OBJECTIVES:
The optimal staffing model for physicians in the ICU is unknown. Patient-to-intensivist ratios may offer a simple measure of workload and be associated with patient mortality and physician burnout. To evaluate the association of physician workload, as measured by the patient-to-intensivist ratio, with physician burnout and patient mortality.
DESIGN:
Cross-sectional observational study.
SETTING:
Fourteen academic centers in the United States from August 2020 to July 2021.
SUBJECTS:
We enrolled ICU physicians and collected data on adult ICU patients under the physician’s care on the single physician-selected study day for each physician.
MEASUREMENTS and MAIN RESULTS:
The primary exposure was workload (self-reported number of patients’ physician was responsible for) modeled as high (>14 patients) and low (≤14 patients). The primary outcome was burnout, measured by the Well-Being Index. The secondary outcome measure was 28-day patient mortality. We calculated odds ratio for burnout and patient outcomes using a multivariable logistic regression model and a binomial mixed effects model, respectively. We enrolled 122 physicians from 62 ICUs. The median patient-to-intensivist ratio was 12 (interquartile range, 10–14), and the overall prevalence of burnout was 26.4% (n = 32). Intensivist workload was not independently associated with burnout (adjusted odds ratio, 0.74; 95% CI, 0.24–2.23). Of 1,322 patients, 679 (52%) were discharged alive from the hospital, 257 (19%) remained hospitalized, and 347 (26%) were deceased by day 28; 28-day outcomes were unknown for 39 of patients (3%). Intensivist workload was not independently associated with 28-day patient mortality (adjusted odds ratio, 1.33; 95% CI, 0.92–1.91).
CONCLUSIONS:
In our cohort, approximately one in four physicians experienced burnout on the study day. There was no relationship be- tween workload as measured by patient-to-intensivist ratio and burnout. Factors other than the number of patients may be important drivers of burnout among ICU physicians.
Keywords: burnout, intensive care unit, mortality, patient-to-intensivist ratio, workforce, workload
Currently, ICU staffing models are varied nationally (1), and prior studies show inconsistent associations of staffing models with patient outcomes (2–5). One aspect of staffing is the number of patients a physician cares for or the patient-to-intensivist ratio, which has been used as an objective measure of workload and staffing in the ICU. Studies suggest that the relationship between patient-to-intensivist ratio is not linear (6, 7), but there is likely a minimum or threshold volume of work, or activity, needed for best patient outcomes (8, 9).
The impact of ICU work and staffing on physician outcomes is less well understood but important. As more physicians leave the profession due to increased moral distress and burnout (10–12), it is important to understand the relationship between ICU work and physician outcomes. Burnout is associated with decreased work performance (13, 14), a desire to leave the ICU (15), and a reduction in clinical hours (16). Small studies have suggested a relationship between physician workload in the ICU and burnout (17, 18). A consensus statement on ICU staffing by the Society of Critical Care Medicine (SCCM) suggests that patient-to-intensivist ratios greater than 14 to 1 may be unfavorable for the physician (19). However, guidelines do not offer strong evidence nor recommendations for measuring physician workload in the ICU (19, 20).
We conducted this study to examine if there was an independent association between the number of patients a physician cares for and burnout among intensivists across multiple academic ICUs in the United States.
MATERIALS AND METHODS
Study Design
We conducted a cross-sectional study across 62 ICUs in 14 academic centers in the United States recruited through the Discovery Network of SCCM (21) from August 2020 through July 2021. Any physician serving as the intensivist for an adult ICU was eligible for inclusion. Sites chose ICUs and study days based on ICU directors’ guidance. Physicians could choose when, on a day during their ICU rotation, to complete study measures. Up to three different physicians working on separate days in the same ICU were eligible, and multiple ICUs within a site were included. The study was granted approval by the institutional review boards (IRBs) of all participating sites (Emory University IRB Study 00000017, May 15, 2020). Informed consent for physicians was implied by completion of study surveys, and study procedures followed were in accordance with institutional ethical standards and the Helsinki Declaration of 1975.
Study Measures and Data Collection
Our primary exposure of interest was physician workload defined as the self-reported number of ICU patients the physician was responsible for on the study day (19). Because there exist no validated measures or definition of ICU workload (1), we also surveyed physicians on other aspects of ICU work, clinical and nonclinical duties that may influence their time in the ICU, including ICU strain, which can be understood as a mismatch between ICU resource supply and demand (22) (full ICU work physician survey, Supplemental Digital Content - Table 1, http://links.lww.com/CCX/B69).
The primary outcome measure was the number of physicians who had a Well-Being Index (WBI) score greater than or equal to 4 measured using the expanded WBI (Supplemental Digital Content - Table 2, http://links.lww.com/CCX/B69) (23, 24), which we defined as burnout based on previous studies (17, 22). The WBI, which was designed to measured distress in dimensions of burnout, fatigue, quality of life, depression, and anxiety, has been used to measure burnout in ICU physicians (17, 25, 26), and it has been shown to have a high predictive value for burnout (23). The WBI was chosen as it is freely available and requires minimal time to complete.
We collected structural information from each ICU as detailed in Supplemental Digital Content - Table 3 (http://links.lww.com/CCX/B69) and information for all patients under the participating physician’s care on the study day as detailed in Supplemental Digital Content - Table 4 (http://links.lww.com/CCX/B69). Patients were followed for 28-day outcome as a key secondary outcome.
Deidentified study data were collected and managed using Research Electronic Data Capture (27, 28).
