Abstract
Lateral medullary syndrome (LMS) is the most common and severe neurological syndrome associated with atherothrombotic occlusion of the intracranial vertebral artery, followed by posterior inferior cerebellar artery and medullary artery occlusion. It presents as a typical triad of oculosympathetic palsy (Horner's syndrome), ipsilateral gait ataxia, and hypoalgesia with ipsilateral thermoanesthesia of the face.
In LMS, the upper motor neuron facial palsy is caused by the involvement of aberrant supranuclear fibers of the facial nerve. The caudal extension of the infarction to the pyramidal tracts may explain contralateral hemiparesis. Here, we have discussed a 42-year-old non-diabetic, hypertensive male with LMS, hemiparesis, and left UMN-type facial palsy. We reported this case because developing nations, have few tertiary level health facilities for neurological examination, and non-neurologists often miss the diagnosis; therefore, the characteristics must be known and understood.
Keywords: Lateral medullary syndrome, Hemiparesis, Facial palsy, Upper motor neuron, Stroke
Highlights
-
•
The patient had hemiparesis, left UMN-type facial palsy, and Horner's syndrome.
-
•
Dejerine's aberrant pyramidal tract could be the cause of UMN-Facial Nerve palsy.
-
•
Caudal extension of lesion to pyramidal tracts explains contralateral hemiparesis.
1. Introduction
Lateral medullary syndrome (LMS), also known as Wallenberg syndrome, was initially recognized and documented in 1961 [1]. This neurological syndrome is caused by involvement of the lateral region of the medulla and is most commonly caused by occlusion of the atherothrombotic vertebral artery, the posterior inferior cerebellar artery (PICA), and followed by the medullary artery. Magnetic resonance imaging is used to make the diagnosis [2].
In addition to these classic clinical findings, Wallenberg syndrome can have various unusual manifestations. Here, the contralateral hemiparesis could be explained by the caudal extension of the infarct involving pyramidal tracts before crossing at the medulla [3]. The involvement of Dejerine's aberrant pyramidal tract might explain facial palsy caused by the infarction of the left facial colliculus and the left lateral medulla [4]. According to SCARE guidelines by Agha RA et.al., we are presenting the case of a patient who experienced upper motor neuron (UMN) facial nerve palsy and hemiparesis after a left lateral medullary infarction [5].
2. Case presentation
A 42-year-old gentleman visited the emergency department with right-side weakness, severe headache, and dizziness that had persisted for four days and was accompanied by significant dizziness and facial deviation. He experienced tingling on the left side of his face and later found that he could not feel pain or temperature changes on that side of his face. There had been several episodes of vomiting, as well as difficulty swallowing, hiccups, and coughing.
He had uncontrolled hypertension for five years and was taking antihypertensive medication, which he discontinued last year. He had a blood pressure of 170/95 mmHg and a pulse rate of 98 beats per minute. He does not smoke cigarettes or drink alcohol.
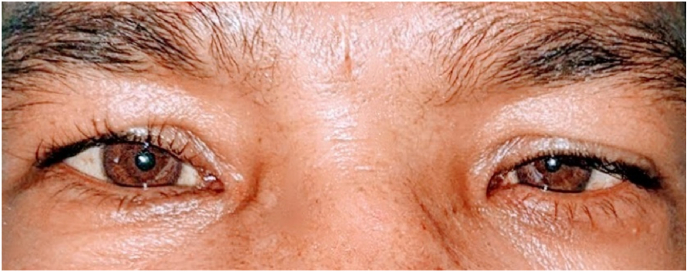
On neurological evaluation and physical examination, the patient had right-sided hemiparesis with motor power of 3/5, loss of pain and temperature on the right side of the body, increased deep tendon reflex (DTR), Babinski reflex positivity, and ataxia. A left-sided horizontal gaze-evoked nystagmus without ophthalmoplegia, Horner's syndrome (Fig. 1), and cerebellar dysarthria were also discovered. The finger-to-nose test demonstrated left-sided cerebellar symptoms. The diagnosis was further complicated by presence of UMN facial nerve palsy with partial upper eyelid ptosis on the left side of his face (Fig. 2).
Fig. 1.
Left side Horner's syndrome showing Miosis, Ptosis.
Fig. 2.
UMN type Facial Nerve Palsy.
The patient had an abnormal lipid profile and increased erythrocyte sedimentation rate (34mm/hr), but all other lab findings reported normal results, including the coagulation profile. A right dorsolateral medullary infarction was discovered during a MRI scan of the brain. In the magnetic resonance angiography (MRA) of the brain and neck arteries, PICA and the left vertebral artery were not visible (Fig. 3). Following the clinicoradiological evaluation, the patient was diagnosed with LMS.
