Abstract
Policy Points.
Current telehealth policy discussions are focused on synchronous video and audio telehealth visits delivered by traditional providers and have neglected the growing number of alternative telehealth offerings.
These alternative telehealth offerings range from simply supporting traditional brick‐and‐mortar providers to telehealth‐only companies that directly compete with them.
We describe policy challenges across this range of alternative telehealth offerings in terms of using the appropriate payment model, determining the payment amount, and ensuring the quality of care.
Keywords: Telehealth, Digital health
For years, telehealth has been touted as a potentially transformative technology that will increase health care access and efficiency. Although the use of telehealth already was growing, the pandemic drove a dramatic expansion. 1 , 2 Many of the temporary telehealth waivers established during the pandemic to spur this growth are set to expire at the end of the public health emergency. This has resulted in intense interest in permanent changes in telehealth policy across state legislatures and Congress. 3 , 4 , 5 The most common forms of telehealth—video visits and, to a lesser extent, audio‐only visits delivered by traditional “brick‐and‐mortar” providers—are the focus of most of the debate. 6 , 7 , 8 , 9 Key components of debate include the types of visits that should be covered, whether there should be payment parity for telehealth and in‐person visits, and whether physicians’ licensure should extend across state lines.
These ongoing debates do not, however, capture the full breadth of telehealth offerings available today and in the near future. Accordingly, we are concerned that any payment and regulatory policies implemented may soon be out of date. An example is Ginger, a telehealth offering that provides members unlimited 24/7 access to behavioral health coaches through text communication in its app, with escalation as needed to virtual therapy sessions with licensed therapists and psychiatrists. 10 Ginger has partnerships with hundreds of employers and recently became an in‐network care option for 14 million Cigna members. 11 With its fully virtual care model, Ginger has much lower overhead costs than a traditional brick‐and‐mortar practice. How, then, should payment rates reflect these lower operational costs? Ginger uses unlicensed health coaches, 12 so how should states ensure quality, given that current licensure‐based mechanisms do not apply? Ginger typically charges a monthly fee per patient, 13 , 14 but such payment models are not reflected in current discussions about payment. Moreover, Ginger is only one of many alternative telehealth products, which are themselves highly heterogeneous, reflecting not only differences in target conditions but also distinct approaches to delivering care.
In this perspective, we first describe the wide array of emerging alternative telehealth offerings and then discuss how these newer models may impact payment policies and regulations. We hope that by raising these issues, we can inform a more holistic telehealth policy strategy.
Emerging Alternative Telehealth Offerings
Given the many existing telehealth typologies, our goal is not to create another comprehensive categorization. 5 , 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 Instead, we want to provide illustrative examples other than synchronous video or audio visits and to explain how they can inform policy debates. We also recognize that the landscape is changing rapidly and that new models of care are emerging that we have not even considered.
Before turning to these emerging telehealth options, we should clarify what we mean by the “traditional delivery system” or, synonymously, “brick‐and‐mortar providers.” We use both these terms to refer to individual practices or large integrated health systems that, until the pandemic began, largely delivered care via in‐person visits. Americans often have long‐term relationships with these brick‐and‐mortar providers, which are licensed by states and provide care across a continuum of care needs from preventive services to acute care to chronic illness management. Even though use of alternative payment models has increased, the predominant payment method for these systems still is fee‐for‐service payment for individual services. Throughout this perspective, we refer to these brick‐and‐mortar providers as “traditional providers” and the typical model in which they operate as the “standard care model.”
During the pandemic, traditional providers adopted telehealth to varying levels. For example, the majority of care provided by behavioral health specialists is now via telemedicine. 2 In other areas of clinical medicine, such as ophthalmology or acute management of a heart attack, the care model has not changed substantively. 18 , 19 One policy issue we touch on later is how to ensure that traditional providers remain financially viable to offer these services as telehealth‐only providers grow more prevalent.
From the perspective of regulation and payment policy, a key dimension on which telehealth offerings vary is how they interact with the traditional health care delivery system. Broadly speaking, offerings either support the traditional system or compete with it. Supporting offerings can be further subdivided into two groups: those that facilitate traditional forms of care and those that augment them. Competing offerings can also be subdivided into two groups: those that indirectly disrupt the traditional system and those that seek to replace it. Figure 1 shows several telehealth offerings that are available today and where they fall across these four groups.
Figure 1.
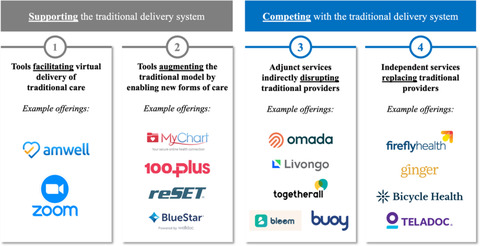
Alternative telehealth landscape and example offerings [Colour figure can be viewed at wileyonlinelibrary.com]
In Figure 1, anchoring the left side are telehealth tools that facilitate the virtual delivery of traditional care via video and audio telehealth visits. Relaxation of HIPAA enforcement during the pandemic temporarily opened the breadth of tools available to enable telehealth visits (e.g., FaceTime). 20 Even so, many traditional providers planning to continue offering telehealth visits after the pandemic have turned to companies such as Zoom or Amwell, which sell access to secure telehealth software. 21 , 22 Despite being virtual, these visits map cleanly to policy precedents for in‐person visits.