Statistical Analysis
Continuous and categorical variables are reported as medians with interquartile ranges (IQRs) and counts with percentages. Workload was modeled as a dichotomous variable of high (>14 patients per physician) or low (≤14 patients per physician) based on the SCCM ICU staffing statement (19). Physician and patient characteristics were compared using Wilcoxon rank-sum test for medians and chi-square test (Fisher exact for counts ≤5) for proportions. For univariate comparison of patient variables between high and low workloads and inclusion of patient variables in the primary endpoint analysis, collected patient data were aggregated by physician. Median values of continuous variables and median percentages of categorical variables were used for univariate and primary endpoint analyses.
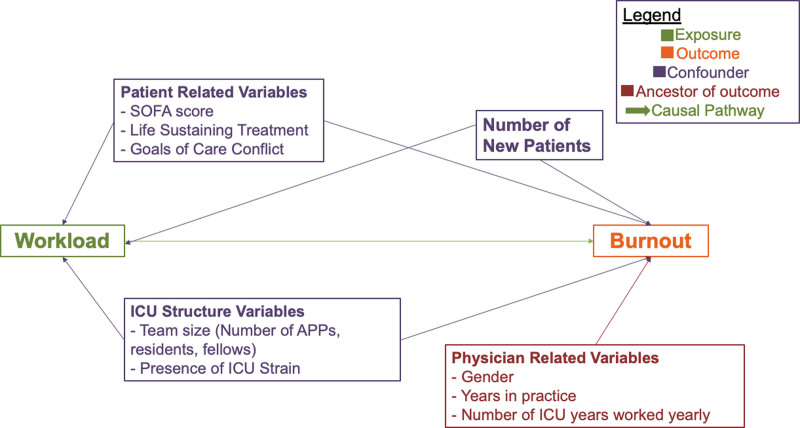
We used a univariate and multivariable logistic regression model to calculate the odds ratio (OR) and 95% CI quantifying the association of physician workload to burnout presence. Covariates for the logistic model were identified a priori using directed acyclic graph theory (Fig. 1) (29), exploring a hypothesized causal relationship between workload and burnout (19, 30). We assessed for statistical interaction between workload and physician gender, years in practice, and ICU weeks worked per year on the association of workload and burnout using the Breslow-Day test.
Figure 1.
Directed acyclic graph (DAG) hypothesizing exposure-outcome relationship for physician workload and burnout. DAG exploring our hypothesized exposure-outcome causal relationship for physician workload (exposure, green) and burnout (outcome, orange). Variables in purple (patient-related variables, ICU structure variables, and number of new patients) represent variables hypothesized and analyzed as confounders (included as covariates in the multivariable model). Physician variables in red (gender, years in practice, and number of weeks worked) represent hypothesized ancestors of burnout and are analyzed as potential interaction variables. Some variables are grouped for figure visual appearance: patient-related variables (Sequential Organ Failure Assessment [SOFA] score, presence of life sustaining treatment, and goals of care conflict), ICU structure variables (team size and presence of ICU strain), and physician related variables (gender, years in practice, and number of ICU weeks worked). APP = advanced practice provider.
We used a binomial mixed-effects logistic regression model to evaluate the association of workload and 28-day patient outcome. The model was restricted to patients with 28-day outcome of alive (includes patients alive and discharged, and patients still hospitalized at day 28) or deceased. Site, ICU, and physician were set as random effects. Fixed effects were determined using directed acyclic graph theory (Supplemental Digital Content - Fig. 1, http://links.lww.com/CCX/B69).
A type I error rate of 0.05 was defined a priori. We designed our study for 80% power to detect a 20% difference in number of physicians with a WBI score greater than or equal to 4 between high and low workload groups, with clustering by site. We conducted one preplanned and three post hoc sensitivity analyses examining quintiles of physician workload and defining workload as: 1) a linear variable of the number of patients physicians had on the study day (31), 2) a linear variable of the number of critical care weeks worked per year, and 3) the day of the ICU service cycle on which the study survey was completed (e.g., day 2 of 7).
Statistical analysis was completed using SAS 9.4 (SAS Institute, Cary, NC) and openepi.com (Copyright 2003, Open Source Epidemiologic Statistics for Public Health, 2008 Andrew G. Dean and Kevin M. Sullivan, Atlanta, GA).
RESULTS
Baseline Physician Characteristics
We enrolled 122 physicians (147 total invited, 83% response rate) across the 14 sites (Table 1; Supplemental Digital Content - Table 5, http://links.lww.com/CCX/B69). Eighty-four (68.9%) physicians were men with a median age of 40.0 years (IQR, 36.0–46.5 yr). Most physicians identified as Caucasian (n = 81 [66.4%]) or Asian (n = 29 [23.8%]). Nearly all (n = 117 [95.9%]) had completed a critical care fellowship as part of their training. Median years in practice was 6.0 (IQR, 3.0–10.0).
Table 1.
