Abstract
Background
Cardiopulmonary rehabilitation (CR) is an effective management approach for heart failure (HF) patients and is delivered by multidisciplinary teams including physiotherapists (PTs). PT attitudes about delivering CR and barriers that might affect referral have not been explored. Thus, this study is aimed to explore PT attitudes about delivering CR programs to patients with HF and identify factors and barriers that might affect referral decisions.
Methods
A cross-sectional online survey was disseminated to all PTs in Saudi Arabia between 19 February and 27 June, 2022. The characteristics of the respondents were described using descriptive statistics. Percentages and frequencies were used to report categorical variables.
Results
Overall, 553 PTs, 289 (52.30%) male and 264 (47.70%) females, completed the online survey. Of these, 360 (65.1%) strongly agreed that CR would improve patients’ physical fitness and 334 (60.4%) strongly agreed that CR would reduce breathlessness in patients with HF. The majority of PTs (321, 58%) strongly agreed that CR would improve HF patients’ palpitation and fatigue. Out of 553 PTs, 349 (63.1%) strongly agreed that CR would improve patients’ ability to perform daily activities. A hospital-supervised program was the preferred mode of delivering CR programs by 499 (90.20%) of the respondents. Apart from the exercise component, stress management was perceived by 455 (82.30%) as an essential component of CR programs. The most common patient-related factor that strongly influenced referral decisions was “fatigue related to disease” (42%). A lack of CR centers was reported by 59.90% as the most common referring barrier.
Conclusion
PTs perceived CR as a successful strategy for patients with HF. Although a supervised hospital-based program with stress management as an essential component aside from the exercise component was perceived as the preferred mode of delivery, CR was lacking, which caused a significant barrier to CR referral from the PTs’ perspective.
Keywords: cardiopulmonary rehabilitation, heart failure, HF, physiotherapists, PT, Saudi Arabia
Introduction
Heart failure (HF) is a serious clinical syndrome associated with signs and symptoms that result from the heart being unable to pump enough blood to meet the body’s needs, leading to reduced organ perfusion and, ultimately, death unless it is treated appropriately.1 HF is a leading cause of morbidity and mortality globally.2 Functional impairment and exercise intolerance are common symptoms in patients with HF. These symptoms frequently worsen with exertion, eventually leading to exacerbations and unnecessary emergency hospital visits.1
Although HF is not curable, the use of pharmacologic and non-pharmacologic interventions can reduce exacerbations and hospitalization.1 One of the mainstays of non-pharmacologic therapy strategies for individuals with HF is cardiopulmonary rehabilitation (CR). CR for patients with HF is a comprehensive multidisciplinary program that includes exercise and educational sessions and outcomes assessment, aiming to improve functional capacity and quality of life.2 A CR program should include a medical examination, patient education, nutritional support, mental health, and psychosocial support, and physical activity counselling.3,4 Given that a CR team from different disciplines is needed to provide these services, a CR team typically includes, but is not limited to, doctors, nurses, physiotherapists (PTs), dietitians, psychologists, and social workers.2,5
Historically, physical activity for patients with HF was thought to aggravate the disease. Several lines of evidence have controversially supported the participation of patients with HF in physical activity as it has been reported that exercise training is safe and well-tolerated in stable patients following HF diagnosis.6–9 Furthermore, studies have shown that CR can reduce hospitalization and improve functional ability, exercise duration, quality of life, peak oxygen consumption and endothelial function in individuals with HF.3,10–14 Interestingly, CR services remain underused globally, including in Saudi Arabia.2,15,16 To the best of our knowledge, Saudi Arabia has only one CR center specifically for patients with cardiovascular diseases, including HF.16 Enhancing the implementation of CR programs in Saudi Arabia requires assessing the attitudes and expectations of healthcare workers, including PTs, about such programs. The important role of PTs in CR includes but is not limited to prescribing a tailored exercise program, providing sufficient details about exercise, running CR programs, and conducting patients’ pre-CR evaluations.16–19 In addition, no previous study explores factors and barriers that may influence PTs’ referral decisions to CR programs in Saudi Arabia. Thus, the purpose of the current study is to assess PTs’ attitudes about delivering CR programs to patients with HF and to identify potential factors and barriers that may affect referral decisions.
