Abstract
Background and Objectives
Breakdowns in clinician-family communication in neurologic intensive care units (neuroICUs) are common, particularly for goals-of-care decisions to continue or withdraw life-sustaining treatments while considering long-term prognoses. Shared decision-making interventions (decision aids [DAs]) may prevent this problem and increase patient-centered care, yet none are currently available. We assessed the feasibility, acceptability, and perceived usefulness of a DA for goals-of-care communication with surrogate decision makers for critically ill patients with severe acute brain injury (SABI) after hemispheric acute ischemic stroke, intracerebral hemorrhage, or traumatic brain injury.
Methods
We conducted a parallel-arm, unblinded, patient-level randomized, controlled pilot trial at 2 tertiary care US neuroICUs and randomized surrogate participants 1:1 to a tailored paper-based DA provided to surrogates before clinician-family goals-of-care meetings or usual care (no intervention before clinician-family meetings). The primary outcomes were feasibility of deploying the DA (recruitment, participation, and retention), acceptability, and perceived usefulness of the DA among surrogates. Exploratory outcomes included outcome of surrogate goals-of-care decision, code status changes during admission, patients' 3-month functional outcome, and surrogates' 3-month validated psychological outcomes.
Results
We approached 83 surrogates of 58 patients and enrolled 66 surrogates of 41 patients (80% consent rate). Of 66 surrogates, 45 remained in the study at 3 months (68% retention). Of the 33 surrogates randomized to intervention, 27 were able to receive the DA, and 25 subsequently read the DA (93% participation). Eighty-two percent rated the DA's acceptability as good or excellent (median acceptability score 2 [IQR 2–3]); 96% found it useful for goals-of-care decision making. In the DA group, there was a trend toward fewer comfort care decisions (27% vs 56%, p = 0.1) and fewer code status changes (no change, 73% vs 44%, p = 0.02). At 3 months, fewer patients in the DA group had died (33% vs 69%, p = 0.05; median Glasgow Outcome Scale 3 vs1, p = 0.05). Regardless of intervention, 3-month psychological outcomes were significantly worse among surrogates who had chosen continuation of care.
Discussion
A goals-of-care DA to support ICU shared decision making for patients with SABI is feasible to deploy and well perceived by surrogates. A larger trial is feasible to conduct, although surrogates who select continuation of care deserve additional psychosocial support.
Clinical Trials Registration
Classification of Evidence
This study provides Class IV evidence that the use of a DA explaining the goals-of-care decision and the treatment options is acceptable and useful to surrogates of incapacitated critically ill patients with ischemic stroke, intracerebral hemorrhage, or traumatic brain injury.
Every 30 seconds, an adult patient in the United States has a severe acute brain injury (SABI) from traumatic brain injury or large ischemic or hemorrhagic stroke, resulting in 200,000 deaths and nearly 1 million survivors living with disability annually.1,2 Routinely in intensive care units (ICUs), surrogate decision makers (surrogates) for these incapacitated patients make difficult goals-of-care decisions to continue or withdraw life-sustaining treatments while considering long-term prognoses. However, breakdowns in clinician-family communication are common in ICUs and can result in poorly informed treatment decisions incongruent with patients' wishes, psychological distress in surrogates, and utilization of expensive, burdensome treatments.3-9
Shared decision-making tools (decision aids [DAs]) have been shown to improve the quality of patients' decisions in a variety of diseases.10-13 Yet, no easily scalable, efficacious DAs exist to help surrogates of patients with SABI in ICUs manage and prepare for goals-of-care decisions by providing surrogates with an appropriate amount of balanced information.14 With input from key stakeholders, we have developed a low-cost, tailored, paper-based DA for surrogates of critically ill patients with SABI, conceptually grounded in the Ottawa Decision Support Framework of Shared Decision-Making,15 to enhance clinician-family goals-of-care communication.16,17 Our DA achieved has excellent acceptability and usability ratings among families recruited from neuroscience-ICU (neuroICU) waiting rooms16,17; however, these ratings so far have been based on families envisioning their use of the DA for hypothetical goals-of-care decisions.
As a next step, we conducted a pilot randomized clinical trial enrolling surrogates making real-life goals-of-care decisions for patients with SABI. The primary objective was to assess the feasibility of recruiting participants relatively early after neuroICU admission and to measure acceptability and perceived usefulness by surrogates. We also tested whether we could successfully retain surrogates in the trial for follow-up 3 months after the decision for the purposes of several exploratory patient and surrogate outcomes.
