Abstract
Policymakers are pursuing strategies to integrate Medicare and Medicaid coverage for individuals enrolled in both programs, known as dual-eligibles or duals. Dual-eligible Special Needs Plans (D-SNPs) are Medicare Advantage plans that exclusively serve duals, with several features intended to enhance care and facilitate integration with Medicaid. This study compared access to, use of, and satisfaction with care among duals enrolled in D-SNPs versus two other forms of Medicare coverage: Medicare Advantage plans not exclusively serving duals, and traditional Medicare. We found that duals generally reported greater access to care, preventive service use, and satisfaction with care in D-SNPs than in traditional Medicare. However, we found fewer differences in these outcomes among duals in D-SNPs versus other Medicare Advantage plans. Compared with non-Hispanic White duals, duals of color were less likely to report receiving better care in D-SNPs versus other Medicare coverage. These findings suggest that D-SNPs altogether have not provided consistently superior or more equitable care and highlight areas where additional federal and state oversight could strengthen incentives for D-SNPs to improve care.
Keywords: Dual-eligibles, managed care, integration, disparities
Dual eligibles, or duals, are enrolled in Medicare and Medicaid and have complex care needs and social risk factors that reflect their eligibility for both programs.(1) Duals qualify for Medicare because of age, disability, or a diagnosis of end-stage renal disease, and qualify for Medicaid because they have low incomes and limited assets. This intersection of medical and social vulnerability makes duals a high-cost and high-need population: duals have a greater burden of chronic and disabling health conditions than Medicare beneficiaries without Medicaid; 46% live alone or in a nursing facility; and duals account for 34% of Medicare spending despite representing 20% of the Medicare population.(1, 2)
Medicaid is intended to address these needs for care and supportive services by providing supplemental coverage that “wraps around” Medicare. For duals, Medicaid pays for services not covered by Medicare, including long-term care, and in some states, dental and vision care. Medicaid also covers Medicare’s premiums and cost sharing.(3) However, analysts have had longstanding concerns that coverage for duals can be poorly coordinated and difficult to navigate because Medicaid (a state program) is separately financed and administered from Medicare (a federal program).(4) These concerns have led policymakers to develop programs that enroll duals in more integrated models of coverage.(5–7)
Most integrated models are built around managed care plans, in which a private insurer is responsible for coordinating care and bears risk for Medicare, and in some cases Medicaid, spending.(8–10) In Medicare, Dual-Eligible Special Needs Plans (D-SNPs) are Medicare Advantage plans that exclusively serve dual-eligibles and have several features intended to enhance coverage and coordinate care for this population.(11, 12) Further, several features of D-SNPs may provide an opportunity to integrate Medicare and Medicaid coverage.
First, D-SNPs are required to develop care management models and tailor provider networks to meet duals’ specialized care needs.(9, 13)
Second, D-SNPs, like other Medicare Advantage plans that do not exclusively serve duals, are required to use rebates (additional payments to plans under Medicare Advantage’s competitive bidding system) to enhance benefits or lower out-of-pocket costs for enrollees. However, unlike other Medicare Advantage plans, D-SNPs often use rebates to supplement Medicaid’s “wrap around” benefits.(14) For example, many D-SNPs cover dental, vision, or supportive services such as transportation to medical providers, for which Medicaid coverage varies by state and can be limited.(9)
Third, D-SNPs are required to have contracts with state Medicaid programs that define the plan’s responsibilities for coordinating care with Medicaid.(10, 13, 14) These contracts are intended to serve as a platform for integrating Medicare and Medicaid coverage. While most contracts include only limited integration requirements (for example, requiring a D-SNP to notify Medicaid when a patient is admitted to the hospital), some contracts require D-SNPs to attain higher levels of integration. At the highest level of integration, a D-SNP or its parent insurer will have a contract to cover enrollees’ Medicaid spending, including long-term care spending, giving the insurer full financial and administrative responsibility for managing dual-eligibles’ care.(9, 11, 14)
D-SNPs are becoming an increasingly prominent part of the Medicare coverage landscape and efforts to integrate coverage for duals.(14) Congress permanently authorized D-SNPs in 2018, and CMS continues to refine integration standards for these plans.(11, 12) In 2022, 4.1 million duals, or roughly 30% of all duals, were enrolled in D-SNPs. D-SNPs also play an important role covering traditionally underserved subpopulations of duals. For example, a recent analysis estimated that 64% of D-SNP enrollees are Black, Hispanic, or other people of color,(15) compared with 48% of the dual population overall.(14) Thus, the performance of D-SNPs has important consequences for health equity.
However, little is known about whether D-SNPs are associated with better care for duals overall, or for duals of color specifically, compared to alternative forms of Medicare coverage: namely, other Medicare Advantage plans that do not exclusively serve duals, and the federally-run traditional Medicare program. We are aware of only two studies that compared care for duals across these types of coverage. One study found that duals in D-SNPs had lower rates of hospital and nursing facility admissions, and greater use of home and community-based services, compared with duals in other Medicare Advantage plans.(16) However, the study did not compare D-SNPs with traditional Medicare. A second study found that D-SNPs generally performed no better than other forms of Medicare coverage on patient experience measures.(15) Neither study examined differences in care by race and ethnicity.
Evidence about the performance of D-SNPs can guide evolving integration policy and incentives for plans to improve care for underserved subpopulations of duals, who may benefit from enhanced coverage and care coordination.(14) Such evidence is also pertinent to Medicare financing, given prior evidence that D-SNPs have received higher per-capita payments and had higher profit margins than other Medicare Advantage plans serving similar patients.(9, 17) Thus, it is critical to examine whether D-SNPs provide better care to duals, commensurate with Medicare’s higher payments to these plans.
To fill this evidence gap, we compared access to care, use of preventive services and emergency care, and satisfaction with care among duals enrolled in D-SNPs, other Medicare Advantage plans, and traditional Medicare. We further examined whether differences in care by type of Medicare coverage varied by race and ethnicity.
