Abstract
Objectives
Preterm children are exposed to many medications in neonatal intensive care units, but little is known about the effect of prematurity on medication use throughout infancy and childhood. We examined prescriptions of cardiovascular medication (CVM), antiseizure medication (ASM), antiasthmatic medication and antibiotics issued/dispensed in the first 10 years of life for very and moderately preterm children compared with term.
Design
Population-based data linkage cohort study linking information from birth records to prescription records.
Setting
Six registries from five countries in the EUROlinkCAT study.
Participants
The study population included 1 722 912 children, of whom 10 820 (0.6%) were very preterm (<32 weeks gestational age (GA)), 92 814 (5.4%) were moderately preterm (32–36 weeks GA), 1 606 643 (93.3%) were born at term (≥37 weeks GA) and 0.7% had missing GA. Children with major or minor congenital anomalies were excluded (including patent ductus arteriosus).
Main outcome measures
Relative risk (RR) of receiving a prescription for CVM, ASM, antiasthmatic and antibiotics.
Results
Very preterm children had a higher RR of receiving a prescription for CVM and ASM than preterm children. For all preterm children, the RR of having a CVM prescription was 3.58 (95% CI 2.06 to 6.23); 2.06 (95% CI 1.73 to 2.41) for ASM; 1.13 (95% CI 0.99 to 1.29) for antiasthmatics and 0.96 (95% CI 0.93 to 0.99) for antibiotics in the first year of life. Increased prescription of CVM, ASM and antiasthmatics persisted for all 10 years of follow-up. Although the RR was highest for CVM and ASM, in absolute numbers more children received prescriptions for antibiotics (42.34%, 95% CI 38.81% to 45.91%) and antiasthmatics (28.40%, 95% CI 16.07% to 42.649%) than for CVM (0.18%, 95% CI 0.12% to 0.25%) and ASM (0.16%, 95% CI 0.13% to 0.20%) in the first year of life.
Conclusion
Preterm children had a higher risk of being prescribed/dispensed CVM, ASM and antiasthmatics up to age 10. This study highlights a need for further research into morbidity beyond age 10.
Keywords: NEONATOLOGY, Public health, Congenital heart disease
STRENGTHS AND LIMITATIONS OF THIS STUDY.
This is a population-based study including data on more than 100 000 children born preterm in six geographically different European regions.
With the high number of children included in our study we are able to report data on relatively infrequently prescribed medications such as antiseizure and cardiovascular medication.
The study includes data for the first 10 years of life and we are thus able to detect impacts of preterm birth extending into childhood.
An important limitation is that we do not have access to the medical files for included children and therefore we do not have information regarding the specific indication for which a medication was prescribed.
Introduction
Complications due to preterm birth, that is, before 37 completed weeks of gestation, is the leading cause of death for children under 5 years of age.1 In high-income countries close to 100% of babies born at a gestational age (GA) of 32 weeks are expected to survive infancy,2 but babies born extremely preterm (<28 weeks GA) and with low birth weight still have a mortality rate of 33%–50% in developed countries.3 The increased survival of children born preterm raises the question ‘does the increased survival come with the price of an increased morbidity in childhood compared with term born children?’. One such indicator of disease burden is prescription of medication, as this will reflect underlying disease. Although a number of studies have addressed prescriptions and use of medications in the neonatal intensive care unit (NICU), little is known about prescriptions after discharge. The few available studies have focused on prescriptions in the first year or two of life,4 5 but long-term follow-up is lacking. Life in the first year after discharge from the NICU is characterised by frequent paediatric visits and an average of 5.5 prescriptions per year.4 One study from the USA found that the most frequently prescribed medication in the first 2 years of life were palivizumab, ranitidine, albuterol, lansoprazole, budesonide and prednisolone.5 Of these medications only palivizumab has a specific indication in preterm infants, and concerns regarding safety and lack of efficacy have been raised for lansoprazole,6 ranitidine7 and budesonide.8 Most research has centred on prescriptions of these medications while for instance cardiovascular medication (CVM) and antiseizure medication (ASM) have received less research interest.
The aim of this study was to evaluate the community prescription of CVM, ASM, antiasthmatics and antibiotics to children born before 37 weeks GA compared with term children from birth up to 10 years of age, as an indicator of chronic disease burden. Furthermore, we aimed to look at differences in prescription of CVM between term (+37 weeks GA), moderately preterm (32–36 weeks GA) and very preterm (<32 weeks GA) children for their first 10 years of life in six different European regions.
Methods
This is a European, population-based linkage cohort study arising from the EUROlinkCAT project.9 The EUROlinkCAT project includes data on morbidity and medication use for children born with congenital anomalies and for reference children without congenital anomalies born in the same geographical area. In the present paper, we focus on these reference children. Five regions provided data on all liveborn children in their region and one region (Tuscany) provided a random 10% sample, matched on date of birth and sex, of their population of reference children. The minimum GA for inclusion was 23 weeks except for Wales where it was 24 weeks. Data were included for children born between 2000 and 2014, but three registries had a shorter study period as linked data in these regions were not available at the start of the study period (table 1).
Table 1.
Overview of the prescription databases from which data were extracted for the study and seize of the study population
| First year of birth | Source of prescriptions | No of children | ||||
| Reference population | <32 GA | 32–36 GA | +37 GA | |||
| Denmark: Funen* | 2000 | Dispensed by pharmacy | 72 290 | 525 | 4045 | 66 625 |
| Finland | 2000 | Dispensed by pharmacy | 755 923 | 4245 | 33 860 | 715 620 |
| Italy: Emilia Romagna | 2008 | Dispensed by pharmacy | 250 829 | 1902 | 16 350 | 232 507 |
| Italy: Tuscany | 2008 | Dispensed by pharmacy | 16 844 | 77 | 926 | 15 840 |
| Spain: Valencian Region | 2010 | Dispensed by pharmacy | 223 760 | 1173 | 14 618 | 202 304 |
| UK: Wales* | 2000 | Prescribed by GP | 403 265 | 2895 | 23 015 | 373 750 |
| Total no of children | 1 722 912 | 10 820 | 92 814 | 1 606 643 | ||
Information includes the source of prescription data (either community pharmacy or GP) and the number of children in each group. The reference population are children without congenital anomalies who were born term. For some databases numbers have been rounded to nearest five to insure anonymity.