Methods
Study Design
Between February 2018 and March 2020, we conducted a parallel-arm, unblinded, patient-level randomized, controlled pilot trial comparing the use of a paper-based DA before initial clinician-family goals-of-care meetings (intervention) to usual care (no intervention before clinician-family meeting). We conducted the study in the respective neuroICUs of 2 academic tertiary care centers in the US Northeast.
Standard Protocol Approvals, Registrations, and Patient Consents
The University of Massachusetts Chan Medical School (UMMS) Institutional Review Board ([IRB] approval number H00004724/H00015764) and the Yale Human Research Protection Program (approval number HIC 2000024430) approved the study. The study was conducted in Good Clinical Practice compliance (Clinicaltrials.gov NCT03833375). There was an unintentional delay for this study's registration on ClinicalTrials.gov due to an initial misunderstanding regarding whether pilot clinical trials of nonbiologic interventions require such registration. Before enrolling the first study patient, the principal investigator (S.M.) reviewed a standard checklist on ClinicalTrials.gov, which suggested that only trials of drugs, biological products, or devices were required to register (question 3).18 NIH funding for the trial had been approved in 2015 without a requirement for ClinicalTrials.gov registration at the time of the funding decision. The first patient was enrolled at UMMS on 2/11/2018, after full UMMS IRB approval. Because of evolving NIH definitions of a clinical trial even for pilot trials, coinciding with the decision to expand the trial to 2 centers (UMMS and Yale) in early 2019, the UMMS IRB advised the PI at that time to register the trial on ClinicalTrials.gov. The trial was then registered on 2/7/2019 before the study expanded to 2 centers. Only 16 participants (of an eventual 66) had been enrolled in the study at UMMS before registration. With approval from our IRBs, we obtained verbal consent from each patient's legally authorized representative, all participating surrogates, and clinicians.
Participants
We screened all admissions to the participating neuroICUs during the study period for patients with hemispheric acute ischemic stroke (AIS), primary intracerebral hemorrhage (ICH), or nonpenetrating traumatic brain injury (TBI). Eligible participants included surrogates of incapacitated patients with these diagnoses who were aged ≥18 years, had been hospitalized for ≥3 days, were judged by their clinicians to be critically ill—defined as either mechanically ventilated likely requiring tracheostomy or dysphagic likely requiring a percutaneous endoscopic gastrostomy (PEG)—and who had not yet participated in a formal goals-of-care discussion about tracheostomy and/or PEG, the likely post-ICU discharge destination, and long-term prognosis. We allowed for multiple surrogates to be enrolled per patient. We excluded surrogates if they were illiterate or non–English speaking. We also enrolled the clinician leading the goals-of-care meeting.
Randomization, Study Groups, and Intervention
We randomized surrogates at the patient level to the intervention or control group via the free online random list sequence generator RANDOM.ORG, using block randomization in blocks of 4 stratified by site. Allocations were placed in sealed envelopes in sequential order.
As previously published,16,17 the DA is a thin spiral-bound booklet at a 6th grade reading-level explaining the goals-of-care decision and the treatment options of survival—including descriptions and photographs of tracheostomy, PEG, and post-ICU care options (long-term acute care hospital, rehab hospital, and nursing home)—or comfort-based care. For each patient, it includes an individualized icon array of estimated 6-month (TBI) or 12-month outcome (ICH and AIS) based on carefully selected and validated hemispheric AIS, ICH, or TBI prediction models, which predict outcome at these time points using mostly admission variables. The DA also includes explicit explanations of the uncertainty of the depicted outcome and a list of variables that may additionally affect outcome but are not included in the prediction model,19,20 with a recommendation to ask the patient's physician about their prognostication and level of uncertainty. A 1-page worksheet—meant to be completed by the surrogate and subsequently brought to the goals-of-care meeting—prompts the surrogate to reflect on patient values and preferences, assess decision readiness and treatment leaning, and note questions for the clinician-family meeting.16,17 The DA was created using a systematic, iterative process with stakeholder input from families and physicians16,17 and is conceptually grounded.15,21
Trained research assistants provided a technical orientation of the DA to the intervention group surrogates without any mention of medical information and reminded them to complete the worksheet and bring it to their upcoming goals-of-care meeting with the clinical team. If the worksheet was not completed or brought to the meeting, research staff provided an empty worksheet to surrogates, who were encouraged but not required to complete it right before the meeting. Research staff also shared with the clinician a copy of the DA's prognostication icon array before each meeting.
