Abstract
Introduction
Acute carbon monoxide poisoning can present with altered mentation, loss of consciousness, and other symptoms. Accurate diagnosis is based on a detailed history, clinical examination, and laboratory evidence. MRI is also crucial in detecting hypoxic-ischemic encephalopathy due to CO poisoning and has established superiority over CT scans. We report an atypical MR imaging pattern seen in a patient post-CO exposure.
Case presentation
We report a case of a 35-year-old South Asian man who presented to the emergency department with loss of consciousness for an undetermined time. GCS on arrival was 4/15. Detailed history, physical examination, and radiological investigations confirmed the diagnosis of carbon monoxide poisoning. He was treated with 100% oxygen.
Conclusion
MRI should be included as a diagnostic workup for suspected CO poisoning patients to evaluate hypoxic-ischemic encephalopathy. This will not only aid in the correct diagnosis but will also help in guiding the correct management of the patients.
Keywords: Carbon monoxide, Poisoning, Neurology, MRI, Altered mentation
Highlights
-
•
Acute carbon monoxide poisoning can present with altered mentation, loss of consciousness, and other symptoms.
-
•
MRI is also crucial in detecting hypoxic-ischemic encephalopathy due to CO poisoning and has established superiority over CT scans.
-
•
MRI should be included as a diagnostic workup for suspected CO poisoning patients to evaluate hypoxic-ischemic encephalopathy. This will not only aid in the correct diagnosis but will also help in guiding the correct management of the patients.
1. Background
Carbon monoxide (CO) is a colorless and odorless gas produced by incomplete combustion of carbon-containing materials. CO poisoning is the major cause of unintentional poisoning in the United States. Unintentional, non-fire-related CO poisoning leads to 4500 deaths and 2100 emergency department visits annually [1]. The clinical presentation of CO poisoning ranges from mild, moderate, and severe. Mainly it presents as nonspecific findings like headache, nausea, and vomiting but can lead to severe complications like delayed neurologic sequelae, seizures, and cardiopulmonary compromise [2]. CO poisoning diagnosis can be challenging in an emergency due to its lethal and covert action; therefore, a thorough approach to rule out other causes is also very important. Suspected patients will have elevated blood carboxyhemoglobin levels most of the time, and some studies saw this effect to a greater extent in chronic smokers [3]. CO poisoning can also lead to focal and widespread neurological manifestations. In that case, patients should undergo magnetic resonance imaging (MRI) to evaluate the extent of brain injury, which has superiority over a computed tomography (CT) scan [[4], [5], [6]]. After diagnosis, 100% oxygen is the mainstay of treatment to release CO from hemoglobin molecules. Existing literature shows that cerebral white matter and basal ganglia are the most affected regions, and some reports have demonstrated cerebellar injury [6,7]. Here we present a case of acute CO poisoning leading to a novel pattern of hypoxic-ischemic injury to the gray matter in frontoparietal and occipitotemporal regions of the cortex. Our work has been reported in line with the SCARE 2020 criteria [8].
2. Case presentation
Thirty-five-year-old Asian gentleman presented to the emergency department with a daytime headache for the past week, nausea and vomiting for the past two days, and loss of consciousness for the past 2 h. His co-worker spotted him unconscious near a machine. He is a mechanical engineer from China and works in an electricity company that has a poor ventilation mechanism. The patient complained of diffuse headaches, causing a band-like squeezing pain in the frontal area, and “body aches” for the past week. He vomited twice in the past 2 h. He never experienced any nausea and vomiting in the past six months and can't recall beyond that. There is no history of weight loss, but he reports decreased appetite. There is no associated pain in the abdomen, constipation, distension, or diarrhea. There is mild breathlessness only during working hours but no palpitations, chest pain, and edema feet. The patient had no critical medical history and took no medications. He has worked as a mechanical engineer for the past ten years.
On physical examination, the Glasgow coma scale (GCS) on arrival was 4/15. Vital signs were recorded as a pulse rate of 82 bpm, a temperature of 36 °C, blood pressure was 115/70, and a respiratory rate of 18 breaths per minute with oxygen saturation of 98% on room air. Physical examination showed an unconscious man lying on the bed with an average build. No cyanosis or respiratory distress was noted. Bilateral breath sounds were normal, and the point of maximal impulse was localized and normal. Neurological examination showed bilaterally symmetrical round and reactive pupil, and the rest of the examination was unremarkable.
