Abstract
Introduction and importance
Parry-Romberg syndrome (PRS) is a rare clinical entity characterized by progressive atrophy of the hemifacial region, occasionally associated with systemic manifestations. The presence of facial muscles spasms is exceptional.
Case presentation
We report the case of a young woman who presented with progressive atrophy of the right hemiface associated with vitiligo and facial muscles spasms. The diagnosis of Parry Romberg syndrome was retained. Electromyogram showed an intermittent motor unit potential. Cerebral MRI showed atrophy of the muscle and subcutaneous fat of the right hemiface. She received corticosteroid in combination with botulinum toxin injection, which stopped the spasms.
Clinical discussion
It is a rare condition with a poorly understood etiology, which is responsible for the delay in diagnosis often noted. The association of this syndrome with neurological signs is exceptional and rarely described in the literature. Injection of botulinum toxin associated with corticosteroids can stop the spasms but only surgery can reduce the facial deformities.
Conclusion
Parry-Romberg syndrome is a rare disease, more frequent in women. It poses a real diagnostic problem and its treatment is poorly codified.
Keywords: Facial muscles spasms, Hemifacial atrophy, Parry-Romberg syndrome, Botulinum toxin
Highlights
-
•
Parry-Romberg syndrome is a rare disease whose prevalence isn't well known.
-
•
This is an unknown disease and is the reason for the delay in diagnosis.
-
•
Facial muscles spams is rarely associated with Parry-Romberg syndrome.
-
•
Botulinum toxin can stop facial muscle spasms.
1. Introduction
The work has been reported in line with the SCARE criteria [1].
Parry-Romberg syndrome (PRS) is a rare disease whose etiopathogeny is poorly understood, manifested by progressive hemifacial atrophy, and sometimes is associated with neurological, cutaneous, ophthalmological, and maxillofacial signs [2,3]. It is not often described in sub-Saharan Africa [4]. We report a case of Parry Romberg syndrome associated with facial muscles spasms and oculomotor impairment.
2. Presentation of case
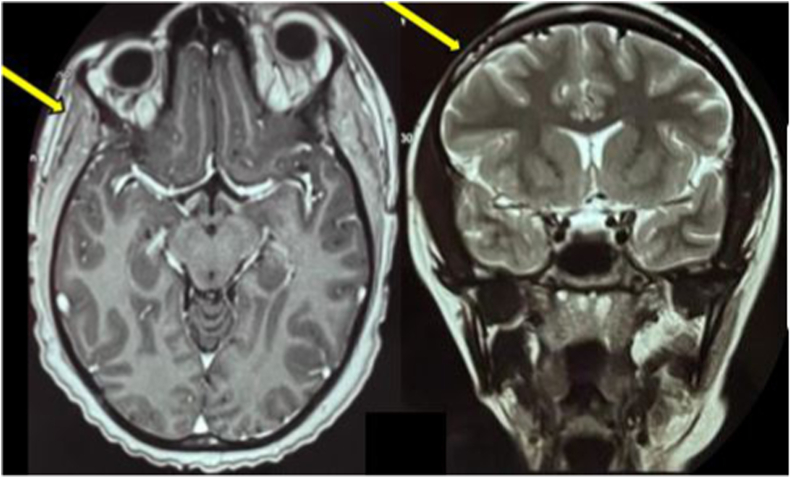
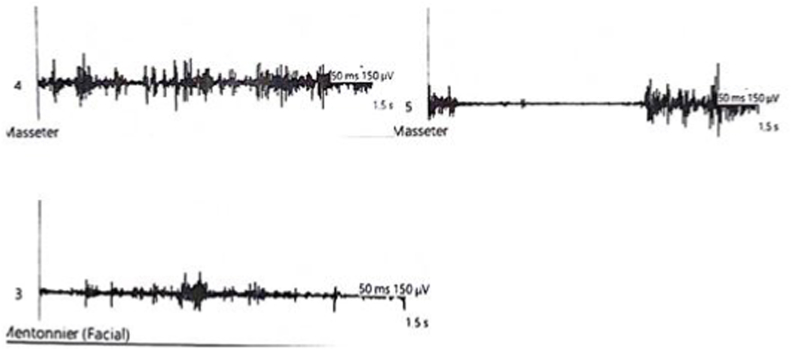
A 24-year-old woman, with a maternal history of vitiligo, presented at his nineteen years, with a persistent chin furrow. Eight months later, intermittent contractions in temporal and masseter muscles appeared during mastication, progressively worsening over several years. A facial deformity appeared secondly, with a frontal saber-shape appearance and atrophy of the right hemiface (Fig. 1). Referred to neurology, after several consultations in oto-rhino-laryngology, ophthalmology, and stomatology, a clinical examination in July 2021 found hemifacial amyotrophy, frontal and brow capillary depilation, enophthalmia, lagophthalmia, and the right abducens (6th cranial nerve) nerve palsy. We also noted intermittent contractions on the right temporal and masseter muscles and vitiligo lesions on the neck, the left scapula, the left axillary region, and the left forearm (Fig. 2). Cerebral MRI showed atrophy of the muscle and subcutaneous fat of the right hemiface on the T1 axial and T2 coronal slices (Fig. 4) but the immunological workup (antinuclear and anti-ECT antibodies) was negative. On the first electromyogram: neurography, detection, and blink reflex were normal. A second electromyogram with surface electrode showed spontaneous, intermittent motor unit potentials (Fig. 3). The diagnosis was Parry-Romberg syndrome at stage 3 of the Guerrerosantos classification. The patient received corticosteroids 1 mg/kg/day in combination with botulinum toxin injections which stopped the spasms but there was persistent atrophy of the hemiface.