Fig. 3.
T2-FLAIR MRI Demonstrating left dorsolateral medullary infarction (A) and MRA of the brain showing absence of left vertebral artery and PICA (B).
MRA: Magnetic Resonance Angiogram; PICA: Posterior Inferior Cerebellar Artery; FLAIR: Fluid Attenuated Inversion Recovery.
Carotid Doppler showed the course and caliber of the bilateral common carotid artery, carotid bulb, and internal carotid artery were narrowed and thickened, but no significant stenosis. The echocardiography demonstrated mild left ventricular wall thickness, Grade I diastolic dysfunction, normal ventricular wall motion, a 65% left ventricular ejection fraction, and no intracardiac clots or masses.
Thrombolysis wasn't done due to the late presentation(>4.5hr). He was managed conservatively with careful blood pressure control. A nasogastric tube was inserted to prevent aspiration due to dysphagia, and the patient received aspirin, clopidogrel, atorvastatin, amlodipine, and losartan. He had paroxysms of pain on the left side of his face at the ophthalmic, maxillary trigeminal nerve distributions, for which he was given pregabalin and amitriptyline; an antihistamine twice daily to control hiccups, as well as a fresh tear over the left eye. He reported less pain frequency and severity over a week. His symptoms improved after four weeks of medication, and he was discharged with a nasogastric tube and a strict physiotherapy training regime. There were no further pain episodes or facial deviation during the three-month period.
3. Discussion
Twenty percent of ischemic events in the brain involve posterior circulation (vertebrobasilar). LMS is the most common syndrome caused by occlusion of the intracranial vertebral artery, the PICA, followed by the medullary artery [6].
As we noted in our report, common vestibulocerebellar symptoms of LMS include nystagmus (horizontal and rotational), vertigo with falling to one side of the lesion, gait ataxia, and dysmetria [1,2]. Pain and temperature loss in the contralateral trunk/limbs (spinothalamic tract) and ipsilateral face (spinal trigeminal nucleus and tract) are among the sensory findings. Other signs of involvement of the nucleus ambiguous include ipsilateral bulbar muscular weakness (e.g., dysphagia, dysarthria, hoarseness) and autonomic dysfunction (e.g., ipsilateral Horner's syndrome, hiccups, and lack of autonomic respiration during sleep) [7].
Sensory symptoms can be explained by the involvement of the dorsal sensory root, formed by central axons that extend into the brainstem and divide into short ascending and long descending fibers. The short ascending fibers are afferent for touch, light pressure, and proprioception. Long ascending fibers carry pain and temperature sensations and extend to the upper cervical segment [8].
High blood pressure, diabetes, and smoking are the most common risk factors. LMS can also be caused by various conditions, such as Ehler-Danlos syndrome, Marfan syndrome, fibromuscular dysplasia, and vertebral artery dissection [9].
In this case, the contralateral hemiparesis can be explained by a caudal extension of the infarction to the pyramidal tract before the decussation at the medulla. Some studies have linked this weakness to the spinocerebellar hypotonic syndrome, while a positive Babinski reaction indicated pyramidal tract involvement in our case [3].
Our patient's UMN facial palsy could be caused by the involvement of Dejerine's aberrant pyramidal tract [10]. At the medulla, the hypothetical loop of supranuclear corticobulbar fibers descends ventromedially, decussate at the superior medulla, and then ascends dorsolaterally to reach the facial nerve nucleus [11].
4. Conclusions
Physicians should be aware of the most common manifestations of LMS, their appropriate management, and evaluation, including various atypical presentations. Regarding our case, UMN-type facial palsy with contralateral hemiparesis raised questions about a simple lateral medullary syndrome diagnosis. Furthermore, because there are few tertiary centers for neurological science in developing countries like ours, such presentations are frequently missed.
Ethical approval
The IRC of Upendra Devkota Memorial National Institute of neurological and Allied Sciences granted ethical approval for this study.
Please state any sources of funding for your research
No fund was obtained to support this case report.
Author contribution
RS, GK contributed to the study concept, data collection, manuscript outlining, writing, and revision. RP, NL and SA contributed to the study concept, and critical revision of the manuscript for content. GK contributed with supervision, and content revision. All named authors accept overall responsibility integrity of the work and have given final approval for its publication.
Please state any conflicts of interest
All authors must disclose any financial and personal relationships with other people or organisations that could inappropriately influence (bias) their work. Examples of potential conflicts of interest include employment, consultancies, stock ownership, honoraria, paid expert testimony, patent applications/registrations, and grants or other funding.
No conflicts of interest
No fund was obtained to support this case report.
