Abstract
IMPORTANCE
Massachusetts introduced health care reform (HCR) in 2006, expecting to expand health insurance coverage and improve outcomes. Because traumatic injury is a common acute condition with important health, disability, and economic consequences, examination of the effect of HCR on patients hospitalized following injury may help inform the national HCR debate.
OBJECTIVE
To examine the effect of Massachusetts HCR on survival rates of injured patients.
DESIGN, SETTING, AND PARTICIPANTS
Retrospective cohort study of 1 520 599 patients hospitalized following traumatic injury in Massachusetts or New York during the 10 years (2002-2011) surrounding Massachusetts HCR using data from the State Inpatient Databases. We assessed the effect of HCR on mortality rates using a difference-in-differences approach to control for temporal trends in mortality.
INTERVENTION
Health care reform in Massachusetts in 2006.
MAIN OUTCOME AND MEASURE
Survival until hospital discharge.
RESULTS
During the 10-year study period, the rates of uninsured trauma patients in Massachusetts decreased steadily from 14.9% in 2002 to 5.0.% in 2011. In New York, the rates of uninsured trauma patients fell from 14.9% in 2002 to 10.5% in 2011. The risk-adjusted difference-in-difference assessment revealed a transient increase of 604 excess deaths (95% CI, 419-790) in Massachusetts in the 3 years following implementation of HCR.
CONCLUSIONS AND RELEVANCE
Health care reform did not affect health insurance coverage for patients hospitalized following injury but was associated with a transient increase in adjusted mortality rates. Reducing mortality rates for acutely injured patients may require more comprehensive interventions than simply promoting health insurance coverage through legislation.
For most Americans, access to health care is mediated by health insurance. Indeed, extending health insurance to more citizens is the centerpiece of the federal government’s efforts to reform the health care system. However, although insurance coverage is associated with improved outcomes for some chronic conditions, such as diabetes mellitus,1 less is known about the effect of health insurance on acute conditions, such as traumatic injury.
The advent of health care reform (HCR) in Massachusetts in 2006 dramatically improved health insurance coverage for the residents of Massachusetts, and this event has been used as a natural experiment to examine the effect of expanded health insurance on several health outcomes.2-5 The goal of this study is to explore the effect of HCR in Massachusetts on insurance coverage and survival in patients hospitalized following traumatic injury. Because all injured persons have access to emergency care, we might expect that survival would be unrelated to a patient’s having health insurance, but several researchers have reported improved survival rates following injury in patients with insurance.6 Thus, the relationship of insurance to survival after injury may not yet be well understood. Our examination of the Massachusetts HCR bellwether may provide guidance to policymakers as they work to further expand health care coverage in the United States.
Methods
Data Source and Case Definition
This analysis was conducted using data from the Healthcare Cost and Utilization Project State Inpatient Databases, a data set that encompasses about 97% of community hospital discharges. We examined data from Massachusetts and New York during the 10 years surrounding Massachusetts HCR (2002-2011), which included 8 417 177 patients admitted to 1 of 154 hospitals in Massachusetts and 26 045 954 patients admitted to 1 of 251 hospitals in New York. The study sample consisted of 1 816 322 trauma patients, defined as any patient with 1 or more International Classification of Diseases, Ninth Revision, codes in the range of 800 through 959.97 (excluding late effects of injury [905-909], foreign bodies [930-939], burns [940-949], and complications of trauma [958]) and an eCode8 that corresponded to 1 of 8 clinical mechanisms of traumatic injury: gunshot wound, self-inflicted gunshot wound, low fall, motor vehicle crash, pedestrian injury, other blunt injuries, stab wound, and laceration. We limited our study to white, black, and Hispanic patients. Patients were defined as uninsured if they were coded as “self-pay” or “no charge.” We excluded 108 584 patients who were younger than 16 years for whom injury severity models based on International Classification of Diseases, Ninth Revision, codes have not been extensively evaluated. We also excluded 52 976 patients who were transferred to another hospital rather than being discharged because we were unable to determine the final survival status of these patients. The final data set included 410 640 trauma patients with an overall mortality of 2.51% from Massachusetts and 1 110 355 trauma patients with an overall mortality of 2.70% from New York. The institutional review board of the University of Vermont judged this research exempt from review because it did not constitute human subjects research.