Fig. 1.
A frontal saber-shape appearance and atrophy of the right.
Fig. 2.
Vitiligo lesion on patient's right.
Fig. 4.
Cerebral MRI showed atrophy of the muscle and subcutaneous fat of the right.
Fig. 3.
Showed spontaneous, intermittent motor unit potentials.
3. Discussion
This is a 24-year-old female patient with a family history of vitiligo who presented progressive atrophy of the hemiface associated with vitiligo lesions in his nineteen years. For this, the diagnosis of Parry Romberg disease was retained. This condition is a clinical phenomenon initially described in 1825 by Dr. Parry [2] and then in 1846 by Dr. Romberg who detailed it as a syndrome [3]. The real incidence and epidemiological characteristics are difficult to demonstrate because of the rarity of this syndrome and the absence of standardized diagnostic criteria [5]. These different factors explain the delay in diagnosis observed in patients suffering from this syndrome. This diagnostic delay was found in our patient who had several consultations over 6 years without a diagnosis. This is a ubiquitous pathology, of etiology not well known with several physiopathological hypotheses evoked. The main ones are genetic and autoimmune. Indeed, some authors thought that Parry Romberg disease is a genetic disease because of family cases reported in the literature, but no study has been able to confirm this. The autoimmune theory seems the most convincing as it is based on the presence of autoimmune abnormalities such as vitiligo, rheumatoid arthritis, myopathy, or the presence of antinuclear antibodies [6]. Our patient presented with haemicoporeal vitiligo lesions as described in the literature even though she was tested negative for antinuclear antibodies. The disease affects more women. It usually appears in the first two decades of life, as evidenced by the case we describe, in which the clinical manifestations started at nineteen years. It is generally unilateral, affecting one hemiface, and atrophy stabilizes after 5 and 10 years [7]. Depending on the severity, 4 types have been described by Guerrerosantos et al. [8]. Our patient has been classified type 3 due to soft tissue thinning and severe atrophy. The presence of neurological signs such as masseter and temporal muscle spasms and right abducens nerve damage is the main feature of our case. These signs are rarely reported in the literature. In a serie of 129 patients with PRS and neurological involvement, Vix et al. reported only 8 cases of muscle spasm (with 4 cases of masseter muscle spasm and 3 cases of facial muscle spam) and 14 cases of oculomotor paralysis [9]. These muscle spasms were reflected by motor unit potentials on the ENMG in our patient. The signs associated with Parry-Romberg syndrome are stomatological or ocular [[10], [11], [12]]. In our patient, the ophthalmological signs are lagophtalmy, enophthalmy, and right eyebrow depilation. These manifestations are found in only 10–35% of cases and can occur before, during, or after facial atrophy. Management involves corticosteroid therapy and immunosuppressants. Local treatment with botulinum toxin injections may be used before surgery [6,7] however, non-invasive treatments have been used in the management of these muscle spasms. Indeed Baduni et al. reported a case of facial muscle spasms in a PRS successfully treated by ultrasound and transcutaneous electric nerve stimulation (TENS) [13]. In contrast to our patient who received corticosteroid therapy in combination with botulinum toxin injections. The evolution was favourable with disappearance of the spasms but there was a persistence of facial atrophy.
4. Conclusion
Parry-Romberg syndrome is a rare disease, more frequent in women. It poses a real diagnostic problem and its treatment is poorly codified. Management requires multidisciplinary collaboration, ranging from medical treatment to slow disease progression to surgery to reduce malformations.
