Abstract
Background:
We aimed to explore the effect of Plan, Do, Check, Act (PDCA) circulation nursing on the prevention of aneurysm after hemodialysis.
Methods:
A total of 139 hemodialysis patients from Oct 2018 to Jan 2020 in Nephrology Department of the First People’s Hospital of Lianyungang, China were enrolled. They were randomly divided into control group and PCDA group, including 58 patients in control group and 81 patients in PCDA group. Patients’ satisfaction, blood flow in arteriovenous internal fistula and the incidence of post-dialysis vascular-related complications were statistically investigated in the two groups.
Results:
The satisfaction of patients in PDCA group was significantly higher than that in control group (P<0.001). In addition, when there was no statistical difference in blood flow between the two groups, the probability of complications such as internal fistula obstruction, thrombosis, infection, secondary puncture and aneurysm was lower in patients in the PDCA group, none of which occurred aneurysm.
Conclusion:
PDCA circulation nursing can effectively improve the quality of care and medical effect of hemodialysis patients with internal arteriovenous fistula, improve patient satisfaction and reduce the incidence of complications.
Keywords: Nursing model, Aneurysm, Hemodialysis
Introduction
End-stage renal disease refers to the end-stage of chronic renal failure caused by various reasons. The disease has a long course, high cost and poor prognosis. It has developed into a major social problem that endangers human health and aggravates the economic burden worldwide (1–3). Hemodialysis can help patients with renal failure to effectively discharge blood toxins and metabolites, and reduce toxic reactions, and arteriovenous internal fistula is the premise of renal failure patients to receive maintenance hemodialysis treatment (4). However, the use of arteriovenous access for a long time, may occur a variety of complications (5). Hemangioma is one of the most common complications. Hemangioma refers to the dilatation of arteriovenous internal fistula accompanied by pulsation, and the tumor wall contains the full thickness of the vascular wall. The inner diameter of the tumor was more than 3 times of the inner diameter of adjacent normal blood vessels and the inner diameter was>2 cm. Hemangioma not only has a great harm to the health of patients, but also because of its obvious changes in the body surface, it will cause great trauma to the patients’ psychology (6). Therefore, good nursing is very important for hemodialysis patients with renal failure, which is not only conducive to improving the medical effect, but also to ensuring medical safety and reducing the probability of complications.
Plan, Do, Check, Act (PDCA) cycle management mode is a kind of quality management in accordance with the planning, implementation, inspection, processing order, and each cycle will raise the starting point to a new level and continue to carry out the cycle of scientific procedures (7). Since 2018, PDCA circulation nursing mode has been applied in the nursing work of patients undergoing hemodialysis due to renal failure, and satisfactory results have been achieved (8).
Materials and Methods
The patients with hemangioma who received maintenance hemodialysis treatment in the Blood Purification Center of the First People’s Hospital of Lianyungang, Lianyungang City, China from Oct 2018 to Jan 2020 were enrolled as the research subjects by the purpose sampling method. Inclusion criteria: 1) Maintenance hemodialysis with a clear diagnosis of end-stage renal disease; 2) No previous history of hemangioma; 3) Over 18 yr old; 4) Stable condition, good mental state, and the ability to successfully complete the interview; 5) Behavioral ability and willingness to participate in the study.
Exclusion criteria: 1) Having serious infectious diseases; 2) Debilitating disease of vital organs; 3) Mental disorders or disorders of consciousness do not work well with researchers; 4) Non-compliance, non-cooperation and refusal to participate in the study.
The study was conducted after obtaining the informed consent of the subjects and the approval of the Ethics Committee of the First People’s Hospital of Lianyungang.
