Abstract
Introduction
Young women in sub‐Saharan Africa account for two‐thirds of all new HIV infections and face high rates of unintended pregnancy. Multipurpose prevention technologies (MPTs) are promising products under development that are designed to simultaneously prevent HIV and unintended pregnancy. Since MPTs will be used in the context of sexual relationships, ensuring acceptability and use requires understanding the role of male partners in MPT use decision‐making.
Methods
This paper draws on qualitative data from 39 couples enrolled in the Microbicide Trials Network (MTN) 045 study, conducted in 2019–2020. Partners completed a discrete choice experiment (DCE), first separately and then jointly, to measure preferences for future MPT attributes and then completed a qualitative interview. We also draw on quantitative data from interviewer observation about who dominated the decision‐making process during the joint DCE. Content analysis was used to examine (1) how couples made decisions on existing non‐MPT HIV and pregnancy prevention products; (2) how couples made decisions on future ideal‐MPT product during the DCE; and (3) how these decision‐making processes varied by decision‐making dominance (10 male, 10 female and 19 equal) and interview type (19 joint and 20 separate).
Results
Existing non‐MPT product decisions focused on trust between partners and product attributes, while future ideal‐MPT product decisions exclusively focused on product attributes. Across existing and future products, preferences for product attributes varied by gender. Male partners were most concerned with limiting side effects impacting sexual pleasure, female partners were most concerned with limiting side effects causing physical symptoms and both were concerned with the return to fertility. Across all dominance and interview types, couples reported making decisions together and female partners were often able to negotiate with male partners for their preferred product or set of product attributes.
Conclusions
Research activities in this study provided an opportunity for couples to openly present their product attribute preferences to their partner, learn about their partner's attribute preferences, negotiate for their ideal set of attributes and ultimately choose attributes that benefited the couple without disempowering the female partner. Future research should focus on the utility of couple‐based decision‐making aids or similar tools for facilitating joint MPT decision‐making.
Keywords: couples, multipurpose prevention technologies, HIV, contraception, pregnancy, decision‐making
1. INTRODUCTION
In sub‐Saharan Africa (SSA), young women account for two‐thirds of new HIV infections and face high rates of unintended pregnancy [1, 2, 3, 4, 5, 6]. Dual method use, or the use of a condom and another contraceptive method, is the most reliable protection against sexually transmitted infections, such as HIV, and unintended pregnancy [7, 8, 9, 10]. Yet, the uptake of dual method use among women in SSA remains low [11, 12, 13, 14, 15, 16, 17]. Clinical studies, acceptability studies and market research suggest women would prefer a single product that prevents both HIV and unintended pregnancy [18, 19, 20, 21]. Currently, the only available single product, or modern multipurpose prevention technology (MPT), is the condom. However, condoms are not an ideal MPT because condom use must be negotiated between partners, often requires a male partner's acceptance, and has a high failure rate compared to other contraceptive methods [22, 23].
Several MPT products are in development, such as oral pills, vaginally inserted products (e.g. rings, inserts and films) and implants [24, 25]. Given that MPT products will be used in the context of sexual relationships, ensuring their acceptability and use requires understanding barriers and facilitators beyond individual and structural factors, such as interpersonal dynamics. Past HIV prevention trials of oral pre‐exposure prophylaxis (PrEP) and the dapivirine vaginal ring have shown the influence of male partners on product use and suggest the importance of their involvement and support in HIV and pregnancy prevention decisions [26, 27, 28, 29, 30, 31]. Previous studies have found that both genders are more likely to report using contraception if they have discussed family planning with their partners, even in couples with discordant fertility goals and where the male partner has a stronger preference for more children [32, 33, 34, 35, 36, 37]. In Malawi, increased contraceptive communication with male partners was a pathway through which a small‐group intervention increased contraceptive use in young women [38]. Despite evidence that HIV and pregnancy prevention communication increases method uptake and adherence, couple‐based communication about these topics is infrequent in SSA [39, 40]. Researchers attribute low levels of communication to prevailing gender norms that emphasize male‐dominated decision‐making regarding sexual and reproductive health issues [32, 39, 41].
This evidence resonates with Lewis's model of interdependence and communal coping [42]. The model posits that when couples are faced with a health decision, their predisposing characteristics (e.g. communication patterns, gender norms, trust and social support) influence a “transformation of motivation” otherwise known as their ability to reorient from individual‐centred decision‐making to couple‐centred decision‐making. Positive and equitable predisposing characteristics can lead to a transformation of motivation and in turn, allows a couple to engage in communal coping where they cooperatively engage in health‐enhancing behaviours (e.g. MPT use) [43, 44, 45, 46, 47]. Given the importance of male partner involvement for many women and the potential for more open communication in relationships to increase HIV prevention and contraceptive use, facilitating equitable decision‐making processes that lead to the transformation of motivation among couples constitutes a promising strategy to support future MPT use.
The Microbicide Trials Network (MTN) 045 study aimed to evaluate couples’ preferences for MPT product attributes and to understand the decision‐making process of couples’ when selecting an ideal MPT product. In the present analysis, we utilized qualitative data from the study to explore (1) how couples made decisions on existing HIV and pregnancy prevention products; (2) how couples made decisions on a future ideal MPT product; and (3) how these decision‐making processes varied by relationship dominance (male partner dominant, female partner dominant or equal contributions) and interview type (together as a couple or separate). By comparing decision‐making processes across existing products, future ideal products, gender dominance and interview type, we aim to understand couples’ priorities for a future MPT product and to inform the development of strategies to increase uptake and adherence to MPT products among couples when they become available for widespread use.
2. METHODS
2.1. Study overview
2.1.1. Main study
The MTN 045 study was designed to elicit couples’ preferences for MPT products in development and how those factors might affect acceptability and adherence to future MPT products [48]. The study enrolled 400 heterosexual couples in Uganda (N = 200) and Zimbabwe (N = 200) between November 2019 and December 2020. Eligible couples had been together for at least 3 months, were willing and able to provide consent, and expressed interest in contraception and/or HIV prevention. The female partner was required to be between the ages of 18 and 40 at enrolment and HIV negative by self‐report. The male partner was required to be 18 years or older. Participants were recruited from communities in Uganda and Zimbabwe through community meetings, stakeholder outreach, and community advisory board engagement activities. All participants were shown placebo versions of hypothetical product forms, and a video introducing the attributes of the hypothetical product forms, included in the discrete choice experiment (DCE). The DCE involved participants making nine choices between two hypothetical products (see Figure 1 for an illustrative example). Following each choice question, participants were asked their preference between their chosen product and male condoms. All participants completed an individual DCE and a joint DCE with their partner.