Methods
Study Design
This is a cross-sectional study conducted between 19 February and 27 June 2022. An online survey platform (Survey Monkey) was used to distribute the survey and collect data.
Questionnaire Tool
We used a modified version of a survey that was previously designed, created, and validated by Aldhahir et al20–23 The questionnaire included eight closed-ended multiple-choice questions.
Participants were informed of the study’s objective and the identity of the principal investigator before beginning the questionnaire. The survey began with a question asking participants if they were interested and willing to participate in this study. The survey stated, “By answering yes in completing the survey question, you freely agree to engage in this study and offer your agreement to utilize your anonymous data for research purposes”. Three to five minutes were the expected duration to complete the questionnaire. The first part collected data about demographic information. The second part asked participants about three domains: effectiveness, components, and delivery methods of CR. This section offered a 5-point Likert scale for responses to all statements, ranging from 1 for “strongly disagree” to 5 for “strongly agree”. The last part asked participants about the patient- and process-related factors that influence referral decisions to CR. Participants were asked to grade factors. The options in this part were “no influence”, “some influence”, and “strong influence”.
Study Population and Sampling Strategy
A convenience sampling strategy was used to recruit participants in this study. The target population was PTs who worked or had potential contact with HF cases. To reach more professionals working in Saudi Arabia, the questionnaire was distributed by the official PT committee and social media (Twitter, WhatsApp, Telegram). The criteria for inclusion in the study were clearly specified in the study invitation.
Sample Size
The design of the study was exploratory; therefore, sample size calculation was not required.
Ethical Approval
Jazan University’s Institutional Review Board approved the study, reference number REC-43/03/041.
Statistical Analysis
The Statistical Package for Social Sciences (SPSS) software Version 25 was used to analyze the data. The reported and displayed categorical variables used percentages and frequencies.
Results
Overall, 553 PTs both male 289 (52.3%) and female 264 (47.7%) completed the online survey between 19 February and 27 June 2022. Respondents were distributed across the Kingdom’s regions as follows: 204 (37%) were from the western region, 160 (29%) were from the central region, 100 (18%) were from the eastern region, 56 (10%) were from the southern region and 33 (6%) were from the northern region (Table 1). The higher percentages of PTs had seven to eight (22.80%) or more than ten (17%) years of clinical experience in caring for patients with HF (Table 1). The most common responsibilities of PTs for caring for HF patients were outpatient clinics (66.4%), followed by in-patient treatment (58.4%) and ongoing management (38.70%) (Table 1).
Table 1.
Demographic Data and Characteristics of All Physiotherapists (N= 553)
| Demographic Variables | Frequency (%) |
|---|---|
| Gender | |
| Male | 289 (52.30%) |
| Female | 264 (47.70%) |
| Geographic Location | |
| Western region | 204 (37%) |
| Central region | 160 (29%) |
| Eastern region | 100 (18%) |
| Southern region | 56 (10%) |
| Northern region | 33 (6%) |
| Year of experience with heart failure patients | |
| < 1 year | 25 (4.50%) |
| 1–2 years | 68 (12.30%) |
| 3–4 years | 71 (12.80%) |
| 5–6 years | 92 (16.60%) |
| 7–8 years | 126 (22.80%) |
| 9–10 years | 77 (13.90%) |
| >10 years | 94 (17%) |
| Responsibilities for care with heart failure patients | |
| Outpatient clinics | 367 (66.40%) |
| In-patient treatment | 323 (58.40%) |
| Ongoing Management | 214 (38.70%) |
| Primary care | 177 (32%) |
| Oxygen Therapy | 147 (26.60%) |
| Non-urgent Care | 85 (15.40%) |
| Diagnosis | 70 (12.70%) |
| Admission Prevention | 67 (12.10%) |
| Urgent Assessments | 56 (10.10%) |
| Medication Check | 48 (8.70%) |
| Prescribing | 20 (3.60%) |
| Others | 7 (1.30%) |
Note: Data are presented as frequencies and percentages.
