Abstract
Introduction
The Segond fracture is an avulsion fracture of the lateral tibial plateau and is widely considered to be pathognomonic of anterior cruciate ligament (ACL) rupture. In addition to ACL rupture, Segond fractures have also been noted to be associated with significant intra-articular pathology such as meniscal injuries as well as extra-articular pathology such as collateral ligament injuries. This is likely due to the fact that the presence of a Segond fracture may represent increased rotatory instability. Whilst several studies have demonstrated the association of a Segond fracture with significant intra-articular pathology, there is a paucity of literature assessing if the combination of an ACL rupture and Segond fracture gives rise to higher rates of concomitant ligamentous and meniscal injuries. The primary objective of this study is to determine if patients with ACL ruptures associated with Segond fractures have higher rates of concomitant ligamentous and meniscal injury, when compared to patients with ACL ruptures without a Segond fracture.
Methods
A retrospective review of all patients who underwent ACL reconstruction in a single institution between 2014 to 2018 was conducted. A review of the patients’ demographics, operative notes, and radiographs was performed. X-rays and MRI scans were double-read by a board-certified radiologist and Orthopaedic surgeon.
Results
A total of 414 subjects were included. The incidence of Segond fracture was 2.4%. The mean age was 24.7±7.4 (range 16 to 60) years and 26.7±7.6 (range 16 to 38) years in patients with and without Segond fractures respectively. 89.9% of patients suffered a non-contact mechanism of injury, with sports injuries being most common (79.5%). There was a significantly higher rate of isolated lateral meniscus tears in patients with Segond fractures compared to those without (50% v.s. 20.8%) based on pre-operative MRI. (p<0.05) There were no other significant differences in associated ligamentous injuries.
Conclusion
The incidence of Segond fracture associated with ACL rupture is 2.4%. There is a significantly higher risk of a concomitant isolated lateral meniscus tear in ACL ruptures associated with a Segond fracture. There is no significantly higher risk of concomitant ligamentous injuries in ACL ruptures associated with a Segond fracture.
Keywords: Arthroscopy, Instability, Knee, Ligament
Abbreviations: CHEE, Cheryl Poh Lay
1. Introduction
The Segond fracture is a small vertical avulsion fracture of the lateral tibial plateau that was first described by French anatomist Dr. Paul Segond in 1879.1 Segond described a fracture that constantly appeared behind and above the lateral tibia plateau resulting from the pull of a fibrous and resistant band during forceful high-energy internal rotation of the femur on the tibia.1, 2, 3 The clinical implication of the Segond fracture was later proposed in 1979 by Woods et al.,4 who reported an association between the Segond fracture and significant knee instability. Further studies subsequently described the association between a Segond fracture and concomitant intra-articular injury, in particular an anterior cruciate ligament (ACL) rupture.2,4,5 In the presence of a Segond fracture, there is an up to 75% chance of a concomitant ACL rupture.6,7 As such, the Segond fracture is now increasingly used as a radiological marker to suggest that further imaging should be performed to rule out intra-articular injury. It is important to be aware that despite being highly associated with an ACL rupture, the overall incidence of Segond fractures in patients with ACL rupture remains low, with rates ranging from 3 to 9%.8, 9, 10, 11 In addition to ACL rupture, Segond fractures have also been noted to be associated with significant intra-articular pathology such as meniscal injuries as well as extra-articular pathology such as collateral ligament injuries.12, 13, 14, 15 This is likely due to the fact that the presence of a Segond fracture may represent increased rotatory instability.9,11, 12, 13
Whilst several studies have demonstrated the association of a Segond fracture with significant intra-articular pathology,6,7,12, 13, 14, 15, 16, 17 there is a paucity of literature assessing if the combination of an ACL rupture and Segond fracture gives rise to higher rates of concomitant ligamentous and meniscal injuries. The primary objective of this study is to determine if patients with ACL ruptures associated with Segond fractures have higher rates of concomitant ligamentous and meniscal injury, when compared to patients with ACL ruptures without a Segond fracture.