Figure 1.
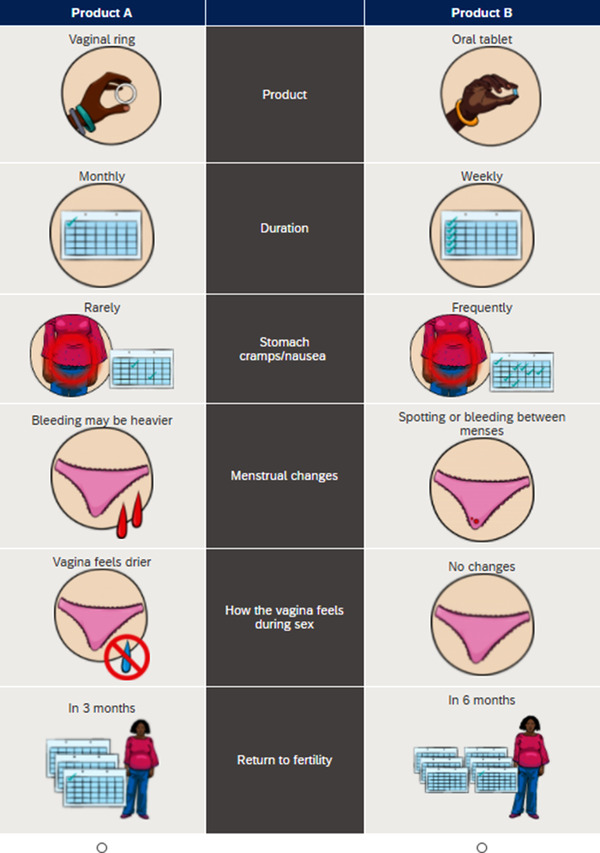
Example of a DCE choice set question. Participants were asked to select which MPT product they would want to use (females) or want their partner to use (males) for HIV and pregnancy prevention.
While the couple was completing the joint DCE, interviewers used a couple observation tool to capture couple dynamics. The tool was developed based on principles from psychology and couples counselling interventions [49, 50]. It included a checklist of attributes discussed and who dominated those discussions (male, female and both equally). Interviewers underwent interactive training on the use of the tool which included practising based on videos of couple interactions, the role of self‐awareness in observations and regular coaching in team meetings throughout the study. A minimum of 20% of sessions were jointly observed by two interviewers and inter‐observer reliability was calculated and monitored. Assessments on which observers disagreed were discussed and a consensus decision was reached. Across sites, the average agreement was 92% (standard deviation [SD] 0.07). Agreement was, on average, 94% (SD 0.05) in Zimbabwe and 86% (SD 0.11) in Uganda. Full details of recruitment procedures, DCE development and DCE results are detailed in the parent study publication [51].
2.1.2. Present study
This analysis includes a subsample of 39 couples from the main study who were purposively subsampled for in‐depth qualitative interviews after both partners individually and jointly completed a DCE and data were collected through the couple observation tool on dominance. The research team at each site invited up to 20 couples to complete interviews, with interviews conducted either with both members of the couple together or separately. Interview questions and themes are detailed in Table 1. The team targeted roughly equal numbers of IDIs conducted with couples together or separately and as well as with couples representing a range of decision‐making dominance (e.g. male partner dominant, female partner dominant or equal contributions). In terms of communication dominance during the DCE, our qualitative sample included 19 couples observed as equal contributors, 10 couples that were male dominant and 10 couples that were female dominant. Couples were interviewed jointly (N = 19) or separately (N = 20), resulting in a total of 59 interviews (19 joint interviews and 40 individual interviews) Additional allowance for couples deemed as interesting cases was made for sample selection. IDIs took place at a separate visit that occurred within 1 month following the main study visit. All participants provided written informed consent at study enrolment and confirmed consent verbally prior to beginning the qualitative interview.
Table 1.
Interview questions
| Theme | Interview questions and illustrative probes |
|---|---|
| Relationship characteristics | Let us start by talking about your relationship. First, tell me how and where you met.
|
How would you describe your relationship with other people now?
|
|
What is it like for couples in your community to talk about (1) pregnancy—including preventing, spacing or planning pregnancy and (2) HIV prevention?
|
|
Could you tell me about the last conversation you had about pregnancy prevention and HIV prevention with your partner?
|
|
| MPT interest | What are some of the reasons why you would want to use a dual‐purpose prevention product for pregnancy and HIV prevention?
|
What are some reasons [you/you and your partner] would not want to use a dual‐purpose prevention product for pregnancy and HIV prevention?
|
|
If you wanted to prevent or space pregnancies and wanted to protect yourself from HIV, would you prefer to use one product that protects against both HIV and pregnancy, or would you rather use two different products—one for HIV prevention and another for pregnancy prevention?
|
|
|
MPT product preference |
[Participants were presented with a visual tool depicting product attributes and features to remind them of the choices of previous interview.] Can you describe the product that [you/you and your partner] chose as your preference for the prevention of HIV and unintended pregnancies when you completed your DCE interview together?
|
| Partner and community influence |
Could you describe how the choices you made individually versus together may have differed?
|
How did you and your partner reach the decision to choose a particular product together?
|
|
What other factors may influence your preference for and interest in the future use of a dual‐purpose prevention product?
|
2.2. Data collection procedures
A semi‐structured interview guide was developed to explore couple dynamics and their influence on HIV prevention and contraceptive decisions, behaviours and preferences. The guide was developed by core study team members (JE, MH and AM) and then reviewed and revised for applicability and content validity by other protocol team members. Specific interview questions of interest for the present analysis pertained to decision‐making around existing and future HIV and pregnancy prevention options and attributes. We used neutral probes to gather detailed responses and elicit illustrative examples where necessary. This gave participants the chance to elaborate on information that they felt was important to tell the interviewer. Experienced study staff conducted the interviews in English and/or Luganda (in Uganda) and Shona (in Zimbabwe). Interviewers were trained on the semi‐structured interview guide, qualitative research principles and on issues specific to interviewing couples, such as handling conflict and engaging both members of the couple.
Interviewers were also trained to maintain some physical distance so as not to intrude when couples were completing activities. However, in cases where couples may not have been communicating verbally, interviewers prompted couples to verbalize their decision‐making processes to allow for accurate assessments of the couple's interaction. All interviewers in Zimbabwe were women, while participants in Uganda could choose a male or female interviewer. The staff member met participants at the study site for a 60‐minute, digitally recorded interview. The study staff used a transcription protocol to transcribe and translate interviews into English. Staff members who conducted the interviews then reviewed the transcripts for transcription and translation accuracy. All transcripts were de‐identified, underwent quality control checks and were stored on a HIPAA‐protected encrypted shared drive. The study was approved by Institutional Review Boards and Ethics Committees in Zimbabwe, Uganda, Canada and the United States.
