Abstract
Background
Special health care needs (SHCNs) individuals experience higher levels of dental problems including accessing oral health (OH) facilities. Improving standard of OH care in SHCNs requires identifying barriers and enablers. The aim of this study was to perform a systematic review of prior researches to identify OH care barriers and enablers for SHCN individuals.
Methods
Electronic searching was conducted systematically in PubMed and Cochrane databases. The PICOS parameters were formulated for the inclusion of studies, and the PRISMA method was used to select the articles. Two reviewers independently screened the articles for eligibility and to minimise the risk of bias in the studies and also searched the contents of key articles, quality of methodology, outcomes and reference lists of all the studies included.
Results
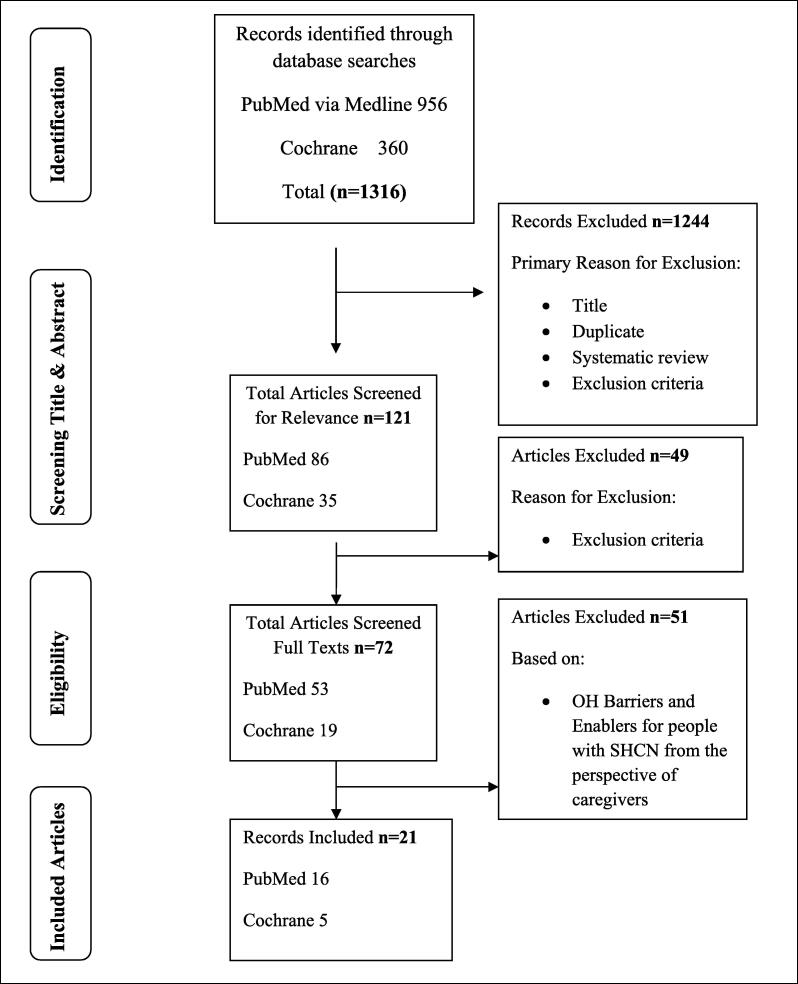
A total of 1316 (PubMed 956, Cochrane 360) studies were found initially and after title and abstract screening and also removal of duplication, reviewers selected 53 papers from PubMED and 19 articles from Cochrane to go through full articles and led to the final confirmation of 21 studies. Common challenges included lack of OH knowledge and awareness, difficulty in accessing treatment, transportation problem, treatment cost, and lack of inter-professional collaboration for specialized services. Potential solutions included OHE training and services for patients and caregivers, easy access to dental services, specialized dental practitioners and use of a combination of expertise to meet the demands of SHCN individuals.
Conclusion
This brief analysis will establish dental obstacles to the provision of information to policymakers for SHCN population at organizational, individuals and policy levels. It will help in effective planning for providing and improving OH care quality in caregivers.
Keywords: Barriers, Enablers, Oral health education, People with special health care needs, Systematic review, Caregiver
1. Introduction
1.1. Background of the study
Dental care is medically necessary for the purpose of preventing and eliminating orofacial diseases, infection and pain, restoring the structure and function of the dentition, and correcting the facial disfiguration or dysfunction (American Academy of Pediatric Dentistry, 2015). However, oral well-being is one of the most neglected areas of treatment in patients with special health care needs (SHCN), as it is very difficult to maintain optimum oral health in people with disabilities (PWDs) (Waldman et al., 2009, Niazi et al., 2016) especially in children with special health care needs (CSHCN). Most of the times substantial dental complications in CSHCN turn into anxiety and cooperation problem, mainly because of their physical limitations, mental disabilities, or behavioral management problems (Pecci-Lloret et al., 2021). For the dental practitioners, sometimes these factors may cause conventional dental examination and treatment more challenging and may undergo general anesthesia (GA) to overcome with less difficulty and higher quality (Blumer et al., 2019). Consequences of poor oral health go beyond immediate physical impacts to severe social integration and quality of life associated with bad odour, changed dental aesthetics, or altered speech that has negative impact on self-image and self-esteem of PWDs (Fiske et al., 2000, Naseem et al., 2016, Hoben et al., 2017).
Unfortunately, individuals with SHCN (or PWDs) particularly CSHCN suffer in extreme due to have different types of medications and special diets, and oral motor habits such as atypical swallowing, sucking lips, or tongue interposition that may cause dental complications (Huang et al., 2020). In case of the older adults, are less likely to obtain regular dental care, despite having a greater need for dental services (Bots‐Vant Spijker et al., 2014) and physical access to dentistry decreases to the PWDs as they become more dependent and less mobile. Impaired oral health paired with poor access to dental care contributes to an undue disease burden and can lead to adverse oral health effects. Furthermore, special diets, various types of medicines, and motor habits related to oral cavity such as atypical swallowing, lip sucking/ biting, or interposition of tongue, may cause development of several oral complications in PWDs, especially in children with SHCN (Ocanto et al. 2020).
However, studies have shown that oral health education (OHE) improves attitudes and knowledge related to oral health (OH), particularly among caregivers of patients with SHCN (Khanagar et al., 2014). Therefore, proper guidance, early diagnosis and the prevention and treatment of oral diseases leads to the provision of primary OH care (World Health Organisation, 2012).