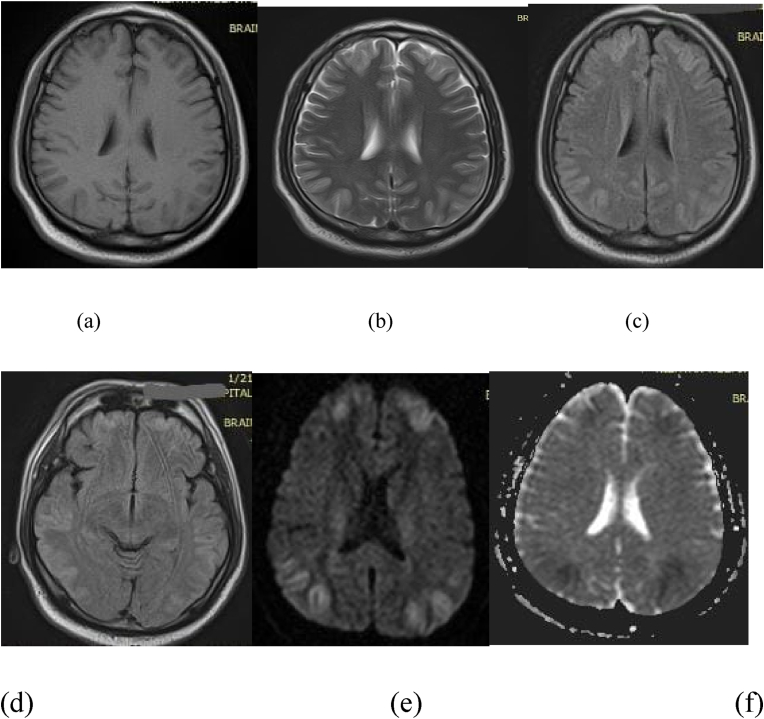
Electrocardiography (ECG) was performed and was normal. After securing the airway and maintaining 100% oxygen via continuous positive airway pressure (CPAP), he was sent to the radiology department for a CT brain to rule out hemorrhage. Emergent CT showed no abnormalities and a provisional diagnosis of carbon monoxide poisoning. Subsequently, he was kept on high-flow oxygen and started to feel better and regained consciousness after some time. MRI was performed after 12 hours and showed bilateral abnormal MR signals hypointense on T1W and hyperintense on T2W and FLAIR sequences. There was also significant diffusion restriction on Diffusion-weighted imaging (DWI) involving bilateral frontoparietal and temporal cortex (Fig. 1).
Fig. 1.
(a–f): a. T1-weighted MRI of the brain with bilateral hypo-intensities in frontal and parietal lobes. b. T2 weighted MRI with abnormal signal (hyper-intense) in bilateral frontal and occipital lobes. c and d. FLAIR sequences at two levels. c) at the level of the body of lateral ventricles showing bilateral hyper-intensities in frontal and parietal lobes. d) at the level of the third ventricle showing bilateral hyper-intensities in frontal, parietal, and temporal lobes. e. Diffusion-weighted imaging (DWI) shows symmetrical bilateral restricted diffusion in the gray matter of frontal and parietal lobes. f. Apparent diffusion coefficient (ADC) map: corresponding areas to figure b show dark areas on ADC map suggesting acute ischemia.
The patient was admitted to the medical unit under supervision and was kept on high flow oxygen for the next 6 hours, after which he felt much better. He was also given intravenous (IV) fluids and metoclopramide IV for nausea and oral acetaminophen for headache. A repeat examination on day 2 of admission was performed and was non-focal with no altered level of consciousness. The patient was oriented to place, person, and time, and the headache improved. He hadn't felt nauseous during the hospital stay and was subsequently discharged. His discharge medications were oral acetaminophen 1000mg three times a day (Tid) for five days. The patient was followed up after seven days, and a repeat neurological examination was unremarkable.
