Abstract
Patients with acute pancreatitis (AP) often require ICU admission, especially when signs of multiorgan failure are present, a condition that defines AP as severe. This disease is characterized by a massive pancreatic release of pro-inflammatory cytokines that causes a systemic inflammatory response syndrome and a profound intravascular fluid loss. This leads to a mixed hypovolemic and distributive shock and ultimately to multiorgan failure. Aggressive fluid resuscitation is traditionally considered the mainstay treatment of AP. In fact, all available guidelines underline the importance of fluid therapy, particularly in the first 24–48 h after disease onset. However, there is currently no consensus neither about the type, nor about the optimal fluid rate, total volume, or goal of fluid administration. In general, a starting fluid rate of 5–10 ml/kg/h of Ringer’s lactate solution for the first 24 h has been recommended. Fluid administration should be aggressive in the first hours, and continued only for the appropriate time frame, being usually discontinued, or significantly reduced after the first 24–48 h after admission. Close clinical and hemodynamic monitoring along with the definition of clear resuscitation goals are fundamental. Generally accepted targets are urinary output, reversal of tachycardia and hypotension, and improvement of laboratory markers. However, the usefulness of different endpoints to guide fluid therapy is highly debated. The importance of close monitoring of fluid infusion and balance is acknowledged by most available guidelines to avoid the deleterious effect of fluid overload. Fluid therapy should be carefully tailored in patients with severe AP, as for other conditions frequently managed in the ICU requiring large fluid amounts, such as septic shock and burn injury. A combination of both noninvasive clinical and invasive hemodynamic parameters, and laboratory markers should guide clinicians in the early phase of severe AP to meet organ perfusion requirements with the proper administration of fluids while avoiding fluid overload. In this narrative review the most recent evidence about fluid therapy in severe AP is discussed and an operative algorithm for fluid administration based on an individualized approach is proposed.
Keywords: Acute pancreatitis, Critical illness, Fluid therapy, Crystalloid solutions, Ringer’s lactate
Introduction
Acute pancreatitis (AP) is an acute inflammatory disease of the pancreas and is among the most common gastrointestinal disorders requiring hospitalization. About 80% of patients with AP have a mild, self-limiting form that needs only brief treatment in a non-critical setting. However, 15–20% of AP episodes are moderately severe or severe, potentially leading to multi-organ failure (MOF), and are burdened by a 20–40% mortality rate [1].
The Atlanta classification for pancreatitis considers two types of AP (interstitial and edematous/necrotizing) and a 3-grade severity scale (mild, moderately severe, severe). Interstitial pancreatitis refers to a diffuse inflammatory edema, while necrotizing pancreatitis is characterized by necrosis involving pancreatic parenchyma and/or the peripancreatic tissue. Both interstitial and necrotizing pancreatitis can be severe; however, interstitial pancreatitis is usually of mild severity, commonly improves in 48 h, and has a mortality rate below 5%. On the other hand, necrotizing pancreatitis, which is observed in 5–10% of patients with AP, often shows a more severe course [2, 3]. The severity of AP is strictly related to the development of MOF, usually involving the cardiocirculatory, renal and pulmonary systems. If organ failure lasts less than 48 h, AP is defined as moderately severe, while it is defined as severe (severe acute pancreatitis, SAP), if organ failure persists for more than 48 h [4]. The discussion of complications not in direct relation with MOF (e.g., pancreatic pseudocysts and perforation of hollow viscus) is beyond the scope of the review and can be found elsewhere [5].
Two peaks of mortality have been identified, i.e., (I) during and (II) after the first week from symptoms development (“early” and “late” phase, respectively) [2]. The early phase is usually characterized by a sterile inflammatory process starting from the pancreas and progressing to a systemic level [6–8]. In this phase, organ failure is linked to the systemic inflammatory response syndrome (SIRS) and has a mortality rate of up to 50%, causing about half of all deaths due to SAP. The second peak of mortality occurs in the “late phase” and is usually secondary to infections of the pancreatic necrotic debris [2, 6, 9–11].
Intensive care unit (ICU) admission is warranted in case of organ failure. With the exception of some special situations (e.g., endoscopic retrograde cholangiopancreatography), no specific therapies exist. The treatment of SAP is, therefore, supportive, mainly based on fluid administration, enteral nutrition, and pain management [12]. Many authors consider intravenous (IV) fluid therapy as the treatment cornerstone for SAP, especially during the first 24 h after disease onset [13].
The aim of this narrative review is to discuss the most recent evidence about fluid therapy in severe AP and to propose an operative algorithm based on an individualized approach to administering intravenous fluids with respect to clinical, hemodynamic, and laboratory monitoring.
Hypovolemia and organ failure
Pathophysiology
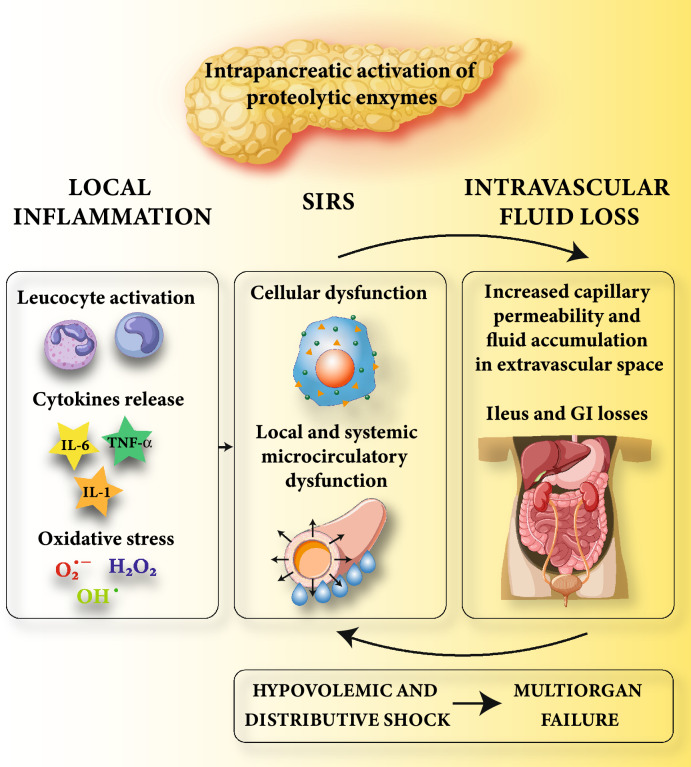
Fluid loss and cytokine release are the two main pathological mechanisms that contribute to AP severity. On the one hand, a massive pancreatic release of pro-inflammatory cytokines (IL-1, TNF-α, and IL-6) leads to SIRS, vasodilatation, and cellular dysfunction [7]. On the other hand, several factors contribute to extensive intravascular fluid loss (Fig. 1). First, vomit and abdominal pain impair feeding and enhance gastrointestinal fluid depletion. Second, insensible losses are increased by the tachypnea and diaphoresis related to pain, systemic inflammation, and fever. Finally, and most importantly, pancreatic inflammation and SIRS are associated with local and systemic increased capillary permeability, favoring extravascular fluid accumulation [7, 14, 15]. Of note, local microcirculatory dysfunction contributes to pancreatic tissue hypoperfusion and ischemia [14, 16] which can spread systemically and further worsen the pancreatic insult [17]. This vicious cycle might be deleterious also for the hollow viscera [18]. In particular, ileus and fluid accumulation within the intestinal lumen might occur. In addition, fluid sequestration frequently occurs in the retroperitoneal space [19], potentially causing intra-abdominal hypertension and abdominal compartment syndrome [20–22].
Fig. 1.
Pathophysiology of fluid loss/hypovolemia in patients with severe acute pancreatitis. The intrapancreatic activation of proteolytic enzymes causes local tissue inflammation with leukocyte activation, cytokines, and reactive oxygen species release. At a systemic level, the massive release of pro-inflammatory cytokines from the injured pancreas leads to SIRS, causing an intravascular fluid loss through vasodilatation, cellular dysfunction, and increased capillary permeability. Ileus, vomit, decreased fluid intake, and increased insensible losses further contribute to intravascular fluid depletion. If not interrupted, this vicious cycle leads to a severe hypovolemic and distributive shock and ultimately to MOF. IL-1 Interleukin-1; TNF-α Tumor necrosis factor; IL-6 Interleukin-6; SIRS Systemic inflammatory response syndrome; GI Gastrointestinal; MOF Multiorgan failure
In summary, patients with SAP are frequently characterized by a severe hypovolemic and distributive shock, which ultimately leads to the development of MOF [23–25]. The extent of fluid depletion/shifts is, however, difficult to assess precisely. Up to four liters of fluid sequestration have been reported in mild pancreatitis at 48 h, and up to six liters in more severe forms [26, 27]. In several studies, greater fluid sequestration has been associated with a higher complication rate and morbidity [28–31].
Fluid resuscitation: general recommendations
Available guidelines for the treatment of AP underline the importance of early fluid therapy [13, 32–37]. However, there is currently no consensus neither about the type nor about the optimal fluid rate or goal of fluid administration [38, 39] (Table 1). In this context, three main features of AP should be kept in mind. First, AP is a dynamic illness that can worsen after initial presentation [40, 41]. Continuous monitoring and reassessment of fluid requirements are, therefore, warranted. Second, AP is considered a time-dependent illness whose outcome could be influenced by the promptness of interventions. Indeed, the first hours from disease onset are considered pivotal to prevent progression of SIRS, MOF, and/or worsening of pancreatic necrosis [42]. On the other hand, however, the administration of excessive amounts of fluids might be detrimental in the presence of an increased capillary-permeability state [6, 43, 44]. Third, hypovolemia in the context of SAP is not a simple loss of intravascular volume, but a combination of hypovolemia and microcirculatory dysfunction due to SIRS. Of note, it is conceivable that fluid therapy might play a role in modulating inflammation and reducing capillary permeability [44–47].
Table 1.