Control surrogates received usual care without a DA. Before their goals-of-care meetings, control participants received 2 pages of printed materials from the American Stroke Association22 (for AIS and ICH) or the Centers for Disease Control23 (for TBI) containing general disease information without information about goals-of-care decision making.
Variables and Data Collection
We collected surrogates' basic demographic information on study enrollment, including numeracy and health literacy. For patients, in addition to demographic data, diagnoses, and standard measures of SABI severity, we collected preexisting code status, preexisting conditions, and ICU complications. At the time of the clinician-family meeting, when it was clear which clinician would be leading the meeting, we collected clinicians' demographics and work experience information.
Primary Outcomes
The primary objective was to assess feasibility of conducting a randomized DA trial in neuroICUs. The other primary objective was to measure acceptability and perceived usefulness of the DA for goals-of-care decision making among surrogates. To assess feasibility, we measured in both groups the number of eligible participants during the screening period, the proportion who agreed to participate (recruitment), and the proportion who completed exploratory outcome assessments, both after the family meeting and at subsequent 3-month phone follow-up (retention). To assess feasibility of using the DA, we also measured in the intervention group the proportion of surrogates who read the DA in full (both via self-report and responses to acceptability questions) and completed the worksheet (participation). We monitored for adverse events, defined as experiencing severe emotional distress from exposure to the DA so that surrogates were unwilling to continue in the study.
We measured intervention surrogates' DA acceptability using the validated Acceptability Scale.24 The scale includes 9 initial items that ask the respondent to rate, on a 4-point Likert scale, the way specific information is presented in the DA regarding the goals-of-care decision. It also contains 7 additional multiple-choice questions assessing perceived length, amount and balance of information, usefulness of the tool for goals-of-care decision making, helpfulness of the worksheet, and comprehensibility of the prognostication page. Two open-ended questions assessed what surrogates liked about the DA or suggested for improvements.
Exploratory Outcomes
Our multiple exploratory outcomes included final goals-of-care decision, code status changes during ICU admission, and 3-month functional outcomes among patients; validated measures of psychological outcomes, knowledge outcomes, and decision quality among surrogates at various study time points; and validated measures of clinician-family prognostic concordance after the goals-of-care meeting. The full study protocol is available in the Supplement.
Sample Size Calculation and Statistical Analyses
Per recommendations for sample size calculations for pilot studies, we based our sample size of 40 patients and their surrogates on the necessities for examining feasibility.25,26 We analyzed our primary feasibility outcomes using standard descriptive statistics. For the Acceptability Scale, we determined the overall percentages of each Likert scale response among all possible Likert responses to the initial 9 questions regarding the way specific information about the goals-of-care decision was presented in the DA. For the 7 additional multiple-choice questions in the Acceptability Scale, we dichotomized outcomes as favorable and unfavorable. In accordance with our previous studies, we targeted a minimum of >70% favorable responses as good acceptability, because our review of the literature did not reveal other accepted cutoffs.16,17 We grouped surrogates' qualitative responses about the DA by positive comments about the DAs and suggestions for improvement.
We assessed trends toward group differences in the exploratory outcomes by comparing categorical, non-normally distributed measures (Wilcoxon rank tests or Fisher exact tests) and continuous, normally distributed measures (2-sample t tests) according to intention to treat. We conducted 2 additional post hoc analyses: (1) per-protocol analysis of selected patient and 3-month surrogate outcomes, in which surrogates who had not read the DA and completed the worksheet were excluded; and (2) stratification of 3-month surrogate outcomes by goals-of-care decision, independent of group allocation. The statistical analysis plan for the exploratory outcomes is available in the Supplement. All analyses were performed using SAS© 9.4 (SAS Institute Inc., Cary, NC).
Data Availability
Anonymized data not published within this article will be made available by request from any qualified investigator. Requests should be made to susanne.muehlschlegel@umassmed.edu.
Results
Primary Outcomes
Recruitment
We approached 83 surrogates of 58 patients, of whom we enrolled 41 patients (71%) and 66 surrogates (1.6 surrogates per patient; 80% consent rate). Randomization resulted in 33 surrogates of 20 patients in the intervention (DA) group and 33 surrogates of 21 patients in the control group (Figure 1).
Figure 1. CONSORT Diagram.
Shown are the number of screened, recruited, and analyzed study participants and reasons for exclusion.