Opinions on Referring Patients with HR to CR
Out of 553 PTs, 360 (65.10%) strongly agreed and 149 (26.90%) agreed that CR would improve patients’ physical fitness. Additionally, 334 (60.40%) strongly agreed and 162 (29.30%) agreed that CR would reduce breathlessness in patients with HF. Further, 321 (58%) strongly agreed and 154 (27.80%) agreed that CR would improve HF patients’ palpitation and fatigue. Out of 553 PTs, 349 (63.10%) strongly agreed and 149 (26.90%) agreed that CR would improve HF patients’ ability to perform daily activities, while 245 (44.30%) strongly agreed and 152 (27.50%) agreed that CR would reduce hospital readmission (Table 2).
Table 2.
Perception on Referring Patients with Heart Failure to Cardiopulmonary Rehabilitation (N= 553)
| Item | Frequency (%) |
|---|---|
| Perception on referring HF patients to CR | |
| I believe CR will improve patients’ physical fitness | |
| Strongly agree | 360 (65.10%) |
| Agree | 149 (26.90%) |
| Neutral | 30 (5.40%) |
| Disagree | 1 (0.20%) |
| Strongly disagree | 13 (2.40%) |
| I believe CR will reduce patients’ breathlessness | |
| Strongly agree | 334 (60.40%) |
| Agree | 162 (29.30%) |
| Neutral | 37 (6.70%) |
| Disagree | 3 (0.50%) |
| Strongly disagree | 17 (3.10%) |
| I believe CR will improve patients’ palpitation and fatigue | |
| Strongly agree | 321 (58%) |
| Agree | 154 (27.80%) |
| Neutral | 54 (9.80%) |
| Disagree | 7 (1.30%) |
| Strongly disagree | 17 (3.10%) |
| I believe CR will improve patients’ ability to perform daily actives | |
| Strongly agree | 349 (63.10%) |
| Agree | 149 (26.90%) |
| Neutral | 39 (7.10%) |
| Disagree | 2 (0.40%) |
| Strongly disagree | 14 (2.50%) |
| I believe CR will reduce hospital readmission | |
| Strongly agree | 245 (44.30%) |
| Agree | 152 (27.50%) |
| Neutral | 77 (13.90%) |
| Disagree | 20 (3.60%) |
| Strongly disagree | 59 (10.70%) |
Note: Data are presented as frequencies and percentages.
Abbreviations: HF, heart failure; CR, cardiopulmonary rehabilitation.
Mode of Delivery and Component of CR
Out of 553 PTs, 499 (90.20%) believed that the preferred way to deliver CR programs was in hospital-supervised programs, followed by 248 (44.80%) in at-home programs. In contrast, an online program with healthcare provider support was the least preferred way to deliver a CR program, chosen by 205 PTs (37.10%) (Table 3).
Table 3.
Mode of Delivery and Component of Cardiopulmonary Rehabilitation (N= 553)
| Item | Frequency (%) |
|---|---|
| The best way to deliver CR program for HF patients | |
| In hospital supervised program. | 499 (90.20%) |
| At home. | 248 (44.80%) |
| Tailored program with HCP support through phone. | 222 (40.10%) |
| Online program with healthcare provider support. | 205 (37.10%) |
| Rank of additional Component of CR program aside from exercise component | |
| Stress management. | 455 (82.30%) |
| Symptoms management. | 435 (78.70%) |
| Weight management. | 430 (77.80%) |
| Smoking cessation. | 364 (65.80%) |
| Information about heart failure disease. | 258 (46.70%) |
| Information about medications. | 215 (38.90%) |
Note: Data are presented as frequencies and percentages.