Physician Characteristics, by Workload Category
| Characteristic | All Physicians, n = 122 | High Workload,a n = 29 | Low Workload,b n = 93 |
|---|---|---|---|
| Demographics | |||
| Age (yr), median (IQR)c | 40.0 (36.0–46.5) | 40.0 (36.0–47.5) | 40.0 (36.0–46.0) |
| Gender, n (%) | |||
| Female | 37 (30.3) | 8 (27.6) | 29 (31.2) |
| Male | 84 (68.9) | 20 (69.0) | 64 (68.8) |
| Not reported/unknown | 1 (0.8) | 1 (3.4) | 0 (0.0) |
| Marital status, n (%) | |||
| Single | 17 (13.9) | 4 (13.8) | 13 (14.0) |
| Partnered | 104 (85.3) | 25 (86.2) | 79 (84.9) |
| Other/unknown | 1 (0.8) | 0 (0) | 1 (1.1) |
| Race, n (%) | |||
| White | 81 (66.4) | 17 (58.6) | 64 (68.8) |
| Black | 4 (3.3) | 3 (10.3) | 1 (1.1) |
| Asian | 29 (23.8) | 7 (24.1) | 22 (23.7) |
| Other | 6 (4.9) | 2 (6.9) | 4 (4.3) |
| Completed a critical care fellowship, n (%) | 117 (95.9) | 27 (93.1) | 90 (96.8) |
| Residency completed, n (%) | |||
| Anesthesia | 11 (9.0) | 4 (13.8) | 7 (7.5) |
| Emergency medicine | 8 (6.6) | 2 (6.9) | 6 (6.5) |
| Internal medicine | 89 (73.0) | 16 (55.2) | 73 (78.5) |
| Combined medicine and pediatrics | 2 (1.6) | 2 (6.9) | 0 (0.0) |
| Neurology | 7 (5.7) | 2 (6.9) | 5 (5.4) |
| Surgery | 4 (3.3) | 3 (10.3) | 1 (1.1) |
| General clinical work characteristics | |||
| Years in practice, median (IQR) | 6 (3, 10) | 8 (3.75, 12) | 5 (3, 9) |
| Weeks on clinical service (per year), median (IQR) | 22 (13–30) | 22 (19–36) | 20 (13–30) |
| % Clinical time on critical care service, median (IQR) | 75 (50–100) | 50 (35–75) | 80 (50–100) |
| Length of service blocks (d), median (IQR) | 7 (7–7) | 7 (7–7) | 7 (6–7) |
| Work nights in-house, n (%) | 52 (42.6) | 7 (24.1) | 45 (48.4) |
| Non-ICU work during ICU, n (%) | |||
| Non-ICU clinical work (e.g., rapid response, clinic, and surgeries) | 25 (20.5) | 7 (24.1) | 18 (19.4) |
| Nonphysician duties (e.g., pharmacy and respiratory therapy) | 12 (9.8) | 4 (13.8) | 8 (8.6) |
| Research work | 40 (32.8) | 7 (24.1) | 33 (35.5) |
| Administrative duties | 46 (37.7) | 11 (37.9) | 35 (37.6) |
| Teaching | 57 (46.7) | 16 (55.2) | 41 (76.2) |
| Duties are burdensome (yes), n (%) | 39 (68.4) | 10 (76.9) | 29 (65.9) |
| Changes in ICU work related to COVID-19 pandemic | |||
| Cared for COVID-19 patients in unit, n (%) | 92 (75.4) | 25 (86.2) | 67 (72.0) |
| Number of ICU patients cared for, n (%) (compared with prepandemic) | |||
| More patients | 32 (26.4) | 10 (34.5) | 22 (23.9) |
| Same or fewer patients | 89 (73.6) | 19 (65.5) | 70 (76.1) |
| Length of ICU service block, n (%) (compared with prepandemic) | |||
| Increased ICU block | 7 (5.8) | 2 (7.1) | 5 (5.4) |
| Same or decreased ICU block | 113 (94.2) | 26 (92.9) | 87 (94.6) |
| Workload characteristics on study day | |||
| Number of patients on study day, median (IQR) | 12 (10–14) | 18 (17–20) | 11 (8–13) |
| Number of new patients on study day, median (IQR) | 2 (0–3) | 4 (1–4) | 1 (0–3) |
| ICU strain present, n (%) | 49 (40.2) | 16 (55.2) | 33 (35.5) |
| Goals of care conflict with patients/family, n (%) | 77 (63.1) | 21 (72.4) | 56 (60.2) |
| Burnout on study day | |||
| Well-Being Index score, median (IQR) | 2 (0–4) | 2 (0–4) | 2 (0–4) |
| Burnout presentd, n (%) | 32 (26.2) | 8 (27.6) | 24 (25.8) |
IQR = interquartile range.
aHigh workload: > 14 patients per physician.
bLow workload: ≤ 14 patients per physician.
cn missing 10, all other variables with n missing <5.
dBurnout is defined as a score ≥4 on Well-Being Index.
Physician Workload Characteristics
The median number of patients physicians cared for on the study day was 12 (IQR, 10–14), with a median of two new patients (IQR, 0–3) (Table 1). Physicians worked a median of 22 weeks clinical service (IQR, 13–30), with a median of 75.0% (IQR, 50.0–100.0) of clinical time being critical care. Fifty-two (42.6%) physicians reported having nighttime shifts in the ICU as part of their clinical time. Forty-nine (40.2%) physicians identified presence of ICU strain, and 77 (63.1%) physicians reported ongoing goals of care (GOC) conflict with patients and/or families on the study day. Ninety-two (75.4%) physicians cared for patients with COVID-19 during their ICU time, with 32 (26.4%) physicians caring for more patients during COVID-19.
