Abstract
Objective
To evaluate the effectiveness and safety of transurethral resection of the prostate (TURP), holmium laser enucleation of the prostate (HoLEP) and thulium laser enucleation of the prostate (ThuLEP) in the treatment of benign prostatic hyperplasia using a network Meta-analysis.
Methods
Randomized controlled trials of TURP, HoLEP and ThuLEP for benign prostatic hyperplasia were collected by computerized searches of databases including CNKI, WANFANG, VIP, PubMed, The Cochrane Library, the Web of Science and Embase, with a search time frame of build to January 2022. The literature was screened and data was extracted by two investigators separately, while the risk of bias of the included studies was evaluated before systematic evaluation and network meta-analysis using ADDIS 1.16.8 software and RevMan 5.3 software.
Results
A total of 27 RCTs with a total of 3335 patients were involved. The results of the network meta-analysis showed that ThuLEP was better than the remaining two procedures in terms of enhancing patients' subjective perception and improving objective indicators, and the incidence of adverse events such as postoperative urethral stricture and urinary incontinence was lower compared with that of conventional TURP in both short- and long-term postoperative follow-ups.
Conclusion
As ThuLEP is effective, safe, and featured with few postoperative complications, it can be the preferred surgical procedure for prostate enlargement. Nevertheless, because of the limited number of studies included, more-sample, multicenter, double-blind clinical randomized controlled trials are required in the future to further verify the findings of the present study.
Keywords: Network meta-analysis, Benign prostatic hyperplasia, Laser, Randomized controlled trials
Network meta-analysis; Benign prostatic hyperplasia; Laser; Randomized controlled trials.
1. Introduction
Benign prostatic hyperplasia (BPH) is a common urological disorder in middle-aged and elderly men, often manifesting as lower urinary tract symptoms including urinary frequency, urgency and difficulty in urination, and with an aging population, the incidence and prevalence of BPH increase each year [1]. Compared with the conservative treatment with drugs, the effect of surgery is obvious and definite, and also receives attention [2]. Transurethral resection of the prostate (TURP) has long been considered the gold standard for the surgical treatment of BPH, but it is related to a number of complications, such as bleeding, urethral stricture, transurethral resection syndrome (TURS). However, because of the complications associated with TURP, such as bleeding, urethral stricture and TURS, there has been a search for a viable alternative to surgery [3].
Holmium laser enucleation of the prostate (HoLEP) was first used by Gilling in 1998 for treating BPH and showed good results [4]. With the dramatic increase in use in recent years, it is even considered the best procedure for treating prostate enlargement in the 21st century [5]. The emerging thulium laser has a shorter wavelength and has been found to have the advantages of smaller size, more efficient operation and more precise tissue incision compared to the holmium laser [6]. Thulium laser enucleation of the prostate (ThuLEP) was first proposed in 2010 by Hermann et al. and is believed to achieve maximum surgical results and minimal side effects regardless of prostate size [7]. In addition, Bozzini et al. found in a multicenter prospective randomized controlled trial (RCT) that HoLEP and ThuLEP had the same surgical outcome for BPH, but the latter reduced intraoperative blood loss and early postoperative complications [8]. Furthermore, TURP was a common clinical procedure for prostate enlargement in the past. Whereas, HoLEP and ThuLEP, as emerging surgical procedures, also occupy an important position in clinical practice, but it is not yet possible to distinguish the advantages and disadvantages of the two laser procedures [9].
Therefore, this study was conducted to assess the efficacy and safety of TURP, HoLEP and ThuLEP in the treatment of prostate enlargement by collecting relevant literature and making reticulated Meta-analysis, hoping to provide clinical reference.
2. Materials and methods
2.1. Search strategy
Computer searches of databases such as CNKI, WANFANG, VIP, PubMed, Embase, the Cochrane Library and the Web of Science were performed to collect RCTs of TURP, HoLEP and ThuLEP for benign prostatic hyperplasia, with a search time frame of build to January 2022. Besides, the search was performed based on a combination of subject terms and free words when the search terms included benign prostatic hyperplasia, Holmium laser, Thulium laser, transurethral resection of prostate, and randomized controlled trial.
2.2. Inclusion and exclusion criteria
Inclusion criteria included: (1) literature involving RCTs in English and Chinese that compared TURP, HoLEP, and ThuLEP; (2) cases of BPH that were clearly diagnosed clinically as requiring surgical treatment, excluding those with symptoms of lower urinary tract obstruction caused by neurological lesions; (3) the indexes provided in the literature, such as operative time, maximum flow rate (Qmax), international prostate symptom score (IPSS), post-void residual (PVR) and the quality of life score (QoL). Exclusion criteria included: (1) review literature, animal trials and conferences due to their lack of raw data; (2) patients with comorbidities that affect the evaluation of efficacy, such as oncology, psychological disorders and diabetes mellitus; (3) literature with unavailable or incomplete data; (4) duplicate publications; (5) non-randomized controlled trials, such as cohort studies and case-control studies.
2.3. Data extraction
The following date were collected from literatures: basic information for inclusion in the study, Qmax, PVR, IPSS and QoL, volume of prostate removed, duration of surgery, length of hospital stay, short-term complications: urinary incontinence and reintroduction of the urinary catheter and long-term complications: bladder neck fibrosis and urethral stricture.
2.4. Literature selection
Two evaluators independently screened the literature, submitted and cross-checked the information. Where there was disagreement, the decision was made through discussion or under the assistance of a third party. Specifically, the literature is screened by first reading the title and abstract, and when irrelevant literature is excluded, the full text is further read to decide whether to include it.
2.5. Evaluation of the risk of bias in the included studies
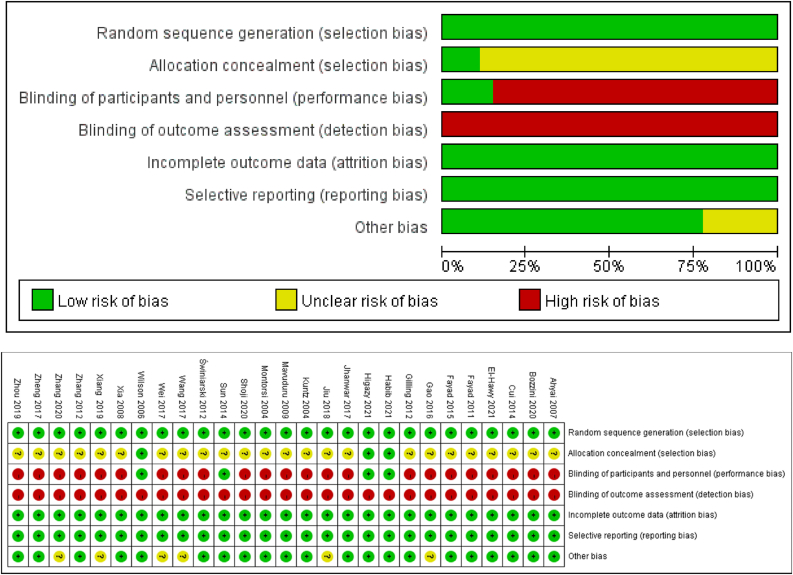
Risk of bias of included studies was assessed by two evaluators in accordance with the Cochrane Handbook Risk of Bias Assessment Tool for RCTs [10].