METHODS
Data
We analyzed the 2015–2019 Medicare Current Beneficiary Survey (MCBS). The MCBS is a national survey of the Medicare population that follows rotating cohorts of Medicare beneficiaries for up to four years.(18) We analyzed restricted-use files that included linked administrative records of Medicare and Medicaid enrollment.
Sample
We analyzed MCBS respondents who received “full” Medicaid for at least one month of the survey year and lived in the community at the time of the survey. We limited analyses to respondents with full Medicaid because these individuals receive comprehensive Medicaid wrap-around coverage, whereas “partial” Medicaid only assists with Medicare premiums, and in some cases, cost sharing.(1) Moreover, recipients of partial Medicaid typically are not the focus of integration policy.(9) We limited analyses to community-dwelling respondents because the MCBS asks different questions about care for respondents living in nursing facilities.
We implemented three additional exclusions. First, we excluded a small number of duals in Special Needs Plans for people with chronic illnesses and enrollees of Medicare-Medicaid Plans created under the CMS Financial Alignment Initiative.(6) (Our sample did not include enrollees of the Program of All-Inclusive Care for the Elderly, an integrated model serving roughly 55,000 people.(14)) Second, we excluded respondents in US territories. Third, we excluded respondents with missing data on covariates.
Classifying Medicare coverage
We used administrative data to classify duals into one of three Medicare coverage types: D-SNPs, other Medicare Advantage plans not exclusively serving duals, and traditional Medicare. Because of small sample sizes, we pooled all respondents in D-SNPs, including those whose plans met both limited and extensive integration standards, into a single category.
A unique feature of Medicare Advantage is that duals can change plans or switch between Medicare Advantage and traditional Medicare during the year. (For other Medicare beneficiaries, “lock-in” provisions restrict such changes to an annual open enrollment period.) For our primary analyses, we categorized Medicare coverage based on January enrollment. We conducted a sensitivity analysis using December enrollment.
Outcomes
We analyzed respondent-reported measures of care in four domains: access to care, use of preventive care, emergency department use, and satisfaction with care. These are areas in which D-SNPs’ coverage of supplemental services, care management strategies, provider networks, and responsibility for coordinating care with Medicaid may affect care. Moreover, D-SNPs, like other Medicare Advantage plans, are incentivized to enhance preventive care, access to care, and patient care ratings via the Medicare Advantage star rating system, which determines whether plans receive bonus payments.
Under the access domain, we assessed whether respondents were able to get needed care in the past year, had a primary care provider, and were able to get needed dental care in the past year.
Under the preventive care domain, we examined whether respondents received a flu vaccine the prior winter and had their blood pressure and blood cholesterol checked in the past year.
We assessed whether respondents reported using a hospital emergency department for care in the past year, since D-SNPs’ emphasis on care management for duals could affect emergency department use.
Finally, we assessed respondents’ satisfaction with their overall care and in five areas: out-of-pocket costs, receipt of information about health problems, ease of getting answers by phone about treatments or medications, convenience of getting to the doctor from home, and availability of specialists. We examined satisfaction with out-of-pocket costs because D-SNPs can cover additional services at no cost to enrollees. Satisfaction with information given about health problems, treatments, and medications reflect aspects of communication and care coordination that may be important for patients with complex care needs. Satisfaction with the convenience of getting to the doctor may reflect the adequacy of provider networks and plans’ coverage of supplemental benefits such as transportation services. Ratings of availability of specialists may reflect the extent to which provider networks meet duals’ specialized care needs. The Appendix gives detailed variable definitions.(19)
Covariates
We used the MCBS to assess several respondent-reported characteristics: race and ethnicity, marital status, and education, and lifetime tobacco use. We used administrative data to assess age, sex, Medicare eligibility due to disability or presence of end-stage renal disease, state of residence, and residence in a rural area. We used the MCBS health status and functioning questionnaire to assess respondent-reported difficulties with activities of daily living (such as eating or bathing), difficulties with instrumental activities of daily living (such as preparing light meals or managing money), and lifetime history of chronic disease (13 indicators). We linked data from the Area Health Resources File to control for the annual per-capita supply of physicians and dentists by county.
Statistical analyses
We used propensity score weighting to balance samples of duals in D-SNPs, other Medicare Advantage plans, and traditional Medicare. We estimated a multinomial propensity score model that predicted respondents’ annual enrollment in one of these coverage categories as a function of the covariates described above, state fixed effects (to account for time-invariant differences across state Medicaid programs), and year fixed effects (to account for secular trends). From these models, we constructed propensity score weights, defined as the inverse of the predicted probability of enrollment in the respondent’s observed coverage in a year.
We then compared access to care, use of preventive care, emergency department use, and satisfaction with care across categories of Medicare coverage. We estimated linear regression models that predicted each outcome as a function of the type of Medicare coverage, adjusting for the covariates described above, state fixed effects, and year fixed effects. We weighted models by a composite of propensity score weights and MCBS survey weights to produce nationally representative estimates.
Finally, we examined the extent to which D-SNP enrollment, compared to other Medicare coverage, was associated with either better or worse care among duals of color vs. non-Hispanic white duals. Duals of color were those identifying their ethnicity as Hispanic or their race as Black, Asian or Pacific Islander, Native American or Alaska Native, Native Hawaiian, another race, or multiracial. We estimated respondent-level linear regression models that predicted each outcome as a function of Medicare coverage, race/ethnicity, and the interaction of these terms. We adjusted for covariates described above, state fixed effects, and year fixed effects, and weighted models by a composite of propensity score weights and survey weights. From these models, we estimated adjusted differences in outcomes among duals of color in D-SNPs versus other Medicare coverage. We estimated analogous differences among non-Hispanic White duals. Last, we compared these differences to quantify the extent to which duals of color, compared to non-Hispanic white duals, experienced relatively better or worse care in D-SNPs versus other Medicare coverage.