Abbreviations: HF, heart failure; CR, cardiopulmonary rehabilitation; HCP, healthcare provider.
Stress management followed by symptom management and weight management were the essential components of the CR program from the PTs’ perspective aside from the exercise component, chosen by 455 (82.30%), 435 (78.7%) and 430 (77.80%), respectively (Table 3).
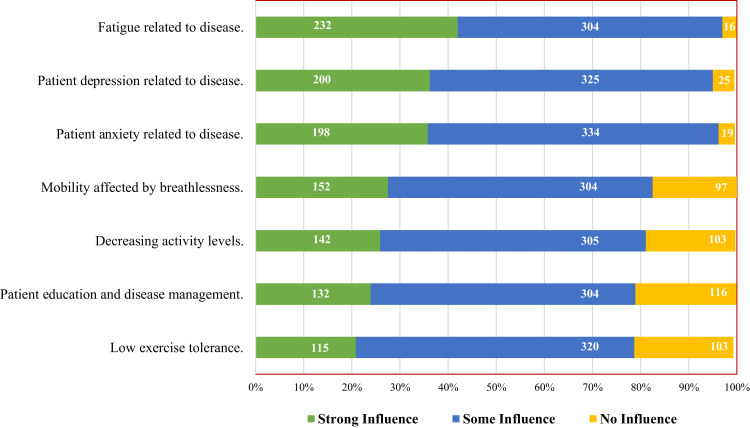
Patient-Related Factors That Influence Referral Decisions to CR
The main factors that strongly influenced the decision to refer patients with HF to CR from the PTs’ perspective included fatigue related to heart failure (42%), followed by depression and anxiety related to HF, chosen by (36.20%) and (35.80%), respectively (Figure 1).
Figure 1.
Patient-related factors that influence referral decision to cardiopulmonary rehabilitation, using strong, some or no influence as a grading tool (n=553).
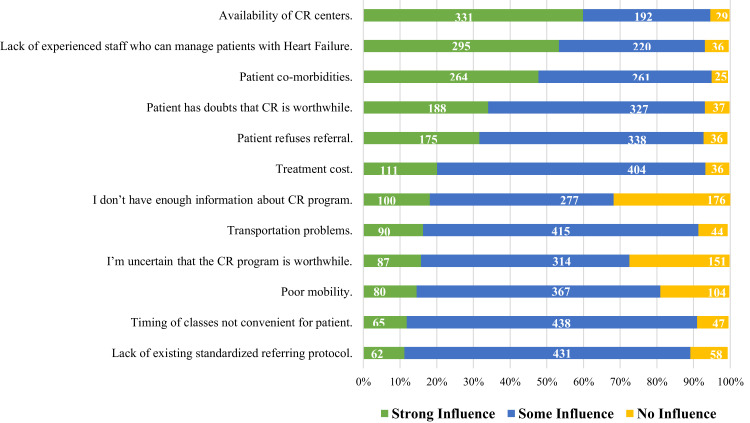
CR Referral Barriers
From the PTs’ perspective, the main barriers that strongly affect the referral process for patients with HF to CR included limited availability of CR centers (59.90%), followed by lack of experienced staff who can manage patients with HF (53.30%) and patient co-morbidities (47.70%) (Figure 2).
Figure 2.
Barriers of not referring patients with Heart Failure to cardiopulmonary rehabilitation, using influence graded as no, some or strong influence (n=553).
Discussion
To the best of our knowledge, this is the first national survey to investigate the opinions of PTs regarding the benefits of CR programs and their essential components and the preferred method of delivery. We also investigated the factors influencing referral to CR and the barriers to referring patients with HF to CR programs in Saudi Arabia. Participants in this national study agreed overall about the effectiveness of CR as a comprehensive program to improve physical activity, address disease-related symptoms, and reduce hospital readmission for patients with HF. They also agreed that hospital-supervised CR is the best way to deliver the program for these patients and included stress and symptoms management as essential components of a comprehensive CR program.