Physicians with high workload had more new patients compared with those with low workload (4 [IQR, 1–4] vs 1 [IQR, 0–3]; p = 0.0001). Although there was no difference in annual clinical weeks between the workload groups (high workload, 22 wk [IQR, 19–36] vs low workload 20 wk [IQR, 13–30]; p = 0.28), physicians with high workload had less critical care time than those with low workload (median % critical care clinical time 50.0% [IQR, 35–75] vs 80.0% [IQR, 50–100]; p = 0.01). More physicians with low workload worked night shifts in the ICU than with high workload (45 [48.4%] vs 7 [24.1%]; p = 0.03). There was no difference in presence of ICU strain between high and low workload groups (16 [55.2%] vs 33 [35.5%]; p = 0.06), or presence of GOC conflict (21 [72.4%] vs 56 [60.2%]; p = 0.23). There was no difference in the number of physicians caring for more patients during COVID-19 compared with prepandemic (high workload 10 physicians [34.5%] vs low workload 22 physicians [23.9%]; p = 0.26).
ICU Characteristics
The 62 study ICUs were across the United States—Northeast (n = 24, 38.7%), South (n = 24, 38.7%), West (n = 8, 12.9%), and Midwest (n = 6, 9.7%) (Table 2). The majority of the included ICUs were medical ICUs (n = 34, 54.8%). In addition to the participating intensivist, ICU providers included advanced practice providers in 46 (74.2%) ICUs, fellows in 42 (67.7%) ICUs, and residents in 39 (62.9%) ICUs. The median number of total providers (excluding the intensivist) during the day was 4 (IQR, 3–6), and there was a median of 2 providers at night (IQR, 1–3). There were more providers present at night in the high workload group (median, 3 [IQR, 2–3] vs 2 [IQR, 1.1–3]; p = 0.01) but no difference in number of providers present during the day (median, 5 [IQR, 4–6] vs 4 [IQR, 3–6]; p = 0.10).
Table 2.
ICU Characteristics by Physician Workload
| Characteristic | All ICUs, n = 62 | ICUs for High Workload Physiciansa, n = 29 | ICUs for Low Workload Physiciansa, n = 93 |
|---|---|---|---|
| General ICU classification | |||
| Academic ICU, n (%) | 60 (96.8) | 28 (96.6) | 91 (97.8) |
| U.S. regionb, n (%) | |||
| North | 24 (38.7) | 4 (13.8) | 39 (41.9) |
| South | 24 (38.7) | 17 (58.6) | 34 (36.6) |
| West | 8 (12.9) | 4 (13.8) | 16 (17.2) |
| Midwest | 6 (9.7) | 3 (10.3) | 4 (4.3) |
| Type of ICU, n (%) | |||
| Medical ICU | 34 (54.8) | 12 (41.4) | 52 (55.9) |
| Combined medical/surgical | 6 (9.7) | 2 (6.9) | 9 (9.7) |
| Cardiac care unit | 5 (8.1) | 1 (3.5) | 12 (12.9) |
| Cardiothoracic surgery | 4 (6.4) | 3 (10.3) | 6 (6.5) |
| Neurointensive care unit | 5 (8.1) | 3 (10.3) | 9 (9.7) |
| Other | 3 (4.8) | 4 (13.8) | 2 (2.1) |
| ICU structure and staff | |||
| Tele-ICU present, n (%) | 23 (37.1) | 13 (44.8) | 37 (39.8) |
| Closed ICU, n (%) | 49 (79.0) | 25 (86.2) | 67 (72.0) |
| If open, requires mandatory critical care consult, n (%) | 10/13 (76.9) | 3/4 (75) | 19/26 (73.1) |
| COVID-19 patients present, n (%) | 49 (79) | 17 (58.6) | 74 (79.6) |
| Day team members, n (%) | |||
| APPs | 46 (74.2) | 25 (86.2) | 73 (78.5) |
| Fellows | 42 (67.7) | 23 (79.3) | 59 (63.4) |
| Residents | 39 (63.9) | 21 (72.4) | 51 (54.8) |
| Number of providers during dayc, median (IQR) | 4 (3–6) | 5 (4–6) | 4 (3–6) |
| Night team members, n (%) | |||
| APPs | 36 (58.1) | 25 (86.2) | 53 (57.0) |
| Fellows | 25 (40.3) | 14 (48.3) | 33 (35.5) |
| Residents | 32 (53.3) | 15 (51.7) | 44 (47.3) |
| Number of providers during nightc, median (IQR) | 2 (1–3) | 3 (2–3) | 2 (1.1–3) |
| Intensivist present at night, n (%) | 32 (51.6) | 7 (24.1) | 45 (48.4) |
| Ancillary staff presence, n (%) | |||
| Occupational therapist | 23 (37.1) | 8 (27.6) | 33 (35.5) |
| Pharmacist | 47 (75.8) | 25 (86.2) | 69 (74.2) |
| Physical therapist | 30 (48.4) | 12 (41.4) | 42 (45.2) |
| Respiratory therapist | 55 (88.7) | 26 (89.7) | 82 (88.2) |
| Social worker | 46 (74.2) | 20 (69.0) | 69 (74.2) |
| Summary ICU datade | |||
| Number of beds available, median (IQR) | 16 (12–20) | 20 (16.5–20) | 16 (12–22) |
| Average Number patients per nurse in ICU ratio, median (IQR) | 2 (2–2) | 2 (2–2) | 2 (2–2) |
| Annual admissions, median (IQR) | 1,192 (750–1,800) | 1,450 (1,279–1,541) | 1,300 (750–2,501) |
| Average length of stay (d), median (IQR) | 4.61 (3.37–5.57) | 5.1 (3.93–5.75) | 4 (3.02–5) |
| Annual average mortality (%), median (IQR) | 11.7 (6.02–19.4) | 5.04 (3.57–7.66) | 11.7 (6.07–19) |
APP = advanced practice provider, IQR = interquartile range.
aEight out 62 ICUs had physicians in both high and low workload groups. ICU characteristics reported for high and low workload groups by each physician.
bRegion of United States based on U.S. Census Bureau of Regions and Divisions.
cNumber of providers during day and night are “excluding” ICU physician.
dSummary ICU data based on last complete calendar year of data available (for most ICUs data are from 2019).
en with missing summary ICU data = 10, all other variables with missing < 2.