Statistical Analysis
Trauma is a different event for patients who are older than 64 years. Elderly persons are 3 times more likely to die than the young, are subject to different mechanisms of injury, and almost always have health insurance (ie, Medicare). Because these 2 subsets of our patient population are so different, we performed separate identical analyses for the 2 groups.
We performed exploratory analyses to examine temporal changes in the proportion of younger patients hospitalized following injury who were uninsured in Massachusetts and New York and compared the result with the insured proportion of the population of these states using data from the US Census Bureau.9
We fit 2 logistic regression models that used mortality as the outcome, one for younger patients and one for elderly patients, that adjusted for identical predictors: age, sex, traumatic shock (International Classification of Diseases, Ninth Revision, code 958.4), extent of anatomical injury (expressed as the logit transformation of the probability of mortality derived from all International Classification of Diseases, Ninth Revision, injury codes using the Trauma Mortality Prediction Model10), mechanism of injury, 11 comorbidities (computed using Healthcare Cost and Utilization Project Comorbidity Software11), and race (coded as white, black, or Hispanic). Insurance status was not included as a predictor in these models because our interest centered on the effect of HCR and we wished to allow for the possibility that HCR might influence survival through its (possible) effect on insurance status. We used robust variance estimators12 to adjust for the correlation of outcomes in individual hospitals.
We computed the excess mortality rate for individual patients as the difference between each patient’s observed and expected mortality rate predicted by our logistic model. We computed excess deaths per 1000 patients for each state-per-year combination as well as the 4 strata required to compute the difference in differences (DinD) result (Massachusetts before HCR, Massachusetts after HCR, New York before HCR, and New York after HCR) as follows:
| (1) |
Where the subscript i indexes all patients within strata j, each strata represents 1 of the 20 possible state-calendar year combinations, and Nj is the number of patients within each such strata.
We then computed the single DinD value of excess deaths per 1000 admissions as:
| (2) |
Confidence intervals were computed using 100 bootstrap resamplings of the data set, stratified by hospital. The underlying logistic regression model contained no predictors that involved either the year or state in which a patient was hospitalized.
All data manipulation and statistical analysis was conducted using Stata/MP, version 13.1 (StataCorp LP).
Results
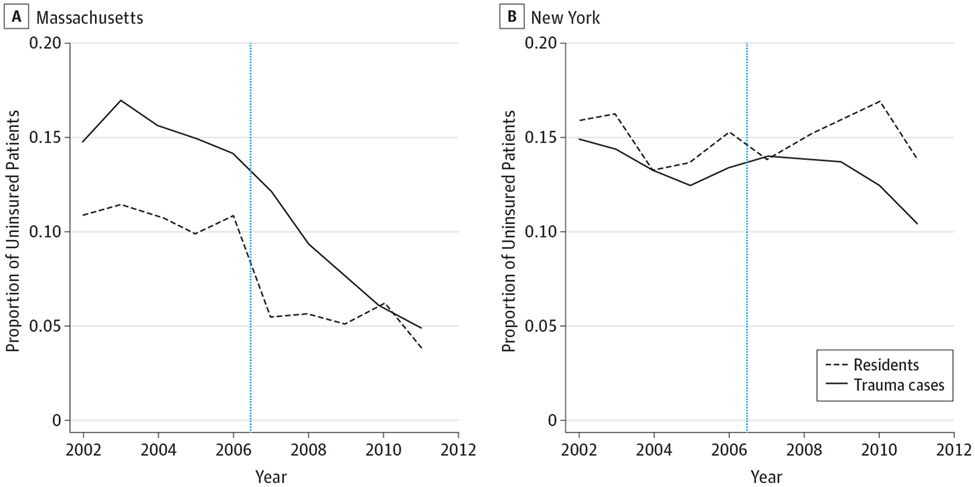
Characteristics of younger and older patients are presented in Table 1 and Table 2. The US Census Bureau reported a 50% reduction in the proportion of uninsured residents in Massachusetts in the year following HCR (Figure 1A). In comparison, HCR had no effect on the proportion of uninsured trauma patients, which steadily decreased throughout the study period, but experienced no obvious change related to HCR. Although a substantial difference in the proportion of Massachusetts residents and Massachusetts trauma patients was evident in 2002, this difference steadily decreased during the 10 years of our study and was eliminated by 2010. New York, which did not adopt HCR, shows no clear trend in the uninsured proportion over time for either residents or trauma patients (Figure 1B). The unadjusted mortality rates were similar before and after HCR in Massachusetts and New York for young patients. The rates in Massachusetts were 1.21% (95% CI, 1.13%-1.30%) pre-HCR and 1.22% (95% CI, 1.15%-1.30%) post-HCR. The rates in New York were 1.43% (1.38%-1.49%) pre-HCR and 1.32% (1.28%-1.37%) post-HCR. The unadjusted mortality rates were higher in the older patient cohort before and after HCR in Massachusetts and New York. The rates in Massachusetts were 3.69% (95% CI, 3.57%-3.82%) pre-HCR and 3.55% (95% CI, 3.44%-3.66%) post-HCR. The rates in New York were 4.50% (95% CI, 4.41%-4.59%) pre-HCR and 3.98% (95% CI, 3.90%-4.05%) post-HCR.
