Abstract
Liver metabolism is strongly linked to bone metabolism, and a significant correlation between nonalcoholic fatty liver disease (NAFLD) and bone mineral density (BMD) in adults has been demonstrated. However, the current relationship between NAFLD and BMD in the adolescent population remains controversial. The purpose of this study was to investigate the specific relationship between NAFLD and BMD in adolescents aged 12 to 19 years in the United States.
The quantitative relationship between NAFLD and total BMD was investigated using multivariate logistic regression and smoothed fitted curve curves based on multiperspective data from the National Health and Nutrition Examination Survey (NHANES).
A total of 740 adolescents were included in this study after excluding unusable samples. The results showed that NAFLD was positively associated with total BMD in adolescents. The results of the subgroup analysis showed that this positive association was mainly found in boys, whites and blacks. The association was not significant in girls, Mexican Americans and other racial groups.
Among US adolescents, there was a significant positive association between NAFLD and total BMD, and this relationship varied by gender and race.
Keywords: adolescents, bone mineral density, cross-sectional study, NAFLD
1. Introduction
Osteoporosis is a long-term disease marked by a decrease in bone mineral density (BMD) that affects groups of all ages. Childhood and adolescence are the periods of peak bone development, with most people reaching peak bone mass(PBM) in late adolescence.[1,2] Findings suggest that elevating a small amount of PBM throughout childhood and adolescence can play a large role in the prevention of osteoporosis.[3] Therefore, focusing on and promoting the accumulation of PBM at an early age is twice as effective in preventing osteoporosis and fractures in adulthood and old age.[4] Risk factors for bone metabolism in adolescents have received increasing attention from researchers in recent years, and a number of biomarkers and chronic diseases have been shown to be significantly associated with BMD.[5–7]
Nonalcoholic fatty liver disease (NAFLD) is the most common chronic liver disease and one of the most prevalent chronic diseases, posing a significant global public health burden. More than a quarter of the population in both the United States and Asia now has NAFLD.[8,9] In addition, the prevalence of NAFLD in adolescents has climbed with the global increase in childhood obesity rates.[10]
Although studies have investigated the relationship between NAFLD and BMD in the past,[11,12] however, most have focused on adult populations. Research on the relationship between NAFLD and BMD in adolescents remains scarce and controversial, and more importantly, there is a lack of gender- and race-specific correlations. Therefore, we investigated the association between NAFLD and total BMD in adolescents aged 12 to 19 from the National Health and Nutrition Examination Survey (NHANES).
2. Materials and Methods
2.1 Study population
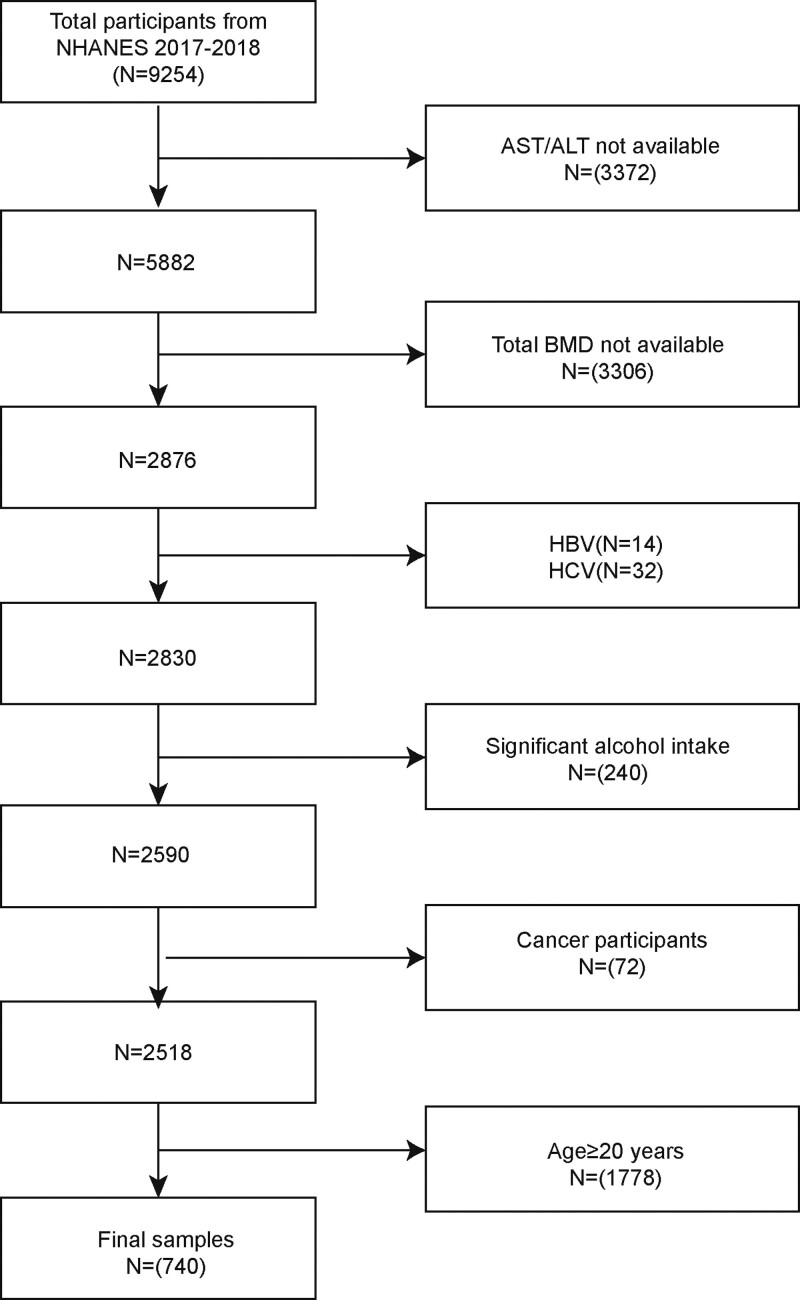