Nursing methods
The control group: Routine management mode was used for treatment. During the treatment of patients, the whole process was supervised, the treatment indicators of patients were tested regularly, and the follow-up treatment plan was customized after the evaluation by the medical staff. PCDA group: PDCA cycle management mode was adopted for treatment, designs the patient management process and measures of hemodialysis center, and continuously improves in the follow-up practice. Conduct standardized training for all members of the management team to deepen and master the diagnosis and treatment plan, as follows:
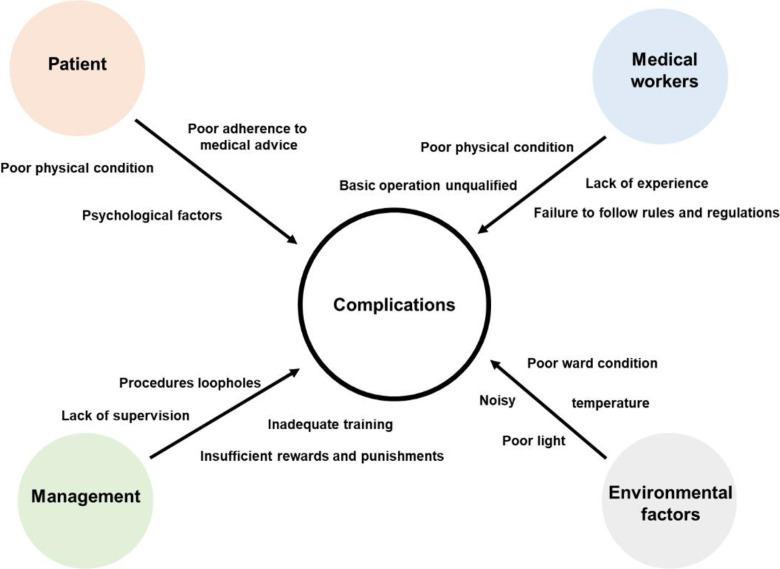
Plan (P) The PDCA circulation nursing group was established by the director of the hemodialysis center, the head nurse and the doctor in charge. After receiving the training of circulatory nursing knowledge, the nursing factors for the occurrence of complications of arteriovenous access in hemodialysis are discussed. Root cause analysis was conducted according to the multi-factor logical analysis table (Fig. 1), the multi-factor logic analysis table will discuss the detailed factors from the perspectives of patients, medical personnel, management system and environmental factors, and the proximal causes were further traced, and effective nursing countermeasures were sought on this basis.
Do (D) 1) Implementing whole-process health education. It included health education in stages before and after dialysis, during dialysis and outside the hospital, and includes patients’ family members in the scope of health education. Use network platform, health information distribution, posters and other propaganda and education methods, the content involves daily precautions, self-monitoring, patients’ self-care knowledge, reasonable exercise, control of blood pressure and blood sugar, etc. Improve the patient’s self-care level; the flow chart of maintenance of hemodialysis key contents was posted on the corridor wall of the department and the waiting area for family members to facilitate the study and viewing of patients and their families. Invite experienced senior nurses to give health education lectures once a month.
2) To strengthen the evaluation of vascular access, the nurse for the first puncture must have a professional senior nurse for diagnostic evaluation and then select a reasonable site for the puncture, and guide the needle during the needle extraction and compression.
3) Enhance training: regular mobile venous fistula puncture training, taught by relevant expert groups, situational and experiential teaching, focusing on the training of arteriovenous fistula nursing operation process, difficulties in the nursing process, fistula maintenance, health education, observation and prevention of complications, etc. The assessment standard of arteriovenous fistula care was developed, and the assessment was organized uniformly after the training.
Check (C) the group leader and the quality control nurse should supervise and inspect the clinical nursing work of the nurses regularly and irregularly through observation, operation and communication, and point out and guide the deficiencies in time. The group leader was responsible for summarizing the deficiencies and problems in nurses’ operation and health education, and the quality control nurses are responsible for grasping the implementation of nursing measures and feedback. The self-nursing ability and complications of the patients were evaluated once every 3 months to understand the feelings and opinions of the patients and their families on various nursing work, which were used as quantitative indicators for the evaluation of the nursing effect.
Act (A) The successful experience of effectively reducing hemodialysis complications was taken as the work basis to guide the nursing work, the existing nursing problems and deficiencies were summarized, the group discussed and analyzed, and the implementation plan was revised, so as to realize the continuous improvement of nursing quality.
Fig. 1:
Multi-factor logical analysis table
Observation target
Patient Satisfaction Survey: The nursing work was scored by patients, which is divided into four grades: dissatisfied (0∼2 points), general (3∼5 points), satisfied (6∼8 points) and very satisfied (9∼10 points).
Blood flow: The blood flow of patients with hemodialysis arteriovenous fistula was measured during the same period of time 3 months after intervention. Insufficiency of blood flow occurs at 200 ml/min.
Hemodialysis complications: The incidence of puncture site redness or bleeding, internal fistula obstruction, thrombosis, infection, secondary puncture and aneurysm during 3 months of hemodialysis in the two groups were counted.
Statistical treatment
SPSS (Chicago, IL, USA) 22.0 statistical software was used. Measurement data were compared by t test, and enumeration data were compared by χ2 or t test of two independent samples. a =0.05 is the test level, and P < 0.05 indicates that the data in this study is statistically significant.