Ethical approval
The ethical committee of the hospital gave the agreement to report this case.
Sources of funding
The authors declare they have received no funding for the preparation of this document.
Author contribution
Ahmadou Bamba Mbodji, Momar Seck, Ngor Side Diagne, Serigne Saliou Mbacké, Ibrahima Faye and Moustapha Ndiaye : these authors participated in the making and correction of this document. All authors agreed with the publication of the document.
Research registration number
1. Name of the registry: Research registry
2. Unique Identifying number or registration ID: researchregistry8292
3. Hyperlink to your specific registration (must be publicly accessible and will be checked): https://www.researchregistry.com/browse-theregistry#home/registrationdetails/631b966b06344e00265e934f/.
Guarantor
Ahmadou Bamba Mbodji
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Provenance and peer review
Not commissioned, externally peer reviewed.
Patient consentment
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Declaration of competing interest
The authors declare no conflict of interest.
References
- 1.Agha R.A., Franchi T., Sohrabi C., Mathew G., Kerwan A., SCARE Group The SCARE 2020 guideline: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 2.Parry C. London Underwoods; 1825. Collection from the Unpublished Medical Writings of the Late C.H Parry; p. 478. London. Underwoods. [Google Scholar]
- 3.Romberg H. 1846. Trophoneurisen. Klinishe Ergebnisse; pp. 75–81. Berlin, Forstner,. Berlin, Forstner. [Google Scholar]
- 4.Maroufi S.E., Bennis A., Chraibi F., Abdellaoui M., Andaloussi I.B. Ulcère de cornée chronique révélant un syndrome de Parry-Romberg: à propos dun cas. Pan Afr. Med. J. 2021;38:53. doi: 10.11604/pamj.2021.38.53.27190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Duymaz A., Karabekmez F.E., Keskin M., Tosun Z. Parry-Romberg syndrome: facial atrophy and its relationship with other regions of the body. Ann. Plast. Surg. 2009;63(4):457–461. doi: 10.1097/SAP.0b013e31818bed6d. [DOI] [PubMed] [Google Scholar]
- 6.Tolkachjov S.N., Patel N.G., Tollefson M.M. Progressive hemifacial atrophy: a review. Orphanet J. Rare Dis. 2015;10:39. doi: 10.1186/s13023-015-0250-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hunstad J., Shifrin D., Kortesis B. Successful treatment of Parry-Romberg syndrome with autologous fat grafting 14-year follow-up and review. Ann. Plast. Surg. 2011;67:423–425. doi: 10.1097/SAP.0b013e31820b3aa8. 16 mai. [DOI] [PubMed] [Google Scholar]
- 8.Guerrerosantos J., Guerrerosantos F., Orozco J. Classification and treatment of facial tissue atrophy in Parry-Romberg disease. Aesthetic Plast Surg. 2007;31(5):424–434. doi: 10.1007/s00266-006-0215-4. oct. [DOI] [PubMed] [Google Scholar]
- 9.Vix J., Mathis S., Lacoste M., Guillevin R., Neau J.P. Neurological manifestations in Parry-Romberg syndrome: 2 case reports. Medicine (Baltimore) 2015;94(28):e1147. doi: 10.1097/MD.0000000000001147. juill. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Janowska M., Podolec K., Lipko-Godlewska S., Wojas-Pelc A. Coexistence of Parry-Romberg syndrome with homolateral segmental vitiligo. pdia. 2013;6:409–411. doi: 10.5114/pdia.2013.39441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Aydın H., Yologlu Z., Sargın H., Metin M.R. Parry-Romberg syndrome. Physical, clinical, and imaging features. Neurosciences (Riyadh) oct 2015;20(4):368–371. doi: 10.17712/nsj.2015.4.20150142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bucher S.F., Seelos K.C., Dodel R.C., Paulus W., Reiser M., Oertel W.H. Pallidal lesions. Structural and functional magnetic resonance imaging. Arch Neurol. 1996;53(7):682–686. doi: 10.1001/archneur.1996.00550070124020. juill. [DOI] [PubMed] [Google Scholar]
- 13.Baduni A., Krishnamoorthy B. Treatment of hemifacial spasm in patient with hemifacial atrophy using combination therapy (ultrasound therapy and TENS): a case report. Kor. J. Pain. oct 2017;30(4):304–307. doi: 10.3344/kjp.2017.30.4.304. [DOI] [PMC free article] [PubMed] [Google Scholar]