Table 1.
Characteristics of Younger Patients Admitted to the Hospital Following Injurya
| Massachusetts |
New York |
||||
|---|---|---|---|---|---|
| Variable | Patients | Before 2006 | After 2006 | Before 2006 | After 2006 |
| Total, No. | 581 067 | 63 528 | 82 647 | 184 182 | 250 710 |
| Age, mean (median), y | 41.3 (43) | 41.2 (43) | 43.2 (46) | 40.1 (41) | 41.6 (44) |
| Uninsured, % | 12.1 | 15.2 | 7.7 | 12.7 | 12.1 |
| Insurance type, % | |||||
| Medicare | 10.1 | 11.5 | 14.6 | 7.9 | 10.0 |
| Medicaid | 22.2 | 13.6 | 17.5 | 22.3 | 25.7 |
| Private | 47.1 | 51.5 | 48.9 | 48.4 | 44.6 |
| Self pay | 10.4 | 7.9 | 3.3 | 12.4 | 11.8 |
| No charge | 1.7 | 7.6 | 4.4 | 0.3 | 0.3 |
| Other | 8.6 | 8.0 | 8.6 | 8.8 | 7.7 |
| Race, % | |||||
| White | 67.3 | 83.1 | 81.2 | 63.9 | 61.5 |
| Black | 19.0 | 8.4 | 9.0 | 22.5 | 22.4 |
| Hispanic | 13.7 | 8.4 | 9.8 | 13.6 | 16.2 |
| Mechanism, % | |||||
| Blunt trauma | 56.4 | 53.2 | 55.9 | 56.2 | 57.8 |
| Gunshot | 2.4 | 1.5 | 1.7 | 2.8 | 2.5 |
| Gunshot, self-inflicted | 0.2 | 0.2 | 0.1 | 0.3 | 0.2 |
| Low fall | 14.0 | 15.6 | 17.6 | 11.8 | 14.3 |
| Motor vehicle crash | 12.0 | 15.0 | 10.9 | 13.5 | 10.4 |
| Injury to pedestrian | 6.7 | 6.1 | 5.8 | 7.0 | 6.9 |
| Stabbing | 3.9 | 3.2 | 3.1 | 4.5 | 3.8 |
| Laceration | 4.4 | 5.2 | 4.9 | 4.0 | 4.2 |
| Shock, % | 0.5 | 0.4 | 0.7 | 0.3 | 0.6 |
| Hospital stay, mean (median), d | |||||
| Survivors | 5.6 (3) | 5.1 (3) | 4.6 (3) | 5.8 (3) | 5.8 (3) |
| Nonsurvivors | 9.4 (3) | 6.7 (2) | 6.3 (3) | 9.9 (3) | 10.7 (4) |
| Mortality, % | 1.3 | 1.2 | 1.2 | 1.4 | 1.3 |
Defined as older than 15 and younger than 65 years.
Table 2.
