Abstract
OBJECTIVES:
As hospitals rapidly implement mechanical thrombectomy (MT) into stroke protocols following the pivotal trials in 2015, access to and outcomes from MT may be poorer for weekend-admitted patients. We sought to investigate whether a “weekend effect” influences MT outcomes nationally.
MATERIALS AND METHODS:
We identified stroke patients from 2010–2014 (pre-trials) to 2015–2017 (posttrials) using the Nationwide Readmissions Database. On multivariate analyses, we determined factors independently associated with receiving MT. Among MT patients, we then determined whether weekend admission was independently associated with inpatient mortality and unfavorable discharge.
RESULTS:
We identified 2,121,462 patients from 2010 to 2014, of whom 1.11% of weekday-admitted and 1.08% of weekend-admitted patients underwent MT. Of the 1,286,501 patients identified from 2015 to 2017, MT was performed in 2.82% and 2.91%, respectively. In the earlier cohort, weekend admission was independently associated with reduced odds of MT (odds ratio [OR] = 0.92, 95% confidence interval [CI]: 0.89–0.95, P < 0.0001), although this was not statistically significant in the later cohort. During both periods, age >80 years was independently associated with a reduced likelihood of receiving MT, and status as a teaching or large bed-size hospital was associated with a greater likelihood. Weekend admission was independently associated with unfavorable discharge only in the 2015–2017 cohort (OR = 1.11, 95% CI: 1.02–1.22, P = 0.02).
CONCLUSIONS:
While nationwide access to MT has improved for weekend-admitted patients, the elderly and those at smaller, nonteaching hospitals remain underserved. Although we found no effect of weekend admission on inpatient mortality, since the major shift in practice, an emerging “weekend effect” may influence discharge outcomes. Data suggest that some hospitals are being challenged to provide this new standard of care efficiently and equitably.
Keywords: Acute ischemic stroke, large-vessel occlusion, mechanical thrombectomy, weekend effect
Introduction
The “weekend effect” theory posits that the quality of care, and resulting outcomes, are poorer for patients admitted during the weekend than those admitted during the weekday.[1] Data from multiple specialties have shown that weekend-admitted patients have greater morbidity and mortality.[1,2,3,4] Evidence of a weekend effect has been shown in the treatment of acute ischemic stroke (AIS), both in the U. S. and internationally,[5,6,7,8,9] including older data on outcomes after mechanical thrombectomy (MT).[10] However, nationally representative data that reflect the recent, widespread implementation of MT into hospital stroke protocols has been lacking.[11,12]
In 2015, the American Heart Association/American Stroke Association (AHA/ASA) strongly recommended MT for patients with anterior circulation, large-vessel occlusions (LVOs),[13] after several landmark studies had demonstrated a significant benefit in functional outcomes.[14,15,16,17,18] As MT then became the standard of care, hospitals have assiduously sought to become Thrombectomy-Capable Stroke Centers (TSCs).[11,19] The time-sensitive nature of performing an MT, as well as the potential financial benefit from obtaining TSC certification, have incentivized hospitals to streamline their stroke protocols by eliminating any delays or inequities in quality of care.[11,19,20] However, systems issues of weekend care-staffing shortages, longer time to mobilize teams, lack of in-house providers including stroke neurologists and interventionalists may delay otherwise efficient stroke protocols and limit the ability to provide quality MT, which can in turn lead to greater morbidity.[1,2,3,4,10]
Using a national database that captures more than half of all U. S. hospitalizations and discharges,[21] we investigate whether weekend admission affects the likelihood of performing MT for AIS patients and whether outcomes differ from those of weekday-admitted patients. By comparing data from before and after the 2015 update to the AHA/ASA guidelines,[13] we sought to determine whether any deleterious weekend effect has been successfully resolved at a national level.
Methods
Data source
The Nationwide Readmissions Database (NRD), sponsored by the Health Care Utilization Project (HCUP), is the largest all-payer national dataset, capturing 58.2% of U. S. admissions in 2017.[21] The NRD receives data from 28 state inpatient databases, accounts for 35 million weighted discharges (18 million unweighted), and tracks patients longitudinally with unique, de-identified patient linkage numbers (PLNs). Information captured includes age, sex, weekend versus weekday admission, inpatient mortality, type of hospital (e.g., size and teaching), length of stay (LOS), insurance, International Classification of Diseases, 9th Revision Clinical Modification (ICD-9 CM) codes (before January 10, 2015), and International Classification of Diseases, 10th Revision Clinical Modification (ICD-10 CM) codes (January 1, 2015, to present). Further details on the NRD design are available at https://www.hcup-us.ahrq.gov/nrdoverview.jsp. As the NRD is publicly available and data are de-identified, this study was exempt from institutional review board approval. All analyses comply with the HCUP data use agreement.
Patient selection
In this retrospective cohort study, we queried the NRD for all patients aged >18 years from 2010 to 2017 who were admitted with a primary diagnosis of AIS (n = 3,615,268, weighted), using ICD-9 codes from January 2010 to September 2015 (436, 433.01, 433.11, 433.21, 433.31, 433.81, 433.91, 434.01, 434.11, and 434.91), and ICD-10 codes from October 2015 to December 2017 (I63.0, I63.1, I63.2, I63.3, I63.4, I63.5, I63.6, I63.8, I63.9). Using PLNs, we excluded duplicate AIS admissions (n = 75,325, weighted), as well as those with missing values on LOS, or elective admissions with LOS <1 day. Our final study population (n = 3,407,964, weighted) was then divided into two cohorts – before the 2015 AHA/ASA updated guidelines[13] (2010–2014) and after (2015–2017).
Outcomes
Our primary outcome was whether or not MT was performed during the index hospitalization for AIS, in both the 2010–2014 and 2015–2017 cohorts. Similar to previous authors,[9,10] we then further categorized patients into weekday (Monday to Friday) and weekend (Saturday and Sunday) admissions (per HCUP definition), and determined factors independently associated with receiving MT. Our secondary aim was to determine whether the outcomes among MT patients admitted during the weekend differed from those admitted during the weekday, in terms of inpatient mortality and odds of unfavorable discharge (to a skilled nursing facility, intermediate care facility, subacute rehabilitation, or similar).
Variables and definitions
Patient-level variables relevant to AIS, including comorbidities (e.g., atrial fibrillation, hypertension, smoking), procedures (e.g., MT, administration of intravenous thrombolytics (IVT), decompressive hemicraniectomy [DHC]), and complications were identified by searching all primary and secondary diagnostic codes using the HCUP-defined Clinical Classification Software (CCS). CCS is a validated tool which groups related procedural and diagnostic ICD-9 and ICD-10 codes into clinically relevant categories (See detailed coding methodology in Supplementary Materials).[21,22,23] Patient discharge was categorized as routine (to home), home with home health care, acute rehabilitation facility, or unfavorable. Unfavorable discharge, a validated surrogate for poor functional status after stroke, is nearly universally documented in administrative databases.[24] Functional status on admission was determined using the All Patient Refined-Diagnosis-Related Groups (APR-DRG) severity of illness subclass, a four-point ordinal scale derived from age, diagnoses, and procedures that ranges from minor loss of function (1) to extreme loss of function (4). The APR-DRG algorithm is a validated, reliable indicator of functional status in stroke for studies using large, administrative databases,[25,26,27] including the NRD.[28]
Statistical analysis
Weekday and weekend-admitted patients were first compared in a univariate analysis (in both 2010–2014 and 2015–2017 cohorts), in which categorical and continuous variables were assessed using the Rao-Scott Chi-square test and the Wilcoxon signed-rank sum test, respectively. We used sampling weights provided in the NRD to generate national estimates. Categorical variables were expressed as a percentage of the group of origin and continuous variables were reported as mean ± standard deviation (SD). Reported probability values were two-tailed and were considered statistically significant if P ≤ 0.05. To determine variables independently associated with receiving MT, we then built a multivariate, survey-weighted logistic regression model, using strata and cluster design to derive odds ratios (OR) and 95% confidence intervals (95% CI) with corresponding P values. Statistically significant (P ≤ 0.05) and/or clinically relevant variables from the univariate analysis were included in the multivariate model. In a similar manner, for our secondary aim, we built separate multivariate models to determine OR for inpatient mortality and unfavorable discharge among weekend-admitted patients treated with MT (with weekday as reference). The model for unfavorable discharge was built after exclusion of patients who died in the hospital. SAS 9.4 (SAS Institute Inc., Cary, North Carolina) was used for data analysis.