1.2. Rationale of the study
Poor oral health (OH) may have a significant effect on overall health. Excessive microbial accumulation in the oral cavity due to inadequate oral hygiene (OH) can lead to increased vulnerabilities to infections of the respiratory tract, such as aspiration pneumonia and arteriosclerosis (El-Rabbany et al., 2015, Sjögren et al., 2008, Desvarieux et al., 2003). Lower chewing output due to inadequately retained teeth and/or tooth prostheses can result in weight loss and, eventually, malnutrition (Saarela et al., 2014). Moreover, discomfort is usually associated with a poorer quality of life as well as impaired dental aesthetics (Porter et al., 2015).
Generally good OH is dependent on adequate oral hygiene and regular access to dentistry (dental clinic or hospital) (Crocombe et al., 2012). Individuals with disabilities, however, have a reduced capacity to perform oral hygiene, being particularly weighed down by the physical or psychological challenges they face (Chalmers et al., 2003, Warren et al., 1997). Consequently, this special group of people relies on caregivers to facilitate oral care, however, in most circumstances, such support networks have not been found to secure high-quality and systemic oral hygiene (Hoben et al., 2017, Weening-Verbree et al., 2013, Forsell et al., 2009). Alternatively, one of the dominant barriers in provision of OH care is challenging faced by caregivers, especially those who experience cooperation problem (Wardh et al., 2012).
Most of the PWDs have not been routinely studied and treated by dental professionals; indeed, oral/dental therapy in the most cases is only available in emergencies and consists of low levels of treatment (Göstemeyer et al., 2019). The provision of evidence-based OH instructions to those with disabilities does not seem to have a sustainable effect on this situation (Godin et al., 2008, Delwel et al., 2018, Hearn and Slack-Smith, 2015). Understanding these obstacles, as well as recognising OH facilitators, will help in establishing programs designed to enhance the OH of people with SHCN by ensuring their appropriate treatment.
1.3. Research questions
The main goal of this systemic review was to identify and analyse the factors (i.e. obstacles and facilitators) associated with OHE, care and services to people with SHCN at individual, systemic (inter-professional integration between dental service providers and caregivers), organisational and policy levels at any interval, with or without a control group. There were many published works that only focused on barriers, whereas facilitators, interventions and follow-up are important issues as well. Since the OHE is provided by multiple stakeholders with different motives, we strive to evaluate these challenges and facilitators from the perspectives of diverse stakeholders, also parents or caregivers has a significant relation to the OH of PWDs as well.
This review allowed us to explore and mark the very recent studies from 2011 to 2020 that provides an assessment of the factors related to the provision of OH care to the PWDs, across all age groups, and it is our moral duty to do so. Identifying these obstacles will not only enable us to provide OH promotion and dental treatment. It will also make possible to break the blockades of different issues which are faced by individuals with SHCN, leading to a standard and comfortable life for PWDs in the future.
2. Materials and methods
2.1. Registration of the protocol and PRISMA guidelines
This systemic review protocol has been registered in the PROSPERO International prospective register of systematic reviews (No. CRD42021275458). It publishes protocols from the systematic reviews prior to the commencement of data extraction for reducing reporting bias (Schiavo, 2019). The reporting of this research followed the guidance of the PRISMA (Tong et al., 2012, Welch et al., 2012).
2.2. Eligibility criteria
This review included all types of published English language research that assessed the obstacles to –and the enabling of – the provision of OHE and services by caregivers and parents to SHCN individuals, with the exception of ‘grey literature’ such as non-peer-reviewed articles, conference papers, working papers, evolutions, textbooks, reports and theses (Table 1).
Table 1.
Inclusion and exclusion criteria.
| Inclusion criteria | Exclusion criteria |
|---|---|
| i) This study limited the search to empirical studies (qualitative, quantitative and mixed methods). Qualitative studies included interviews, focus groups or surveys, and quantitative studies focused on clinical trials, cross-sectional studies, randomised controlled trials, non-randomised trials with or without control groups, cohort or case control studies and surveys. | i) Non-empirical works, systematic reviews, textbooks and theses were excluded from the study. |
| ii) Only primary data from the articles were included. | ii) People who affected by mental health disorders were not included. Also, people with SHCN who remain at home within a supportive living environment were excluded. |
| iii) This study focused on individuals with different types of disabilities such as physical, developmental, intellectual, autism spectrum disorder (ASD), hearing impaired and others. | iii) Individuals with visual impairment were excluded as well, as conventional teaching methods such as visual aids and disclosing agents are not useful for them to maintain oral hygiene. Alternative teaching aids such as an OHE booklet in Braille and audio narration of the booklet need to be used to educate them. |
| iv) Articles written in the English language from 1st January 2011 to 31st December 2020 have been included. | iv) Papers written in the languages other than English were excluded, as we did not have access to them, and studies published before 2011 were excluded as well. |
| v) Hospital-based studies were excluded. |
Two authors of the current review formulated the following the PICOS parameters for the inclusion of studies:
2.2.1. Population
Any caregiver from nursing homes, care homes, rehabilitation centres or organisations involved in the delivery of oral or dental services to the handicapped was included. Parents or guardians of people with SHCN – as well as children, adolescents, adults and the elderly with physical and intellectual disabilities or hearing impaired – were also included.
2.2.2. Intervention
Any intervention with or without a control group was needed for the studies on oral hygiene or oral/dental treatment for the SHCN population.
2.2.3. Control
Monitor None (this analysis was not a comparative efficacy study, therefore, there was no need of a control group or comparator in the studies).
2.2.4. Outcomes
Qualitative and quantitative evidence on influences (e.g. behaviours, expertise, values of OH care practitioners or other factors affecting behaviour) that function as obstacles (i.e. obstacle to oral health care providers) or facilitators (i.e. oral health care provision factors) for the provision of oral/dental care to PWDs.
2.2.5. Setting
Any normal setting where oral/dental health care (e.g. care homes, rehabilitation centres and nursing home care) were provided.
2.3. Information sources
Electronic searches: We searched for studies reported from 1st January 2011 to 31st December 2020 (PubMed via Medline and Cochrane databases), as it was good to use sources published in the past 10 years to identify research (Table 2) that is more current and reflective of very recent information (to minimise publication bias). Moreover, sources which are used for research in the health sciences fields (e.g. medical, dentistry, and nursing) change quickly, as we know, with the accession of new knowledge and the necessity to transfer it rapidly to practitioners in this field.
Table 2.