The second group represents telehealth tools that augment the traditional model by enabling new forms of care. These include patient portal messages and remote patient monitoring (remote collection and transmission of physiological measurements, such as blood glucose levels or blood pressure). Before the pandemic, patients and providers already used many of these communication methods but typically were not reimbursed. Instead, these methods were provided for free, following the paradigm that reimbursement for individual visits encompassed a provider's time before and after the visits (e.g., sending a letter to patients about their lab test results). Under this paradigm, responding to a portal message or giving patients feedback on their latest blood pressure measurement was simply supporting the care given during a visit. By facilitating frequent interchanges between patients and providers, these augmenting tools offer new facets to care delivery outside traditional “visits.” At the same time, they challenge our current payment system, 23 something we shall return to later.
Also included in this second group are offerings often referred to as “digital therapeutics,” 24 such as Pear's reSET product for substance use disorders or Weldoc's BlueStar product for diabetes management, which deliver software‐based interactive lessons and coaching to reinforce behavior change. These offerings diverge from the status quo by relying on software, rather than people or drugs, to help treat patients. At the same time, these products are designed to work alongside the traditional model. For example, they are intended to be recommended to patients by their traditional providers and are designed to have those providers involved in care. Some, like reSET, require prescriptions from a clinician, similar to traditional pharmaceutical drugs (e.g., small molecules or biologics). 25 reSET also has a provider portal that gives traditional providers visibility into patients’ usage of the application (e.g., lessons completed) and patient‐reported measures such as cravings and triggers. 25
The last two groups are telehealth offerings competing with the traditional system. The third group represents adjunct telehealth services indirectly disrupting traditional providers. It includes products such as Omada Health's and Livongo's chronic disease management platforms. Both products offer access to human health coaches (through both text and audio/video interaction), remote patient monitoring, interactive curated lessons (and other resources) through their software, and an online peer community. 26 , 27 Also included are less holistic products such as Togetherall and Bloom, which offer subsets of the services offered by Omada's and Livongo's packages. In Togetherall's case, it is the online peer community, 28 and in Bloom's, it is the interactive lessons. 29 Finally, we include tools like Buoy, an artificial intelligence‐enabled symptom checker that allows patients to input their symptoms, gives them a list of potential diagnoses, and directs them to appropriate sites of care (e.g., advising them to seek immediate care). 30 In this case, software is potentially replacing the role of a traditional provider in diagnosis and triage.
The key distinction we make separating this third group from the prior group is that patients can receive this care without the knowledge or involvement of traditional providers. They also are indirectly competing with the standard model. While they do not claim to replace the care that a typical provider offers, if these products succeed, then patients should have fewer needs from the traditional healthcare system. For example, if Omada's diabetes coaching is successful, then patients will have fewer office visits, hospitalizations, or even procedures. Traditional providers will still be needed, of course, when care needs exceed what can be delivered by these alternative approaches.
Our final group is those independent telehealth services that replace traditional providers for a subset of care. This group includes offerings such as Ginger, Bicycle Health, and Firefly Health. Ginger is a product we mentioned earlier that seeks to replace the standard of care for less severe behavioral health conditions and even has the option to escalate care to licensed therapists and psychiatrists. 10 Bicycle Health tries to accomplish something similar for substance use disorders, offering virtual access to licensed providers to prescribe and monitor medication‐assisted treatment. 31 Firefly Health is a fully virtual primary care practice with the explicit goal of replacing its patients’ traditional primary care providers. 32 Finally, Teladoc, perhaps the best‐known telehealth provider, has made a name for itself over the last decade as a convenient telehealth‐only source of care for low‐acuity issues historically addressed by traditional providers. 33 , 34 , 35
We acknowledge that there may be instances where traditional providers direct their patients toward these competing services. Indeed, many of the offerings we have referred to as “indirectly disrupting” actively market themselves as adjuncts, filling gaps in care and working in conjunction with traditional providers. For example, a provider may recommend Omada to help patients manage a chronic condition. Provider groups might “white‐label” Buoy's symptom checker tool and offer access via its patient portal. Even offerings that replace traditional providers may form partnerships with those very organizations they seek to replace. Integrated health systems facing capacity constraints may contract with Teladoc to offload care for low‐margin patients while ensuring they still remain “in‐system” for future care needs. These partnerships could also have the added benefit of offering patients access to care outside standard office hours. In these instances, traditional providers are still being replaced. The difference is that they willingly allow this to happen for select services: accepting scope‐limited changes in the interest of larger goals such as increasing patient access to care, improving quality, or lowering costs. These new services may attract patients to traditional providers or eliminate otherwise unprofitable care. They may be particularly appealing if the traditional provider is at risk for total medical expenses.
We emphasize these four groups because we believe they highlight distinct policy challenges. However, as we have noted, current discussions have focused almost entirely on those related to the first group: telehealth tools that simply facilitate traditional care. Augmenting telehealth tools, while still supporting the traditional system, bring new concerns, such as the growing need to establish payment mechanisms to compensate traditional providers for services like secure patient messaging that in the past have not been billed directly. The remaining two groups that seek to disrupt or replace the traditional delivery system bring other challenges, such as ensuring that traditional providers continue providing services that these competing telehealth models cannot.
Policy Challenges for Telehealth Models
Telehealth models present a range of new challenges for policymakers, but broadly these can be divided into two areas: (1) pricing: what forms of payment should be used and how much should be paid, and (2) quality: ensuring quality of care. Figure 2 summarizes these, and they also are described in more detail later.
Figure 2.
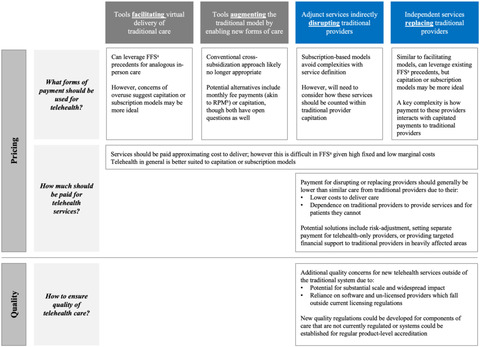
Policy considerations across the telehealth landscape [Colour figure can be viewed at wileyonlinelibrary.com]
aFee‐for‐service; bRemote patient monitoring
Pricing
What Forms of Payment Should Be Used for Telehealth?