The NHANES is an ongoing cross-sectional survey in the United States with a very wide variety of non-multi-angle data. The research ethics review committee of the National Center for Health Statistics authorized the study protocol. Written consent was provided by all subjects or guardians of subjects at the time of recruitment. We excluded 3372 individuals with missing aspartate aminotransferase (AST) and alanine aminotransferase (ALT) data, 72 with a cancer diagnosis, 3006 with missing BMD data, 240 participants with heavy alcohol consumption, 1778 individuals older than 19 years, and 46 individuals with hepatitis B or C. Finally, 740 adolescents were included in this study (Fig. 1).
Figure 1.
Flow chart of participants selection. BMD = bone mineral density, CAP = controlled attenuation parameter, HBV = hepatitis B virus, HCV = hepatitis C virus, NHANES = National Health and Nutrition Examination Survey.
2.2 Study variables
The activity of AST is measured by the interaction of alpha-ketoglutarate with L-aspartate to produce L-glutamate and oxaloacetate. Oxaloacetate is converted to malate by malate dehydrogenase (MDH), and NADH is oxidized to NAD. The reduction in NADH absorbance, measured at 340 nm (secondary wavelength = 700 nm), is related to serum AST activity. The interaction of alpha-ketoglutarate with L-alanine to generate L-glutamate and pyruvate is catalyzed by the enzyme ALT. Pyruvate is converted to lactate by LDH, while NADH is transformed to NAD by LDH. The reduction in NADH absorbance (measured at 340 nm; secondary wavelength is 700 nm) is proportional to ALT serum activity. Children and adolescents in WHO standards (2007) with AST/ALT ratio are less than 1 and ultrasound evidence of hepatic steatosis.[13] Dual-energy X-ray absorptiometry was performed to assess total BMD. Covariates includes age, serum iron, gender, waist circumference, glycated hemoglobin, race, poverty to income ratio, total cholesterol, low-density lipoprotein-cholesterol, ALT, diabetes status, alkaline phosphatase (ALP), high-density lipoprotein-cholesterol, gamma-glutamyl transferase (GGT), body mass index, AST, controlled attenuation parameter (CAP), and liver stiffness measure (LSM) were all covariates in this study.
2.3 Statistical analysis
All analyses were performed using R (version 4.2) or Empowerstats (version 4.1). All data were analyzed statistically after weighting according to the NCHS analysis guidelines. We investigated the linear and nonlinear relationships between NAFLD and BMD mainly using multiple logistic regression analysis and smoothed fitted curves. Subgroup analysis was used to investigate whether the above relationships remained consistent across different groups.
3. Results
3.1 Baseline characteristics
There were 740 adolescent participants in this study, including 597 non-NAFLD participants and 143 NAFLD participants. NAFLD adolescents showed significant differences from non-NAFLD adolescents in all covariates except in glycosylated hemoglobin, low-density lipoprotein, serum iron, ALP, and diabetes status in both groups. In contrast, NAFLD participants were more likely to be boys and Mexican Americans. Adolescents with NAFLD had higher bone mineral density, as well as higher body mass index (BMI) and waist circumference. Adolescents with NAFLD also tended to have a higher socioeconomic status (Table 1).
Table 1.