2.6. Statistical analysis
The Bayesian model-based ADDIS (Aggregate Data Drug Information System, version 1.16.8) software was used for the mesh meta-analysis. The software employs a Markov chain-Monte Carlo (MCMC) method using a Bayesian framework to evaluate the data a prior, thus achieving a mesh meta-analysis. The initial iteration was set at 50 000 iterations, and the deviance information criterion (DIC) was compared between the random effects model and the fixed effects model to determine the degree of fit of the model. Apart from that, the odds ratio (OR) was employed for the dichotomous effects, and the mean difference (MD) was used for the continuous effects, both of which were featured with 95% confidence interval (CI). Additionally, a consistency model was adopted for the reticulated Meta-analysis, and P < 0.05 was considered a statistically significant difference. Moreover, inconsistency was tested using a nodal analysis model, with P > 0.05 indicating no evidence of inconsistency between direct and indirect comparisons. While, convergence of the reticulated Meta-analysis was tested using the potential scale reduced factor (PSRF). If the PSRF was close to 1, the study converged well and the conclusions drawn from the Meta-analysis were reliable.
3. Results
3.1. Literature search results and quality assessment
A preliminary review of 6421 papers from various databases was conducted, and after a screening process, finally, 27 papers included in the analysis [11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37] and involved studies that were all two-by-two comparisons. Besides, the total number of literature on the comparison of HoLEP and TURP was 19 [11, 12, 13, 14, 16, 17, 18, 22, 23, 24, 25, 26, 27, 29, 30, 31, 32, 33, 34] and 5 [15, 19, 21, 35, 36] on ThuLEP and TURP respectively, and 3 on the comparison of HoLEP and ThuLEP [8, 20, 37]. The results of the literature screening process are shown in Figure 1.
Figure 1.
Flow diagram of search in different databases.
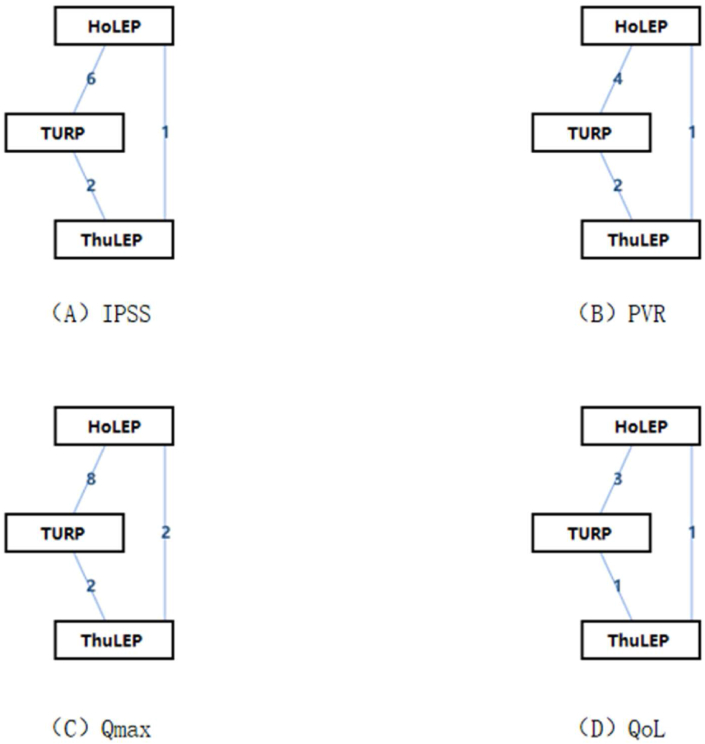
The basic characteristics of the study are shown in Table 1, and the finding of the risk of bias evaluation are presented in Figure 2, while the net relationship diagram of the included interventions with short-term effects is displayed in Figure 3. Other than that, as shown in Table 2, the PSRFs were all close to 1, indicating good convergence. The results of direct and indirect comparisons concerning the included studies were consistent under the nodal analysis model (P > 0.05).
Table 1.
Characteristics of included studies.
| Studies | Location | Interventions | Participants | Age (years) | Prostate volume | Qmax (ml/s) | IPSS | PVR (ml) | QoL | ||||
| Kuntz 2004 | Germany and Egypt | HoLEP | 100 | 68.0 ± 7.3 | 53.5 ± 20.0 | 4.9 ± 3.8 | N/A | 238 ± 163 | N/A | ||||
| TURP | 100 | 68.7 ± 8.2 | 49.9 ± 21.1 | 5.9 ± 3.9 | N/A | 216 ± 177 | N/A | ||||||
| Montorsi 2004 | Italy | HoLEP | 52 | 65.14 | 70.3 ± 36.7 | 8.2 ± 3.2 | 21.6 ± 6.7 | N/A | 4.6 ± 1.1 | ||||
| TURP | 48 | 64.5 | 56.2 ± 19.4 | 7.8 ± 3.6 | 21.9 ± 7.2 | N/A | 4.7 ± 1 | ||||||
| Wilson 2006 | New Zealand | HoLEP | 30 | 71.1 ± 1.1 | 77.8 ± 5.6 | 8.4 ± 0.5 | N/A | N/A | 4.8 ± 0.2 | ||||
| TURP | 30 | 70.3 ± 1.0 | 70.0 ± 5.0 | 8.3 ± 0.4 | N/A | N/A | 4.7 ± 0.2 | ||||||
| Ahyai 2007 | Germany | HoLEP | 100 | 68 | 53.5 | 4.9 ± 3.8 | N/A | 237 ± 163 | N/A | ||||
| TURP | 100 | 68.7 | 49.9 | 5.9 ± 3.9 | N/A | 216 ± 177 | N/A | ||||||
| Xia 2008 | China | ThuLEP | 52 | 68.9 ± 7.7 | 59.2 ± 17.7 | 8.0 ± 2.8 | 21.9 ± 6.7 | 93.1 ± 32.1 | 4.7 ± 0.9 | ||||
| TURP | 48 | 69.3 ± 7.3 | 55.1 ± 16.3 | 8.3 ± 3.0 | 20.8 ± 5.8 | 85.0 ± 36.7 | 4.5 ± 1.1 | ||||||
| Mavuduru 2009 | India | HoLEP | 15 | 69.86 ± 9.6 | 36.53 ± 12.33 | 5.79 ± 2.7 | 22.53 ± 4.79 | 91 ± 30 | N/A | ||||
| TURP | 15 | 66.46 ± 5.79 | 36.33 ± 11.4 | 6.9 ± 2.5 | 21.4 ± 3.7 | 103 ± 27 | N/A | ||||||
| Fayad 2011 | Egypt | HoLEP | 30 | 60.07 ± 4.51 | 76.5 ± 17.22 | 7.39 | 22.55 | N/A | N/A | ||||
| TURP | 30 | 61.2 ± 4.21 | 80.6 ± 17.79 | 6.98 | 22.17 | N/A | N/A | ||||||
| Gilling 2012 | New Zealand | HoLEP | 31 | 71.70 ± 1.10 | 77.68 ± 32.13 | 8.28 ± 2.18 | N/A | 116.14 ± 85.09 | 4.79 ± 1.07 | ||||