2. Materials and methods
A retrospective review of an ACL registry including consecutive patients who underwent surgical ACL reconstruction in a single tertiary hospital from January 2014 to December 2018 was conducted. The study included all patients from the start of the registry until the commencement of data collection after ethical approval was obtained. The inclusion criteria included patients aged 16 years–60 years who had undergone primary ACL reconstruction surgery. Patients with concomitant lower limb fractures of the femur or tibia or did not have the complete imaging performed or data were excluded from this study.
A review of the patients’ demographics, clinical charts, operative notes, and radiographs was performed. Plain radiography and magnetic resonance imaging (MRI) scans of the injured knee were double-read by a board-certified Radiologist and Orthopaedic surgeon to establish the presence of a Segond fracture (Fig. 1.). The presence of bone marrow edema, as well as concomitant injuries to the posterior cruciate ligament (PCL), medial collateral ligament (MCL), lateral collateral ligament (LCL), medial and lateral meniscus was also reviewed. The assessment for the presence of a Segond fracture was performed according to published criteria (a visible bone flake at the superolateral rim of the tibia).5 Ligamentous injuries were classified into varying degrees of severity in accordance to the grading system proposed by Stoller et al.18 Grade 0 is defined as intact ligament. Grade 1 is defined as peri-ligamentous injury with edema but absence of displacement, thickening and discontinuity. Grade 2 is defined as a partial tear of the ligament with intra-ligamentous T2 hyperintensities but fibres still being in continuity. Grade 3 is defined as a complete tear with complete lack of continuity in the ligament fibres. Meniscus injuries were classified into intact and torn, regardless of the complexity of tear. Operative notes were reviewed for correlation of the radiographic findings.
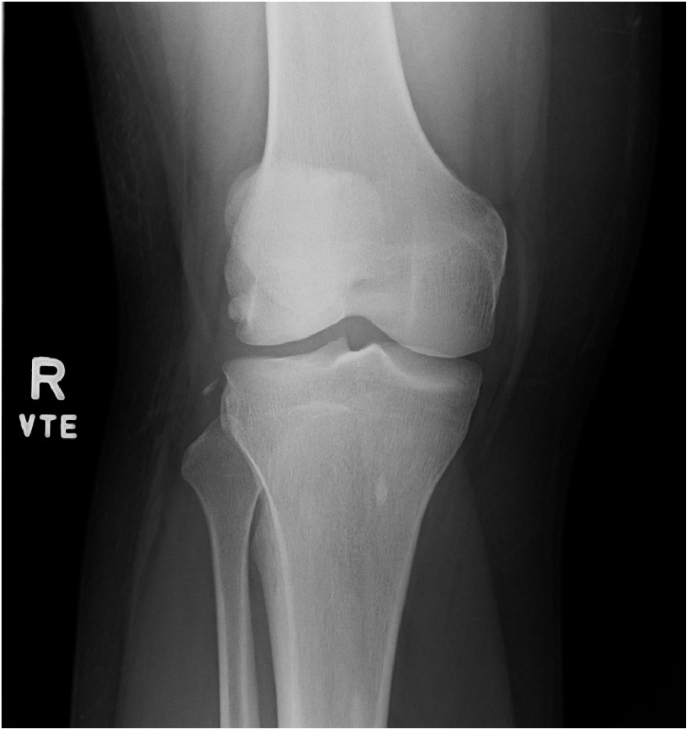
Fig. 1.
Anteroposterior X-ray of the right knee showing a Segond fracture – a fleck of bone at the superolateral rim of the tibia.
Descriptive statistics were presented in terms of means, standard deviations (SD), medians and ranges for continuous variables and in percentages for categorical variables. The significance of differences between groups was determined using the Student unpaired t-test for normally distributed data. For categorical data, the significance of differences between the groups was determined using the Chi-square test. Statistical analysis was performed using the IBM® SPSS® Statistics software platform. A p-value < 0.05 was used to denote statistical significance.