2.3. Data analysis
Structured debriefing reports documenting key themes, questions from the semi‐structured interview guide and constructs from Lewis's model of interdependence and communal coping were used to derive the preliminary codebook [42]. Six team members (MK, SS, AM, MH, MS and AY) reviewed two randomly selected transcripts to identify and discuss additional codes. The study team reviewed the codebook for gaps and redundancies. Two co‐authors (MK and SS) then revised the codes and corresponding definitions to develop a final codebook. Four coders (MK, AY, SS and EO) independently applied codes to a total of 59 transcripts (19 joint and 40 individual interviews).
To achieve consistency in the application of codes, the study team (coders, content experts and site personnel) coded 8–10 transcripts per week and convened weekly to discuss discrepancies and reach a consensus. Members from each site's study team were present in the coding meetings to share insights based on their involvement in data collection and familiarity with transcripts. Throughout coding, the study team used consensus to resolve areas of disagreement, made necessary changes with code applications in Dedoose (SocioCultural Research Consultants, LLC; Los Angeles, California) and subsequently achieved satisfactory agreement to establish consistency in the application of codes.
Once all coding and inter‐rater reliability exercises were completed, the lead author developed an analysis plan. The analysis team used content analysis to examine the results of the coding process across participants and synthesized the information based on emerging themes and sub‐themes in summary memos. The analysis was structured to understand the differences and similarities between participants regarding dominance, couple versus individual decision‐making and conflicts in using existing HIV and pregnancy prevention products. Mentions of decision‐making changes in each interview were counted and summarized by direction of change and dominance (Table 2). The analysis team prepared detailed syntheses of findings from the summary memos and met every week to discuss key themes and ensure appropriate interpretation within the context of analytical objectives.
Table 2.
Mentions of DCE decision change during the qualitative interview
| Total | Equal contribution | Male dominance | Female dominance | |||||
|---|---|---|---|---|---|---|---|---|
| N = 59 | (%) | n = 21 | (%) | n = 20 | (%) | n = 18 | (%) | |
| MP changed FP's decision | 11 | (19%) | 3 | (14%) | 6 | (30%) | 2 | (11%) |
| FP changed MP's decision | 27 | (46%) | 10 | (48%) | 8 | (40%) | 9 | (50%) |
| MP and FP same decision | 5 | (8%) | 2 | (10%) | 1 | (5%) | 2 | (11%) |
| No mention of decision change | 16 | (27%) | 6 | (29%) | 5 | (25%) | 5 | (28%) |
3. RESULTS
3.1. Partner and couple characteristics
Our sample included 39 couples who participated in the MTN‐045 study. The median age of the female partner was 26 years (interquartile range [IQR] 18–38) and was 30 years for male partners (IQR 19–45). Most female partners had a secondary school education (64%, N = 25) and had previously given birth (74%, N = 29). Similarly, most male partners had a secondary school education (74%, N = 29) and were fathers (74%, N = 29).
The mean duration of relationships was 5.4 years (range 0.7–21) with most couples reporting that they jointly made decisions about family planning (74%, N = 29), were married or cohabitating (82%, N = 32) and currently used a pregnancy prevention method (82%, N = 32). The most used method was oral contraceptive pills (33%, N = 13) (Table 3). Across the 59 interviews, it was most often mentioned that female partners were able to change a male partner's DCE decision ( = 27, 46%) follow by no mention of decision change (N = 26, 27%), male partners changing a female partner's decision (N = 11, 19%) and both partners having the same decision (N = 5, 8%).
Table 3.
Couple characteristics
| Total couples (N = 39) | Equal contribution (N = 19) | Male dominance (N = 10) | Female dominance (N = 10) | |||||
|---|---|---|---|---|---|---|---|---|
| Age in years (mean, median and range) | ||||||||
| Female partner | 26, 25 | (18–38) | 26, 25 | (18–38) | 25, 23 | (19–33) | 25, 25 | (18–38) |
| Male partner | 30, 30 | (19–45) | 29, 30 | (19–45) | 31, 36 | (20–40) | 29, 28 | (21–38) |
| Completed secondary school | ||||||||
| Female partner | 25 | (64%) | 14 | (74%) | 5 | (50%) | 6 | (60%) |
| Male partner | 29 | (74%) | 14 | (74%) | 9 | (90%) | 6 | (60%) |
| Married or cohabitating | 32 | (82%) | 14 | (74%) | 10 | (100%) | 8 | (80%) |
| Type of pregnancy prevention method currently used | ||||||||
| Oral pills | 13 | (33%) | 6 | (32%) | 4 | (40%) | 3 | (30%) |
| Injectable (or shot) | 6 | (15%) | 4 | (21%) | 1 | (10%) | 1 | (10%) |
| Implant | 5 | (13%) | 4 | (21%) | 0 | (0%) | 1 | (10%) |
| IUD | 1 | (3%) | 0 | (0%) | 0 | (0%) | 1 | (10%) |
| Male condom | 10 | (26%) | 7 | (37%) | 2 | (20%) | 1 | (10%) |
| Natural method | 3 | (8%) | 3 | (16%) | 0 | (0%) | 0 | (0%) |
| None | 7 | (18%) | 1 | (5%) | 2 | (20%) | 4 | (40%) |
| Relationship duration in years (mean, median and range) | 5.4, 3 | (0.7–21) | 4.7, 2 | (0.7–21) | 6.1, 3.5 | (2–14) | 5.8, 2.5 | (1–19) |
| Joint decision‐making on family planning | 29 | (74%) | 16 | (84%) | 7 | (70%) | 6 | (60%) |
| Interview type | ||||||||
| Joint | 19 | (49%) | 12 | (63%) | 3 | (30%) | 4 | (40%) |
| Separate | 20 | (51%) | 7 | (37%) | 7 | (70%) | 6 | (60%) |
3.2. Decision‐making among existing HIV and pregnancy prevention options
In our sample, decision‐making discussions related to HIV prevention had different drivers and motivators than decision‐making discussions about pregnancy prevention. Decision‐making discussions related to HIV prevention centred on trust between partners and decision‐making discussions related to pregnancy prevention centred on attributes of contraceptive methods. The following paragraphs detail how HIV and pregnancy prevention decision‐making processes varied by relationship dominance (equal, male and female) but not by interview type (joint and individual).
