndoPredict’s value. Endocr. Relat. Cancer. 2018;25:123–130. doi: 10.1530/ERC-17-0396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Prat A, et al. Ribociclib plus letrozole versus chemotherapy for postmenopausal women with hormone receptor-positive, HER2-negative, luminal B breast cancer (CORALLEEN): an open-label, multicentre, randomised, phase 2 trial. Lancet Oncol. 2020;21:33–43. doi: 10.1016/S1470-2045(19)30786-7. [DOI] [PubMed] [Google Scholar]
- 54.Ellis MJ, et al. Outcome prediction for estrogen receptor–positive breast cancer based on postneoadjuvant endocrine therapy tumor characteristics. J. Natl Cancer Inst. 2008;100:1380–1388. doi: 10.1093/jnci/djn309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Suman VJ, Ellis MJ, Ma CX. The ALTERNATE trial: assessing a biomarker driven strategy for the treatment of post-menopausal women with ER+/Her2- invasive breast cancer. Chin. Clin. Oncol. 2015;4:34. doi: 10.3978/j.issn.2304-3865.2015.09.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ma CX, et al. ALTERNATE: Neoadjuvant endocrine treatment (NET) approaches for clinical stage II or III estrogen receptor-positive HER2-negative breast cancer (ER+HER2- BC) in postmenopausal (PM) women: alliance A011106. J. Clin. Oncol. 2020;38(Suppl. 15):504. doi: 10.1200/JCO.2020.38.15_suppl.504. [DOI] [Google Scholar]
- 57.Kalinsky K, et al. 21-Gene assay to inform chemotherapy benefit in node-positive breast cancer. N. Engl. J. Med. 2021;385:2336–2347. doi: 10.1056/NEJMoa2108873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sparano JA, et al. Clinical and genomic risk to guide the use of adjuvant therapy for breast cancer. N. Engl. J. Med. 2019;380:2395–2405. doi: 10.1056/NEJMoa1904819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Piccart M, et al. 70-gene signature as an aid for treatment decisions in early breast cancer: updated results of the phase 3 randomised MINDACT trial with an exploratory analysis by age. Lancet Oncol. 2021;22:476–488. doi: 10.1016/S1470-2045(21)00007-3. [DOI] [PubMed] [Google Scholar]
- 60.Prat A, et al. Correlative biomarker analysis of intrinsic subtypes and efficacy across the MONALEESA phase III studies. J. Clin. Oncol. 2021 doi: 10.1200/JCO.20.02977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Dieci MV, et al. Impact of estrogen receptor levels on outcome in non-metastatic triple negative breast cancer patients treated with neoadjuvant/adjuvant chemotherapy. NPJ Breast Cancer. 2021;7:101. doi: 10.1038/s41523-021-00308-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Gingras I, Gebhart G, de Azambuja E, Piccart-Gebhart M. HER2-positive breast cancer is lost in translation: time for patient-centered research. Nat. Rev. Clin. Oncol. 2017;14:669–681. doi: 10.1038/nrclinonc.2017.96. [DOI] [PubMed] [Google Scholar]
- 63.Nitz UA, et al. De-escalation strategies in HER2-positive early breast cancer (EBC): final analysis of the WSG-ADAPT HER2+/HR- phase II trial: efficacy, safety, and predictive markers for 12 weeks of neoadjuvant dual blockade with trastuzumab and pertuzumab ± weekly pac. Ann. Oncol. 2017;28:2768–2772. doi: 10.1093/annonc/mdx494. [DOI] [PubMed] [Google Scholar]
- 64.Graeser M. LBA2 — Impact of RNA expression signatures and tumor infiltrating lymphocytes (TILs) for pathological complete response (pCR) and survival after 12 week de-escalated neoadjuvant pertuzumab + trastuzumab ± paclitaxel in the WSG-HER2+/HR- ADAPT trial. Ann. Oncol. 2021;32(Suppl. 2):S48. doi: 10.1016/j.annonc.2021.03.215. [DOI] [Google Scholar]
- 65.Schettini F, et al. PAM50 HER2-enriched subtype and pathological complete response in HER2-positive early breast cancer: a meta-analysis. Ann. Oncol. 2019;30:v82. doi: 10.1093/annonc/mdz240.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Prat A, et al. A multivariable prognostic score to guide systemic therapy in early-stage HER2-positive breast cancer: a retrospective study with an external evaluation. Lancet Oncol. 2020;21:1455–1464. doi: 10.1016/S1470-2045(20)30450-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Agostinetto E, Eiger D, Punie K, de Azambuja E. Emerging therapeutics for patients with triple-negative breast cancer. Curr. Oncol. Rep. 2021;23:57. doi: 10.1007/s11912-021-01038-6. [DOI] [PubMed] [Google Scholar]
- 68.Bianchini G, et al. LBA13 Tumour infiltrating lymphocytes (TILs), PD-L1 expression and their dynamics in the NeoTRIPaPDL1 trial. Ann. Oncol. 2020;31(Suppl. 4):S1145–S1146. doi: 10.1016/j.annonc.2020.08.2241. [DOI] [Google Scholar]
- 69.Loibl S, et al. A randomised phase II study investigating durvalumab in addition to an anthracycline taxane-based neoadjuvant therapy in early triple-negative breast cancer: clinical results and biomarker analysis of GeparNuevo study. Ann. Oncol. 2019;30:1279–1288. doi: 10.1093/annonc/mdz158. [DOI] [PubMed] [Google Scholar]