Results
Overall 139 patients were randomly divided into two groups: control group (n = 58), 27 males and 31 females. PCDA group (n = 81), 39 males and 42 females. The basic information of the two groups of patients is shown in Table 1. There was no statistical difference in age and duration of dialysis treatment between the two groups. First of all, we counted the satisfaction results of patients in the two groups, and the results showed that the average score of the control group was 6.38 points, while that of the PDCA group was 7.93 points.
Table 1:
Basic information of patients
| Groups | Gender | Numbers | Age(year) | Hemodialysis time (month) |
|---|---|---|---|---|
| Control | Male | 27 | 51.62±10.29 | 41.70±15.71 |
| Female | 31 | 48.77±11.80 | ||
| PDCA | Male | 39 | 53.14±12.33 | 44.10±19.93 |
| Female | 42 | 46.83±9.57 |
In the PDCA nursing mode, patients’ satisfaction was significantly higher than that in the general nursing mode group, and more significantly (P<0.001), there were no dissatisfied patients in the PCDA group (Table 2).
Table 2:
Patient Satisfaction Statistics
| Groups | Total | Dissatisfied (0–2) | general (3–5) | satisfied (6–8) | very satisfied (9–10) | Average |
|---|---|---|---|---|---|---|
| % | % | % | % | |||
| Control | 58 | 8.62 | 20.69 | 34.58 | 22.41 | 6.38 |
| PDCA | 81 | 0.00 | 7.41 | 48.15 | 44.44 | 7.93 |
This fully demonstrated the great advantage of PCDA group in improving patients’ satisfaction. It is not only that PCDA group can improve patients’ treatment experience, but also that when conflicts occur, it can be quickly improved through PCDA mode to resolve conflicts.
We also analyzed the effect of PCDA on medical outcomes. The blood flow in the arteriovenous internal fistula is the guarantee of hemodialysis efficiency, while the blood flow in the two groups was similar, and the PCDA group did not have a negative effect on the blood flow. However, two cases of insufficient blood flow occurred in the control group, while none occurred in the PCDA group (Table 3). Most importantly, we counted the probability of complications in the two groups. As shown in Table 4, the probability of common complications in dialysis was reduced in the PCDA group, none of the hemangiomas occurred in the PCDA group.
Table 3:
Blood flow statistics
| Groups | Total | Blood flow (ml/min, x±s) | Insufficient blood flow |
|---|---|---|---|
| Control | 58 | 307.14±130.74 | 2 |
| PDCA | 81 | 322.86 ±119.52 | 0 |
Table 4:
Patient Complications Statistics
| Groups | Total | Hemangioma % | Hemangioma % | Vascular Occlusion % | Hypertension % | Electrolyte disturbance % |
|---|---|---|---|---|---|---|
| Control | 58 | 6.90 | 5.17 | 3.45 | 18.97 | 12.07 |
| PDCA | 81 | 0.00 | 1.23 | 0.00 | 2.47 | 1.23 |
Discussion
Hemodialysis has brought great convenience to the treatment of patients with end-stage renal disease (9). However, the complications during dialysis seriously affect the quality of life of patients, among which hemangioma is the most important and it is urgent to adopt scientific and standard nursing to prevent complications (10, 11). PDCA cycle, also known as Deming cycle, plays an important role in the analysis of root causes, formulation of management countermeasures, implementation of quality control and realization of quality improvement through four processes of planning, implementation, inspection and treatment (12).
The adoption of PDCA nursing mode can not only significantly improve patient satisfaction, but also our study showed that PDCA nursing mode has great benefits in reducing the risk of hemangioma and other complications in hemodialysis patients. In the PDCA model, we found through pre-planned analysis that the lack of systematic health education and low patient participation were the main reasons for hemangioma complications in hemodialysis. In order to popularize the nursing knowledge of hemodialysis to patients and their families, improve the participation of patients, we have adopted a variety of ways and staged health education, such as health brochures, corridor billboards, health lectures, etc., to create a good learning environment for patients and increase the intervention dimension and frequency of health education. This helped patients to understand relevant knowledge more easily and develop good self-care habits in daily life. At the same time, it was also helpful to encourage family members to participate in the daily care of patients and play a synergistic role.