All models were estimated with robust standard errors clustered on respondents. Additional details about our analyses are in the Appendix.(19)
Supplementary analyses
We conducted several supplementary analyses. First, because duals can change Medicare coverage during the year, we classified duals according to their Medicare coverage in December. Second, we examined whether response rates to questions used to construct outcome variables differed by Medicare coverage. Other sensitivity analyses are described in the Appendix.(19)
Limitations
Our study had several limitations. First, the MCBS did not explicitly ask about coordination of services financed by Medicare (inpatient care) and Medicaid (long-term care), where D-SNPs may be able to improve care coordination.(5) Second, small sample sizes limited our ability to detect small but potentially salient differences in care by Medicare coverage, race, and ethnicity. Small samples also precluded us from analyzing differences in care between D-SNPs with higher versus lower levels of Medicaid integration. Third, our study period preceded the introduction of new integration standards for D-SNPs, which took effect in 2021.(11) However, the extent of D-SNP integration with Medicaid continues to evolve due to changes in federal and state policy,(7, 12) and our findings can inform ongoing reforms. Fourth, although we used propensity score weighting to adjust for observable differences among individuals with different Medicare coverage, unmeasured differences may have biased our estimates.
RESULTS
Sample characteristics
Our sample consisted of 9,885 respondent-year observations, representing 32,420,651 person-years in the community-dwelling dual-eligible population from 2015–2019 (Appendix Exhibit 1) (19). In this population, 18.1% of duals were enrolled in D-SNPs, 13.4% were enrolled in other Medicare Advantage plans, and 68.5% were in traditional Medicare (Appendix Exhibit 2) (19).
Fully 67.2% of duals in D-SNPs were people of color, exceeding the proportions in other Medicare Advantage plans (59.3%) and traditional Medicare (52.0%) (Exhibit 1). Duals in D-SNPs were more likely to be female and have less than a high school education than duals with other Medicare coverage. A smaller proportion of duals in D-SNPs qualified for Medicare because of a disability or end-stage renal disease than duals in traditional Medicare. However, similar or slightly higher proportions of duals in D-SNPs had chronic diseases such as diabetes and hypertension than duals with other Medicare coverage.
Exhibit 1:
Characteristics of dual eligibles enrolled in Dual Eligible Special Needs Plans, other Medicare Advantage plans, and traditional Medicare
| Characteristic | D-SNPs | Other Medicare Advantage | Traditional Medicare | |
|---|---|---|---|---|
| Age, years | 66.2 | 67.6 | 60.9 | **** |
| Female, % | 66.5 | 61.1 | 59.7 | ** |
| Race and ethnicity, % in category: b | ||||
| White, non-Hispanic | 31.9 | 40.4 | 46.7 | **** |
| Black, non-Hispanic | 26.0 | 17.0 | 20.1 | |
| Hispanic | 33.5 | 32.4 | 18.7 | |
| Asian or Pacific Islander | 4.0 | 6.8 | 6.8 | |
| Multiracial or other race c | 3.7 | 3.1 | 6.4 | |
| Education, % in category: d | ||||
| Less than high school education | 45.4 | 41.2 | 39.2 | ** |
| High school or vocational education | 31.3 | 35.1 | 37.0 | |
| College education or higher | 22.4 | 23.3 | 23.1 | |
| Marital status, % in category: | ||||
| Married | 21.4 | 26.1 | 20.5 | ** |
| Separated or divorced | 33.7 | 27.4 | 29.5 | |
| Widowed | 20.9 | 23.8 | 17.9 | |
| Never married | 23.9 | 22.6 | 32.0 | |
| Any lifetime tobacco use, % | 50.5 | 50.0 | 52.7 | |
| Eligible for Medicare because of disability or end-stage renal disease, % e | 33.9 | 34.7 | 50.9 | **** |
| Number of difficulties with activities of daily living f | 1.26 | 1.42 | 1.40 | |
| Number of difficulties with instrumental activities of daily living g | 1.04 | 1.22 | 1.29 | **** |
| Rural resident, % h | 4.6 | 2.3 | 10.0 | **** |
| Presence of chronic conditions, % reporting a prior diagnosis: | ||||
| Diabetes | 46.9 | 43.6 | 37.8 | **** |
| Coronary artery disease | 7.9 | 10.2 | 8.7 | |
| Hypertension | 70.0 | 69.3 | 62.8 | **** |
| Myocardial infarction | 14.1 | 13.5 | 11.7 | |
| Congestive heart failure | 9.6 | 10.5 | 10.7 | |
| Coronary heart disease | 10.7 | 8.7 | 8.2 | |
| Hyperlipidemia | 66.1 | 62.3 | 58.5 | **** |
| Cancer | 14.9 | 10.3 | 13.8 | ** |
| Depression | 45.8 | 43.5 | 46.9 | |
| Behavioral health disorder | 18.8 | 15.9 | 23.8 | **** |
| Asthma or chronic obstructive pulmonary disease | 30.5 | 28.3 | 30.9 | |
| Osteoporosis | 21.6 | 21.4 | 17.5 | ** |
| Rheumatoid Arthritis | 33.6 | 32.2 | 26.5 | **** |
Statistical significance is denoted as follows:
P<0.001,
P<0.01,
P<0.05,
P<0.01.
P-values are for differences in the means or proportions of each characteristic among dual eligibles enrolled in Dual Eligible Special Needs Plans (D-SNPs), other Medicare Advantage plans not exclusively serving dual eligibles, and traditional Medicare.
Notes: Estimates based on a sample of 9,885 observations in the 2015–2019 Medicare Current Beneficiary Survey (MCBS), limited to community-dwelling full-benefit dual-eligibles. When weighted, this sample represents 32,420,651 person-years.
Characteristics of dual-eligibles by category of Medicare coverage, weighted by survey weights to produce nationally representative estimates. Characteristics weighted by a composite of propensity score weights and survey weights are reported in Appendix Exhibit 3 (full sample) and Appendix Exhibit 4 (stratified by race and ethnicity).