GA, gestational age; GP, general practitioner.
Information on medication was available by linking children identified in birth records to local electronic prescription databases in each of the six regions. All children in the six regions needed to have a valid identification (ID) number to be identified in the relevant prescription database. Four regions had valid IDs for >99% of children, one region had valid IDs for 95% of children (Emilia Romagna), and one had valid IDs for 85% of children (Wales). The proportion was lower for Wales as information on prescriptions were obtained only from general practitioners who contributed to the Secure Anonymised Information Linkage database. In total, 1 722 912 children aged up to 10 years of age had a valid ID that allowed them to be identified in a prescribing database, between the years 2000 and 2015 (table 1).
Analyses were performed according to three age groups (<1 year, 1–4 years and 5–9 years). GA at birth was categorised as very preterm (<32 weeks GA), moderately preterm (32–36 weeks GA) and term births (37+ weeks GA).
Exclusions
Children with a code for a major or minor congenital anomaly in the hospital in-patient databases were excluded from the study population, that is, any child with a WHO International Statistical Classification of Diseases and Related Health Problems 9th revision (code with 74–75) or 10th Revision code (Q-chapter).10 This criteria also excluded children with a patent ductus arteriosus (PDA).
Minimum number of prescriptions
A child must have at least one prescription to be classified as exposed to a medication. In epidemiology, risk has been defined as ‘the probability of an event during a specified period of time’,11 and as such uses the term risk for the probability of receiving medication.
Small numbers
In two of the participating registries extraction of small numbers were not allowed, we, therefore, restricted the analysis to fourth level in the ATC system as outlined below.
Classification of medication
Cardiovascular medication
As previously described in detail in Damkjaer et al,12 antiarrhythmic medication is classified according to the Vaughan Williams classification (VWC).13 Antihypertensive medication and diuretics were classified according to the Anatomical Therapeutic Classification (ATC) system codes reported in the electronic prescription databases. In brief, this gave us the categories outlined below:
Any CVM: All ATC codes beginning with C01-C03 and C07-C09, excluding C01BA51, C01BA71, C01CA24
VWC1 (fast sodium-channel blockers) : ATC codes beginning with C01BA (excluding C01BA51 and C01BA71), C01BB and C01BC (ie, procainamide, lidocaine and flecanide).
VWC2 (beta-blockers): ATC codes beginning with C07A (ie, atenolol, propranolol).
VWC3 (potassium-channel blockers): ATC codes beginning with C01BD (ie, nefidipine).
VWC5 (other mechanism of action): ATC codes C01AA05 (ie, digoxin, adenosine).
Antihypertensives: ATC codes beginning with C08 and C09.
Diuretics: ATC codes beginning with C03.
ASM
Medication used for the treatment of epilepsy/seizures were stratified into four groups:
Any ASM: all medication included in the ATC system beginning with N03.
First generation ASM: ATC codes beginning with N03AA, N03AB, N03AE, N03AF (ie, phenobarbital, phenytoin, clonazepam, carbamazepine).
Second generation ASM: ATC codes beginning with N03AX (ie, lamotrigine, gabapentin, topiramate and levetiracetam).
Fatty acid derivatives (FAD): ATC codes beginning with N03AG (ie, valproic acid, valpromid, progabide).
Antiasthmatics
All medication used in the treatment of obstructive airway diseases as classified under ATC codes beginning with R03. These were divided into the following categories:
Antiasthmatic: ATC codes beginning with R03.
Beta-2-agonists: ATC codes beginning with R03AC, which comprises all inhaled selective beta-2-adrenoreceptor agonists (ie, salbutamol, terbutaline, fenoterol).
Glucocorticoids: ATC codes beginning with R03BA which includes all inhaled glucocorticoids (ie, beclometasone, budesonide, fluticasone) except combinations with adrenergics and anticholinergics which are classified under R02AK and R03AL.
Antibiotics
In this study, the broad term ‘antibiotics’ is used to cover all systemic antibacterials as defined by the ATC system using codes beginning with J01. All topical antibiotics (ointments/ creams) for skin infections, drops for eye or ear infections, antibiotics that are administered intravenously and antibiotics not classified under the ATC code J01 were not included. Medications were then stratified into three subgroups:
Any antibiotic: ATC codes J01.
Penicillins: ATC codes J01C (comprises both beta-lactamase sensitive and resistant penicillins plus combinations with beta-lactamase-inhibitors).
Macrolides: ATC codes J01F (also includes lincosamides and streptogramins).
Statistical methods
Each registry standardised their data using the EUROlinkCAT common data model,14 which enabled them to run a centrally written analysis script on their individual case data. The number of children prescribed/dispensed at least one prescription and the number of child years observed during each year of age were calculated in children according to GA at birth categorised into very preterm (GA <32 weeks), moderately preterm (GA 32–36 weeks) and term (GA 37+ weeks) and submitted to the central results repository at Ulster University (only aggregate data; no individual case data were provided to Ulster University). The aggregate results for all registries were then provided to the researchers. The risk of being prescribed/dispensed a medication at a particular year of age was calculated as the number of children prescribed/dispensed at least one prescription when they were that age divided by the number of child years observed during the same age year (to allow for children being censored during the year). The relative risks (RRs) of being prescribed/dispensed a medication in preterm children (<37 weeks GA) compared with in term children (37+ weeks GA) were calculated for each year of age within each registry. The data were then combined and analysed by performing an inverse variance random effects meta-analysis of the RR and 95% CIs of being prescribed/dispensed a medication at each year of age in preterm children (<37 weeks GA) group compared with the risk in term children (37+weeks GA). In addition the RR for <32 weeks GA and 32–36 weeks GA compared with term children (37+ weeks GA) were calculated within three age groups (<1 year, 1–4 years, 5–9 years). Three registries had no information on children over 7 years of age, as their data started in 2008 (Emilia Romagna and Tuscany) and 2010 (Valencian Region), so they were excluded from the 5–9 years’ analysis.9
Patient and public involvement
Patients/parents were not involved in the study design, however as part of the project we have plans for dissemination and knowledge exchange with parents as described in detail on our webpage15 and protocol paper.9
Results
Population characteristics
The study population included 1 722 912 children, of whom 10 820 (0.6%) were very preterm (<32 weeks GA), 92 814 (5.4%) were preterm (32–37 weeks GA), 1 606 643 (93.3%) were term (table 1) and 0.7% had missing GA in the databases (these were evenly distributed among participating regions).