Overall, levels of trust influenced frequency and topics of discussion as well as reported behaviours. For example, couples expressing a high level of trust reported increased HIV testing and limited condom use. In contrast, couples with a low level of trust reported infrequent HIV prevention discussions and constant vigilance which included asking the partner about where they go outside of the home, if they have met someone of the opposite gender at work and about who is calling them or sending them text messages. Couples with low levels of trust additionally reported that suggesting or accepting condom use indicated engagement in sexual relationships outside of the partnership.
MP: One only thing I caution her about is to be faithful. I told her that in case she is found HIV positive in future, that will be the end of our relationship. That if we are tested and she is found positive and I negative we shall end our relationship there and then. I know if she suggests condoms she is unfaithful. (Equal Dominance, Individual Interview, Zimbabwe)
Contraceptive method attribute discussions largely focused on differing partner preferences for return to fertility and interest in limiting the female partner's experience of side effects and decreases in the male partner's sexual pleasure. Among couples deemed to contribute equally to decision‐making (equal dominance), couples reported being open to communication on HIV and pregnancy prevention. Reasons for communication and prevention product use included needing to keep each other safe from HIV, birth spacing of future children and financial needs related to childcare.
MP: Usually it is her (female partner) who says that she does not at all want to get pregnant because of our financial status as I said earlier. She does not want to get into that before we are prepared. It is only that for the first pregnancy she was still young after school. And I also don't want it (getting another child) like I told you earlier. So we talk about it (prevention of pregnancy). She welcomed it and she said that the product will work for us if we sit down and choose together what can be better for us. (Equal Dominance, Individual Interview, Uganda)
In terms of HIV prevention, equal dominance couples reported testing for HIV more frequently, disclosing their results to their partners and deciding not to use condoms based on trust built from both behaviours. In terms of pregnancy prevention, equal dominance couples reported discussing the advantages and disadvantages of specific contraceptive methods together and choosing products that satisfied both partners and limited physical side effects for the female partner.
Couples dominated by either male or female member reported communication on HIV and pregnancy prevention to be infrequent and occasionally fraught. Reasons for infrequent communication included gendered beliefs on whether HIV and pregnancy prevention decisions should be openly discussed and assumptions that initiating discussions indicated the existence of other sexual partners.
MP: That when you are faithful to each other, you also become jealous of each other.
So, when talking about HIV prevention, you just emphasize one thing that you need to be faithful to each other to prevent HIV. But even if the woman is the one who is having other sexual partners, it is not easy for the man to tell the wife to use the condoms whenever she has sex with other men. It will appear as if he is giving her the permission to carry on with her reckless behaviour. So, that will stop people from discussing such issues. (Male Dominance, Individual Interview, Zimbabwe)
Male‐ and female‐dominated couples reported that fears of infidelity drove either partner to suggest HIV testing and condom use. However, condom use was largely dictated by male partners because condoms are regarded as a male product and male partners are often the final decision makers. There were differences in stated views regarding pregnancy prevention comparing male and female dominance couples. In male dominance couples, couples reported that pregnancy prevention choices were made according to the sexual needs and fertility interests of male partners. Male partners were unsupportive of methods with high costs, a delayed return to fertility or side effects that inhibited sex, such as irregular bleeding, decreased libido and vaginal dryness.
FP: The other issue is that most men do not like those family planning methods that we use because of side effects like irregular bleeding so they don't like them and that's why in most cases the men refuse the women to use them because you are bleeding and he cannot fulfil his need.
MP: And there is a way they change the woman
FP: That's when one says do not use it again
MP: There is a way they change the woman.
MP: The woman's sex libido is low and sometimes she doesn't completely want sex because she has no feelings
(Male Dominance, Joint Interview, Uganda)
In female dominance couples, couples reported that the female partner was “allowed” to choose the product because she was the one to use it and experience the side effects.
FP: He will say whatever you like. Sometimes I say I'm going for an injection and he just says, whatever you want is what you do. If what you have is not working for you, you can change it. So in the end it's my decision to make. (Female Dominance, Individual Interview, Zimbabwe)
3.3. Decision‐making regarding future MPT attribute preferences
When discussing decision‐making during the DCE activity, couples mentioned it as a negotiation among the prescribed set of potential product attributes with limited mentions of trust. Male partners were most concerned with side effects impacting sexual pleasure (change in menses and vaginal dryness), female partners were most concerned with side effects causing physical symptoms (headache, cramps and heavy bleeding) and both partners were concerned with the return to fertility.
FP: I think that at first, we were looking at my health as a woman, because I will be the one using the product, secondly we were looking at how it helps my partner to be free in the home [to be happy and satisfied sexually]. Such that I feel that if we use this product, his chances of having extra marital affairs will be slimmer, so it is important for us as family. I think that my partner was more concerned about how the vagina feels, that it should not be too dry, or too wet. Because dryness it will make me feel pain during sex, If it becomes too wet, it would not be good. (Male Dominance, Joint Interview, Uganda)
Many couples acknowledged that the attributes and product they chose when they completed the DCE alone was different than the attributes and product they chose when they completed the DCE with their partner.
MP: Haa, when I chose alone and when we made the choices together, what was different was, the woman was the one who would be using the products, so most of the choices were her preferences. Because in doing things we should be in agreement. Even if I have what I like, and my wife doesn't like it, I shouldn't oppose it. (Equal Contributor, Individual Interview, Zimbabwe)
When there was disagreement on the importance of specific attributes during the DCE, couples described a process of joint decision‐making where each partner was able to present their views and openly discuss their preferences. Though female partners across all dominance types were often able to convince their male partner to choose their preferred product or set of attributes (Table 2), the reasons for which their partner made the final decision varied by relationship dominance (equal, male and female). We did not find substantial differences by interview type (joint and individual).
Among equal and female dominance couples, couples often reported that the male partner “allowed” the female partner to make the decision on the final product, which was similar to reports from participants on existing product decision‐making. Reasons for relegating the final decision were that female partners cannot be forced and should like the product, are the ones who will use the product, experience side effects of the product and have a reliable judgement from their previous product experiences.