Race and ethnicity are self-reported by MCBS respondents. Approximately 1.1% of MCBS respondents in our sample did not report their race or ethnicity (not shown in table).
Includes dual-eligibles who self-identified as Native Hawaiian, Native American or Alaska Native, another race, or multiracial.
Approximately 0.6% of MCBS respondents in our sample did not report their education (not shown in table).
Propensity score and outcome models included separate indicators for whether beneficiaries were eligible for Medicare due to disability vs. end-stage renal disease (eligibility for Medicare due to age was the reference).
Number of activities daily living that a respondent reported difficulty performing or did not perform due to health (bathing, dressing, eating, using the toilet, walking, and getting into or out of a chair or bed).
Number of instrumental activities daily living that that a respondent reported any difficulty performing or did not perform due to health (using the telephone, shopping, managing money, doing light housework, and preparing meals).
Residence in a rural area based on Office of Management and Budget Core-Based Statistical Area designations.
Source: Authors’ analyses of the MCBS from 2015–2019.
Weighting by a composite of propensity score weights and survey weights improved balance on most characteristics across Medicare coverage categories (Appendix Exhibit 3) (19). Sample characteristics were also balanced when we separately analyzed duals of color and non-Hispanic white duals (Appendix Exhibit 4) (19).
Adjusted differences in care by type of Medicare coverage
Compared to duals with traditional Medicare, duals in D-SNPs reported better access to care on two of three access measures, were more likely to receive preventive services, and reported higher rates of satisfaction on four of six measures (P<0.10 for all comparisons; Exhibits 2 and 3). However, some of these differences were modest. For example, compared to duals in traditional Medicare, duals in D-SNPs were 3.6 percentage points more likely to obtain needed dental care and 1.9 percentage points more likely to report being satisfied with their overall care. For comparison, 78.3% of all duals were able to obtain needed dental care and 92.9% were satisfied with their overall care. The margin by which duals reported greater preventive service use and satisfaction with care in D-SNPs versus traditional Medicare was larger on other measures—notably, flu vaccinations and satisfaction with out-of-pocket costs.
Exhibit 2:
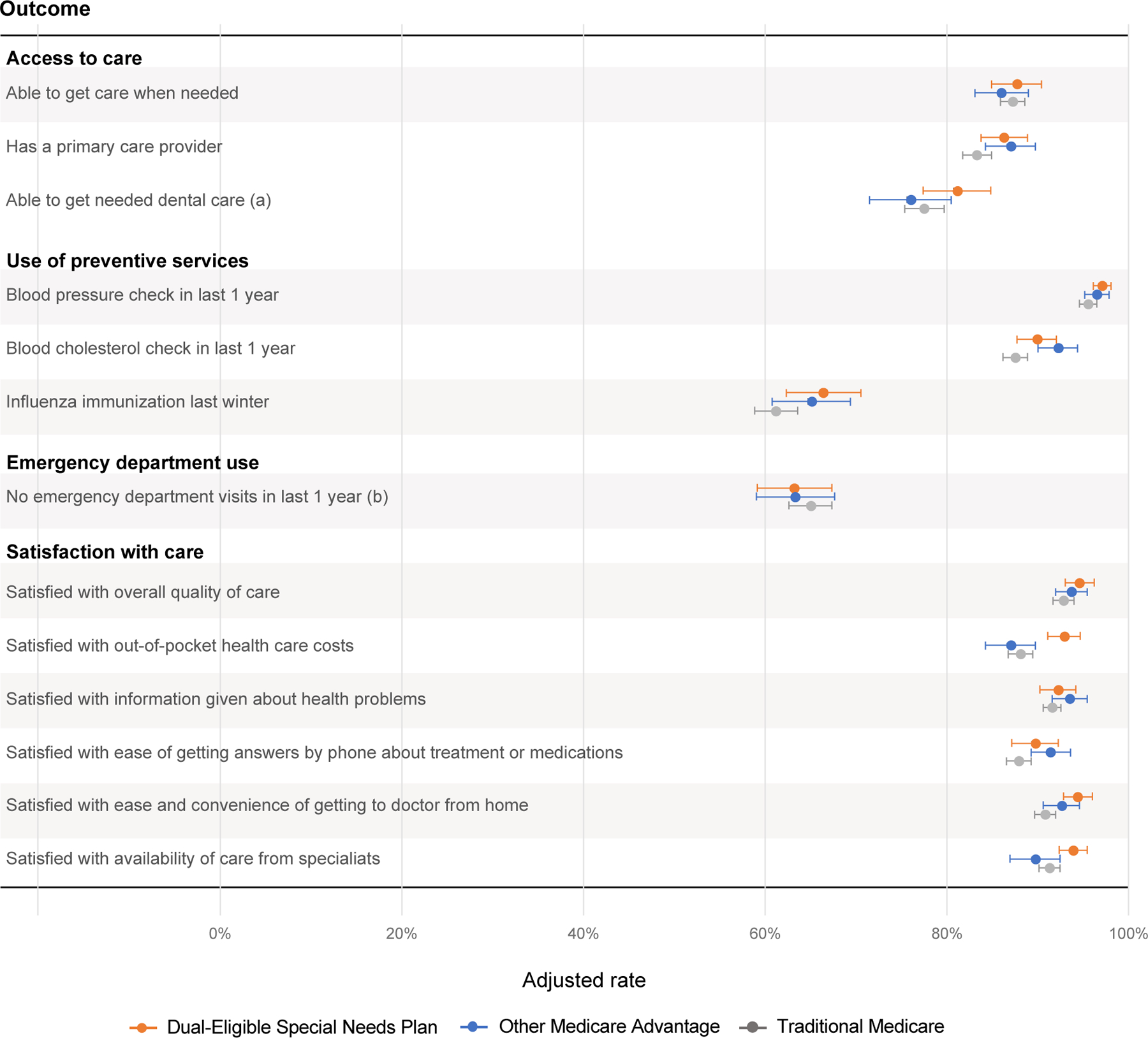
Access to, use of, and satisfaction with care among dual-eligibles enrolled in Dual Eligible Special Needs Plans, other Medicare Advantage plans, and traditional Medicare
Notes: Figure displays adjusted rates of study outcomes among dual eligibles in Dual Eligible Special Needs Plans (D-SNPs), other Medicare Advantage plans not exclusively serving dual eligibles, and traditional Medicare. Shaded circles show adjusted estimates. Error bars show 95% confidence intervals, constructed using robust standard errors clustered at the respondent level to account intra-person correlation over time. Estimates adjusted for covariates in Exhibit 1, annual supply of physicians per 1,000 county residents, annual supply of dentists per 1,000 county residents, state fixed effects, and year fixed effects, and weighted by a composite of propensity score weights and survey weights. Adjusted estimates calculated using the method of average marginal effects (see Appendix for details). Exhibit 3 reports corresponding regression estimates for the adjusted differences in study outcomes between dual eligibles enrolled in D-SNPs vs. other Medicare Advantage plans or traditional Medicare.