Table 1 summarizes the characteristics of enrolled surrogates and patients. Treatment groups were balanced regarding surrogate and patient characteristics. Additional details regarding patient and clinician characteristics are shown in eTables 1 and 2, links.lww.com/WNL/C199.
Table 1.
Surrogate and Patient Characteristics by Intervention Group

Participation in Intervention Arm
Of the 33 surrogates randomized to intervention, 6 surrogates did not receive the DA for various reasons (Figure 1). Of the 27 surrogates who received the DA, 25 (93%) read the DA, and 20 (74%) completed the worksheet.
Study Retention
The surrogate retention rate at 3 months was 70% for the intervention group and 67% for the control group (combined 68%). Reasons for nonretention are shown in Figure 1.
Acceptability and Perceived Usefulness
One surrogate randomized to intervention did not complete the Acceptability Scale (missing data). Of the remaining surrogates, most (82%) rated the presentation of information related to the goals-of-care decision in the DA as good (56%) or excellent (26%; Figure 2 multicolor bar; median acceptability score 2 [IQR 2–3], where 0 poor to 3 excellent). All additional items on the Acceptability Scale were rated favorably by 75%–96% of surrogates (Figure 2; blue bars). Of note, 96% found the DA useful when making the goals-of-care decision in their family member. Table 2 summarizes the qualitative feedback about the DA.
Figure 2. Acceptability Data.
(A) The multicolor bar represents a composite of 9 questions related to the acceptability of the content of the DA as rated by the surrogates randomized to intervention. (B) The light blue bars represent favorable responses related to additional specific questions about the DA. Favorable was defined as just right for the length of the DA and amount of information; balanced for the presentation of the decision options; yes on DA usefulness for making goals-of-care decisions; easy to understand the different potential outcomes on the way prognosis was explained; easier on how the tester thought the DA helped with making the decision; and yes on enough information for surrogates to decide on goals of care for the patient. DA = decision aid.
Table 2.
Qualitative Results During Acceptability Testing Among Intervention Surrogates
Exploratory Outcomes
Patient Outcomes
eTables 3 and 4, links.lww.com/WNL/C199, summarize all exploratory patient outcomes. There was a trend toward fewer patients in the DA group transitioning to comfort care only (4 [27%] vs 9 [56%]; p = 0.1). Significantly fewer patients in the DA group had their code status changed compared with the control group (no code status change, 11 [73%] vs 7 [44%]; p = 0.02). When including only those 16 patients whose surrogates had previously both read the DA and completed the worksheet, a trend toward fewer code status changes in the intervention group (p = 0.08), and differences in the final goals-of-care decision (p = 0.11) remained. There was no difference in the time to clinician-family meeting, total number of meetings, and duration of meetings (eTable 3, links.lww.com/WNL/C199).
At 3 months, a smaller proportion of patients in the DA group had died (5 [33%] vs 11 [69%]; p = 0.05), with survivors living with severe disability (median Glasgow Outcome Scale 3 vs 1; p = 0.05). No differences in ICU or hospital length-of-stay or ventilation days were found (eTable 4, links.lww.com/WNL/C199).
Surrogate Outcomes
All exploratory surrogate outcomes are shown in eTables 5–8, links.lww.com/WNL/C199. At 3 months, the mean Hospital Anxiety and Depression Scale (HADS; 18 [SD 11] vs 11 [7.6]; p = 0.01) and Impact of Events Scale–Revised (IES-R, a measure of posttraumatic stress disorder or PTSD; 32 [18] vs 21 [15]; p = 0.04; eTable 5, links.lww.com/WNL/C199) scores were worse in the DA group compared with the control group, whose means had decreased from earlier time points. This between-group difference also remained in the per-protocol analysis including only those 16 intervention arm surrogates who completed the worksheet and were retained at 3 months Overall, regardless of intervention vs control group allocation, 3-month surrogate HADS was significantly worse among families of patients who survived compared with those who had been made comfort measures, with a similar trend for IES-R (eTable 6, links.lww.com/WNL/C199).
Also at 3 months, decision regret was low in both groups but trended higher in intervention surrogates (median decision regret 15 [IQR 5–35] vs 5 [IQR 0–15] on a 100-point scale; p = 0.09), with the same trend persisting in the per-protocol analysis (eTable 7, links.lww.com/WNL/C199). There was no difference in the clinician-surrogate prognostic concordance scores, except when each dyad was asked about patient's survival of the hospitalization, where prognostic discordance was higher in the intervention group (eTable 8, links.lww.com/WNL/C199).