Results
Acute ischemic stroke cohorts
A total of 2,121,462 patients were admitted with a primary diagnosis of AIS from 2010 to 2014, of whom 549,979 (25.9%) were admitted during the weekend. From 2015 to 2017, 1,286,501 AIS patients were admitted, of whom 332,388 (25.8%) were during the weekend. On univariate analysis, demographics, comorbidities, insurance status, and hospital characteristics of weekday-admitted AIS patients were similar to weekend-admitted patients in both cohorts [Table 1].
Table 1.
Baseline characteristics of patients admitted with acute ischemic stroke, 2010-2014 and 2015-2017
| Variables | 2010-2014 |
2015-2017 |
||||
|---|---|---|---|---|---|---|
| Weekdays (n=1,571,483), n (%) | Weekends (n=549,979), n (%) | P | Weekdays (n=954,113), n (%) | Weekends (n=332,388), n (%) | P | |
| Age (years) | <0.0001 | <0.0001 | ||||
| 18-49 | 7.92 | 7.70 | Reference | 7.83 | 7.52 | Reference |
| 50-79 | 58.7 | 58.1 | 0.18 | 60.7 | 60.0 | 0.02 |
| ≥80 | 33.4 | 34.2 | <0.0001 | 31.5 | 32.5 | <0.0001 |
| Sex (male reference) | ||||||
| Female | 51.6 | 52.1 | 0.0008 | 50.6 | 51.1 | 0.0005 |
| Inpatient treatment | ||||||
| MT | 1.11 | 1.08 | 0.34 | 2.82 | 2.91 | 0.11 |
| IVT | 8.23 | 8.78 | <0.0001 | 11.1 | 11.9 | <0.0001 |
| DHC | 0.40 | 0.45 | 0.018 | 0.24 | 0.26 | 0.28 |
| Complications | ||||||
| ICH | 3.16 | 3.32 | 0.001 | 3.98 | 4.12 | 0.034 |
| Hydrocephalus | 0.50 | 0.52 | 0.33 | 0.52 | 0.52 | 0.99 |
| Cerebral edema | 3.38 | 3.64 | <0.0001 | 4.71 | 5.05 | <0.0001 |
| Comorbidities | ||||||
| Hypertension | 82.4 | 82.8 | 0.0048 | 84.3 | 84.3 | 0.904 |
| Smoking | 29.0 | 28.9 | 0.24 | 36.8 | 36.3 | 0.002 |
| Drug abuse | 2.48 | 2.58 | 0.018 | 2.72 | 2.71 | 0.86 |
| Alcohol abuse | 4.39 | 4.52 | 0.017 | 4.50 | 4.61 | 0.10 |
| Obesity | 10.3 | 10.3 | 0.57 | 12.8 | 12.7 | 0.43 |
| Chronic liver disease | 1.20 | 1.18 | 0.57 | 1.58 | 1.53 | 0.15 |
| Chronic renal disease | 14.6 | 14.5 | 0.18 | 16.4 | 15.9 | <0.0001 |
| Hypothyroidism | 13.6 | 13.7 | 0.24 | 14.0 | 14.1 | 0.37 |
| DM | 36.1 | 35.6 | 0.0004 | 37.5 | 37.0 | 0.001 |
| Dyslipidemia | 56.0 | 55.9 | 0.76 | 58.1 | 58.0 | 0.39 |
| Atrial fibrillation | 24.5 | 25.2 | <0.0001 | 25.6 | 26.3 | <0.0001 |
| CHF | 14.4 | 14.5 | 0.12 | 15.5 | 15.5 | 0.89 |
| PVD | 9.85 | 9.67 | 0.035 | 9.96 | 9.95 | 0.93 |
| Valvular disease | 10.0 | 10.1 | 0.53 | 10.2 | 10.2 | 0.95 |
| Long-term use of Anti-thrombotics | 14.1 | 14.3 | 0.098 | 24.1 | 24.2 | 0.25 |
| Long-term use of Anticoagulants | 6.96 | 7.07 | 0.15 | 8.82 | 8.74 | 0.38 |
| Functional status (APR-DRG) | <0.0001 | 0.0005 | ||||
| 1-2 (mild to moderate loss of function) | 60.5 | 59.9 | Reference | 58.6 | 58.1 | Reference |
| 3-4 (major to extreme loss of function) | 39.5 | 40.1 | <0.0001 | 41.4 | 41.9 | 0.0005 |
| Discharge outcomes | <0.0001 | <0.0001 | ||||
| Routine to home | 40.0 | 38.4 | Reference | 40.9 | 39.2 | Reference |
| HHC | 18.7 | 18.7 | <0.0001 | 16.7 | 16.6 | <0.0001 |
| Acute rehabilitation | 1.63 | 1.71 | <0.0001 | 1.32 | 1.29 | 0.41 |
| Adverse discharge (SNF, ICF, subacute rehabilitation, or similar) | 33.8 | 34.9 | <0.0001 | 35.5 | 37.1 | <0.0001 |
| AMA | 0.64 | 0.58 | 0.11 | 0.89 | 0.87 | 0.36 |
| Death in hospital | 5.09 | 5.43 | <0.0001 | 4.60 | 4.86 | <0.0001 |
| Missing data | 0.181 | 0.1969 | 0.043 | 0.09 | 0.09 | 0.43 |
| Insurance status | 0.0067 | <0.0001 | ||||
| Medicare | 67.6 | 67.9 | Reference | 67.3 | 68.1 | Reference |
| Medicaid | 7.24 | 7.30 | 0.22 | 8.57 | 8.50 | 0.062 |
| Private | 17.5 | 17.1 | 0.015 | 17.7 | 17.0 | <0.0001 |
| Self-pay | 4.48 | 4.50 | 0.38 | 3.54 | 3.57 | 0.99 |
| Other | 3.20 | 3.15 | 0.33 | 2.89 | 2.80 | 0.011 |
| Hospital characteristics | <0.0001 | <0.0001 | ||||
| Small bed-size | 11.3 | 10.8 | Reference | 14.6 | 13.9 | Reference |
| Medium bed-size | 24.3 | 24.2 | 0.038 | 27.9 | 27.7 | 0.0004 |
| Large bed-size | 64.5 | 65.0 | <0.0001 | 57.5 | 58.5 | <0.0001 |
| Teaching hospital (reference, nonteaching) | 50.9 | 51.9 | <0.0001 | 66.2 | 67.4 | <0.0001 |
| Median household income by patient zip code | 0.13 | 0.0009 | ||||
| 0-25th percentile | 31.1 | 30.9 | Reference | 31.0 | 30.5 | Reference |
| 26th-50th percentile | 25.4 | 25.4 | 0.42 | 26.0 | 26.2 | 0.0069 |
| 51st-75th percentile | 22.7 | 22.8 | 0.097 | 23.7 | 23.6 | 0.13 |
| 76th-100th percentile | 19.2 | 19.4 | 0.061 | 17.9 | 18.3 | 0.0001 |
| Missing | 1.57 | 1.62 | 0.049 | 1.41 | 1.43 | 0.17 |
MT: Mechanical thrombectomy, IVT: Intravenous thrombolysis, DHC: Decompressive hemicraniectomy, ICH: Intracerebral hemorrhage, DM: Diabetes mellitus, CHF: Congestive heart failure, PVD: Peripheral vascular disease, HHC: Home with home health care, SNF: Skilled nursing facility, ICF: Intermediate care facility, AMA: Against medical advice, APR-DRG: All patient refined-diagnosis-related groups
Overall mechanical thrombectomy data
The overall frequency of MTs performed per 100,000 AIS cases increased annually from 685 in 2010, to 2,133 in 2015, and 3,493 in 2017 [Figure 1]. This increase was seen among all hospital types (small, medium, and large bed-size, as well as teaching and nonteaching). Within the 2010–2014 cohort, a total of 1.11% of weekday-admitted AIS patients received a MT compared to 1.08% among those who were weekend-admitted, which was not statistically significant on univariate analysis (P = 0.34). A greater overall proportion of the 2015–2017 cohort received MT, although the difference between weekdays and weekends was again not statistically significant (2.82% and 2.91%, respectively, P = 0.11).