MP: Like I told you that my wife has a right to decide because the method is to go in her body, I could not impose anything on her, just because when it is time to go into her periods she informs me about it because I know what she goes through with the pain. So I realized that maybe that alone could save her the pain of the cramps. So I went by her choice as she had that fear that it may give her pains, though she had never used it. I would support her by advising her about side effects but since she experiences most of these I left her to make most of the final decisions. (Female Dominance, Individual Interview, Uganda)
Among male dominance couples, some female partners reported having to accept the choice of their male partner though they would have chosen differently if they could make an independent decision. In addition, some female partners in this couple dominance type reported not sharing their product preferences with their partners after discovering that they were different than the male partner's preferences. Reasons for accepting male partner preference included perceived fears of abandonment due to decreased sexual pleasure, male partners being the head of the household and limiting potential blame for outcomes.
FP: I accepted his choice. You know, even if it fails to work but when you had selected it together with your partner, there is no blaming you because you had agreed together with him. (Male Dominance, Individual Interview, Uganda)
3.4. Benefits of joint decision‐making during DCE
Reported benefits of joint decision‐making afforded by the DCE did not vary by dominance type or interview type. Benefits specifically included building trust, improving communication and deciding on an ideal product that served the couple instead of the individual. These benefits ultimately led to greater satisfaction in their final choice of products and attribute characteristics.
FP: [Making a choice as a couple] is important…we enjoyed it so much because we were together so no one would blame the other. We both understood the method and made a choice out of our decision. So in case of any changes no one will question the other because we are aware that there will either be a change or not. (Male Dominance, Joint Interview, Zimbabwe)
Couples reported that joint decision‐making during the DCE also increased male partner awareness of potential product side effects and how to support their partner in product use. Having discussions about all types of products also provided an opportunity to correct misinformation and learn more about existing options.
MP: I have no challenge sitting as a couple to make a decision. Actually, it is very important because if I make the choice alone there are some important things that I may ignore or I may not see it but if we are together she may advise me or I advise her so we have no challenges sitting as a couple. I learned more about products as they are now through the discussion and how to support her (Equal Contribution, Joint Interview, Uganda)
4. DISCUSSION
In a study of couples’ preferences for future MPT products to prevent HIV and unintended pregnancy conducted in Uganda and Zimbabwe, we collected qualitative data to understand how couples made decisions about the future MPT products presented, drawing also on discussions of their decisions related to existing HIV and pregnancy prevention options. We then evaluated whether decision‐making processes varied by couples’ relationship dominance (female‐dominated, male‐dominated and equal contribution) and interview type (couple interviewed jointly or separately). We found that decisions on products focused on trust and product attributes and varied by relationship dominance, but not by interview type.
Existing product decisions focused on trust and product attributes, while future product decisions exclusively focused on product attributes. Trust was primarily associated with the HIV prevention aspect of existing product decisions rather than the pregnancy prevention aspect. Trusting couples frequently communicated about HIV prevention and cooperatively made decisions on HIV testing and condom use. Mistrusting couples infrequently communicated about HIV prevention and reported that initiating related discussions or condom use signalled the existence of other sexual partners. Other studies among young couples in SSA have similarly found partners unable to discuss HIV testing and condom use without raising suspicions of infidelity which in turn impacted their ability to engage in HIV prevention behaviours [52, 53, 54, 55]. Given that the topic of trust was largely absent from future product decisions, our results suggest that MPTs could potentially minimize the need for continued HIV prevention negotiation among couples and the associated infidelity implications that prevent cooperative decision‐making to reduce HIV risk. In contrast to existing HIV prevention options, most couples in our sample reported open communication about existing pregnancy prevention options and a willingness to discuss future products. Thus, our results additionally suggest the potential acceptability of MPT communication among couples which will be important for uptake and adherence with future products.
Across existing and future products, preferences for product attributes varied by gender. Male partners were most concerned with limiting side effects impacting sexual pleasure (changes in menstrual bleeding and vaginal dryness), female partners were most concerned with limiting side effects causing physical symptoms (headaches, stomach pain and heavy bleeding) and both were concerned with the return to fertility. Though our results reflect known gender‐based barriers to contraceptive uptake [55, 56, 57], they add valuable context to the existing literature on MPT product preferences which has largely excluded the perspective of male partners [21, 58, 59, 60, 61, 62], who often wield considerable influence in couple‐based sexual and reproductive health decision‐making in the region [32, 39, 53, 63, 64, 65]. Our results also highlight the need for future MPTs to align with gendered product attribute preferences and the need for future MPT messaging to be clear about product side effects.
Across all relationship dominance types, couples reported making decisions together and female partners were often able to negotiate with male partners for their preferred product or set of product attributes. Many couples also acknowledged that the attributes and product they chose when they completed the DCE alone was different than the attributes and product they chose when they completed the DCE with their partner. Couples reported that the DCE provided a way to openly present their attribute preferences to their partner, learn about their partner's attribute preferences and make decisions that benefited the couple. Our results suggest that joint decision‐making activities (like the DCE) that focus on product attributes pertinent to choice and use could potentially provide an opportunity for a “transformation of motivation” (e.g. a mechanism in Lewis's model of interdependence and communal coping) which sets the stage for communal coping (e.g. MPT uptake and adherence). Female partners’ ability to negotiate for their preferences was also encouraging given prevailing gender norms and existing apprehension among researchers, practitioners and providers that involving male partners in sexual and reproductive decision‐making disempowers women [30, 55, 66, 67, 68, 69]. In addition, we know that many women do want to involve their male partners in their sexual and reproductive decision‐making, and doing so can improve the duration of product use [34, 39, 70, 71]. Future research to explore if couples’ attribute preferences and priorities elicited through the joint DCE align with their actual prevention choices will be essential to informing the development of provider‐delivered counselling and other interventions to support future MPT use.
This study has several important limitations. First, with a purposively selected sample, our findings cannot be generalized to a wider population. The couples in our study were willing to enrol in a study together and were interested in HIV prevention and family planning, which may not reflect the interests or experiences of other couples in Zimbabwe or Uganda. We were relatedly unable to measure the impact of relationship stability on MPT preference, which also limits our ability to generalize to the experiences of all couples in either country. Despite these limitations, we were able to include couples with a range of relationship dominance types and relationship lengths. Second, the transcripts were translated from Luganda and Shona to English and as with any translation, there was undoubtedly some level of information and understanding that was lost during the interpretation process. To minimize these losses, transcripts underwent quality control checks by those conducting and transcribing the interviews. Likewise, individuals from both site teams were involved in coding discussions and reviewing analysis. Third, it is possible that our results are partially reflective of observer presence during the DCE and social desirability bias underlying the reported interest in joint decision‐making. However, comments from male partners suggest that they felt comfortable describing their role as the primary decision maker. Separate interviews for male and female partners, with the option of gender‐matched interviewers, if preferred (Uganda only) allowed for openness. We did not find differences in patterns of decision‐making comparing the couple and individual interviews. Finally, though this was a couple‐based study, we must acknowledge that there are many other social network actors and processes that influence HIV and pregnancy prevention product use decisions.