- 70.Ren X-Y, et al. Mismatch repair deficiency and microsatellite instability in triple-negative breast cancer: a retrospective study of 440 patients. Front. Oncol. 2021;11:570623. doi: 10.3389/fonc.2021.570623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Emens LA, et al. The tumor microenvironment (TME) and atezolizumab + nab-paclitaxel (A+nP) activity in metastatic triple-negative breast cancer (mTNBC): IMpassion130. J. Clin. Oncol. 2021;39(Suppl. 15):1006. doi: 10.1200/JCO.2021.39.15_suppl.1006. [DOI] [Google Scholar]
- 72.Doroshow DB, et al. PD-L1 as a biomarker of response to immune-checkpoint inhibitors. Nat. Rev. Clin. Oncol. 2021;18:345–362. doi: 10.1038/s41571-021-00473-5. [DOI] [PubMed] [Google Scholar]
- 73.Agostinetto E, et al. Progress and pitfalls in the use of immunotherapy for patients with triple negative breast cancer. Expert Opin. Investig. Drugs. 2022;31:567–591. doi: 10.1080/13543784.2022.2049232. [DOI] [PubMed] [Google Scholar]
- 74.Savas P, et al. Clinical relevance of host immunity in breast cancer: from TILs to the clinic. Nat. Rev. Clin. Oncol. 2016;13:228–241. doi: 10.1038/nrclinonc.2015.215. [DOI] [PubMed] [Google Scholar]
- 75.Murphy WJ, Longo DL. The surprisingly positive association between obesity and cancer immunotherapy efficacy. JAMA. 2019;321:1247–1248. doi: 10.1001/jama.2019.0463. [DOI] [PubMed] [Google Scholar]
- 76.Routy B, et al. Gut microbiome influences efficacy of PD-1-based immunotherapy against epithelial tumors. Science. 2018;359:91–97. doi: 10.1126/science.aan3706. [DOI] [PubMed] [Google Scholar]
- 77.Eiger D, Agostinetto E, Saúde-Conde R, de Azambuja E. The exciting new field of HER2-low breast cancer treatment. Cancers. 2021;13:1015. doi: 10.3390/cancers13051015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Modi S, et al. Trastuzumab deruxtecan in previously treated her2-low advanced breast cancer. N. Engl. J. Med. 2022 doi: 10.1056/NEJMoa2203690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Lenzer J, Brownlee S. Should regulatory authorities approve drugs based on surrogate endpoints? BMJ. 2021;374:n2059. doi: 10.1136/bmj.n2059. [DOI] [PubMed] [Google Scholar]
- 80.Dawoud D, Naci H, Ciani O, Bujkiewicz S. Raising the bar for using surrogate endpoints in drug regulation and health technology assessment. BMJ. 2021;374:n2191. doi: 10.1136/bmj.n2191. [DOI] [PubMed] [Google Scholar]
- 81.Xie W, et al. A systematic review and recommendation for reporting of surrogate endpoint evaluation using meta-analyses. JNCI Cancer Spectr. 2019;3:pkz002. doi: 10.1093/jncics/pkz002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.No authors listed. Validity of surrogate endpoints in oncology: Executive summary of rapid report A10-05, Version 1.1. Institute for Quality and Efficiency in Health Care: Executive Summaries (Institute for Quality and Efficiency in Health Care, 2005). [PubMed]
- 83.Loibl S, et al. Durvalumab improves long-term outcome in TNBC: results from the phase II randomized GeparNUEVO study investigating neodjuvant durvalumab in addition to an anthracycline/taxane based neoadjuvant chemotherapy in early triple-negative breast cancer (TNBC) J. Clin. Oncol. 2021;39(Suppl. 15):506. doi: 10.1200/JCO.2021.39.15_suppl.506. [DOI] [Google Scholar]
- 84.Wolchok JD, et al. Guidelines for the evaluation of immune therapy activity in solid tumors: immune-related response criteria. Clin. Cancer Res. 2009;15:7412–7420. doi: 10.1158/1078-0432.CCR-09-1624. [DOI] [PubMed] [Google Scholar]
- 85.Hoos A, et al. Improved endpoints for cancer immunotherapy trials. J. Natl Cancer Inst. 2010;102:1388–1397. doi: 10.1093/jnci/djq310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Hoos A. Evolution of end points for cancer immunotherapy trials. Ann. Oncol. 2012;23:viii47–viii52. doi: 10.1093/annonc/mds263. [DOI] [PubMed] [Google Scholar]
- 87.Torrisi R, et al. Neoadjuvant chemotherapy in hormone receptor-positive/HER2-negative early breast cancer: when, why and what? Crit. Rev. Oncol. Hematol. 2021;160:103280. doi: 10.1016/j.critrevonc.2021.103280. [DOI] [PubMed] [Google Scholar]
- 88.Symmans WF, et al. Long-term prognostic risk after neoadjuvant chemotherapy associated with residual cancer burden and breast cancer subtype. J. Clin. Oncol. 2017;35:1049–1060. doi: 10.1200/JCO.2015.63.1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.FDA. Table of Surrogate Endpoints that were the Basis of Drug Approval or Licensure https://www.fda.gov/drugs/development-resources/table-surrogate-endpoints-were-basis-drug-approval-or-licensure (2022).