Figure 1.
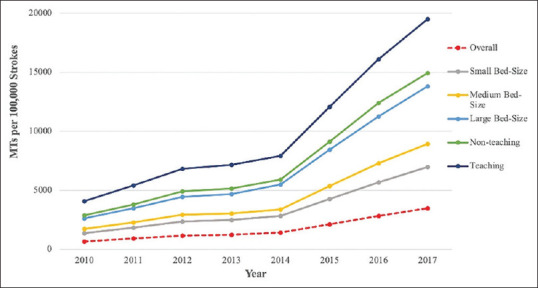
Trend of frequencies of MTs performed per 100,000 strokes in various hospital types, 2010-2017. MT: Mechanical thrombectomies
Factors independently associated with receiving mechanical thrombectomy
In our multivariate model of the 2010–2014 cohort, however, weekend admission was independently associated with a reduced likelihood of receiving MT compared to weekday admission (OR: 0.92, 95% CI: 0.89–0.95, P < 0.0001). This effect was not statistically significant in the 2015–2017 cohort [Table 2]. Advanced age >80 years was strongly associated with a reduced odds of receiving MT in the 2010–2014 cohort (OR: 0.43, 95% CI: 0.41–0.46, P < 0.0001), and to a lesser, yet still statistically significant extent in the 2015–2017 cohort (OR: 0.65, 95% CI: 0.62-0.68, P < 0.0001). In both cohorts, MT was also independently associated with private insurance and admission to large, teaching hospitals [Table 2]. In addition, regarding factors related to the severity of strokes treated with thrombectomy, MT was independently associated with receiving IVT, having intracranial hemorrhage and/or cerebral edema as sequelae, major to extreme loss of function on admission (APR-DRG severity 3–4), and atrial fibrillation [Table 2].
Table 2.
Factors associated with odds of receiving mechanical thrombectomy in 2010-2014 and 2015-2017, multivariate model
| Variables | 2010-2014 |
2015-2017 |
||
|---|---|---|---|---|
| OR | P | OR | P | |
| Weekend admission (weekday reference) | 0.92 (0.89-0.95) | <0.0001 | 0.98 (0.94-1.02) | 0.2379 |
| Age groups (years) | ||||
| 18-49 | Reference | Reference | ||
| 50-79 | 0.73 (0.70-0.77) | <0.0001 | 0.88 (0.84-0.91) | <0.0001 |
| ≥80 | 0.43 (0.41-0.46) | <0.0001 | 0.65 (0.62-0.68) | <0.0001 |
| Female sex (male reference) | 1.04 (1.02-1.07) | 0.0033 | - | - |
| Treatments and complications | ||||
| IVT | 10.8 (10.5-11.1) | <0.0001 | 4.75 (4.65-4.86) | <0.0001 |
| DHC | 0.90 (0.82-0.99) | 0.0282 | 0.92 (0.76-1.12) | 0.4121 |
| ICH | 2.90 (2.80-3.01) | <0.0001 | 3.06 (2.96-3.15) | <0.0001 |
| Hydrocephalus | 1.14 (1.02-1.27) | 0.0181 | 1.05 (0.90-1.23) | 0.5219 |
| Cerebral edema | 2.67 (2.57-2.78) | <0.0001 | 2.79 (2.71-2.88) | <0.0001 |
| Comorbidites | ||||
| Hypertension | 0.88 (0.85-0.91) | <0.0001 | 0.86 (0.84-0.89) | <0.0001 |
| Smoking | 0.91 (0.88-0.94) | <0.0001 | 0.84 (0.82-0.86) | <0.0001 |
| Liver disease | - | - | 0.83 (0.75-0.91) | 0.0001 |
| Obesity | 1.16 (1.11-1.21) | <0.0001 | - | - |
| Renal failure | 0.68 (0.65-0.71) | <0.0001 | 0.76 (0.73-0.78) | <0.0001 |
| Hypothyroidism | 0.99 (0.90-1.07) | 0.7225 | 0.97 (0.92-1.03) | 0.3086 |
| DM | 0.82 (0.80-0.85) | <0.0001 | 0.72 (0.70-0.74) | <0.0001 |
| Dyslipidemia | 0.92 (0.90-0.95) | <0.0001 | 0.87 (0.85-0.89) | <0.0001 |
| Atrial Fibrillation | 2.39 (2.32-2.47) | <0.0001 | 2.50 (2.44-2.57) | <0.0001 |
| CHF | 1.20 (1.15-1.24) | <0.0001 | 1.28 (1.25-1.32) | <0.0001 |
| PVD | 1.47 (1.41-1.54) | <0.0001 | 1.35 (1.31-1.40) | <0.0001 |
| Valvular disease | 1.16 (1.12-1.21) | <0.0001 | 1.12 (1.09-1.16) | <0.0001 |
| Long term use of anti-thrombotics | - | - | 0.79 (0.76-0.81) | <0.0001 |
| Long term use of anticoagulants | 1.38 (1.32-1.44) | <0.0001 | 1.20 (1.16-1.25) | <0.0001 |
| Insurance status | ||||
| Medicare | Reference | Reference | ||
| Medicaid | 1.06 (1.01-1.12) | 0.0293 | 1.07 (1.02-1.12) | 0.0026 |
| Private insurance | 1.16 (1.11-1.20) | <0.0001 | 1.22 (1.18-1.26) | <0.0001 |
| Self-pay | 1.07 (1.0-1.15) | 0.0579 | 1.18 (1.11-1.26) | <0.0001 |
| No charge/other | 0.94 (0.87-1.02) | 0.1617 | 1.16 (1.09-1.24) | <0.0001 |
| Hospital characteristics | ||||
| Small bed-size | Reference | Reference | ||
| Medium bed-size | 1.40 (1.28-1.53) | <0.0001 | 2.18 (2.05-2.32) | <0.0001 |
| Large bed-size | 3.86 (3.57-4.18) | <0.0001 | 5.07 (4.78-5.38) | <0.0001 |
| Teaching hospital (reference, nonteaching) | 3.32 (3.21-3.44) | <0.0001 | 3.08 (2.98-3.19) | <0.0001 |
| Median household income by patient zip code | ||||
| 0-25th percentile | Reference | Reference | ||
| 26th-50th percentile | 1.10 (1.06-1.14) | <0.0001 | 1.05 (1.02-1.08) | 0.0032 |
| 51st-75th percentile | 1.24 (1.20-1.29) | <0.0001 | 1.13 (1.10-1.17) | <0.0001 |
| 76th-100th percentile | 1.23 (1.18-1.28) | <0.0001 | 1.12 (1.09-1.15) | <0.0001 |
| Missing | 1.10 (0.98-1.23) | 0.1193 | 1.02 (0.92-1.12) | 0.7494 |
| Functional status (APR-DRG) | ||||
| 1-2 (mild to moderate loss of function) | Reference | Reference | ||
| 3-4 (major to extreme loss of function) | (42.128-35.724) 49.680 | <0.0001 | (44.428-38.403) 51.398 | <0.0001 |
IVT: Intravenous thrombolysis, DHC: Decompressive hemicraniectomy, ICH: Intracerebral hemorrhage, DM: Diabetes mellitus, CHF: Congestive heart failure, PVD: Peripheral vascular disease, APR-DRG: All patient refined-diagnosis-related groups, OR: Odds ratio
Outcomes of mechanical thrombectomy patients
Our multivariate model in Table 3 describes the effect of weekend admission on inpatient mortality and unfavorable discharge among patients who underwent MT, controlling for clinically and statistically significant variables (including APR-DRG functional status, as done by previous authors).[28] Weekend-admitted patients undergoing MT did not have a statistically significant difference in inpatient mortality compared to those admitted during the weekday (variable of reference), during both periods. From 2010 to 2014, we found no effect of weekend admission on unfavorable discharge. However, during the 2015–2017 time period, weekend admission was independently associated with unfavorable discharge (OR: 1.11, 95% CI: 1.02–1.22, P = 0.02). From the 2010–2014 to 2015–2017 time periods, average LOS among weekend-admitted patients decreased slightly from 3.43 days (±1 SD 2.03–7.53) to 2.83 days (1.70–4.79), P < 0.0001, which was similar among weekday-admitted patients, which decreased from 3.46 (1.78–7.02) to 2.78 days (1.50–5.30), P < 0.0001.