CVM
Prescription of CVM at each year of age
The risk of receiving a CVM prescription for preterm children (<37 weeks GA) compared with term children was highest in the first year of life (RR 3.58, 95% CI 2.06 to 6.23) and slowly decreased for each consecutive year up to age 9 years (figure 1A). The percentages of preterm children receiving a CVM prescription were 0.18% (95% CI 0.12% to 0.25%) in the first year of life, 0.06% (95% CI 0.03% to 0.09%) for ages 1–4 years and 0.07% (95% CI 0.02 to 0.14) for ages 5–9 years (table 2).
Figure 1.
Relative risk (RR) of receiving a prescription for all preterm (<37 GA) vs term (+37 GA) children for their first 10 years of life. Data plotted are the RR and error bars indicated 95% CIs. Each point on the graph indicates a child year, that is, from age 0 until the day before turning 1 year are termed <1 and from one till the day before turning 2 is termed <2, etc. The dotted line indicates an RR of 1 which is that of term children. Data are shown for (A) cardiovascular medication (CVM); (B) antiseizure medication (ASM); (C) antiasthmatic medication and (D) antibiotics. The highest RR is observed for CVM in the first year of life. For CVM, ASM and antiasthmatics the RR remains elevated compared with term children for all 10 years included in the analysis. Centres with data on <1000 children <37 GA were excluded from the analysis; for the two first years of life data were included from all six regions, for ages 2 years to <6 years five regions, ages 6 to <8 years 4 regions and 8 to <10 years three regions. GA, gestational age.
Table 2.
Percentage of preterm (<37 GA) children with a prescription and relative risk for preterm (< 37 GA) vs term (+37 GA) children for receiving a prescription
| Medication | <1 year | 1–4 years | 5–9 years | |||
| Percentage of preterm (<37 GA) children with a prescription (N=103 634) | RR for preterm (< 37 GA) vs term (+37 GA) children | Percentage of preterm (<37 GA) children with a prescription (N=102 309) | RR for preterm (< 37 GA) vs term (+37 GA) children | Percentage of preterm (<37 GA) children with a prescription (N=60 489) | RR for preterm (< 37 GA) vs term (+37 GA) children | |
| Any CVM | 0.18 (0.12–0.25) | 3.58 (2.06–6.23) | 0.06 (0.03–0.09) | 2.05 (1.71–2.46) | 0.07 (0.02–0.14) | 1.43 (1.04–1.97) |
| Diuretics | 0.07 (0.01–0.16) | 7.19 (2.29–22.60) | 0.01 (0.01–0.02) | 3.29 (2.09–5.17) | 0.00 (0.00–0.00) | 2.35 (1.34–4.10) |
| Antihypertensives | 0.02 (0.00–0.03) | 2.34 (0.94–5.82) | 0.01 (0.01–0.03) | 1.66 (1.12–2.48) | 0.02 (0.01–0.03) | 1.68 (1.22–2.32) |
| VWC2 (beta-blockers) | 0.07 (0.05–0.09) | 2.82 (2.24–3.55) | 0.06 (0.03–0.09) | 2.12 (1.68–2.67) | 0.05 (0.01–0.18) | 1.32 (1.07–1.63) |
| Any ASM | 0.16 (0.13–0.20) | 2.06 (1.76–2.41) | 0.27 (0.22–0.32) | 1.77 (1.50–2.08) | 0.38 (0.31–0.46) | 1.59 (1.48–1.70) |
| New ASM | 0.02 (0.01–0.05) | 2.03 (1.44–2.85) | 0.08 (0.06–0.12) | 1.87 (1.50–2.35) | 0.13 (0.11–0.15) | 1.70 (1.43–2.02) |
| Old ASM | 0.08 (0.06–0.10) | 2.09 (1.67–2.61) | 0.07 (0.05–0.09) | 1.84 (1.32–2.58) | 0.11 (0.08–0.14) | 1.80 (1.35–2.38) |
| FAD | 0.07 (0.04–0.11) | 2.21 (1.78–2.74) | 0.17 (0.13–0.22) | 1.75 (1.53–2.00) | 0.22 (0.18–0.27) | 1.63 (1.50–1.78) |
| Any antiasthmatic | 28.40 (16.07–42.64) | 1.13 (0.99–1.29) | 25.67 (18.35–33.75) | 1.20 (1.04–1.37) | 12.84 (11.44–14.31) | 1.21 (1.07–1.36) |
| Beta-2-agonists | 14.83 (8.45–22.63) | 1.29 (1.06–1.56) | 14.93 (12.13–17.96) | 1.31 (1.14–1.51) | 7.77 (6.55–9.09) | 1.22 (1.10–1.36) |
| Glucocorticoids | 10.47 (2.70–22.47) | 1.41 (0.94–2.12) | 12.91 (6.54–21.04) | 1.34 (1.05–1.70) | 7.80 (5.94–9.87) | 1.28 (1.11–1.48) |
| Any antibacterial | 42.34 (38.81–45.91) | 0.96 (0.93–0.99) | 51.05 (47.63–54.46) | 1.02 (0.98–1.06) | 29.41 (26.42–32.49) | 1.02 (0.98–1.07) |
| Penicillins | 37.19 (33.58–40.88) | 0.95 (0.92–0.98) | 43.44 (41.72–45.16) | 1.03 (0.99–1.07) | 22.79 (21.67–23.94) | 1.03 (0.98–1.08) |
| Macrolides | 8.43 (5.94–11.30) | 0.95 (0.94–0.97) | 13.62 (9.76–18.01) | 1.07 (1.02–1.12) | 6.90 (4.84–9.30) | 1.06 (0.98–1.15) |
Data are shown in three age groups and for each class of medication. The total number of children being prescribed/dispensed medication is indicated by the N number. Due to small numbers data on VWC1, VWC3 and VWC5 are not available.
ASM, antiseizure medication; CVM, cardiovascular medication; FAD, fatty acid derivatives; GA, gestational age; RR, relative risk; VWC1, Vaughn Williams class 1.
