Abstract
Cesarean scar ectopic pregnancy (CSEP) is rare, occurring in 1:1800 to 1:2625 pregnancies. It is classified into two types: endogenous, which grows inside the uterine cavity; and exogenous, which grows outward, toward the bladder. Both types are associated with increased maternal morbidity and mortality. The case report describes a 25-year-old woman with a viable first-trimester CSEP treated with both methotrexate and operative resection. Management was in a low-resource setting.
Keywords: Cesarean scar pregnancy, Ectopic pregnancy, Low-resource setting, Viable ectopic pregnancy
Highlights
-
•
Cesarean scar ectopic pregnancy (CSEP) is rare.
-
•
We report the management of a viable first-trimester CSEP in a low-resource setting.
-
•
Management involved methotrexate followed by operative resection with laparotomy.
1. Introduction
Cesarean scar ectopic pregnancy (CSEP) occurs when an early pregnancy implants in the scar from a previous cesarean section. Its prevalence is estimated to range from 1:1800 to 1:2656 pregnancies [1].
There are two types of CSEP: endogenous and exogenous [1,2]. Endogenous grows into the uterine cavity and has the potential to reach viable gestation but with risk of placenta accreta and major obstetric hemorrhage. Exogenous grows outward, toward the bladder, and has the potential for scar rupture and intra-abdominal bleeding. Both types are associated with increased maternal morbidity and mortality. Hence early diagnosis is crucial.
Here, we present the case of a 25-year-old woman with a known viable first-trimester CSEP refractory to medical treatment thus requiring surgical management. This case report has been drafted under the CARE guidelines [3].
2. Case Presentation
A 25-year-old woman with 6 weeks of amenorrhea presented to the department of obstetrics and gynecology complaining of vaginal bleeding for 1 day and lower abdominal pain for 5 days. She had previously attended a local clinic where a viable CSEP had been diagnosed. She was treated with a single dose of methotrexate, intramuscularly in the local clinic, and then was referred to the department of obstetrics and gynecology.
The patient's obstetrical history included two cesarean sections due to fetal distress. She was para 2 + 1 (ectopic). General examination revealed no positive findings. Abdominal examination revealed tenderness at the left side of the cesarean section scar. On speculum examination, the cervix was normal, with no discharge or bleeding. On bimanual examination, the cervix was pointed upwards, the uterus was bulky and there was no adnexal tenderness.
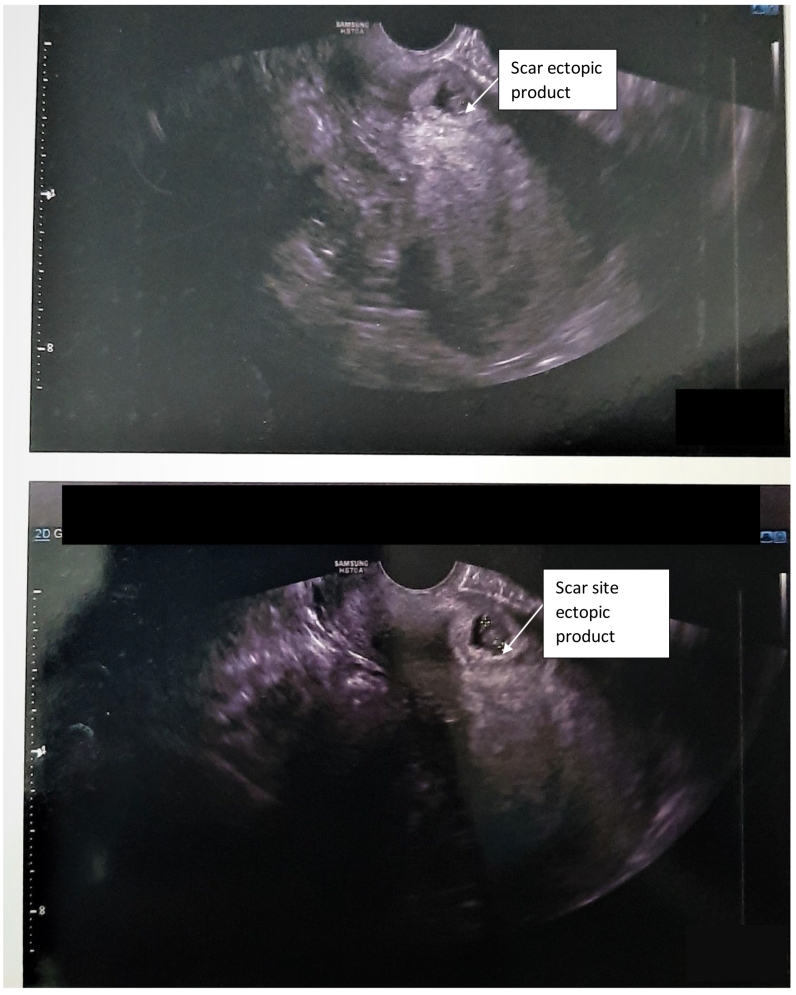
On investigation, the patient's blood and urine profiles were all within the normal limits except for slight anemia (10 g/dl). Beta-HCG level was 1100 mIU/ml, corresponding to the level of the 4th week. Transvaginal 4D sonography showed a 6 mm sac within the cesarean section scar with a positive fetal heartbeat. 3D ultrasonography showed a bulky uterus (123 × 47 × 56 mm) and anteverted in position with a thin myometrium (<3 mm). A diagnosis of a viable first-trimester CSEP was made [Fig. 1].