| TURP | 30 | 70.30 ± 1.00 | 70.00 ± 27.78 | 8.26 ± 2.18 | N/A | 126.67 ± 116.77 | 4.70 ± 1.10 | ||||||
| Świniarski 2012 | Poland | ThuLEP | 54 | 68.3 ± 6.8 | 62.03 ± 23.7 | 7.73 ± 3.52 | 20.38 ± 2.59 | 166.2 ± 110.5 | 4.7 ± 1.0 | ||||
| TURP | 52 | 69.3 ± 7.2 | 66.5 ± 22 | 8.57 ± 3.61 | 20.85 ± 6.03 | 152.0 ± 112.2 | 4.9 ± 1.0 | ||||||
| Zhang 2012 | China | ThuLEP | 71 | 76.2 ± 9.7 | 46.6 ± 25.2 | 6.87 | 24.97 | 65.06 | 5.56 | ||||
| HoLEP | 62 | 73.4 ± 10.3 | 43.5 ± 23.0 | 7.39 | 22.89 | 64.74 | 5.67 | ||||||
| Cui 2014 | China | ThuLEP | 47 | 67.8 ± 10.1 | 48.0 ± 18.3 | 8.62 ± 3.93 | 21.1 ± 6.2 | 91.9 ± 119.3 | N/A | ||||
| TURP | 49 | 70.4 ± 7.02 | 54.8 ± 27.4 | 8.40 ± 3.5 | 20.2 ± 6.8 | 59.8 ± 106.4 | N/A | ||||||
| Sun 2014 | China | HoLEP | 82 | 72.16 ± 7.53 | N/A | 5.28 ± 1.88 | 24.40 ± 3.78 | 115.83 ± 102.57 | N/A | ||||
| TURP | 82 | 71.91 ± 7.53 | N/A | 5.69 ± 1.42 | 24.55 ± 3.86 | 108.01 ± 115.83 | N/A | ||||||
| Fayad 2015 | Egypt | HoLEP | 60 | 60.85 | 68.15 | 6.9593 | 23.2222 | N/A | N/A | ||||
| TURP | 60 | 60.35 | 67.2 | 6.6291 | 23.4 | N/A | N/A | ||||||
| Gao 2016 | China | HoLEP | 54 | 71.2 ± 6.5 | 48.3 ± 24.5 | N/A | N/A | N/A | N/A | ||||
| TURP | 54 | 71.4 ± 6.6 | 48.3 ± 24.5 | N/A | N/A | N/A | N/A | ||||||
| Jhanwar 2017 | India | HoLEP | 72 | 67.70 ± 7.44 | 75.6 ± 12.84 | 8.4 ± 1.48 | 26.01 ± 2.08 | 184.8 ± 32.2 | N/A | ||||
| TURP | 72 | 66.78 ± 7.81 | 74.5 ± 12.56 | 8.7 ± 1.02 | 25.85 ± 2.22 | 187.1 ± 38.5 | N/A | ||||||
| Wang 2017 | China | HoLEP | 74 | 66.31 ± 8.27 | 76.59 ± 10.13 | 5.84 ± 2.08 | 22.09 ± 4.63 | 69.65 ± 25.71 | N/A | ||||
| TURP | 75 | 66.64 ± 8.55 | 78.04 ± 9.85 | 5.81 ± 2.11 | 21.97 ± 4.61 | 73.37 ± 30.86 | N/A | ||||||
| Wei 2017 | China | HoLEP | 65 | 65.02 ± 9.46 | N/A | N/A | N/A | N/A | N/A | ||||
| TURP | 65 | 66.42 ± 9.67 | N/A | N/A | N/A | N/A | N/A | ||||||
| Zheng 2017 | China | HoLEP | 44 | 69.12 ± 7.51 | N/A | N/A | N/A | N/A | N/A | ||||
| TURP | 44 | 67.82 ± 6.61 | N/A | N/A | N/A | N/A | N/A | ||||||
| Jiu 2018 | China | HoLEP | 49 | 58.65 ± 5.21 | 55.26 ± 9.32 | 8.71 ± 1.13 | 14.25 ± 2.41 | N/A | N/A | ||||
| TURP | 49 | 58.71 ± 5.23 | 55.19 ± 9.40 | 8.65 ± 1.11 | 14.23 ± 2.36 | N/A | N/A | ||||||
| Xiang 2019 | China | HoLEP | 80 | 69.9 | N/A | N/A | 23.57 ± 8.32 | N/A | 1.56 ± 1.04 | ||||
| TURP | 80 | 72.1 | N/A | N/A | 24.66 ± 9.11 | N/A | 1.92 ± 1.55 | ||||||
| Zhou 2019 | China | ThuLEP | 60 | 62.24 ± 7.21 | 60.03 ± 13.40 | 7.90 ± 2.40 | 24.20 ± 3.80 | 120.20 ± 30.40 | N/A | ||||
| TURP | 60 | 63.41 ± 6.93 | 62.10 ± 14.20 | 8.20 ± 2.80 | 23.70 ± 3.20 | 113.10 ± 32.60 | N/A | ||||||
| Shoji 2020 | Japan | ThuLEP | 70 | 72 | 53 | 5.8 | 23 | 72 | 5 | ||||
| TURP | 70 | 73 | 53 | 5.8 | 23 | 79 | 5 | ||||||
| Zhang 2020 | China | HoLEP | 58 | 71.8 ± 3.9 | 93.0 ± 7.2 | 7.1 ± 2.8 | 24 | 172.9 | 5 | ||||
| ThuLEP | 58 | 72.7 ± 3.1 | 91.8 ± 6.9 | 6.6 ± 2.3 | 23 | 165.5 | 5 | ||||||
| Bozzini 2021 | Italy, France, Switzerland | HoLEP | 143 | 69.5 ± 15.54 | 86.3 ± 46.7 | 8.2 ± 6.71 | 17.9 ± 6.95 | 90.4 ± 120.44 | 5.6 ± 0.42 | ||||
| ThuLEP | 143 | 67.1 ± 17.83 | 90.2 ± 42.7 | 7.9 ± 8.05 | 18.2 ± 7.31 | 115.5 ± 130.54 | 5.8 ± 0.34 | ||||||
| El-Hawy 2021 | Egypt | HoLEP | 55 | 63.79 ± 5.6 | 74.5 ± 9.75 | 6.69 ± 2.4 | 24.02 ± 3.56 | 164.04 ± 31.2 | N/A | ||||
| TURP | 59 | 64.12 ± 6.9 | 75.02 ± 9.23 | 6.58 ± 2.1 | 25.05 ± 4.10 | 157.75 ± 32.4 | N/A | ||||||
| Habib 2021 | Egypt | HoLEP | 73 | 65.95 ± 6.76 | 105.8 ± 46.12 | 4.54 ± 3.65 | 26.53 ± 4.29 | 155.4 ± 120.3 | 5 | ||||
| TURP | 72 | 65.59 ± 6.72 | 102.95 ± 19.69 | 4.7 ± 3.43 | 25.4 ± 2.91 | 161.36 ± 107.68 | 4 | ||||||
| Higazy 2021 | Egypt | HoLEP | 54 | 66.17 ± 7.22 | 135.19 ± 34.84 | 3.3 ± 3.4 | 28.8 ± 2.1 | 160 ± 53 | 4.4 ± 0.5 | ||||
| TURP | 53 | 67.72 ± 6.48 | 125.00 ± 26.93 | 3.9 ± 3.3 | 28.9 ± 2.1 | 169 ± 56 | 4.4 ± 0.5 | ||||||
TURP: transurethral resection of the prostate; HoLEP: holmium laser enucleation of the prostate; ThuLEP: thulium laser enucleation of the prostate; Qmax: maximum flow rate; PVR: post-void residual; IPSS: international prostate symptom score; QoL: the quality of life.