CR is increasingly known as an effective and safe non-pharmacological treatment for patients with HF.24,25 It alleviates HF-related symptoms such as dyspnea and fatigue and helps to improve physical capacity, cardiopulmonary fitness, and quality of life, leading to reduced HF-related hospital admission.26,27 In this study, PTs perceived CR as an effective management program for patients with HF and that having more years of clinical experience in dealing with these patients was a key factor in reaching this view. Our findings are in line with a previous study that reported that the level of clinical experience as a healthcare professional can be a factor in enhancing professionals’ knowledge about the benefits of CR programs.28
The most frequently selected barrier to referring patients to CR programs was accessibility to CR centers. The literature has reported a limited number of centers in Saudi Arabia providing CR programs for this population, and such centers only accommodate a limited number of patients with cardiac conditions.16 In addition, our findings are similar to previous investigations into the barriers to setting up pulmonary rehabilitation programs in Saudi Arabia, which reported that lack of capacity in medical facilities is one of the main barriers.20,29,30 This lack in the current clinical practice indicates the need across the country to establish and formulate comprehensive CR programs that meet current international clinical guidelines. In achieving this, it is essential to note that CR could be integrated within clinical sites by employing multidisciplinary collaboration.28
The second common barrier to the referral process highlighted in this study is the lack of experienced and well-trained staff who can manage patients with HF. A recent clinical review noted that Saudi Arabia had a shortage of healthcare workers, which may affect the quality of medical services delivered to patients with cardiac disease.28 This review highlighted the number of clinical disciplines required to manage patients with cardiovascular disease but suggested that multidisciplinary teams could implement CR programs. It suggested that the government implement and provide a training plan to upskill current healthcare professionals. In addition, offering high-quality training to provide the labor that could be useful in managing patients with HF is crucial.
We observed that patient co-morbidities were also reported as a major barrier. Patients living with HF tend to have co-existing chronic conditions, which include pulmonary dysfunction, hypertension, diabetes mellitus, musculoskeletal conditions, cognitive limitations, and depression.31 Moreover, patients with HF often have an age-related limitations, such as physical disability, frailty, or visual or hearing impairments.4 Also, HF disease-related symptoms, including dyspnea and fatigue, may affect patients’ ability to exercise and could prevent referral to CR programs. Our findings are in line with previous studies investigating the barriers to CR that highlighted that patients with HF who have co-existing comorbidities are more likely to not enroll on CR programs.32,33 Therefore, a tailored comprehensive CR program that meets patients’ needs must be delivered. Also, low-intensity exercise modes should be considered, to fit patients’ fitness levels, preferences, and goals. They should also consider patients’ medical conditions to enhance their participation in the program.
In this study, most PTs reported that hospital-based supervised programs would be the most suitable way to deliver CR for patients with HF. This could be related to the fact that patients with HF need additional monitoring and direct supervision from the professional team to prevent any cardiac-related event that may arise during CR. However, this would be a challenging option due to the current situation in Saudi Arabia, as the number of rehabilitation centers and professional teams that can manage patients with HF is limited. Hence, an alternative option to deliver the rehabilitation service could be considered to overcome this issue. Home-based CR may be a viable option because it is as effective as a conventional CR program in improving HF-related symptoms.34,35 Furthermore, home-based programs could offer greater accessibility for those living in rural areas and, thus, have the potential of improving the uptake of CR.