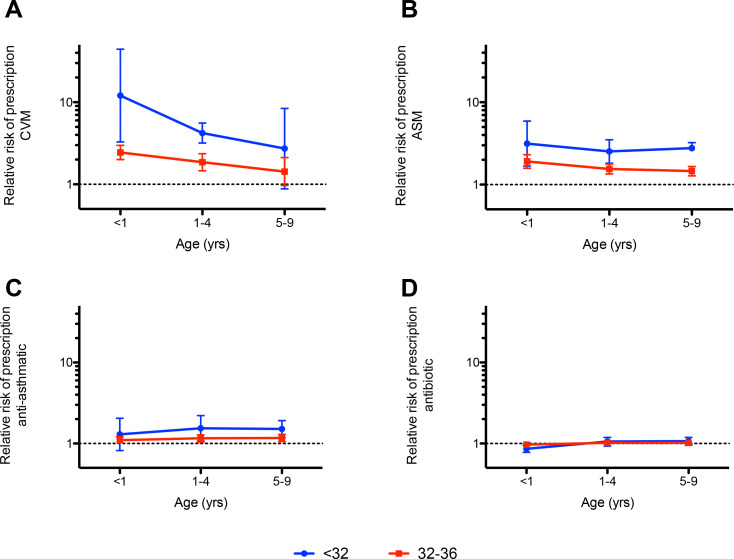
Impact of preterm birth on CVM prescriptions
A dose dependent effect was observed that is, the lower the GA at birth, the higher the RR of receiving a CVM prescription in their first year of life compared with term children. In very preterm children (<32 weeks GA), the RR was 12.06 (95% CI 3.28 to 44.35) and in moderately preterm (32–37 weeks GA) the RR was 2.44 (95% CI 2.00 to 2.98). The dose dependent effect of preterm birth on prescriptions of CVM was present across all age groups included in the study (figure 2A).
Figure 2.
Relative risk (RR) of receiving a prescription for very preterm (<32 GA, blue line) and preterm (32–36 GA, red line) vs term children in their 10 years of life. Data are pooled into three age categories; <1 years; 1–4 years and 5–9 years. Error bars indicated 95% CIs. The dotted line indicate an RR of 1 which is that of term children. Please note the logarithmic scale of the y-axis. Data are shown for (A) cardiovascular medication (CVM); (B) antiseizure medication (ASM); (C) antiasthmatic medication; (D) antibiotics. An increased relative risk of prescription is observed for CVM, ASM and antiasthmatic medication for the three age groups, but not for antibiotics. Centres with data on <1000 children <37 GA were excluded from the analysis; for the two first years of life data was included from all six regions, for ages 2 to <6 years five regions, ages 6 to <8 years 4 regions and 8 to <10 years three regions. GA, gestational age.
Pharmacological types of CVM prescribed/dispensed
VWC2 (beta-blockers): The RR for receiving a VWC2 prescription in preterm vs term children, was 2.82 (95% CI 2.24 to 3.55) in the first year of life, 2.12 (95% CI 1.68 to 2.67) for ages 1–4 years and 1.32 (95% CI 1.07 to 1.63) for ages 5–9 years. The percentage of preterm children receiving a beta-blocker in their first year of life was 0.07% (95% CI 0.05% to 0.09%).
Diuretics
The RR of having a diuretic prescribed/dispensed was highest in the first year of life (RR 7.19; 95% CI 2.29 to 22.60) and then decreased for ages 1–4 years (RR 3.29; 95% CI 2.09 to 5.17) and 5–9 years (RR 2.35; 95% CI 1.34 to 4.10). The percentage of preterm children receiving a diuretic in their first year of life was 0.07% (95% CI 0.01% to 0.16%).
Antihypertensives
Prescriptions for antihypertensives remained stable at an RR of around 2 for all three age groups, that is, 2.34 (95% CI 0.94 to 5.82), 1.67 (95% CI 1.12 to 2.48) and 1.68 (95% CI 1.22 to 2.32) for ages <1, 1–4 and 5–9 years, respectively. The percentage of preterm children receiving antihypertensive prescriptions in their first year of life was 0.02% (95% CI 0.00% to 0.03%).
VWC1, VWC3, VWC5: numbers were too small to report.
Regional differences in prescription
Figure 3A displays the RR of receiving a CVM prescription in the first year of life for each of the regions included in the meta-analysis reported above. A significantly increased RR was observed for five of the six regions (range of RR 2.18–8.70) with the exception of Tuscany where there was no increased RR and the CIs were extremely wide.
Figure 3.
Relative risk (RR) of receiving a prescription for all preterm (<37 GA) vs term (+37GA) children in the first year of life. Error bars indicate 95% CIs. Data are shown for all of the six regions individually (black) and the total (red) for (A) cardiovascular medication (CVM); (B) antiseizure medication (ASM); (C) antiasthmatic medication and (D) antibiotics. Please note the logarithmic scale of the x-axis in the upper panel, while in the lower panel the scale is linear but the x-axis values varies between graphs. GA, gestational age.
Antiseizure medication
Prescriptions of ASM at each year of age
At each individual year of age during the 10-year follow-up period, prescriptions of ASM were higher for preterm (<37 weeks GA) than for term children. The RR decreased with age, but prescriptions remained significantly higher for preterm than term children (figure 1B). The percentages of preterm children receiving a prescription in a year increased with age from 0.16% (95% CI 0.13% to 0.20%) for ages <1 year, 0.27% (95% CI 0.22% to 0.32%) for ages 1–4 years to 0.38% (95% CI 0.31% to 0.46%) for ages 5–9 years (table 2).
Impact of preterm birth on ASM prescription
In the first year of life children born very preterm (<32 weeks GA) and moderately preterm (32–36 weeks GA) had a higher RR of being prescribed/dispensed an ASM compared with term children (RR 3.15, 95% CI 1.68 to 5.90 and RR 1.91, 95% CI 1.58 to 2.31). The effect of increased prescription with lower GA was seen across all age groups (figure 2B).
Pharmacological types of ASM prescribed/dispensed
The same pattern of an increased RR at around 2 of being prescribed/dispensed an ASM was observed for all three pharmacological types of ASM (first/second generation and FAD) for the first 10 years of life. There was an increase in percentage of children receiving a prescription with age for all three age groups (for details, please see table 2).
Regional differences in prescription
An increased risk for preterm children compared with term children was observed across all six regions (RR range 1.41–2.43, figure 3B), although for both Italian regions the increase was not statistically significant.