Main studies investigating fluid administration in acute pancreatitis
| Authors | Study design | Type of IV fluid | Rate of administration | Resuscitation endpoint | Study endpoint | Results |
|---|---|---|---|---|---|---|
| De-Madaria E, [130] | RCT (n = 249) | RL | Aggressive: bolus 20 ml/kg–3 ml/kg/h Moderate: bolus 10 ml/kg–1.5 ml/kg/h. In both groups, assessments at 3, 12, 24, 48, and 72 h to check for fluid overload or hypovolemia | BUN, Ht, UO, signs of dehydration, SBP | Development of moderately severe or severe pancreatitis during the hospitalization. Safety outcome signs of fluid overload | No difference in the primary outcome between the two groups. Higher incidence of fluid overload in the aggressive resuscitation group |
| Gad MM, [39] | Metanalysis (n = 2686) | / | Aggressive vs Non-aggressive | / | Mortality, PN, OF, AKI, RF | No difference between the two groups |
| Li L, [134] | RC (n = 912) | / | Rapid: ≥ 3 ml/kg/h Slow: < 3 ml/kg/h | / | Rate of MV, LOS | MV and hospital LOS associated with rapid FT in SAP and Ht ≥ 44% |
| Cuèllar-Monterrubio JE, [135] | RCT (n = 88) | Hartmann solution | Aggressive: bolus 20 ml/kg–3 ml/kg/h for 24 h -30 ml/kg/day Non-aggressive: 1.5 ml/kg/h for 24 h, then 30 ml/kg/day | Vital signs, UO, BUN, Ht, lactate, SIRS | Development of SIRS and OF | No difference in outcome |
| Ye B, [88] | RC (n = 179) | NS, RL |
Aggressive (> 4 L/day) Non-aggressive (< 4 L/day) |
Vital sign, UO > 0.5 ml/kg/h, Ht < 45% |
AKI development Chloride exposure |
> 4 L/day and higher chloride exposure associated with AKI |
| Yamashita T, [51] | RC (n = 1097) | / |
Aggressive ≥ 6 lt/day Non-aggressive < 6 lt/day |
/ | In-hospital mortality | ≥ 6 L within 24 h associated with less mortality |
| Buxbaum JL, [131] | RCT (n = 60) | RL |
Aggressive: 20 ml/h bolus + 3 ml/kg/h Standard: 10 ml/h + 1.5 ml/kg/h (median 3.91 L/24 h) |
Ht, BUN, Cr |
Decrease in Ht, BUN, Cr Reduced pain Tolerance to oral feeding |
Higher clinical improvement, reduced SIRS development, and less hemoconcentration in Aggressive group |
| Singh VK, [77] | RC (n = 1010) | / |
FVER Group I < 500 ml Group II 500–1000 ml Group III > 1000 ml FV24 Group I < 3200 ml Group II 3200 – 4300 ml Group III > 4300 ml |
/ | LC, OF, Invasive treatment, mortality |
FVER 500–1000 ml and > 1000 ml associated with better outcomes FV24 > 4300 ml associated with higher LC |
| Weitz [136] | RC (n = 391) | Ringer’s solution | / | / | Severity, LC, OF, PN | Higher fluid volume associated with severity and LC |
| Wall I, [50] | RC (n = 286) | / |
Until year 1998 = 113 ml/h in first 6 h From 1998 to 2008 = 284 ml/h in first 6 h |
/ | OF, PN, mortality | Less mortality and PN up to year 2008 |
| Warndorf MG, [49] | RC (n = 434) | NS (in 85% of cases) |
Early FT: ≥ 1/3 of the total 72 h fluid volume administered in the first 24 h Late FT: < 1/3 administered in the first 24 h (2.403 ml/24 h) |
/ | Mortality, SIRS, OF, ICU, LOS | Less SIRS, ICU, OF associated with early FT |
| De-Madaria E, [74] | RC (n = 247) |
NS plus D5%/D10% |
FT volume in first 24 h: Group A: < 3.1 L Group B: 3.1 – 4.1 L Group C: > 4.1 L |
Ht < 44%, UO > 50 ml/h, low Cr, normal SBP | OF, PN, APFC, mortality | Group C had more RF and AKI rate |
| Kuwabara K, [76] | RC (n = 9849) | Crystalloids |
FV48 FVR |
/ | Mortality, MV, Dialysis |
Higher FV48 associated with increased rate of MV, dialysis, mortality Higher FVR associated with lower mortality in the severe AP group |
| Wu B, [47] | RCT | NS vs RL | Standard 20 ml/kg bolus + 3 ml/kg/h vs physician judgment | BUN | SIRS | No difference between different rates; difference between RL and NS |
| Mole DJ, [137] | RC (n = 30) | NS, HS, D5-50%, sodium bicarbonate, phosphate; colloids (Gelofusine, Albumin 4.5%); blood products | / | Physician’s judgment | Volume of fluids administered | Less fluids associated with higher mortality |
| Gardner TB, [48] | RC (n = 45) | NS (71%), D5% + NaCl 0.45% (20%), RL (9%) |
Early FT: 203 ml/h in first 24 h Late FT: 71 ml/h in first 24 h |
/ | Mortality, OF, LOS | Higher mortality rate in Agg group |
| Mao E, [79] | RCT (n = 115) | NS, RL, plasma, HES 6% | Depending on goal-Ht |
Ht < 35% vs > 35% |
Incidence of sepsis, mortality | Goal Ht < 35%: major incidence of sepsis and higher mortality rate. Higher amount of fluid volume |
| Mao E, [78] | RCT (n = 76) | NS, RL, plasma, HES 6% |
Group I: 10–15 ml/kg/h Group II: 5–10 ml/kg/h |
HR, MAP, UO, Ht < 35% | APACHE II score, MV, ACS and sepsis incidence, mortality | Group I: higher incidence of MV and ACS, higher mortality rate |
| Eckerwall G [75] | RC (n = 99) | Crystalloids, Colloids (mainly albumin) |
> 4000 ml/24 h Vs< 4000 ml/24 h |
/ | Respiratory complications, ICU admission rate, mortality | More respiratory complications and need for intensive care admissions with > 4000 ml/24 h |
/ Not specified; AKI Acute kidney injury; APFC Acute peripancreatic fluid collections; ACS Acute Compartment Syndrome; BUN Blood urea nitrogen; Cr Creatinine; D5–10–50% Dextrose solution 5–10–50%; FT fluid therapy; FVER Fluid Volume in Emergency Room, within 4 h from admission; FV24 Fluid volume administered in first 24 h, since admission to the hospital ward. FV48 Fluid volume per day in the initial 48 h; FVR (Fluid volume ratio) Average fluid volume per day in the first 48 h, compared to fluid volume per day during total hospitalization; HD Hemodialysis; Ht Hematocrit; HES 6% Hydroxyethyl starch 6%; ICU Intensive Care Unit; LOS Hospital Length of stay; LC Local complications; MV Mechanical ventilation; NS Normal saline; PN Pancreatic necrosis; OF organ failure; RF Respiratory failure; RC Retrospective Cohort, RCT Randomized Clinical Trial; RL Ringer Lactate; SBP Systolic blood pressure; SIRS Systemic Inflammatory Response Syndrome; UO Urinary output
Some studies have shown that the rapid reversal of hypovolemia is associated with improved outcomes [48–52]. In addition, multiple animal experiments suggested that adequate fluid therapy could reduce pancreatic damage and in some cases mortality [53–55]. Based on these results, most guidelines advocate for early and adequate fluid resuscitation.
Some laboratory values such as hematocrit (Ht) and blood urea nitrogen (BUN) have been traditionally considered markers of hypovolemia and might contribute to the assessment of fluid status. High values at admission and their increase during the first 24–48 h could thus indicate inadequate fluid resuscitation [56, 57].
Hemoconcentration (i.e., high Ht) is associated with high fluid sequestration and increased blood viscosity, which, by itself, might contribute to impaired pancreatic microcirculation, favoring pancreatic necrosis [28]. Several studies reported a higher probability of severe disease when Ht ≥ 45% at admission [57–60]. Likewise, the failure to reduce Ht within the first 24 h has been linked to inadequate fluid therapy and worse outcomes.
In addition, hypovolemia might lead to an increase in BUN. Its specificity is, however, low, as the increase might be multifactorial: hypovolemia, renal failure, increased protein catabolism, and gastrointestinal bleeding [61]. Nevertheless, high BUN values at admission (≥ 20 mg/dL, equivalent to plasma urea ≥ 42 mg/dL), regardless of the underlying cause, and increasing values at 24 h have been found to be predictive of organ failure/mortality [61–65].
While both parameters are discussed in literature, Ht might be a more appealing endpoint to guide fluid resuscitation, as compared to BUN, being the latter more influenced by other pathological conditions that are common in the critically ill patients. Moreover, Ht is relatively simple to measure, as it is commonly calculated from the results of the point-of-care arterial blood gas analysis.
Infusion rate and cumulative administered volume
The optimal timing and rate of fluid administration are still unknown. Available guidelines recommend early and aggressive fluid therapy [13, 38]. This definition refers to a higher fluid rate in the first hours of the disease and a lower rate in the following days.
Gardner et al. retrospectively analyzed fluid administration over the first 72 h of hospitalization in a group of 45 patients with SAP [48]. When more than one-third of the cumulative fluid volume was infused within the first 24 h, the treatment was classified as “early”, while it was defined as “late resuscitation” if less than one-third of the cumulative volume was infused within the first day. As expected, the difference in fluid volume administered in the first 24 h was marked: almost five liters in the “early” and less than 2 liters in the “late” resuscitation group. Interestingly, the “early” experienced significantly lower mortality as compared to the “late” group. Based on Gardner’s and other similar findings, progressively larger amounts of fluid have been administered in the early phases of SAP [49, 50].
Currently, different guidelines suggest a starting fluid rate for patients with AP presenting with features of hypovolemia (Table 2) [13, 33, 34]:
5–10 ml/kg/h for the first 24 h until resuscitation goals are achieved [33]. Suggested goals are heart rate (HR) < 120 bpm, mean arterial pressure (MAP) > 65 mmHg, urinary output (UO) > 0.5 ml/kg/h, and Ht 35–44%.
250–500 ml/h of isotonic crystalloid for the first 12–24 h, with little benefit beyond this time period and with the goal to decrease BUN and Ht [13].
150–600 ml/h in patients with shock or dehydration, until MAP > 65 mmHg and UO > 0.5 ml/kg/h, and 130–150 ml/h in patients without severe signs of hypovolemia [34].
Table 2.