In this study, most PTs proposed that patient education on how to manage their disease-related symptoms and how to manage stress needs to be implemented in the program alongside physical training. This is consistent with the current American College of Cardiology (ACC), American Heart Association (AHA), Heart Failure Society of America (HFSA) and British Association for Cardiovascular Prevention and Rehabilitation (BACPR) clinical guidelines regarding the main components of CR.36,37 Patients with HF have limited knowledge and awareness about their condition and how to manage their symptoms, which could be a leading factor in hospital readmission and decreased quality of life.38,39 Therefore, promoting patient education is essential as it helps in managing HF-related symptoms and controlling disease-related episodes, which improves patients’ overall health and well-being.
Limitations
Limitations to this study should be highlighted. The study was based on a convenience sampling strategy, which might cause a potential selection bias. Secondly, the study did not include other healthcare professionals who could be involved in the care of patients with HF. Moreover, it would have benefited from qualitative interviews to gather greater in-depth information regarding the barriers to CR programs.
Conclusions
PTs agreed on the effectiveness of CR in improving desired clinical outcomes. While a supervised hospital-based program was the preferred mode of CR delivery, limited CR services exist. The lack of CR centers was a major barrier to referring patients with HF. Stress management was perceived as an essential component of the CR programs, in addition to the exercise component.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: executive summary: a report of the American College of Cardiology/American Heart Association joint committee on clinical practice guidelines. Circulation. 2022;145(18):e876–e894. doi: 10.1161/CIR.0000000000001062 [DOI] [PubMed] [Google Scholar]
- 2.Bozkurt B, Fonarow GC, Goldberg LR, et al. Cardiac rehabilitation for patients with heart failure: JACC expert panel. J Am Coll Cardiol. 2021;77(11):1454–1469. doi: 10.1016/j.jacc.2021.01.030 [DOI] [PubMed] [Google Scholar]
- 3.Pina IL, Apstein CS, Balady GJ, et al. Exercise and heart failure: a statement from the American Heart Association Committee on exercise, rehabilitation, and prevention. Circulation. 2003;107(8):1210–1225. doi: 10.1161/01.CIR.0000055013.92097.40 [DOI] [PubMed] [Google Scholar]
- 4.Forman DE, Sanderson BK, Josephson RA, et al. Heart failure as a newly approved diagnosis for cardiac rehabilitation: challenges and opportunities. J Am Coll Cardiol. 2015;65(24):2652–2659. doi: 10.1016/j.jacc.2015.04.052 [DOI] [PubMed] [Google Scholar]
- 5.Cooper LB, Hernandez AF. Assessing the quality and comparative effectiveness of team-based care for heart failure: who, what, where, when, and how. Heart Fail Clin. 2015;11(3):499–506. doi: 10.1016/j.hfc.2015.03.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.O’Connor CM, Whellan DJ, Lee KL, et al. Efficacy and safety of exercise training in patients with chronic heart failure: HF-ACTION randomized controlled trial. JAMA. 2009;301(14):1439–1450. doi: 10.1001/jama.2009.454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Beckers PJ, Denollet J, Possemiers NM, et al. Combined endurance-resistance training vs. endurance training in patients with chronic heart failure: a prospective randomized study. Eur Heart J. 2008;29(15):1858–1866. doi: 10.1093/eurheartj/ehn222 [DOI] [PubMed] [Google Scholar]
- 8.Mandic S, Tymchak W, Kim D, et al. Effects of aerobic or aerobic and resistance training on cardiorespiratory and skeletal muscle function in heart failure: a randomized controlled pilot trial. Clin Rehabil. 2009;23(3):207–216. doi: 10.1177/0269215508095362 [DOI] [PubMed] [Google Scholar]
- 9.Tyni-Lenne R, Gordon A, Europe E, et al. Exercise-based rehabilitation improves skeletal muscle capacity, exercise tolerance, and quality of life in both women and men with chronic heart failure. J Card Fail. 1998;4(1):9–17. doi: 10.1016/S1071-9164(98)90503-6 [DOI] [PubMed] [Google Scholar]
- 10.Davies EJ, Moxham T, Rees K, et al. Exercise training for systolic heart failure: cochrane systematic review and meta-analysis. Eur J Heart Fail. 2010;12(7):706–715. doi: 10.1093/eurjhf/hfq056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Haykowsky MJ, Timmons MP, Kruger C, et al. Meta-analysis of aerobic interval training on exercise capacity and systolic function in patients with heart failure and reduced ejection fractions. Am J Cardiol. 2013;111(10):1466–1469. doi: 10.1016/j.amjcard.2013.01.303 [DOI] [PubMed] [Google Scholar]