Characteristics of the participants.
| NAFLD (n = 143) | Non-NAFLD (n = 597) | P value | |
|---|---|---|---|
| Age (yr) | 16.323 ± 2.330 | 15.425 ± 2.242 | .00006 |
| Gender (%) | .00002 | ||
| Male | 68.728 | 47.529 | |
| Female | 31.272 | 52.471 | |
| Race/ethnicity (%) | .00373 | ||
| Non-Hispanic White | 45.080 | 54.667 | |
| Non-Hispanic Black | 6.234 | 10.647 | |
| Mexican American | 27.865 | 15.186 | |
| Other race | 20.821 | 19.499 | |
| Income to poverty ratio | 1.930 ± 1.509 | 2.640 ± 1.651 | .00005 |
| Diabetes (%) | .67200 | ||
| Yes | 1.853 | 0.953 | |
| No | 98.147 | 99.047 | |
| BMI (kg/m2) | 28.348 ± 6.620 | 22.889 ± 5.090 | <.00001 |
| Waist circumference (cm) | 94.151 ± 17.205 | 79.075 ± 12.212 | <.00001 |
| Laboratory features | |||
| HbA1c (%) | 5.239 ± 0.294 | 5.247 ± 0.391 | .82971 |
| Total cholesterol (mmol/L) | 4.247 ± 0.820 | 4.022 ± 0.738 | .00252 |
| LDL-cholesterol (mmol/L) | 2.441 ± 0.688 | 2.277 ± 0.625 | .06438 |
| HDL-cholesterol (mmol/L) | 1.225 ± 0.254 | 1.385 ± 0.300 | <.00001 |
| ALT (IU/L) | 34.641 ± 36.163 | 13.219 ± 5.419 | <.00001 |
| AST (IU/L) | 24.701 ± 16.826 | 19.729 ± 7.180 | <.00001 |
| ALP (IU/L) | 135.599 ± 91.895 | 153.442 ± 103.612 | .07592 |
| GGT (IU/L) | 24.028 ± 12.986 | 12.915 ± 5.997 | <.00001 |
| Serum iron (µmol/L) | 16.927 ± 7.778 | 16.451 ± 7.201 | .50970 |
| Total bone mineral density (µmol/L) | 1.073 ± 0.124 | 1.025 ± 0.120 | .00252 |
| CAP (dB/m) | 254.139 ± 69.290 | 210.251 ± 45.298 | <.00001 |
| LSM (kPa) | 5.487 ± 3.132 | 4.722 ± 1.593 | .00007 |
Mean + SD for continuous variables: P value was calculated by weighted linear regression model.
% for categorical variables: P value was calculated by weighted chi-square test.
ALP = alkaline phosphatase, ALT = alanine transaminase, AST = aspartate aminotransferase, BMI = body mass index, CAP = controlled attenuation parameter, GGT = gamma-glutamyl transferase, HbA1c (%) = glycated hemoglobin, HDL = high-density lipoprotein, LDL = low-density lipoprotein, LSM = liver stiffness measure, NAFLD = nonalcoholic fatty liver disease.
3.2 Association between NAFLD and total BMD
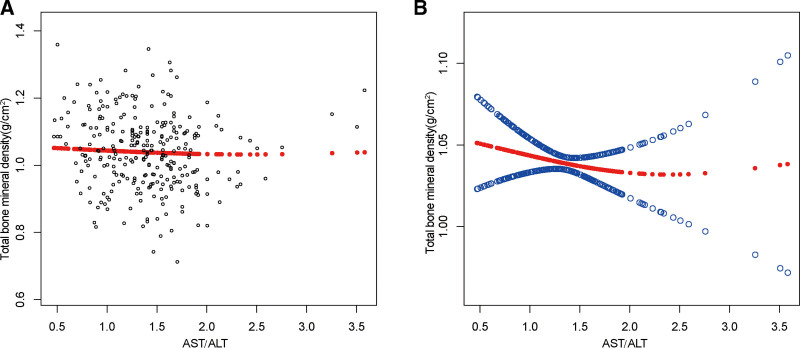
The results of multivariate regression analysis showed that NAFLD showed a strong independent positive correlation with total BMD in the unadjusted model (0.048 [0.025, 0.071]). This positive correlation was maintained when adjusting for covariates, as in the partially adjusted model (0.016 [–0.003, 0.035]) and the fully adjusted model (0.012 [-0.015, 0.039]). In addition to this, we further used smoothed curve fitting to examine the nonlinear relationship between NAFLD and total BMD, and the results verified a positive correlation between NAFLD and total BMD (Fig. 2).
Figure 2.