Characteristics of Elderly Patients Admitted to the Hospital Following Injurya
| Massachusetts |
New York |
||||
|---|---|---|---|---|---|
| Variable | Patients | Before 2006 | After 2006 | Before 2006 | After 2006 |
| Total, No. | 704 189 | 90 306 | 116 683 | 205 974 | 291 226 |
| Age, mean (median), y | 81.56 (82) | 81.67 (82) | 81.91 (83) | 81.25 (82) | 81.59 (82) |
| Uninsured, % | 0.53 | 0.70 | 0.33 | 0.54 | 0.56 |
| Insurance type | |||||
| Medicare | 89.00 | 90.59 | 90.72 | 87.60 | 88.75 |
| Medicaid | 1.02 | 0.32 | 0.50 | 1.73 | 1.01 |
| Private | 8.40 | 7.63 | 7.56 | 9.23 | 8.37 |
| Self pay | 0.50 | 0.58 | 0.30 | 0.53 | 0.54 |
| No charge | 0.03 | 0.13 | 0.03 | 0.01 | 0.02 |
| Other | 1.06 | 0.76 | 0.88 | 0.91 | 1.31 |
| Race, % | |||||
| White | 90.80 | 97.64 | 96.49 | 90.28 | 86.86 |
| Black | 4.88 | 1.50 | 1.76 | 5.69 | 6.60 |
| Hispanic | 4.31 | 0.86 | 1.74 | 4.03 | 6.54 |
| Mechanism, % | |||||
| Blunt trauma | 59.64 | 58.17 | 57.23 | 63.36 | 58.76 |
| Gunshot | 0.02 | 0.01 | 0.01 | 0.02 | 0.02 |
| Gunshot, self-inflicted | 0.01 | 0.01 | 0.01 | 0.01 | 0.02 |
| Low fall | 35.87 | 37.53 | 39.35 | 31.36 | 36.87 |
| Motor vehicle crash | 2.95 | 3.02 | 2.33 | 3.51 | 2.77 |
| Injury to pedestrian | 1.02 | 0.8 | 0.60 | 1.26 | 1.07 |
| Stabbing | 0.09 | 0.08 | 0.07 | 0.09 | 0.08 |
| Laceration | 0.40 | 0.39 | 0.40 | 0.39 | 0.41 |
| Shock, % | 0.13 | 0.07 | 0.20 | 0.08 | 0.15 |
| Hospital stay, mean (median), d | |||||
| Survivors | 6.69 (5) | 5.66 (4) | 5.05 (4) | 7.73 (6) | 6.90 (5) |
| Nonsurvivors | 10.60 (6) | 8.08 (5) | 7.03 (5) | 12.39 (8) | 11.16 (7) |
| Mortality, % | 4.02 | 3.69 | 3.55 | 4.50 | 3.98 |
Defined as older than 64 years.
Figure 1. Proportion of Population Younger Than 65 Years Without Insurance by State and Year.
A, In Massachusetts, the uninsured rates for trauma patients gradually decreased while the decrease for nontrauma patients was concentrated around the introduction of health care reform. B, In New York, the uninsured rates remained largely unchanged. The vertical blue line indicates the introduction of health care reform in 2006.
The 2 logistic mortality models, one for younger patients and one for elderly patients, accurately discriminated between survivors and nonsurvivors. The area under the receiver operating characteristic curve was 0.93 for the younger patients and 0.79 for the elderly patients. Although the 2 models used identical predictors, the model for elderly patients had a lower receiver operating characteristic statistic, reflecting the greater difficulty involved in predicting mortality in this group of patients whose clinical outcome may be driven more by comorbidities and complications than by acute injuries.13 Calibration plots showed close agreement between the observed and expected rates of insurance for both models.