- 12.Santos FV, Chiappa GR, Ramalho SHR, et al. Resistance exercise enhances oxygen uptake without worsening cardiac function in patients with systolic heart failure: a systematic review and meta-analysis. Heart Fail Rev. 2018;23(1):73–89. doi: 10.1007/s10741-017-9658-8 [DOI] [PubMed] [Google Scholar]
- 13.Taylor RS, Mallett S, Miles A, et al. Exercise-based cardiac rehabilitation for chronic heart failure: the EXTRAMATCH II individual participant data meta-analysis. Health Technol Assess. 2019;23(25):1–98. doi: 10.3310/hta23660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kitzman DW, Brubaker PH, Herrington DM, et al. Effect of endurance exercise training on endothelial function and arterial stiffness in older patients with heart failure and preserved ejection fraction: a randomized, controlled, single-blind trial. J Am Coll Cardiol. 2013;62(7):584–592. doi: 10.1016/j.jacc.2013.04.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Balady GJ, Ades PA, Bittner VA, et al. Referral, enrollment, and delivery of cardiac rehabilitation/secondary prevention programs at clinical centers and beyond: a presidential advisory from the American Heart Association. Circulation. 2011;124(25):2951–2960. doi: 10.1161/CIR.0b013e31823b21e2 [DOI] [PubMed] [Google Scholar]
- 16.Rashed M, Theruvan N, Gad A, et al. Cardiac rehabilitation: future of heart health in Saudi Arabia, a perceptual view. World J Cardiovasc Dis. 2020;10(09):666–677. doi: 10.4236/wjcd.2020.109064 [DOI] [Google Scholar]
- 17.Bäck M, Öberg B, Krevers B. Important aspects in relation to patients’ attendance at exercise-based cardiac rehabilitation–facilitators, barriers and physiotherapist’s role: a qualitative study. BMC Cardiovasc Disord. 2017;17(1):1–10. doi: 10.1186/s12872-017-0512-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Certo CM. History of cardiac rehabilitation. Phys Ther. 1985;65(12):1793–1795. doi: 10.1093/ptj/65.12.1793 [DOI] [PubMed] [Google Scholar]
- 19.Dalal HM, Doherty P, Taylor RS. Cardiac rehabilitation. BMJ. 2015;351:h5000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Aldhahir AM, Alqahtani JS, Alghamdi SM, et al. Physicians’ attitudes, beliefs and barriers to a pulmonary rehabilitation for COPD patients in Saudi Arabia: a cross-sectional study. Healthcare. 2022;10(5):904. doi: 10.3390/healthcare10050904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Spruit MA, Singh SJ, Garvey C, et al. An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013;188(8):e13–e64. doi: 10.1164/rccm.201309-1634ST [DOI] [PubMed] [Google Scholar]
- 22.Hill K, Vogiatzis I, Burtin C. The importance of components of pulmonary rehabilitation, other than exercise training, in COPD. Eur Respir Rev. 2013;22(129):405. doi: 10.1183/09059180.00002913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Holland AE, Cox NS, Houchen-Wolloff L, et al. Defining modern pulmonary rehabilitation. an official American thoracic society workshop report. Ann Am Thorac Soc. 2021;18(5):e12–e29. doi: 10.1513/AnnalsATS.202102-146ST [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McDonagh TA, Metra M, Adamo M, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: developed by the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) With the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2021;42(36):3599–3726. doi: 10.1093/eurheartj/ehab368 [DOI] [PubMed] [Google Scholar]
- 25.Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;62(16):e147–e239. doi: 10.1016/j.jacc.2013.05.019 [DOI] [PubMed] [Google Scholar]
- 26.Long L, Mordi IR, Bridges C, et al. Exercise‐based cardiac rehabilitation for adults with heart failure. Cochrane Database Syst Rev. 2019;1(1). doi: 10.1002/14651858.CD003331.pub5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Taylor RS, Long L, Mordi IR, et al. Exercise-based rehabilitation for heart failure: cochrane systematic review, meta-analysis, and trial sequential analysis. JACC. 2019;7(8):691–705. doi: 10.1016/j.jchf.2019.04.023 [DOI] [PubMed] [Google Scholar]
- 28.Abu Hasheesh MO. Health care professionals’ awareness and knowledge of cardiac rehabilitation programs among cardiovascular disease patients in Al-Madinah, Saudi Arabia; 2014.