Publications distribution (by year).
| Year | Total Articles, PubMed search (n = 956) | Total Articles, Cochrane search (n = 360) |
|---|---|---|
| 2011 | 55 | – |
| 2012 | 61 | – |
| 2013 | 83 | – |
| 2014 | 123 | – |
| 2015 | 128 | – |
| 2016 | 112 | – |
| 2017 | 118 | 28 |
| 2018 | 116 | 33 |
| 2019 | 150 | 52 |
| 2020 | 70 | 54 |
2.4. Keywords search strategy
Two authors experienced in database searching developed the search strategy. The search terms for search domains were consolidated using pronged search technique based on the Boolean operators “AND” and “OR” in conjunction with different Medical subject terms. Each search record was documented as date of search, database, keywords, number of studies included and number of eligible studies. The strategy of searching was as responsive as we expected, given some poor indexing (i.e. those with disabilities are often referred to using numerous terms such as vulnerable, physically disadvantaged or handicapped). The following strategy was developed for PubMed: (((((((disable) OR special health care needs) OR physically disadvantage) OR handicapped) OR vulnerable) OR nursing home residents)))))) AND (oral health education) AND ((((rehabilitation centre) OR nursing home) OR care home) OR long term care facilities)))) AND (((((oral hygiene) OR oral health) OR dental care) OR oral care) OR mouth care))))) AND ((caregivers) OR care providers)) AND (parents) AND (knowledge attitude practice))))))).
During Cochrane database searching, trials matched ((((((disable) OR special needs) OR physically disadvantage) OR handicapped) OR vulnerable) OR nursing home residents) AND (oral health education) AND (knowledge attitude practice)))))) in Title Abstract Keyword - with a Cochrane Library publication date between January 2011 and December 2020, in Cochrane Protocols, Trials, Clinical Answers, Special Collections with 'Oral Health' in Cochrane Group.
3. Results
3.1. Search results of the studies
A total of 1,316 publications (956 from PubMed, 360 from Cochrane) were identified (Fig. 1) through advanced searches (additional filter and search limit) with different titles. The researchers only referred to the most relevant publications related to the topic and fit the scope of this study between the periods of 1st January 2011 to 31st December 2020. According to the PRISMA framework, the study followed four steps (identification, screening title and abstract, eligibility and included articles) in the article selection process (Fig. 1).
Fig. 1.
Flow of the literature search and review (modified PRISMA Diagram).
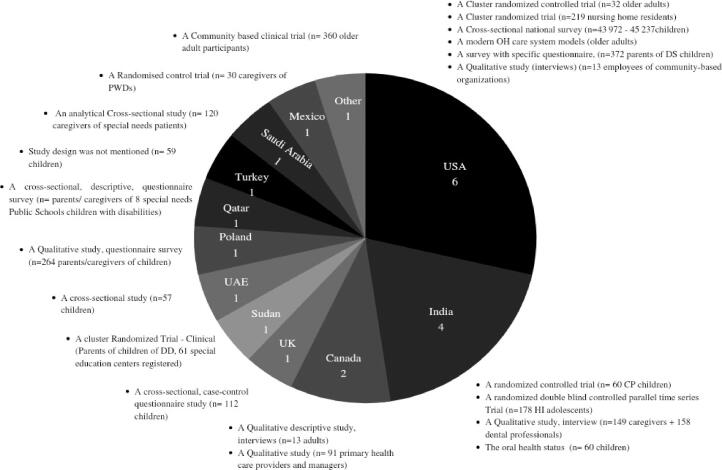
After screening of titles, removal of duplicate studies, systemic reviews and based on exclusion criteria, 86 papers were selected from PubMed and 35 articles from the Cochrane database. Two reviewers individually screened the titles and abstracts of all the selected articles to include, and also decided which articles needed to be excluded and full text screening. From these, 53 studies from PubMed and 19 studies from Cochrane were selected by the reviewers after independently assessing the quality of methodology and results of the studies (to minimise the risk of bias). The lists of studies were then compared by the reviewers, and disagreements were sorted out through detailed discussion for each study. Ultimately, this led to the inclusion of 21 articles based on OH barriers and enablers for people with SHCN from the perspective of caregivers– 16 from PubMed (13 from the initial search and 3 from the revised search) and 5 from Cochrane (Fig. 1) – consisting of 5 randomised control trials, 5 cross-sectional studies, 2 clinical trials, 6 qualitative studies, 1 quantitative study and 2 others (Fig. 2).
Fig. 2.
Info-graphic chart of countries and study design.
The authors’ affiliations with various countries were included; articles appeared in peer-reviewed journals and spanned at least 11 countries (country name not found for 1 article which was a community based clinical trial). Fig. 2 shows that USA tops the list with 6 papers (2 cluster randomises trials, 1 cross-sectional survey, 1 modern OH care system model, 1 qualitative study and 1 survey) out of the selected 21, followed by India 4 papers (2 randomised controlled trials, 1 qualitative and 1 quantitative), Canada 2 (both were qualitative studies); UK, United Arab Emirates, Qatar and Saudi Arabia with 1 paper each (all were cross-sectional studies); 4 documents were published from Sudan, Poland, and Mexico with different study designs (cluster randomised trial, qualitative study and randomised control trial, respectively); only 1 paper from Turkey where study design was not mentioned (Fig. 2).
3.2. Quality appraisal
Two reviewers separately evaluated the study design quality through using three validated checklists whether included studies were appropriate or not.
Clinical studies with or without a control group and with or without randomized allotment of study participants—Quality Assessment Tool for Quantitative Studies (QATQS) (Thomas et al., 2004). The QATQS is a reliable and valid apparatus which evaluates the studies whether there is selection bias, study design, confounding factors, methods of data collection, blinding, withdrawals and dropouts, intervention integrity, and analyses (Thomas et al., 2004, Armijo-Olivo et al., 2012).
Cross-sectional studies- Estabrooks’ Quality Assessment and Validity Tool for Cross-Sectional Studies which was prepared based on the guidelines of Cochrane (Clarke et al., 2001) and other evidence-based scale (Kmet et al., 2004). Reviewers evaluate methodological quality of the studies through sampling category, measurements used, and statistical data analysis.
Qualitative studies- Critical Appraisal Skills Program (CASP, 2013) is the Qualitative Research Checklist that assesses whether (a) research aims are clearly stated; (b) qualitative method, study design, strategy of recruitment, and data collection procedures are appropriate; (c) relationships between the researchers and participants are appropriately considered; (d) ethical issues are sufficiently mentioned; (e) data analyses are adequately rigorous; (f) findings are clearly addressed; and (g) research is valuable in general.
Each included study was rated on the overall quality; using a rating method evolved by de Vet et al. (1997) and scored with a feasible range of 0–1 and the studies were ranked as weak (≤0.50), low moderate (0.51–0.66), high moderate (0.67–0.79), or strong (≥0.80).