Suggested fluid therapy regimens in severe acute pancreatitis
| Authors, year | IV infusion rate (in the first 24 h) | Goals/endpoints | Comments |
|---|---|---|---|
| De Waele E et al. [70] | 5–10 ml/kg/h | / | Up to 250–500 ml/h for 24 h. Up to ≥ 5000 ml may be necessary |
| Working group IAP/APA, [33]; Hines OJ, Pandol SJ, [5] | 5–10 ml/kg/h |
Clinical targets (UO > 0.5 -1 ml/kg/h) Invasive targets (ITBV, SVV) Laboratory markers (Ht 35–44%) |
2500–4000 mL in the first 24 h are usually sufficient |
| Buxbaum et al. [131] | 20 mL/kg bolus, then 3 ml/kg/h | Urea, Ht, creatinine |
Higher clinical improvement with aggressive IV hydration Tested only on mild AP |
| DiMagno MJ, [66] | 5–10 ml/kg/h until hemodynamic stability, then 3 ml/kg/h | HR < 120, MAP 65–86 mmHg, UO > 50 ml/h |
After 6 h check BUN: ••••••If < 20 mg/dl or falling: change to 1.5 ml/kg/h ••••••If not, infusion of 5–10 ml/kg/h |
| Yokoe M et al. [34] | 150–600 ml/h | MAP > 65 mmHg and UO > 0.5 ml/kg/h | Reduce to 130–150 ml/h when dehydration and shock are reversed |
| Pezzilli R et al. [36] | Initial bolus of 20 ml/kg within 30–45 min, then 2 ml/kg/h | Normal UO, MAP, HR. BUN < 20 mg/dL, Ht 35–44% | Monitor every 8–12 h for the first 24–48 h |
| Aggarwal et al. [67] | Bolus 1000 mL in 1 h, then 3 ml/kg/h (200 ml/h) | UO > 0.5 ml/kg/h, Ht 25–35%, drop in BUN | Continue for 24–48 h, until signs of volume depletion disappear |
| Tenner S et al. [13] | 250–500 ml/h | Decrease Ht and BUN | Benefits are limited to first 12–24 h |
| Fisher MJ, Gardner TB, [82] | 250–300 ml/h | Enough to produce a UO of 0.5 ml/kg/h | Tailor on patients’ characteristic, urine output, blood pressure, and modest decrease in hematocrit |
| Nasr JY, Papachristou GI, [132] | Initial bolus 20 ml/kg, followed by 150–300 ml/h (3 ml/kg/h) | BUN, Ht | Subsequent maintenance: 2–3 ml/kg/h |
| Wu BU et al. [47] |
Bolus 20 ml/kg in 30 min, then 3 ml/kg/h maintenance (1.5 ml/kg/h for less hypovolemic patients) |
Decreased BUN level | No improved outcome in early goal directed therapy was evidenced |
| Pandol S et al. [133] |
Level of dehydration: fluid rate -Severe: 500–1000 ml/h -Moderate: 300–500 ml/h -Mild: 250–350 ml/h |
Vital signs, UO, Ht | Reassess every 1–2 h |
AP Acute Pancreatitis; BUN Blood urea nitrogen; HR Heart rate; Ht Hematocrit; ITBV Intrathoracic blood volume; MAP Mean arterial pressure; UO Urine output; SVV Stroke volume variation; / Not specified
Other infusion strategies are reported in Table 2. After the early critical phase, fluid rate is usually reduced to 2–3 ml/kg/h [36, 47, 66, 67]. Close clinical monitoring and the definition of clear resuscitation goals are fundamental [68]. Generally accepted targets are urinary output, reversal of tachycardia and hypotension, and improvement of laboratory markers, such as BUN and Ht. The usefulness of different endpoints to guide fluid therapy is still debated. There is, however, general agreement regarding the importance of close monitoring of fluid status, to reduce the risks of fluid overload [13, 69].
In most cases, a cumulative volume of 2.5–4 L during the first 24 h has been shown to be sufficient to reach the resuscitative targets [33]. However, clinicians should be aware that up to five or more liters per day may be required in the initial phase [51, 70].
Complications of excessive fluid administration
Despite the clear benefits of IV fluid therapy, excessive administration of fluids can lead to several complications. Overall, markedly positive fluid balances are associated with worse outcomes in critically ill patients [71]. Fluid might be retained in the interstitial space leading to interstitial edema, impaired organ perfusion, and possibly acute pulmonary edema. In the specific context of SAP, intestinal wall edema and retroperitoneal edema are feared complications for abdominal compartment syndrome development [22]. A global increased permeability syndrome (GIPS) might develop in the context of persistent systemic inflammation (i.e., high capillary leak) and positive cumulative fluid balance (i.e., edema formation and polycompartment syndromes) with persistent organ failure [72, 73]. It is, therefore, fundamental to tailor fluid therapy carefully.
Many authors described in observational studies an association between high IV fluid volumes and increased intra-abdominal pressure, increased organ failure, and mortality in the specific setting of AP [74–76]. The observational nature of these studies, despite multiple corrections and normalizations, limits the soundness of the findings, as patients with more severe forms of AP usually require more fluids and have a worse prognosis. In this context, it is, therefore, difficult to establish the definitive causal relationship between fluid volume and outcome [43, 77].
To date, only a few randomized clinical trials (RCTs) have compared a more aggressive versus a more conservative resuscitation strategy. A Chinese group conducted two RCTs on patients with SAP. In the first study [78], a group received a fixed fluid rate of 10–15 ml/kg/h, while the second group received 5–10 ml/kg/h, as needed to achieve hemodynamic stability. In the second trial [79], a group received IV fluids at admission rapidly aiming at a Ht < 35%, while the other group had a Ht target > 35%. In both studies, the authors report a higher incidence of sepsis, higher complications due to fluid overload, and a higher mortality rate when fluids were administered in high volume. The results of these studies are, however, not definitive, as several flaws (unclear randomization method, unreported incidence of necrosis, contradictory data on the amount of volume infused) have been identified [80–82].
In summary, it is still unknown how to identify the correct amount and rate of IV fluid to prevent or reverse the evolution of organ failure and reduce the complications due to fluid overload.
According to the most recent evidence and experts’ opinion, fluid therapy should be tailored based on patient’s needs, enhanced in the first hours, and continued only for the appropriate time frame. For this reason, fluid therapy is usually discontinued or significantly reduced after the first 24 after admission. Of note, patients who do not show a prompt clinical response after the first 6–12 h of fluid therapy might not benefit from a large fluid administration [13, 66, 82, 83].
Types of intravenous fluids
The ideal IV fluid in the context of SAP should improve hemodynamics/organ perfusion by restoring extracellular fluid volume while modulating inflammatory response in the presence of altered capillary permeability. Crystalloids and colloids are the two broad fluid categories available in the critical care setting. In theory, they have different distributions within fluid compartments, resulting in different intravascular volume expansions. Importantly, they show different adverse effects [84–86].
Studies comparing different fluid administration strategies in AP used different types or combinations of IV fluids: normal saline (NS), balanced crystalloids, or mixed strategies using a combination of crystalloids and colloids (such as albumin, starches, and fresh frozen plasma) [38]. Different IV fluids likely have a different impact on some clinical outcomes [87]. In a retrospective study, Ye et al. observed that an aggressive resuscitation strategy was associated with an increased incidence of acute kidney injury in patients with SAP [88]. Of note, both high volume resuscitation (> 4 L in the first 24 h) and high chloride exposure due to NS infusion were independent risk factors for acute kidney injury. High concentrations of serum chloride have been associated with renal failure in critically ill patients also in other studies [87, 89].
Crystalloids
Normal saline (0.9% sodium chloride solution) and balanced crystalloid solutions (such as Ringer’s lactate) are broadly used fluids. Balanced solutions are more similar to extracellular fluid as they contain some organic anions (buffers), which are metabolized once delivered to the patient and allow to lower the chloride concentration of the fluid. Different crystalloids have different strong ion differences (SID), i.e., the difference between strong cations (mainly [Na +]) and strong anions ([Cl-]). According to Stewart’s acid–base approach, SID is an independent variable affecting the pH of a biological solution [90, 91]. Normal plasma SID ranges between 33–40 mEq/L, according to the used definition. A reduction in SID, shifts the system toward acidosis while an increase in SID toward alkalosis [92]. The SID of infused crystalloids (after metabolism of the organic anions) might, therefore, significantly alter plasma SID and, therefore, affect pH [85, 86]. Normal saline has a SID of 0 mEq/L as Na+ and Cl− have the same concentration, and its net effect is, therefore, always acidifying. On the other hand, the infusional SID of balanced crystalloids ranges between 28 and 55 mEq/L with a reduced effect on plasma acid–base [93].
Ringer’s lactate solution (RL), a slightly hypotonic, balanced crystalloid, has been compared to NaCl 0.9% for fluid resuscitation in a small RCT in patients with AP [47]. In this trial, patients randomized to RL had a reduced prevalence of SIRS and a lower concentration of C-reactive protein at 24 h post-admission. Similar results were described by other authors [46, 94–97].
These findings might be explained by a possible immunomodulatory, anti-inflammatory, and organ-protective effect of lactate, but also to a detrimental effect of high chloride concentrations [98]. Indeed, experimental animal studies suggest that an exogenous hydrochloric acid load might worsen AP, as the local acidification at the pancreatic acinar level could favor pancreatic edema/necrosis [99]. While clinical data on this topic are lacking, these findings provide an additional rationale for avoiding the exogenous acid load resulting from the infusion of large volumes of NaCl 0.9%. Finally, it might be worth mentioning that isotonic fluids, besides providing water, contain large quantities of sodium, which might contribute to water and salt overload, ultimately favoring edema formation [100–102].
Colloids
Colloids are solutions based on semi-synthetic or plasma-derived molecules dissolved in crystalloids. Human albumin, starches, gelatines, and dextrans are the colloids used in clinical practice. In theory, these molecules are large enough to be retained by semi-permeable membranes and should exert higher colloidal-osmotic pressures than crystalloids. Their putative advantage is the achievement of higher volume expansions with less infused volume and the longer persistence in the intravascular space, conceptually leading to less edema formation and better hemodynamic stability [71, 84]. However, their use in critically ill patients is highly debated [89]. Indeed, no definite benefit exists over crystalloids on mortality, and colloids are rather known for their potentially harmful effects [103].
In the specific context of AP, experiments conducted in animals suggest that resuscitation with dextrans could be superior to crystalloids, possibly due to improved pancreatic perfusion [104, 105]. In humans, only a few studies assessed the use of colloids for fluid resuscitation of patients with AP/SAP. Zhao et al. compared patients treated with hydroxyethyl starch (HES) and NS in a 1:1 ratio to patients treated with NS alone and observed a shorter time to hemodynamic stability and microcirculation perfusion improvement in the first group [45]. However, HES administration has been largely investigated in critically ill patients and the adverse effects have been shown in large RCTs [106, 107]. Thus, current evidence does not support HES use in most patients admitted to the ICU, including those with SAP [108].
It is, therefore, clear that no conclusive evidence exists about the ideal fluid in SAP and guidelines do not provide a definitive indication, given the moderate quality of the available evidence [109, 110]. However, most experts and guidelines recommend crystalloids, and among them, RL is usually indicated as the fluid of choice [111].
Fluid resuscitation: an individualized approach
Recent data support the importance of a tailored and individualized fluid therapy in the context of SAP requiring ICU admission [112]. As described above, early and aggressive fluid therapy can be beneficial for some, but deleterious for other patients. Aggressive fluid therapy might be well-tolerated in patients with mild AP, as the patient is able to eliminate fluids in excess. On the contrary, patients with SAP have persistent organ failure and markedly increased vascular permeability. Here, a large amount of IV fluids might lead to water and salt overload and further worsen the disease [68, 83, 113]. Given the potential harm of an inappropriate administration of fluids in critically ill patients, patients need to be carefully monitored [114].
