To the Editor:
People with kidney disease receiving dialysis continue to have high rates of morbidity, anxiety, and depression, all leading to poor quality of life.1 Capacity to understand the best treatment choices can be limited, resulting in poor decision-making and poor health outcomes.2,3 Peer mentoring has been used to inform people receiving dialysis based on the premise that people who have gone through the dialysis experience are best suited to assist others.4,5 These relationships can influence decisions by increasing knowledge, skills, and social support, resulting in improved quality of life.6
Since 2011, The National Kidney Foundation (NKF) has provided the NKF PEERS program, a national, telephone-based peer support program that aims to help people adjust to living with chronic kidney disease, dialysis, or a kidney transplant (https://www.kidney.org/peers).7 The program provides a mentor training program, assessment and matching of mentors with mentees, and complete confidentiality of mentor-mentee telephone conversation content. By 2015, the program trained 80 patient peer mentors and connected over 423 people seeking support. The program reported favorable experience by mentees.8
Despite the success of the NKF PEERS program with the people who used it, it is not clear what level of engagement an unselected dialysis population would have with it. Thus, we aimed to evaluate the feasibility of NKF PEERS when offered to incident in-center hemodialysis (HD) patients, including an assessment of the interest in the program (proportion who would engage with the program), and the logistics and required resources for running the program. Ethical approval with waiver of consent was obtained from an independent review board (ASPIRE-IRB #SP122PEERNKF).
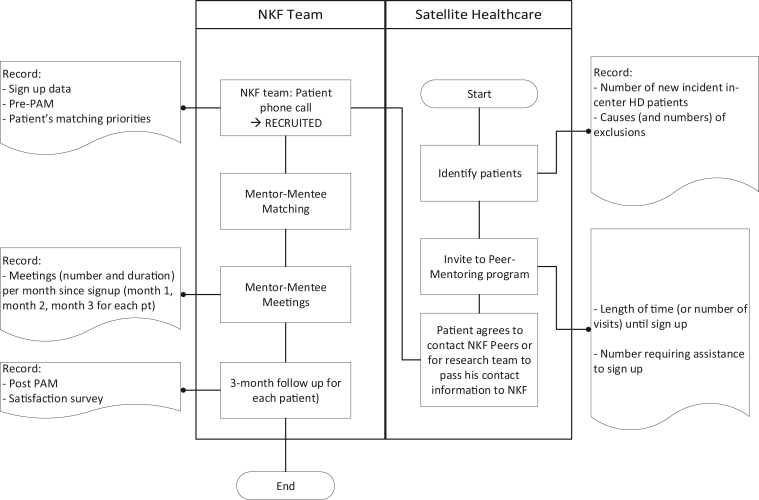
HD centers were chosen to be involved following discussion with each center’s clinical team. Adult incident HD patients, able to communicate in English, were introduced to the NKF PEERS program in their first week of dialysis by social workers trained on the study. Patients agreeing to participate would then have to call the program or provide their information through a web form to receive a call from the NKF team. During this initial interview, matching criteria were identified. The NKF oversight clinician would match the patient to an appropriate mentor. Mentors called mentees through an app called PeerStrong (InquisitHealth Inc) which allowed mentors and mentees to connect without disclosing personal contact information. Mentees are not required to use the app to connect with a mentor and can simply receive a toll-free call. We anticipated that over a 12-month period, 100 patients would complete the matching process and carry out mentor-mentee meetings (Fig 1). This number of participants was based on internal information as we anticipated having more than 130 eligible patients from 11 centers over 12 months and that about 100 patients would go through the program.
Figure 1.
Study design. Abbreviations: HD, hemodialysis; NKF, National Kidney Foundation; PAM, Patient Activation Measures Survey.
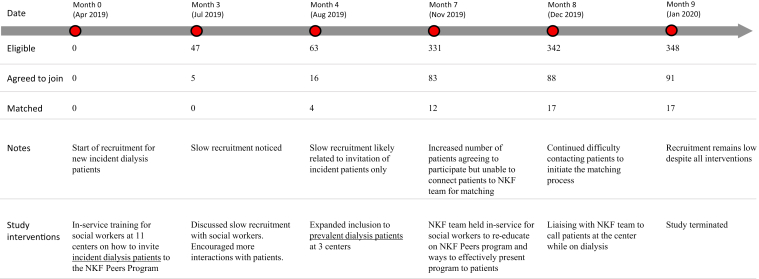
Following a review of the recruitment progress at the 4-month time point, only 4 (6%) of the eligible patients completed the matching step. Social workers highlighted that most incident patients indicated “having enough information” from their healthcare team, resulting in low interest in joining the PEERS program. Furthermore, people starting dialysis may have been overwhelmed at the start of their dialysis journey. On the advice of the study social workers, we expanded the eligibility criteria to prevalent dialysis patients at 3 of the 11 initial centers. Subsequently, we observed that patients who indicated interest did not call the NKF PEERS team and did not respond to calls by the team. The challenge remained despite several attempts to resolve the issue by trying to establish the calls while on dialysis. At 9 months, despite multiple interventions, only 17 patients were matched (5% of invited eligible patients). At this stage, the study was terminated. Figure 2 summarizes the progress of the study with challenges and attempted interventions.
Figure 2.