The barriers to and enablers for OH services identified in the literatures from different special needs groups within different region sand disability classes, are presented in Table 3, along with authors, study designs, ages and the quality of studies.
3.3. Internal barriers and enablers
Among the included studies, one of the most frequently cited barriers to oral treatment was ‘lack of personal oral care knowledge and attitude of caregivers’ (Alyafei et al., 2020 Shah et al., 2018, Gonzalez et al., 2013, Sara Amir Hassan and ElTyeb, 2017). In this case, OHE training programs and practical strategies were enablers to improving the knowledge of OH workers or care providers, the effectiveness of which was assessed in robust studies.
‘Lack of awareness on oral treatment facilities and oral disease prevention by’ (Cruz et al., 2016, Gerreth and Borysewicz-Lewicka, 2016) and lack of skilled and educated care providers (Harnagea et al., 2018) were also identified as two of the most frequent impediments to the provision of OH care. Training and education concerning OH services, as well as increasing awareness among parents and caregivers, were found to be potential enablers in combating patient reluctance towards routine dental check-ups.
A second main barrier was found in how ‘oral health was a low priority and poorly organised process and policies by policy makers’ (Harnagea et al., 2018, Cruz et al., 2016). Supportive government policies and proper OHE programs with satisfactory budget distributions and fundraising were the facilitators for this issue.
Another important, barrier-creating issue noted in the studies was the very uncooperative nature and behavioural problems of PWDs, especially CWDs (Alkhabuli et al., 2019, Alyafei et al., 2020, Barry et al., 2014, Weintraub et al., 2018). Relentless motivation and counselling therapy were noted to produce effective outcomes.
Less staff availability, combined with heavy workloads, and limited time for the residents inside centres (Sahana et al., 2013, Weintraub et al., 2018) was another hurdle, and collaborating with individuals across many disciplines, along with comprehensive preparation, was mentioned by one author (Sahana and Shivakumar, 2013) as an enabler.
3.4. External barriers and enablers
As regards external barriers, financial hardship was in the topmost position (Alyafei et al., 2020, Gerreth and Borysewicz-Lewicka, 2016, Duker et al., 2020). This systematic review found the funding of oral services to be one of the biggest hurdles for parents in securing treatment for their CWDs, and the same obstacle regarding low income (Schensu et al., 2019) was noticed in the case of adult PWDs as well. More specifically, poor OH conditions and the potentially high cost of dental treatments could further compromise the already vulnerable status of PWDs. The solution lay with more public financing for dental/oral services and seeking more efficient ways to improve dental facilities for people with SHCN.
The other most common external problems noted in the studies (Gerreth and Borysewicz-Lewicka, 2016, Rashid-Kandvani et al., 2015, Duker et al., 2020, Helgeson and Glassman, 2013, Vpk et al., 2020) were geographic location of dental care facilities, transportation problems for PWDs in accessing clinics and the lack of expert dentists who could treat CWDs, including PWDs. Community disagreement regarding fluoride therapy (Cruz et al., 2016), racial/ethnic differences (Guarnizo-Herreño and Wehby, 2012), interacting with dental workers and dental chair pain with anxiety experienced by people with SHCN (Rashid-Kandvani et al., 2015) were also found as obstacles in the provision of OH care for the SHCN population. These issues should be addressed through inter-professional collaboration using innovative models and partnerships with community-based groups and early identification agencies or organisations that provide comprehensive treatment and coordination with caregivers or parents as well, since they were assumed to have the primary decision-making role for people with SHCN.
There were few special groups who required special facilities according to their needs, such as children with hearing impairment (HI) (Hashmi et al., 2019) and cerebral palsy (CP) (Vpk et al., 2020). Sign language training could be an enabler for dental professionals and care providers, helping them to communicate with those with HI and to understand their problems and provide appropriate treatments. Again, for patients with CP, the video-based OHE has been found to be effective in improving the parents’ or caregivers’ knowledge and, in turn, their child’s oral health (Vpk et al., 2020).
4. Discussion
This systematic review has drawn a complete picture and marked many factors serving as fences and facilitators in providing better OH care and dental treatment for different groups of children, adults and the elderly with disabilities as perceived by care providers. Individuals from disabled groups in different regions are exposed to various oral complications and difficulties in getting oral health care. Furthermore, there are many common barriers faced by almost all PWDs along with specific barriers existing in each group. The main finding of the present study was the number of high quality study- there was no study.
Also, to our knowledge, it is the only study that incorporated the studies not only from Western and European countries, but also from all the seven continents (Asia, Europe, North America, South America, Antarctica and Africa) in order to obtain a better idea of OH care factors related to SHCN populations in different regions of the world (study from Australia was not included, as no relevant article could be found). We also attempted to draw a complete picture as to where the gaps were in the field of oral treatment and what the possible solutions should be. This brief analysis established dental obstacles to the provision of information to policy makers, stakeholders and dental practitioners for people with SHCN at policy, organizational and individual levels.
This review also highlighted a few of the shortcomings in the available researches, given, for example, the absence of effective studies, unsuitable study designs, small sample sizes, insufficient interventions and avoidance of follow-up. While several intervention studies did possess good qualities (high moderate) where methodological qualities were good enough and dominant barriers and enablers were explained well, there were also a few studies (weak) in which those were unclear. Furthermore, in few studies there were no specific intervention noted, or there were individually tailored interventions which were not effective for actual standards of oral health. Moreover, interventions were used to improve OH knowledge, not for oral health. Another salient factor –long-term follow-up – was highlighted in only one study (Akgün et al., 2019), even though it is a necessary component of sound OH maintenance.
The lack of awareness of caregivers/parents to disclose dental care issues with PWDs and the knowledge, attitude and practices of caregivers were found to be the key obstacles to proper intervention (Alkhabuli et al., 2019, Lamba et al., 2015), followed by transportation for people with special needs to access the clinics (Barry et al., 2014), the cost of treatment and dental care, limited agency resources, restrictive administrative- and system-level policies, low parental demand, community disagreement regarding fluoridation, the perceived lack of dentists who could treat children with disabilities, racial/ethnic differences, suboptimal skills, challenges in implementation, dental clinic location and institutionalising and co-occurring defects. Apart from these issues, lack of coordination of dental care with other social or community services is another recurring barrier. It is evident from our review that lack of integration between dentistry and community services exist globally.