Antiasthmatics
Prescription of antiasthmatics at each year of age for all preterm born children (<37 weeks GA)
For all preterm children, the RR of being prescribed/dispensed a prescription for antiasthmatic medication was significantly higher than for term children for all 10 years of follow-up. The RR was relatively stable around 1.2 for all 10 years (figure 1C).
Impact of prematurity on antiasthmatic prescription
There was no discernible dose dependent effect of prematurity on prescription of antiasthmatic medication, that is, for both very preterm and moderately preterm children the RR for prescription of antiasthmatics in the three different age categories remained around 1.3 (figure 2C). In total 28% of all preterm born children received a prescription for any antiasthmatic medication in the first year of life.
Pharmacological types of antiasthmatics prescribed/dispensed
Beta-2-agonists: The RR for receiving or having a prescription for a beta-2-agonist was around 1.3 for all age categories, that is, 1.29 (95% CI 1.06 to 1.56) for ages <1 years, 1.31 (95% CI 1.14 to 1.51) for ages 1–4 years and 1.22 (95% CI 1.10 to 1.36) for ages 4–9 years.
Glucocorticoids: The RR for being prescribed/dispensed a prescription for a beta-2-agonist was around 1.3 for all age categories, that is, 1.41 (95% CI 0.94 to 2.12) for ages <1 years, 1.34 (95% CI 1.05 to 1.70) for ages 1–4 years and 1.28 (95% CI 1.11 to 1.48) for ages 4–9 years.
Regional differences in prescription: In three of six regions (UK: Wales, DK: Funen and Finland) there was a significantly increased RR of prescription for preterm children in the first year of life, whereas in the three other regions no significant difference between term and preterm children was observed (figure 3C).
Antibiotics
Prescription of antibiotics at each year of age: The RR of preterm children having an antibiotic prescription issued/dispensed compared with term children was slightly lower in the first year of life. There were no significant differences in risk between preterm and term children during the next 9 years of follow-up (figure 1D).
Impact of preterm birth on prescriptions for antibiotics: In the first year of life children born very preterm (<32 weeks GA) and moderately preterm (32–36 weeks GA) had a lower RR of receiving a prescription for antibiotics than term children (RR 0.86, 95% CI 0.78 to 0.95 and RR 0.97, 95% CI 0.95 to 1.00). For the age categories 1–4 years and 5–9 years, there was no difference in prescriptions compared with term children. Furthermore, we did not observe a dose dependent effect of preterm birth on prescription, that is, no effect of decreasing GA on RR for prescription (figure 2D).
Pharmacological types of antibiotics prescribed/dispensed
Any antibiotics: 42.34% (95% CI 38.81% to 45.91%) received a prescription in their first year of life, 51.05% (95% CI 47.63% to 54.46%) were issued/dispensed a prescription each year for ages 1–4 years and 29.41% (95% CI 26.42% to 32.49%) each year for ages 5–9 years.
Penicillins: were prescribed/dispensed for 37.19% (95% CI 33.58% to 40.88%) of children <1 years, 43.44% (95% CI 41.72% to 45.16%) had a penicillin prescription each year for ages 1–4 years and 22.79% (95% CI 21.67% to 23.94%) each year for ages 5–9 years.
Macrolides: 8.43% (95% CI 5.94% to 11.30%) received a prescription in their first year of life, 13.62 (95% CI 9.76 to 18.01) were issued/dispended a prescription for macrolides each year for ages 1–4 years and 6.90% (95% CI 4.84% to 9.30%) each year for ages 5–9 years.
Regional differences in prescription: A significantly decreased RR for prescription of antibiotics was observed in four of six regions (figure 3D).
Discussion
To our knowledge, this is the first study to examine medications prescribed/dispensed for cardiovascular diseases, neurological seizures, asthma and infections in a paediatric cohort comparing preterm and term born children up to ten years of age. We show that children born preterm had an increased risk compared with term children of being prescribed/dispensed CVM, ASM and antiasthmatic medication. For CVM and ASM, risks were higher for earlier gestations. For CVM, the increased RR was most pronounced in the first year of life, whereas for ASM the risk was at a constant level for the first 10 years of life. Although the RR was highest for CVM and ASM, in absolute numbers more children were receiving prescriptions for antibiotics and antiasthmatics than for CVM and ASM. In the first year of life preterm children had a reduced RR for receiving antibiotics compared with term children.
An important limitation of our study is that all preterm children with a code for PDA are excluded as we excluded all children with congenital anomalies as defined in the method section. There is an inverse relationship between GA and PDA, such that the more preterm an infant is born the higher the probability that arterial duct will not close spontaneously.16 Furthermore, it has been established that having a PDA is associated with prolonged mechanical ventilation, bronchopulmonary BPD and necrotising enterocolitis.16 17 Therefore, the net effect of excluding infants with a PDA is that we may be underestimating the true burden of morbidity for the group of preterm born children. Also this study only assesses prescription patterns, and as such we are not able to assess whether or not medication are prescribed rationally in accordance with the current standards of evidence, further studies are need to address this question.
Cardiovascular medication
The highest RR in this study was for diuretics in the first year of life. Although the RR was higher for preterm children with respect to all CVM, it is important to note that in absolute terms few children were prescribed these medications. In preterm born children, development of BPD is the most frequent chronic morbidity and strongly predicts both death and disability in childhood.18–20 The most regularly prescribed medication to infants admitted with an exacerbation in BPD is diuretics21 and as much as 86% of infants admitted for BPD exacerbation will follow a treatment course for >5 days with diuretics.22 It therefore seems plausible that the high RR for diuretics in the first year of life most likely reflects either chronic treatment for BPD or shorter periods given in relation to exacerbations in BPD. However, there is a lack of evidence on the efficacy of diuretics in preterm children. For example, a Cochrane review examining the risks and benefits of administration of diuretics (furosemide) to preterm children in the NICU at a postmenstrual age <40 weeks with ongoing or incipient chronic lung disease found that ‘furosemide administration has either inconsistent effects or no detectable effect’.23 There are no systematic reviews for long-term use of diuretics to infants/children after discharge from the NICU. In view of this, it is noteworthy that we in this study find that there is an increased prescription of diuretics to preterm born children up to 10 years of age. The increased RR for prescription of antihypertensives (which includes ACE inhibitors) and beta-blockers could reflect chronic heart failure treatment as these are recommended first-line therapies for paediatric heart failure.24 As with diuretics for BPD heart failure treatment in adults with congenital heart defects are generally based on position statements rather than solid evidence,25 a problem that ‘is even more pertinent in children’.26 The few available studies on heart failure treatments in children have either failed to show an effect or have been underpowered.27–29 Future studies are needed to address whether or not these patterns of increased prescription of CVM can affect clinical course or outcome in preterm children.