Patient Characteristics
A total of 1,322 patients were included in the study with median patient age of 61.0 years (IQR, 50.0–70.0) (Table 3). The most common ICU admission diagnosis was respiratory failure (n = 575, 43.5%), with 693 patients (52.4%) on invasive mechanical ventilation (IMV) and 449 patients (34.0%) requiring vasopressors in the 24 hours prior to the study day. The median Sequential Organ Failure Assessment (SOFA) score was 4.0 (IQR, 2.0–8.0). There was no difference in presence of IMV (median percentage, 53% [IQR, 36–65] in high workload vs 55% [IQR, 36.5–65] in low; p = 0.81), vasopressors (median percentage, 29% [IQR, 13–38] in high vs 31.5% [IQR, 17.5–50] in low; p = 0.19), or SOFA score (median score, 4.5 [IQR, 2.0–7.0] in high vs 4.0 [IQR, 2.8–6.0] in low; p = 0.87) between workload groups.
Table 3.
Patient Characteristics for Full Patient Cohort
| Characteristic | All Patients, n = 1,322 |
|---|---|
| Patient age (yr), median (IQR) | 61.0 (50.0–70.0) |
| Patient body mass indexa, median (IQR) | 28.60 (23.82–34.74) |
| Gender, n (%) | |
| Male | 765 (57.9) |
| Female | 556 (42.1) |
| Race, n (%) | |
| White | 654 (49.5) |
| Black | 476 (36.0) |
| Asian | 26 (2.0) |
| Unknown | 158 (11.9) |
| Other | 8 (0.6) |
| Hispanic, n (%) | |
| Full code on ICU admission, n (%) | 107 (8.1) |
| ICU admission diagnosis, n (%) | 1,232 (93.2) |
| Respiratory failure | 575 (43.5) |
| Sepsis/septic shock | 173 (13.1) |
| Postoperative state | 121 (9.1) |
| Otherb | 453 (34.3) |
| COVID-19 present, n (%) | 275 (20.8) |
| Life sustaining treatment, n (%) | |
| Invasive mechanical ventilation | 693 (52.4) |
| Vasopressorsa | 449 (34.0) |
| Continuous renal replacement therapy | 150 (11.3) |
| Extracorporeal membranous oxygenation | 39 (3.0) |
| Left heart support | 37 (2.8) |
| Sequential Organ Failure Assessment score, median (IQR) | 4 (2–8) |
| 28-d outcome | |
| Discharged alive | 679 (51.4) |
| Hospitalized—non-ICU floor | 144 (10.9) |
| Hospitalized—ICU | 113 (8.5) |
| Deceased | 347 (26.2) |
| Unknown | 39 (3.0) |
| Length of ICU Stay (d), median (IQR) | 9 (4–20) |
IQR = interquartile range.
an missing: body mass index = 18, vasopressors = 15, all other variables with n missing <5.
bOther diagnosis includes: myocardial infarction, arrhythmias, stroke, gastrointestinal bleed, heart failure, renal failure, toxic ingestion, pulmonary embolism, trauma, undifferentiated shock, cardiac arrest, diabetic ketoacidosis, cardiogenic shock, seizure, and altered mental status.
Primary Aim: Physician Burnout and Association With Workload
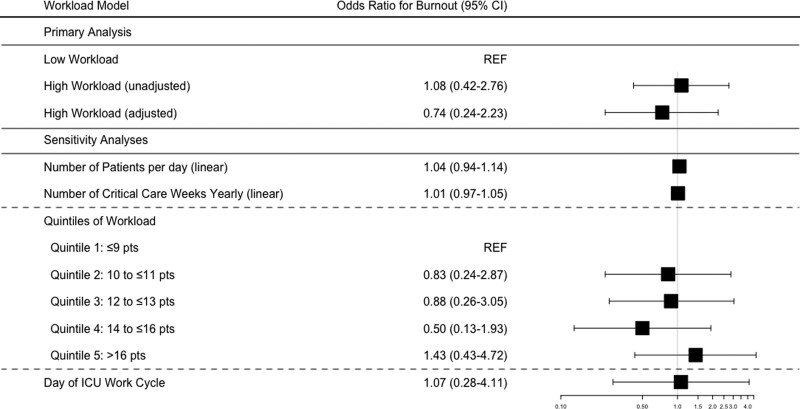
Thirty-two of the physicians (26.4%) had a WBI score greater than or equal to 4, meeting the threshold for burnout (Table 1). The median WBI score was 2 (IQR, 0–4). ICU strain was more likely to be perceived by physicians with burnout compared with those without burnout (59.4% vs 33.7%; p = 0.04). Additionally, median-aggregated patient SOFA score was higher for physicians experiencing burnout compared with those not (median aggregated SOFA, 5 [IQR, 3–7] vs 4 [IQR, 2–6]; p = 0.02). In the multivariable model, there was no difference in odds of burnout in the high workload group compared with low workload group (adjusted OR, 0.74; 95% CI, 0.25–2.24) (Fig. 2; Supplemental Digital Content - Table 6, http://links.lww.com/CCX/B69). There was no interaction between workload and physician gender, years worked, or total clinical time on the association with burnout.
