Abstract
Introduction
Midgut malrotation is a congenital condition caused by insufficient normal intestinal rotation following physiologic gut herniation. Reverse rotation of the midgut is the rarest kind of intestinal malrotation, accounting for about 2%–4% of all cases.
Case presentation
We report a case of a 26-year-old South Asian gravida with a previous history of quadruple miscarriage and ovulation induction, presented as intestinal obstruction due to reverse malrotation. An MRI of the abdomen indicated that the mesentery had become twisted around the SMA, resulting in a “whirlpool” pattern. Open exploration was done to accomplish lysis of restricting bands with appendectomy.
Conclusion
Intestinal obstruction in pregnancy is uncommon, but when unrecognized in a timely fashion, it is associated with significant maternal and fetal mortality. A simple release of constricting bands without antimesenteric transposition seems to be the safest option in this situation.
Keywords: Reverse malrotation, Volvulus, Bands, Whirlpool sign, Midgut, Case report
Highlights
-
•
Midgut malrotation is a congenital condition caused by insufficient normal intestinal rotation following physiologic gut herniation.
-
•
Intestinal obstruction in pregnancy is uncommon, but when unrecognized in a timely fashion, it is associated with significant maternal and fetal mortality.
-
•
A simple release of constricting bands without antimesenteric transposition seems to be the safest option in this situation.
1. Background
Incomplete intestinal rotation and fixation are denominated malrotation and usually have a congenital etiology. Although malrotation can be asymptomatic, the condition is often linked to volvulus and intestinal obstruction and is thus mainly diagnosed in newborn infants [1].
Pregnancy is an exception, as particular clinical manifestations of intestinal malrotation and obstruction may occur, accounting for approximately 2%–4%. Such instances may endanger both the mother and the fetus. Pregnancy complications due to intestinal obstruction are extremely rare, with an incidence of between 1/5000 and 1/66000. Most cases are diagnosed between the second and third trimesters [2]. Volvulus of the entire midgut, stenosis of the transverse colon, and obstruction of the duodenojejunal junction are common complications of reverse rotation [3]. In this study, we report the rare case of intestinal obstruction associated with reverse malrotation in pregnancy. This case report has been reported in line with the SCARE 2020 criteria [4].
2. Case presentation
A 26-year-old Asian lady in her 25th week of gestation presented to the emergency department with a history of recurrent bilious vomiting, distention of the abdomen, and inability to pass flatus and stools for ten days. She was admitted for similar complaints in Hyderabad, but there was no improvement in her condition then she was referred to our institute. She denied any history of fever, diarrhea, hematochezia, and melena.
She is Gravida 2, Para 1, and Miscarriage 1. She has a history of the polycystic ovarian disease (PCOD) and had ovulation induction two years back for pregnancy. She conceived a quadruplet in her previous pregnancy and had fetal reduction at 23 weeks for two of the four babies afterward; she had preterm labor followed by miscarriage. This was her precious pregnancy, and conceived again through ovulation induction. She had cervical cerclage at 20 weeks, given her previous history of miscarriage. She did not have similar complaints in her previous pregnancy. Her mother gave a history of similar complaints in childhood which was managed conservatively. She had no history of previous surgery.
At the time of presentation, she was dehydrated, sick looking, anxious, and afebrile with a heart rate of 110/m and blood pressure of 100/60 mmHg with continuous nasogastric drainage of bile of approximately 200–300 ml/day. She was catheterized with high-colored urine. Her abdomen was compatible with gestational age, with mild diffuse tenderness and distended. Immediate fluid resuscitation and an urgent ultrasound abdomen were done to assess fetal well-being, which was normal.
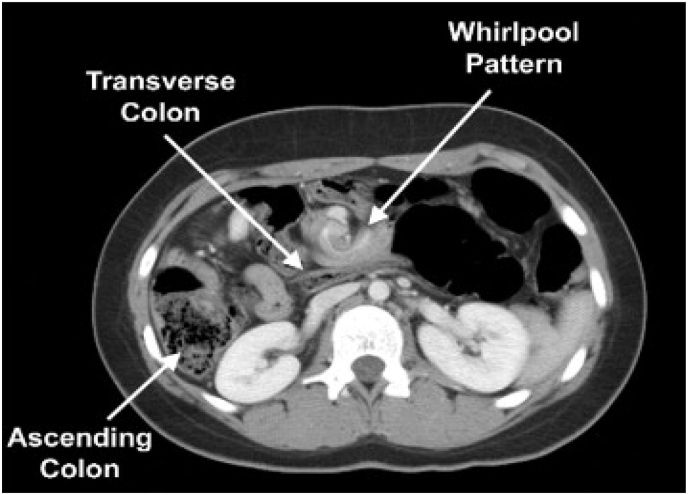
Her computed tomography (CT) abdomen revealed that mesentery was twisted around the superior mesenteric artery (SMA), resulting in a ‘‘whirlpool’’ sign. The dilated ascending colon had moved to the left abdomen. The transverse colon was located behind the SMA. The above findings suggested intestinal obstruction mainly due to midgut volvulus (Fig. 1).