Classification of Evidence
This study provides Class IV evidence that the use of a DA explaining the goals-of-care decision and the treatment options is acceptable and useful to surrogates of incapacitated critically ill patients with ischemic stroke, ICH, or TBI.
Discussion
We found both that it was feasible to conduct a randomized trial of a goals-of-care DA during the care of critically ill patients with SABI with successful post-ICU follow-up and that surrogates rated the tool as highly acceptable and useful in making goals-of-care decisions. Our exploratory outcomes suggest that surrogates in the DA arm were less likely to change patient code status and that surrogates who do ultimately select continuation of care for their family members are at a higher risk of adverse 3-month psychological outcomes.
Although other DAs have been designed for surrogates of general ICU patients to complete after a patient has undergone prolonged mechanical ventilation (i.e., ≥5–10 days)27,28 or for surrogates of patients with stroke alone,29 our DA was tailored for all 3 of the most common types of SABI in neuroICUs and as such was designed with the option of being used as soon as 72 hours following admission. Before this study, it was unclear whether surrogates would even accept using a DA amidst the unique stress of a neuroICU environment. Our study confirms that the DA is not only acceptable but that surrogates nearly unanimously perceive it to be useful. Although 93% of intervention surrogates read the DA, 74% completed the worksheet; this suggests that although it is indeed feasible for surrogates to use a DA before family meetings, maximizing the proportion of families who complete the worksheet will require staff education and championing.
We acknowledge that the finding of fewer patient code status limitations among the intervention group in our exploratory analyses may potentially have in part been a result of the DA content. Our DA heavily prompts surrogates to consider patients' values and preferences when making decisions and to focus on the principles of substituted judgment.30 We believe that the purpose of the DA is not to proactively steer surrogates toward or away from comfort measures but to reduce common biases and promote patient-centered decisions.30-32 Notably, decision regret was quite low in both groups, with the observed minimal differences likely being clinically not meaningful.
The persistence of high levels of depression, anxiety, and PTSD in the intervention arm surrogates at 3 months compared with a decline in control arm surrogates may partly be due to the DA itself, although it is more likely due to higher levels of psychological distress in caregivers of ICU survivors that has been previously described.33-35 This suggests that a goals-of-care DA for patients with SABI may potentially need to be coupled with an intervention to also prevent chronic emotional distress in families of ICU survivors.36,37 Similar to a large DA trial in ICU patients with prolonged ventilation,27 the exploratory results of this pilot study also did not detect a consistent, reliable effect of the DA on clinician-surrogate prognostic concordance.38,39 Only when asked specifically about patient's chance of surviving the hospitalization were clinicians actually more optimistic than surrogates in the DA group, a finding contrary to previous literature.38 Given the finding is also contrary to our data from the other prognostic discordance questions in this study, we hypothesize that it is possibly a byproduct of multiple comparisons in a limited data set.
Our feasibility study and intervention have several limitations. We enrolled a predominantly non-Hispanic White patient and surrogate population from the US East Coast limiting generalizability. Our intervention was paper based, which, compared with web-based tools, is less portable and shareable among family members when geographically distant. Digital DAs allow integration of videos to reach lower-literacy surrogates.40,41 We are currently converting our DA into a digital DA for future use. We did not track how many surrogates required reminders by research staff to complete the worksheet and did not audio-record the clinician-family meetings, limiting us from further exploring how well the DA content was directly integrated into family meetings. For this pilot study, we did not include a direct measure of caregiver burden, an important confounder in the context of our exploratory 3-month surrogate psychological outcomes. We did not conduct a qualitative exploration of surrogates' values and reasons for choosing a specific goals-of-care decision owing to budget limitations and the need to balance participant burden. We did not adjust for clustering of clinicians leading the family meetings; sample sizes were small, and groups were dependent because some physicians cared for patients in both treatment groups. Future studies will need to factor in this clustering when estimating sample sizes.
We successfully demonstrated feasibility and high acceptability of our paper-based goals-of-care DA for surrogates of patients with SABI in neuroICUs. Although additional psychosocial support of surrogates during and following goals-of-care decisions—especially for those surrogates who choose prolonged survival for patients—would likely need to be considered as part of future study design, our data support proceeding with an appropriately powered randomized trial to assess the efficacy of our goals-of-care DA on patient, family, and health care utilization outcomes.
Acknowledgment
The authors thank the families, patients, and clinicians who participated and the bedside staff at both study sites. They also thank Douglas B. White, MD, MAS, for his advice on our research (named with permission).