Clinical endpoints that could guide fluid resuscitation in patients with SAP can be classified in three groups: noninvasive clinical parameters (1), invasive hemodynamic parameters (2), and laboratory markers (3).
Clinical parameters that are commonly and easily monitored are MAP, HR, and UO. A high HR and/or a low MAP and UO can be indicative of low circulating blood volume, oxygen delivery, and impaired end-organ perfusion [115]. An HR < 120/min, a MAP between 65 and 85 mmHg, and UO > 0.5 ml/kg/h are desirable endpoints in the management of SAP. Abnormal values alone or with other signs of organ hypoperfusion should prompt fluid administration in the early phase, [116, 117]. The skin mottling score and the capillary refill time are other useful clinical markers of microvascular perfusion and could be helpful clinical parameters in this context [118].
Invasive hemodynamic parameters, such as those obtained from a central line catheter or from the arterial pulse contour analysis, are useful to assess hypovolemia and fluid responsiveness. Static indices of cardiac preload like central venous pressure (CVP) are still used in common practice, though their use is highly debated. CVP values might be useful as a safety limit to avoid fluid overload in the setting of right-heart failure. Calibrated hemodynamic monitoring systems, such as PiCCO (Pulsion Medical Systems SE, Feldkirchen, Germany), are based on transpulmonary thermodilution. Such systems are commonly available in the ICU and have been investigated also in the specific setting of SAP with promising results [119–122], showing that PiCCO parameters could better correlate with changes in cardiac output and could guide fluid resuscitation with favorable outcomes.
Lactate levels and central venous saturation are indirect markers of organ perfusion and oxygen delivery [123]. Inadequate organ perfusion and inadequate oxygen utilization at the cellular level are the ultimate result of massive fluid loss in early SAP and also a key feature of hemodynamic shock state. In addition, Ht and BUN, as previously mentioned, are useful laboratory markers which could help estimate the degree of fluid sequestration at admission.
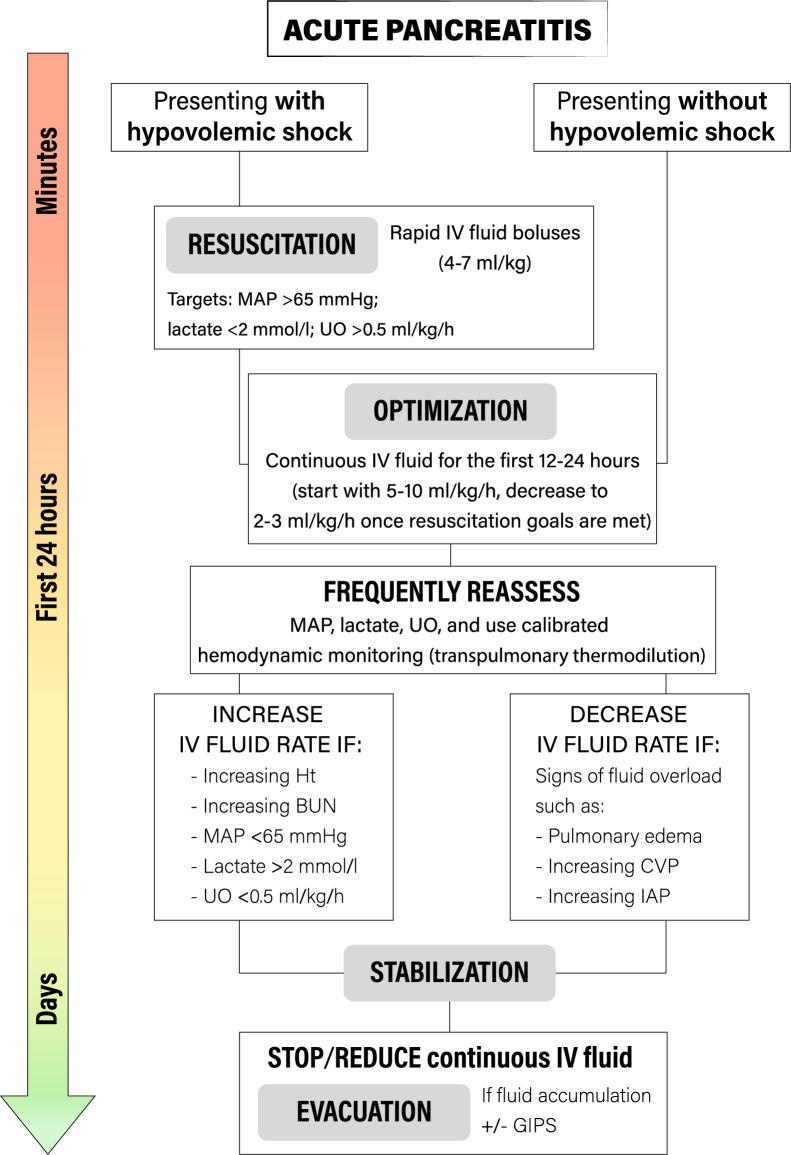
Four distinct phases of fluid resuscitation for critically ill patients have been recently proposed and conceptualized through the R.O.S.E. acronym (Resuscitation, Optimization, Stabilization, Evacuation), which could also be adapted for patients with SAP [114]. In the hyperacute phase (phase 1, Resuscitation), the patient might be in hypovolemic shock and the physician must provide an early, adequate goal-directed fluid management with an abundant fluid infusion. A positive fluid balance is inevitable and tolerated to achieve adequate perfusion. In the Optimization phase (phase 2), although still hypovolemic, patients with SAP present a more compensated shock. The individual fluid requirement must be regularly assessed. The goal is to maintain adequate tissue oxygenation to limit organ damage and to maintain a neutral fluid balance to avoid fluid overload. Intra-abdominal pressure measurement has been advocated in patients with abdominal problems, to monitor the possible development of abdominal compartment syndrome [124, 125]. The Stabilization (phase 3) evolves over the following days and signs of circulatory shock are absent. Fluids are needed only to replenish ongoing losses. Finally, the Evacuation (phase 4) starts with spontaneous evacuation (the “flow” phase) when the acute insult resolves. When evacuation is not spontaneous, a strategy of active fluid removal, using diuretics, might be pursued [71]. If this model is applied to the clinical context of SAP in its early phase, most of the fluid therapy is directed to reverse hypovolemia in the Resuscitation and Optimization phases. In both cases, an individualized approach for fluids administration is advocated.
A single clinical marker alone unlikely reflects the overall volume status and the assessment of multiple parameters simultaneously is considered more reliable [113]. The patient should be frequently reassessed during the first 24 h, ideally every 2–3 h to adjust fluid administration based on modification in these parameters, to avoid under- or over-treatment [56, 68] (Fig. 2).
Fig. 2.
Proposed algorithm for fluid resuscitation in severe acute pancreatitis. Hypovolemic shock is reversed with intravenous balanced crystalloids until Resuscitation goals are met. In the Optimization phase, a continuous infusion should be provided to meet ongoing fluid losses. A continuous Reassessment is required to assess further needs for fluids, guided by advanced hemodynamic monitoring systems, aiming to define the real fluid requirements while evaluating any signs of fluid overload. The Stabilization evolves over the following days. Here, fluids are needed only to replenish ongoing losses and the evacuation starts with spontaneous or induced evacuation when the acute insult resolves. IV Intravenous; MAP Mean arterial pressure; UO Urinary output; Ht Hematocrit; BUN Blood urea nitrogen; IAP Intra-abdominal pressure; CVP Central venous pressure; GIPS Global increased permeability syndrome
Over the first Resuscitation phase and the following Optimization phase, the use of vasopressors (like norepinephrine) could be considered [126]. During SAP, hypotension is partially due to vasodilation and an hyperdynamic circulatory state usually follows fluid resuscitation [127, 128]. In the very early phase, fluids are virtually mandatory, but vasopressors might be administered as an adjunct to temporarily increase a low MAP—while fluid resuscitation is ongoing. During the following stages, fluid requirement is constantly reassessed: a vasopressor can be used when a low MAP is a concern, but the patient seems otherwise euvolemic. However, a patient with SAP and clear signs of hypovolemia should not receive vasopressor instead of fluids, given the risk of further organ hypoperfusion. Once fluid status is optimized de-escalation should be considered [129].
Recent and ongoing research
Three main questions are still not completely answered about fluid therapy during SAP. First, the optimal rate and the extent of fluid administration in the early phase of the disease. Second, the most accurate clinical and laboratory endpoint to guide fluid resuscitation. Third, the best fluid that, administered in large volume, could guarantee the highest efficacy and safety [38].
WATERFALL is a very recently published RCT [130]. The study aimed at comparing aggressive versus moderate fluid resuscitation in patients with AP. Patients who met the criteria for moderately severe or severe disease at baseline were excluded. A total of 122 subjects received an aggressive (RL 20 ml/kg bolus administered over 2 h followed by RL 3 ml/kg/h) and other 127 patients received a moderate fluid resuscitation (RL bolus 10 ml/kg in case of hypovolemia or no bolus in normovolemic patients, followed by RL 1.5 ml/kg/h.). Patients in the aggressive resuscitation group developed a significative higher fluid overload as compared to the moderate resuscitation group, with no improvement in clinical outcomes [130].
Other ongoing RCTs are mainly focused on the comparison between normal saline and other crystalloids. Farrell et al. plan to enroll 80 pediatric patients with acute pancreatitis receiving either RL or NS to assess inflammatory markers and SIRS status at 24 and 48 h (clinicaltrials.gov NCT03242473). Poropat et al. aim to enroll 276 adult patients with acute pancreatitis to receive either Plasmalyte or normal saline as an initial bolus of 10 ml/kg in the first 60 min after randomization, and then at a rate of 2 ml/kg for the next 72 h (Clinicaltrials.Gov NCT04688645). The primary endpoint of the study is the incidence of SIRS.
Conclusions
Fluid therapy is a key treatment of patients admitted to the ICU with severe forms of acute pancreatitis. A broadly accepted early and aggressive fluid therapy has been recently questioned due to potential harm and not definitive efficacy in clinical trials. Since there is a possible risk of under-resuscitation when a fixed infusion rate is used, a more tailored approach is warranted. It should be based on a careful assessment of the patient’s volume status, with enhanced volume expansion in the first hours of admission for the most severe cases. Crystalloids, and in particular RL, are the fluids of choice, with a suggested initial fluid rate usually ranging between 5–10 ml/kg/h. Then, if at any time during the first 24 h resuscitation goals are met, it is reasonable to reduce fluid rate to 2–3 ml/kg/h. Patients with SAP should be strictly monitored in the ICU, where advanced hemodynamic monitoring systems are available to guide clinicians.