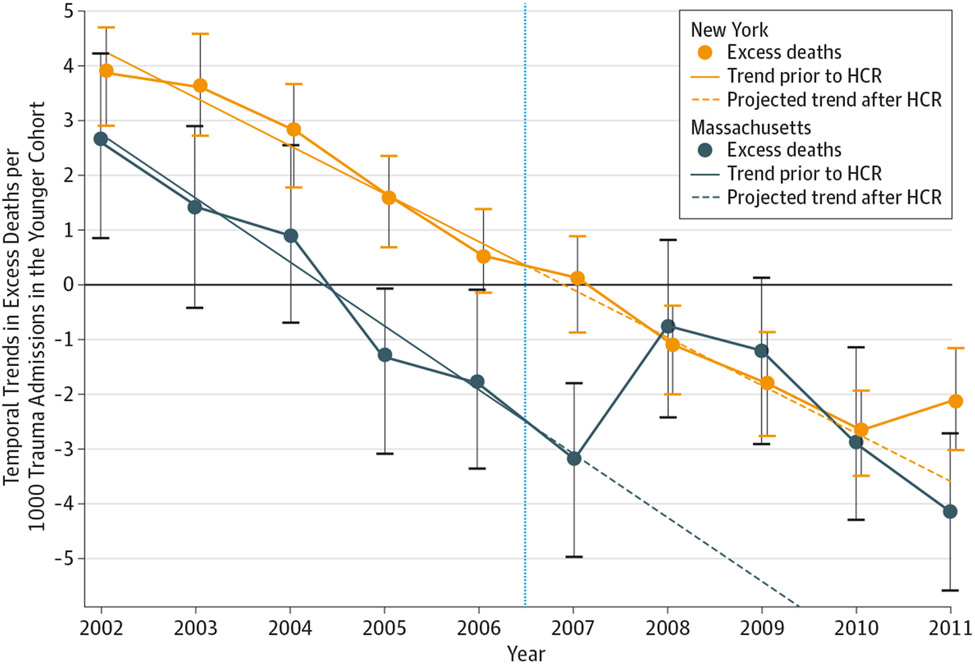
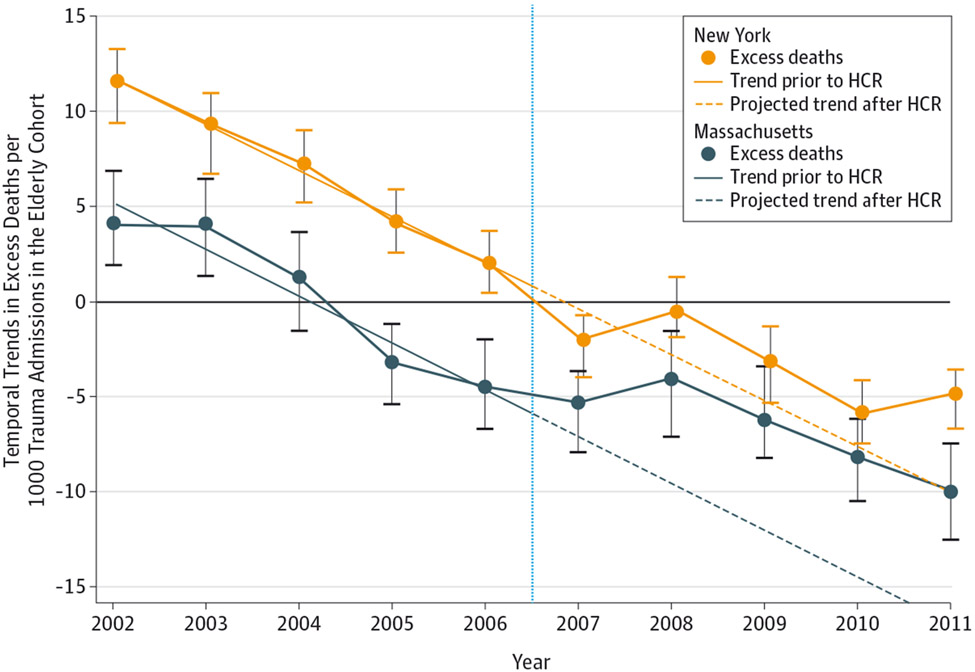
A risk-adjusted DinD model fit to the younger patients found 105 excess deaths (95% CI, 35-180) among the younger group during the post-HCR period in Massachusetts. A model using the same predictors was fit to patients older than 64 years and found 499 excess deaths (95% CI, 313-669) in the post-HCR period in Massachusetts. Overall, there were 604 excess deaths (95% CI, 419-790) attributable to HCR, approximately 12.0% of all post-HCR deaths in Massachusetts. Among the younger cohort, the fewer excess deaths in Massachusetts trauma patients were seen throughout the study period, except for a transient increase from 2008 through 2010 that returned back to the lower trend of fewer excess deaths by 2011 (eTable 1 in the Supplement). Among the elderly cohort of Massachusetts trauma patients, the same trend for fewer excess deaths was seen throughout the study period, with a small transient increase in 2008 that returned to fewer excess deaths from 2009 through 2011 (eTable 2 in the Supplement). Plots of excess deaths per 1000 admissions during the 10 years of our study show that, in general, outcomes in Massachusetts are better than in New York but that in the period following HCR, excess mortality rates in Massachusetts transiently increased for both younger (Figure 2) and elderly (Figure 3) trauma patients. In the younger patients, the increase in excess deaths following HCR in Massachusetts is striking, but the effect of HCR on excess deaths is more subtle for the elderly patients. Nevertheless, examination of the graph for elderly patients (Figure 3) shows that there were fewer excess deaths in Massachusetts than New York in every year before HCR but that the number of excess deaths in Massachusetts and New York were similar in each year following HCR, highlighting the increased adjusted mortality rate among the elderly in Massachusetts following HCR.