Antiseizure medication
Increased prescription of ASM probably reflects an increased risk for epilepsy among preterm born children. It has previously been shown that there is an inverse dose-response curve with decreasing GA increasing epilepsy risk later in life,30 a phenomenon we also observe in our data. A recent meta-analysis estimated that the increased OR for epilepsy for children born preterm versus term was 2.14 which is consistent with our estimates of increased ASM prescription.31 It is noteworthy, in our data, that while the RR for ASM prescription was relatively stable over the age groups, in absolute terms the number of children receiving treatment roughly doubles from <1 years of age to the age group 5–9 years. The cumulative incidence of epilepsy increases through childhood,32 but it seems that the extra RR conferred by preterm birth is present for at least 10 years after birth. Randomised controlled trials on management of epilepsy in infants are lacking, and as pointed ‘There is no high-level evidence to support any particular current agents for use in infants with seizures’.33 Treatment strategies are thus based on expert opinion rather than solid evidence.34 In this study the RR for prescription of both first/second generation ASM and FAD are remarkably similar, suggesting that no group is preferred specifically for the epilepsy forms associated with preterm birth. Again studies of medication efficacy are warranted in this patient group.
Antiasthmatic medication
Preterm birth has been associated with an increased risk of childhood asthma or wheezing disorder with an increased OR of 1.46,35 although considerable heterogeneity across studies have been noted.36 A Danish cohort study reported a strong inverse association with GA and purchase of antiasthmatics (defined as purchasing both an inhaled beta-2-agonist and glucocorticoids) and found that OR decreased as the age of children increased.37 The waning effect of preterm birth with advancing age has later been shown to progress beyond 11 years of age.38 In this study, preterm birth is associated with an increased risk of being prescribed/dispensed antiasthmatics at an RR around 1.2 which is similar to that reported in the Danish study, although we did not observe a waning effect with age for the 10 years follow-up after birth. In absolute numbers 28% of preterm children are prescribed antiasthmatics in their first year of life which then declines to around 13% for ages 5–9 years, so although the RR is lower than for CVM and ASM in absolute numbers far more children were prescribed antiasthmatics than CVM and ASM. Prescriptions of inhaled beta-2-agonist and glucocorticoids in our study were not substantially different and seems to suggest that children, if treated with antiasthmatics, are treated with both.
Antibiotics
This study did not find a dose dependent effect of preterm birth on RR for prescription of antibiotics. Lorch et al looked at the effect of GA on antibiotic prescription in children born <32 weeks GA for the first year of life and did not find an effect of GA on prescription of antibiotics for very preterm born infants.39 In contrast, it has been reported for children from 2 years of age and older that lower GA resulted in higher prescription rates of antibiotics up until ages 10–11 years where an inverse pattern was observed with decreasing prescription.40 The authors reported a similar pattern with respect to hospital admission for airway infections.40 Several studies have reported higher rates of admissions for respiratory infections both in infancy and childhood for preterm born children.41–43 The study by Lorch et al did not include a control group, and their finding of lower prescription rates cannot be corroborated by other studies. The higher rates of hospitalisations due to infections for preterm born infants and children reported by other studies might provide some part of the explanation for our data. Our study included prescriptions for children outside hospitals only as we did not include medication given during hospital admissions. Further, preterm born infants stay in hospital for up to 3 months after birth and therefore they are less ‘exposed’ to prescriptions (as defined in our study) in the first year of life. It is also possible that the lower RR in the first year of life reflects that preterm children are kept more at home and shielded from infections than term children. In teenagers it has been suggested that there is an ex-preterm behavioural phenotype44 that may lead to a more socially isolated life-style with less exposure to infections.40 It can be speculated that there might be a similar behavioural pattern in parents during infancy.
Regional differences
Overall we observed similar trends across all six European regions included in this study. As there is considerable overlap of confidence intervals between various European regions we cannot for certain identify clinically relevant differences in prescription between geographical regions. Due to a small sample from Tuscany, this subcohort failed to find any differences in prescription patterns for preterm vs term born children.
Conclusion
Children born preterm are at a higher risk of being prescribed/dispensed prescriptions for CVM, ASM and antiasthmatic medication in their first 10 years of life. The higher risk was also present for the moderate preterm born children. While it is known that children born preterm are vulnerable, this study demonstrates that these children have an excess risk of chronic diseases requiring medication up to age 10 years. Future studies should assess if the excess morbidity associated with preterm birth continues into adolescence/young adulthood or if it levels off after ten years of age. Preterm born infants have a long life a head of them when they start out the PICU. Optimisation of management though infancy and childhood can have profound consequence of quality of life for many years to come, in light of this it seems peculiar that so little of the current prescription practice for ex-preterm infants and children are based on solid scientific evidence.
Supplementary Material
Footnotes
Contributors: MD: wrote first draft of the paper and revised the paper after feedback and responsible for the overall content of the paper. ML: Extraction and analysis of local registry data. Part of steering group and helped design of the study. Gave continuous input in the process of drafting the paper. SKU: extraction and analysis of local registry data. Gave continuous input in the process of drafting the paper. EB: extraction and analysis of local registry data. Gave continuous input in the process of drafting the paper. CC-C: Extraction and analysis of local registry data. Gave continuous input in the process of drafting the paper. AC: Extraction and analysis of local registry data. Gave continuous input in the process of drafting the paper. LG-V: Extraction and analysis of local registry data. Gave continuous input in the process of drafting the paper. JEG: Extraction and analysis of local registry data. Gave continuous input in the process of drafting the paper. MG: Extraction and analysis of local registry data. Gave continuous input in the process of drafting the paper. AH: Extraction and analysis of local registry data. Gave continuous input in the process of drafting the paper. SJ: Extraction and analysis of local registry data. Gave continuous input in the process of drafting the paper. AN: Extraction and analysis of local registry data. Gave continuous input in the process of drafting the paper. AP: Extraction and analysis of local registry data. Gave continuous input in the process of drafting the paper. JT: Extraction and analysis of local registry data. Gave continuous input in the process of drafting the paper. IS: Extraction and analysis of local registry data. Gave continuous input in the process of drafting the paper. Gave continuous input in the process of drafting the paper. EG: Extraction and analysis of local registry data. Part of steering group and helped design of the study. Gave continuous input in the process of drafting the paper. JKM: Extraction and analysis of local registry data and meta-analysis of pooled data from each individual registry. Help revised paper. Part of steering group who designed the study.