3. Discussion
We reported a case of a patient presenting with frontal headache, vomiting, and an altered level of consciousness later diagnosed as carbon monoxide poisoning. On radiological investigations, this patient showed a very unique involvement of gray matter in frontoparietal and occipitotemporal regions of the cortex. Along with that watershed ischemia of anterior cerebral artery/middle cerebral artery (ACA/MCA) and middle cerebral artery/posterior cerebral artery (MCA/PCA) territory was also observed. Existing literature has reported various cases of neurological complications of carbon monoxide poisoning [2,5]. This case reports a rare radiological pattern of involvement of the brain in CO poisoning.
The most common organ affected by acute CO poisoning is the brain. Many previous studies suggest that the most common brain parts affected by CO poisoning are bilateral globus pallidus, basal ganglia, and cerebral white matter [[9], [10]]. Although the exact mechanism of damage by carbon monoxide and pathophysiology is unknown, some review of the literature suggests that through known and unknown processes, carbon monoxide causes inhibition of electron transport chain [11], lipid peroxidation [12], leucocyte adhesion to microvasculature (oxidative), and the release of nitric oxide from platelets and endothelium. In addition, CO is also shown to injure the blood-brain barrier causing cytotoxic and cerebral edema [13].
Several case reports have demonstrated that neuroimaging has superiority in diagnosing acute carbon monoxide poisoning neurotoxicity and neuropathological changes in the brain. MRI is a more sensitive and preferred modality over CT scan in this regard [[4], [5], [6], [7]]. Most of the neuropathological changes are present in the white matter of the cerebrum and basal ganglia, so abnormal signals can be detected easily by T1, T2, flair, and diffusion-weighted MRI scan due to cytotoxic edema and ischemia [5]. Therefore, patients with suspected carbon monoxide poisoning and equivocal diagnosis should undergo MRI to further the diagnostic process and correct management of the patient.
Current guidelines recommend the treatment of acute carbon monoxide poisoning with 100% oxygen. Also, some studies suggest that hyperbaric oxygen therapy, compared to normobaric oxygen therapy, is associated with fewer complications and delayed neurological syndrome (DNS) [14]. Therefore, rapid diagnosis and treatment aid in the correct management of patients, and knowledge of atypical imaging patterns is helpful in this regard.
4. Conclusion
MRI should be included as a diagnostic workup for suspected CO poisoning patients to evaluate hypoxic-ischemic encephalopathy. MRI has greater sensitivity than CT scan and should be preferred in scenarios of CO poisoning. This will not only aid in the correct diagnosis in the patient but will also help in guiding the correct management of the patient with potentially low-cost treatment like hyperbaric oxygen and will save the patients.
Ethical approval
N/A.
Sources of funding
No funding was received for this case report.
Authors contributions
ASS conceived and designed the study. HR and ASA were responsible for data collection and acquisition of data. HR, JY, and HM analyzed and/or interpreted the data. HM and HR performed the literature review. ASA, HR, and HM wrote the initial manuscript. ASS and SS critically revised the manuscript. All authors have approved the final manuscript.
Research registration number
Name of the registry: NA.
Unique Identifying number or registration ID: NA.
Hyperlink to your specific registration (must be publicly accessible and will be checked): NA.
Guarantor
Dr Hamza Maqsood
Nishtar Medical University
And Hospital, Multan, Pakistan
Phone: +923168435531
Email address: hamzamaqsood381@gmail.com
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Availability of data and materials
Not applicable.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Declaration of competing interest
No conflict of interest.
Acknowledgment
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.amsu.2022.104655.
Contributor Information
Alen Sam Saji, Email: samalen9900@gmail.com.
Muhammad Hassan Raza, Email: hraza875@gmail.com.
Abdul Sattar Anjum, Email: drasanjum@gmail.com.
Hamza Maqsood, Email: hamzamaqsood381@gmail.com.
Javeriya Yousaf, Email: ali07ee64@gmail.com.
Sheraz Saleem, Email: mkamranmd15@gmail.com.