a Question not asked in the 2015 MCBS.
b Question was asked only of new survey respondents in the 2015 and 2016 MCBS.
Source: Authors’ analyses of the MCBS from 2015–2019.
Exhibit 3:
Overall differences in dual eligibles’ access to, use of, and satisfaction with care in Dual Eligible Special Needs Plans, other Medicare Advantage plans, and traditional Medicare
| Adjusted differences
b |
|||
|---|---|---|---|
| Outcome | Overall Mean among dual eligibles a | D-SNPs vs. traditional Medicare | D-SNPs vs. other Medicare Advantage |
| Estimates (percentage points) | |||
| Access to care | |||
| Able to get care when needed | 87.3 | 0.5 | 1.7 |
| Has a primary care provider | 83.6 | 2.9** | −0.7 |
| Able to get dental care when needed c | 78.3 | 3.6* | 5.0* |
| Use of preventive care | |||
| Blood pressure check in last 1 year | 95.9 | 1.6** | 0.6 |
| Blood cholesterol check in last 1 year | 87.7 | 2.4* | −2.3 |
| Influenza immunization last winter | 62.7 | 5.2** | 1.3 |
| Emergency department use | |||
| No emergency department visits in last 1 year d | 64.8 | −1.8 | −0.1 |
| Satisfaction with care | |||
| Satisfied with overall quality of care | 92.9 | 1.9* | 1.0 |
| Satisfied with out-of-pocket health care costs | 88.7 | 4.8**** | 5.9**** |
| Satisfied with information given about health problems | 91.8 | 0.6 | −1.3 |
| Satisfied with ease of getting answers by phone about treatment or medications | 88.3 | 1.8 | −1.7 |
| Satisfied with ease and convenience of getting to doctor from home | 91.3 | 3.6**** | 1.8 |
| Satisfied with availability of care from specialists | 91.6 | 2.6** | 4.2*** |
Statistical significance is denoted as follows:
P<0.10,
P<0.05,
P<0.01,
P<0.001.
Overall mean among all dual eligibles in our sample over the 2015–2019 period, weighted by survey weights.
Adjusted difference in the rate of each outcome between dual eligibles enrolled in D-SNPs vs. traditional Medicare (left column) or in D-SNPs vs. other Medicare Advantage plans not exclusively serving dual eligibles (right column). Estimates adjusted for covariates in Exhibit 1, annual supply of physicians per 1,000 county residents, annual supply of dentists per 1,000 county residents, state fixed effects, and year fixed effects, and weighted by a composite of propensity score weights and survey weights. Adjusted differences reported in this exhibit correspond to the differences in adjusted estimates graphed in Exhibit 2.
Question not asked in the 2015 MCBS.
Question was asked only of new survey respondents in the 2015 and 2016 MCBS.
We found fewer differences in access to, use of, and satisfaction with care between D-SNPs and other Medicare Advantage plans (Exhibits 2 and 3). On access measures, duals in D-SNPs only reported better access to dental care than duals in other Medicare Advantage plans. We found no differences between D-SNPs and other Medicare Advantage plans on preventive care use. Compared to duals in other Medicare Advantage plans, duals in D-SNPs reported higher rates of satisfaction on only two of six care satisfaction measures (out-of-pocket costs and availability of care from specialists).
We did not find differences in satisfaction with the ease of getting answers by phone about treatments or medications, or with the provision of information to address health problems, across categories of Medicare coverage. We also found no differences in emergency department use by coverage type.
Approximately 90% of duals had the same type of Medicare coverage in January and December of the same year (Appendix Exhibit 5) (19). Findings were similar when we categorized duals by Medicare coverage in December and in other sensitivity analyses (Appendix Exhibit 6) (19). Response rates to survey questions used to measure outcomes were generally high and comparable across coverage categories (Appendix Exhibit 7) (19).
Differences by race and ethnicity
The extent to which duals reported greater access to care, use of preventive care, and satisfaction with care in D-SNPs versus other Medicare coverage differed by race and ethnicity (Exhibit 4). On access measures, only non-Hispanic White duals—but not duals of color—were more likely to receive needed dental care in D-SNPs versus other Medicare coverage. For example, among non-Hispanic White duals, those enrolled in D-SNPs were 10.7 percentage points more likely to receive needed dental care than those in traditional Medicare. Among duals of color, this difference was small and statistically insignificant (-0.4 percentage points). Consequently, we estimated that duals of color were 11.1 percentage points less likely to have better access to dental care in D-SNPs versus other Medicare Advantage plans, compared to the difference among non-Hispanic White duals.