For telehealth services with direct in‐person analogs, payment via fee‐for‐service can leverage existing in‐person precedents. Services with in‐person precedents include not only synchronous video or audio visits conducted by traditional providers but also several of the replacing telehealth offerings we have discussed, such as Firefly Health or Ginger. But even though telehealth's greater convenience improves access, it may simultaneously encourage overutilization in a fee‐for‐service setting. 36 This suggests that alternative payment models, such as capitation or partial capitation, may be valuable. If patients’ ties to their providers or the providers’ scope of practice are limited (e.g., specialty care for a time‐limited condition or a narrow telehealth‐only replacing offering), a monthly subscription permitting access to telehealth services (perhaps up to a visit limit) may be more appropriate. Our distinction between subscription and capitation is that the subscription fee covers only the care from that provider, whereas capitation covers care from other providers as well.
Because the majority of augmenting or disrupting telehealth offerings we have discussed do not have analogous in‐person services, simply porting over existing fee‐for‐service payments is not possible. Many disrupting telehealth offerings, such as Omada and Livongo, have focused on monthly subscription fees as their primary means of payment. In some cases, a portion of the fee might be tied to performance metrics like member satisfaction, cost reductions, or health outcomes such as weight loss. 37 , 38 , 39 A subscription fee per user or employee avoids complex definitions of services when the services are a mix of visits and asynchronous exchanges (with a person or even software).
For augmenting telehealth models, the path forward on payment format is more ambiguous. In the past, traditional providers have not billed directly for augmenting telehealth services such as responding to patients’ portal messages or monitoring patients’ self‐reported blood pressure or glucose measurements. Instead, the assumption was that these relatively low‐cost services would be cross‐subsidized by the patients’ other directly billable services. For digital therapeutics like Pear Therapeutic's reSET, even though the product itself is reimbursed in a way similar to that of traditional pharmaceuticals or durable medical equipment, the traditional provider does not directly bill for its role in monitoring progress. 40
Several ongoing trends suggest that the cross‐subsidization approach to pay for these services may no longer be tenable. First, augmenting telehealth volumes grew substantially during the pandemic. For example, the volume of patients’ portal messages seeking medical advice increased by 57% across the more than 300 health systems using Epic's electronic health record. 41 Having experienced the convenience and accessibility benefits of these offerings, patients are likely to continue demanding care through these new modalities. As these services grow to become a substantial fraction of total providers’ activity, so too will the need for reimbursing providers’ time delivering care and coordinating with adjunctive telehealth providers. Second, as more complex augmenting telehealth options emerge, providers will be reluctant to devote the necessary resources for patients’ joining unless they are promised reimbursement. Third, as products become more sophisticated (e.g., digital therapeutics like BlueStar or reSET) or as patients and providers grow more adept at leveraging these new modalities (e.g., patients become more skilled at addressing care needs through messaging rather than requiring a visit), augmenting telehealth models may increasingly replace in‐person visits, thereby diminishing the revenue that had been used to cross‐subsidize unreimbursed services and activities.
One strategy to pay for these augmenting telehealth offerings is to introduce new fee‐for‐service payments. Accordingly, new codes and related payments have been established for telephone calls and, more recently, select patient portal messages called “e‐visits.” The number and complexity of restrictions on when e‐visit codes can be used, in addition to their modest reimbursement, have, however, limited the codes’ utility and uptake. A provider can bill for an e‐visit only if the portal message is for a new medical issue not related to a recent office visit, if the message was initiated by the patient, if the patient's consent was obtained, and if a “clinical decision” was made. 23 In addition, the providers’ low reimbursement may only partially offset their administrative cost of submitting a fee‐for‐service bill. Indeed, one study estimated these costs at $20 for a single bill. 42
A related but somewhat distinct approach to paying for augmenting telehealth services would be to broaden the definitions of services and to charge monthly fees for different components of the services. These types of monthly payments sit between a fee‐for‐service payment and capitation. For example, reimbursement for remote patient monitoring (RPM) is not for individual measurements but is a monthly payment. Using specific CPT codes, Medicare (and many commercial payers) pays for remote data collection over 30 days as long as there are 16 days of data collection in that period. Additionally, the providers’ time spent communicating results with patients and incorporating the data into care management is aggregated over the month and reimbursed in 20‐minute increments. 43 Analogous models could be constructed for portal messages or digital therapeutics, in which providers charge payers monthly for time spent responding to messages or interpreting data from a digital therapy, as long as it reaches a certain minimal threshold.
While such monthly fee payment models can help pay for this care, they also can introduce new problems. First, it is difficult to create an intuitive service definition given that the “service” is often actually composed of many small activities occurring over time. 23 For example, for RPM, on the sixteenth day of data collection, reimbursement becomes applicable and the service flips from nonbillable to billable, but clinically there is nothing magical about 16 versus 15 days of data collection. The effort required for documenting and navigating the rules of these new complex codes will be frustrating to providers and entail expenses.
Second, patient cost‐sharing tied to reimbursement adds further complexities. If patients who previously uploaded blood pressure measurements are now given an automatic blood pressure cuff that uploads data every day, they will now be charged for services that were previously free and may be unsure why they are being billed. This can complicate communication between the patient and the provider, particularly since the lack of an in‐person visit means that patients’ payments must be collected remotely.
Finally, as noted earlier, the administrative costs of submitting a bill are substantial, and therefore the service must be defined broadly enough to justify efforts to collect reimbursement even if that service definition is broader than what is clinically sensible.