Figure 2.
Risk of bias in included studies.
Figure 3.
Network diagram of short-term outcomes.
TURP: transurethral resection of the prostate; HoLEP: holmium laser enucleation of the prostate; ThuLEP: thulium laser enucleation of the prostate; (A) IPSS: international prostate symptom score; (B) PVR: post-void residual; (C) Qmax: maximum flow; (D) QoL: the quality of life.
Table 2.
Results of node-splitting models.
| A |
||||
|---|---|---|---|---|
| Name | Direct Effect | Indirect Effect | Overall | P-Value |
| IPSS | ||||
| HoLEP, TURP | 0.32 (−0.15, 0.81) | 1.58 (−0.40, 3.30) | 0.37 (−0.14, 0.93) | 0.17 |
| HoLEP, ThuLEP | −0.60 (−2.45, 0.92) | −2.00 (−2.82, −0.55) | −1.57 (−2.42, −0.33) | 0.21 |
| TURP, ThuLEP | −2.27 (−3.09, −1.00) | −0.96 (−2.72, 0.68) | −1.95 (−2.74, −0.82) | 0.22 |
| PVR | ||||
| HoLEP, TURP | 4.54 (−1.75, 10.23) | 7.03 (−8.59, 22.11) | 4.95 (−0.50, 9.62) | 0.73 |
| HoLEP, ThuLEP | 5.60 (−6.82, 18.13) | 3.42 (−7.76, 13.73) | 4.34 (−3.33, 11.48) | 0.74 |
| TURP, ThuLEP | −1.26 (−10.01, 7.11) | 1.07 (−12.30, 15.09) | −0.60 (−7.32, 6.36) | 0.76 |
| Qmax | ||||
| HoLEP, TURP | −1.70 (−3.77, 0.56) | 3.67 (−2.31, 10.15) | −1.08 (−3.25, 1.12) | 0.1 |
| HoLEP, ThuLEP | 2.59 (−1.76, 7.06) | −2.73 (−7.87, 2.13) | 0.29 (−3.31, 3.76) | 0.1 |
| TURP, ThuLEP | −1.00 (−5.56, 3.38) | 4.30 (−0.64, 9.25) | 1.38 (−2.26, 4.91) | 0.1 |
| QoL | ||||
| HoLEP, TURP | −0.01 (−0.17, 0.19) | −0.29 (−0.82, 0.20) | −0.03 (−0.18, 0.14) | 0.25 |
| HoLEP, ThuLEP | −0.10 (−0.34, 0.14) | 0.20 (−0.26, 0.68) | −0.06 (−0.24, 0.20) | 0.23 |
| TURP, ThuLEP | 0.20 (−0.26, 0.63) | −0.09 (−0.42, 0.19) | −0.03 (−0.25, 0.24) | 0.26 |
| B |
||||
|---|---|---|---|---|
| Name | Direct Effect | Indirect Effect | Overall | P-Value |
| IPSS | ||||
| HoLEP, TURP | 0.82 (−0.23, 1.86) | −0.01 (−3.41, 3.44) | 0.76 (−0.17, 1.66) | 0.6 |
| HoLEP, ThuLEP | −0.50 (−3.17, 2.15) | 0.37 (−1.97, 2.60) | −0.03 (−1.61, 1.66) | 0.59 |
| TURP, ThuLEP | −0.46 (−2.54, 1.57) | −1.32 (−4.26, 1.49) | −0.79 (−2.34, 0.82) | 0.6 |
| PVR | ||||
| HoLEP, TURP | 7.71 (1.07, 15.65) | 12.07 (−10.12, 35.23) | 8.04 (2.18, 15.08) | 0.68 |
| HoLEP, ThuLEP | 10.23 (−8.63, 29.40) | 5.92 (−9.21, 22.40) | 7.57 (−2.90, 19.20) | 0.67 |
| TURP, ThuLEP | −1.60 (−15.91, 11.84) | 2.63 (−18.89, 21.94) | −0.42 (−11.04, 9.82) | 0.68 |
| Qmax | ||||
| HoLEP, TURP | −1.28 (−2.54, 0.01) | 2.46 (−1.64, 6.90) | −0.98 (−2.29, 0.42) | 0.09 |
| HoLEP, ThuLEP | 2.33 (−0.49, 5.37) | −1.42 (−4.71, 1.92) | 0.75 (−1.52, 3.10) | 0.08 |
| TURP, ThuLEP | −0.08 (−3.09, 2.93) | 3.63 (0.58, 7.06) | 1.71 (−0.55, 4.07) | 0.08 |
| QoL | ||||
| HoLEP, TURP | −0.10 (−0.53, 0.32) | 0.33 (−0.80, 1.53) | −0.05 (−0.44, 0.31) | 0.41 |
| HoLEP, ThuLEP | −0.00 (−0.92, 0.91) | −0.42 (−1.28, 0.37) | −0.21 (−0.85, 0.32) | 0.42 |
| TURP, ThuLEP | −0.32 (−1.05, 0.36) | 0.10 (−0.92, 1.14) | −0.16 (−0.75, 0.35) | 0.41 |
| C |
||||
|---|---|---|---|---|
| Name | Direct Effect | Indirect Effect | Overall | P-Value |
| Operative time (mins) | ||||
| HoLEP, TURP | −11.96 (−21.10, −2.98) | −12.88 (−44.85, 19.40) | −12.00 (−20.32, −3.61) | 0.96 |
| HoLEP, ThuLEP | −1.33 (−21.69, 18.75) | −1.04 (−28.01, 25.62) | −1.24 (−16.87, 14.79) | 0.98 |
| TURP, ThuLEP | 11.16 (−14.10, 37.21) | 10.58 (−12.32, 33.15) | 10.87 (−5.35, 27.55) | 0.96 |
| Resected tissues(g) | ||||
| HoLEP, TURP | −5.25 (−11.38, 0.44) | 2.38 (−16.01, 20.89) | −4.62 (−10.12, 0.83) | 0.4 |
| HoLEP, ThuLEP | −1.15 (−12.43, 9.90) | −8.78 (−24.05, 6.40) | −3.99 (−13.02, 5.40) | 0.41 |
| TURP, ThuLEP | −3.38 (−17.97, 10.76) | 4.14 (−8.81, 16.79) | 0.72 (−8.49, 10.23) | 0.41 |
| Hospital stay (hours) | ||||
| HoLEP, TURP | 16.81 (4.95, 29.36) | 44.96 (6.94, 82.15) | 19.55 (6.81, 31.95) | 0.14 |
| HoLEP, ThuLEP | −1.05 (−21.76, 19.50) | −29.42 (−62.85, 5.50) | −8.46 (−27.99, 10.67) | 0.13 |
| TURP, ThuLEP | −45.81 (−77.57, −15.11) | −17.86 (−41.80, 5.44) | −28.01 (−48.79, −7.56) | 0.13 |
| Catheterization time (hours) | ||||
| HoLEP, TURP | 25.41 (16.11, 34.31) | 40.29 (5.85, 73.51) | 26.45 (17.80, 35.01) | 0.36 |
| HoLEP, ThuLEP | −1.05 (−19.07, 17.87) | −16.10 (−45.82, 13.43) | −5.08 (−20.36, 9.85) | 0.35 |
| TURP, ThuLEP | −41.50 (−70.25, −12.17) | −26.66 (−46.21, −5.85) | −31.54 (−47.72, −15.88) | 0.35 |
| Hemoglobin loss (gm/dl) | ||||
| HoLEP, TURP | −1.41 (−5.25, 2.42) | −0.43 (−10.66, 9.61) | −1.27 (−4.55, 1.93) | 0.83 |
| HoLEP, ThuLEP | −1.18 (−8.29, 6.05) | −2.13 (−10.25, 5.90) | −1.54 (−6.52, 3.28) | 0.84 |
| TURP, ThuLEP | −0.67 (−7.70, 6.55) | 0.31 (−7.45, 8.64) | −0.30 (−5.24, 4.57) | 0.84 |
| D |
||||
|---|---|---|---|---|
| Name | Direct Effect | Indirect Effect | Overall | P-Value |
| Recatheterization | ||||
| HoLEP, TURP | 0.62 (−0.42, 1.86) | −9.49 (−50.76, 1.19) | 0.55 (−0.52, 1.76) | 0.08 |
| HoLEP, ThuLEP | −18.61 (−43.45, −0.51) | −0.23 (−4.28, 3.12) | −1.14 (−4.76, 1.61) | 0.07 |