Meanwhile, a coordinated organisational response to develop collaboration between dental and disability services and training for caregivers and PWDs, as well as OHE plus training programs, need to be given high priority by policy makers in order to enhance the OH knowledge, attitudes and practices of parents/caregivers. Not only are proper preparation and dental health campaigns effective in increasing understanding and knowledge, these programs and strategies can also improve the capabilities and skills of OH professionals in the treatment of oral disease. By increasing their knowledge about OH, caregivers can motivate those with disabilities to pursue their own dental care when they are able to do that independently. Without such remediation, more dental diseases in children with disabilities (CWDs), as well as in adults and the elderly with SHCN, could be generated each year, making our path to maintaining the provision of proper oral care to these individuals more difficult.
Therefore, higher authorities in government, policy makers and dental clinic authorities must provide appropriate opportunities for PWDs to visit dental clinics without difficulty and to receive affordable treatment, as regular and long-term follow-up contributes to prevention efforts and health care provision for most children, as well as adults and older individuals, with disabilities.
In terms of OH literacy at the individual level, care providers can motivate or encourage people with SHCN to engage in oral care on their own. Although individuals with special needs lack confidence in working independently, positive reinforcement, customised face-to-face counselling based on individual needs, interactive group education, the development of strategic plans or a combination of strategies may improve their self-sufficiency. It is important to note that in order to motivate people with SHCN, care providers should themselves be motivated. Therefore, guiding and training caregivers in how to motivate and encourage this special population group, avoiding the risk of bias, are strongly recommended.
One of the most frequent barriers found from the included studies was behavioural issues. In the case of behavioural problems, two core strategies that were not used or analysed in most of the studies. First, was the motivational technique in the context of long-lasting care, by which caregivers could motivate the CWDs, including PWDs, to perform their daily oral hygiene routines on their own. Furthermore, it was found to be important for the dentist and caregivers to know the child’s level of understanding, and that a friendly communication manner should thus be practiced (American Academy of Paediatric Dentistry, 2012). Unfortunately, a limitation found in all of the studies (Alkhabuli et al., 2019, Alyafei et al., 2020), except one (Weintraub et al., 2018), was the failure to consider management of behaviour. Second, was management of providing dental treatment. As active or passive behavioral management (cognitive, motor, and sensory factors) techniques in CSHCN patients, diagnosis and treatments under general anesthesia (GA) can be the best option for dental practitioners (Blumer et al., 2019). Moreover, found from a very recent study (Pecci-Lloret et al., 2021), dental prevention measures and treatments under general anesthesia is safe and useful technique for CSHCN with minimal postoperative complications and also suitable for all patients with no age limit, with a recognized disability. Parents, caregivers and dental professionals should work together for OH care maintenance that has behavioural issues. Consequently, GA should be included and standardized among dental public programs in order to secure the safe delivery of dental treatment (Pecci-Lloret et al., 2021).
The implementation of technology to address OH-related issues can open up a new landscape for future research. A modern technology-based study conducted in the USA (Helgeson and Glassman, 2013) designed a new OH care system model for older adults and PWDs in order to solve the access problem presented by traditional dental clinics. Accordingly, this sort of new model can be designed for specific community organisations where underserved and/or high-risk groups of people stay, work and obtain health care or social services. Also, when conventional methods are not working properly, technology can be more effective in fulfilling these individuals’ needs and in offering a better form of health care delivery.
Of note, several flaws were identified in the included articles, such as the lack of coordination between dental care and other social or community services, and it was evident from our review that this disconnect is a global problem. Separately, it was also noticeable that some PWDs faced accumulative challenges since they belong to multiple groups with different language, educational, cultural and ethnic barriers – for instance, a person with a disability living in a rural area belonging to a minority group or ethnic group. Furthermore, a noteworthy limitation was observed in the studies (Schensu et al., 2019, Harnagea et al., 2018, Hartshorn et al., 2021) on the elderly with SHCN, specifically a lack of information on specific health issues (e.g. Alzheimer’s disease or dementia). In the case of elderly PWDs (with dementia), regular and continuous follow-up, combined with an additional awareness of care staff members regarding oral hygiene maintenance, is needed, since studies found that having Alzheimer’s disease or dementia is significantly related to worse oral hygiene (Weintraub et al., 2018, Kusdhany et al., 2015, Saito et al., 2018).
PWDs of all ages deserve much support and effort on their behalf in order to increase the benefits they receive from caregivers and policy makers alike. It is essential to have a structured clear OHE strategy and budgets by policymakers. Also needs counselling at the individual level, relentless motivation and follow-up are essential to having good OH, which is connected to the needs and expectations of PWDs.
Key strength of this analysis is the rapid review method with a comprehensive search process, which gives both a quick picture and an in-depth analysis of the current obstacles to – and enablers of – OH services for the SHCN population to inform caregivers, policy makers and service providers.
5. Limitations of the study
This systematic review was limited to publications in English due to a lack of expertise in other international languages. Also excluded were grey literature, book chapters, case reports, systematic reviews, theses and articles published prior to 2011. It was further limited by excluding people with mental health disorders or visual impairment.
There were three main limitations of this study. First was, not to discuss findings based on the specific disability group. Here in the present study, various groups of individuals with SHCN are included who may faced different types of hurdles and the facilitators could be different types as well. Second, this study also did not separate different age groups (children, adult and elderly) whose oral complications specifically dental caries should be managed differently especially in CSHCN who are again considered as three groups such as under 6 years old (deciduous dentition), 6–14 years of age (mixed dentition) and above 14 years (permanent dentition). Third, few studies were included in this systemic review which were comprised of cluster-randomised trials (Weintraub et al., 2018, Hartshorn et al., 2021, Sara Amir Hassan and ElTyeb, 2017), where the participants from different groups might not be treated differently. Therefore, those studies might be biased, and there might have been an influence on the outcomes.
The studies included in this review were small in number and their methodological quality was limited, these were the primary limitations of the present study. Moreover, the reviewers did not strive to communicate with the authors of the studies to acquire ambiguous study particulars. Consequently, undeclared details of methodology may have dropped the quality assessment scores of the included studies.
Reviewers conducted searches of two comprehensive databases only and included articles through applying meticulous methods as well as identified by the hand search when the titles met our inclusion criteria only. However, we did not search grey literatures in databases and, as a consequence, may have missed pertinent works. Notwithstanding these limitations, this review reports on the wide range of OH care-related problems and contributing factors among people with SHCN.
6. Conclusions
Findings of the present systemic review reflect a critical gap in the literature which can be considered from 2 directions. First, research on factors to oral care for people with SHCN have been presented at specific region and disability classes with remarkable similarities between these groups. Even though quite a few solutions that tackle these barriers were recognised in the selected studies, yet there was not enough data to support their efficacy or cost efficiency of such solution.