Moreover, paying a monthly fee may still incentivize overuse, depending on the price (which we discuss in more detail later). 44 Although expanding telehealth products may have substantial fixed costs for the providers (in device procurement, other necessary infrastructure, provider education, and integration into care workflows), once those initial costs have been absorbed, the marginal costs of treating another patient can be low, and providers have a strong incentive to treat as many patients as possible. Scalability is made easier because traditional providers can turn to external companies to obtain devices and for help onboarding patients. 45 Amid the clinical uncertainty as to which patients will benefit from these tools and how they should be used, providers currently have broad discretion in selecting which patients will receive them and for how long they should use them. The concern is that many patients who will not benefit from these alternative telehealth options will want to use them and that providers will have a financial incentive to facilitate that use.
One approach to address the problem of overuse in these forms of monthly payments is to use traditional tools such as increasing out‐of‐pocket costs or requiring prior authorization. Alternatively, payments can be shifted to capitated or partial capitation models. Giving providers responsibility for the quality and the total cost of care for a population of patients may better align incentives. Traditional providers will be rewarded for offering more telehealth options only when they reduce the total cost of care and, depending on performance measures, when they improve the quality of care. At the same time, traditional providers are also cautioned not to overprescribe to patients who will not benefit. For providers using both telehealth modalities and in‐person care, capitation models can greatly simplify the administrative burden as well. This benefit will only increase as the array of telehealth offerings expands, giving providers the flexibility to incorporate new technologies into their practice without having to track the complex coding rules often inherent in a traditional fee‐for‐service or monthly fee payment model.
Nonetheless, capitation approaches come with their own issues. First, how best to implement capitation is unclear amid the numerous design and implementation barriers that have been discussed elsewhere. 46 , 47 , 48 , 49 , 50 Second, while capitation may make better use of augmenting telehealth services, it is unclear how it might handle disrupting or replacing telehealth services. Generally, capitation is problematic if entities receiving capitation payments are held responsible for using services they do not control directly or via referral. For example, a traditional primary care provider paid through capitation may appropriately feel that it should not be responsible for a patient that independently begins using Omada's diabetes management program. Accordingly, payers might choose to reimburse disrupting or replacing telehealth services only if the patient's primary care provider offers a referral, thereby echoing the “gatekeeper” models that have been used for specialty services. Or payers may fund access to disrupting or replacing telehealth services through a separate funding stream. For example, employers could pay a telehealth‐only mental health provider a fee per user or, if they are worried about too many users, a (lower) fee per employee.
How Much Should Be Paid for Telehealth Services and Should There Be Associated Changes to Payment to Brick‐and‐Mortar Providers?
The appropriate payment amount for telehealth services will depend on the form of payment, but in general, telehealth services should be paid enough to support their use but not so much as to encourage overuse. This will be accomplished if the payment can approximate the cost to deliver care. But because telehealth services often have high fixed costs and low marginal costs, pricing them at cost to deliver is inherently challenging for a fee‐for‐service model. If prices are set at marginal cost, fixed costs are not covered, and access may be insufficient. If prices are set at average cost, access will be supported but the gap between price and marginal cost will encourage overuse. This is a fundamental issue for all the telehealth models we have discussed (as well as for many other high‐fixed and low‐marginal cost technologies such as MRI machines). The solution, as we noted, is often to move away from fee‐for‐service. An example is subscription models that cover fixed costs and perhaps pay a low per‐service price.
Regardless of which payment system is used, payment for telehealth services from disrupting or replacing providers should also generally be lower than payment for similar care from a traditional provider. One argument for this is that telehealth‐only providers can typically provide services at a lower price. For example, Firefly Health has substantial financial advantages over traditional primary care providers owing to reduced expenses associated with facility space, equipment, and front‐office staff. These “practice expenses” make up a substantial fraction of current payments; indeed, in Medicare's fee‐schedule, practice expenses represent 45% of all payments to providers. 51 Many alternative telehealth offerings have sought other ways of making care more efficient as well. For example, relying more on lower‐cost unlicensed providers or information technology, such as remote patient monitoring or digital therapeutics, reduces the labor costs necessary to care for a given patient. This in turn allows a provider to care for more patients and decreases the costs per patient treated.
Another important reason for lower payments is that disrupting or replacing alternative telehealth options are inherently dependent on the traditional health care system to provide what they cannot. Many of these disrupting or replacing telehealth offerings target a limited set of conditions (e.g., low‐acuity behavioral health issues), provide only a subset of services (e.g., just psychotherapy), or are appropriate for only certain patients, often on the healthier end of the spectrum. For example, Bicycle Health's fully virtual medication‐assisted treatment program would be inappropriate for unstable patients with opioid use disorder. The relatively high level of technology literacy and infrastructure required to fully leverage these offerings places additional restrictions on what types of patients can benefit from them. 53 , 54 , 55 These telehealth patients will likely be disproportionately healthy, high‐income, and educated; that is the type of patients more likely to have commercial insurance, which on average reimburses more for the same service. Traditional providers typically cross‐subsidize the care for sicker patients through their care of healthier patients with lower‐acuity issues or commercial insurance. Losing these higher‐margin patients to alternative telehealth offerings may be viewed as a form of “cherry‐picking,” with both negative health equity implications for patients and negative financial impacts on traditional providers.
We want to clarify that competition from disrupting and replacing telehealth offerings is not bad. In fact, these new offerings can improve quality or reduce costs and push traditional providers to do the same. Instead, our concern is that when competition focuses predominantly on capturing high‐margin patients, it can have pernicious effects. If these newer telehealth providers can capture significant market share within this segment, this may threaten the long‐term financial viability of traditional providers and diminish access for patients for whom virtual care is not appropriate.