| TURP, ThuLEP | −0.95 (−4.92, 2.39) | −14.11 (−40.91, −0.13) | −1.69 (−5.31, 1.03) | 0.11 |
| Urethral stricture | ||||
| HoLEP, TURP | 0.82 (−0.14, 2.03) | −1.04 (−5.50, 2.32) | 0.71 (−0.16, 1.59) | 0.33 |
| HoLEP, ThuLEP | −0.84 (−4.75, 1.88) | 0.85 (−0.96, 3.05) | 0.33 (−1.20, 1.85) | 0.26 |
| TURP, ThuLEP | −0.06 (−1.63, 1.74) | −1.93 (−5.82, 1.42) | −0.36 (−1.77, 0.98) | 0.29 |
| Bladder neck contracture | ||||
| HoLEP, TURP | −0.39 (−1.79, 0.82) | 3.48 (−5.08, 34.26) | −0.39 (−1.71, 0.89) | 0.61 |
| HoLEP, ThuLEP | −4.58 (−17.70, 6.21) | −1.43 (−3.70, 0.91) | −1.32 (−3.79, 0.78) | 0.6 |
| TURP, ThuLEP | −0.80 (−3.18, 1.12) | −3.72 (−27.56, 11.84) | −0.93 (−3.30, 0.85) | 0.74 |
| Urinary incontinence | ||||
| HoLEP, TURP | −0.42 (−1.06, 0.17) | −0.12 (−1.73, 1.52) | −0.39 (−0.88, 0.13) | 0.72 |
| HoLEP, ThuLEP | −0.78 (−1.83, 0.14) | −1.05 (−2.48, 0.31) | −0.88 (−1.62, −0.16) | 0.75 |
| TURP, ThuLEP | −0.63 (−1.82, 0.66) | −0.43 (−1.55, 0.70) | −0.47 (−1.28, 0.23) | 0.83 |
TURP: transurethral resection of the prostate; HoLEP: holmium laser enucleation of the prostate; ThuLEP: thulium laser enucleation of the prostate. Qmax: maximum flow rate; PVR: post-void residual; IPSS: international prostate symptom score; QoL: the quality of life. (A): short-term outcomes; (B): long-term outcomes; (C): perioperation-related outcomes; (D): complications.
3.2. Results of the network meta-analysis
3.2.1. Treatment effects
3.2.1.1. Comparison of short-term (3 months) postoperative treatment outcomes
A total of 9 studies reported IPSS at 3 months postoperatively, with lower scores for ThuLEP and HoLEP compared to TURP [ThuLEP: MD = -1.95, 95% CI (−2.74, -0.82); HoLEP: MD = -0.37, 95% CI (−0.93,0.14)]. The probability of ThuLEP as sort 3 was 99% and that of HoLEP as sort 2 was 94%, the same as for TURP as sort 1. Therefore, the rank order of IPSS at 3 months postoperatively for the three surgical procedures from smallest to largest was ThuLEP, HoLEP, and TURP. Besides, 7 studies showed a reduction in PVR at 3 months postoperatively compared to TURP for both HoLEP and ThuLEP [ThuLEP: MD = -0.60, 95% CI (−7.32, 6.36); HoLEP: MD = -4.95, 95% CI (−9.62, 0.50)]. In addition, there was 87% probability of HoLEP as sort 3, 48% probability of ThuLEP as sort 2 and 56% probability of TURP as sort 1. Thus, the rank order of PVR at 3 months postoperatively for the three surgical procedures was HoLEP, ThuLEP, and TURP from least to greatest. Beyond that, 12 studies presented Qmax at 3 months postoperatively, which was better as a benign indicator with greater values, with ThuLEP and HoLEP being better than TURP [ThuLEP: MD = 1.38, 95% CI (−2.26, 4.91); HoLEP: MD = 1.08, 95% CI (−1.12, 3.25)]. The probability of ThuLEP as sort 1 was 55%, while that of HoLEP as sort 2 was 50% and TURP as sort 3 was 70%. Hence, the rank order of Qmax at 3 months postoperatively for the three surgical procedures from largest to smallest was ThuLEP, HoLEP, and TURP. In terms of QoL, a total of 5 studies reported that ThuLEP and TURP were lower than HoLEP [ThuLEP: MD = -0.06, 95% CI (−0.24, 0.20); TURP: MD = -0.03,95% CI (−0.18, 0.14)]. The ranking order of QoL at 3 months postoperatively for the three surgical procedures from smallest to largest was ThuLEP, TURP, and HoLEP. Then, overall ThuLEP had a better short-term treatment outcome.
3.2.1.2. Comparison of long-term (12 months) postoperative treatment outcomes
A total of 9 papers reported IPSS, and meta-analysis revealed that ThuLEP and HoLEP were superior to TURP [ThuLEP: MD = -0.79, 95% CI (−2.34, 0.82); HoLEP: MD = -0.76, 95% CI (−1.66, 0.17)]. The rank order of IPSS scores at 12 months after surgery for the three surgical procedures from smallest to largest was ThuLEP, HoLEP, and TURP. Besides, 10 papers reported PVR, and the meta-analysis showed that HoLEP and ThuLEP were superior to TURP [ThuLEP: MD = -0.42, 95% CI (−11.04, 9.82); HoLEP: MD = -8.04, 95% CI (−15.08, −2.18)]. The rank order of PVR at 12 months after surgery for the three surgical procedures from least to most was HoLEP, ThuLEP, and TURP. 14 papers showed Qmax, and meta-analysis revealed that HoLEP and ThuLEP were superior to TURP [ThuLEP: MD = 1.71, 95% CI (−0.55, 4.07); HoLEP: MD = 0.98, 95% CI (−0.42, 2.29)]. The rank order of Qmax at 12 months after surgery for the three surgical procedures from largest to smallest was ThuLEP, HoLEP, and TURP. Moreover, a total of 8 papers reported QoL, and ThuLEP and TURP were superior to HoLEP [ThuLEP: MD = -0.16, 95% CI (−0.75, 0.35); TURP: MD = -0.05, 95% CI (−0.44, 0.31)]. The order of superiority of their ranking probabilities was ThuLEP, TURP, and HoLEP. Therefore, the long-term treatment outcome of ThuLEP was also better. Combining the short-term and long-term postoperative results of the three surgical procedures, ThuLEP had the best results, followed by HoLEP and TURP.