Exhibit 4:
Racial and ethnic differences in dual eligibles’ access to, use of, and satisfaction with care in Dual Eligible Special Needs Plans, other Medicare Advantage plans, and traditional Medicare
| Adjusted differences among
dual eligibles of color a |
Adjusted differences among
Non-Hispanic White dual eligibles a |
Comparison of adjusted
differences by race and ethnicity b |
||||
|---|---|---|---|---|---|---|
| Outcome | D-SNPs vs. traditional Medicare | D-SNPs vs. other Medicare Advantage | D-SNPs vs. traditional Medicare | D-SNPs vs. other Medicare Advantage | D-SNPs vs. traditional Medicare | D-SNPs vs. other Medicare Advantage |
| Estimates (percentage points) | ||||||
| Access to care | ||||||
| Able to get care when needed | −0.9 | 1.3 | 2.2 | 2.3 | −3.2 | −1.0 |
| Has a primary care provider | 2.5 | −1.0 | 3.5 | −0.2 | −1.0 | −0.8 |
| Able to get dental care when needed c | −1.2 | −0.4 | 7.7** | 10.7** | −8.9* | −11.1* |
| Use of preventive care | ||||||
| Blood pressure check in last 1 year | 0.7 | 1.6 | 2.4** | −1.1 | −1.6 | 2.7 |
| Blood cholesterol check in last 1 year | 0.4 | −2.3 | 4.6** | −3.0 | −4.2* | 0.7 |
| Influenza immunization last winter | 7.9*** | 6.6* | 1.1 | −5.5 | 6.8 | 12.1** |
| Emergency department use | ||||||
| No emergency department visits in last 1 year d | −3.3 | −2.4 | 0.6 | 3.3 | −3.8 | −5.7 |
| Satisfaction with care | ||||||
| Satisfied with overall quality of care | 0.4 | −0.9 | 4.0*** | 3.3* | −3.6* | −4.2* |
| Satisfied with out-of-pocket health care costs | 3.8** | 6.0** | 6.5**** | 6.9*** | −2.7 | −0.9 |
| Satisfied with information given about health problems | −0.4 | −2.5 | 2.5 | 0.7 | −2.9 | −3.2 |
| Satisfied with ease of getting answers by phone about treatment or medications | −0.2 | −3.2 | 4.5* | 0.4 | −4.7 | −3.6 |
| Satisfied with ease and convenience of getting to doctor from home | 3.2** | −0.5 | 4.7*** | 5.3** | −1.6 | −5.9** |
| Satisfied with availability of care from specialists | 0.5 | −1.3 | 5.0*** | 10.7**** | −4.5** | −12.0**** |
Statistical significance is denoted as follows:
P<0.10,
P<0.05,
P<0.01,
P<0.001.
Regression-adjusted differences between Dual Eligible Special Needs Plans (D-SNPs), traditional Medicare, and other Medicare Advantage plans not exclusively serving dual eligibles, among dual eligibles of color (left pair of columns) and non-Hispanic White dual eligibles (middle pair of columns). Estimates adjusted for covariates in Exhibit 1, annual supply of physicians per 1,000 county residents, annual supply of dentists per 1,000 county residents, state fixed effects, and year fixed effects, and weighted by a composite of propensity score weights and survey weights. Statistical significance tests conducted using robust standard errors clustered at the respondent level to account intra-person correlation over time. MCBS respondents who did not report their race or ethnicity were excluded.
Columns report a comparison of two differences: (1) the adjusted difference in outcomes between D-SNPs and other Medicare coverage (i.e., traditional Medicare and other Medicare Advantage plans) among dual eligibles of color, compared with (2) the analogous difference among non-Hispanic White dual eligibles. Positive numbers indicate that the adjusted difference between D-SNPs and other Medicare coverage is greater among dual eligibles of color, relative to the analogous difference among non-Hispanic White dual eligibles. For example, we estimated that dual eligibles of color were 12.1 percentage points more likely to have received a flu vaccination in D-SNPs than in other Medicare Advantage plans, compared with the analogous difference among non-Hispanic White dual eligibles. Negative numbers indicate that the adjusted difference between D-SNPs and other Medicare coverage is smaller among dual eligibles of color than among non-Hispanic White dual eligibles. For example, we estimated that dual eligibles of color were 12.0 percentage points less likely to be more satisfied with the availability of care from specialists in D-SNPs than other Medicare Advantage plans compared to the difference among non-Hispanic White dual eligibles.
Question not asked in the 2015 MCBS.
Question was asked only of new survey respondents in the 2015 and 2016 MCBS.
Source: Authors’ analyses of the MCBS from 2015–2019.
Non-Hispanic White duals were more likely to receive blood pressure and cholesterol screenings in D-SNPs versus traditional Medicare. However, duals of color were not more likely to receive these services in D-SNPs compared with other Medicare coverage. Conversely, among duals of color, receipt of flu vaccinations was higher in D-SNPs versus other types of Medicare coverage.
On care satisfaction measures, duals of color in D-SNPs reported greater satisfaction than those in traditional Medicare and other Medicare Advantage plans only with respect to out-of-pocket costs. Duals of color were not more likely to report satisfaction with their overall care, ease of getting to the doctor, or availability of care from specialists in D-SNPs versus other Medicare Advantage plans. However, in each of these areas, non-Hispanic White duals reported greater satisfaction in D-SNPs versus other Medicare Advantage plans. Consequently, duals of color were 4.2 percentage less likely to be satisfied with their overall care in D-SNPs than in other Medicare Advantage plans, compared to differences among non-Hispanic White duals.
Further, duals of color in D-SNPs reported lower absolute levels of access to dental care and satisfaction with overall care than non-Hispanic White duals in D-SNPs (Appendix Exhibit 8).
DISCUSSION
This study used national survey data to compare dual-eligibles’ access to, use of, and satisfaction with care in D-SNPs, other Medicare Advantage plans not exclusively serving duals, and traditional Medicare. We had three main findings. First, duals in D-SNPs generally reported greater access to care, use of preventive services, and satisfaction with care than duals in traditional Medicare, although some differences were small. Second, we found fewer differences in care between D-SNPs and other Medicare Advantage plans not exclusively serving duals, because other Medicare Advantage plans often performed comparably to—or sometimes better than—D-SNPs. Third, enrollment in D-SNPs, versus other Medicare coverage, was associated with fewer and smaller improvements in care among duals of color than among non-Hispanic White duals.