Second, within the OH field, disability has been considered a negative OH outcome rather than a population with ongoing OH care needs. Support from care providers and dental professionals are needed in order to specifically tailor the strategy especially intervention for improving oral care for PWDs. However, any strategies that are robustly assessed should be practical; otherwise, caregivers will continue to struggle with providing accurate oral care and ensuring the OH of special needs populations.
Overall quality of the included studies was low moderate to high moderate and distinctly highlights the necessity for more effective as well as rigorous researches on fences and enablers, as recognized by caregivers, in providing oral care to PWDs. Higher standards and effective studies are recommended to reduce major issues without severe effects on general health and quality of life of the PWDs, as well as to the health care system. Future studies should be required meticulously designed interventions to focus on the hurdles to OH care of the specific age groups with specific disabled groups by care providers. Those interventions should be piloted, trialed or experimented and amended (if necessary) in particularly designed randomized trials, followed by the guidance of the Dental Research Council.
CRediT authorship contribution statement
Afsary Jahan Khan, Budi Aslinie Md Sabri, Mas Suryalis Ahmad: Conceptualization, Data curation, Funding acquisition, Project administration, Supervision, Manuscript reviewing & editing.
Funding
This study was supported by the grant 600-UiTMSEL (PI. 5/4) (030/2020).
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
We would like to thank all the authors for working together. We also want to extend our gratitude to the good souls who supported with literature search technique, reviewed the manuscript and also provided suggestions throughout the study for improving it.
Footnotes
Peer review under responsibility of King Saud University. Production and hosting by Elsevier.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.sdentj.2022.08.008.
Contributor Information
Afsary Jahan Khan, Email: 2020291188@isiswa.uitm.edu.my.
Budi Aslinie Md Sabri, Email: budiaslinie@uitm.edu.my.
Mas Suryalis Ahmad, Email: drsuryalis@uitm.edu.my.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- Akgün E.O., Volkan Çiftçi D.D., Dogan M.C. Oral health status and dental treatment for children with learning disabilities in southern Turkey. J. Disabil. Oral Health. 2019;20(2):73–81. [Google Scholar]
- Alkhabuli J.O., Essa E.Z., Al-Zuhair A.M., Jaber A.A. Oral Health Status and Treatment Needs for Children with Special Needs: A Cross-Sectional Study. Pesqui. Bras. Odontopediatria Clín. Integr. 2019;19 doi: 10.4034/PBOCI.2019.191.127. [DOI] [Google Scholar]
- Alyafei N.A., Jaleel B.N.F., Mathew T. Exploring the Barriers to Oral Health Care Perceived by Parents/Caregivers of Children with Disabilities in Qatar. Dentistry. 2020;10:559. doi: 10.35248/2161-1122.20.10.559. [DOI] [Google Scholar]
- American Academy of Pediatric Dentistry (2012). Council on Clinical Affairs. Guideline on Management of Dental Patients with Special Health Care Needs. Clin. Pract. Guidelines. 34(5), 160–65. [PubMed]
- American Academy of Pediatric Dentistry (2015). Policy on medically necessary care. Pediatr Dent. 37 (special issue),18–22.
- Armijo-Olivo S., Stiles C.R., Hagen N.A., Biondo P.D., Cummings G.G. Assessment of study quality for systematic reviews: a comparison of the Cochrane Collaboration Risk of Bias Tool and the Effective Public Health Practice Project Quality Assessment Tool: methodological research. J. Eval. Clin. Pract. 2012;18:12–18. doi: 10.1111/j.1365-2753.2010.01516.x. [DOI] [PubMed] [Google Scholar]
- Barry S., O’Sullivan E.A., Toumba K.J. Barriers to dental care for children with autism spectrum disorder. Eur. Arch. Pediatr. Dent. 2014;15(2):127–134. doi: 10.1007/s40368-013-0075-y. [DOI] [PubMed] [Google Scholar]
- Blumer S., Costa L., Peretz B. Success of Dental Treatments under Behavior Management, Sedation and General Anesthesia. J. Clin. Pediatr. Dent. 2019;43:413–416. doi: 10.17796/1053-4625-43.6.9. [DOI] [PubMed] [Google Scholar]
- Bots-VantSpijker P.C., Vanobbergen J.N., Schols J.M., Schaub R.M., Bots C.P., de Baat C. Barriers of delivering oral health care to older people experienced by dentists: a systematic literature review. Community Dent. Oral Epidemiol. 2014;42(2):113–121. doi: 10.1111/cdoe.12068. [DOI] [PubMed] [Google Scholar]
- Chalmers J.M., Carter K.D., Spencer A.J. Oral diseases and conditions in community-living older adults with and without dementia. Spec. Care Dentist. 2003;23(1):7–17. doi: 10.1111/j.1754-4505.2003.tb00283.x. [DOI] [PubMed] [Google Scholar]
- Critical Appraisal Skills Programme (CASP) (2013). CASP Qualitative Research Checklist: 10 Questions to Help You Make Sense of Qualitative Research. http://www.casp-uk.net/#!casp-tools-checklists/c18f8 (last access 20th March, 2022).