List of abbreviations
- CO
Carbon monoxide
- CT
Computed tomography
- MRI
Magnetic resonance imaging
- GCS
Glasgow coma scale
- IV
intravenous
- ACA
Anterior cerebral artery
- MCA
Middle cerebral artery
- PCA
Posterior cerebral artery
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Centers for Disease Control and Prevention . Centers for Disease Control and Prevention; 2021, April 16. Carbon Monoxide Poisoning 2019 Case Definition.https://ndc.services.cdc.gov/case-definitions/carbon-monoxide-poisoning-2019/ Retrieved. [Google Scholar]
- 2.Wu C.T., Huang J.L., Hsia S.H. Acute carbon monoxide poisoning with severe cardiopulmonary compromise: a case report. Cases J. 2009 Jan 14;2(1):52. doi: 10.1186/1757-1626-2-52. PMID: 19144167; PMCID: PMC2637259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schimmel J., George N., Schwarz J., Yousif S., Suner S., Hack J.B. Carboxyhemoglobin levels induced by cigarette smoking outdoors in smokers. J. Med. Toxicol. 2018 Mar;14(1):68–73. doi: 10.1007/s13181-017-0645-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.O'Donnell P., Buxton P.J., Pitkin A., Jarvis L.J. The magnetic resonance imaging appearances of the brain in acute carbon monoxide poisoning. Clin. Radiol. 2000 Apr;55(4):273–280. doi: 10.1053/crad.1999.0369. PMID: 10767186. [DOI] [PubMed] [Google Scholar]
- 5.Jasne A.S., Alsherbini K.H., Smith M.S., Pandhi A., Vagal A., Kanter D. Cerebellar hippocampal and basal nuclei transient edema with restricted diffusion (CHANTER) syndrome. Neurocritical Care. 2019;31(2):288–296. doi: 10.1007/s12028-018-00666-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kanaya N., Imaizumi H., Nakayama M., Nagai H., Yamaya K., Namiki A. The utility of MRI in acute stage of carbon monoxide poisoning. Intensive Care Med. 1992;18(6):371–372. doi: 10.1007/BF01694368. PMID: 1469165. [DOI] [PubMed] [Google Scholar]
- 7.Mascalchi M., Petruzzi P., Zampa V. MRI of cerebellar white matter damage due to carbon monoxide poisoning: case report. Neuroradiology. 1996 May;38(Suppl 1):S73–S74. doi: 10.1007/bf02278124. PMID: 8811685. [DOI] [PubMed] [Google Scholar]
- 8.Agha R.A., Franchi T., Sohrabi C., Mathew G., Kerwan A., SCARE Group The SCARE 2020 guideline: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 9.Norman C.A., Halton D.M. Is carbon monoxide a workplace teratogen? A review and evaluation of the literature. Ann. Occup. Hyg. 1990;34(4):335–347. doi: 10.1093/annhyg/34.4.335. [DOI] [PubMed] [Google Scholar]
- 10.Lin W.C., Lu C.H., Lee Y.C., et al. White matter damage in carbon monoxide intoxication assessed in vivo using diffusion tensor MR imaging. AJNR Am J Neuroradiol. 2009;30(6):1248–1255. doi: 10.3174/ajnr.A1517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhang J., Piantadosi C.A. Mitochondrial oxidative stress after carbon monoxide hypoxia in the rat brain. J. Clin. Invest. 1992;90(4):1193–1199. doi: 10.1172/JCI115980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thom S.R. Carbon monoxide-mediated brain lipid peroxidation in the rat. J. Appl. Physiol. 1985;68(3):997–1003. doi: 10.1152/jappl.1990.68.3.997. 1990. [DOI] [PubMed] [Google Scholar]
- 13.Fan H.C., Wang A.C., Lo C.P., Chang K.P., Chen S.J. Damage of cerebellar white matter due to carbon monoxide poisoning: a case report. Am. J. Emerg. Med. 2009 Jul;27(6):757.e5–757.e7. doi: 10.1016/j.ajem.2008.10.021. PMID: 19751650. [DOI] [PubMed] [Google Scholar]
- 14.Weaver L.K., Valentine K.J., Hopkins R.O. Carbon monoxide poisoning: risk factors for cognitive sequelae and the role of hyperbaric oxygen. Am. J. Respir. Crit. Care Med. 2007;176(5):491–497. doi: 10.1164/rccm.200701-026OC. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Not applicable.