5. CONCLUSIONS
Young women in many parts of SSA face high rates of HIV and unintended pregnancy and studies have documented keen interest by women in a product that combines HIV prevention and contraception. Given that MPTs will be used in the context of sexual relationships, ensuring uptake and adherence requires understanding whether and how to involve male partners in MPT use decision‐making for women who are in heterosexual relationships. The research activities in this study (DCE, survey questions completed jointly about preferences and qualitative interviews) prompted conversations that supported joint decision‐making among couples, regardless of relationship dominance type. These activities provided an opportunity for couples to openly present their attribute preferences to their partner, learn about their partner's attribute preferences, negotiate for their ideal set of attributes and ultimately make decisions that benefited the couple without disempowering the female partner. Developing couple‐based decision‐making aids or other tools may provide a mechanism through which women can negotiate with male partners to support their transformation of motivation, thereby encouraging MPT uptake and adherence when they become available for widespread use.
COMPETING INTERESTS
The authors have no competing interests or financial interests relevant to this article to disclose.
AUTHORS’ CONTRIBUTIONS
AMM and JE led study development and oversight as protocol chair and co‐chair. PM, JN, IR, PM and JE led data collection activities at their research sites and contributed to the interpretation of the results. MKSQ provided overall study coordination and contributed to study development and the interpretation of the results. MH helped conceptualize the analysis and contributed to the interpretation of the results. MCDS contributed to manuscript writing and the interpretation of the results. SRS coded and analysed data and contributed to manuscript writing and the interpretation of the results. MAL reviewed the manuscript and contributed to the interpretation of the results. JP contributed as DAIDS medical officer with key contributions to protocol development and management. NLB led manuscript development, analysis and writing. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
FUNDING
This research was supported by the Microbicide Trials Network (MTN). From 2006 until 2021, the MTN was part of the HIV/AIDS clinical trial network and was funded by the National Institute of Allergy and Infectious Diseases (UM1AI068633, UM1AI068615 and UM1AI106707), with co‐funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development and the National Institute of Mental Health, all components of the U.S. National Institutes of Health.
DISCLAIMER
The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
ACKNOWLEDGEMENTS
The authors would like to acknowledge the efforts of the CUPID study teams, particularly their creativity and persistence in restarting the study after a 2‐month COVID‐19‐related pause, and then conducting the research with safety protocols in place during the COVID‐19 pandemic. We would also like to thank the members of the protocol team for their leadership in guiding study development and implementation.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
REFERENCES
- 1. MacPhail C, Pettifor AE, Pascoe S, Rees HV. Contraception use and pregnancy among 15–24 year old South African women: a nationally representative cross‐sectional survey. BMC Med. 2007;5:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. UNAIDS . Women and HIV: a spotlight on adolescent girls and young women. UNAIDS; 2019. [Google Scholar]
- 3. Kott A. Rates of unintended pregnancy remain high in developing regions. Int Perspect Sex Reprod Health. 2011;37:46–7. [Google Scholar]
- 4. Mayondi GK Wirth K, Morroni C, Moyo S, Ajibola G, Diseko M, et al. Unintended pregnancy, contraceptive use, and childbearing desires among HIV‐infected and HIV‐uninfected women in Botswana: across‐sectional study. BMC Public Health. 2016;16:44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Mukiira C, Mumah J, Kabiru CW, Izugbara CO. Unintended pregnancy by the numbers: a look at Kenya. 2014.
- 6. Christofides NJ, Jewkes RK, Dunkle KL, Nduna M, Shai NJ, Sterk C. Early adolescent pregnancy increases risk of incident HIV infection in the Eastern Cape, South Africa: a longitudinal study. J Int AIDS Soc. 2014;17:18585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Pazol K, Kramer MR, Hogue CJ. Condoms for dual protection: patterns of use with highly effective contraceptive methods. Public Health Rep. 2010;125:208–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gebrehiwot SW, Azeze GA, Robles CC, Adinew YM. Utilization of dual contraception method among reproductive age women on antiretroviral therapy in selected public hospitals of Northern Ethiopia. Reprod Health. 2017;14:125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lopez LM, Stockton LL, Chen M, Steiner MJ, Gallo MF. Behavioral interventions for improving dual‐method contraceptive use. Cochrane Database Syst Rev. 2014;CD010915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. O'Leary A. Are dual‐method messages undermining STI/HIV prevention? Infect Dis Obstet Gynecol. 2011;2011:691210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kosugi H, Shibanuma A, Kiriya J, Wafula SW, Jimba M. Consistent condom use among highly effective contraceptive users in an HIV‐endemic area in rural Kenya. PLoS One. 2019;14:e0216208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kopp DM, Tang JH, Stuart GS, Miller WC, O'Shea MS, Hosseinipour MC, et al. Dual method use among postpartum HIV‐infected and HIV‐uninfected Malawian women: a prospective cohort study. Infect Dis Obstet Gynecol. 2017;2017:e1475813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Mbita G, Mwanamsangu A, Plotkin M, Casalini C, Shao A, Lija G, et al. Consistent condom use and dual protection among female sex workers: surveillance findings from a large‐scale, community‐based combination HIV prevention program in Tanzania. AIDS Behav. 2020;24:802–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Odutola A, Baisley K, Hayes RJ, Rusizoka M, Tanton C, Weiss HA, et al. Pregnancy and contraceptive use among women participating in an HIV prevention trial in Tanzania. Sex Transm Infect. 2012;88:436–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Toska E, Cluver L, Laurenzi CA, Wittesaele C, Sherr L, Zhou S, et al. Reproductive aspirations, contraception use and dual protection among adolescent girls and young women: the effect of motherhood and HIV status. J Int AIDS Soc. 2020;23(Suppl 5):e25558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Osuafor GN, Maputle SM. Dual protection and contraceptive method use among women in heterosexual relationships in Mahikeng, South Africa. Afr J Reprod Health. 2017;21:64–72. [DOI] [PubMed] [Google Scholar]