Funding: This project has received funding from the European Union’s Horizon 2020 research and innovation programme under grant agreement No. 733001. The views presented here are those of the authors only, and the European Commission is not responsible for any use that may be made of the information presented here.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
No data are available. A condition for local ethics approval for linking databases are that we are not allowed to share data.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
All registries that are part of the EUROCAT network have the required ethics permissions and procedures for routine surveillance, data collection and transmission of anonymised data to the EUROCAT central database. In accordance with national guidelines, the registries submitted evidence of these permissions to the EUROlinkCAT ethics portfolio. The central data repository Ulster University also obtained ethics approval (approval number FCNUR-21-060). Local registries follow national legislation as to whether parental consent is needed for registration of babies with anomalies. For details please refer to separate protocol paper.
References
- 1. Liu L, Oza S, Hogan D, et al. Global, regional, and national causes of under-5 mortality in 2000-15: an updated systematic analysis with implications for the sustainable development goals. Lancet 2016;388:3027–35. 10.1016/S0140-6736(16)31593-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Manuck TA, Rice MM, Bailit JL, et al. Preterm neonatal morbidity and mortality by gestational age: a contemporary cohort. Am J Obstet Gynecol 2016;215:103.e1–103.e14. 10.1016/j.ajog.2016.01.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Glass HC, Costarino AT, Stayer SA, et al. Outcomes for extremely premature infants. Anesth Analg 2015;120:1337–51. 10.1213/ANE.0000000000000705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wade KC, Lorch SA, Bakewell-Sachs S, et al. Pediatric care for preterm infants after NICU discharge: high number of office visits and prescription medications. J Perinatol 2008;28:696–701. 10.1038/jp.2008.74 [DOI] [PubMed] [Google Scholar]
- 5. Levin JC, Beam AL, Fox KP, et al. Medication utilization in children born preterm in the first two years of life. J Perinatol 2021;41:1732–8. 10.1038/s41372-021-00930-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Orenstein SR, Hassall E, Furmaga-Jablonska W, et al. Multicenter, double-blind, randomized, placebo-controlled trial assessing the efficacy and safety of proton pump inhibitor lansoprazole in infants with symptoms of gastroesophageal reflux disease. J Pediatr 2009;154:514–20. 10.1016/j.jpeds.2008.09.054 [DOI] [PubMed] [Google Scholar]
- 7. Santana RNS, Santos VS, Ribeiro-Júnior RF, et al. Use of ranitidine is associated with infections in newborns hospitalized in a neonatal intensive care unit: a cohort study. BMC Infect Dis 2017;17:375. 10.1186/s12879-017-2482-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Shah VS, Ohlsson A, Halliday HL, et al. Early administration of inhaled corticosteroids for preventing chronic lung disease in very low birth weight preterm neonates. Cochrane Database Syst Rev 2017;1:Cd001969. 10.1002/14651858.CD001969.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Morris JK, Garne E, Loane M, et al. EUROlinkCAT protocol for a European population-based data linkage study investigating the survival, morbidity and education of children with congenital anomalies. BMJ Open 2021;11:e047859. 10.1136/bmjopen-2020-047859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. EUROCAT . Minor anomalies and other conditions for exclusion. Available: https://eu-rd-platform.jrc.ec.europa.eu/sites/default/files/JRC-EUROCAT-Section-3.2-23-9-2020.pdf
- 11. Cole SR, Hudgens MG, Brookhart MA, et al. Risk. Am J Epidemiol 2015;181:246–50. 10.1093/aje/kwv001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Damkjaer M, Urhoj SK, Tan J, et al. Prescription of cardiovascular medication in children with congenital heart defects across six European regions from 2000 to 2014: data from the EUROlinkCAT population-based cohort study. BMJ Open 2022;12:e057400. 10.1136/bmjopen-2021-057400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Fuster V, Rydén LE, Cannom DS, et al. [ACC/AHA/ESC 2006 guidelines for the management of patients with atrial fibrillation--excutive summary]. Rev Port Cardiol 2007;26:383–446. [PubMed] [Google Scholar]
- 14. Loane M, Densem J, Given J. EUROlinkCAT common data model: morbidity 2022. 10.12140/RG2.2.29365.9484 [DOI]
- 15. EUROlinkCAT . Parents area, 2017. Available: https://www.eurolinkcat.eu/*parentsarea*
- 16. de Klerk JCA, Engbers AGJ, van Beek F, et al. Spontaneous closure of the ductus arteriosus in preterm infants: a systematic review. Front Pediatr 2020;8:541. 10.3389/fped.2020.00541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Terrin G, Di Chiara M, Boscarino G, et al. Morbidity associated with patent ductus arteriosus in preterm newborns: a retrospective case-control study. Ital J Pediatr 2021;47:9. 10.1186/s13052-021-00956-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Patel RM, Kandefer S, Walsh MC, et al. Causes and timing of death in extremely premature infants from 2000 through 2011. N Engl J Med 2015;372:331–40. 10.1056/NEJMoa1403489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Schmidt B, Asztalos EV, Roberts RS, et al. Impact of bronchopulmonary dysplasia, brain injury, and severe retinopathy on the outcome of extremely low-birth-weight infants at 18 months: results from the trial of indomethacin prophylaxis in preterms. JAMA 2003;289:1124–9. 10.1001/jama.289.9.1124 [DOI] [PubMed] [Google Scholar]
- 20. Gough A, Spence D, Linden M, et al. General and respiratory health outcomes in adult survivors of bronchopulmonary dysplasia: a systematic review. Chest 2012;141:1554–67. 10.1378/chest.11-1306 [DOI] [PubMed] [Google Scholar]