These findings raise concerns about the value of care provided by D-SNPs. Because D-SNPs specialize in managing care for duals, can tailor enhanced benefits for these patients, and are required to have contracts with Medicaid programs to coordinate care—features intended to enhance integration—the hope has been that D-SNPs would provide superior care for duals. While we found that enrollment in D-SNPs was associated with better care compared to traditional Medicare, the gains were more isolated when we compared D-SNPs to other Medicare Advantage plans. D-SNPs only performed better than other Medicare Advantage plans in areas related to satisfaction with out-of-pocket costs and where D-SNPs frequently provide supplemental benefits (for example, dental coverage). Notably, D-SNPs did not perform better than other Medicare Advantage plans in areas pertinent to care coordination, such as communication with patients about health problems, treatments, and medications. These findings are worrisome given the expectation that D-SNPs, by specializing in care for duals, would provide more robust care management tailored to this population. Further, prior analyses found that D-SNPs have received higher payments per enrollee than other Medicare Advantage plans serving dual-eligibles.(17) Despite receiving higher payments, D-SNPs do not appear to provide substantially better care to duals than other Medicare Advantage plans, particularly in areas that may be important for patients with complex care needs.
Our results also raise concerns about equity: where D-SNPs provided better care compared with other Medicare coverage, the gains did not accrue equally to duals of color. One might expect traditionally underserved populations, including duals of color, would benefit more from D-SNPs’ enhanced coverage and coordination with Medicaid. Yet on several measures of access (ability to get needed dental care), preventive care (blood pressure and cholesterol screenings), and satisfaction (overall satisfaction and availability of specialists), only non-Hispanic White duals reported relatively better care in D-SNPs versus other Medicare coverage. Nearly one-half of duals, and two-thirds of D-SNP enrollees, are people of color. Thus, our findings highlight a missed opportunity for D-SNPs to improve care for a large subset of enrollees, which would meaningfully advance health equity.
Looking forward, and options for policy
While these findings are concerning, we note that they reflect an average among D-SNP enrollees from 2015–2019 and do not represent the performance of any single plan. During our study period, most D-SNPs had limited administrative responsibility for coordinating care with Medicaid and few had attained more substantial Medicaid integration (for example, bearing risk for Medicare and Medicaid spending).(9) During our study period, and increasingly since, more D-SNPs have become integrated with Medicaid.(20) The most integrated plans, known as Fully Integrated Dual-Eligible SNPs (FIDE-SNPs), either directly cover Medicaid benefits for enrollees, or cover benefits through a companion Medicaid managed care plan operated by the D-SNP’s parent insurer.(14) In principle, this arrangement creates incentives for plans to develop care management strategies to deliver the most efficient mix of services, because the same insurer is at risk for Medicare and Medicaid spending for the same patients. Emerging evidence from single states suggests that fully integrated plans improve quality of care in some areas and reduce hospital utilization.(5, 21, 22) Thus, there is potential for duals to experience better care in D-SNPs as integration with Medicaid increases.
However, our results also highlight the importance of monitoring whether care improvements accrue equally to traditionally underserved populations. Stratified reporting of performance for subgroups of enrollees (for example, by race and ethnicity) could facilitate monitoring of disparities and inform how policymakers and plans advance health equity, which CMS identified as a policy priority in recent regulatory changes pertaining to D-SNPs.(12, 23) Currently, CMS reports race- and ethnicity-stratified performance for Medicare Advantage plans,(24) including D-SNPs, but it does not incorporate stratified estimates into Medicare Advantage star ratings, which summarize a plan’s overall performance and determine whether plans receive bonus payments. Some analysts have proposed stratifying performance measures and incorporating assessments of equitable care into star ratings.(25, 26) These changes could be particularly constructive for D-SNPs, both by drawing attention to how plans perform for underserved patients and creating incentives for D-SNPs to invest in better care for those patients (for example, enhancing transportation services to improve access to care for duals of color). Stratified reporting could also build on emerging efforts to improve monitoring of D-SNP performance, which include a recently finalized CMS decision to report star ratings for D-SNPs separately from other plans under the same Medicare Advantage contract.(12) State Medicaid programs may also play a role in catalyzing change by leveraging their contracts with D-SNPs to require that plans meet equity-focused goals for quality reporting and performance improvement.
The role of D-SNPs in providing coverage to duals is likely to increase, both from organic enrollment growth and as CMS prepares to wind down the Financial Alignment Initiative’s Medicare-Medicaid Plans, which CMS has signaled may be converted into D-SNPs.(7) Our results suggest that D-SNPs have considerable room to improve as they grow, and that improvements may be facilitated by greater attention to how plans perform for duals of color. Both CMS (through its regulatory oversight of Medicare Advantage plans), and states (through contracts with D-SNPs), could play complementary roles in monitoring plan performance and creating incentives to advance equity.
Conclusion
During the period 2015–2019, we found that dual-eligibles in D-SNPs generally had greater access to care, use of preventive services, and satisfaction with care than duals in traditional Medicare. However, we found fewer differences between D-SNPs and other Medicare Advantage plans not exclusively serving duals. We also found that, compared with non-Hispanic White duals, duals of color were less likely to report better care in D-SNPs versus other Medicare coverage. These findings raise concerns about whether D-SNPs have delivered superior and equitable care and highlight areas where federal regulation and state oversight could incentivize plans to improve performance and advance health equity.
Supplementary Material
Acknowledgements
Supported by grants from Arnold Ventures and the Agency for Healthcare Research and Quality (grant K01HS026727). This work does not necessarily reflect the views of Arnold Ventures or the Agency for Healthcare Research and Quality. The authors thank John Lovelace, UPMC Health Plan, for helpful comments on an earlier draft of this manuscript.