Fig. 1.
CT scan of the abdomen with contrast showing intestinal obstruction.
She and her family were explained about the surgery and its consequences. After providing informed consent, she was taken for exploratory laparotomy. After discussion with a gynecologist, the decision to operate was prompted by the history of progressive worsening of her symptoms, large volume of nasogastric effluent, and clinical and radiological picture of high-grade bowel obstruction.
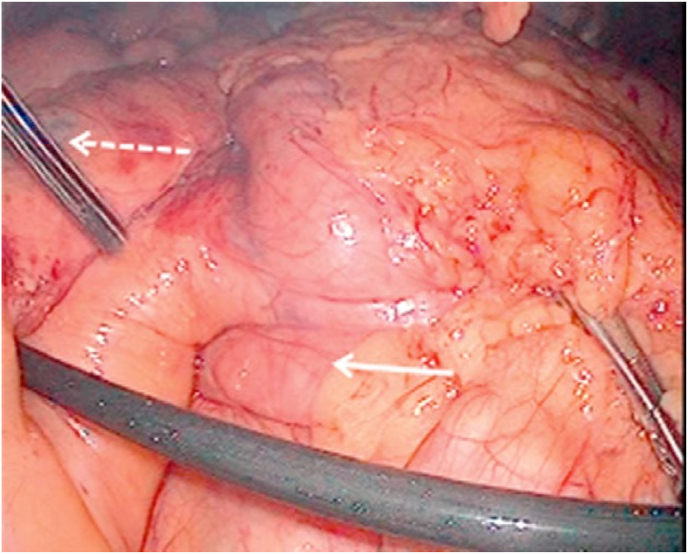
Diagnostic laparoscopy was performed and it was found that the mesentery of the colon and small intestine was insufficiently attached. The right colon and the small intestinal mesentery were twisted. The duodenum and duodenojejunal junction were curved in front of the transverse colon, and the transverse colon passed through the tunnel behind the mesenteric root. There was compression of the colon via SMA. Intestinal reverse rotation with volvulus was confirmed (Fig. 2). Laparoscopy converted into open exploration was done to perform lysis of constricting bands with appendectomy. The colon was left in situ. The operative approach worked well for the patient to resolve acute obstruction. She recovered after surgery. There were no other events during the follow-up. She delivered a healthy baby at term.
Fig. 2.
Intraoperative findings of reverse malrotation (Arrows = Compromised Vasculature).
3. Discussion
We reported a case of a pregnant woman presenting with a history of recurrent bilious vomiting, distention of the abdomen, and not being able to pass flatus and stools for ten days, later diagnosed as a reverse rotation of the intestine leading to intestinal obstruction. Open exploration was done to perform lysis of constricting bands with appendectomy.
There are three stages of midgut rotation. Stage 1: Midgut undergoes 90-degree counter-clockwise rotation. Stage 2: Midgut rotates to 270°. Stage 3: Mesenteric fixation occurs during this stage [5]. Malrotation is a defect in which intestinal rotation is incomplete, and mesenteric fixation does not occur. Malrotation can occur during any of the stages of gut rotation but usually occurs during the 10th week [6].
A rare presentation of intestinal malrotation is known as reverse malrotation. Reverse malrotation is twice as common in females than males and is more common in the second stage. Reverse malrotation most commonly presents in infancy or early adulthood with intestinal obstruction and volvulus of the nonfixed cecum and colonic obstruction by superior mesenteric vessels [7].
Reverse malrotation has three types. 1) transverse colon obstruction due to compression by superior mesenteric vessels, 2) mobile right colon volvulus, and 3) obstruction of duodenum and jejunum [8].
As proposed by Estrada, it takes place when the post-arterial bowel segment reduces back into the abdomen first; thus, the transverse colon is brought behind the duodenum and the Superior Mesenteric Artery. A case of intestinal malrotation in a pregnant woman was previously described in 1927 by Donald [9]. The authors present a rare case of complete large bowel obstruction with no prior surgical history caused by previously undiagnosed reversed intestinal rotation. On laparotomy, her transverse colon was positioned beneath the root of the small bowel mesentery and entirely occluded by congenital fibrous bands.
Intestinal obstruction is rare in pregnancy but is associated with significant maternal and fetal mortality. Intestinal blockage necessitates quick diagnosis, and aggressive management may be required to reduce the morbidity and mortality associated with this rare pregnancy condition [10].