The association between NAFLD and total bone mineral density. (a) Each black point represents a sample. (b) The solid red line represents the smooth curve fit between variables. Blue bands represent the 95% of confidence interval from the fit. Age, gender, race, body mass index, poverty to income ratio, diabetes status, waist circumference, HbA1c (%), total cholesterol, LDL-cholesterol, HDL-cholesterol, ALT, ALP, GGT, AST, serum iron, total bone mineral density, CAP and LSM were adjusted. ALP = alkaline phosphatase, ALT = alanine aminotransferase, AST = aspartate aminotransferase, CAP = controlled attenuation parameter, GGT = gamma-glutamyl transferase, HbA1c (%) = glycated hemoglobin, HDL = high-density lipoprotein, LDL = low-density lipoprotein, LSM = liver stiffness measure. NAFLD = nonalcoholic fatty liver disease.
3.3. Subgroup analysis
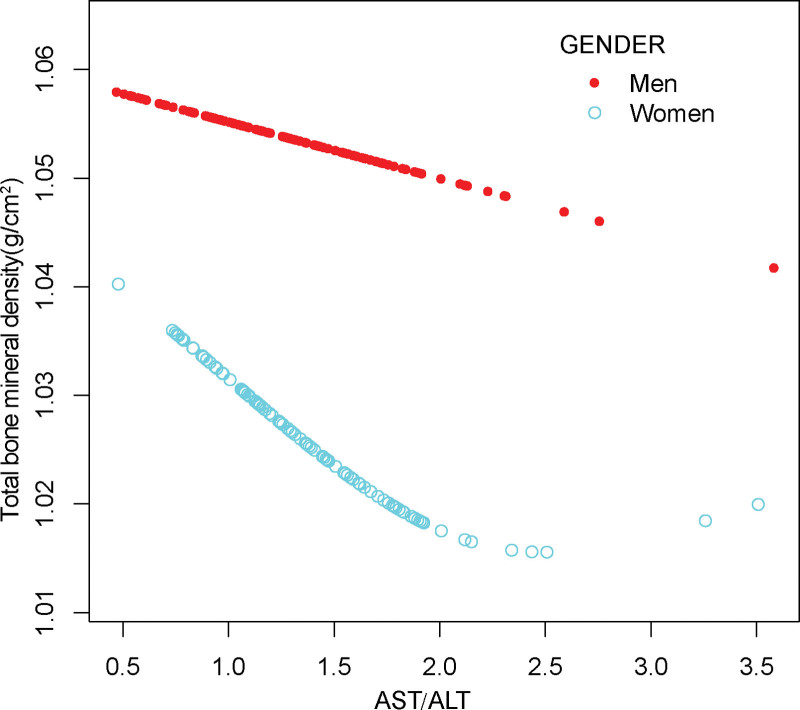
To further verify whether the relationship between NAFLD and total BMD differs across different groups of US adolescents, we conducted subgroup analyses by gender and race. We found that this positive association remained significant only in boys, white and black races, but not in girls, Mexican Americans and other racial groups.
For boys, NAFLD exhibited a significant positive association with BMD in unadjusted Model (0.074 [0.029, 0.119]), but the association became insignificant in Model 2 (0.042 [0.006, 0.078]) and Model 3 (0.007 [–0.036, 0.049]) when covariates were adjusted. In contrast, the relationship between NAFLD and BMD became negatively correlated when all variables were adjusted for girls. In addition, the nonlinear relationship was characterized by smooth curve fittings and generalized additive models (Table 2 and Fig. 3).
Table 2.
Association between NAFLD and total bone mineral density (g/cm2) stratified by gender.
| Model 1: β (95% CI, P) | Model 2: β (95% CI, P) | Model 3: β (95% CI, P) | |
|---|---|---|---|
| Non-NAFLD | Reference | Reference | Reference |
| NAFLD | 0.048 (0.025, 0.071) .00006 |
0.016 (–0.003, 0.035) .10899 |
0.012 (–0.015, 0.039) .39327 |
| Males | |||
| Non-NAFLD | Reference | Reference | Reference |
| NAFLD | 0.062 (0.030, 0.095) .00021 |
0.008 (–0.017, 0.033) .51872 |
0.011 (–0.028, 0.049) .59332 |
| Females | |||
| Non-NAFLD | Reference | Reference | Reference |
| NAFLD | 0.011 (–0.023, 0.046) .51859 |
0.008 (–0.022, 0.039) .58534 |
–0.021 (–0.068, 0.026) .38129 |
HbA1c = glycated hemoglobin, HDL = high-density lipoprotein, LDL = low-density lipoprotein, NAFLD = nonalcoholic fatty liver disease.
Model 1: No covariates were adjusted. Model 2: Age, gender, race were adjusted.
Model 3: Age, gender, race, body mass index, poverty to income ratio, diabetes status, waist circumference, HbA1c (%), total cholesterol, LDL-cholesterol, HDL-cholesterol, ALT, ALP, GGT, AST, serum iron, total bone mineral density, CAP and LSM were adjusted. In the subgroup analysis stratified by gender or race, the model is not adjusted for the stratification variable itself.