3.2.2. Surgical situation
The surgery of each procedure was judged based on the weight of the prostate tissue removed and the combination of the operation time and intraoperative blood loss. In terms of the weight of prostate tissue removed, which was taken as a benign indicator, meta-analysis showed that ThuLEP and HoLEP were superior to TURP [ThuLEP: MD = 0.72, 95% CI (−8.49, 10.23); HoLEP: MD = 4.62, 95% CI (−0.83, 10.12)]. As for operative time, the meta-analysis manifested that TURP was significantly shorter than ThuLEP and HoLEP [ThuLEP: MD = 10.87, 95% CI (−5.35, 27.55); HoLEP: MD = 12.00, 95% CI (3.61, 20.32)], and the rank order of the three surgical procedures from shortest to longest operative time was TURP, ThuLEP, HoLEP. When it comes to blood loss, the results of meta-analysis showed that TURP and ThuLEP were superior to HoLEP [ThuLEP: MD = -1.54, 95% CI (−6.52, 3.28); TURP: MD = -1.27, 95% CI (−4.55, 1.93)]. The order of superiority of the ranked probabilities was ThuLEP, TURP, and HoLEP. Therefore, combined with the weight of prostate tissue removed, the operative time and blood loss, ThuLEP was superior to other surgical procedures with the least amount of blood loss, moderate operative time, and prostate tissue removed.
3.2.3. Post-operative recovery
The duration of the postoperative indwelling urinary catheter was obviously shorter for ThuLEP and HoLEP [ThuLEP: MD = -31.54, 95% CI (−47.72, -15.88); HoLEP: MD = -26.45, 95% CI (−35.01, -17.80)]. The order of ranking probabilities was ThuLEP, HoLEP, and TURP, where the former two had noticeable advantages in terms of length of stay [ThuLEP: MD = -28.01, 95% CI (−48.79, -7.56); HoLEP: MD = -19.55, 95% CI (−31.95, -6.81)]. Whereas, the order of superiority of the ranked probabilities was ThuLEP, HoLEP, and TURP. Therefore, the combined analysis on the duration of the postoperative indwelling urinary catheter and length of hospital stay revealed that ThuLEP had better postoperative recovery, followed by HoLEP and TURP.
3.2.4. Postoperative complications
Some patients required reintroduction of the urinary catheter after surgery, and the incidence of ThuLEP [RR = 0.18, 95% CI (0.00, 2.80)] and HoLEP [RR = 0.58, 95% CI (0.17, 1.67)] were lower than that of TURP. The order of merit of their ranking probabilities was ThuLEP, HoLEP, and TURP. Concerning bladder neck contracture, the incidence of ThuLEP [RR = 0.27, 95% CI (0.02, 2.18)] and TURP [RR = 0.68, 95% CI (0.18,2.42)] were lower than that of HoLEP, and the order of merit of their ranking probabilities was ThuLEP, TURP, HoLEP. In complications of urethral strictures, HoLEP [RR = 0.49, 95% CI (0.20, 1.17)] and ThuLEP [RR = 0.70, 95% CI (0.17, 2.67)] were lower than TURP, and the ranked probability order of superiority was HoLEP, ThuLEP and TURP. In urinary incontinence ThuLEP [RR = 0.41, 95% CI (0.20, 0.86)] and TURP [RR = 0.68, 95% CI (0.41, 1.14)] were lower than HoLEP, and the ranked probability order of superiority and inferiority was ThuLEP, TURP, and HoLEP. Moreover, in terms of postoperative complications, the overall order of superiority and inferiority, when analyzing the above indicators, was ThuLEP, HoLEP, and TURP.
4. Discussion
TURP has been considered the gold standard for the surgical treatment of BPH patients, and is performed when the prostate is <80 ml in volume, whereas open surgery is conducted for large prostate volumes of 80–100 ml [38]. However, the significant adverse event rate of TURP and the bleeding and trauma associated with open surgery have led researchers and surgeons to develop new surgical treatments in pursuit of better efficacy and greater safety.
Since the first use of Nd:YAG laser for BPH by Costello et al. in 1992 [39], various lasers have been used in the surgical treatment of prostate enlargement with good results in recent years [19, 22]. Different types of lasers have different characteristics, and with the change in surgical approaches, the combination of the two has become diverse. The diversity of laser procedures provides a variety of options for clinical surgical treatment, but it is not easy to choose the best one. Besides, the commonly used lasers include holmium laser, thulium laser, and green laser, etc. Rieken et al. summarized the physical properties of different lasers and the current therapeutic effects of clinical laser surgery [40], and found that the penetration depth of thulium laser is around 0.2 mm, while that of the holmium laser is about 0.4 mm, and that of the green laser is as deep as 0.8 mm. Laser enucleation with holmium and green lasers can improve urinary symptoms and scores to a great extent, and is comparable to TURP.
In this study, 27 randomized controlled trials with totally 3335 patients were included. The efficacy and safety of ThuLEP, HoLEP and TURP for prostate enlargement were indirectly compared and ranked by means of a reticulated meta-analysis. In addition, the efficacy of the three surgical modalities was evaluated by short-term (3 months after surgery) and long-term (12 months after surgery) follow-up, and the occurrence of postoperative complications was judged by the presence of urethral stricture, urinary incontinence, bladder neck contracture and reintroduction of catheterization, mainly based on four indicators, namely Qmax, PVR, IPSS and QoL. The results showed that ThuLEP had better short-term and long-term outcomes than the remaining two, with almost significant advantages in terms of objective indicators (Qmax and PVR) and subjective perceptions (IPSS and QoL). Apart from that, ThuLEP is less likely to have complications such as postoperative urethral strictures and reintroduction of urinary catheters. Despite the longer operative time of ThuLEP [MD = 10.87, 95% CI (−5.35, 27.55)], there were advantages regarding resection of prostate tissue [MD = 0.72, 95% CI (−8.49,10.23)] and reduction of intraoperative blood loss [MD = -1.54, 95% CI (−6.52, 3.28)], which may be related to the physical properties of the thulium laser that has a wavelength of approximately 2.0 μm and can operate in both continuous and pulsed wave modes to cut tissue more precisely through higher energy utilization and shallower depth of tissue penetration [41]. Holmium laser, a commonly used energy modality for prostate enucleation, also offers many advantages over TURP, in spite of the longer operative time [MD = 10.87, 95% CI (−5.35, 27.55)]. For example, the postoperative indwelling urinary catheter time [MD = -26.45, 95% CI (−35.01,-17.80)] and hospital stay [MD = -19.55, 95% CI (−31.95, -6.81)] were extremely shorter, and the postoperative outcome was also better and with fewer complications, similar to the findings of zhong et al. [41].
There are some limitations in this systematic evaluation: ① there are few RCTs on holmium and thulium laser surgical modalities with small sample sizes, because these two surgical modalities have only been performed in recent years; ② more literature does not elaborate on randomized control methods and blinding; ③ a little literature uses WebPlotDigitizer 4.5 for data extraction because the original data are not available, which may introduce bias. Therefore, more high-quality, large-sample RCTs should be performed in the future to offer more definitive evidence for the selection of the best surgical approach.
In conclusion, based on the results of the network Meta-analysis and ranking, ThuLEP is a superior surgical procedure for the treatment of prostate enlargement, and it has the advantages of good efficacy, high safety and rapid postoperative recovery.