Fig. 1.
Transvaginal 4D ultrasonogaph (TVS) showing Cesarean scar ectopic pregnancy (CSEP).
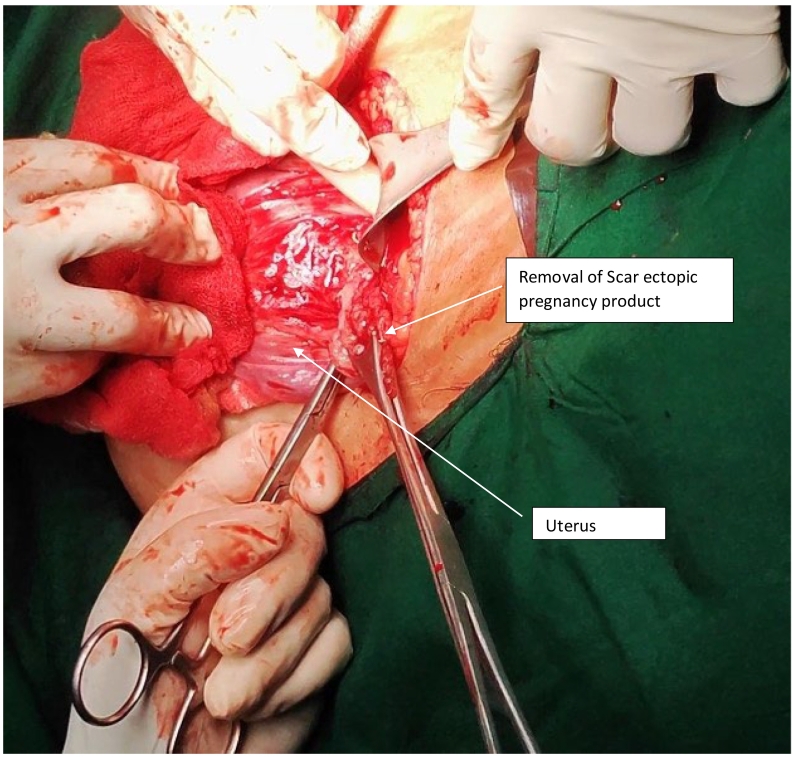
Operative resection with laparotomy was undertaken. An incision was made over the bulge. Intraoperative findings were a soft and vascular mass at the site of previous scar mark [Fig. 2]. Products communicating with the uterine cavity were removed. The tissue was sent for histopathological examination and the diagnosis of CSEP was confirmed.
Fig. 2.
Laparotomy showing resection of ectopic pregnancy.
3. Discussion
Viable CSEP is uncommon; it generally presents in the first trimester. Signs and symptoms vary according to the severity and duration of the condition [1]. Almost one-third of the cases are reported to be asymptomatic at presentation [1]. Symptoms include abdominal pain, pelvic pain, and painless vaginal bleeding. If the patient presents with signs and symptoms of hypovolemic shock then ruptured CSEP must be considered [1].
Many risk factors for CSEP have been delineated, such as maternal age above 35 years, gravidity >3, history of a cesarean delivery done in a rural setting, and an interval of <5 years between the current pregnancy and a previous cesarean delivery [4]. Despite being associated with previous cesarean sections, it is not well established if the number of previous cesarean sections is associated with an increased risk of CSEP [1].
The gold standard for diagnosis of CSEP via imaging is transvaginal ultrasound [5], which, along with abdominal ultrasound, can help visualize the uterus with the bladder and the gestational sac. The following criteria have been proposed for the ultrasound criteria [6]:
-
•
empty uterine cavity with empty and closed cervical canal;
-
•
a triangular, oval, or round gestational sac that fills the niche of the scar;
-
•
placenta and/or gestational sac over the scar of a previous cesarean section;
-
•
a thin or absent layer of myometrium between the gestational sac and the bladder;
-
•
the yolk sac, embryo, and cardiac activity may be absent or present;
-
•
evidence of trophoblast/placental circulation on color flow Doppler, characterized by low impedance (pulsatility index <1) and high velocity (peak velocity > 20 cm/s) blood flow;
-
•
negative ‘sliding organs’ signs.