Figure 2.
Forest plot of odds ratios for burnout with workload definitions. All odds ratios and CI generated by logistic regression. Burnout was defined at Well-Being Index score ≥ 4. Low workload less than or equal to 14 patients per physician; high workload greater than 14 patients per physician. Unadjusted analysis—univariate logistic regression model. Adjusted analysis—multivariable logistic regression model, n = 118, adjusted for median Sequential Organ Failure Assessment score, % on invasive mechanical ventilation, % on vasopressors, #new patients, total # people on ICU team, Goals of care conflict, and ICU strain. Sensitivity analyses—unadjusted logistic regression models for alternative definitions of workload. Number of patients per day per physician as a linear variable. Number of critical care weeks worked yearly as a linear variable. Quintiles of workload refers to patients per physician. Day of continuous ICU work cycle (i.e., day 2 of 7), as a linear variable.
Secondary Aim: Patient Outcomes and Association With Workload
At 28 days, 679 patients (51.4%) were alive and discharged from the hospital, and 347 patients (26.2%) were deceased (Table 3). Two hundred fifty-seven (19.4%) patients remained hospitalized at day 28 with 113 (8.5%) still in the ICU and 144 (10.9%) on a non-ICU hospital ward. Thirty-nine (3.0%) patients’ 28-day outcome was unknown. Median ICU length of stay was 9 days (IQR, 4–20). A binomial mixed-effects model restricted to the patients alive or deceased showed no difference in odds of death in the high workload group compared with low workload group (OR, 1.33; 95% CI, 0.92–1.91) (Supplemental Digital Content - Table 7, http://links.lww.com/CCX/B69).
Sensitivity Analyses
There was no difference in the association of workload with burnout for physicians in all sensitivity analyses (Fig. 2; Supplemental Table 6, http://links.lww.com/CCX/B69).
DISCUSSION
Our study captured intensivist workload, measured as the number of patients cared for. Study ICUs were primarily recruited through SCCM’s Discovery Network and were similar to ICUs and patients represented in other Discovery network studies (32, 33). The overall prevalence of burnout in our cohort of ICU physicians was 26.4%, and there was no difference in the prevalence of burnout between physicians with high workload (>14 patients per physician) versus low workload (≤14 patients per physician). At 28 day, there was no difference in odds of patient death in the high workload group compared with the low workload group.
Despite evidence that workload and job demands are perceived as drivers of burnout (25, 30), we did not observe any difference in the presence of burnout in physicians with greater than 14 patients. One explanation for equal burnout prevalence between workload groups may be greater burnout in the low workload group related to the higher frequency of night duties and greater amount of critical care time. It is also possible that physicians in our study did experience greater stress related to ICU work that is not captured by assessing the number of patients cared for.
Current literature cites the prevalence of burnout among ICU physicians to range from 25% to 50% (1, 11, 34). Our results fall on the lower end of this. Physicians who have burnout may have been less likely to participate due to less time or inclination to complete another task, leading to decreased measured burnout. However, 83% of physicians who were asked participated. Our study also had more physicians identifying as men and early to mid-career clinicians; we did not find any interaction of gender or years in practice on the association of workload to burnout. Use of the WBI, which measures distress (which includes, but is not limited to, burnout), may not have captured physicians experiencing burnout without distress in other domains. Although the study took place during the COVID-19 pandemic, overall prevalence of COVID-19 among patients was 20%, which may indicate we sampled physicians at periods of relatively low COVID-19 prevalence and consequently less stress. Some physicians did report changes in number of patients and/or length of ICU service block related to COVID-19, but there was no difference between workload groups limiting our ability to discern how the pandemic may have impacted our study. Mikkelsen et al (17) found that 2-week clinical workload, compared with one-week, was associated with higher levels of burnout. Our sensitivity analysis did not show similar results, which may be due, in part, to shorter clinical blocks as the majority of physicians (n = 114 [93.4%]) worked in 7-day service blocks, and 105 physicians (86.1%) completed survey measures on days 1 through 4 of a 7-day (or longer) ICU service block.
Our results can suggest other potential drivers of burnout in the ICU. The majority of intensivists indicated that non-ICU responsibilities and ICU strain contributed to their burden of work; and there was a significant relationship between ICU strain and burnout (p = 0.04). Although some studies have examined the relationship between strain and patient outcomes (35, 36), greater understanding of the relationship between strain and physician outcomes could help understand which aspects of ICU work relate to burnout. Additionally, physicians experiencing burnout had more acutely ill patients than physicians without burnout (p = 0.02). Though these results are not adjusted for multiple comparisons and must be interpreted with caution, they are hypotheses generating and warrant further investigation.
Our study has limitations. First, there is high likelihood of selection bias. We gave site flexibility in choosing ICUs, physicians, and study days for participation and captured a group of younger physicians working mostly in medical ICUs in academic institutions. It is possible that physicians in the study represent a less distressed sample (analogous to the “healthy worker” bias) (37). Our study did not include intensivists in the community setting, who may have different ICU structure and staffing models. Inclusion of community intensivists may have yielded a different prevalence of burnout.