Abbreviations
- AP
Acute pancreatitis
- BUN
Blood urea nitrogen
- Ht
Hematocrit
- HR
Heart rate
- ICU
Intensive care unit
- IV
Intravenous
- MAP
Mean arterial pressure
- MOF
Multi-organ failure
- NS
Normal saline
- RCT
Randomized clinical trial
- RL
Ringer lactate
- SAP
Severe acute pancreatitis
- SID
Strong ion difference
- SIRS
Systemic inflammatory response syndrome
- UO
Urine output
Author contributions
TL and SS conceived the manuscript. AC, SS, and TL performed the literature search and drafted the manuscript. SS drafted the figures. The article was critically reviewed and revised by all authors. All authors read and approved the final manuscript.
Declarations
Competing interests
None of the authors has any conflicts of interest to declare. There was also no specific funding for the research and no specific grants received from any funding agency in the public, commercial, or not-for-profit domains.
Footnotes
The original online version of this article was revised: The author name Niels Van Regenmortel which was incorrectly written as Niels Van Regenemortel has been corrected.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Andrea Crosignani and Stefano Spina share first authorship
Change history
6/14/2023
A Correction to this paper has been published: 10.1186/s13613-023-01149-2
References
- 1.Boxhoorn L, Voermans RP, Bouwense SA, Bruno MJ, Verdonk RC, Boermeester MA, et al. Acute pancreatitis. Lancet. 2020;396:726–734. doi: 10.1016/S0140-6736(20)31310-6. [DOI] [PubMed] [Google Scholar]
- 2.Banks PA, Bollen TL, Dervenis C, Gooszen HG, Johnson CD, Sarr MG, et al. Classification of acute pancreatitis–2012: revision of the Atlanta classification and definitions by international consensus. Gut. 2013;62:102–111. doi: 10.1136/gutjnl-2012-302779. [DOI] [PubMed] [Google Scholar]
- 3.Sureka B, Bansal K, Patidar Y, Arora A. Imaging lexicon for acute pancreatitis: 2012 Atlanta classification revisited. Gastroenterol Rep. 2016;4:16–23. doi: 10.1093/gastro/gov036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Banks PA. Acute pancreatitis: landmark studies, management decisions, and the future. Pancreas. 2016;45:633–640. doi: 10.1097/MPA.0000000000000632. [DOI] [PubMed] [Google Scholar]
- 5.Hines OJ, Pandol SJ. Management of severe acute pancreatitis. BMJ. 2019;367:l6227. doi: 10.1136/bmj.l6227. [DOI] [PubMed] [Google Scholar]
- 6.Garg PK, Singh VP. Organ failure due to systemic injury in acute pancreatitis. Gastroenterology. 2019;156:2008–2023. doi: 10.1053/j.gastro.2018.12.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Singh P, Garg PK. Pathophysiological mechanisms in acute pancreatitis: current understanding. Indian J Gastroenterol. 2016;35:153–166. doi: 10.1007/s12664-016-0647-y. [DOI] [PubMed] [Google Scholar]
- 8.Zhou M-T, Chen C-S, Chen B-C, Zhang Q-Y, Andersson R. Acute lung injury and ARDS in acute pancreatitis: mechanisms and potential intervention. World J Gastroenterol. 2010;16:2094–2099. doi: 10.3748/wjg.v16.i17.2094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Johnson CD, Abu-Hilal M. Persistent organ failure during the first week as a marker of fatal outcome in acute pancreatitis. Gut. 2004;53:1340–1344. doi: 10.1136/gut.2004.039883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mofidi R, Duff MD, Wigmore SJ, Madhavan KK, Garden OJ, Parks RW. Association between early systemic inflammatory response, severity of multiorgan dysfunction and death in acute pancreatitis. Br J Surg. 2006;93:738–744. doi: 10.1002/bjs.5290. [DOI] [PubMed] [Google Scholar]
- 11.Padhan RK, Jain S, Agarwal S, Harikrishnan S, Vadiraja P, Behera S, et al. Primary and secondary organ failures cause mortality differentially in acute pancreatitis and should be distinguished. Pancreas. 2018;47:302–307. doi: 10.1097/MPA.0000000000000998. [DOI] [PubMed] [Google Scholar]
- 12.James TW, Crockett SD. Management of acute pancreatitis in the first 72 hours. Curr Opin Gastroenterol. 2018;34:330–335. doi: 10.1097/MOG.0000000000000456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tenner S, Baillie J, DeWitt J, Vege SS. American college of gastroenterology guideline: management of acute pancreatitis. Am J Gastroenterol. 2013;108:1400–1415. doi: 10.1038/ajg.2013.218. [DOI] [PubMed] [Google Scholar]
- 14.Gardner TB, Vege SS, Pearson RK, Chari ST. Fluid resuscitation in acute pancreatitis. Clin Gastroenterol Hepatol. 2008;6:1070–1076. doi: 10.1016/j.cgh.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 15.Komara NL, Paragomi P, Greer PJ, Wilson AS, Breze C, Papachristou GI, et al. Severe acute pancreatitis: capillary permeability model linking systemic inflammation to multiorgan failure. Am J Physiol Liver Physiol. 2020;319:G573–G583. doi: 10.1152/ajpgi.00285.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Klar E, Schratt W, Foitzik T, Buhr H, Herfarth C, Messmer K. Impact of microcirculatory flow pattern changes on the development of acute edematous and necrotizing pancreatitis in rabbit pancreas. Dig Dis Sci. 1994;39:2639–2644. doi: 10.1007/BF02087702. [DOI] [PubMed] [Google Scholar]
- 17.Tenner S. Initial management of acute pancreatitis: critical issues during the first 72 hours. Am J Gastroenterol. 2004;99:2489–2494. doi: 10.1111/j.1572-0241.2004.40329.x. [DOI] [PubMed] [Google Scholar]
- 18.Juvonen PO, Tenhunen JJ, Heino AA, Merasto M, Paajanen HE, Alhava EM, et al. Splanchnic tissue perfusion in acute experimental pancreatitis. Scand J Gastroenterol. 1999;34:308–314. doi: 10.1080/00365529950173744. [DOI] [PubMed] [Google Scholar]
- 19.Tyberg A, Karia K, Gabr M, Desai A, Doshi R, Gaidhane M, et al. Management of pancreatic fluid collections: a comprehensive review of the literature. World J Gastroenterol. 2016;22:2256–2270. doi: 10.3748/wjg.v22.i7.2256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Malbrain MLNG, De Waele JJ, De Keulenaer BL. What every ICU clinician needs to know about the cardiovascular effects caused by abdominal hypertension. Anaesthesiol Intensive Ther. 2015;47:388–399. doi: 10.5603/AIT.a2015.0028. [DOI] [PubMed] [Google Scholar]
- 21.De Laet IE, Malbrain MLNG, De Waele JJ. A Clinician’s guide to management of intra-abdominal hypertension and abdominal compartment syndrome in critically Ill patients. Crit Care. 2020;24:97. doi: 10.1186/s13054-020-2782-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.De Waele JJ, Leppäniemi AK. Intra-abdominal hypertension in acute pancreatitis. World J Surg. 2009;33:1128–1133. doi: 10.1007/s00268-009-9994-5. [DOI] [PubMed] [Google Scholar]
- 23.Isenmann R, Henne-Bruns D, Adler G. Shock and acute pancreatitis. Best Pract Res Clin Gastroenterol. 2003;17:345–355. doi: 10.1016/S1521-6918(03)00016-7. [DOI] [PubMed] [Google Scholar]
- 24.Yegneswaran B, Kostis JB, Pitchumoni CS. Cardiovascular manifestations of acute pancreatitis. J Crit Care. 2011;26(225):e11–e18. doi: 10.1016/j.jcrc.2010.10.013. [DOI] [PubMed] [Google Scholar]
- 25.García M, Calvo JJ. Cardiocirculatory pathophysiological mechanisms in severe acute pancreatitis. World J Gastrointest Pharmacol Ther. 2010;1:9–14. doi: 10.4292/wjgpt.v1.i1.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Agarwal N, Pitchumoni CS. Simplified prognostic criteria in acute pancreatitis. Pancreas. 1986;1:69–73. doi: 10.1097/00006676-198601000-00013. [DOI] [PubMed] [Google Scholar]
- 27.Banks PA. Predictors of severity in acute pancreatitis. Pancreas. 1991;6(Suppl 1):S7–12. doi: 10.1097/00006676-199101001-00003. [DOI] [PubMed] [Google Scholar]
- 28.De-Madaria E, Banks PA, Moya-Hoyo N, Wu BU, Rey-Riveiro M, Acevedo-Piedra NG, et al. Early factors associated with fluid sequestration and outcomes of patients with acute pancreatitis. Clin Gastroenterol Hepatol. 2014;12:997–1002. doi: 10.1016/j.cgh.2013.10.017. [DOI] [PubMed] [Google Scholar]
- 29.Sauven P, Playforth MJ, Evans M, Pollock AV. Fluid sequestration: an early indicator of mortality in acute pancreatitis. Br J Surg. 1986;73:799–800. doi: 10.1002/bjs.1800731013. [DOI] [PubMed] [Google Scholar]
- 30.Takeda T, Nakai Y, Mizuno S, Suzuki T, Sato T, Hakuta R, et al. Fluid sequestration is a useful parameter in the early identification of severe disease of acute pancreatitis. J Gastroenterol Springer Japan. 2019;54:359–366. doi: 10.1007/s00535-018-1531-6. [DOI] [PubMed] [Google Scholar]
- 31.Ranson JHC. Risk factors in acute pancreatitis. Hosp Pract. 1985;20:69–73. doi: 10.1080/21548331.1985.11703034. [DOI] [PubMed] [Google Scholar]
- 32.Crockett SD, Wani S, Gardner TB, Falck-Ytter Y, Barkun AN, American Gastroenterological Association Institute Clinical Guidelines Committee American gastroenterological association institute guideline on initial management of acute pancreatitis. Gastroenterology. 2018;154:1096–1101. doi: 10.1053/j.gastro.2018.01.032. [DOI] [PubMed] [Google Scholar]
- 33.Working Group IAP/APA Acute Pancreatitis Guidelines IAP/APA evidence-based guidelines for the management of acute pancreatitis. Pancreatology. 2013;13:e1–15. doi: 10.1016/j.pan.2013.07.063. [DOI] [PubMed] [Google Scholar]
- 34.Yokoe M, Takada T, Mayumi T, Yoshida M, Isaji S, Wada K, et al. Japanese guidelines for the management of acute pancreatitis: Japanese guidelines 2015. J Hepatobiliary Pancreat Sci. 2015;22:405–432. doi: 10.1002/jhbp.259. [DOI] [PubMed] [Google Scholar]