- Clarke M, Oxman A. D. The Cochrane Library; Oxford: 2001. Cochrane reviewer’s handbook 4.1.4. [Google Scholar]
- Crocombe L.A., Broadbent J.M., Thomson W.M., Brennan D.S., Poulton R. Impact of dental visiting trajectory patterns on clinical oral health and oral health-related quality of life. J. Public Health Dent. 2012;72(1):36–44. doi: 10.1111/j.1752-7325.2011.00281.x. [DOI] [PubMed] [Google Scholar]
- Cruz S., Chi D.L., Huebner C.E. Oral health services within community-based organizations for young children with special health care needs. Spec. Care Dentist. 2016;36(5):243–253. doi: 10.1111/scd.12174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Vet H.C.W., de Bie R.A., van der Heijden G.J.M.G., Verhagen A.P., Sijpkes P., Knipschild P.G. Systematic reviews on the basis of methodological criteria. Physiotherapy. 1997;83:284–289. [Google Scholar]
- Delwel S., Binnekade T.T., Perez R.S., Hertogh C.M., Scherder E.J., Lobbezoo F. Oral hygiene and oral health in older people with dementia: a comprehensive review with focus on oral soft tissues. Clin. Oral Investig. 2018;22(1):93–108. doi: 10.1007/s00784-017-2264-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desvarieux M., Demmer R.T., Rundek T., Boden-Albala B., Jacobs D.R., Jr., Papapanou P.N., Sacco R.L. Relationship between periodontal disease, tooth loss, and carotid artery plaque: the Oral Infections and Vascular Disease Epidemiology Study (INVEST) Stroke. 2003;34(9):2120–2125. doi: 10.1161/01.STR.0000085086.50957.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duker L.I.S., Richter M., Lane J.C., Polido J.C., Sharon A., Cermak S.A. Oral Care Experiences and Challenges for Children with Down Syndrome: Reports From Caregivers. Pediatr. Dentist. 2020;42(6):430–435. [PMC free article] [PubMed] [Google Scholar]
- El-Rabbany M., Zaghlol N., Bhandari M., Azarpazhooh A. Prophylactic oral health procedures to prevent hospital-acquired and ventilator-associated pneumonia: a systematic review. Int. J. Nurs. Stud. 2015;52(1):452–464. doi: 10.1016/j.ijnurstu.2014.07.010. [DOI] [PubMed] [Google Scholar]
- Fiske J., Griffiths J., Jamieson R., Manger D. Guidelines for oral health care for long-stay patients and residents. Gerodontology. 2000;17(1):55–64. doi: 10.1111/j.1741-2358.2000.00055.x. [DOI] [PubMed] [Google Scholar]
- Forsell M., Sjögren P., Johansson O. Need of assistance with daily oral hygiene measures among nursing home resident elderly versus the actual assistance received from the staff. Open Dent. J. 2009;3:241. doi: 10.2174/1874210600903010241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerreth K., Borysewicz-Lewicka M. Access barriers to dental health care in children with disability. A questionnaire study of parents. J. Appl. Res. Intellect. Disabilities. 2016;29(2):139–145. doi: 10.1111/jar.12164. [DOI] [PubMed] [Google Scholar]
- Godin G., Bélanger-Gravel A., Eccles M., Grimshaw J. Healthcare professionals' intentions and behaviours: A systematic review of studies based on social cognitive theories. Implement. Sci. 2008;3(1):36. doi: 10.1186/1748-5908-3-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez E.E., Nathe C.N., Logothetis D.D., Pizanis V.G., Sanchez-Dils E. Training caregivers: disabilities and dental hygiene. Int. J. Dent. Hyg. 2013;11(4):293–297. doi: 10.1111/idh.12019. [DOI] [PubMed] [Google Scholar]
- Göstemeyer G., Baker S.R., Schwendicke F. Barriers and facilitators for provision of oral health care in dependent older people: a systematic review. Clin. Oral Investig. 2019;23(3):979–993. doi: 10.1007/s00784-019-02812-4. [DOI] [PubMed] [Google Scholar]
- Guarnizo-Herreño C.C., Wehby G.L. Explaining racial/ethnic disparities in children’s dental health: a decomposition analysis. Am. J. Public Health. 2012;102(5):859–866. doi: 10.2105/AJPH.2011.300548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harnagea H., Lamothe L., Couturier Y., Emami E. How primary health care teams perceive the integration of oral health care into their practice: A qualitative study. PloS one. 2018;13(10):e0205465. doi: 10.1371/journal.pone.0205465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartshorn J.E., Cowen H.J., Comnick C.L. Cluster randomized control trial of nursing home residents’ oral hygiene following the Mouth Care Matters education program for certified nursing assistants. Spec. Care Dentist. 2021;41:372–380. doi: 10.1111/scd.12577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hashmi S., Mohanty V.R., Balappanavar A.Y., Yadav V., Kapoor S., Rijhwani K. Effectiveness of dental health education on oral hygiene amonghearing impaired adolescents in India: A randomized control trial. Spec. Care Dentist. 2019;39(3):274–280. doi: 10.1111/scd.12374. [DOI] [PubMed] [Google Scholar]
- Hearn L., Slack-Smith L. Oral health care in residential aged care services: barriers to engaging health-care providers. Aust. J. Prim. Health. 2015;21(2):148–156. doi: 10.1071/PY14029. [DOI] [PubMed] [Google Scholar]
- Helgeson M., Glassman P. Oral health delivery systems for older adults and people with disabilities. Spec. Care Dentist. 2013;33(4):177–189. doi: 10.1111/scd.12038. [DOI] [PubMed] [Google Scholar]
- Hoben M., Clarke A., Huynh K.T., Kobagi N., Kent A., Hu H., Pereira R.A., Xiong T., Yu K., Xiang H., Yoon M.N. Barriers and facilitators in providing oral care to nursing home residents, from the perspective of care aides: A systematic review and meta-analysis. Int. J. Nurs. Stud. 2017;73:34–51. doi: 10.1016/j.ijnurstu.2017.05.003. [DOI] [PubMed] [Google Scholar]
- Huang L., Freed G.L., Dalziel K. Children with Special Health Care Needs: How Special Are Their Health Care Needs? Acad. Pediatr. 2020;20:1109–1115. doi: 10.1016/j.acap.2020.01.007. [DOI] [PubMed] [Google Scholar]
- Khanagar S., Kumar A., Rajanna V., Badiyani B.K., Jathanna V.R., Kini P.V. Oral health care education and its effect on caregivers’ knowledge, attitudes, and practices: a randomized controlled trial. J. Int. Soc. Prev. Community Dent. 2014;4(2):122. doi: 10.4103/2231-0762.139843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kmet L, Lee R, Cook L. Standard quality assessment criteria for evaluating primary research papers from variety of fields. Edmonton: Heritage Foundation for Medical research; 2004. [Google Scholar]
- Kusdhany L., Rahardjo T.B., Agustin D., Masulili C. Oral hygiene status and cognitive function in Indonesian elderly. Int. J. Clin. Prev. Dent. 2015;11(4):261–264. [Google Scholar]
- Lamba R., Rajvanshi H., Sheikh Z., Khurana M., Saha R. Oral Hygiene Needs of Special Children and the Effects of Supervised Tooth Brushing. Int. J. Sci. Study. 2015;3(5):30–35. [Google Scholar]