Figure 2. Temporal Trends in Excess Deaths per 1000 Trauma Admissions in the Younger Cohort.
In New York, the number of excess trauma deaths per 1000 admissions gradually decreased over time, while in Massachusetts, an increase in excess trauma deaths per 1000 admissions followed the introduction of health care reform and continued for 3 years. The vertical blue line indicates the introduction of health care reform in 2006; error bars, 95% CIs. Separate trend lines have been superimposed on excess deaths per 1000 admissions for Massachusetts and New York in the period prior to the introduction of health care reform and extrapolated into the 5 years following health care reform. The horizontal line at 0 divides more excess deaths from fewer excess deaths.
Figure 3. Temporal Trends in Excess Deaths per 1000 Trauma Admissions in the Elderly Cohort.
In New York, the number of excess trauma deaths per 1000 admissions gradually decreased over time, while in Massachusetts, a similar gradual decrease was interrupted following the introduction of health care reform. Since all elderly patients are insured, these trends must be unrelated to insurance status. The vertical blue line indicates the introduction of health care reform in 2006; error bars, 95% CIs. Separate trend lines have been superimposed on excess deaths per 1000 admissions for Massachusetts and New York in the period prior to the introduction of health care reform and extrapolated into the 5 years following health care reform. The horizontal line at 0 divides more excess deaths from fewer excess deaths.
Discussion
Introduced in Massachusetts in 2006, HCR was a bold experiment that deserves careful examination in its own right and because it may prefigure aspects of national HCR.
In our analysis, we sought to understand the effect of HCR on survival following traumatic injury by comparing mortality rates in Massachusetts before and after HCR with those of a contiguous state (New York) that did not implement HCR. Such DinD models have long been used by economists to examine the effects of policy changes14 and increasingly are being used by health care researchers.15
The US Census Bureau reports that in its first year, Massachusetts HCR was associated with a 50% reduction in the percentage of uninsured Massachusetts residents, but we found that this improvement did not apply to patients who were hospitalized following an injury. Because private insurers naturally prefer to enroll low-risk clients, this observation has face validity, but the ability of private insurers to so accurately identify young patients who are at risk for traumatic injury seems preternatural. We did observe a steady reduction in the percentage of uninsured young trauma patients in Massachusetts that erased the difference between the proportions of uninsured residents and uninsured trauma patients by the end of the 10-year study period, but because this steady improvement was under way 4 years before HCR, it seems unlikely that this improvement was a result of HCR. Health care reform could make no substantive difference in insurance coverage for elderly persons because almost all elderly patients had health insurance before the implementation of HCR and continued to be insured afterward.
Our finding that HCR was associated with a transient increase in excess deaths was unexpected. Indeed, given the described association between insurance coverage and increased survival in trauma patients,16 we had expected excess deaths in Massachusetts to decline as a result of slowly increasing insurance coverage in Massachusetts during the study period. However, it is possible that insurance coverage does not improve survival following injury. Instead, it may be that the previously reported advantage of insured patients is an epiphenomenon, the result of hospital administrators’ efforts to obtain insurance coverage for uninsured trauma patients immediately after hospital admission. Many patients who die will die without insurance simply because early death prevented hospital staff from obtaining insurance for them. This spurious cause-and-effect relationship between insurance coverage and survival is the result of survivor treatment assignment bias,17 a well-known but often ignored18 problem that can arise when a time-dependent treatment, such as insurance status, is specified as if it is fixed at baseline. The risk of survivor treatment assignment bias among young trauma patients is especially high because both death and change in insurance status typically occur early in patients’ hospital stays. A recent analysis of trauma patients in a data set similar to the State Inpatient Databases, the National Inpatient Sample, found that the apparent association of health insurance with increased survival was entirely due to survivor treatment assignment bias.19 However, even granting that HCR might not have been expected to reduce excess deaths in the young as a result of increased insurance coverage, the finding that excess deaths increased in the young following HCR is troubling.