Figure 3.
The association between NAFLD and total bone mineral density stratified by gender. Age, gender, race, body mass index, poverty to income ratio, diabetes status, waist circumference, HbA1c (%), total cholesterol, LDL-cholesterol, HDL-cholesterol, ALT, ALP, GGT, AST, serum iron, total bone mineral density, CAP and LSM were adjusted. ALP = alkaline phosphatase, ALT = alanine aminotransferase, AST = aspartate aminotransferase, CAP = controlled attenuation parameter, GGT = gamma-glutamyl transferase, HbA1c (%) = glycated hemoglobin, HDL = high-density lipoprotein, LDL = low-density lipoprotein, LSM = liver stiffness measure. NAFLD = nonalcoholic fatty liver disease.
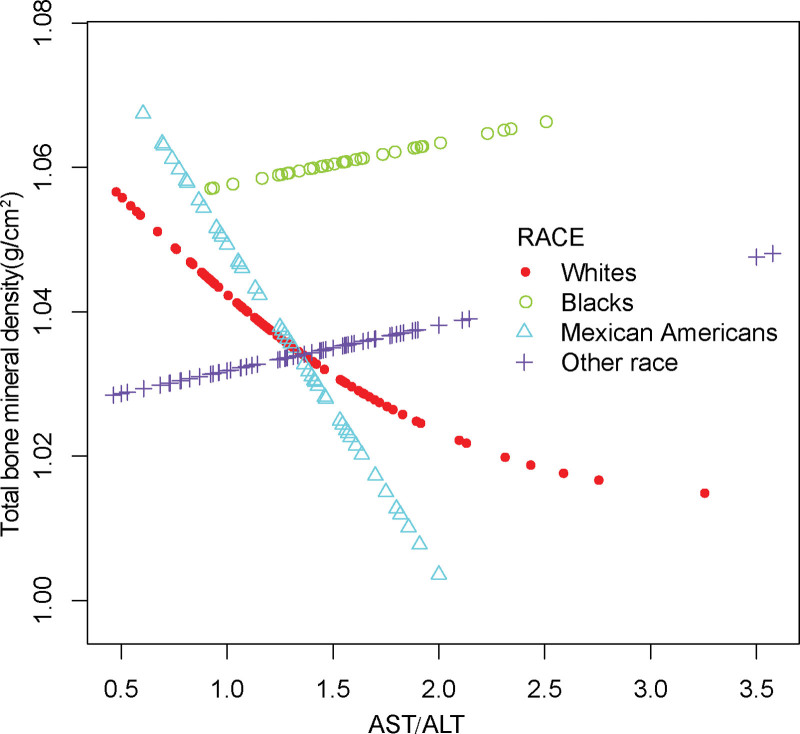
For whites, the positive association was in Model 1 (0.074 [0.029, 0.119]) and maintained in Model 2 (0.042 [0.006, 0.078]), but not in Model 3 (0.007 [–0.036, 0.049)]. For blacks, the relationship as same as males, only existed in unadjusted Model (0.104 [0.036, 0.172]) but not in Model 2 (0.039 [–0.018, 0.097]) and Model 3 (0.063 [–0.055, 0.180]). Of note, among Mexican Americans and other race, the relationship between NALFD and BMD became reversed when adjusted for age, sex, race, or all covariates. Details of the racial subgroup analysis, smoothed fit curves and generalized weighted models are shown in Table 3 and Figure 4.
Table 3.
Association between NAFLD and total bone mineral density (g/cm2) stratified by race.
| Race/ethnicity (%) | Model 1: β (95% CI), P | Model 2: β (95% CI), P | Model 3: β (95% CI), P |
|---|---|---|---|
| Non-Hispanic White | |||
| Non-NAFLD | Reference | Reference | Reference |
| NAFLD | 0.074 (0.029, 0.119) .00137 | 0.042 (0.006, 0.078) .02410 | 0.007 (–0.036, 0.049) .75493 |
| Non-Hispanic Black | |||
| Non-NAFLD | Reference | Reference | Reference |
| NAFLD | 0.104 (0.036, 0.172) .00330 | 0.039 (–0.018, 0.097) .18237 | 0.063 (–0.055, 0.180) .30790 |
| Mexican American | |||
| Non-NAFLD | Reference | Reference | Reference |
| NAFLD | 0.014 (–0.029, 0.056) .53772 | –0.017 (–0.052, 0.017) .33073 | –0.081 (–0.164, 0.001) .06098 |
| Other race | |||
| Non-NAFLD | Reference | Reference | Reference |
| NAFLD | 0.023 (–0.014, 0.060) .22227 | –0.008 (–0.040, 0.025) .64476 | –0.013 (–0.049, 0.023) .47906 |
Model 1: No covariates were adjusted. Model 2: Age, gender, race were adjusted. Model 3: Age, gender, race, body mass index, poverty to income ratio, diabetes status, waist circumference, HbA1c (%), total cholesterol, LDL-cholesterol, HDL-cholesterol, ALT, ALP, GGT, AST, serum iron, total bone mineral density, CAP and LSM were adjusted. In the subgroup analysis stratified by gender or race, the model is not adjusted for the stratification variable itself.