One way to address these issues is to risk‐adjust payments to both traditional providers and the alternative telehealth offerings with which they compete, based on factors like socioeconomic status. This would increase payments to traditional providers and decrease payments to alternative telehealth offerings. Appropriate adjustment can also incentivize disrupting and replacing telehealth providers to increase the accessibility of their services for patients facing digital access barriers or develop new solutions for more severely ill patients. Yet, designing a system to adjust for patient complexity may be administratively burdensome and infeasible in the near term. A proper adjustment would likely require the inclusion of hard‐to‐observe patient traits beyond the age‐ and condition‐based characteristics most frequently used today, including factors specific to telehealth, like digital literacy and broadband availability. 53 , 54 , 55 It is also important to acknowledge that risk‐adjusted payments from a single payer cannot address the fact that telehealth providers may preferentially attract patients with commercial insurance.
In lieu of better risk adjustment, payment rates for fee‐for‐service, capitation, or subscription could differ for care delivered by telehealth‐only providers versus telehealth care delivered by brick‐and‐mortar traditional providers. Separate payment systems may enable payers to capture efficiency gains from telehealth‐only providers while still rewarding hybrid models that offer in‐person care. This has not been the norm for payers like Medicare, which uses a single fee schedule for all providers, but one could create a distinct category of telehealth‐only providers. 56 Alternatively, instead of changing fee schedules across the board, payers could give targeted financial support to those traditional providers most affected by cherry‐picking by disrupting or replacing providers. Such models could take inspiration from existing targeted government programs such as Critical Access Hospitals, Federally Qualified Health Centers, and Disproportionate Share Hospitals. For both these approaches, key implementation questions remain, such as the precise distinction between traditional brick‐and‐mortar providers and telehealth‐only providers. For example, whether that line is best drawn as a binary split or whether a more granular spectrum is more appropriate (e.g., defining multiple provider categories based on their telehealth activity as a fraction of total billed activities).
Quality
How to Ensure Quality of Telehealth Care?
While ensuring quality has been an important consideration for all telehealth models (e.g., understanding in what contexts virtual care can match the quality of in‐person care), new disrupting or replacing telehealth models pose distinct challenges. Because they do not face the overhead costs of having brick‐and‐mortar facilities, these offerings can quickly grow and have the potential to reach millions of patients across the country. Thus, a low‐quality disrupting or replacing telehealth offering can cause substantial harm. Yet these products are poor fits for existing regulatory frameworks for maintaining quality. While recognizing that individual provider licensing is imperfect as evidenced by the substantial variation in quality across traditional providers, 57 , 58 licensing nonetheless is a means to ensure a quality floor. In the case of augmenting telehealth offerings, the assumption is that licensed traditional providers can similarly ensure a minimum level of quality for the telehealth services they incorporate into care. However, this framework breaks down when it encounters disrupting or replacing telehealth models that circumvent traditional providers and seek to create value by delivering care largely through lower‐cost and nonlicensed providers or software solutions. Examples are Omada, which positions nonlicensed health coaches as patients’ primary source of guidance for managing their chronic conditions; 27 , 59 , 60 Bloom, which relies on software to deliver interactive mental coaching lessons; 29 and Buoy, which uses artificial intelligence to diagnose and triage patients. 30 Even though many of these offerings insist that their services are not technically “medical treatments,” this could be debated, given that the care they provide can meaningfully impact health outcomes. 12 , 60
The Federal Drug Administration (FDA) can regulate software and devices. But focusing on these components alone does not fully capture alternative telehealth offerings, as they may be a bundle of services from nonlicensed providers, licensed providers, devices, and software. For example, the FDA regulates Livongo's blood glucose meter as a medical device. 37 , 61 The issue is that the device is just one part of Livongo's larger care package. Another complexity is that the bundle of services is likely to change over time as the offering is adapted, such as adding components to a software platform.
The appropriate mechanism for ensuring quality likely depends on the specific telehealth service being considered. In some cases, new quality regulations could be developed for components of care that are not currently regulated. For example, states could create new licensure for health coaches. The assumption is that certifying the parts will ensure the quality of the whole. But determining when additional certification is needed because the model has changed requires full knowledge of the product‐operating model, which may not be readily available.
An alternative strategy may be either a voluntary or a mandated accreditation of telehealth products at the overall product level, similar to that for hospitals or patient‐centered medical homes. 62 A detailed evaluation of workflows, staff training, and software can help ensure the quality of the most critical bundle components as well as the bundle's functioning as a whole. Regular reevaluations can ensure that modifications to services and software updates are factored into its accreditation status.
Conclusions
The telehealth landscape is much broader than current policy discussions would suggest. Many emerging telehealth offerings challenge the typical paradigm of how care is provided. In some cases, they seek to augment traditional providers, and in other cases, the goal is to disrupt or replace them. Many of these companies raise new and important policy challenges that we believe should be factored into a holistic and forward‐looking telehealth policy strategy.
In this perspective, we have highlighted a number of these policy challenges. Additional research will be critical to quantify the relative importance of these challenges and to guide the specific policy design. There is little research evaluating the impact of many of these alternative telehealth offerings on care quality and costs. These evaluations should also focus on identifying the clinical contexts in which they are valuable and those in which they are not (e.g., RPM improves quality for only certain conditions or patient types). High‐value use cases can then be supported, and low‐value use cases might be deterred through new policies. Another important topic is understanding how different payment models affect the utilization of alternative telehealth offerings. Finally, amid the growing presence of disrupting and replacing telehealth offerings, we need to conduct studies to quantify the magnitude of cherry‐picking behavior and its impacts on traditional providers’ finances. Related work could identify which providers or areas are hurt most by the growth of alternative telehealth providers, thereby enabling targeted policy efforts.