- 17. MacPhail C, Pettifor A, Pascoe S, Rees H. Predictors of dual method use for pregnancy and HIV prevention among adolescent South African women. Contraception. 2007;75:383–9. [DOI] [PubMed] [Google Scholar]
- 18. Karim SA, Baxter C, Frohlich J, Karim QA. The need for multipurpose prevention technologies in sub‐Saharan Africa. BJOG Int J Obstet Gynaecol. 2014;121(Suppl 5):27–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Begg L, Brodsky R, Friedland B, Mathur S, Sailer J, Creasy G. Estimating the market size for a dual prevention pill: adding contraception to pre‐exposure prophylaxis (PrEP) to increase uptake. BMJ Sex Reprod Health. 2021;47:166–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. van der Straten A, Agot K, Ahmed K, Weinrib R, Browne EN, Manenzhe K, et al. The Tablets, Ring, Injections as Options (TRIO) study: what young African women chose and used for future HIV and pregnancy prevention. J Int AIDS Soc. 2018;21:e25094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Hynes JS, Sales JM, Sheth AN, Lathrop E, Haddad LB. Interest in multipurpose prevention technologies to prevent HIV/STIs and unintended pregnancy among young women in the United States. Contraception. 2018;97:277–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Warren M. Condoms: the multipurpose prevention technologies that already exist. BJOG Int J Obstet Gynaecol. 2014;121:9–11. [DOI] [PubMed] [Google Scholar]
- 23. Warren EA, Paterson P, Schulz WS, Lees S, Eakle R, Stadler J, et al. Risk perception and the influence on uptake and use of biomedical prevention interventions for HIV in sub‐Saharan Africa: a systematic literature review. PLoS One. 2018;13:e0198680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. HIV prevention research, development and implementation pipeline in 2021—and beyond. AVAC; 2019. [Google Scholar]
- 25. Friedland BA, Mathur S, Haddad LB. The promise of the dual prevention pill: a framework for development and introduction. Front Reprod Health. 2021;3:682689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Farquhar C, Kiarie JN, Richardson BA, Kabura MN, John FN, Nduati RW, et al. Antenatal couple counseling increases uptake of interventions to prevent HIV‐1 transmission. J Acquir Immune Defic Syndr. 2004;37:1620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Jani N, Mathur S, Kahabuka C, Makyao N, Pilgrim N. Relationship dynamics and anticipated stigma: key considerations for PrEP use among Tanzanian adolescent girls and young women and male partners. PLoS One. 2021;16:e0246717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Roberts ST, Nair G, Baeten JM, Palanee‐Philips T, Schwartz K, Reddy K, et al. Impact of male partner involvement on women's adherence to the dapivirine vaginal ring during a phase III HIV prevention trial. AIDS Behav. 2020;24:1432–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Montgomery CM, Lees S, Stadler J, Morar NS, Ssali A, Mwanza B, et al. The role of partnership dynamics in determining the acceptability of condoms and microbicides. AIDS Care. 2008;20:733–40. [DOI] [PubMed] [Google Scholar]
- 30. Montgomery ET, van der Straten A, Chidanyika A, Chipato T, Jaffar S, Padian N. The importance of male partner involvement for women's acceptability and adherence to female‐initiated HIV prevention methods in Zimbabwe. AIDS Behav. 2011;15:959–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Montgomery ET, van der Straten A, Stadler J, Hartmann M, Magazi B, Mathebula F, et al. Male partner influence on women's HIV prevention trial participation and use of pre‐exposure prophylaxis: the importance of “understanding”. AIDS Behav. 2015;19:784–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Hartmann M, Gilles K, Shattuck D, Kerner B, Guest G. Changes in couples’ communication as a result of a male‐involvement family planning intervention. J Health Commun. 2012;17:802–19. [DOI] [PubMed] [Google Scholar]
- 33. Tumlinson K, Speizer IS, Davis JT, Fotso JC, Kuria P, Archer LH. Partner communication, discordant fertility goals, and contraceptive use in urban Kenya. Afr J Reprod Health. 2013;17:79–90. [PMC free article] [PubMed] [Google Scholar]
- 34. Sarnak DO, Wood SN, Zimmerman LA, Karp C, Makumbi F, Kibira SPS, et al. The role of partner influence in contraceptive adoption, discontinuation, and switching in a nationally representative cohort of Ugandan women. PLoS One. 2021;16:e0238662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Prata N, Bell S, Fraser A, Carvalho A, Neves I. Partner support for family planning and modern contraceptive use in Luanda, Angola. Afr J Reprod Health. 2017;21:35–48. [DOI] [PubMed] [Google Scholar]
- 36. Bhushan NL, Fisher EB, Maman S, Speizer IS, Gottfredson NC, Phanga T, et al. Communication, social norms, and contraceptive use among adolescent girls and young women in Lilongwe, Malawi. Women Health. 2021;61:440–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Bhushan NL, Phanga T, Maseko B, Vansia D, Kamtsendero L, Gichane MW, et al. Contraceptive conversations among adolescent girls and young women and their partners, peers, and older female family members in Lilongwe, Malawi: a qualitative analysis. Stud Fam Plann. 2021;52(4):397–413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Bhushan NL, Fisher EB, Gottfredson NC, Maman S, Speizer IS, Phanga T, et al. The mediating role of partner communication on contraceptive use among adolescent girls and young women participating in a small‐group intervention in Malawi: a longitudinal analysis. Glob Public Health. 2022;17(7):1392–1405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Blanc AK, Tsui AO, Croft TN, Trevitt JL. Patterns and trends in adolescents’ contraceptive use and discontinuation in developing countries and comparisons with adult women. Int Perspect Sex Reprod Health. 2009;35:63–71. [DOI] [PubMed] [Google Scholar]
- 40. Chandra‐Mouli V, McCarraher DR, Phillips SJ, Williamson NE, Hainsworth G. Contraception for adolescents in low and middle income countries: needs, barriers, and access. Reprod Health. 2014;11:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Mbweza E, Norr KF, McElmurry B. Couple decision making and use of cultural scripts in Malawi. J Nurs Scholarsh. 2008;40:12–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Lewis MA, McBride CM, Pollak KI, Puleo E, Butterfield RM, Emmons KM. Understanding health behavior change among couples: an interdependence and communal coping approach. Soc Sci Med. 2006;62:1369–80. [DOI] [PubMed] [Google Scholar]