Declarations
Author contribution statement
Jiusong Yan: Conceived and designed the experiments; Analyzed and interpreted the data; Wrote the paper.
Liang Gao: Conceived and designed the experiments.
Junyong Zhang: Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data.
Guangyong Xu: Performed the experiments.
Funding statement
Junyong Zhang was supported by the National Natural Science Youth Fund, China [81803057].
Data availability statement
Data included in article/supp. material/referenced in article.
Declaration of interest’s statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
References
- 1.Griebling T.L. Worldwide prevalence estimates of lower urinary tract symptoms, overactive bladder, urinary incontinence, and bladder outlet obstruction. BJU Int. 2011;108(7):1138–1139. doi: 10.1111/j.1464-410X.2011.10498.x. [DOI] [PubMed] [Google Scholar]
- 2.Gratzke C., Bachmann A., Descazeaud A., Drake M.J., Madersbacher S., Mamoulakis C., Oelke M., Tikkinen K.A.O., Gravas S. EAU guidelines on the assessment of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. Eur. Urol. 2015;67(6):1099–1109. doi: 10.1016/j.eururo.2014.12.038. [DOI] [PubMed] [Google Scholar]
- 3.Reich O., Gratzke C., Bachmann A., Seitz M., Schlenker B., Hermanek P., Lack N., Stief C.G. Morbidity, mortality and early outcome of transurethral resection of the prostate: a prospective multicenter evaluation of 10,654 patients. J. Urol. 2008;180(1):246–249. doi: 10.1016/j.juro.2008.03.058. [DOI] [PubMed] [Google Scholar]
- 4.Fraundorfer M.R., Gilling P.J. Holmium:YAG laser enucleation of the prostate combined with mechanical morcellation: preliminary results. Eur. Urol. 1998;33(1):69–72. doi: 10.1159/000019535. [DOI] [PubMed] [Google Scholar]
- 5.Michalak J., Tzou D., Funk J. HoLEP: the gold standard for the surgical management of BPH in the 21(st) Century. Am. J. Clin. Exp. Urol. 2015;3(1):36–42. [PMC free article] [PubMed] [Google Scholar]
- 6.Fried N.M., Murray K.E. High-power thulium fiber laser ablation of urinary tissues at 1.94 microm. J. Endourol. 2005;19(1):25–31. doi: 10.1089/end.2005.19.25. [DOI] [PubMed] [Google Scholar]
- 7.Herrmann T.R., Bach T., Imkamp F., Georgiou A., Burchardt M., Oelke M., Gross A.J. Thulium laser enucleation of the prostate (ThuLEP): transurethral anatomical prostatectomy with laser support. Introduction of a novel technique for the treatment of benign prostatic obstruction. World J. Urol. 2010;28(1):45–51. doi: 10.1007/s00345-009-0503-0. [DOI] [PubMed] [Google Scholar]
- 8.Bozzini G., Berti L., Aydoğan T.B., Maltagliati M., Roche J.B., Bove P., Besana U., Calori A., Pastore A.L., Müller A., et al. A prospective multicenter randomized comparison between holmium laser enucleation of the prostate (HoLEP) and thulium laser enucleation of the prostate (ThuLEP) World J. Urol. 2021;39(7):2375–2382. doi: 10.1007/s00345-020-03468-6. [DOI] [PubMed] [Google Scholar]
- 9.Zhang X., Shen P., He Q., Yin X., Chen Z., Gui H., Shu K., Tang Q., Yang Y., Pan X., et al. Different lasers in the treatment of benign prostatic hyperplasia: a network meta-analysis. Sci. Rep. 2016;6 doi: 10.1038/srep23503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cumpston M., Li T., Page M.J., Chandler J., Welch V.A., Higgins J.P., Thomas J. Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst. Rev. 2019;10 doi: 10.1002/14651858.ED000142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kuntz R.M., Ahyai S., Lehrich K., Fayad A. Transurethral holmium laser enucleation of the prostate versus transurethral electrocautery resection of the prostate: a randomized prospective trial in 200 patients. J. Urol. 2004;172(3):1012–1016. doi: 10.1097/01.ju.0000136218.11998.9e. [DOI] [PubMed] [Google Scholar]
- 12.Montorsi F., Naspro R., Salonia A., Suardi N., Briganti A., Zanoni M., Valenti S., Vavassori I., Rigatti P. Holmium laser enucleation versus transurethral resection of the prostate: results from a 2-center, prospective, randomized trial in patients with obstructive benign prostatic hyperplasia. J. Urol. 2004;172(5 Pt 1):1926–1929. doi: 10.1097/01.ju.0000140501.68841.a1. [DOI] [PubMed] [Google Scholar]
- 13.Wilson L.C., Gilling P.J., Williams A., Kennett K.M., Frampton C.M., Westenberg A.M., Fraundorfer M.R. A randomised trial comparing holmium laser enucleation versus transurethral resection in the treatment of prostates larger than 40 grams: results at 2 years. Eur. Urol. 2006;50(3):569–573. doi: 10.1016/j.eururo.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 14.Ahyai S.A., Lehrich K., Kuntz R.M. Holmium laser enucleation versus transurethral resection of the prostate: 3-year follow-up results of a randomized clinical trial. Eur. Urol. 2007;52(5):1456–1463. doi: 10.1016/j.eururo.2007.04.053. [DOI] [PubMed] [Google Scholar]
- 15.Xia S.J., Zhuo J., Sun X.W., Han B.M., Shao Y., Zhang Y.N. Thulium laser versus standard transurethral resection of the prostate: a randomized prospective trial. Eur. Urol. 2008;53(2):382–389. doi: 10.1016/j.eururo.2007.05.019. [DOI] [PubMed] [Google Scholar]
- 16.Mavuduru R.M., Mandal A.K., Singh S.K., Acharya N., Agarwal M., Garg S., Kumar S. Comparison of HoLEP and TURP in terms of efficacy in the early postoperative period and perioperative morbidity. Urol. Int. 2009;82(2):130–135. doi: 10.1159/000200786. [DOI] [PubMed] [Google Scholar]
- 17.Fayad A.S., Sheikh M.G., Zakaria T., Elfottoh H.A., Alsergany R. Holmium laser enucleation versus bipolar resection of the prostate: a prospective randomized study. Which to choose? J. Endourol. 2011;25(8):1347–1352. doi: 10.1089/end.2011.0059. [DOI] [PubMed] [Google Scholar]
- 18.Gilling P.J., Wilson L.C., King C.J., Westenberg A.M., Frampton C.M., Fraundorfer M.R. Long-term results of a randomized trial comparing holmium laser enucleation of the prostate and transurethral resection of the prostate: results at 7 years. BJU Int. 2012;109(3):408–411. doi: 10.1111/j.1464-410X.2011.10359.x. [DOI] [PubMed] [Google Scholar]
- 19.Świniarski P.P., Stępień S., Dudzic W., Kęsy S., Blewniewski M., Różański W. Thulium laser enucleation of the prostate (TmLEP) vs. transurethral resection of the prostate (TURP): evaluation of early results. Cent. Eur. J. Urol. 2012;65(3):130–134. doi: 10.5173/ceju.2012.03.art6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhang F., Shao Q., Herrmann T.R., Tian Y., Zhang Y. Thulium laser versus holmium laser transurethral enucleation of the prostate: 18-month follow-up data of a single center. Urology. 2012;79(4):869–874. doi: 10.1016/j.urology.2011.12.018. [DOI] [PubMed] [Google Scholar]