NAFLD = nonalcoholic fatty liver disease.
Figure 4.
The association between NAFLD and total bone mineral density stratified by race. Age, gender, race, body mass index, poverty to income ratio, diabetes status, waist circumference, HbA1c (%), total cholesterol, LDL-cholesterol, HDL-cholesterol, ALT, ALP, GGT, AST, serum iron, total bone mineral density, CAP and LSM were adjusted. ALP = alkaline phosphatase, ALT = alanine aminotransferase, AST = aspartate aminotransferase, CAP = controlled attenuation parameter, GGT = gamma-glutamyl transferase, HbA1c (%) = glycated hemoglobin, HDL = high-density lipoprotein, LDL = low-density lipoprotein, LSM = liver stiffness measure. NAFLD = nonalcoholic fatty liver disease.
4. Discussion
In the present study, our results suggest a positive association between NAFLD and middle BMD in adolescents. Not only that, we further investigated potential gender and racial differences using subgroup analysis, and the results demonstrated that this positive association was significant in boys, White and Black groups, and not significant in girls, Mexican Americans and other races.
Past epidemiological studies on the relationship between NAFLD and BMD have focused on adult populations, and observational studies with adolescents are still very few and controversial. There was notable change in BMD among adolescents with NAFLD and controls, according to a recent meta-analysis of 6 cross-sectional studies.[14] However, in another study, the researchers concluded that NAFLD was only associated with osteoporotic fractures but not with a significant reduction in BMD.[15] Two large cohort studies from China also concluded a significant association between NAFLD and osteoporotic fractures.[16] In addition, several epidemiological studies from Asia have shown significant gender differences in the relationship between NAFLD and BMD, with greater variation in BMD especially in the menopausal female population.[17–21] Our findings also confirm this gender difference. Gender differences have also been repeatedly mentioned in past studies on bone metabolism, especially in older women.[22,23] In addition, our findings suggest that there are racial differences in the relationship between NAFLD and BMD in adolescents. However, after reviewing the past literature, we found that the underlying mechanisms regarding this condition are currently unexplained.
The mechanisms behind the relationship between NAFLD and BMD are controversial. Many researchers have elaborated on the possible reasons for this relationship. First, it has been suggested that insulin resistance is an important mediator of this relationship and that insulin resistance can affect changes in a variety of inflammatory metabolic factors and bone metabolites, which can further lead to accelerated or slowed bone loss.[24,25] Other studies have suggested that the relationship between NAFLD and BMD is mainly mediated by obesity and body fat content,[26] a higher BMI may help to prevent bone loss by increasing mechanical loading. An epidemiological study of the relationship between diabetes and BMD illustrates another possible reason,[27] some researchers have argued that the effects of multiple chronic diseases on the same individual are diverse and complex, and that considering the effects of only one of these diseases on bone metabolism would be very prone to bias in the observations. This bias is further increased when the results are applied to different genders or races, as evidenced by the study from China.[19,20] The most predominant view regarding gender differences in the relationship between NAFLD and BMD is the significant difference in sex hormones in different sex and age groups. In postmenopausal women, estrogen deficiency is considered a major cause of osteoporosis and fractures.[28,29] Estrogen can affect the activity of osteoblasts and osteoclasts by a variety of pathways, thereby affecting the conduct of bone metabolism.[30,31] Indeed, not only does estrogen have multiple effects on bone metabolism, but there is also a strong link between estrogen and disease progression in NAFLD. This also prompts us to fully consider the gender, age, race, and individual differences of the study population in epidemiological studies.
Several strengths exist in our study. Since current studies on the association between NAFLD and BMD have focused on adults, the present study explored the relationship between NAFLD and BMD in adolescents. In addition, our findings were consistent with the inclusion of ethnically diverse adolescents and due to the representative sampling characteristics of NHANES, we investigated potential gender and ethnic differences in the association between NAFLD and BMD using weighted data. However, there are limitations to our study as well. First, our retrospective study design makes it hard to conclude a causal association between NAFLD and total BMD in adolescents. To explain the mechanisms and potential gender and ethnic differences in the relationship between NAFLD and BMD in adolescents, additional large-sample, multilevel observational studies are needed to confirm this. Second, NAFLD is diagnosed based on the AST/ALT ratio, which may be biased for estimating the prevalence of the disease. Therefore, alternative validation of the involvement of NAFLD in bone metabolism is necessary to avoid data bias.