Registration of research studies
-
1.
Name of the registry: NA
-
2.
Unique Identifying number or registration ID: NA
-
3.
Hyperlink to your specific registration (must be publicly accessible and will be checked): NA
Guarantor
Ramesh Shrestha.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Acknowledgments
We would like to thank all attending physicians from the Department of Neurology and Radiology Department at Upendra Devkota Memorial Neurological Institute and Allied Sciences.
Contributor Information
Ramesh Shrestha, Email: the1ramesh.stha@gmail.com.
Ghanshyam Kharel, Email: gskharel@gmail.com.
Shraddha Acharya, Email: acharya.shraddha54@gmail.com.
Rohit Pandit, Email: rpandit419@gmail.com.
Nitu Limbu, Email: nitulimbu76@gmail.com.
References
- 1.Saha R., Alam S., Hossain M.A. Lateral medullary syndrome (Wallenberg's Syndrome) - a Case Report. Faridpur Med. Coll. J. 2010;5(1):35–36. doi: 10.3329/fmcj.v5i1.6813. https://www.banglajol.info/index.php/FMCJ/article/view/6813 Available from: [DOI] [Google Scholar]
- 2.Kim J.S. Pure lateral medullary infarction: clinical–radiological correlation of 130 acute, consecutive patients. Brain. 2003 Aug 1;126(8):1864–1872. doi: 10.1093/brain/awg169. https://academic.oup.com/brain/article/126/8/1864/307992 Available from: [DOI] [PubMed] [Google Scholar]
- 3.Chakraborty U., Banik B., Chandra A., Pal J. An atypical manifestation of lateral medullary syndrome. Oxf. Med. Case Rep. 2019 Dec 31;2019(12):527–529. doi: 10.1093/omcr/omz139. https://academic.oup.com/omcr/article/2019/12/527/5691272 Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Terrence C., Costa R., Fromm G. An unusual case of paroxysmal facial pain. J. Neurol. 1979 Aug 1;221(2):73–76. doi: 10.1007/BF00313104. https://link.springer.com/article/10.1007/BF00313104 Available from: [DOI] [PubMed] [Google Scholar]
- 5.Agha R.A., Franchi T., Sohrabi C., Mathew G., Kerwan A., SCARE Group The SCARE 2020 Guideline: Updating Consensus Surgical CAse REport (SCARE) Guidelines. Int. J. Surg. Lond. Engl. 2020 Dec;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. https://pubmed.ncbi.nlm.nih.gov/33181358 Available from: [DOI] [PubMed] [Google Scholar]
- 6.Huynh T.R., Decker B., Fries T.J., et al. Lateral medullary infarction with cardiovascular autonomic dysfunction: an unusual presentation with review of the literature. Clin. Auton. Res. 2018;28:569–576. doi: 10.1007/s10286-018-0502-6. https://link.springer.com/article/10.1007/s10286-018-0502-6 Available from: [DOI] [PubMed] [Google Scholar]
- 7.Kk P., K R., P C, Aiyappan S.K., N D A Rare Variant of Wallenberg's Syndrome: Opalski syndrome. J. Clin. Diagn. Res.: J. Clin. Diagn. Res. 2014 Jul;8(7):MD05–6. doi: 10.7860/jcdr/2014/9547.4626. Available from: https://europepmc.org/article/PMC/4149101, PMID: 25177595; PMCID: PMC4149101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Notices of recent publications. Brain. 1939;62(Issue 1):125. doi: 10.1093/brain/62.1.125. [DOI] [Google Scholar]
- 9.Sacco R.L., Freddo L., Bello J.A., Odel J.G., Onesti S.T., Mohr J.P. Wallenberg's Lateral Medullary Syndrome: Clinical-Magnetic Resonance Imaging Correlations. Arch. Neurol. 1993 Jun 1;50(6):609–614. doi: 10.1001/archneur.1993.00540060049016. https://jamanetwork.com/journals/jamaneurology/article-abstract/592384 Available from: [DOI] [PubMed] [Google Scholar]
- 10.Campbell W.W., Barohn R.J. 2020. DeJong's the Neurologic Examination. [Google Scholar]
- 11.Srinivasan M., Bindu B., Gobinathan S., Balasubramanian S., Nithyanandam A., Shanbhogue K.R. An Unusual presentation Of Lateral Medullary Syndrome With Ipsilateral UMN Facial Palsy - An Anatomical Postulate. Ann. Indian Acad. Neurol. 2005 Jan 1;8(1):37. https://www.annalsofian.org/article.asp?issn=0972-2327;year=2005;volume=8;issue=1;spage=37;epage=40;aulast=srinivasan;type=0 Available from: [Google Scholar]