- 21.Cui D., Sun F., Zhuo J., Sun X., Han B., Zhao F., Jing Y., Lu J., Xia S. A randomized trial comparing thulium laser resection to standard transurethral resection of the prostate for symptomatic benign prostatic hyperplasia: four-year follow-up results. World J. Urol. 2014;32(3):683–689. doi: 10.1007/s00345-013-1103-6. [DOI] [PubMed] [Google Scholar]
- 22.Sun N., Fu Y., Tian T., Gao J., Wang Y., Wang S. An W: holmium laser enucleation of the prostate versus transurethral resection of the prostate: a randomized clinical trial. Int. Urol. Nephrol. 2014;46(7):1277–1282. doi: 10.1007/s11255-014-0646-9. [DOI] [PubMed] [Google Scholar]
- 23.Fayad A.S., Elsheikh M.G., Zakaria T., Elfottoh H.A., Alsergany R., Elshenoufy A., Elghamarawy H. Holmium laser enucleation of the prostate versus bipolar resection of the prostate: a prospective randomized study. “Pros and cons”. Urology. 2015;86(5):1037–1041. doi: 10.1016/j.urology.2015.08.004. [DOI] [PubMed] [Google Scholar]
- 24.Gao X. Comparison of clinical effect of electro-prostatectomy and transurethral holium laser enucleation of prostate on benign prostatic hyperplasia. J Chin. Foreign Med. J. 2016;35(26):10–12. [Google Scholar]
- 25.Jhanwar A., Sinha R.J., Bansal A., Prakash G., Singh K., Singh V. Outcomes of transurethral resection and holmium laser enucleation in more than 60 g of prostate: a prospective randomized study. Urol. Ann. 2017;9(1):45–50. doi: 10.4103/0974-7796.198904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang Y.C., Li C., Wang J.Q. Comparison of long-term clinical efficacy between transurethral holium laser enucleation of prostate and electro-prostatectomy. J. China Health Stand. Manage. 2017;8(26):57–59. [Google Scholar]
- 27.Wei N. Comparison of short-term efficacy between transurethral holium laser enucleation of prostate and electro-prostatectomy. J Chin. Commun. Doctors. 2017;33(33) 27–28,30. [Google Scholar]
- 28.Zheng D.B., Wang J.F., Jing Z.T., Hu B., Zhang J.X. Comparison of efficacy between transurethral holium laser enucleation of prostate and electro-prostatectomy on benign prostatic hyperplasia. J Acta Acad. Med. Xuzhou. 2017;37(12):829–831. [Google Scholar]
- 29.Jiu Q.S., Niu Z.H., Huang T.T., Du W.J., Chen F. Clinical effect of transurethral holium laser enucleation of prostate on benign prostatic hyperplasia. J. Qingdao Med. J.. 2018;50(6):404–406. [Google Scholar]
- 30.Xiang H., Su K.D., Zhou J.H. Effect of transurethral holium laser enucleation of prostate and transurethral electro-prostatectomy on benign prostatic hyperplasia. J. World Clin. Med. 2019;13(4):44. [Google Scholar]
- 31.El-Hawy M.M., Eldakhakhny A., AbdEllatif A., Salem E.A., Ragab A., Elsharkawy M.S., Abdelghani M.M., Alshara L., Hasanein M.G., Ismail A.H., et al. Two-year follow-up after holmium laser enucleation of the prostate and bipolar transurethral resection of the prostate: a prospective randomized study. Afr. J. Urol. 2021;27(1) [Google Scholar]
- 32.Habib E.I., ElSheemy M.S., Hossam A., Morsy S., Hussein H.A., Abdelaziz A.Y., Abdelazim M.S., Fathy H. Holmium laser enucleation versus bipolar plasmakinetic resection for management of lower urinary tract symptoms in patients with large-volume benign prostatic hyperplasia: randomized-controlled trial. J. Endourol. 2021;35(2):171–179. doi: 10.1089/end.2020.0636. [DOI] [PubMed] [Google Scholar]
- 33.Higazy A., Tawfeek A.M., Abdalla H.M., Shorbagy A.A., Mousa W., Radwan A.I. Holmium laser enucleation of the prostate versus bipolar transurethral enucleation of the prostate in management of benign prostatic hyperplasia: a randomized controlled trial. Int. J. Urol. 2021;28(3):333–338. doi: 10.1111/iju.14462. [DOI] [PubMed] [Google Scholar]
- 34.Zhou W.H., Zhu X.S., MKMJ·WBLHR. Zhao W., Liu H.T. Effect of transurethral Thulium laser Enucleation of prostate on sexual function of patients with benign prostatic hyperplasia in Kashgar region of Xinjiang. J Mod. Urol. 2019;24(4):296–299. [Google Scholar]
- 35.Shoji S., Hanada I., Otaki T., Ogawa T., Yamada K., Uchida T., Higure T., Kawakami M., Kim H., Nitta M., et al. Functional outcomes of transurethral thulium laser enucleation versus bipolar transurethral resection for benign prostatic hyperplasia over a period of 12 months: a prospective randomized study. Int. J. Urol. 2020;27(11):974–980. doi: 10.1111/iju.14341. [DOI] [PubMed] [Google Scholar]
- 36.Zhang J., Ou Z., Zhang X., He W., Wang R., Mo M., Chen L., Xu R., Jiang S., Peng X., et al. Holmium laser enucleation of the prostate versus thulium laser enucleation of the prostate for the treatment of large-volume prostates > 80 ml: 18-month follow-up results. World J. Urol. 2020;38(6):1555–1562. doi: 10.1007/s00345-019-02945-x. [DOI] [PubMed] [Google Scholar]
- 37.Oelke M., Bachmann A., Descazeaud A., Emberton M., Gravas S., Michel M.C., N'Dow J., Nordling J., de la Rosette J.J. EAU guidelines on the treatment and follow-up of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. Eur. Urol. 2013;64(1):118–140. doi: 10.1016/j.eururo.2013.03.004. [DOI] [PubMed] [Google Scholar]
- 38.Costello A.J., Johnson D.E., Bolton D.M. Nd:YAG laser ablation of the prostate as a treatment for benign prostatic hypertrophy. Laser Surg. Med. 1992;12(2):121–124. doi: 10.1002/lsm.1900120202. [DOI] [PubMed] [Google Scholar]
- 39.Rieken M., Bachmann A. Laser treatment of benign prostate enlargement–which laser for which prostate? Nat. Rev. Urol. 2014;11(3):142–152. doi: 10.1038/nrurol.2014.23. [DOI] [PubMed] [Google Scholar]
- 40.Bach T., Muschter R., Sroka R., Gravas S., Skolarikos A., Herrmann T.R., Bayer T., Knoll T., Abbou C.C., Janetschek G., et al. Laser treatment of benign prostatic obstruction: basics and physical differences. Eur. Urol. 2012;61(2):317–325. doi: 10.1016/j.eururo.2011.10.009. [DOI] [PubMed] [Google Scholar]
- 41.Zhong J., Feng Z., Peng Y., Liang H. A systematic review and meta-analysis of efficacy and safety following holmium laser enucleation of prostate and transurethral resection of prostate for benign prostatic hyperplasia. Urology. 2019;131:14–20. doi: 10.1016/j.urology.2019.03.034. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data included in article/supp. material/referenced in article.