Table 3.
Effect of weekend admission on outcomes in mechanical thrombectomy population, multivariate models
| Outcome variable | 2010-2014 |
2015-2017 |
||
|---|---|---|---|---|
| OR | P | OR | P | |
| Inpatient mortality | 0.97 (0.83-1.12) | 0.65 | 1.08 (0.96-1.21) | 0.20 |
| Adverse discharge (to SNF/ICF/subacute rehabilitation)a | 1.04 (0.89-1.22) | 0.63 | 1.11 (1.02-1.22) | 0.02 |
Models were adjusted for admission day (i.e., weekday vs. weekend), age, sex, IVT, DHC, ICH, hydrocephalus, cerebral edema, hypertension, smoking, drug abuse, alcoholism, PVD, valvular disease, atrial fibrillation, long term use of antithrombotics, long-term use of anti-coagulants, insurance status, bed-size of hospital, teaching status of hospital, median income, and baseline functional status (APR-DRG), aModel run after excluding inpatient deaths. IVT: Intravenous thrombolysis, DHC: Decompressive hemicraniectomy, ICH: Intracerebral hemorrhage, PVD: Peripheral vascular disease, APR-DRG: All patient refined-diagnosis-related groups, OR: Odds ratio, SNF: Skilled nursing facility, ICF: Intermediate care facility
Discussion
Although AIS remains a leading cause of death and disability,[29] the “weekend effect” among stroke patients is understudied. To the best of our knowledge, this is the first study to use large, population-level datasets to investigate whether the rapidly evolving endovascular management of stroke is subject to a weekend effect, in terms of the likelihood of receiving the treatment and post-treatment outcomes. In this analysis of more recent, nationally representative data, we found that overall, a small weekend effect had initially been present in terms of the likelihood of receiving MT, but then resolved after the 2015 update to the AHA/ASA guidelines.[13] However, certain subgroups of patients, particularly the elderly, remained significantly less likely to receive MT. In terms of outcomes, weekend admission was independently associated with more frequent unfavorable discharges in the postguidelines, 2015–2017 cohort. Our data suggest that, on a national level, non–uniform access to and varying outcomes from endovascular treatment remain. These findings may be related to rapidly changing hospital practices and socioeconomic influences following the guidelines update.
Prior studies have demonstrated a greater overall mortality and morbidity among stroke patients who are admitted during the weekend,[5,6,7,8] attributing this to an off-hours phenomenon of hospital “systems inadequacies,[4]” also reported during holiday[6] and nighttime admissions.[8,30] For patients undergoing MT, existing data have primarily assessed outcomes from single centers, or reflect patterns of MT usage prior to the updated guidelines.[13] Further, few have used administrative databases to determine factors that affect the likelihood of a patient receiving an MT. Overall, institutional studies have had mixed results in assessing whether weekend admission influences outcomes.[31,32,33] However, a pre-guidelines study of patients undergoing MT, which used the nationwide inpatient sample (NIS), found that those admitted to nonteaching hospitals during the weekend were 60% more likely to have moderate or severe disability at discharge.[10] In another NIS study that investigated trends of MT by comparing pre- to post-guidelines data, the probability of a good outcome had slightly improved.[12] Similar to our data, the authors found that MT had more than doubled in utilization, and that the proportion of patients receiving concurrent IVT with MT had declined (60.3% in 2010–2014 to 43.4% in 2015–2017 in our data).[12] In addition, a smaller proportion underwent DHC in the later cohort, consistent with prior data,[34] however demographics and comorbidities of the earlier and later cohorts were generally similar.
Although our data showed no overall effect of weekend admission on inpatient mortality, we did find evidence of a weekend effect in the postguidelines cohort, in terms of a modestly increased likelihood of unfavorable discharge (as mentioned earlier, a surrogate for poorer functional outcome among stroke patients[24]) relative to their weekday counterparts. Although seemingly counterintuitive, this finding may in fact be related to the recent, widespread implementation of MTs into a large variety of hospital settings, driven by positive results from clinical trials[14,15,16,17,18] and strong financial incentives to become TSCs.[11,12,19] Indeed, the latter NIS study found that approximately 50% more hospitals had started providing MT after the guidelines update.[12] As a result, a growing proportion of MTs are being performed at nonteaching, lower-volume centers, and while this has greatly improved access to MT, the likelihood of a good functional outcome is known to be marginally lower in such settings.[10,11] Our findings of modestly poorer weekend outcomes are in contrast to the overall outcomes reported in the NIS data,[12] possibly because the study did not account for the effect of weekend admission. In addition, the NRD captures approximately three times as many unique hospitalizations as the NIS, and thereby may be considered statistically more representative of the U. S. population.[12,21]
Unlike higher-volume, academic hospital settings (where the functional benefits of MT were initially shown[14,15,16,17,18]), lower-volume centers often lack the resources to have a comparable level of prompt neuroimaging, appropriate patient selection, interventionalist availability, stroke nursing, and rehab capabilities.[11] In effect, although MT has become more widely available (approximately five-fold from 2010 to 2017 in our data), there is evidence of a new weekend effect, likely as hospitals rapidly adapt and optimize their clinical infrastructure to become endovascular-capable. Indeed, some hospitals have implemented and streamlined LVO protocols to mitigate the weekend effect.[35]
Weekend admission no longer affected the odds of receiving MT postguidelines, suggesting that this implementation has by and large been successful. The difference in outcomes, however, suggests that the full course of hospitalization may not yet be optimized, which may be related to in-hospital as well as pre-hospital factors.[36,37,38] As stroke treatment relies on highly protocolized, time-sensitive workflow algorithms with multidisciplinary coordination, a weekend effect may result from even minor delays or inadequacies in a necessarily well-orchestrated sequence of events from triage to diagnosis, to appropriate treatment and aftercare. System inadequacies on the weekend may include insufficient nursing or interventional staff, longer transport times to computed tomography scan or to the interventional suite, greater door-to-reperfusion or imaging-to-reperfusion times, and unavailable equipment.[1,2,3,4,32,33,39]
Further, unlike stroke patients who only receive IVT, the outcomes of LVO patients rely heavily on the availability and technical ability of the subspecialized proceduralist, which may result in a weekend effect similar to that observed among patients undergoing coronary reperfusion[40] and carotid endarterectomies.[4] Weekend coverage by more junior interventionalists or those with commitments to multiple hospitals may affect access to and outcomes of MT, as appropriate patient selection and time to MT strongly influence functional outcomes.[20] A weekend effect may also be due to implicit, unconscious biases on behalf of the physician, in that the clinical context of the stroke (e.g., inconvenient off-hours time) is known to affect judgment, even when assessing objective information.[31]
Such biases and system inadequacies may result in nonuniform access to subspecialty services.[31,35] Although weekend admission did not seem to affect overall access to MT postguidelines, other demographic and socioeconomic factors influenced the likelihood of receiving the treatment. The very elderly (age >80 years), in particular, were significantly less likely to receive MT than younger patients with similar comorbidities and socioeconomic status, despite the fact that, as the population ages, the >80 years of age group now accounts for nearly one third of AIS patients. Although overall outcomes of octogenarians with LVOs are poorer, MT still provides a substantial functional benefit in appropriately selected patients.[41,42,43] While a proportion of the elderly may have a poorer baseline functional status that could preclude them from MT, it is unclear to which degree other biases are at work, such as a hesitancy to intervene due to perceived futility of care. Indeed, patients >80 years were excluded or under-represented in many of the clinical trials,[41,42,43] and preconceived notions about the futility of treatment may prompt withdrawal of care, which may in turn influence outcomes.[44] Technical factors, such inadequate vascular access due to tortuous, atherosclerotic vessels, may also play a role. In terms of other subgroups, patients admitted to large bed-size or teaching hospitals, those with private insurance, and those who were wealthier were more likely to receive MT, consistent with prior studies.[10,45]
Our study has several limitations. As is true with any retrospective study that analyzes large, coding-based administrative data, sensitivity and specificity may differ based on codes, granularity may be limited, and small fraction of the data may be missing or misrepresented. In addition, associations are not necessarily proof of causality, and certain findings may reach statistical significance due to large sample sizes. The coding system nationwide changed from ICD-9 to ICD-10 for Q4 2015 (at approximately the same time as the AHA/ASA guidelines update), which may have temporarily introduced coding errors as financial coders became more proficient.[12] To minimize this effect, we calculated month-by-month frequencies of codes to verify that sudden shifts in data did not occur, and we used validated ICD-9 and ICD-10 codes similar to prior authors.[12] Although databases such as the NRD provide nationally representative data, certain details relevant to MT are not included, such as the severity of the stroke (e.g., National Institutes of Health Stroke Scale), the thrombolysis in cerebral infarction grade, imaging details, time to reperfusion, or technical details of the procedure. In addition, the NRD does not include variables for ethnicity, geographical location, whether a center is a TSC, or quality of life metrics.[21]
Future efforts should focus on determining, on a hospital-by-hospital basis, factors that may contribute to unequal access to and outcomes from MT, as the treatment becomes increasingly more common. This may include overcoming substantial social, economic, and logistical hurdles. Indeed, one study found that treatment interval periods decrease with better protocol experience.[35] As national datasets become available with each successive year, future, nationally representative studies should then determine whether our findings have persisted after 2017.