3. Results
A total of 550 patients were eligible. After the exclusion criteria was applied, a total of 414 patients were available for analysis. The patients were divided into 2 groups, with Group 1 being patients without a Segond fracture and Group 2 being patients with a Segond fracture. Group 1 consisted of 404 (97.6%) patients, with 322 males and 82 females. Group 2 consisted of 10 (2.4%) patients, with 9 males and 1 female. The mean age of patients was 24.7 ± 7.4 (range 16–60) years and 26.7 ± 7.6 (range 16–38) years in Group 1 and 2 respectively. Overall, 89.8% of patients suffered a non-contact mechanism of injury. Sports injuries accounted for 79.5% of the mechanism of injury, with the most common sports being football (46.8%), basketball (14.3%) and martial arts (5.8%). The patients were all non-professional athletes with largely low-velocity type injuries. There were no significant differences in the demographics, side of injury and mechanism of injury between both groups (Table 1). The distribution of activities resulting in injury is detailed in Table 2.
Table 1.
Demographics.
| Group 1 N = 404 | Group 2 N = 10 | P-Value | |
|---|---|---|---|
| Age, years | 24.7 (SD 7.4) | 26.7 (SD 7.6) | 0.70 |
| Gender | 0.42 | ||
| Female | 82 (20.3%) | 1 (10.0%) | |
| Male | 322 (79.7%) | 9 (90.0%) | |
| Side of Injury | 0.57 | ||
| Left | 198 (49.0%) | 4 (40.0%) | |
| Right | 206 (51.0%) | 6 (60.0%) | |
| Mechanism of Injury | 0.72 | ||
| Non-Contact | 286/318 (89.9%) | 6/7 (85.7%) | |
| Contact | 32/318 (10.1%) | 1/7 (14.3%) |
Table 2.
Distribution of activities.
| Activity | Number of Patients (%) |
|---|---|
| Sports | 329 |
| Soccer | 154 (46.8%) |
| Basketball | 47 (14.3%) |
| Martial Arts | 19 (5.8%) |
| Netball | 16 (4.9%) |
| Badminton | 11 (3.3%) |
| Others | 82 (24.9%) |
| Trauma | 85 |
| Fall | 48 (60%) |
| Road Traffic Accident | 11 (18.3%) |
| Others | 26 (30.6%) |
In Group 1, the most commonly associated injuries were that of medial meniscus and lateral meniscus tears, with 200 (49.5%) and 160 (39.6%) patients sustaining these injuries respectively. In Group 2, MRI imaging revealed that the most commonly associated injuries were lateral meniscus tears, medial meniscus tears and bone edema, with 6 (60.0%), 2 (20.0%) and 2 (20.0%) of patients sustaining these injuries respectively. When analysing isolated medial meniscal tears (without associated lateral meniscal tears), Group 1 had 124 (30.7%) patients and Group 2 had 1 (10.0%) patient. This difference was not significant. However, there were significantly more patients with isolated lateral meniscal tears (without associated medial meniscal tears) in Group 2 (5, 50.0%) compared to Group 1 (84, 20.8%) (p < 0.05). There were no other significant differences in associated ligamentous injuries between both groups. Detailed results of the associated injuries in both groups are summarised in Table 3.
Table 3.
Associated Injuries on MRI imaging.