- 90.Gyawali B, Hey SP, Kesselheim AS. Evaluating the evidence behind the surrogate measures included in the FDA’s table of surrogate endpoints as supporting approval of cancer drugs. eClinicalMedicine. 2020 doi: 10.1016/j.eclinm.2020.100332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Schnipper LE, et al. Updating the American Society of Clinical Oncology value framework: revisions and reflections in response to comments received. J. Clin. Oncol. 2016;34:2925–2934. doi: 10.1200/JCO.2016.68.2518. [DOI] [PubMed] [Google Scholar]
- 92.Dafni U, et al. Detailed statistical assessment of the characteristics of the ESMO magnitude of clinical benefit scale (ESMO-MCBS) threshold rules. ESMO Open. 2017;2:e000216. doi: 10.1136/esmoopen-2017-000216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Wolf I, et al. Implementation of the ESMO-magnitude of clinical benefit scale: real world example from the 2022 Israeli National Reimbursement Process. ESMO Open. 2022;7:100379. doi: 10.1016/j.esmoop.2021.100379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Masuda N, et al. Adjuvant capecitabine for breast cancer after preoperative chemotherapy. N. Engl. J. Med. 2017;376:2147–2159. doi: 10.1056/NEJMoa1612645. [DOI] [PubMed] [Google Scholar]
- 95.von Minckwitz G, et al. Trastuzumab emtansine for residual invasive HER2-positive breast cancer. N. Engl. J. Med. 2019;380:617–628. doi: 10.1056/NEJMoa1814017. [DOI] [PubMed] [Google Scholar]
- 96.Tutt ANJ, et al. Adjuvant olaparib for patients with BRCA1- or BRCA2-mutated breast cancer. N. Engl. J. Med. 2021;384:2394–2405. doi: 10.1056/NEJMoa2105215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Heil J, et al. Eliminating the breast cancer surgery paradigm after neoadjuvant systemic therapy: current evidence and future challenges. Ann. Oncol. 2020;31:61–71. doi: 10.1016/j.annonc.2019.10.012. [DOI] [PubMed] [Google Scholar]
- 98.Pfob A, et al. Intelligent vacuum-assisted biopsy to identify breast cancer patients with pathologic complete response (ypT0 and ypN0) after neoadjuvant systemic treatment for omission of breast and axillary surgery. J. Clin. Oncol. 2022;40:1903–1915. doi: 10.1200/JCO.21.02439. [DOI] [PubMed] [Google Scholar]
- 99.Giuliano AE, et al. Effect of axillary dissection vs no axillary dissection on 10-year overall survival among women with invasive breast cancer and sentinel node metastasis: the ACOSOG Z0011 (Alliance) randomized clinical trial. JAMA. 2017;318:918–926. doi: 10.1001/jama.2017.11470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Donker M, et al. Radiotherapy or surgery of the axilla after a positive sentinel node in breast cancer (EORTC 10981-22023 AMAROS): a randomised, multicentre, open-label, phase 3 non-inferiority trial. Lancet Oncol. 2014;15:1303–1310. doi: 10.1016/S1470-2045(14)70460-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Ignatiadis M, Sledge GW, Jeffrey SS. Liquid biopsy enters the clinic — implementation issues and future challenges. Nat. Rev. Clin. Oncol. 2021;18:297–312. doi: 10.1038/s41571-020-00457-x. [DOI] [PubMed] [Google Scholar]
- 102.Garcia-Murillas I, et al. Mutation tracking in circulating tumor DNA predicts relapse in early breast cancer. Sci. Transl Med. 2015;7:302ra133. doi: 10.1126/scitranslmed.aab0021. [DOI] [PubMed] [Google Scholar]
- 103.Garcia-Murillas I, et al. Assessment of molecular relapse detection in early-stage breast cancer. JAMA Oncol. 2019;5:1473–1478. doi: 10.1001/jamaoncol.2019.1838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Papakonstantinou A, et al. Prognostic value of ctDNA detection in patients with early breast cancer undergoing neoadjuvant therapy: a systematic review and meta-analysis. Cancer Treat. Rev. 2022;104:102362. doi: 10.1016/j.ctrv.2022.102362. [DOI] [PubMed] [Google Scholar]