Contributor Information
Eric T. Roberts, Department of Health Policy and Management, University of Pittsburgh School of Public Health, Phone: 412-383-0439
Jennifer M. Mellor, Department of Economics, William and Mary, Phone: 757-221-1913
REFERENCES
- 1.Data Book: Beneficiaries dually eligible for Medicare and Medicaid. Report Washington, DC: Medicare Payment Advisory Commission and Medicaid and CHIP Payment and Access Commission; 2022. February 2022. [Google Scholar]
- 2.Kasper JD, O’Malley Watts M, Lyons B. Chronic Disease and Co‐Morbidity Among Dual Eligibles: Implications for Patterns of Medicaid and Medicare Service Use and Spending Washington, DC: Kaiser Family Foundation; 2010. July 2010. [Google Scholar]
- 3.Young K, Garfield R, Musumeci M, Clemans-Cope L, Lawton E. Medicaid’s Role for Dual Eligible Beneficiaries Washington, DC: Kaiser Family Foundation; 2013. August 2013. [Google Scholar]
- 4.Grabowski DC. Medicare and Medicaid: conflicting incentives for long-term care. Milbank Q 2007;85(4):579–610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Keohane LM, Zhou Z, Stevenson DG. Aligning Medicaid and Medicare Advantage Managed Care Plans for Dual-Eligible Beneficiaries. Med Care Res Rev 2022;79(2):207–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grabowski DC, Joyce NR, McGuire TG, Frank RG. Passive Enrollment Of Dual-Eligible Beneficiaries Into Medicare And Medicaid Managed Care Has Not Met Expectations. Health Aff (Millwood) 2017;36(5):846–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Keohane LM, Hwang A. Health Affairs Forefront [Internet] Washington, DC: Health Affairs. 2022. [cited 2022]. [Google Scholar]
- 8.Elmaleh-Sachs A, Schneider EC. Strange Bedfellows: Coordinating Medicare and Medicaid to Achieve Cost-Effective Care for Patients with the Greatest Health Needs. J Gen Intern Med 2020;35(12):3671–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chapter 12: Promoting integration in dual-eligible special needs plans Washignton, DC: Medicare Payment Advisory Commission; 2019. [Google Scholar]
- 10.Chapter 2: Integrating Care for Dually Eligible Beneficiaries: Policy Issues and Options Washington, DC: Medicaid and CHIP Payment and Access Commission; 2020. June 2020. [Google Scholar]
- 11.Donovan S Additional Guidance on CY 2021 Medicare-Medicaid Integration Requirements for Dual Eligible Special Needs Plans (D-SNPs) Baltimore, MD: Centers for Medicare and Medicaid Services; 2020. [Google Scholar]
- 12.Medicare Program; Contract Year 2023 Policy and Technical Changes to the Medicare Advantage and Medicare Prescription Drug Benefit Programs. Federal register 2022;87(89):27704–6. [Google Scholar]
- 13.Medicare Advantage Special Needs Plans: CMS Should Improve Information Available about Dual-Eligible Plans’ Performance Washington, DC: US Government Accountability Office; 2012. September 2012. [Google Scholar]
- 14.Chapter 6: Improving Integration for Dually Eligible Beneficiaries: Strategies for State Contracts with Dual Eligible Special Needs Plans Washington, DC: Medicaid and CHIP Payment and Access Commission; 2021. June 2021. [Google Scholar]
- 15.Haviland AM, Elliott MN, Klein DJ, Orr N, Hambarsoomian K, Zaslavsky AM. Do dual eligible beneficiaries experience better health care in special needs plans? Health Serv Res 2021;56(3):517–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Feng Z, Wang J, Gadaska A, Knowles M, Haber S, Infber MJ, et al. Comparing Outcomes for Dual Eligible Beneficiaries in Integrated Care: Final Report Washington, DC; 2021. September 2021. [Google Scholar]
- 17.Medicare Advantage: Special Needs Plans Were More Profitable, on Average, than Plans Available to All Beneficiaries in 2011 Washington, DC: US Government Accountability Office; 2013. December 19, 2013. [Google Scholar]
- 18.2018 Medicare Current Beneficiary Survey Data User’s Guide: Survey File Centers for Medicare and Medicaid Services; 2020. September 24, 2020.
- 19. To access the appendix, click on the Details tab of the article online.
- 20.Chapter 4: Establishing a Unified Program for Dually Eligible Beneficiaries: Design Considerations Washington, DC: Medicaid and CHIP Payment and Access Commission; 2021. March 2021. [Google Scholar]
- 21.Kim H, Charlesworth CJ, McConnell KJ, Valentine JB, Grabowski DC. Comparing Care for Dual-Eligibles Across Coverage Models: Empirical Evidence From Oregon. Med Care Res Rev 2019;76(5):661–77. [DOI] [PubMed] [Google Scholar]
- 22.Anderson WL, Long SK, Feng Z. Effects of Integrating Care for Medicare-Medicaid Dually Eligible Seniors in Minnesota. J Aging Soc Policy 2020;32(1):31–54. [DOI] [PubMed] [Google Scholar]
- 23.Damberg CL, Elliott MN. Opportunities to Address Health Disparities in Performance-Based Accountability and Payment Programs. JAMA Health Forum 2021;2(6):e211143-e. [DOI] [PubMed] [Google Scholar]
- 24.Stratified Reporting Baltimore, MD: Centers for Medicare and Medicaid Services, Office of Minority Health; 2022. [Available from: https://www.cms.gov/About-CMS/Agency-Information/OMH/research-and-data/statistics-and-data/stratified-reporting.
- 25.Meyers DJ, Rahman M, Mor V, Wilson IB, Trivedi AN. Association of Medicare Advantage Star Ratings With Racial, Ethnic, and Socioeconomic Disparities in Quality of Care. JAMA Health Forum 2021;2(6):e210793-e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Agniel D, Martino SC, Burkhart Q, Hambarsoomian K, Orr N, Beckett MK, et al. Incentivizing Excellent Care to At-Risk Groups with a Health Equity Summary Score. J Gen Intern Med 2021;36(7):1847–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