- Naseem M., Shah A.H., Khiyani M.F., Khurshid Z., Zafar M.S., Gulzar S., AlJameel A.H., Khalil H.S. Access to oral health care services among adults with learning disabilities: a scoping review. Annali di Stomatologia. 2016;7(3):52. doi: 10.11138/ads/2016.7.3.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niazi F., Naseem M., Khurshid Z., Zafar M.S., Almas K. Role of Salvadorapersica chewing stick (miswak): A natural toothbrush for holistic oral health. Eur. J. Dent. 2016;10(2):301. doi: 10.4103/1305-7456.178297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ocanto R., Levi-Minzi M.A., Chung J., Sheehan T., Padilla O., Brimlow D. The development and implementation of a training program for pediatric dentistry residents working with patients diagnosed with ASD in a special needs dental clinic. J. Dent. Educ. 2020;84:397–408. doi: 10.1002/jdd.12049. [DOI] [PubMed] [Google Scholar]
- Pecci-Lloret M.P., Guerrero-Gironés J., López-González B., Rodríguez-Lozano F.J., Oñate-Cabrerizo D., Oñate-Sánchez R.E., Pecci-Lloret M.R. Dental Treatments under General Anesthesia on Children with Special Health Care Needs Enrolled in the Spanish Dental Care Program. J. Clin. Med. 2021;10:182. doi: 10.3390/jcm10020182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porter J., Ntouva A., Read A., Murdoch M., Ola D., Tsakos G. The impact of oral health on the quality of life of nursing home residents. Health Qual. life Outcomes. 2015;13(1):102. doi: 10.1186/s12955-015-0300-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rashid-Kandvani F., Nicolau B., Bedos C. Access to dental services for people using a wheelchair. Am. J. Public Health. 2015;105(11):2312–2317. doi: 10.2105/AJPH.2015.302686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saarela R.K., Soini H., Hiltunen K., Muurinen S., Suominen M., Pitkala K. Dentition status, malnutrition and mortality among older service housing residents. J. Nutr. Health Aging. 2014;18(1):34–38. doi: 10.1007/s12603-013-0358-3. [DOI] [PubMed] [Google Scholar]
- Sahana S., Bambal A., Saxena V., Shivakumar G.C. Overcoming barriers to access dental care for the disabled children - A rising public health. J. Indian Public Health Dentist. 2013;9(18):553–556. [Google Scholar]
- Saito S., Ohi T., Murakami T., et al. Association between tooth loss and cognitive impairment in community-dwelling older Japanese adults: a 4-year prospective cohort study from the Ohasama study. BMC Oral Health. 2018;18:142. doi: 10.1186/s12903-018-0602-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sara Amir Hassan, ElTyeb, 2017. Oral health education for caregivers of children with disabilities. https://clinicaltrials.gov/show/nct03157596, 2017 | added to central: 31 may 2018 | 2018 issue 5 (last access on 5th September, 2021).
- Schensu J., Reisine S., Grady J., Li J. Good oral health: an innovative protocol for a community based clinical trial to improve oral health in older adults and people with disabilities. JMIR Preprints. 2019;8(12):e14555. doi: 10.2196/14555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schiavo J.H. PROSPERO: an international register of systematic review protocols. Med. Ref. Serv. Q. 2019;38:171–180. doi: 10.1080/02763869.2019.1588072. [DOI] [PubMed] [Google Scholar]
- Shah A.H., Naseem M., Khan M.S., Asiri F.Y., AlQarni I., Gulzar S., Nagarajappa R. Oral health knowledge and attitude among caregivers of special needs patients at a Comprehensive Rehabilitation Centre: an analytical study. Annali di Stomatologia. 2018;8(3):110. doi: 10.11138/ads/2017.8.3.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sjögren P., Nilsson E., Forsell M., Johansson O., Hoogstraate J. A systematic review of the preventive effect of oral hygiene on pneumonia and respiratory tract infection in elderly people in hospitals and nursing homes: effect estimates and methodological quality of randomized controlled trials. J. Am. Geriatr. Soc. 2008;56(11):2124–2130. doi: 10.1111/j.1532-5415.2008.01926.x. [DOI] [PubMed] [Google Scholar]
- Thomas B.H., Ciliska D., Dobbins M., Micucci S. A process for systematically reviewing the literature: providing the research evidence for public health nursing interventions. Worldviews Evid. Based Nurs. 2004;1:176–184. doi: 10.1111/j.1524-475X.2004.04006.x. [DOI] [PubMed] [Google Scholar]
- Tong A., Flemming K., McInnes E., Oliver S., Craig J. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med. Res. Methodol. 2012;12(1):181. doi: 10.1186/1471-2288-12-181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vpk V., Mohanty V.R., Balappanavar A.Y., Juneja M., Gupta V., Kapoor S. Effectiveness of different parenting interventions on oral hygiene of cerebral palsy children: A randomized controlled trial. Spec. Care Dentist. 2020;40(4):335–343. doi: 10.1111/scd.12481. [DOI] [PubMed] [Google Scholar]
- Waldman H.B., Rader R., Perlman S.P. Health related issues for individuals with special health care needs. Dent. Clin. North Am. 2009;53(2):183–193. doi: 10.1016/j.cden.2008.12.008. [DOI] [PubMed] [Google Scholar]
- Wardh I., Jonsson M., Wikstrom M. Attitudes to and knowledge about oral health care among nursing home personnel- an area in need of improvement. Gerodontology. 2012;29(2):e787–e792. doi: 10.1111/j.1741-2358.2011.00562.x. [DOI] [PubMed] [Google Scholar]
- Warren J.J., Chalmers J.M., Levy S.M., Blanco V.L., Ettinger R.L. Oral health of persons with and without dementia attending a geriatric clinic. Spec. Care Dentist. 1997;17(2):47–53. doi: 10.1111/j.1754-4505.1997.tb00866.x. [DOI] [PubMed] [Google Scholar]
- Weening-Verbree L., Huisman-de Waal G., van Dusseldorp L., van Achterberg T., Schoonhoven L. Oral health care in older people in long term care facilities: a systematic review of implementation strategies. Int. J. Nurs. Stud. 2013;50(4):569–582. doi: 10.1016/j.ijnurstu.2012.12.004. [DOI] [PubMed] [Google Scholar]
- Weintraub J.A., Zimmerman S., Ward K., Wretman C.J., Sloane P.D., Stearns S.C., Poole P., Preisser J.S. Improving Nursing Home Residents’ Oral Hygiene: Results of a Cluster Randomized Intervention Trial. J. Am. Med. Dir. Assoc. 2018;19(12):1086–1109. doi: 10.1016/j.jamda.2018.09.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welch, V., Petticrew, M., Tugwell, P., Moher, D., O'Neill, J., Waters, E., White, H., PRISMA-Equity Bellagio group, 2012. PRISMA-Equity 2012 extension: reporting guidelines for systematic reviews with a focus on health equity. PLoS Med. 9(10), e1001333. [DOI] [PMC free article] [PubMed]
- World Health Organisation, 2012. Oral health: fact sheet No. 318.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.