- 105.Turner N. Primary results of the c-TRAK TN trial: a clinical trial utilising ctDNA mutation tracking to detect minimal residual disease and trigger intervention in patients with moderate and high risk early stage triple negative breast cancer. Cancer Res. 2021;82(Suppl. 4):GS3-06. doi: 10.1016/j.annonc.2022.11.005. [DOI] [PubMed] [Google Scholar]
- 106.Lipsyc-Sharf M, et al. Circulating tumor DNA (ctDNA) and late recurrence in high-risk, hormone receptor–positive, HER2-negative breast cancer (CHiRP) J. Clin. Oncol. 2022;40(Suppl. 16):103. doi: 10.1200/JCO.2022.40.16_suppl.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Lipsyc-Sharf M, et al. Circulating tumor DNA and late recurrence in high-risk hormone receptor–positive, human epidermal growth factor receptor 2–negative breast cancer. J. Clin. Oncol. 2022;40:2408–2419. doi: 10.1200/JCO.22.00908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Gebhart G, et al. 18F-FDG PET/CT for early prediction of response to neoadjuvant lapatinib, trastuzumab, and their combination in HER2-positive breast cancer: results from Neo-ALTTO. J. Nucl. Med. 2013;54:1862–1868. doi: 10.2967/jnumed.112.119271. [DOI] [PubMed] [Google Scholar]
- 109.Connolly RM, et al. TBCRC 008: early change in 18F-FDG uptake on PET predicts response to preoperative systemic therapy in human epidermal growth factor receptor 2-negative primary operable breast cancer. J. Nucl. Med. 2015;56:31–37. doi: 10.2967/jnumed.114.144741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Connolly RM, et al. Updated results of TBCRC026: phase II trial correlating standardized uptake value with pathological complete response to pertuzumab and trastuzumab in breast cancer. J. Clin. Oncol. 2021;39:2247–2256. doi: 10.1200/JCO.21.00280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Pérez-García JM, et al. Chemotherapy de-escalation using an 18F-FDG-PET-based pathological response-adapted strategy in patients with HER2-positive early breast cancer (PHERGain): a multicentre, randomised, open-label, non-comparative, phase 2 trial. Lancet Oncol. 2021;22:858–871. doi: 10.1016/S1470-2045(21)00122-4. [DOI] [PubMed] [Google Scholar]
- 112.Longo SK, Guo MG, Ji AL, Khavari PA. Integrating single-cell and spatial transcriptomics to elucidate intercellular tissue dynamics. Nat. Rev. Genet. 2021;22:627–644. doi: 10.1038/s41576-021-00370-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Taichman DB, et al. Sharing clinical trial data: a proposal from the international committee of medical journal editors. Ann. Intern. Med. 2016;164:505–506. doi: 10.7326/M15-2928. [DOI] [PubMed] [Google Scholar]
- 114.Collyar D. An essential partnership: patient advocates and cooperative groups. Semin. Oncol. 2008;35:553–555. doi: 10.1053/j.seminoncol.2008.07.009. [DOI] [PubMed] [Google Scholar]
- 115.Katz ML, et al. Patient advocates’ role in clinical trials: perspectives from Cancer and Leukemia Group B investigators and advocates. Cancer. 2012;118:4801–4805. doi: 10.1002/cncr.27485. [DOI] [PubMed] [Google Scholar]
- 116.Sparano JA, et al. Long-term follow-up of the E1199 phase III trial evaluating the role of taxane and schedule in operable breast cancer. J. Clin. Oncol. 2015;33:2353–2360. doi: 10.1200/JCO.2015.60.9271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Hamy A-S, et al. Prognostic value of the residual cancer burden index according to breast cancer subtype: validation on a cohort of BC patients treated by neoadjuvant chemotherapy. PLoS One. 2020;15:e0234191. doi: 10.1371/journal.pone.0234191. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.