Glossary
- AIS
acute ischemic stroke
- DA
decision aid
- HADS
Hospital Anxiety and Depression Scale
- ICH
intracerebral hemorrhage
- ICU
intensive care unit
- IES-R
Impact of Events Scale–Revised
- IRB
Institutional Review Board
- neuroICU
neuroscience-ICU
- PEG
percutaneous endoscopic gastrostomy
- SABI
severe acute brain injury
- TBI
traumatic brain injury
- UMMS
University of Massachusetts Chan Medical School
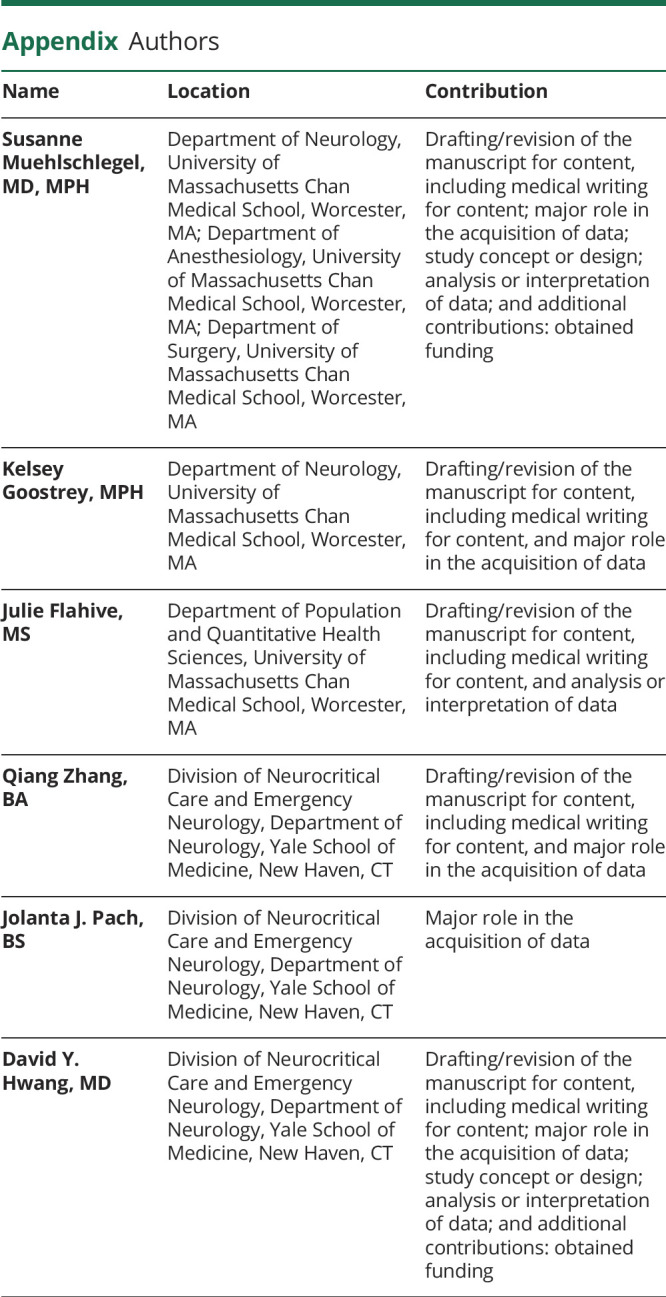
Appendix. Authors
Footnotes
Editorial, page 593
Class of Evidence: NPub.org/coe
Study Funding
This study was funded by NIH/NICHD grant 5K23HD080971 (PI: S. Muehlschlegel) and philanthropic funds from the Apple Pickers Foundation, Westerly, RI (D.Y. Hwang). This project was additionally supported by the University of Massachusetts Medical School Center for Clinical and Translational Science, which is funded by the NIH Clinical and Translational Science Award to the University of Massachusetts Medical School (UL1TR000161).
Disclosure
The authors report no relevant disclosures. Go to Neurology.org/N for full disclosures.
References
- 1.Center for Disease Control. Stroke facts [online]. Accessed January 10, 2021. cdc.gov/stroke/facts.htm.
- 2.Centers for Disease Control and Prevention. Get the facts: TBI data [online]. Accessed September 9, 2021. cdc.gov/traumaticbraininjury/data/index.html.