Fortunately, the increase in mortality among trauma patients following Massachusetts HCR resolved within a few years. It may not be possible to retrospectively reconstruct the causal pathway responsible for the increased excess deaths following HCR and its subsequent resolution. Indeed, it is unlikely that HCR was the only factor involved because other events, such as an economic recession, coincided with HCR and cannot be ruled out as in some way contributory. However, the recession also affected New York, and our DinD design implicitly controls for the recession as well as any other unspecified events that may have affected both Massachusetts and New York in a similar manner. Although the State Inpatient Databases data set does not allow us to speculate on the mechanism by which HCR may have undermined survival in our cohort of injured patients, we can offer one observation: adjusted mortality rates increased following HCR in both the younger and elderly cohorts in our analysis. Because almost all patients in the elderly cohort had health insurance before and after the introduction of HCR, the increase in mortality rates in the elderly cohort cannot have been directly related to insurance status. Thus, insurance coverage per se is unlikely to be the cause of the observed increase in mortality.
Two other groups have recently reported worse outcomes in Massachusetts following HCR. Albert et al20 studied patients who underwent invasive cardiovascular procedures before and after Massachusetts HCR and found an increase in hospital-adjusted odds of death following HCR among less-educated patients. Lasser et al5 found that hospital readmission rates increased in Massachusetts compared with New Jersey and New York following HCR, leading these authors to observe, “… Massachusetts health reform—which only dealt with payment mechanisms rather than the organization of care—had no impact on the increasing fragmentation of patient care and lack of coordinated care transitions that may perpetuate high readmission rates.” Our finding that mortality rates increased for trauma patients following HCR is perhaps the most unsettling result to date but likely stems from the same root cause: administratively encouraging insurance coverage fails to address, and may even undermine, the fundamental structural changes required to improve health care outcomes.
Our study has limitations. Although DinD models allow researchers to control for many sources of potential bias, these models rely on the assumption that the comparison group experiences a temporal trend in outcome similar to the experimental group. Although Massachusetts and New York are contiguous states, we cannot rule out the possibility that New York experienced trends in traumatic injury or care of trauma patients that differed from Massachusetts. In addition, our study is based on administrative data and is subject to all the limitations of such data sets.
Conclusions
We find that although the percentage of uninsured residents in Massachusetts sharply decreased following HCR, the percentage of uninsured trauma patients showed no such inflection. Instead, the percentage of uninsured trauma patients steadily declined during the 10 years surrounding HCR. In addition, we find that HCR in Massachusetts was associated with a transiently increased adjusted mortality rate, accounting for as many as 604 excess deaths during 4 years.
There are compelling arguments for providing health insurance to all citizens of the United States, but our analysis suggests that simply providing health insurance incentives and subsidies does not improve survival for trauma patients. Devoting resources directly to the infrastructure of health care may be a more effective strategy than simply spending these resources on increased insurance coverage. Ours is thus a cautionary tale for health care reformers: successful HCR for trauma patients will likely require more complex interventions than simply promoting health insurance coverage legislatively.
Supplementary Material
Funding/Support:
This study was supported by grant R01MD006231 from the National Institute on Minority Health and Health Disparities, National Institutes of Health.
Role of the Funder/Sponsor:
The National Institute on Minority Health and Health Disparities, National Institutes of Health, had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Conflict of Interest Disclosures: None reported.
Contributor Information
Turner Osler, Department of Surgery, University of Vermont, Colchester.
Laurent G. Glance, Department of Anesthesiology, University of Rochester, Rochester, New York.
Wenjun Li, Department of Medicine, University of Massachusetts Medical School, Worcester.
Jeffery S. Buzas, Department of Mathematics and Statistics, University of Vermont, Burlington.
David W. Hosmer, School of Public Health and Health Sciences, University of Massachusetts, Worcester.