| Group 1 N = 404 | Group 2 N = 10 | P-Value | |
|---|---|---|---|
| Posterior cruciate ligament (PCL) tear | 11 (2.7%) | 0 (0%) | 0.60 |
| Medial collateral ligament (MCL) tear | 39 (9.6%) | 1 (10.0%) | 0.97 |
| Lateral collateral ligament (MCL) tear | 17 (4.2%) | 0 (0%) | 0.51 |
| Medial meniscus tear | 200 (49.5%) | 2 (20.0%) | 0.07 |
| Isolated medial meniscus tear | 121 (30.0%) | 1 (10.0%) | 0.17 |
| Lateral meniscus tear | 160 (39.6%) | 6 (60.0%) | 0.20 |
| Isolated lateral meniscus tear | 84 (20.8%) | 5 (50.0%) | <0.05 |
| Bi-meniscal Tear | 76 (18.8%) | 1 (10.0%) | 0.48 |
| Bone marrow edema | 155 (38.4%) | 2 (20.0%) | 0.24 |
Operative findings of the intra-articular injuries revealed that Group 1 had a lower incidence of lateral meniscal injuries (198, 49.0%) compared to Group 2 (6, 60.0%) but this did not reach statistical significance. There was a higher rate of medial meniscal injuries in Group 1 (168, 41.6%) compared to Group 2 (2, 20.0%) but this too was not significant. The operative findings of intra-articular injuries are detailed in Table 4.
Table 4.
Associated Injuries intra-operative findings.
| Group 1 N = 404 | Group 2 N = 10 | P-Value | |
|---|---|---|---|
| Posterior cruciate ligament (PCL) tear | 5 (1.2%) | 0 (0%) | 0.72 |
| Medial meniscus tear | 168 (41.8%) | 2 (20.0%) | 0.17 |
| Isolated medial meniscus tear | 82 (20.3%) | 1 (10.0%) | 0.42 |
| Lateral meniscus tear | 198 (49.0%) | 6 (60.0%) | 0.50 |
| Isolated lateral meniscus tear | 112 (27.7%) | 5 (50.0%) | 0.12 |
| Bi-meniscal Tear | 86 (21.3%) | 1 (10.0%) | 0.39 |
4. Discussion
The presence of a Segond fracture is useful as it is well established as a radiological marker of significant intra-articular injury.2, 3, 4, 5, 6, 7 The anatomical relations, contribution to knee stability, impact on severity of concomitant injury and prognostic value of a Segond fracture are currently controversial. The anterolateral complex (ALC), and in particular the anterolateral ligament (ALL), is of particular interest when analysing Segond fractures. The presence of the ALL and its attachment onto the region of on the proximal tibia was reported by Claes et al.19 He found that the attachment of the ALL on the proximal tibia coincided with the origin of the Segond fracture and thus concluded that the Segond fracture is a direct avulsion of the ALL. This is currently controversial, as whilst some studies20,21 have concurred with this finding, other authors have argued that the Segond fracture may arise as a result of the ALC, rather than the ALL alone.22, 23, 24 An expert group consensus meeting25 has since concluded that multiple anatomical structures make up the ALC and it is currently unclear which structure is primarily responsible for the Segond fracture. This uncertainty makes it difficult to identify the mechanism of injury that results in a Segond fracture and the implications of sustaining one. This study did not attempt to re-assess the origin of the Segond fracture.
Concomitant ligamentous and meniscus injuries are common in ACL rupture.26,27 However, there appears to be a relative paucity of literature examining the concomitant ligamentous and meniscal injuries with ACL rupture in the presence of a Segond fracture. Klos et al. reported that a prevalence of Segond fracture ranging from 29% to 33% in patients with MCL injury. They postulated that the likely association between MCL injuries and Segond fracture may be related to excessive valgus movement of the knee.14 21 reported a 35%, 30% and 23% incidence of concomitant MCL, medial and lateral meniscus injuries respectively,12 while 22 reported a 62%, 8% and 38% incidence of concomitant MCL, LCL and medial meniscus injuries respectively.13 Sulaiman et al. found a higher incidence of lateral meniscus tear in patients with Segond fractures (49.1%) as compared to those without (32.6%).15 This study found that was no significantly increased risk of concomitant ligamentous injuries in ACL ruptures with Segond fractures. However, there was a significantly increased risk of sustaining a concurrent isolated lateral meniscus tear (as detected on pre-operative MRI) in ACL ruptures with a Segond fracture. This corresponds to an earlier study by Sulaiman et al.15 and is likely due to the fact that the disruption of the ALC results in increased rotatory instability.11, 12, 13 Monaco et al. performed a cadaveric biomechanical study and found that whilst isolated ACL tears had a mild effect on rotational stability, the presence of a Segond fracture had a significant effect on axial tibial rotation during the execution of a pivot-shift test.28 Another cadaveric biomechanical study by Parsons et al. injury to the ALL worsened the degree of the pivot-shift phenomenon.29 Increased pivot shift, in turn, has been described to increase the risks of concomitant lateral meniscus injury in the ACL-injured knee.30, 31, 32, 33 These published data support our finding that a concomitant isolated lateral meniscus tear is more common in ACL ruptures with a Segond fracture when reviewing the MRI.