Although video and audio visits by traditional providers are currently the most common forms of telehealth, in the long term the emerging telehealth options we have highlighted may become dominant. Before the pandemic, telehealth‐only providers were growing at a much higher rate than telehealth use among existing providers was. 34 With significant investment pouring into telehealth, 63 this growth should only accelerate. Accordingly, the challenges described here should only increase in importance over the coming years. What better time to tackle them than the present?
Funding/Support: The writing of this article was supported by grants from Arnold Ventures. The content is solely the responsibility of the authors and does not necessarily represent the official views of Arnold Ventures.
Acknowledgments: None.
Conflict of Interest Disclosures: Dr. Mehrotra received consulting support from the Pew Charitable Trust and Sanofi for input on emerging telemedicine models. Dr. Chernew is chair of the Medicare Payment Advisory Commission (MedPAC), which has debated Medicare telemedicine policy. The views expressed here are the personal views of Dr. Chernew and not of MedPAC.
References
- 1. Patel SY, Mehrotra A, Huskamp HA, Uscher‐Pines L, Ganguli I, Barnett ML. Trends in outpatient care delivery and telemedicine during the covid‐19 pandemic in the US. JAMA Intern Med. 2021;181(3):388. 10.1001/jamainternmed.2020.5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Mehrotra A, Chernew ME, Linetsky D, Hatch H, Cutler D, Schneider EC. The impact of covid‐19 on outpatient visits in 2020: visits remained stable, despite a late surge in cases. Commonwealth Fund. 2/22/2021. doi: 10.26099/bvhf-e411. [DOI]
- 3. Governor's Press Office . Governor Baker signs health care legislation increasing access to quality, affordable care, promoting telehealth and protecting access to covid‐19 testing, treatment. Massachusetts governor. https://www.mass.gov/news/governor‐baker‐signs‐health‐care‐legislation‐increasing‐access‐to‐quality‐affordable‐care. Published January 1, 2021. Accessed February 26, 2021.
- 4. Health Subcommittee Hearing on Charting the Path Forward for Telehealth . 2021. https://waysandmeans.house.gov/legislation/hearings/health‐subcommittee‐hearing‐charting‐path‐forward‐telehealth. Accessed September 11, 2021.
- 5. Koma W, Cubanski J, Neuman T. Medicare and telehealth: coverage and use during the covid‐19 pandemic and options for the future. KFF. https://www.kff.org/medicare/issue‐brief/medicare‐and‐telehealth‐coverage‐and‐use‐during‐the‐covid‐19‐pandemic‐and‐options‐for‐the‐future/. Published May 19, 2021. Accessed September 11, 2021.
- 6. Mehrotra A, Bhatia RS, Snoswell CL. Paying for telemedicine after the pandemic. JAMA. 2021;325(5):431. 10.1001/jama.2020.25706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Mehrotra A, Wang B, Snyder G. Telemedicine: what should the post‐ pandemic regulatory and payment landscape look like? Commonwealth Fund. https://www.commonwealthfund.org/publications/issue‐briefs/2020/aug/telemedicine‐post‐pandemic‐regulation. Published August 5, 2020. Accessed February 24, 2021.
- 8. Shachar C, Engel J, Elwyn G. Implications for telehealth in a postpandemic future: regulatory and privacy issues. JAMA. 2020;323(23):2375‐2376. 10.1001/jama.2020.7943. [DOI] [PubMed] [Google Scholar]
- 9. Mehrotra A, Nimgaonkar A, Richman B. Telemedicine and medical licensure—potential paths for reform. N Engl J Med. 2021;384(8):687‐690. 10.1056/NEJMp2031608. [DOI] [PubMed] [Google Scholar]
- 10. The Ginger Experience. Ginger.com. https://www.ginger.com/experience. Accessed September 11, 2021.
- 11. Barnes V. Ginger brings on‐demand mental healthcare to 14 million Cigna behavioral health customers nationwide. Business wire. https://www.businesswire.com/news/home/20210428005278/en/Ginger‐Brings‐On‐Demand‐Mental‐Healthcare‐to‐14‐Million‐Cigna‐Behavioral‐Health‐Customers‐Nationwide. Published April 28, 2021. Accessed September 11, 2021.
- 12. Ginger US: Medical p.c . terms of service. Ginger.com. https://www.ginger.com/medical‐services‐terms‐of‐use. Published April 1, 2021. Accessed September 11, 2021.
- 13. Bryant B. Ginger plots course to grow value‐based business, break into Medicaid. Behavioral Health Business. https://bhbusiness.com/2021/04/09/ginger‐plots‐course‐to‐grow‐value‐based‐business‐break‐into‐medicaid/. Published April 9, 2021. Accessed September 11, 2021.
- 14. Ginger FAQ . Ginger.com . https://www.ginger.com/faq. Accessed September 11, 2021.
- 15. New Engl J Med. Catalyst . What is telehealth? https://catalyst.nejm.org/doi/full/10.1056/CAT.18.0268. Published online February 1, 2018. Accessed September 15, 2021.