REFERENCES
- 1.Flavin NE, Mulla ZD, Bonilla-Navarrete A, et al. Health insurance and the development of diabetic complications. South Med J. 2009;102(8):805–809. [DOI] [PubMed] [Google Scholar]
- 2.Loehrer AP, Song Z, Auchincloss HG, Hutter MM. Massachusetts health care reform and reduced racial disparities in minimally invasive surgery. JAMA Surg. 2013;148(12):1116–1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bond AM, White C. Massachusetts coverage expansion associated with reduction in primary care utilization among Medicare beneficiaries. Health Serv Res. 2013;48(6, pt 1):1826–1839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sommers BD, Long SK, Baicker K. Changes in mortality after Massachusetts health care reform: a quasi-experimental study. Ann Intern Med. 2014;160(9):585–593. [DOI] [PubMed] [Google Scholar]
- 5.Lasser KE, Hanchate AD, McCormick D, Manze MG, Chu C, Kressin NR. The effect of Massachusetts health reform on 30 day hospital readmissions: retrospective analysis of hospital episode statistics. BMJ. 2014;348:g2329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Haider AH, Weygandt PL, Bentley JM, et al. Disparities in trauma care and outcomes in the United States: a systematic review and meta-analysis. J Trauma Acute Care Surg. 2013;74(5):1195–1205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Boufous S, Williamson A. Reporting of the incidence of hospitalised injuries: numerator issues. Inj Prev. 2003;9(4):370–375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lawrence BA, Miller TR, Weiss HB, Spicer RS. Issues in using state hospital discharge data in injury control research and surveillance. Accid Anal Prev. 2007;39(2):319–325. [DOI] [PubMed] [Google Scholar]
- 9.US Census Bureau. Health insurance historical tables: HIB series. http://www.census.gov/hhes/www/hlthins/data/historical/HIB_tables.html. Accessed February 16, 2014. [Google Scholar]
- 10.Glance LG, Osler TM, Mukamel DB, Meredith W, Wagner J, Dick AW. TMPM-ICD9: a trauma mortality prediction model based on ICD-9-CM codes. Ann Surg. 2009;249(6):1032–1039. [DOI] [PubMed] [Google Scholar]
- 11.Healthcare Cost and Utilization Project. Comorbidity software, version 3.7. http://www.hcup-us.ahrq.gov/toolssoftware/comorbidity/comorbidity.jsp. Accessed February 17, 2014. [Google Scholar]
- 12.Williams RL. A note on robust variance estimation for cluster-correlated data. Biometrics. 2000;56(2):645–646. [DOI] [PubMed] [Google Scholar]
- 13.Osler T, Hales K, Baack B, et al. Trauma in the elderly. Am J Surg. 1988;156(6):537–543. [DOI] [PubMed] [Google Scholar]
- 14.Angrist JD, Pischke JS. Mostly Harmless Econometrics: An Empiricist's Companion. Princeton, NJ: Princeton University Press; 2008. [Google Scholar]
- 15.French B, Heagerty PJ. Analysis of longitudinal data to evaluate a policy change. Stat Med. 2008;27(24):5005–5025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Haider AH, Weygandt PL, Bentley JM, Monn MF, Rehman KA, Zarzaur BL, Cooper LA. Disparities in trauma care and outcomes in the United States: a systematic review and meta-analysis. J Trauma Acute Care Surg. 2013;74(5):1195–1205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Austin PC, Mamdani MM, van Walraven C, Tu JV. Quantifying the impact of survivor treatment bias in observational studies. J Eval Clin Pract. 2006;12(6): 601–612. [DOI] [PubMed] [Google Scholar]
- 18.van Walraven C, Davis D, Forster AJ, Wells GA. Time-dependent bias was common in survival analyses published in leading clinical journals. J Clin Epidemiol. 2004;57(7):672–682. [DOI] [PubMed] [Google Scholar]
- 19.Osler T, Glance LG, Li W, Buzas JS, Wetzel ML, Hosmer DW. The association of race and health insurance with mortality following traumatic injury. J Trauma. In press. [Google Scholar]
- 20.Albert MA, Ayanian JZ, Silbaugh TS, et al. Early results of Massachusetts healthcare reform on racial, ethnic, and socioeconomic disparities in cardiovascular care. Circulation. 2014;129(24):2528–2538. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.