Study flow diagram demonstrating uptake of peer mentor program. Abbreviation: NKF, National Kidney Foundation.
We observed that only about a fourth of eligible incident patients indicated interest. The reasons for this are unclear and may be related to the patient being overwhelmed by commencing dialysis or the perception that they received sufficient support from the center staff with no need to contact outside support. The proportion of patients indicating interest remained the same when we opened recruitment to prevalent patients. Furthermore, among those who indicated interest, only about 1 in 5 followed through and matched. As a result, only 5% (17/348) of invited eligible patients joined the program. Reasons for not embracing telephone mentoring has been previously reported in education mentoring.9 In our study the reasons may include fear of the unknown or a lack of interest in telephone-based interactions. Logistic difficulties in connecting patients with the NKF PEERS team may have played a role in the low number of patients reaching the matching step (patient not answering calls from unknown numbers, not able to call within working hours), but these did not improve following multiple interventions we put in place (Fig 2).
Strategies to improve success may rely on offering both face-to-face and remote interactions and increasing modes of contact using improved video technology. It is clear that telephone support has its place; however, only a small proportion of US dialysis patients (approximately 1%) use this service.8 Therefore, although remote peer support may be a strategy to enhance participation, this is not always the case. An alternative model using face-to-face peer mentoring has been described in US HD centers with exemplars from NKF Michigan, Virginia, and California.10,4,6 Although these programs have reported relative success, face-to-face mentoring can be resource-intensive, requiring organizational support and committed local champions.4
In conclusion, we observed low interest among in-center HD patients to join a telephonic peer mentoring program. Given that we still believe peer mentoring can be a positive strategy for people starting HD, we recommend future studies include a formal needs assessment. We encourage HD centers to pursue peer mentor models that fit their own context in order to promote patient experts supporting others. This may be face-to-face or potentially a hybrid model utilizing technologies that are being advanced through programs led by NKF PEERS.
Article Information
Authors’ Contributions
Research idea and study design: BS, WFH, PNB, KCD, JA; data acquisition: MA, JA; data analysis/interpretation: WFH, KCD, PNB, BS; statistical analysis: WFH, PNB; supervision or mentorship: BS. Each author contributed important intellectual content during manuscript drafting or revision and agrees to be personally accountable for the individual’s own contributions and to ensure that questions pertaining to the accuracy or integrity of any portion of the work, even one in which the author was not directly involved, are appropriately investigated and resolved, including with documentation in the literature if appropriate.
Support
This study was supported by a grant from Satellite Healthcare (#SP122_PeerNKF).
Financial Disclosure
Author Bennett is a past employee of Satellite Healthcare. Authors Hussein, Atwal, and Schiller are current employees of Satellite Healthcare. Authors Argentina and Collins are current employees of the National Kidney Foundation.
Peer Review
Received May 25, 2022 as a submission to the expedited consideration track with 3 external peer reviews. Direct editorial input from the Editor-in-Chief. Accepted in revised form July 07, 2022.
References
- 1.Daniel S.C., Azuero A., Gutierrez O.M., Heaton K. Examining the relationship between nutrition, quality of life, and depression in hemodialysis patients. Qual Life Res. 2021;30(3):759–768. doi: 10.1007/s11136-020-02684-2. [DOI] [PubMed] [Google Scholar]
- 2.Ghodsian S., Ghafourifard M., Ghahramanian A. Comparison of shared decision making in patients undergoing hemodialysis and peritoneal dialysis for choosing a dialysis modality. BMC Nephrol. 2021;22(1):67. doi: 10.1186/s12882-021-02269-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Subramanian L., Zhao J., Zee J., et al. Use of a decision aid for patients considering peritoneal dialysis and in-center hemodialysis: a randomized controlled trial. Am J Kidney Dis. 2019;74(3):351–360. doi: 10.1053/j.ajkd.2019.01.030. [DOI] [PubMed] [Google Scholar]
- 4.Bennett P.N., St Clair Russell J., Atwal J., Brown L., Schiller B. Patient-to-patient peer mentor support in dialysis: improving the patient experience. Semin Dial. 2018;31(5):455–461. doi: 10.1111/sdi.12703. [DOI] [PubMed] [Google Scholar]
- 5.Haugen C. Lessons learned: implementation of peer-to-peer mentor program in individuals requiring hemodialysis. Nephrol Nurs J. 2021;48(4):399–412. [Google Scholar]
- 6.St Clair Russell J.S.C., Southerland S., Huff E.D., Thomson M., Meyer K.B., Lynch J.R. A peer-to-peer mentoring program for in-center hemodialysis: a patient-centered quality improvement program. Nephrol Nurs J. 2017;44(6):481–496. [PubMed] [Google Scholar]
- 7.What is NKF PEERS? National Kidney Foundation. https://www.kidney.org/patients/peers Published 2021.
- 8.Collins K. NKF Peers mentoring program: an overview and lessons learned. J Nephrol Soc Work. 2016;40:25–33. [Google Scholar]
- 9.Murphy W.M. From E-mentoring to blended mentoring: increasing students’ developmental initiation and mentors’ satisfaction. Acad Manag Learn Educ. 2011;10(4):606–622. [Google Scholar]
- 10.Peer mentoring. National Kidney Foundation of Michigan. https://www.nkfm.org/help-information/patient-services/peer-mentoring Published 2020.