5. Conclusion
Our findings suggest a significant positive correlation between NAFLD and total BMD in adolescents. There were gender differences and racial differences in this relationship.
Acknowledgements
We thank the National Health and Nutrition Examination Surveys for providing the data.
Authors contributions
Conceptualization: Ruijie Xie, Ya Zhang.
Data curation: Ruijie Xie, Ya Zhang.
Funding acquisition: Mingjiang Liu.
Investigation: Ruijie Xie, Mingjiang Liu.
Methodology: Ruijie Xie, Ya Zhang, Mingjiang Liu.
Software: Ruijie Xie, Ya Zhang.
Validation: Ruijie Xie, Mingjiang Liu.
Visualization: Ruijie Xie.
Writing – original draft: Ruijie Xie.
Writing – review & editing: Tao Yan, Xiongjie Huang, Songlin Xie, Changxiong Liu, Mingjiang Liu.
Abbreviations:
- ALT =
- alanine aminotransferase
- AST =
- aspartate aminotransferase
- BMD =
- bone mineral density
- CAP =
- controlled attenuation parameter
- NAFLD =
- nonalcoholic fatty liver disease
- NHANES =
- National Health and Nutrition Examination Survey
The datasets generated during and/or analyzed during the current study are publicly available.
RX, YZ, and TY contributed equally to this work.
The studies involving human participants were reviewed and approved by NCHS Ethics Review Board. The patients/participants provided their written informed consent to participate in this study.
This study Funded by the Scientific Research Project of Hunan Health and Family Planning Commission to ML(A2017018).
The authors have no conflicts of interest to disclose.The survey data are publicly available on the internet for data users and researchers throughout the world (www.cdc.gov/nchs/nhanes/).
How to cite this article: Xie R, Zhang Y, Yan T, Huang X, Xie S, Liu C, Liu M. Relationship between nonalcoholic fatty liver disease and bone mineral density in adolescents. Medicine 2022;101:41(e31164).
Contributor Information
Ruijie Xie, Email: 71008671@qq.com.
Ya Zhang, Email: 15575625260@163.com.
Tao Yan, Email: 307343213@qq.com.
Xiongjie Huang, Email: mymail801020@sina.com.
Songlin Xie, Email: 71008671@qq.com.
Changxiong Liu, Email: usclmj@163.com.
References
- [1].Baxter-Jones A, Faulkner R, Forwood M, et al. Boe mass. J Bone Min Res. 2011;26:1729–39. [DOI] [PubMed] [Google Scholar]
- [2].Pan K, Zhang C, Yao X. et al. Association between dietary calcium intake and BMD in children and adolescents. Endocrine Connect. 2020;9:194–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].van der Sluis I, de Muinck Keizer-Schrama S. Osteoporosis in childhood: bone density of children in health and disease. J Pediatr Endocrinol Metab. 2001;14:817–32. [DOI] [PubMed] [Google Scholar]
- [4].Pan K, Yao X, Liu M, et al. Association of serum uric acid status with bone mineral density in adolescents aged 12–19 years. Front Med. 2020;7:255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Xie R, Huang X, Liu Q, et al. Positive association between high-density lipoprotein cholesterol and bone mineral density in U.S. adults: the NHANES 2011–2018. J Orthop Surg Res. 2022;17:92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Xie R, Huang X, Zhang Y, et al. High low-density lipoprotein cholesterol levels are associated with osteoporosis among adults 20–59 years of age. Int J Gen Med. 2022;15:2261–2270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Ouyang Y, Quan Y, Guo C, et al. Saturation effect of body mass index on bone mineral density in adolescents of different ages: a population-based study. Front Endocrinol (Lausanne). 2022;13:922903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Fan J, Kim S, Wong V, New trends on obesity and NAFLD in Asia. J Hepatol. 2017;67:862–873 [DOI] [PubMed] [Google Scholar]
- [9].Powell EE, Wong VW, Rinella M, Non-alcoholic fatty liver disease. Lancet. 2021;397:2212–2224 [DOI] [PubMed] [Google Scholar]
- [10].Farrell G, Wong V, Chitturi S. NAFLD in Asia – as common and important as in the West. Nat Rev Gastroenterol Hepatol. 2013;10:307–18. [DOI] [PubMed] [Google Scholar]