- 35.Leppäniemi A, Tolonen M, Tarasconi A, Segovia-Lohse H, Gamberini E, Kirkpatrick AW, et al. 2019 WSES guidelines for the management of severe acute pancreatitis. World J Emerg Surg. 2019;14:27. doi: 10.1186/s13017-019-0247-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pezzilli R, Zerbi A, Campra D, Capurso G, Golfieri R, Arcidiacono PG, et al. Consensus guidelines on severe acute pancreatitis. Dig Liver Dis. 2015;47:532–543. doi: 10.1016/j.dld.2015.03.022. [DOI] [PubMed] [Google Scholar]
- 37.Working Party of the British Society of Gastroenterology. Association of Surgeons of Great Britain and Ireland. Pancreatic Society of Great Britain and Ireland. Association of Upper GI Surgeons of Great Britain and Ireland UK guidelines for the management of acute pancreatitis. Gut. 2005;54:iii1–9. doi: 10.1136/gut.2004.057026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Haydock MD, Mittal A, Wilms HR, Phillips A, Petrov MS, Windsor JA. Fluid therapy in acute pancreatitis: anybody’s guess. Ann Surg. 2013;257:182–188. doi: 10.1097/SLA.0b013e31827773ff. [DOI] [PubMed] [Google Scholar]
- 39.Gad MM, Simons-Linares CR. Is aggressive intravenous fluid resuscitation beneficial in acute pancreatitis? A meta-analysis of randomized control trials and cohort studies. World J Gastroenterol. 2020;26:1098–1106. doi: 10.3748/wjg.v26.i10.1098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.De Madaria E, Martínez J, Pérez-Mateo M. The dynamic nature of fluid resuscitation in acute pancreatitis. Clin Gastroenterol Hepatol. 2012;10:95–96. doi: 10.1016/j.cgh.2011.08.020. [DOI] [PubMed] [Google Scholar]
- 41.Beger HG, Rau BM. Severe acute pancreatitis: clinical course and management. World J Gastroenterol. 2007;13:5043–5051. doi: 10.3748/wjg.v13.i38.5043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sinha A, Vázquez NQ, Faghih M, Afghani E, Zaheer A, Khashab MA, et al. Early predictors of fluid sequestration in acute pancreatitis. Pancreas. 2016;45:306–310. doi: 10.1097/MPA.0000000000000444. [DOI] [PubMed] [Google Scholar]
- 43.De-Madaria E, Garg PK. Fluid therapy in acute pancreatitis—aggressive or adequate? Time for reappraisal. Pancreatology. 2014;14:433–435. doi: 10.1016/j.pan.2014.09.008. [DOI] [PubMed] [Google Scholar]
- 44.Sarr MG. Early fluid “resuscitation/therapy” in acute pancreatitis. Ann Surg. 2013;257:189–190. doi: 10.1097/SLA.0b013e318280e19e. [DOI] [PubMed] [Google Scholar]
- 45.Zhao G, Zhang J-G, Wu H-S, Tao J, Qin Q, Deng S-C, et al. Effects of different resuscitation fluid on severe acute pancreatitis. World J Gastroenterol. 2013;19:2044–2052. doi: 10.3748/wjg.v19.i13.2044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.De-Madaria E, Herrera-Marante I, González-Camacho V, Bonjoch L, Quesada-Vázquez N, Almenta-Saavedra I, et al. Fluid resuscitation with lactated Ringer’s solution vs normal saline in acute pancreatitis: A triple-blind, randomized, controlled trial. United Eur Gastroenterol J. 2018;6:63–72. doi: 10.1177/2050640617707864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wu BU, Hwang JQ, Gardner TH, Repas K, Delee R, Yu S, et al. Lactated ringer’s solution reduces systemic inflammation compared with saline in patients with acute pancreatitis. Clin Gastroenterol Hepatol. 2011;9:710–717.e1. doi: 10.1016/j.cgh.2011.04.026. [DOI] [PubMed] [Google Scholar]
- 48.Gardner TB, Vege SS, Chari ST, Petersen BT, Topazian MD, Clain JE, et al. Faster rate of initial fluid resuscitation in severe acute pancreatitis diminishes in-hospital mortality. Pancreatology. 2009;9:770–776. doi: 10.1159/000210022. [DOI] [PubMed] [Google Scholar]
- 49.Warndorf MG, Kurtzman JT, Bartel MJ, Cox M, Mackenzie T, Robinson S, et al. Early fluid resuscitation reduces morbidity among patients with acute pancreatitis. Clin Gastroenterol Hepatol. 2011;9:705–709. doi: 10.1016/j.cgh.2011.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wall I, Badalov N, Baradarian R, Iswara K, Li JJ, Tenner S. Decreased mortality in acute pancreatitis related to early aggressive hydration. Pancreas. 2011;40:547–550. doi: 10.1097/MPA.0b013e318215368d. [DOI] [PubMed] [Google Scholar]
- 51.Yamashita T, Horibe M, Sanui M, Sasaki M, Sawano H, Goto T, et al. Large volume fluid resuscitation for severe acute pancreatitis is associated with reduced mortality: a multicenter retrospective study. J Clin Gastroenterol. 2019;53:385–391. doi: 10.1097/MCG.0000000000001046. [DOI] [PubMed] [Google Scholar]
- 52.Hirota M, Mayumi T, Shimosegawa T. Acute pancreatitis bundles: 10 clinical regulations for the early management of patients with severe acute pancreatitis in Japan. J Hepatobiliary Pancreat Sci. 2014;21:829–830. doi: 10.1002/jhbp.163. [DOI] [PubMed] [Google Scholar]
- 53.Knol JA, Inman MG, Strodel WE, Eckhauser FE. Pancreatic response to crystalloid resuscitation in experimental pancreatitis. J Surg Res. 1987;43:387–392. doi: 10.1016/0022-4804(87)90095-3. [DOI] [PubMed] [Google Scholar]
- 54.Kerner T, Vollmar B, Menger MD, Waldner H, Messmer K. Determinants of pancreatic microcirculation in acute pancreatitis in rats. J Surg Res. 1996;62:165–171. doi: 10.1006/jsre.1996.0190. [DOI] [PubMed] [Google Scholar]
- 55.Niederau C, Crass RA, Silver G, Ferrell LD, Grendell JH. Therapeutic regimens in acute experimental hemorrhagic pancreatitis. Effects of hydration, oxygenation, peritoneal lavage, and a potent protease inhibitor. Gastroenterology. 1988;95:1648–1657. doi: 10.1016/S0016-5085(88)80091-X. [DOI] [PubMed] [Google Scholar]
- 56.Banks PA, Freeman ML. Practice guidelines in acute pancreatitis. Am J Gastroenterol. 2006;101:2379–2400. doi: 10.1111/j.1572-0241.2006.00856.x. [DOI] [PubMed] [Google Scholar]
- 57.Koutroumpakis E, Wu BU, Bakker OJ, Dudekula A, Singh VK, Besselink MG, et al. Admission hematocrit and rise in blood urea nitrogen at 24 h outperform other laboratory markers in predicting persistent organ failure and pancreatic necrosis in acute pancreatitis: a post Hoc analysis of three large prospective databases. Am J Gastroenterol. 2015;110:1707–1716. doi: 10.1038/ajg.2015.370. [DOI] [PubMed] [Google Scholar]
- 58.Brown A, Orav J, Banks PA. Hemoconcentration is an early marker for organ failure and necrotizing pancreatitis. Pancreas. 2000;20:367–372. doi: 10.1097/00006676-200005000-00005. [DOI] [PubMed] [Google Scholar]
- 59.Baillargeon JD, Orav J, Ramagopal V, Tenner SM, Banks PA. Hemoconcentration as an early risk factor for necrotizing pancreatitis. Am J Gastroenterol. 1998;93:2130–2134. doi: 10.1111/j.1572-0241.1998.00608.x. [DOI] [PubMed] [Google Scholar]
- 60.Brown A, Baillargeon J-D, Hughes MD, Banks PA. Can fluid resuscitation prevent pancreatic necrosis in severe acute pancreatitis? Pancreatology. 2002;2:104–107. doi: 10.1159/000055899. [DOI] [PubMed] [Google Scholar]
- 61.Wu BU, Bakker OJ, Papachristou GI, Besselink MG, Repas K, van Santvoort HC, et al. Blood urea nitrogen in the early assessment of acute pancreatitis: an international validation study. Arch Intern Med. 2011;171:669–676. doi: 10.1001/archinternmed.2011.126. [DOI] [PubMed] [Google Scholar]
- 62.Gardner TB. BUN Level as a marker of severity in acute pancreatitis: simple, universal, and accurate. Arch Intern Med. 2011;171:676–677. doi: 10.1001/archinternmed.2011.125. [DOI] [PubMed] [Google Scholar]
- 63.Wu BU, Johannes RS, Sun X, Tabak Y, Conwell DL, Banks PA. The early prediction of mortality in acute pancreatitis: a large population-based study. Gut. 2008;57:1698–1703. doi: 10.1136/gut.2008.152702. [DOI] [PubMed] [Google Scholar]
- 64.Wu BU, Johannes RS, Conwell DL, Banks PA. Early hemoconcentration predicts increased mortality only among transferred patients with acute pancreatitis. Pancreatology. 2009;9:639–643. doi: 10.1159/000181175. [DOI] [PubMed] [Google Scholar]
- 65.Wu BU, Banks PA. Clinical management of patients with acute pancreatitis. Gastroenterology. 2013;144:1272–1281. doi: 10.1053/j.gastro.2013.01.075. [DOI] [PubMed] [Google Scholar]
- 66.DiMagno MJ. Clinical update on fluid therapy and nutritional support in acute pancreatitis. Pancreatology. 2015;15:583–588. doi: 10.1016/j.pan.2015.09.005. [DOI] [PubMed] [Google Scholar]
- 67.Aggarwal A. Fluid resuscitation in acute pancreatitis. World J Gastroenterol. 2014;20:18092. doi: 10.3748/wjg.v20.i48.18092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Bortolotti P, Saulnier F, Colling D, Redheuil A, Preau S. New tools for optimizing fluid resuscitation in acute pancreatitis. World J Gastroenterol. 2014;20:16113. doi: 10.3748/wjg.v20.i43.16113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Lee PJ, Papachristou GI. New insights into acute pancreatitis. Nat Rev Gastroenterol Hepatol. 2019;16:479–496. doi: 10.1038/s41575-019-0158-2. [DOI] [PubMed] [Google Scholar]
- 70.De Waele E, Malbrain MLNG, Spapen HD. How to deal with severe acute pancreatitis in the critically ill. Curr Opin Crit Care. 2019;25:150–156. doi: 10.1097/MCC.0000000000000596. [DOI] [PubMed] [Google Scholar]
- 71.Vincent JL. Fluid management in the critically ill. Kidney Int. 2019;96:52–57. doi: 10.1016/j.kint.2018.11.047. [DOI] [PubMed] [Google Scholar]
- 72.Malbrain MLNG, Marik PE, Witters I, Cordemans C, Kirkpatrick AW, Roberts DJ, et al. Fluid overload, de-resuscitation, and outcomes in critically ill or injured patients: a systematic review with suggestions for clinical practice. Anaesthesiol Intensive Ther. 2014;46:361–380. doi: 10.5603/AIT.2014.0060. [DOI] [PubMed] [Google Scholar]