Conclusions
To the best of our knowledge, there has not been a recent, updated study of nationally representative data that assesses the presence of a weekend effect on MT before and after the significant change in the standard of care for stroke in 2015. Our data suggest that weekend admission affected overall access to MT before the 2015 guidelines update, but this effect was no longer present thereafter, likely as the updated guidelines have resulted in an appropriate, national shift in practice. As the trend of performing MT becomes more common and available, however, a new, post-guidelines weekend effect has become evident as poorer-than-expected outcomes, and certain subgroups of patients, such as the elderly, may still be under-treated. This new effect of weekend admission may be due to lower volume centers providing the treatment, which may be more susceptible to systems inadequacies and implicit biases.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Supplementary Table 1.
International Classification of Diseases, 9th revision and International Classification of Diseases, 10th revision codes for variables
| Variables | ICD-9 | ICD-10 |
|---|---|---|
| AIS | 436, 433.01, 433.11, 433.21, 433.31, 433.81,433.91, 434.01, 434.11, 434.91 | I63.0, I63.1, I63.2, I63.3, I63.4, I63.5, I63.6, I63.8, I63.9 |
| ICH (including IPH and SAH) | 431, 430, 432.9 | I60, I61, I62.9 |
| IVT | 991.0, V45.88 | Z92.82, 3E03317 |
| MT | 39.74 | 03CP3, 03CQ3, 03CL3, 03CK3, 03CG3 |
| Percutaneous endoscopic gastrostomy | 43.11-43.19 | 0DH64UZ, 0DH63UZ |
| Tracheostomy | 31.10, 31.20, 31.21, or 31.29 | 0B114, 0B113 |
| Decompressive craniectomy | 01.24, 01.25, 01.39, 01.53, 01.59, 02.02 | 0WC1, 0WH1, 0WW1, 0WP1, 0WJ1, 0WH1, 0W91, 0NW0, 0NP0, 0NH0, 0N80, 00W0, 00J0, 0N50, 0NB0, 0090, 00C0, 00H0, 00P0, 00W0, 00B7, 0050, 00B0, 0NS0 |
| Cerebral edema | 348.5, 348.4 | G93.5, G93.6 |
| Hydrocephalus | 331.4 | G91.1, G91.4, G91.8, G91.9 |
| Carotid endarterectomy | 38.12 | 03CK, 03CL |
| Carotid angioplasty/stent placement | 00.63, 00.64 | 037K3, 037K4, 037L3, 037L4 |
| Intracranial angioplasty/stent placement | 00.62, 00.65 | 037G3, 037G4 |
| Postprocedure stroke | 997.02 | I97.821, I97.811 |
| Anticoagulants | V58.61 | Z79.01 |
| Anti-thrombotics | V58.63, V58.66 | Z79.02, Z79.82 |
| Smoking | V15.82, 305.1 | Z87.891, F17 |
| Atrial fibrillation | 427.31, 427.32 | I48 |
| Dyslipidemia | CCS 53 | CCS 53 |
| Cm_Chf, Cm_Perivasc, Cm_Valve, Cm_Drug, Cm_Alcohol, Cm_Htn_C, Cm_Obese, Cm_Liver, Cm_Renlfail, Cm_Hypothy, Cm_Dmcx, and Cm_Dm | Comorbidity measures are assigned using the AHRQ comorbidity software. The AHRQ comorbidity measures identify coexisting medical conditions that are not directly related to the principal diagnosis, or the main reason for admission, and are likely to have originated prior to the hospital stay. Comorbidities are identified using ICD-9-CM diagnoses and the DRG in effect on the discharge date. Derived from https://www.hcup-us.ahrq.gov/tools_software.jsp | |
| APR-DRG | APR-DRGs are assigned using software developed by 3m health information systems. This severity measure includes the base APR-DRG, the severity of illness subclass, and the risk of mortality subclass within each base APR-DRG. Derived from https://www.hcup-us.ahrq.gov/db/vars/aprdrg/nisnote.jsp | |
The CCS for ICD-9-CM is based on the ICD-9-CM, which is a uniform and standardized coding system. The ICD-9-CM’s multitude >14,000 diagnosis codes and >3900 procedure codes are collapsed into a smaller number of clinically meaningful categories. These are generally more useful for presenting descriptive statistics. Derived from https://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp. AIS: Acute ischemic stroke, DRG: Diagnosis-related group, CCS: Clinical Classifications Software, ICD: International Classification of Diseases, ICD-9-CM: ICD, 9th Revision, clinical modification, ICH: Intracerebral hemorrhage, IPH: Intraparenchymal hemorrhage, SAH: Subarachnoid hemorrhage, IVT: Intravenous thrombolysis, MT: Mechanical thrombectomy, APR-DRG: All patient refined-DRG, AHRQ: Agency for healthcare research and quality
Supplementary File 2: Tables of Covariates used in Table 3
Table A.
Covariates for mortality outcome, 2010-2014
| Covariate | OR | 95% CI | P |
|---|---|---|---|
| Weekend admission (weekday reference) | 0.966 | 0.83-1.124 | 0.6533 |
| Age groups (years) | |||
| 18-49 | Reference | ||
| 50-79 | 2.158 | 1.685-2.763 | <0.0001 |
| ≥80 | 3.773 | 2.857-4.983 | <0.0001 |
| Female sex (male reference) | 0.904 | 0.788-1.036 | 0.1464 |
| Treatments and complications | |||
| IVT | 0.878 | 0.756-1.019 | 0.0864 |
| DHC | 0.882 | 0.614-1.269 | 0.4987 |
| ICH | 1.546 | 1.328-1.8 | <0.0001 |
| Hydrocephalus | 4.34 | 2.908-6.48 | <0.0001 |
| Cerebral edema | 3.498 | 2.929-4.177 | <0.0001 |
| Comorbidites | |||
| Hypertension | 1.139 | 0.958-1.353 | 0.1396 |
| Smoking | 0.916 | 0.789-1.064 | 0.2518 |
| Drug abuse | 0.52 | 0.334-0.81 | 0.0038 |
| Alcohol abuse | 0.939 | 0.692-1.274 | 0.6841 |
| Obesity | 0.831 | 0.646-1.069 | 0.1499 |
| Liver failure | 0.739 | 0.39-1.402 | 0.3546 |
| Renal failure | 1.094 | 0.886-1.352 | 0.4039 |
| Hypothyroidism | 0.808 | 0.667-0.98 | 0.0303 |
| DM | 1.09 | 0.906-1.312 | 0.3593 |
| Hyperlipidemia | 0.682 | 0.598-0.776 | <0.0001 |
| Atrial fibrillation | 0.827 | 0.712-0.959 | 0.0123 |
| CHF | 1.325 | 1.137-1.544 | 0.0003 |
| PVD | 1.262 | 1.056-1.509 | 0.0106 |
| Valvular disorders | 0.66 | 0.528-0.826 | 0.0003 |
| Long-term use of anti-thrombotics | 1.094 | 0.932-1.285 | 0.2732 |
| Long-term use of anticoagulants | 0.947 | 0.743-1.206 | 0.6581 |
| Insurance status | |||
| Medicare | Reference | ||
| Medicaid | 0.869 | 0.649-1.163 | 0.3435 |
| Private insurance | 0.853 | 0.729-0.999 | 0.0483 |
| Self-pay | 1.14 | 0.766-1.699 | 0.5177 |
| Other | 1.143 | 0.819-1.596 | 0.432 |
| Hospital characteristics | |||
| Small bed-size | Reference | ||
| Medium bed-size | 1.62 | 1.086-2.416 | 0.0182 |
| Large bed-size | 1.441 | 1.009-2.058 | 0.0442 |
| Teaching hospital versus nonteaching hospital | 0.818 | 0.666-1.004 | 0.0547 |
| Median household income by patient zip code | |||
| 0-25th percentile | Reference | ||
| 26th-50th percentile | 1.085 | 0.899-1.31 | 0.395 |
| 51st-75th percentile | 1.222 | 0.989-1.509 | 0.063 |
| 76th-100th percentile | 1.252 | 1.029-1.523 | 0.0247 |
IVT: Intravenous thrombolysis, DHC: Decompressive hemicraniectomy, ICH: Intracerebral hemorrhage, DM: Diabetes mellitus, CHF: Congestive heart failure, PVD: Peripheral vascular disease, OR: Odds ratio, CI: Confidence interval
Table B.