- 43. Rogers AJ, Achiro L, Bukusi EA, Hatcher AM, Kwena Z, Musoke PL, et al. Couple interdependence impacts HIV‐related health behaviours among pregnant couples in southwestern Kenya: a qualitative analysis. J Int AIDS Soc. 2016;19:21224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Conroy AA, McGrath N, van Rooyen H, Hosegood V, Johnson MO, Fritz K, et al. Power and the association with relationship quality in South African couples: implications for HIV/AIDS interventions. Soc Sci Med. 2016;153:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Conroy AA. The influence of relationship power dynamics on HIV testing in rural Malawi. J Sex Res. 2015;52:347–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Montgomery CM, Watts C, Pool R. HIV dyadic intervention: an interdependence and communal coping analysis. PLoS One. 2012;7:e40661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Fonner VA, Ntogwisangu J, Hamidu I, Joseph J, Fields J, Evans E, et al. “We are in this together:” dyadic‐level influence and decision‐making among HIV serodiscordant couples in Tanzania receiving access to PrEP. BMC Public Health. 2021;21:720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Minnis A, Etima J, Quinn MS, Musara P, Kemigisha D, Browne E, et al. Heterosexual couples’ preferences for dual‐purpose prevention products for HIV and pregnancy prevention: the CUPID study (MTN‐045) in Uganda and Zimbabwe. J Int AIDS Soc. 2021;24:17–8. [Google Scholar]
- 49. Anme T, Tokutake K, Tanaka E, Watanabe T, Tomisaki E, Mochizuki Y, et al. Short version of the Interaction Rating Scale Advanced (IRSA‐Brief) as a practical index of social competence development. Int J Appl Psychol. 2013;3(6):169–73. [Google Scholar]
- 50. Humbad MN, Donnellan MB, Klump KL, Burt SA. Development of the Brief Romantic Relationship Interaction Coding Scheme (BRRICS). J Fam Psychol. 2011;25:759–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Minnis AM, Etima J, Musara P, Browne EN, Mutero P, Kemigisha D, et al. Couples’ preferences for “2 in 1” multipurpose prevention technologies to prevent both HIV and pregnancy: results of a discrete choice experiment in Uganda and Zimbabwe. AIDS Behav. 2022.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Parker L, Pettifor A, Maman S, Sibeko J, MacPhail C. Concerns about partner infidelity are a barrier to adoption of HIV‐prevention strategies among young South African couples. Cult Health Sex. 2014;16:792–805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Leddy A, Chakravarty D, Dladla S, de Bruyn G, Darbes L. Sexual communication self‐efficacy, hegemonic masculine norms and condom use among heterosexual couples in South Africa. AIDS Care. 2016;28:228–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Crankshaw TL, Voce A, Butler LM, Darbes L. Expanding the relationship context for couple‐based HIV prevention: elucidating women's perspectives on non‐traditional sexual partnerships. Soc Sci Med. 2016;166:169–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Kriel Y, Milford C, Cordero J, Suleman F, Beksinska M, Steyn P, et al. Male partner influence on family planning and contraceptive use: perspectives from community members and healthcare providers in KwaZulu‐Natal, South Africa. Reprod Health. 2019;16:89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Ndinda C, Ndhlovu T, Khalema NE. Conceptions of contraceptive use in rural KwaZulu‐Natal, South Africa: lessons for programming. Int J Environ Res Public Health. 2017;14(4):353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Bain LE, Amu H, Tarkang EE. Barriers and motivators of contraceptive use among young people in sub‐Saharan Africa: a systematic review of qualitative studies. PLoS One. 2021;16:e0252745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Quaife M, Eakle R, Cabrera Escobar MA, Vickerman P, Kilbourne‐Brook M, Mvundura M, et al. Divergent preferences for HIV prevention: a discrete choice experiment for multipurpose HIV prevention products in South Africa. Med Decis Making. 2018;38:120–33. [DOI] [PubMed] [Google Scholar]
- 59. Laborde ND, Leslie J, Krogstad E, Morar N, Mutero P, Etima J, et al. Perceptions of the “Fabric” – an exploratory study of a novel multi‐purpose technology among women in sub Saharan Africa. PLoS One. 2018;13:e0204821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Minnis AM, Krogstad E, Shapley‐Quinn MK, Agot K, Ahmed K, Danielle Wagner L, et al. Giving voice to the end‐user: input on multipurpose prevention technologies from the perspectives of young women in Kenya and South Africa. Sex Reprod Health Matters. 2021;29:1927477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Terris‐Prestholt F, Hanson K, MacPhail C, Vickerman P, Rees H, Watts C. How much demand for new HIV prevention technologies can we really expect? Results from a discrete choice experiment in South Africa. PLoS One. 2013;8:e83193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Minnis AM, Roberts ST, Agot K, Weinrib R, Ahmed K, Manenzhe K, et al. Young women's ratings of three placebo multipurpose prevention technologies for HIV and pregnancy prevention in a randomized, cross‐over study in Kenya and South Africa. AIDS Behav. 2018;22:2662–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Mbweza E, Norr KF, McElmurry B. Couple decision making and use of cultural scripts in Malawi. J Nurs Scholarsh. 2008;40:12–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Gause NK, Brown JL, Welge J, Northern N. Meta‐analyses of HIV prevention interventions targeting improved partner communication: effects on partner communication and condom use frequency outcomes. J Behav Med. 2018;41:423–40. [DOI] [PubMed] [Google Scholar]
- 65. Mosha IH, Ruben R. Communication, knowledge, social network and family planning utilization among couples in Mwanza, Tanzania. Afr J Reprod Health. 2013;17:57–69. [PubMed] [Google Scholar]
- 66. Tao AR, Onono M, Baum S, Grossman D, Steinfeld R, Cohen CR, et al. Providers’ perspectives on male involvement in family planning in the context of a cluster‐randomized controlled trial evaluating integrating family planning into HIV care in Nyanza Province, Kenya. AIDS Care. 2015;27:31–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Stern E, Pascoe L, Shand T, Richmond S. Lessons learned from engaging men in sexual and reproductive health as clients, partners and advocates of change in the Hoima district of Uganda. Cult Health Sex. 2015;17:190–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Aborigo RA, Reidpath DD, Oduro AR, Allotey P. Male involvement in maternal health: perspectives of opinion leaders. BMC Pregnancy Childbirth. 2018;18:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Matseke MG, Ruiter RA, Barylski N, Rodriguez VJ, Jones DL, Weiss SM, et al. A qualitative exploration of the meaning and understanding of male partner involvement in pregnancy‐related care among men in rural South Africa. J. Soc Behav Health Sci. 2017;11. [PMC free article] [PubMed] [Google Scholar]
- 70. Nalwadda G, Mirembe F, Tumwesigye NM, Byamugisha J, Faxelid E. Constraints and prospects for contraceptive service provision to young people in Uganda: providers’ perspectives. BMC Health Serv Res. 2011;11:220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Bellizzi S, Palestra F, Pichierri G. Adolescent women with unintended pregnancy in low‐ and middle‐income countries: reasons for discontinuation of contraception. J Pediatr Adolesc Gynecol. 2019;33(2):144–48. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.