Management of ectopic pregnancy can be expectant, medical or surgical. A meta-analysis by Cali et al. [7] showed that CSEP with positive fetal/embryonic cardiac activity managed expectantly is associated with high maternal morbidity, including severe hemorrhage and early uterine rupture. Expectant management of CSEP with no cardiac activity requires close surveillance and monitoring [7]. Other management options include methotrexate, surgical sac aspiration, hysteroscopic evacuation, uterine artery embolization, laparoscopic removal, hysterectomy and open surgical treatment. Dilation and curettage are inadequate as trophoblastic tissue is located outside the uterine cavity and the procedure can rupture the uterus through the scar.
In a study of 26 patients, 19 with suspected CSP treated with intramuscular and intragestational methotrexate had a favorable outcome [8]. In our case, a single intramuscular dose of methotrexate was given at a local clinic (beta HCG levels were < 15,000 IU/ml) prior to referral. As it was unsuccessful we proceeded to operative resection [1,9].
Contributors
Abhigan Babu Shrestha shaped the concept, wrote all aspects of the paper and was involved in patient care.
Sajina Shrestha helped write all aspects of the paper.
Ariful Islam Ovi helped write all aspects of the paper.
Tasnim Ayesha helped write all aspects of the paper.
Sima Basak was involved in patient care and manuscript revision.
Minara Parvin Soma was involved in patient care and manuscript revision.
Mst. Irine Parvin was involved in patient care and manuscript revision.
All authors approved the final submitted manuscript.
Funding
No funding from an external source supported the publication of this case report.
Patient consent
Written informed consent was obtained from the parents of the patient for publication of this case report and accompanying images.
Provenance and peer review
This article was not commissioned and was peer reviewed.
Declaration of Competing Interest
The authors declare that they have no conflict of interest regarding the publication of this case report.
References
- 1.Society for Maternal-Fetal Medicine (SMFM), Miller Russell, Gyamfi-Bannerman Cynthia. Publications committee. Society for Maternal-Fetal Medicine Consult Series #63: Cesarean scar ectopic pregnancy. Am. J. Obstet. Gynecol. 2022 Sep;227(3):B9–B20. doi: 10.1016/j.ajog.2022.06.024. [DOI] [PubMed] [Google Scholar]
- 2.Patel M.A. Scar ectopic pregnancy. J. Obstet. Gynaecol. India. 2015;65:372–375. doi: 10.1007/s13224-015-0817-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gagnier J.J., Riley D., Altman D.G., Moher D., Sox H., Kienle G. The CARE guidelines. Dtsch. Arztebl. Int. 2013;110:603–608. doi: 10.3238/arztebl.2013.0603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhou X., Li H., Fu X. Identifying possible risk factors for cesarean scar pregnancy based on a retrospective study of 291 cases. J. Obstet. Gynaecol. Res. 2020;46:272–278. doi: 10.1111/jog.14163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Koplay M., Dogan N.U., Sivri M., Erdogan H., Dogan S., Celik C. Ectopic pregnancy in a cesarean section scar: successful management using vacuum aspiration under laparoscopic supervision-mini review of current literature. Case Rep. Surg. 2016;2016:7460687. doi: 10.1155/2016/7460687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Caesarean Scar ectopic pregnancy Ectopic Pregnancy Foundation. 2022. https://www.ectopicpregnancy.co.uk/for-professionals/caesarean-scar-ectopic-pregnancy/ (accessed September 19, 2022)
- 7.Calì G., Timor-Tritsch I.E., Palacios-Jaraquemada J., Monteaugudo A., Buca D., Forlani F., Familiari A., Scambia G., Acharya G., D’Antonio F. Outcome of cesarean scar pregnancy managed expectantly: systematic review and meta-analysis. Ultrasound Obstet. Gynecol. 2018;51:169–175. doi: 10.1002/uog.17568. [DOI] [PubMed] [Google Scholar]
- 8.Rizk B., Holliday C.P., Owens S., Abuzeid M. Cervical and cesarean scar ectopic pregnancies: diagnosis and management. Middle East Fertil. Soc. J. 2013;18:67–73. doi: 10.1016/j.mefs.2013.01.011. [DOI] [Google Scholar]
- 9.Glenn T.L., Bembry J., Findley A.D., Yaklic J.L., Bhagavath B., Gagneux P., Lindheim S.R. Cesarean scar ectopic pregnancy: current management strategies. Obstet. Gynecol. Surv. 2018;73:293–302. doi: 10.1097/OGX.0000000000000561. [DOI] [PubMed] [Google Scholar]