- 3.Lynn J, Teno JM, Phillips RS, et al. Perceptions by family members of the dying experience of older and seriously ill patients. SUPPORT Investigators. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments. Ann Intern Med. 1997;126(2):97-106. [DOI] [PubMed] [Google Scholar]
- 4.Anderson WG, Arnold RM, Angus DC, Bryce CL. Posttraumatic stress and complicated grief in family members of patients in the intensive care unit. J Gen Intern Med. 2008;23(11):1871-1876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Azoulay E, Chevret S, Leleu G, et al. Half the families of intensive care unit patients experience inadequate communication with physicians. Crit Care Med. 2000;28(8):3044-3049. [DOI] [PubMed] [Google Scholar]
- 6.Azoulay E, Pochard F, Kentish-Barnes N, et al. , FAMIREA Study Group. Risk of post-traumatic stress symptoms in family members of intensive care unit patients. Am J Respir Crit Care Med. 2005;171(9):987-994. [DOI] [PubMed] [Google Scholar]
- 7.Wendler D, Rid A. Systematic review: the effect on surrogates of making treatment decisions for others. Ann Intern Med. 2011;154(5):336-346. [DOI] [PubMed] [Google Scholar]
- 8.White DB, Engelberg RA, Wenrich MD, Lo B, Curtis JR. Prognostication during physician-family discussions about limiting life support in intensive care units. Crit Care Med. 2007;35(2):442-448. [DOI] [PubMed] [Google Scholar]
- 9.Quinn T, Moskowitz J, Khan MW, et al. What families need and physicians deliver: contrasting communication preferences between surrogate decision-makers and physicians during outcome prognostication in critically ill TBI patients. Neurocrit Care. 2017;27(2):154-162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stacey D, Legare F, Lewis K, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2017;4:CD001431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stacey D, Legare F, Lewis KB. Patient decision aids to engage adults in treatment or screening decisions. JAMA. 2017;318(7):657-658. [DOI] [PubMed] [Google Scholar]
- 12.Ankolekar A, Dekker A, Fijten R, Berlanga A. The benefits and challenges of using patient decision aids to support shared decision making in health care. JCO Clin Cancer Inform. 2018;2:1-10. [DOI] [PubMed] [Google Scholar]
- 13.Barry MJ, Edgman-Levitan S. Shared decision making: pinnacle of patient-centered care. N Engl J Med. 2012;366(9):780-781. [DOI] [PubMed] [Google Scholar]
- 14.Muehlschlegel S, Shutter L, Col N, Goldberg R. Decision aids and shared decision-making in neurocritical care: an unmet need in our NeuroICUs. Neurocrit Care. 2015;23(1):127-130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.O'Connor AM. Ottawa decision support Framework [online]. Accessed January 1, 2021. decisionaid.ohri.ca/docs/develop/ODSF.pdf.
- 16.Muehlschlegel S, Hwang DY, Flahive J, et al. Goals-of-care decision aid for critically ill patients with TBI: development and feasibility testing. Neurology. 2020;95(2):e179-e193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Goostrey KJ, Jones K, Lee C, et al. Adapting a traumatic brain injury goals-of-care decision aid for critically ill patients to intracerebral hemorrhage and hemispheric acute ischemic stroke. Crit Care Explor. 2021;3:e0357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Clinicaltrials.gov. Checklist for Evaluating whether a Clinical Trial or Study Is an Applicable Clinical Trial (ACT) under 42 CFR 11.22(b) for Clinical Trials Initiated on or After January 18, 2017 [online]. Accessed 11 28, 2021. prsinfo.clinicaltrials.gov/ACT_Checklist.pdf. [Google Scholar]
- 19.Evans LR, Boyd EA, Malvar G, et al. Surrogate decision-makers' perspectives on discussing prognosis in the face of uncertainty. Am J Respir Crit Care Med. 2009;179(1):48-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jones K, Quinn T, Mazor KM, Muehlschlegel S. Prognostic uncertainty in critically ill patients with traumatic brain injury: a multicenter qualitative study. Neurocrit Care. 2021;35(2):311-321. [DOI] [PubMed] [Google Scholar]
- 21.Legare F, O'Connor AM, Graham ID, Wells GA, Tremblay S. Impact of the Ottawa Decision Support Framework on the agreement and the difference between patients' and physicians' decisional conflict. Med Decis Making. 2006;26(4):373-390. [DOI] [PubMed] [Google Scholar]
- 22.American stroke association patient stroke education handout [online]. Accessed January 10, 2021. strokeassociation.org/-/media/stroke-files/stroke-resource-center/prevention/patient-education-handout-ucm_452860.pdf?la=en&hash=7D0FA4B95B1499BC0B05DFEE1B44C98A402993B4.