- 73.Duchesne JC, Kaplan LJ, Balogh ZJ, Malbrain MLNG. Role of permissive hypotension, hypertonic resuscitation and the global increased permeability syndrome in patients with severe hemorrhage: adjuncts to damage control resuscitation to prevent intra-abdominal hypertension. Anaesthesiol Intensive Ther. 2015;47:143–155. doi: 10.5603/AIT.a2014.0052. [DOI] [PubMed] [Google Scholar]
- 74.De-Madaria E, Soler-Sala G, Sánchez-Payá J, Lopez-Font I, Martínez J, Gómez-Escolar L, et al. Influence of fluid therapy on the prognosis of acute pancreatitis: a prospective cohort study. Am J Gastroenterol. 2011;106:1843–1850. doi: 10.1038/ajg.2011.236. [DOI] [PubMed] [Google Scholar]
- 75.Eckerwall G, Olin H, Andersson B, Andersson R. Fluid resuscitation and nutritional support during severe acute pancreatitis in the past: What have we learned and how can we do better? Clin Nutr. 2006;25:497–504. doi: 10.1016/j.clnu.2005.10.012. [DOI] [PubMed] [Google Scholar]
- 76.Kuwabara K, Matsuda S, Fushimi K, Ishikawa KB, Horiguchi H, Fujimori K. Early crystalloid fluid volume management in acute pancreatitis: association with mortality and organ failure. Pancreatology. 2011;11:351–361. doi: 10.1159/000328965. [DOI] [PubMed] [Google Scholar]
- 77.Singh VK, Gardner TB, Papachristou GI, Rey-Riveiro M, Faghih M, Koutroumpakis E, et al. An international multicenter study of early intravenous fluid administration and outcome in acute pancreatitis. United Eur Gastroenterol J. 2017;5:491–498. doi: 10.1177/2050640616671077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Mao E, Tang Y, Fei J, Qin S, Wu J, Li L, et al. Fluid therapy for severe acute pancreatitis in acute response stage. Chin Med J. 2009;122:169–173. [PubMed] [Google Scholar]
- 79.Mao E-Q, Fei J, Peng Y-B, Huang J, Tang Y-Q, Zhang S-D. Rapid hemodilution is associated with increased sepsis and mortality among patients with severe acute pancreatitis. Chin Med J. 2010;123:1639–1644. [PubMed] [Google Scholar]
- 80.Thomson A. Intravenous fluid therapy in acute pancreatitis: a critical review of the randomized trials. ANZ J Surg. 2018;88:690–696. doi: 10.1111/ans.14320. [DOI] [PubMed] [Google Scholar]
- 81.Trikudanathan G, Navaneethan U, Vege SS. Current controversies in fluid resuscitation in acute pancreatitis. Pancreas. 2012;41:827–834. doi: 10.1097/MPA.0b013e31824c1598. [DOI] [PubMed] [Google Scholar]
- 82.Fisher JM, Gardner TB. The “Golden Hours” of management in acute pancreatitis. Am J Gastroenterol. 2012;107:1146–1150. doi: 10.1038/ajg.2012.91. [DOI] [PubMed] [Google Scholar]
- 83.Forsmark CE, Swaroop Vege S, Wilcox CM. Acute Pancreatitis. N Engl J Med. 2016;375:1972–1981. doi: 10.1056/NEJMra1505202. [DOI] [PubMed] [Google Scholar]
- 84.Finfer S, Myburgh J, Bellomo R. Intravenous fluid therapy in critically ill adults. Nat Rev Nephrol. 2018;14:541–557. doi: 10.1038/s41581-018-0044-0. [DOI] [PubMed] [Google Scholar]
- 85.Langer T, Ferrari M, Zazzeron L, Gattinoni L, Caironi P. Effects of intravenous solutions on acid-base equilibrium: from crystalloids to colloids and blood components. Anaesthesiol Intensive Ther. 2014;46:350–360. doi: 10.5603/AIT.2014.0059. [DOI] [PubMed] [Google Scholar]
- 86.Langer T, Limuti R, Tommasino C, van Regenmortel N, Duval ELIM, Caironi P, et al. Intravenous fluid therapy for hospitalized and critically ill children: rationale, available drugs and possible side effects. Anaesthesiol Intensive Ther. 2018;50:49–58. doi: 10.5603/AIT.a2017.0058. [DOI] [PubMed] [Google Scholar]
- 87.Semler MW, Self WH, Wanderer JP, Ehrenfeld JM, Wang L, Byrne DW, et al. balanced crystalloids versus saline in critically ill adults. N Engl J Med. 2018;378:829–839. doi: 10.1056/NEJMoa1711584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Ye B, Mao W, Chen Y, Tong Z, Li G, Zhou J, et al. Aggressive resuscitation is associated with the development of acute kidney injury in acute pancreatitis. Dig Dis Sci. 2019;64:544–552. doi: 10.1007/s10620-018-5328-5. [DOI] [PubMed] [Google Scholar]
- 89.Martin C, Cortegiani A, Gregoretti C, Martin-Loeches I, Ichai C, Leone M, et al. Choice of fluids in critically ill patients. BMC Anesthesiol. 2018;18:200. doi: 10.1186/s12871-018-0669-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Morgan TJ. The meaning of acid-base abnormalities in the intensive care unit: part III—effects of fluid administration. Crit Care. 2005;9:204–211. doi: 10.1186/cc2946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Kaplan LJ, Frangos S. Clinical review: acid-base abnormalities in the intensive care unit—part II. Crit Care. 2005;9:198–203. doi: 10.1186/cc2912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Langer T, Brusatori S, Carlesso E, Zadek F, Brambilla P, Ferraris Fusarini C, et al. Low noncarbonic buffer power amplifies acute respiratory acid-base disorders in patients with sepsis: an in vitro study. J Appl Physiol. 2021;131:464–473. doi: 10.1152/japplphysiol.00787.2020. [DOI] [PubMed] [Google Scholar]
- 93.Langer T, Carlesso E, Protti A, Monti M, Comini B, Zani L, et al. In vivo conditioning of acid–base equilibrium by crystalloid solutions: an experimental study on pigs. Intensive Care Med. 2012;38:686–693. doi: 10.1007/s00134-011-2455-2. [DOI] [PubMed] [Google Scholar]
- 94.Choosakul S, Harinwan K, Chirapongsathorn S, Opuchar K, Sanpajit T, Piyanirun W, et al. Comparison of normal saline versus lactated Ringer’s solution for fluid resuscitation in patients with mild acute pancreatitis, a randomized controlled trial. Pancreatology. 2018;18:507–512. doi: 10.1016/j.pan.2018.04.016. [DOI] [PubMed] [Google Scholar]
- 95.Aboelsoud MM, Siddique O, Morales A, Seol Y, Al-Qadi MO. Fluid choice matters in critically-ill patients with acute pancreatitis: lactated ringer’s vs isotonic saline. R I Med J. 2016;99:39–42. [PubMed] [Google Scholar]
- 96.Iqbal U, Anwar H, Scribani M. Ringer’s lactate versus normal saline in acute pancreatitis: a systematic review and meta-analysis. J Dig Dis. 2018;19:335–341. doi: 10.1111/1751-2980.12606. [DOI] [PubMed] [Google Scholar]
- 97.Lee A, Ko C, Buitrago C, Hiramoto B, Hilson L, Buxbaum J, et al. Lactated Ringers vs normal saline resuscitation for mild acute pancreatitis: a randomized trial. Gastroenterology. 2021;160:955–957.e4. doi: 10.1053/j.gastro.2020.10.044. [DOI] [PubMed] [Google Scholar]
- 98.Hoque R, Farooq A, Ghani A, Gorelick F, Mehal WZ. Lactate reduces liver and pancreatic injury in toll-like receptor—and inflammasome-mediated inflammation via GPR81-mediated suppression of innate immunity. Gastroenterology. 2014;146:1763–1774. doi: 10.1053/j.gastro.2014.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Bhoomagoud M, Jung T, Atladottir J, Kolodecik TR, Shugrue C, Chaudhuri A, et al. Reducing extracellular pH sensitizes the acinar cell to secretagogue-induced pancreatitis responses in rats. Gastroenterology. 2009;137:1083–1092. doi: 10.1053/j.gastro.2009.05.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Van Regenmortel N, Hendrickx S, Roelant E, Baar I, Dams K, Van Vlimmeren K, et al. 154 compared to 54 mmol per liter of sodium in intravenous maintenance fluid therapy for adult patients undergoing major thoracic surgery (TOPMAST): a single-center randomized controlled double-blind trial. Intensive Care Med. 2019;45:1422–1432. doi: 10.1007/s00134-019-05772-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Van Regenmortel N, Moers L, Langer T, Roelant E, De Weerdt T, Caironi P, et al. Fluid-induced harm in the hospital: look beyond volume and start considering sodium. From physiology towards recommendations for daily practice in hospitalized adults. Ann Intensive Care. 2021;11:79. doi: 10.1186/s13613-021-00851-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Van Regenmortel N, Langer T, De Weerdt T, Roelant E, Malbrain M, Van den Wyngaert T, et al. Effect of sodium administration on fluid balance and sodium balance in health and the perioperative setting. Extended summary with additional insights from the MIHMoSA and TOPMAST studies. J Crit Care. 2022;67:157–165. doi: 10.1016/j.jcrc.2021.10.022. [DOI] [PubMed] [Google Scholar]
- 103.Hahn RG. Adverse effects of crystalloid and colloid fluids. Anaesthesiol Intensive Ther. 2017;49:303–308. doi: 10.5603/AIT.a2017.0045. [DOI] [PubMed] [Google Scholar]
- 104.Schmidt J, Huch K, Mithöfer K, Hotz HG, Sinn HP, Buhr HJ, et al. Benefits of various dextrans after delayed therapy in necrotizing pancreatitis of the rat. Intensive Care Med. 1996;22:1207–1213. doi: 10.1007/BF01709338. [DOI] [PubMed] [Google Scholar]
- 105.Klar E, Herfarth C, Messmer K. Therapeutic effect of isovolemic hemodilution with dextran 60 on the impairment of pancreatic microcirculation in acute biliary pancreatitis. Ann Surg. 1990;211:346–353. doi: 10.1097/00000658-199003000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Myburgh JA, Mythen MG. Resuscitation fluids. N Engl J Med. 2013;369:1243–1251. doi: 10.1056/NEJMra1208627. [DOI] [PubMed] [Google Scholar]
- 107.Myburgh JA, Finfer S, Bellomo R, Billot L, Cass A, Gattas D, et al. Hydroxyethyl starch or saline for fluid resuscitation in intensive care. N Engl J Med. 2012;367:1901–1911. doi: 10.1056/NEJMoa1209759. [DOI] [PubMed] [Google Scholar]
- 108.European Medicines Agency (EMA). Hydroxyethyl-starch solutions ( HES ) no longer to be used in patients with sepsis or burn injuries or in critically ill patients. 2014; https://www.ema.europa.eu/en/documents/referral/hydroxyethyl-starch-solutions-hes-no-longer-be-used-patients-sepsis-burn-injuries-critically-ill_en-0.pdf. Accessed 24 Feb 2022.