On the other hand, the advantage of PDCA mode was that it could concentrate the strength of departments and systematically analyze the hidden problems in each link of hemodialysis. In view of the possible causes of complications, we should pool our wisdom to find the most appropriate solutions and give targeted interventions. In our actual implementation process, after PDCA group discussion, we took many effective measures, such as strengthening health education through a variety of ways to improve patients’ self-management ability. Improve the operation process, strengthen the professional training of nurses, each patient has a team member to carry out vascular assessment, multi-pronged approach, avoid the risk factors of possible complications, effectively reduce the incidence of complications. At the same time, the quality management system and the evaluation mechanism of supervision were further improved, the participation consciousness of personnel at all levels was strengthened, the division of labor was clear, each member knew their respective responsibilities, and the weak links were effectively controlled.
In the PDCA cycle, nursing staff have higher autonomy, participation right and management right through group cooperation and pooling of wisdom to formulate countermeasures, implement and review, which fully improves their enthusiasm and initiative of participation. This was conducive to the continuous discovery and solution of problems, and ultimately improve the implementation rate of nursing measures, which played a good role in preventing the occurrence of complications such as aneurysm. Meanwhile, it was also conducive to the establishment of a good atmosphere of the department, the collective learning of the department, the joint improvement of a better working process, and the formation of good cohesion.
Conclusion
PDCA nursing mode had great benefits for hemodialysis patients, it can significantly improve the quality of nursing, improve patient satisfaction, reduce complications and other risks, hence it is worth promoting.
Ethical considerations
Ethical issues (Including plagiarism, informed consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc.) have been completely observed by the authors.
Acknowledgements
No funding was received.
Footnotes
Conflicts of interest
The authors declare that there is no conflict of interest.
References
- 1.O’Connor NR, Corcoran AM. (2012). End-stage renal disease: symptom management and advance care planning. Am Fam Physician, 85(7): 705–10. [PubMed] [Google Scholar]
- 2.Zoccali C, Moissl U, Chazot C, Mallamaci F, Tripepi G, Arkossy O, Wabel P, Stuard S. (2017). Chronic Fluid Overload and Mortality in ESRD. J Am Soc Nephrol, 28(8): 2491–2497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sumida K, Kovesdy CP. (2017). Disease Trajectories Before ESRD: Implications for Clinical Management. Semin Nephrol, 37(2): 132–143. [DOI] [PubMed] [Google Scholar]
- 4.Qian Q. (2018). Acid-base alterations in ESRD and effects of hemodialysis. Semin Dial, 31(3): 226–235. [DOI] [PubMed] [Google Scholar]
- 5.Murea M, Geary RL, Davis RP, Moossavi S. (2019). Vascular access for hemodialysis: A perpetual challenge. Semin Dial, 32(6): 527–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tsuzuki T, Iwata H, Murase Y, Takahara T, Ohashi A. (2018). Renal tumors in end-stage renal disease: A comprehensive review. Int J Urol, 25(9): 780–786. [DOI] [PubMed] [Google Scholar]
- 7.Chen Y, Zheng J, Wu D, Zhang Y, Lin Y. (2020). Application of the PDCA cycle for standardized nursing management in a COVID-19 intensive care unit. Ann Palliat Med, 9(3): 1198–1205. [DOI] [PubMed] [Google Scholar]
- 8.Yang Z, Ma X, Chen Y, Cao Y, Li Q, Pan X, Wang L. (2021). Effects of a Quality Improvement Program to Reduce Central Venous Catheter-Related Infections in Hemodialysis Patients. Am J Med Sci, 361(4): 461–468. [DOI] [PubMed] [Google Scholar]
- 9.Liew A. (2018). Perspectives in renal replacement therapy: Haemodialysis. Nephrology (Carlton), 23 Suppl 4: 95–99. [DOI] [PubMed] [Google Scholar]
- 10.Masud A, Costanzo EJ, Zuckerman R, Asif A. (2018). The Complications of Vascular Access in Hemodialysis. Semin Thromb Hemost, 44(1): 57–59. [DOI] [PubMed] [Google Scholar]
- 11.Florescu MC, Qiu F, Plumb TJ, Fillaus JA. (2014). Endovascular treatment of arteriovenous graft pseudoaneurysms, indications, complications, and outcomes: a systematic review. Hemodial Int, 18(4): 785–92. [DOI] [PubMed] [Google Scholar]
- 12.Fukui T. (2012) [Patient safety and quality of medical care. Editorial: From evidence-based medicine to PDCA cycle]. Nihon Naika Gakkai Zasshi, 101(12): 3365–7. [DOI] [PubMed] [Google Scholar]