- 23.Traumatic brain injury statistics get the facts [online]. Accessed April 2, 2021. cdc.gov/traumaticbraininjury/get_the_facts.html.
- 24.O'Connor AM, Cranney A. Acceptability scale [online]. Accessed January 10, 2021. decisionaid.ohri.ca/eval_accept.html.
- 25.Leon AC, Davis LL, Kraemer HC. The role and interpretation of pilot studies in clinical research. J Psychiatr Res. 2011;45(5):626-629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kraemer HC, Mintz J, Noda A, Tinklenberg J, Yesavage JA. Caution regarding the use of pilot studies to guide power calculations for study proposals. Arch Gen Psychiatry. 2006;63(5):484-489. [DOI] [PubMed] [Google Scholar]
- 27.Cox CE, White DB, Hough CL, et al. Effects of a personalized web-based decision aid for surrogate decision makers of patients with prolonged mechanical ventilation: a randomized clinical trial. Ann Intern Med. 2019;170(5):285-297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Suen AO, Butler RA, Arnold RM, et al. A pilot randomized trial of an interactive web-based tool to support surrogate decision-makers in the ICU. Ann Am Thorac Soc. 2020;18(7):1191-1201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chen EP, Arslanian-Engoren C, Newhouse W, et al. Development and usability testing of understanding stroke, a tailored life-sustaining treatment decision support tool for stroke surrogate decision makers. BMC Palliat Care. 2020;19(1):110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kon AA, Davidson JE, Morrison W, Danis M, White DB, American College of Critical Care Medicine, American Thoracic Society. Shared decision making in ICUs: an American college of critical care medicine and American thoracic society policy statement. Crit Care Med. 2016;44(1):188-201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Creutzfeldt CJ, Holloway RG. Treatment decisions after severe stroke: uncertainty and biases. Stroke. 2012;43(12):3405-3408. [DOI] [PubMed] [Google Scholar]
- 32.Holloway RG, Benesch CG, Burgin WS, Zentner JB. Prognosis and decision making in severe stroke. JAMA. 2005;294(6):725-733. [DOI] [PubMed] [Google Scholar]
- 33.Meyers EE, Presciutti A, Shaffer KM, et al. The impact of resilience factors and anxiety during hospital admission on longitudinal anxiety among dyads of neurocritical care patients without major cognitive impairment and their family caregivers. Neurocrit Care. 2020;33(2):468-478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Beesley SJ, Hirshberg EL, Wilson EL, et al. Depression and change in caregiver burden among family members of intensive care unit survivors. Am J Crit Care. 2020;29(5):350-357. [DOI] [PubMed] [Google Scholar]
- 35.Kreitzer N, Bakas T, Kurowski B, et al. The experience of caregivers following a moderate to severe traumatic brain injury requiring ICU admission. J Head Trauma Rehabil. 2020;35(3):E299–E309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dionne-Odom JN, White DB. Reconceptualizing how to support surrogates making medical decisions for critically ill patients. JAMA. 2021;325(21):2147-2148. [DOI] [PubMed] [Google Scholar]
- 37.Vranceanu AM, Bannon S, Mace R, et al. Feasibility and efficacy of a resiliency intervention for the prevention of chronic emotional distress among survivor-caregiver dyads admitted to the neuroscience intensive care unit: a randomized clinical trial. JAMA Netw Open. 2020;3(10):e2020807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zier LS, Sottile PD, Hong SY, Weissfield LA, White DB. Surrogate decision makers' interpretation of prognostic information: a mixed-methods study. Ann Intern Med. 2012;156(5):360-366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lee Char SJ, Evans LR, Malvar GL, White DB. A randomized trial of two methods to disclose prognosis to surrogate decision makers in intensive care units. Am J Respir Crit Care Med. 2010;182(7):905-909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Barclay PA, Bowers CA. Design for the illiterate: a scoping review of tools for improving the health literacy of electronic health resources. Proc Hum Factors Ergon Soc Annu Meet. 2017;61:545-549. [Google Scholar]
- 41.Arcia A, Suero-Tejeda N, Bales ME, et al. Sometimes more is more: iterative participatory design of infographics for engagement of community members with varying levels of health literacy. J Am Med Inform Assoc. 2016;23(1):174-183. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Anonymized data not published within this article will be made available by request from any qualified investigator. Requests should be made to susanne.muehlschlegel@umassmed.edu.