Covariates for mortality outcome, 2015-2017
| Covariate | OR | 95% CI | P |
|---|---|---|---|
| Weekend admission (weekday reference) | 1.079 | 0.964-1.208 | 0.1848 |
| Age groups (years) | |||
| 18-49 | Reference | ||
| 50-79 | 1.718 | 1.416-2.083 | <0.0001 |
| ≥80 | 2.771 | 2.22-3.458 | <0.0001 |
| Female sex (male reference) | 0.812 | 0.739-0.892 | <0.0001 |
| Treatments and complications | |||
| IVT | 0.834 | 0.764-0.912 | <0.0001 |
| DHC | 1.227 | 0.869-1.733 | 0.244 |
| ICH | 1.617 | 1.445-1.808 | <0.0001 |
| Hydrocephalus | 4.222 | 3.173-5.616 | <0.0001 |
| Cerebral edema | 3.704 | 3.308-4.148 | <0.0001 |
| Comorbidities | |||
| Hypertension | 0.959 | 0.836-1.101 | 0.554 |
| Smoking | 0.954 | 0.84-1.083 | 0.4622 |
| Drug abuse | 0.769 | 0.564-1.048 | 0.0963 |
| Alcohol abuse | 0.789 | 0.618-1.006 | 0.0562 |
| Obesity | 1.041 | 0.906-1.196 | 0.5705 |
| Liver failure | 1.063 | 0.705-1.602 | 0.7707 |
| Renal failure | 1.336 | 1.168-1.528 | <0.0001 |
| Hypothyroidism | 0.843 | 0.731-0.974 | 0.0202 |
| DM | 1.324 | 1.196-1.465 | <0.0001 |
| Hyperlipidemia | 0.812 | 0.732-0.901 | <0.0001 |
| Atrial fibrillation | 0.915 | 0.818-1.025 | 0.1238 |
| CHF | 1.207 | 1.074-1.358 | 0.0017 |
| PVD | 1.272 | 1.104-1.466 | 0.0009 |
| Valvular disorders | 0.709 | 0.61-0.825 | <0.0001 |
| Long-term use of anti-thrombotics | 0.726 | 0.631-0.837 | <0.0001 |
| Long-term use of anticoagulants | 1.026 | 0.873-1.207 | 0.7538 |
| Insurance status | |||
| Medicare | Reference | ||
| Medicaid | 0.885 | 0.727-1.076 | 0.2206 |
| Private insurance | 0.653 | 0.563-0.757 | <0.0001 |
| Self-pay | 0.959 | 0.695-1.324 | 0.8002 |
| Other | 1.154 | 0.894-1.488 | 0.2712 |
| Hospital characteristics | |||
| Small bed-size | Reference | ||
| Medium bed-size | 1.008 | 0.756-1.344 | 0.9558 |
| Large bed-size | 0.915 | 0.706-1.186 | 0.5014 |
| Teaching hospital versus nonteaching hospital | 0.832 | 0.696-0.995 | 0.0439 |
| Median household income by patient zip code | |||
| 0-25th percentile | Reference | ||
| 26th-50th percentile | 1.077 | 0.925-1.255 | 0.3361 |
| 51st-75th percentile | 1.204 | 1.048-1.383 | 0.0087 |
| 76th-100th percentile | 1.036 | 0.9-1.193 | 0.6205 |
IVT: Intravenous thrombolysis, DHC: Decompressive hemicraniectomy, ICH: Intracerebral hemorrhage, DM: Diabetes mellitus, CHF: Congestive heart failure, PVD: Peripheral vascular disease, OR: Odds ratio, CI: Confidence interval
Table C.
Covariates for adverse discharge outcome, 2010-2014
| Covariate | OR | 95% CI | P |
|---|---|---|---|
| Weekend admission (weekday reference) | 1.04 | 0.889-1.216 | 0.6261 |
| Age groups (years) | |||
| 18-49 | Reference | ||
| 50-79 | 1.827 | 1.519-2.197 | <0.0001 |
| ≥80 | 3.69 | 2.915-4.67 | <0.0001 |
| Female sex (male reference) | 0.983 | 0.865-1.116 | 0.7891 |
| Treatments and complications | |||
| IVT | 0.87 | 0.762-0.993 | 0.0391 |
| DHC | 2.123 | 1.299-3.469 | 0.0027 |
| ICH | 1.96 | 1.668-2.302 | <0.0001 |
| Hydrocephalus | 5.226 | 2.17-12.587 | 0.0002 |
| Cerebral edema | 2.248 | 1.859-2.718 | <0.0001 |
| Comorbidities | |||
| Hypertension | 1.001 | 0.848-1.181 | 0.9931 |
| Smoking | 0.733 | 0.637-0.843 | <0.0001 |
| Drug abuse | 1.067 | 0.736-1.547 | 0.7308 |
| Alcohol abuse | 1.122 | 0.885-1.422 | 0.3414 |
| Obesity | 0.89 | 0.739-1.073 | 0.2212 |
| Liver failure | 0.61 | 0.363-1.026 | 0.0626 |
| Renal failure | 1.074 | 0.835-1.38 | 0.5786 |
| Hypothyroidism | 0.785 | 0.629-0.979 | 0.0318 |
| DM | 1.287 | 1.129-1.468 | 0.0002 |
| Hyperlipidemia | 0.664 | 0.584-0.755 | <0.0001 |
| Atrial fibrillation | 1.256 | 1.054-1.496 | 0.0108 |
| CHF | 1.156 | 0.995-1.345 | 0.0589 |
| PVD | 1.208 | 1.013-1.442 | 0.0355 |
| Valvular disorders | 0.834 | 0.72-0.967 | 0.0161 |
| Long-term use of anti-thrombotics | 0.797 | 0.655-0.97 | 0.024 |
| Long-term use of anticoagulants | 0.708 | 0.601-0.833 | <0.0001 |
| Insurance status | |||
| Medicare | Reference | ||
| Medicaid | 0.829 | 0.66-1.04 | 0.1052 |
| Private insurance | 0.67 | 0.571-0.786 | <0.0001 |
| Self-pay | 0.278 | 0.193-0.4 | <0.0001 |
| Other | 0.467 | 0.333-0.655 | <0.0001 |
| Hospital characteristics | |||
| Small bed-size | Reference | ||
| Medium bed-size | 0.783 | 0.5-1.225 | 0.2834 |
| Large bed-size | 0.617 | 0.454-0.839 | 0.0021 |
| Teaching hospital versus nonteaching hospital | 0.873 | 0.709-1.075 | 0.2017 |
| Median household income by patient zip code | |||
| 0-25th percentile | Reference | ||
| 26th-50th percentile | 0.815 | 0.662-1.003 | 0.0531 |
| 51st-75th percentile | 0.795 | 0.652-0.97 | 0.024 |
| 76th-100th percentile | 0.717 | 0.598-0.861 | 0.0004 |
IVT: Intravenous thrombolysis, DHC: Decompressive hemicraniectomy, ICH: Intracerebral hemorrhage, DM: Diabetes mellitus, CHF: Congestive heart failure, PVD: Peripheral vascular disease, OR: Odds ratio, CI: Confidence interval
Table D.