We chose the WBI for its shorter format, accessibility, and as a recommended assessment by the National Academy of Medicine (38). Since the WBI was not designed to measure burnout directly, there is risk of misclassification bias, and use of a different instrument may have led to different results. The WBI has been validated against the Maslach Burnout Inventory (14) with a high predictive value for burnout (23), and several studies of ICU physicians have used the WBI to measure and identify burnout (17, 25, 26). Our study is also limited by our chosen definition of workload—the number of patients cared for—and categorization of workload as high and low based on a cutoff of 14 patients; this is, an objective, easily calculated metric, but it may not sufficiently capture ICU workload. Our workload groups were of unequal sizes and may have also skewed results. The sensitivity analyses using different measures of workload showed results similar to our primary analysis. As with all survey-based studies, self-reporting may lead to information bias. Additionally, factors not measured in the study, such as support outside of other ICU team members, workplace culture, time spent on the electronic medical record and documentation, and/or nonprofessional duties may contribute to perceived workload. Finally, our study may have been underpowered as our power calculations assumed equal site-by-site enrollment.
CONCLUSIONS
Our study showed that one in four academic ICU physicians experienced burnout and did not demonstrate an association between the number of patients a physician cared for and burnout in the ICU. Future studies may benefit from incorporating qualitative methods to explore how to measure workload and factors of ICU work associated with psychologic well-being.
ACKNOWLEDGMENTS
We thank Taylor Barnes, Kesany Boupapanh, Sandi Capelli, Daniel Ceusters, Lianne Del Cruz, Aditi Desai, Krisha Desai, Olivia Krol, Meagan Mayo, Prakriti Mehta, Kinjal Mistry, Max Monahan, Alicia Morris, Keyla Ordonez, Ithan Peltan, Elizabeth Peters, Amy Rovitelli, and Sui Tsang for contributions to study coordination and data collection.
Supplementary Material
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (http://journals.lww.com/ccejournal).
Supported, in part, by the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Number UL1TR002378. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Dr. Agarwal reports funding from National Institute of General Medical Sciences T32 Training Grant (T32GM095442, principal investigator: C. M. Coopersmith). Dr. Dickert reports funding from the National Institutes of Health and Agency for Healthcare Research and Quality, and for consulting for Abiomed. Dr. Sevransky reports funding to institution from the Marcus foundation, Department of Defense, Center for Diseases Control Foundation. The remaining authors have disclosed that they do not have any potential conflicts of interest.
This work was performed at the Albert Einstein College of Medicine, Emory Center for Critical Care, Emory University School of Medicine, Medical University of South Carolina, Oregon Health and Science University, Tulane University School of Medicine, University of Miami Miller School of Medicine, University of Michigan School of Medicine, University of Pennsylvania, University of Rochester Medical Center, University of Utah, Washington University School of Medicine in St. Louis, Weill Cornell Medical College, University of Florida, and Yale School of Medicine.
REFERENCES
- 1.Pastores SM, Kvetan V, Coopersmith CM, et al. ; Academic Leaders in Critical Care Medicine (ALCCM) Task Force of the Society of the Critical Care Medicine: Workforce, workload, and burnout among intensivists and advanced practice providers: A narrative review. Crit Care Med 2019; 47:550–557 [DOI] [PubMed] [Google Scholar]
- 2.Venkataraman R, Ramakrishnan N: Outcomes related to telemedicine in the intensive care unit: What we know and would like to know. Crit Care Clin 2015; 31:225–237 [DOI] [PubMed] [Google Scholar]
- 3.Kerlin MP, Harhay MO, Kahn JM, et al. : Nighttime intensivist staffing, mortality, and limits on life support: A retrospective cohort study. Chest 2015; 147:951–958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kerlin MP, Small DS, Cooney E, et al. : A randomized trial of nighttime physician staffing in an intensive care unit. N Engl J Med 2013; 368:2201–2209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wilcox ME, Chong CA, Niven DJ, et al. : Do intensivist staffing patterns influence hospital mortality following ICU admission? A systematic review and meta-analyses. Crit Care Med 2013; 41:2253–2274 [DOI] [PubMed] [Google Scholar]
- 6.Gershengorn HB, Harrison DA, Garland A, et al. : Association of intensive care unit patient-to-intensivist ratios with hospital mortality. JAMA Intern Med 2017; 177:388–396 [DOI] [PubMed] [Google Scholar]
- 7.Gershengorn HB, Pilcher DV, Litton E, Anstey M, Garland A, Wunsch H: Association of patient-to-intensivist ratio with hospital mortality in Australia and New Zealand. Intensive Care Med 2022; 48:179–189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nguyen YL, Wallace DJ, Yordanov Y, et al. : The volume-outcome relationship in critical care: A systematic review and meta-analysis. Chest 2015; 148:79–92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kahn JM, Goss CH, Heagerty PJ, et al. : Hospital volume and the outcomes of mechanical ventilation. N Engl J Med 2006; 355:41–50 [DOI] [PubMed] [Google Scholar]
- 10.Kane L: ‘Death by 1000 Cuts’: Medscape National Physician Burnout & Suicide Report 2021. 2021. Available at: https://www.medscape.com/slideshow/2021-lifestyle-burnout-013456?src=wnl_physrep_210123_burnout2021&uac=186615BG&impID=3148805&faf=1#2. Accessed March 25, 2022