- 29.Alsubaiei ME, Cafarella P, Frith P, et al. Barriers for setting up a pulmonary rehabilitation program in the Eastern Province of Saudi Arabia. Ann Thorac Med. 2016;11(2):121. doi: 10.4103/1817-1737.180028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Aldhahir AM, Alghamdi S, Alqahtani J, et al. Pulmonary rehabilitation for COPD: a narrative review and call for further implementation in Saudi Arabia. Ann Thorac Med. 2021;16(4):299–305. doi: 10.4103/atm.atm_639_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Triposkiadis FK, Skoularigis J. Prevalence and importance of comorbidities in patients with heart failure. Curr Heart Fail Rep. 2012;9(4):354–362. doi: 10.1007/s11897-012-0110-z [DOI] [PubMed] [Google Scholar]
- 32.Im HW, Baek S, Jee S, et al. Barriers to outpatient hospital-based cardiac rehabilitation in Korean patients with acute coronary syndrome. Ann Rehabil Med. 2018;42(1):154–165. doi: 10.5535/arm.2018.42.1.154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Park LG, Schopfer DW, Zhang N, et al. Participation in cardiac rehabilitation among patients with heart failure. J Card Fail. 2017;23(5):427–431. doi: 10.1016/j.cardfail.2017.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Anderson L, Sharp GA, Norton RJ, et al. Home‐based versus centre‐based cardiac rehabilitation. Cochrane Database Syst Rev. 2017;2017(6). doi: 10.1002/14651858.CD007130.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kraal JJ, Van den Akker-Van Marle ME, Abu-Hanna A, et al. Clinical and cost-effectiveness of home-based cardiac rehabilitation compared to conventional, centre-based cardiac rehabilitation: results of the FIT@ Home study. Eur J Prev Cardiol. 2017;24(12):1260–1273. doi: 10.1177/2047487317710803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cowie A, Buckley J, Doherty P, et al. British Association for Cardiovascular Prevention and Rehabilitation (BACPR). Standards and core components for cardiovascular disease prevention and rehabilitation. Heart. 2019;105(7):510–515. doi: 10.1136/heartjnl-2018-314206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yancy CW, Jessup M, Bozkurt B, et al. 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines and the heart failure society of America. J Am Coll Cardiol. 2017;70(6):776–803. doi: 10.1016/j.jacc.2017.04.025 [DOI] [PubMed] [Google Scholar]
- 38.Strömberg A. The crucial role of patient education in heart failure. Eur J Heart Fail. 2005;7(3):363–369. doi: 10.1016/j.ejheart.2005.01.002 [DOI] [PubMed] [Google Scholar]
- 39.Michalsen A, König G, Thimme W. Preventable causative factors leading to hospital admission with decompensated heart failure. Heart. 1998;80(5):437–441. doi: 10.1136/hrt.80.5.437 [DOI] [PMC free article] [PubMed] [Google Scholar]