Covariates for adverse discharge outcome, 2015-2017
| Covariates | OR | 95% CI | P |
|---|---|---|---|
| Weekend admission (weekday reference) | 1.117 | 1.02-1.224 | 0.0173 |
| Age groups (years) | |||
| 18-49 | Reference | ||
| 50-79 | 1.692 | 1.458-1.964 | <0.0001 |
| ≥80 | 3.284 | 2.711-3.98 | <0.0001 |
| Female sex (male reference) | 1.084 | 0.993-1.184 | 0.0703 |
| Treatments and complications | |||
| IVT | 0.892 | 0.818-0.974 | 0.0104 |
| DHC | 4.342 | 2-9.428 | 0.0002 |
| ICH | 2.548 | 2.25-2.885 | <0.0001 |
| Hydrocephalus | 2.27 | 1.281-4.023 | 0.005 |
| Cerebral edema | 3.565 | 3.095-4.106 | <0.0001 |
| Comorbidites | |||
| Hypertension | 1.141 | 1.027-1.269 | 0.0145 |
| Smoking | 0.88 | 0.81-0.956 | 0.0025 |
| Drug abuse | 0.951 | 0.714-1.268 | 0.7335 |
| Alcohol abuse | 1.123 | 0.934-1.349 | 0.217 |
| Obesity | 1.143 | 1.007-1.298 | 0.0384 |
| Liver failure | 1.099 | 0.777-1.553 | 0.593 |
| Renal failure | 1.061 | 0.927-1.215 | 0.3861 |
| Hypothyroidism | 0.964 | 0.866-1.072 | 0.4993 |
| Diabetes mellitus | 1.453 | 1.307-1.615 | <0.0001 |
| Hyperlipidemia | 0.845 | 0.781-0.914 | <0.0001 |
| Atrial fibrillation | 1.068 | 0.971-1.175 | 0.1726 |
| CHF | 1.34 | 1.22-1.471 | <0.0001 |
| PVD | 1.199 | 1.07-1.343 | 0.0017 |
| Valvular disorders | 0.884 | 0.784-0.996 | 0.0426 |
| Long-term use of anti-thrombotics | 0.841 | 0.735-0.963 | 0.012 |
| Long-term use of anticoagulants | 0.859 | 0.761-0.971 | 0.0147 |
| Insurance status | |||
| Medicare | Reference | ||
| Medicaid | 0.608 | 0.521-0.71 | <0.0001 |
| Private insurance | 0.567 | 0.505-0.637 | <0.0001 |
| Self-pay | 0.29 | 0.236-0.356 | <0.0001 |
| Other | 0.614 | 0.47-0.802 | 0.0004 |
| Hospital characteristics | |||
| Small bed-size | Reference | ||
| Medium bed-size | 1.539 | 1.146-2.066 | 0.0042 |
| Large bed-size | 1.227 | 0.929-1.62 | 0.1501 |
| Teaching hospital versus nonteaching hospital | 0.957 | 0.759-1.207 | 0.7109 |
| Median household income by patient zip code | |||
| 0-25th percentile | Reference | ||
| 26th-50th percentile | 0.837 | 0.747-0.939 | 0.0024 |
| 51st-75th percentile | 0.836 | 0.744-0.938 | 0.0024 |
| 76th-100th percentile | 0.803 | 0.699-0.922 | 0.0019 |
IVT: Intravenous thrombolysis, DHC: Decompressive hemicraniectomy, ICH: Intracerebral hemorrhage, DM: Diabetes mellitus, CHF: Congestive heart failure, PVD: Peripheral vascular disease, OR: Odds ratio, CI: Confidence interval
References
- 1.Bell CM, Redelmeier DA. Mortality among patients admitted to hospitals on weekends as compared with weekdays. N Engl J Med. 2001;345:663–8. doi: 10.1056/NEJMsa003376. [DOI] [PubMed] [Google Scholar]
- 2.Glance LG, Osler T, Li Y, Lustik SJ, Eaton MP, Dutton RP, et al. Outcomes are worse in US patients undergoing surgery on weekends compared with weekdays. Med Care. 2016;54:608–15. doi: 10.1097/MLR.0000000000000532. [DOI] [PubMed] [Google Scholar]
- 3.Pauls LA, Johnson-Paben R, McGready J, Murphy JD, Pronovost PJ, Wu CL. The weekend effect in hospitalized patients: A meta-analysis. J Hosp Med. 2017;12:760–6. doi: 10.12788/jhm.2815. [DOI] [PubMed] [Google Scholar]
- 4.O'Donnell TF, Schermerhorn ML, Liang P, Li C, Swerdlow NJ, Wang GJ, et al. Weekend effect in carotid endarterectomy. Stroke. 2018;49:2945–52. doi: 10.1161/STROKEAHA.118.022305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Angerer S, Buttinger K, Stummer H. The weekend effect revisited: Evidence from the Upper Austrian stroke registry. Eur J Health Econ. 2019;20:729–37. doi: 10.1007/s10198-019-01035-4. [DOI] [PubMed] [Google Scholar]
- 6.Huang HK, Chang WC, Hsu JY, Wang JH, Liu PS, Lin SM, et al. Holiday season and weekend effects on stroke mortality: A nationwide cohort study controlling for stroke severity. J Am Heart Assoc. 2019;8:e011888. doi: 10.1161/JAHA.118.011888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fang J, Saposnik G, Silver FL, Kapral MK. Investigators of the Registry of the Canadian Stroke Network. Association between weekend hospital presentation and stroke fatality. Neurology. 2010;75:1589–96. doi: 10.1212/WNL.0b013e3181fb84bc. [DOI] [PubMed] [Google Scholar]
- 8.Ogbu UC, Westert GP, Slobbe LC, Stronks K, Arah OA. A multifaceted look at time of admission and its impact on case-fatality among a cohort of ischaemic stroke patients. J Neurol Neurosurg Psychiatry. 2011;82:8–13. doi: 10.1136/jnnp.2009.202176. [DOI] [PubMed] [Google Scholar]
- 9.Adil MM, Vidal G, Beslow LA. Weekend effect in children with stroke in the nationwide inpatient sample. Stroke. 2016;47:1436–43. doi: 10.1161/STROKEAHA.116.013453. [DOI] [PubMed] [Google Scholar]
- 10.Saad A, Adil MM, Patel V, Owada K, Winningham MJ, Nahab F. Clinical outcomes after thrombectomy for acute ischemic stroke on weekends versus weekdays. J Stroke Cerebrovasc Dis. 2014;23:2708–13. doi: 10.1016/j.jstrokecerebrovasdis.2014.06.006. [DOI] [PubMed] [Google Scholar]
- 11.Saber H, Navi BB, Grotta JC, Kamel H, Bambhroliya A, Vahidy FS, et al. Real-world treatment trends in endovascular stroke therapy. Stroke. 2019;50:683–9. doi: 10.1161/STROKEAHA.118.023967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Atchaneeyasakul K, Liaw N, Lee RH, Liebeskind DS, Saver JL. Patterns of mechanical thrombectomy for stroke before and after the 2015 pivotal trials and US national guideline update. J Stroke Cerebrovasc Dis. 2020;29:105292. doi: 10.1016/j.jstrokecerebrovasdis.2020.105292. [DOI] [PubMed] [Google Scholar]
- 13.Powers WJ, Derdeyn CP, Biller J, Coffey CS, Hoh BL, Jauch EC, et al. 2015 American Heart Association/American Stroke Association focused update of the 2013 guidelines for the early management of patients with acute ischemic stroke regarding endovascular treatment: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2015;46:3020–35. doi: 10.1161/STR.0000000000000074. [DOI] [PubMed] [Google Scholar]
- 14.Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015;372:1009–18. doi: 10.1056/NEJMoa1414792. [DOI] [PubMed] [Google Scholar]
- 15.Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015;372:1019–30. doi: 10.1056/NEJMoa1414905. [DOI] [PubMed] [Google Scholar]
- 16.Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015;372:11–20. doi: 10.1056/NEJMoa1411587. [DOI] [PubMed] [Google Scholar]
- 17.Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM, et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med. 2015;372:2285–95. doi: 10.1056/NEJMoa1415061. [DOI] [PubMed] [Google Scholar]
- 18.Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. 2015;372:2296–306. doi: 10.1056/NEJMoa1503780. [DOI] [PubMed] [Google Scholar]
- 19.Shen YC, Chen G, Hsia RY. Community and hospital factors associated with stroke center certification in the United States, 2009 to 2017. JAMA Netw Open. 2019;2:e197855. doi: 10.1001/jamanetworkopen.2019.7855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Saver JL, Goyal M, van der Lugt A, Menon BK, Majoie CB, Dippel DW, et al. Time to treatment with endovascular thrombectomy and outcomes from ischemic stroke: A meta-analysis. JAMA. 2016;316:1279–88. doi: 10.1001/jama.2016.13647. [DOI] [PubMed] [Google Scholar]