- 16. Kvedar J, Coye MJ, Everett W. Connected health: a review of technologies and strategies to improve patient care with telemedicine and telehealth. Health Aff (Millwood). 2014;33(2):194‐199. 10.1377/hlthaff.2013.0992. [DOI] [PubMed] [Google Scholar]
- 17. Tuckson RV, Edmunds M, Hodgkins ML. Telehealth. New Engl J Med. 10/19/2017. 10.1056/NEJMsr1503323. 10.1056/NEJMsr1503323. [DOI] [PubMed]
- 18. Patel SY, Mehrotra A, Huskamp HA, Uscher‐Pines L, Ganguli I, Barnett ML. Variation in telemedicine use and outpatient care during the covid‐19 pandemic in the United States: study examines variation in total US outpatient visits and telemedicine use across patient demographics, specialties, and conditions during the covid‐19 pandemic. Health Aff (Millwood). 2021;40(2):349‐358. 10.1377/hlthaff.2020.01786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Dorsey ER, Topol EJ. State of telehealth. N Engl J Med. 2016;375(2):154‐161. 10.1056/NEJMra1601705. [DOI] [PubMed] [Google Scholar]
- 20. HHS Office for Civil Rights (OCR) . Notification of enforcement discretion for telehealth remote communications during the covid‐19 nationwide public health emergency. HHS.gov. https://www.hhs.gov/hipaa/for‐professionals/special‐topics/emergency‐preparedness/notification‐enforcement‐discretion‐telehealth/index.html. Published March 17, 2020. Accessed November 12, 2021.
- 21. Video conferencing, web conferencing, webinars, screen sharing. zoom. https://explore.zoom.us/en/healthcare/. Accessed October 15, 2021.
- 22. Telemedicine technology for health systems. Amwell. https://business.amwell.com/telemedicine‐solution‐hospitals/. Accessed October 15, 2021.
- 23. Adler‐Milstein J, Mehrotra A. Paying for digital health care—problems with the fee‐for‐service system. N Engl J Med. 2021;385(10):871‐873. 10.1056/NEJMp2107879. [DOI] [PubMed] [Google Scholar]
- 24. Digital Therapeutics Alliance Product Library . Digital therapeutics alliance. http://dtxalliance.org/understanding‐dtx/product‐library/. Accessed September 12, 2021.
- 25. Pear Therapeutics . reSET clinician information. https://2kw3qa2w17x12whtqxlb6sjc‐wpengine.netdna‐ssl.com/wp‐content/uploads/2019/08/PEAR‐MKT‐024‐reSET‐Clin‐Brief‐Sum_Dec2019.pdf. Published online 2019. Accessed September 12, 2019.
- 26. Livongo® . Virtual health management program and support. Livongo. https://www.livongo.com/. Accessed September 11, 2021.
- 27. Omada for Members . Our Approach. https://www.omadahealth.com/our‐approach/members. Published 2021. Accessed May 2, 2021.
- 28. Togetherall . A safe online community to support mental health. https://togetherall.com/en‐us/. Accessed September 13, 2021.
- 29. Bloom . CBT therapy & self‐care. App store. https://apps.apple.com/us/app/bloom‐cbt‐therapy‐self‐care/id1475128511. Accessed September 13, 2021.
- 30. Buoy Health . Symptom checker. https://www.buoyhealth.com/multi‐symptom‐checker. Accessed September 13, 2021.
- 31. Bicycle Health . How it works. https://www.bicyclehealth.com/how‐it‐works. Accessed September 12, 2021.
- 32. Firefly Health . Help—frequently asked questions. https://www.firefly.health/help. Accessed September 13, 2021.
- 33. Teladoc Health . Virtual care enablement & delivery. Teladoc. https://www.teladochealth.com/what‐we‐do/. Accessed September 13, 2021.
- 34. Teladoc Health Inc . 2020 Teladoc Health Inc. Annual report. https://s21.q4cdn.com/672268105/files/doc_financials/2020/ar/2020‐Annual‐Report‐(1).pdf. Published online December 31, 2021. Accessed September 13, 2021.
- 35. Poon SJ, Schuur JD, Mehrotra A. Trends in visits to acute care venues for treatment of low‐acuity conditions in the united states from 2008 to 2015. JAMA Intern Med. 2018;178(10):1342‐1349. 10.1001/jamainternmed.2018.3205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Ashwood JS, Mehrotra A, Cowling D, Uscher‐Pines L. Direct‐to‐consumer telehealth may increase access to care but does not decrease spending. Health Aff (Millwood). 2017;36(3):485‐491. 10.1377/hlthaff.2016.1130. [DOI] [PubMed] [Google Scholar]
- 37. Livongo Health, Inc . Form S‐1. https://www.sec.gov/Archives/edgar/data/1639225/000119312519185159/d731249ds1.htm. Published online December 9, 2019. Accessed September 12, 2021.
- 38. Sweeney E. Omada Health made its name with its technology. Now it's luring insurers with operational innovation. FierceHealthcare. https://www.fiercehealthcare.com/tech/omada‐health‐diabetes‐digital‐health‐operational‐innovation‐cigna‐bcbs‐minnesota‐sean‐duffy. Published September 12, 2018. Accessed September 13, 2021.
- 39. Lovett L. How digital therapeutic company Omada Health has taken a cue from life sciences. MobiHealthNews. https://www.mobihealthnews.com/news/north‐america/how‐digital‐therapeutic‐company‐omada‐health‐has‐taken‐cue‐life‐sciences. Published July 11, 2019. Accessed September 13, 2021.
- 40. Powell AC, Bowman MB, Harbin HT. Reimbursement of apps for mental health: findings from interviews. JMIR Ment Health. 2019;6(8):e14724. 10.2196/14724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Holmgren AJ, Downing NL, Tang M, Sharp C, Longhurst C, Huckman RS. Assessing the impact of the COVID‐19 pandemic on clinician ambulatory electronic health record use. J Am Med Inform Assoc. 2022;29(3):453‐460. 10.1093/jamia/ocab268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Tseng P, Kaplan RS, Richman BD, Shah MA, Schulman KA. Administrative costs associated with physician billing and insurance‐related activities at an academic health care system. JAMA. 2018;319(7):691. 10.1001/jama.2017.19148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Centers for Medicare & Medicaid Services . Revisions to payment policies under the physician fee schedule and other revisions to part b for CY 2019; Medicare shared savings program requirements; quality payment program; Medicaid promoting interoperability program; quality payment program‐extreme and uncontrollable circumstance policy for the 2019 MIPS payment year; provisions from the Medicare shared savings program‐accountable care organizations‐pathways to success; and expanding the use of telehealth services for the treatment of opioid use disorder under the substance use‐disorder prevention that promotes opioid recovery and treatment (SUPPORT) for patients and communities act. Federal Register. https://www.federalregister.gov/documents/2018/11/23/2018‐24170/medicare‐program‐revisions‐to‐payment‐policies‐under‐the‐physician‐fee‐schedule‐and‐other‐revisions#h‐81. Published November 23, 2018. Accessed September 11, 2021.