- [11].Xie R, Liu M, Relationship between non-alcoholic fatty liver disease and degree of hepatic steatosis and bone mineral density. Front Endocrinol. 2022;13:85110–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Li H, Luo H, Zhang Y, et al. Association of metabolic dysfunction-associated fatty liver disease and liver stiffness with bone mineral density in american adults. Front Endocrinol (Lausanne). 2022;13: 891382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Rodrigo T, Samaranayake D, Nimali Seneviratne S, et al. Effects of probiotics combined with dietary and lifestyle modification on clinical, biochemical, and radiological parameters in obese children with NASH/NAFLD: a randomized clinical trial. Clin Exp Pediatr. 2021;65:304–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Sun Y, Dai W, Liang Y, et al. Relationship between nonalcoholic fatty liver disease and bone mineral density in adolescents with obesity: a meta-analysis. Diabet Metab Syndr Obes. 2019;12:199–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Mantovani A, Gatti D, Zoppini G, et al. Association between nonalcoholic fatty liver disease and reduced bone mineral density in children: a meta-analysis. Hepatology (Baltimore, Md.). 2019;70:812–23. [DOI] [PubMed] [Google Scholar]
- [16].Chen H, Yang H, Hsueh K, et al. Increased risk of osteoporosis in patients with nonalcoholic fatty liver disease: a population-based retrospective cohort study. Medicine. 2018;97:e12835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Ahn S, Seo D, Kim S, et al. The relationship between fatty liver index and bone mineral density in Koreans: KNHANES 2010–2011. Osteoporosis Int. 2018;29:181–190. [DOI] [PubMed] [Google Scholar]
- [18].Chen D, Xu Q, Wu X, et al. The combined effect of nonalcoholic fatty liver disease and metabolic syndrome on osteoporosis in postmenopausal females in Eastern China. Int J Endocrinol. 2018;2018:2314769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Cui R, Sheng H, Rui X, et al. Low bone mineral density in Chinese adults with nonalcoholic fatty liver disease. Int J Endocrinol. 2013;2013:396545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Wang Y, Wen G, Zhou R, et al. Association of nonalcoholic fatty liver disease with osteoporotic fractures: a cross-sectional retrospective study of Chinese individuals. Front Endocrinol. 2018;9:408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Yang H, Shim S, Ma B, et al. Association of nonalcoholic fatty liver disease with bone mineral density and serum osteocalcin levels in Korean men. Eur J Gastroenterol Hepatol. 2016;28:338–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Filip R, Radzki R, Bieńko M, Novel insights into the relationship between nonalcoholic fatty liver disease and osteoporosis. Clin Interv Aging. 2018;13:1879–1891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Ballestri S, Nascimbeni F, Baldelli E, et al. NAFLD as a sexual dimorphic disease: role of gender and reproductive status in the development and progression of nonalcoholic fatty liver disease and inherent cardiovascular risk. Adv Therapy. 2017;34:1291–1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Yilmaz Y, Review article: non-alcoholic fatty liver disease and osteoporosis – clinical and molecular crosstalk. Aliment Pharmacol Therap. 2012;36:345–52. [DOI] [PubMed] [Google Scholar]
- [25].Guañabens N, Parés A, Osteoporosis in chronic liver disease. Liver Int. 2018;38:776–785 [DOI] [PubMed] [Google Scholar]
- [26].Younossi Z, Anstee Q, Marietti M, et al. Global burden of NAFLD and NASH: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol. 2018;15:11–20. [DOI] [PubMed] [Google Scholar]
- [27].O’Keefe J, Bhatti S, Patil H, et al. Effects of habitual coffee consumption on cardiometabolic disease, cardiovascular health, and all-cause mortality. J Am Coll Cardiol. 2013;62:1043–51. [DOI] [PubMed] [Google Scholar]
- [28].Moon S, Lee Y, Kim S, Association of nonalcoholic fatty liver disease with low bone mass in postmenopausal women. Endocrine. 2012;42:423–9. [DOI] [PubMed] [Google Scholar]
- [29].Xia M, Lin H, Yan H, et al. The association of liver fat content and serum alanine aminotransferase with bone mineral density in middle-aged and elderly Chinese men and postmenopausal women. J Transl Med. 2016;14:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Melville K, Kelly N, Khan S, et al. Female mice lacking estrogen receptor-alpha in osteoblasts have compromised bone mass and strength. J Bone Min Res. 2014;29:370–9. [DOI] [PubMed] [Google Scholar]
- [31].Kodama I, Niida S, Sanada M, et al. Estrogen regulates the production of VEGF for osteoclast formation and activity in op/op mice. J Bone Min Res. 2004;19:200–6. [DOI] [PubMed] [Google Scholar]