- 21.NRD Overview. [Healthcare Cost and Utilization Project (HCUP).] 2017. Available from: http://www.hcup-us.ahrq.gov/nrdoverview.jsp . [Last accessed on 2021 Jul 15]
- 22.HCUP CCS. Rockville, MD: Agency for Healthcare Research and Quality; 2017. Healthcare Cost and Utilization Project (HCUP) Available from: https://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp . [Last accessed on 2021 Jul 15] [PubMed] [Google Scholar]
- 23.Reid LD, Fingar KR. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville (MD): Agency for Healthcare Research and Quality (US); 2006. Inpatient stays and emergency department visits involving traumatic brain injury, 2017: Statistical brief #255. [PubMed] [Google Scholar]
- 24.Qureshi AI, Chaudhry SA, Sapkota BL, Rodriguez GJ, Suri MF. Discharge destination as a surrogate for Modified Rankin Scale defined outcomes at 3- and 12-months poststroke among stroke survivors. Arch Phys Med Rehabil. 2012;93:1408–13. doi: 10.1016/j.apmr.2012.02.032. e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Faigle R, Urrutia VC, Cooper LA, Gottesman RF. Individual and system contributions to race and sex disparities in thrombolysis use for stroke patients in the United States. Stroke. 2017;48:990–7. doi: 10.1161/STROKEAHA.116.015056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Prabhakaran S, McNulty M, O'Neill K, Ouyang B. Intravenous thrombolysis for stroke increases over time at primary stroke centers. Stroke. 2012;43:875–7. doi: 10.1161/STROKEAHA.111.640060. [DOI] [PubMed] [Google Scholar]
- 27.Chaudhry SA, Afzal MR, Chaudhry BZ, Zafar TT, Safdar A, Kassab MY, et al. Rates of adverse events and outcomes among stroke patients admitted to primary stroke centers. J Stroke Cerebrovasc Dis. 2016;25:1960–5. doi: 10.1016/j.jstrokecerebrovasdis.2016.01.045. [DOI] [PubMed] [Google Scholar]
- 28.Stein LK, Agarwal P, Thaler A, Kwon CS, Jette N, Dhamoon MS. Readmission to a different hospital following acute stroke is associated with worse outcomes. Neurology. 2019;93:e1844–51. doi: 10.1212/WNL.0000000000008446. [DOI] [PubMed] [Google Scholar]
- 29.Sidney S, Sorel ME, Quesenberry CP, Jaffe MG, Solomon MD, Nguyen-Huynh MN, et al. Comparative trends in heart disease, stroke, and all-cause mortality in the United States and a large integrated healthcare delivery system. Am J Med. 2018;131:829–36. doi: 10.1016/j.amjmed.2018.02.014. e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Almallouhi E, Al Kasab S, Harvey JB, Reardon C, Alawieh A, Girotra T, et al. Impact of treatment time on the long-term outcome of stroke patients treated with mechanical thrombectomy. J Stroke Cerebrovasc Dis. 2019;28:185–90. doi: 10.1016/j.jstrokecerebrovasdis.2018.09.033. [DOI] [PubMed] [Google Scholar]
- 31.Nikoubashman O, Probst T, Schürmann K, Othman AE, Matz O, Brockmann MA, et al. Weekend effect in endovascular stroke treatment: do treatment decisions, procedural times, and outcome depend on time of admission? J Neurointerv Surg. 2017;9:336–9. doi: 10.1136/neurintsurg-2015-012220. [DOI] [PubMed] [Google Scholar]
- 32.Mpotsaris A, Kowoll A, Weber W, Kabbasch C, Weber A, Behme D. Endovascular stroke therapy at nighttime and on weekends-as fast and effective as during normal business hours? J Vasc Interv Neurol. 2015;8:39–45. [PMC free article] [PubMed] [Google Scholar]
- 33.Almekhlafi MA, Hockley A, Desai JA, Nambiar V, Mishra S, Volny O, et al. Overcoming the evening/weekend effects on time delays and outcomes of endovascular stroke therapy: The Calgary Stroke Program experience. J Neurointerv Surg. 2014;6:729–32. doi: 10.1136/neurintsurg-2013-011000. [DOI] [PubMed] [Google Scholar]
- 34.Rumalla K, Ottenhausen M, Kan P, Burkhardt JK. Recent nationwide impact of mechanical thrombectomy on decompressive hemicraniectomy for acute ischemic stroke. Stroke. 2019;50:2133–9. doi: 10.1161/STROKEAHA.119.025063. [DOI] [PubMed] [Google Scholar]
- 35.Raymond SB, Akbik F, Stapleton CJ, Mehta BP, Chandra RV, Gonzalez RG, et al. Protocols for endovascular stroke treatment diminish the weekend effect through improvements in off-hours care. Front Neurol. 2018;9:1106. doi: 10.3389/fneur.2018.01106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Santana Baskar P, Cordato D, Wardman D, Bhaskar S. In-hospital acute stroke workflow in acute stroke - Systems-based approaches. Acta Neurol Scand. 2021;143:111–20. doi: 10.1111/ane.13343. [DOI] [PubMed] [Google Scholar]
- 37.Chowdhury SZ, Baskar PS, Bhaskar S. Effect of prehospital workflow optimization on treatment delays and clinical outcomes in acute ischemic stroke: A systematic review and meta-analysis. Acad Emerg Med. 2021;28:781–801. doi: 10.1111/acem.14204. [DOI] [PubMed] [Google Scholar]
- 38.Baskar PS, Chowdhury SZ, Bhaskar SM. In-hospital systems interventions in acute stroke reperfusion therapy: A meta-analysis. Acta Neurol Scand. 2021;144:418–32. doi: 10.1111/ane.13476. [DOI] [PubMed] [Google Scholar]
- 39.Mehta BP, Leslie-Mazwi TM, Chandra RV, Bell DL, Sun CH, Hirsch JA, et al. Reducing door-to-puncture times for intra-arterial stroke therapy: A pilot quality improvement project. J Am Heart Assoc. 2014;3:e000963. doi: 10.1161/JAHA.114.000963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sorita A, Ahmed A, Starr SR, Thompson KM, Reed DA, Prokop L, et al. Off-hour presentation and outcomes in patients with acute myocardial infarction: Systematic review and meta-analysis. BMJ. 2014;348:f7393. doi: 10.1136/bmj.f7393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: A meta-analysis of individual patient data from five randomised trials. Lancet. 2016;387:1723–31. doi: 10.1016/S0140-6736(16)00163-X. [DOI] [PubMed] [Google Scholar]
- 42.Jayaraman MV, McTaggart RA. Endovascular treatment of anterior circulation large vessel occlusion in the elderly. Front Neurol. 2017;8:713. doi: 10.3389/fneur.2017.00713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sussman ES, Martin B, Mlynash M, Marks MP, Marcellus D, Albers G, et al. Thrombectomy for acute ischemic stroke in nonagenarians compared with octogenarians. J Neurointerv Surg. 2020;12:266–70. doi: 10.1136/neurintsurg-2019-015147. [DOI] [PubMed] [Google Scholar]
- 44.Becker KJ, Baxter AB, Cohen WA, Bybee HM, Tirschwell DL, Newell DW, et al. Withdrawal of support in intracerebral hemorrhage may lead to self-fulfilling prophecies. Neurology. 2001;56:766–72. doi: 10.1212/wnl.56.6.766. [DOI] [PubMed] [Google Scholar]
- 45.Rinaldo L, Rabinstein AA, Cloft H, Knudsen JM, Castilla LR, Brinjikji W. Racial and ethnic disparities in the utilization of thrombectomy for acute stroke. Stroke. 2019;50:2428–32. doi: 10.1161/STROKEAHA.118.024651. [DOI] [PubMed] [Google Scholar]