- 44. Mecklai K, Smith N, Stern AD, Kramer DB. Remote patient monitoring—overdue or overused? N Engl J Med. 2021;384(15):1384‐1386. 10.1056/NEJMp2033275. [DOI] [PubMed] [Google Scholar]
- 45. 100Plus . Remote patient monitoring devices. https://www.100plus.com/. Accessed September 11, 2021.
- 46. Frakt AB, Mayes R. Beyond capitation: how new payment experiments seek to find the “sweet spot” in amount of risk providers and payers bear. Health Aff (Millwood) . 2012;31(9):1951‐1958. 10.1377/hlthaff.2012.0344. [DOI] [PubMed] [Google Scholar]
- 47. Frank RG, Glazer J, McGuire TG. Measuring adverse selection in managed health care. J Health Econ. 2000;19(6):829‐854. 10.1016/S0167-6296(00)00059-X. [DOI] [PubMed] [Google Scholar]
- 48. Mechanic RE, Santos P, Landon BE, Chernew ME. Medical group responses to global payment: early lessons from the “alternative quality contract” in Massachusetts. Health Aff (Millwood). 2011;30(9):1734‐1742. 10.1377/hlthaff.2011.0264. [DOI] [PubMed] [Google Scholar]
- 49. Peikes D, Dale S, Ghosh A, et al. The comprehensive primary care initiative: effects on spending, quality, patients, and physicians. Health Aff (Millwood). 2018;37(6):890‐899. 10.1377/hlthaff.2017.1678. [DOI] [PubMed] [Google Scholar]
- 50. Dale SB, Ghosh A, Peikes DN, et al. Two‐year costs and quality in the comprehensive primary care initiative. N Engl J Med. 2016;374(24):2345‐2356. 10.1056/NEJMsa1414953. [DOI] [PubMed] [Google Scholar]
- 51. Burgette L, Liu J, Miller B, et al. Practice expense methodology and data collection research and analysis. Interim phase II report. RAND Corporation. https://www.rand.org. 2018. 10.7249/RR2166. Accessed September 12, 2021. [DOI]
- 52. Craig J. How to know if suboxone is right for you or a loved one. Bicycle Health. https://www.bicyclehealth.com/blog/how‐to‐know‐if‐suboxone‐is‐right‐for‐you‐or‐a‐loved‐one. Published January 7, 2021. Accessed September 12, 2021.
- 53. Ramsetty A, Adams C. Impact of the digital divide in the age of covid‐19. J Am Med Inform Assoc. 2020;27(7):1147‐1148. 10.1093/jamia/ocaa078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Chang JE, Lai AY, Gupta A, Nguyen AM, Berry CA, Shelley DR. Rapid transition to telehealth and the digital divide: implications for primary care access and equity in a post‐covid era. Milbank Q. 2021;99(2):340‐368. 10.1111/1468-0009.12509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Patel SY, Rose S, Barnett ML, Huskamp HA, Uscher‐Pines L, Mehrotra A. Community factors associated with telemedicine use during the covid‐19 pandemic. JAMA Network Open. 2021;4(5):e2110330. 10.1001/jamanetworkopen.2021.10330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Medicare Payment Advisory Commission . March 2021 report to the Congress: Medicare payment policy. 2021. https://medpac.gov/docs/default‐source/default‐document‐library/mar21_medpac_report_to_the_congress_secv2.pdf?sfvrsn=0. Accessed September 15, 2021.
- 57. Bates DW, Singh H. Two decades since To Err Is Human : an assessment of progress and emerging priorities in patient safety. Health Aff (Millwood). 2018;37(11):1736‐1743. 10.1377/hlthaff.2018.0738. [DOI] [PubMed] [Google Scholar]
- 58. Song Z, Kannan S, Gambrel RJ, et al. Physician practice pattern variations in common clinical scenarios within 5 US metropolitan areas. JAMA Health Forum. 2022;3(1):e214698. 10.1001/jamahealthforum.2021.4698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Omada Health . Frequently asked questions. https://www.omadahealth.com/frequently‐asked‐questions. Accessed September 11, 2021.
- 60. Omada Health . Terms of use. https://www.omadahealth.com/terms‐of‐use. Published February 1, 2017. Accessed September 13, 2021.
- 61. Livongo Health, Inc . Livongo blood glucose monitoring system section 510(k) premarket submission. https://www.accessdata.fda.gov/cdrh_docs/pdf20/K200277.pdf. Published online May 11, 2020. Accessed September 12, 2021.
- 62. Patient‐Centered Medical Home (PCMH) . NCQA. https://www.ncqa.org/programs/health‐care‐providers‐practices/patient‐centered‐medical‐home‐pcmh/. Accessed January 3, 2022.
- 63. Bestsennyy O, Gilbert G, Harris A, Rost J. Telehealth: a post‐covid‐19 reality? McKinsey. https://www.mckinsey.com/industries/healthcare‐systems‐and‐services/our‐insights/telehealth‐a‐quarter‐trillion‐dollar‐post‐covid‐19‐reality. Published July 9, 2021. Accessed September 15, 2021.