- 11.Moll V, Meissen H, Pappas S, et al. : The coronavirus disease 2019 pandemic impacts burnout syndrome differently among multiprofessional critical care clinicians-a longitudinal survey study. Crit Care Med 2022; 50:440–448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moreno-Mulet C, Sansó N, Carrero-Planells A, et al. : The impact of the COVID-19 pandemic on ICU healthcare professionals: A mixed methods study. Int J Environ Res Public Health 2021; 18:9243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.West CP, Dyrbye LN, Sloan JA, et al. : Single item measures of emotional exhaustion and depersonalization are useful for assessing burnout in medical professionals. J Gen Intern Med 2009; 24:1318–1321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Maslach C, Jackson SE, Leiter MP: Maslach Burnout Inventory Manual. Fourth Edition. Menlo Park, CA, Mind Garden Inc. 1996 [Google Scholar]
- 15.Burghi G, Lambert J, Chaize M, et al. : Prevalence, risk factors and consequences of severe burnout syndrome in ICU. Intensive Care Med 2014; 40:1785–1786 [DOI] [PubMed] [Google Scholar]
- 16.Dewa CS, Jacobs P, Thanh NX, et al. : An estimate of the cost of burnout on early retirement and reduction in clinical hours of practicing physicians in Canada. BMC Health Serv Res 2014; 14:254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mikkelsen ME, Anderson BJ, Bellini L, et al. : Burnout, and fulfillment, in the profession of critical care medicine. Am J Respir Crit Care Med 2019; 200:931–933 [DOI] [PubMed] [Google Scholar]
- 18.Ward NS, Read R, Afessa B, et al. : Perceived effects of attending physician workload in academic medical intensive care units: A national survey of training program directors. Crit Care Med 2012; 40:400–405 [DOI] [PubMed] [Google Scholar]
- 19.Ward NS, Afessa B, Kleinpell R, et al. ; Members of Society of Critical Care Medicine Taskforce on ICU Staffing: Intensivist/patient ratios in closed ICUs: A statement from the Society of Critical Care Medicine taskforce on ICU staffing. Crit Care Med 2013; 41:638–645 [DOI] [PubMed] [Google Scholar]
- 20.Ward NS, Howell MD: Intensivist-to-patient ratios in ICUs: Is there a number? Curr Opin Anaesthesiol 2015; 28:172–179 [DOI] [PubMed] [Google Scholar]
- 21.Discovery, the Critical Care Research Network. 2021. Available at: [https://www.sccm.org/Research/Research/Discovery-Research-Network]. Accessed March 25, 2022
- 22.Halpern SD: ICU capacity strain and the quality and allocation of critical care. Curr Opin Crit Care 2011; 17:648–657 [DOI] [PubMed] [Google Scholar]
- 23.Dyrbye LN, Satele D, Shanafelt T: Ability of a 9-item well-being index to identify distress and stratify quality of life in us workers. J Occup Environ Med 2016; 58:810–817 [DOI] [PubMed] [Google Scholar]
- 24.Dyrbye LN, Satele D, Sloan J, Shanafelt TD: Utility of a brief screening tool to identify physicians in distress. J Gen Intern Med 2013; 28:421–427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gomez S, Anderson BJ, Yu H, Gutsche J, et al. : Benchmarking critical care well-being: Before and after the coronavirus disease 2019 pandemic. Crit Care Explor 2020; 2:e0233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kerlin MP, Silvestri JA, Klaiman T, et al. Critical care clinician wellness during the covid-19 pandemic: A longitudinal analysis. Ann Am Thorac Soc 2022; 19:329–331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Harris PA, Taylor R, Minor BL, et al. ; REDCap Consortium: The REDCap consortium: Building an international community of software platform partners. J Biomed Inform 2019; 95:103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Harris PA, Taylor R, Thielke R, et al. : Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009; 42:377–381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Greenland S, Pearl J, Robins JM: Causal diagrams for epidemiologic research. Epidemiology 1999; 10:37–48 [PubMed] [Google Scholar]
- 30.Shanafelt TD, Noseworthy JH: Executive leadership and physician well-being: Nine organizational strategies to promote engagement and reduce burnout. Mayo Clin Proc 2017; 92:129–146 [DOI] [PubMed] [Google Scholar]
- 31.Bennette C, Vickers A: Against quantiles: Categorization of continuous variables in epidemiologic research, and its discontents. BMC Med Res Methodol 2012; 12:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sevransky JE, Chai ZJ, Cotsonis GA, et al. : Survey of annual staffing workloads for adult critical care physicians working in the United States. Ann Am Thorac Soc 2016; 13:751–753 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Johnson SW, Garcia MA, Sisson EKQ, et al. : Hospital variation in management and outcomes of acute respiratory distress syndrome due to COVID-19. Crit Care Explor 2022; 10:e0638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Embriaco N, Azoulay E, Barrau K, et al. : High level of burnout in intensivists: Prevalence and associated factors. Am J Respir Crit Care Med 2007; 175:686–692 [DOI] [PubMed] [Google Scholar]
- 35.Hua M, Halpern SD, Gabler NB, et al. : Effect of ICU strain on timing of limitations in life-sustaining therapy and on death. Intensive Care Med 2016; 42:987–994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vranas KC, Jopling JK, Scott JY, et al. : The association of ICU acuity with outcomes of patients at low risk of dying. Crit Care Med 2018; 46:347–353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shrank WH, Patrick AR, Brookhart MA: Healthy user and related biases in observational studies of preventive interventions: A primer for physicians. J Gen Intern Med 2011; 26:546–550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.National Academy of Medicine Action Collaborative on Clinician Well-Being and Resilience. Validated Instruments to Assess Work-Related Dimensions of Well-Being. 2022. Available at: https://nam.edu/valid-reliable-survey-instruments-measure-burnout-well-work-related-dimensions/. Accessed March 25, 2022
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.