Our study reports rare reverse malrotation, causing large bowel obstruction in a pregnant woman. There was a delay in her case due to hesitancy in performing teratogenic imaging in pregnancy and nonspecific chief complaints mimicking hyperemesis gravidarum. She was explained the nature of the imaging technique, and a CT abdomen was performed. We took her to the operating room, suspecting bowel obstruction based on the clinical grounds. We performed exploratory laparotomy, which was challenging because of the gravid uterus and distended bowels obscuring the view. Laparoscopy converted into open exploration was done to perform lysis of constricting bands with appendectomy. The colon was left in situ.
4. Conclusion
To the best of our knowledge, this is the rare case report of reversed rotation causing large bowel obstruction in a pregnant woman. Intestinal obstruction in pregnancy is uncommon, but when unrecognized in a timely fashion, it is associated with significant maternal and fetal mortality. A simple release of constricting bands without antimesenteric transposition seems to be the safest option in this situation.
Ethical approval
NA.
Please state any sources of funding for your research
No funding was received for this case report.
Author contribution
AB conceived and designed the study. AB and HN were responsible for data collection and acquisition of data. AB, HM, and MWN analyzed and/or interpreted the data. HM and HN performed the literature review. AB, HM, and HN wrote the initial manuscript. HM and MWN critically revised the manuscript. All authors have approved the final manuscript.
Please state any conflicts of interest
No conflict of interest.
Consent
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. Written informed consent was also taken from the patient's next of kin, his son in this case. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Registration of research studies
-
1.
Name of the registry: NA
-
2.
Unique Identifying number or registration ID: NA
-
3.
Hyperlink to your specific registration (must be publicly accessible and will be checked): NA
Guarantor
Dr Hamza Maqsood, Nishtar Medical University, And Hospital, Multan, Pakistan, Phone: +923168435531, Email address: hamzamaqsood381@gmail.com.
Provenance and peer review
Not commissioned, externally peer reviewed.
Acknowledgment
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.amsu.2022.104570.
Contributor Information
Anjali Bhartiya, Email: dranjee24@gmail.com.
Hamza Maqsood, Email: hamzamaqsood381@gmail.com.
Hamna Naeem, Email: hamnanaeem853@gmail.com.
Muhammad Wajeeh Nazar, Email: muhammadwajeehnazar@gmail.com.
List of Abbreviations
- MRI
Magnetic resonance imaging
- PCOD
Polycystic ovarian disease
- SMA
Superior mesenteric artery
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Husberg B., Salehi K., Peters T., et al. Congenital intestinal malrotation in adolescent and adult patients: a 12-year clinical and radiological survey. SpringerPlus. 2016;5:245. doi: 10.1186/s40064-016-1842-0. Published 2016 Mar 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhao X.Y., Wang X., Li C.Q., Zhang Q., He A.Q., Liu G. Intestinal obstruction in pregnancy with reverse rotation of the midgut: a case report. World J Clin Cases. 2020;8(16):3553–3559. doi: 10.12998/wjcc.v8.i16.3553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guerra M., Iacuzzo C., Scotton G., Biloslavo A., de Manzini N. A rare case of reverse midgut rotation and jejunal transmesenteric internal hernia in an adult with Beckwith-Wiedemann syndrome. Ann. Ital. Chir. 2021;92:560–564. [PubMed] [Google Scholar]
- 4.Agha R.A., Franchi T., Sohrabi C., Mathew G., Kerwan A., SCARE Group The SCARE 2020 guideline: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 5.Singh U., Baker A. Midgut malrotation: a rare presentation of bowel obstruction in the adult. J. Surg. Case Rep. 2021;(7) doi: 10.1093/jscr/rjab309. 2021. Published 2021 Jul 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yang L., Chen H., Lv G., et al. Evaluation of ultrasonography in fetal intestinal malrotation with midgut volvulus. Ginekol. Pol. 2022 Feb doi: 10.5603/gp.a2021.0237. [DOI] [PubMed] [Google Scholar]
- 7.Anand U., Kumar R., Priyadarshi R.N., Kumar B., Kumar S., Singh V.P. Comparative study of intestinal malrotation in infant, children, and adult in a tertiary care center in India. Indian J. Gastroenterol. 2018;37(6):545–549. doi: 10.1007/s12664-018-0914-1. [DOI] [PubMed] [Google Scholar]
- 8.Jarvis J.K., Rambhajan A. Adult intestinal malrotation in a non-paediatric hospital in trinidad: a case report and literature review. Cureus. 2020;12(12) doi: 10.7759/cureus.12305. Published 2020 Dec 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aranovich D., Schrier I. Reversed intestinal rotation presented as bowel obstruction in a pregnant woman. Case Rep Surg. 2015 doi: 10.1155/2015/870437. 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Daimon A., Terai Y., Nagayasu Y., et al. A case of intestinal obstruction in pregnancy diagnosed by MRI and treated by intravenous hyperalimentation. Case Rep Obstet Gynecol. 2016 doi: 10.1155/2016/8704035. 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.