- 21. Bamat NA, Kirpalani H, Feudtner C, et al. Medication use in infants with severe bronchopulmonary dysplasia admitted to United States children's hospitals. J Perinatol 2019;39:1291–9. 10.1038/s41372-019-0415-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Slaughter JL, Stenger MR, Reagan PB. Variation in the use of diuretic therapy for infants with bronchopulmonary dysplasia. Pediatrics 2013;131:716–23. 10.1542/peds.2012-1835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Stewart A, Brion LP. Intravenous or enteral loop diuretics for preterm infants with (or developing) chronic lung disease. Cochrane Database Syst Rev 2011;9:CD001453. 10.1002/14651858.CD001453.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Masarone D, Valente F, Rubino M, et al. Pediatric heart failure: a practical guide to diagnosis and management. Pediatr Neonatol 2017;58:303–12. 10.1016/j.pedneo.2017.01.001 [DOI] [PubMed] [Google Scholar]
- 25. Baumgartner H, De Backer J, Babu-Narayan SV. 2020 ESC guidelines for the management of adult congenital heart disease: the task force for the management of adult congenital heart disease of the European Society of cardiology (ESC). endorsed by: association for European paediatric and congenital cardiology (AEPC), International Society for adult congenital heart disease (ISACHD). European Heart Journal 2020;42:563–645. 10.1093/eurheartj/ehaa554 [DOI] [Google Scholar]
- 26. Damkjær M, Poulsen CB, Wang T. Douglas ADAMs and the question of arterial blood pressure in mammals. Acta Physiol 2020;228:e13452. 10.1111/apha.13452 [DOI] [PubMed] [Google Scholar]
- 27. Alabed S, Sabouni A, Al Dakhoul S, et al. Beta-Blockers for congestive heart failure in children. Cochrane Database Syst Rev 2020;7:Cd007037. 10.1002/14651858.CD007037.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Shaddy RE, Boucek MM, Hsu DT, et al. Carvedilol for children and adolescents with heart failure: a randomized controlled trial. JAMA 2007;298:1171–9. 10.1001/jama.298.10.1171 [DOI] [PubMed] [Google Scholar]
- 29. Elkiran O, Sandikkaya A, Kocak G, et al. Evaluation by N-terminal prohormone of brain natriuretic peptide concentrations and Ross scoring of the efficacy of digoxin in the treatment of heart failure secondary to congenital heart disease with left-to-right shunts. Pediatr Cardiol 2013;34:1583–9. 10.1007/s00246-013-0683-7 [DOI] [PubMed] [Google Scholar]
- 30. Hirvonen M, Ojala R, Korhonen P, et al. The incidence and risk factors of epilepsy in children born preterm: a nationwide register study. Epilepsy Res 2017;138:32–8. 10.1016/j.eplepsyres.2017.10.005 [DOI] [PubMed] [Google Scholar]
- 31. Li W, Peng A, Deng S, et al. Do premature and postterm birth increase the risk of epilepsy? an updated meta-analysis. Epilepsy Behav 2019;97:83–91. 10.1016/j.yebeh.2019.05.016 [DOI] [PubMed] [Google Scholar]
- 32. Aaberg KM, Gunnes N, Bakken IJ, et al. Incidence and prevalence of childhood epilepsy: a nationwide cohort study. Pediatrics 2017;139:e20163908. 10.1542/peds.2016-3908 [DOI] [PubMed] [Google Scholar]
- 33. Wilmshurst JM, Gaillard WD, Vinayan KP, et al. Summary of recommendations for the management of infantile seizures: Task force report for the ILAE Commission of pediatrics. Epilepsia 2015;56:1185–97. 10.1111/epi.13057 [DOI] [PubMed] [Google Scholar]
- 34. Wheless JW, Clarke DF, Arzimanoglou A, et al. Treatment of pediatric epilepsy: European expert opinion, 2007. Epileptic Disord 2007;9:353–412. 10.1684/epd.2007.0144 [DOI] [PubMed] [Google Scholar]
- 35. Been JV, Lugtenberg MJ, Smets E, et al. Preterm birth and childhood wheezing disorders: a systematic review and meta-analysis. PLoS Med 2014;11:e1001596. 10.1371/journal.pmed.1001596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Castro-Rodriguez JA, Forno E, Rodriguez-Martinez CE, et al. Risk and protective factors for childhood asthma: what is the evidence? J Allergy Clin Immunol Pract 2016;4:1111–22. 10.1016/j.jaip.2016.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Damgaard AL, Hansen BM, Mathiasen R, et al. Prematurity and prescription asthma medication from childhood to young adulthood: a Danish national cohort study. PLoS One 2015;10:e0117253. 10.1371/journal.pone.0117253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Damgaard ALdeB, Gregersen R, Lange T, et al. The increased purchase of asthma medication for individuals born preterm seems to wane with age: a register-based longitudinal national cohort study. PLoS One 2018;13:e0199884. 10.1371/journal.pone.0199884 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Lorch SA, Wade KC, Bakewell-Sachs S, et al. Antibiotic use in premature infants after discharge from the neonatal intensive care unit. Clin Pediatr 2010;49:249–57. 10.1177/0009922809336358 [DOI] [PubMed] [Google Scholar]
- 40. Garioud ALdeB, Skoven FH, Gregersen R, et al. The increased susceptibility to airway infections after preterm birth does not persist into adolescence. PLoS One 2020;15:e0238382. 10.1371/journal.pone.0238382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Haataja P, Korhonen P, Ojala R, et al. Hospital admissions for lower respiratory tract infections in children born moderately/late preterm. Pediatr Pulmonol 2018;53:209–17. 10.1002/ppul.23908 [DOI] [PubMed] [Google Scholar]
- 42. Miller JE, Hammond GC, Strunk T, et al. Association of gestational age and growth measures at birth with infection-related admissions to hospital throughout childhood: a population-based, data-linkage study from Western Australia. Lancet Infect Dis 2016;16:952–61. 10.1016/S1473-3099(16)00150-X [DOI] [PubMed] [Google Scholar]
- 43. Rona RJ, Gulliford MC, Chinn S. Effects of prematurity and intrauterine growth on respiratory health and lung function in childhood. BMJ 1993;306:817–20. 10.1136/bmj.306.6881.817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Johnson S, Marlow N. Preterm birth and childhood psychiatric disorders. Pediatr Res 2011;69:11R–18. 10.1203/PDR.0b013e318212faa0 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No data are available. A condition for local ethics approval for linking databases are that we are not allowed to share data.