- 109.Vege SS, DiMagno MJ, Forsmark CE, Martel M, Barkun AN. Initial medical treatment of acute pancreatitis: american gastroenterological association institute technical review. Gastroenterology. 2018;154:1103–1139. doi: 10.1053/j.gastro.2018.01.031. [DOI] [PubMed] [Google Scholar]
- 110.Stigliano S, Sternby H, de Madaria E, Capurso G, Petrov MS. Early management of acute pancreatitis: a review of the best evidence. Dig Liver Dis. 2017;49:585–594. doi: 10.1016/j.dld.2017.01.168. [DOI] [PubMed] [Google Scholar]
- 111.Di Martino M, Van Laarhoven S, Ielpo B, Ramia JM, Manuel-Vázquez A, Martínez-Pérez A, Pavel M, Beltran Miranda P, Orti-Rodríguez R, de la Serna S, Ortega Rabbione GJ, Sanz-Garcia A, Martín-Pérez E. Systematic review and meta-analysis of fluid therapy protocols in acute pancreatitis: type, rate and route. HPB. 2021;23(11):1629–1638. doi: 10.1016/j.hpb.2021.06.426. [DOI] [PubMed] [Google Scholar]
- 112.Maraví Poma E, Zubia Olascoaga F, Petrov MS, Navarro Soto S, Laplaza Santos C, Morales Alava F, SEMICYUC et al. Recommendations for intensive care management of acute pancreatitis. Med intensiva. 2012;2013(37):163–179. doi: 10.1016/j.medin.2013.01.007. [DOI] [PubMed] [Google Scholar]
- 113.Huber W, Malbrain MLNG. Goal-directed fluid resuscitation in acute pancreatitis: shedding light on the penumbra by dynamic markers of preload? Intensive Care Med. 2013;39:784–786. doi: 10.1007/s00134-012-2783-x. [DOI] [PubMed] [Google Scholar]
- 114.Malbrain MLNG, Langer T, Annane D, Gattinoni L, Elbers P, Hahn RG, et al. Intravenous fluid therapy in the perioperative and critical care setting: executive summary of the international fluid academy (IFA) Ann Intensive Care. 2020;10:64. doi: 10.1186/s13613-020-00679-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Wilkman E, Kaukonen K-M, Pettilä V, Kuitunen A, Varpula M. Early hemodynamic variables and outcome in severe acute pancreatitis: a retrospective single-center cohort study. Pancreas. 2013;42:272–278. doi: 10.1097/MPA.0b013e318264c9f7. [DOI] [PubMed] [Google Scholar]
- 116.Hirota M, Takada T, Kitamura N, Ito T, Hirata K, Yoshida M, et al. Fundamental and intensive care of acute pancreatitis. J Hepatobiliary Pancreat Sci. 2010;17:45–52. doi: 10.1007/s00534-009-0210-7. [DOI] [PubMed] [Google Scholar]
- 117.Nassar TI, Qunibi WY. AKI Associated with acute pancreatitis. Clin J Am Soc Nephrol. 2019;14:1106–1115. doi: 10.2215/CJN.13191118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Hariri G, Joffre J, Leblanc G, et al. Narrative review: clinical assessment of peripheral tissue perfusion in septic shock. Ann Intensive Care. 2019;9:37. doi: 10.1186/s13613-019-0511-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Hofkens P-J, Verrijcken A, Merveille K, Neirynck S, Van Regenmortel N, De Laet I, et al. Common pitfalls and tips and tricks to get the most out of your transpulmonary thermodilution device: results of a survey and state-of-the-art review. Anaesthesiol Intensive Ther. 2015;47:89–116. doi: 10.5603/AIT.a2014.0068. [DOI] [PubMed] [Google Scholar]
- 120.Huber W, Umgelter A, Reindl W, Franzen M, Schmidt C, von Delius S, et al. Volume assessment in patients with necrotizing pancreatitis: a comparison of intrathoracic blood volume index, central venous pressure, and hematocrit, and their correlation to cardiac index and extravascular lung water index. Crit Care Med. 2008;36:2348–2354. doi: 10.1097/CCM.0b013e3181809928. [DOI] [PubMed] [Google Scholar]
- 121.Sun Y, Lu Z-H, Zhang X-S, Geng X-P, Cao L-J, Yin L. The effects of fluid resuscitation according to PiCCO on the early stage of severe acute pancreatitis. Pancreatology. 2015;15:497–502. doi: 10.1016/j.pan.2015.06.006. [DOI] [PubMed] [Google Scholar]
- 122.Trepte CJC, Bachmann KA, Stork JH, Friedheim TJ, Hinsch A, Goepfert MS, et al. The impact of early goal-directed fluid management on survival in an experimental model of severe acute pancreatitis. Intensive Care Med. 2013;39:717–726. doi: 10.1007/s00134-012-2775-x. [DOI] [PubMed] [Google Scholar]
- 123.Vincent J-L, De Backer D. Circulatory shock. N Engl J Med. 2013;369:1726–1734. doi: 10.1056/NEJMra1208943. [DOI] [PubMed] [Google Scholar]
- 124.Mallédant Y, Malbrain MLNG, Reuter DA. What’s new in the management of severe acute pancreatitis? Intensive Care Med. 2015;41:1957–1960. doi: 10.1007/s00134-015-3903-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.De Waele JJ, Ejike JC, Leppäniemi A, De Keulenaer BL, De Laet I, Kirkpatrick AW, et al. Intra-abdominal hypertension and abdominal compartment syndrome in pancreatitis, paediatrics, and trauma. Anaesthesiol Intensive Ther. 2015;47:219–227. doi: 10.5603/AIT.a2015.0027. [DOI] [PubMed] [Google Scholar]
- 126.Jacobs R, Lochy S, Malbrain MLNG. Phenylephrine-induced recruitable preload from the venous side. J Clin Monit Comput. 2019;33(3):373–376. doi: 10.1007/s10877-018-0225-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Beger HG, Bittner R, Büchler M, Hess W, Schmitz JE. Hemodynamic data pattern in patients with acute pancreatitis. Gastroenterology. 1986;90(1):74–79. doi: 10.1016/0016-5085(86)90077-6. [DOI] [PubMed] [Google Scholar]
- 128.Di Carlo V, Nespoli A, Chiesa R, Staudacher C, Cristallo M, Bevilacqua G, Staudacher V. Hemodynamic and metabolic impairment in acute pancreatitis. World J Surg. 1981;5(3):329–339. doi: 10.1007/BF01657989. [DOI] [PubMed] [Google Scholar]
- 129.Jacobs R, Jonckheer J, Malbrain MLNG. Fluid overload FADEs away! Time for fluid stewardship. J Crit Care. 2018;48:458–461. doi: 10.1016/j.jcrc.2018.08.027. [DOI] [PubMed] [Google Scholar]
- 130.de Madaria E, Buxbaum JL, Maisonneuve P, de GarcíaParedes GA, Zapater P, Guilabert L, et al. Aggressive or moderate fluid resuscitation in acute pancreatitis. N Engl J Med. 2022;387(11):989–1000. doi: 10.1056/NEJMoa2202884. [DOI] [PubMed] [Google Scholar]
- 131.Buxbaum JL, Quezada M, Da B, Jani N, Lane C, Mwengela D, et al. Early aggressive hydration hastens clinical improvement in mild acute pancreatitis. Am J Gastroenterol. 2017;112:797–803. doi: 10.1038/ajg.2017.40. [DOI] [PubMed] [Google Scholar]
- 132.Nasr JY, Papachristou GI. Early fluid resuscitation in acute pancreatitis: a lot more than just fluids. Clin Gastroenterol Hepatol. 2011;9:633–634. doi: 10.1016/j.cgh.2011.03.010. [DOI] [PubMed] [Google Scholar]
- 133.Pandol SJ, Saluja AK, Imrie CW, Banks PA. Acute pancreatitis: bench to the bedside. Gastroenterology. 2007;132:1127–1151. doi: 10.1053/j.gastro.2007.01.055. [DOI] [PubMed] [Google Scholar]
- 134.Li L, Jin T, Wen S, Shi N, Zhang R, Zhu P, et al. Early rapid fluid therapy is associated with increased rate of noninvasive positive-pressure ventilation in hemoconcentrated patients with severe acute pancreatitis. Dig Dis Sci. 2020;65:2700–2711. doi: 10.1007/s10620-019-05985-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Cuéllar-Monterrubio JE, Monreal-Robles R, González-Moreno EI, Borjas-Almaguer OD, Herrera-Elizondo JL, García-Compean D, et al. Nonaggressive versus aggressive intravenous fluid therapy in acute pancreatitis with more than 24 hours from disease onset. Pancreas. 2020;49:579–583. doi: 10.1097/MPA.0000000000001528. [DOI] [PubMed] [Google Scholar]
- 136.Weitz G, Woitalla J, Wellhöner P, Schmidt K, Büning J, Fellermann K. Detrimental effect of high volume fluid administration in acute pancreatitis—a retrospective analysis of 391 patients. Pancreatology. 2014;14:478–483. doi: 10.1016/j.pan.2014.07.016. [DOI] [PubMed] [Google Scholar]
- 137.Mole DJ, Hall A, McKeown D, Garden OJ, Parks RW. Detailed fluid resuscitation profiles in patients with severe acute pancreatitis. HPB. 2011;13:51–58. doi: 10.1111/j.1477-2574.2010.00241.x. [DOI] [PMC free article] [PubMed] [Google Scholar]