The increased risk of lateral meniscus tears was not significant when analysing the intra-operative findings. One possible explanation is the time lag to surgery. Multiple studies have shown that delay to definitive surgery increases the risk of chondral and meniscal injuries in the ACL-deficient knee.34, 35, 36 In addition, whilst MRI is an effective diagnostic modality for evaluating meniscal injuries,37 there remains the possibility of missed meniscal lesions. These reasons may explain why there was a difference between the rates of MRI diagnosed meniscal lesions and the intra-operatively identified meniscal lesions. Our study finding of an increased risk of concomitant isolated lateral meniscal injuries associated with the Segond fracture highlights the importance of meticulous assessment of the lateral meniscus when reviewing the MRI.
This study found a 2.4% incidence of Segond fractures in patients undergoing ACL reconstruction. The rate of Segond fractures in this study is lower than published rates from previous reports.8, 9, 10, 11 One possible explanation is that the current cohort was engaged in largely recreational level sporting activities and had suffered low-velocity type injuries. In addition, whilst the exact mechanism of a Segond fracture is uncertain, there is published data on a higher incidence of Segond fractures in patients injured during downhill skiing as compared with other mechanisms of injury.11 Indeed, this is likely due in part to the high velocity nature of the sport. In our cohort, only 3 (0.7%) patients suffered an ACL injury due to skiing. The choice of sport and level of participation may explain our lower incidence of Segond fractures, although further research should be done to establish the effect of the various sporting activities and risk of sustaining a Segond fracture.
The influence of Segond fractures on treatment outcomes, namely after ACL reconstruction surgery, has been well studied. While Ferretti et al. reported good clinical outcomes after direct repair of the Segond fracture and plication of the anterolateral capsule in a small series of patients with ACL rupture associated with Segond fractures,38 the current consensus is that the presence of a Segond fracture does not significantly influence knee stability and treatment outcomes.9,39,40 A recent systematic review12 concluded that unrepaired Segond fractures do not appear to have any significant negative effect on postoperative stability or risk of graft failure or revision surgery after ACL reconstruction. The scope of this study did not extend to evaluating the effect of Segond fractures on treatment outcomes in our population.
5. Limitations
This study is a retrospective database study. There is a small number of patients with Segond fractures but this is due to the inherent rarity of the Segond fracture. In addition, conservatively treated patients were not included as an operative procedure was required to confirm the presence of associated intra-articular injuries. Incomplete registry data also limited the reporting of interval delay between injury and surgery. This study also did not seek to correlate the presence of a Segond facture to clinical outcomes such as knee stability and re-injury rates. The authors suggest that future studies with a larger series of Segond fractures can be performed to achieve more generalizable results. Furthermore, these future studies can study the relationship of Segond fracture and clinical outcomes of ACL reconstruction.
6. Conclusion
The incidence of Segond fracture associated with ACL rupture is 2.4%. There is a significantly higher risk of a concomitant isolated lateral meniscus tear seen on MRI in ACL ruptures associated with a Segond fracture. There is no significantly higher risk of concomitant ligamentous injuries in ACL ruptures associated with a Segond fracture.
7. Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors, and no material support of any kind was received.
Declaration of competing interest
The authors declare that they and/or their institutions do not have any financial and personal relationships with other people or organizations that could inappropriately influence (bias) their work.
References
- 1.Skinner E.J., Davis D.D., Varacallo M. StatPearls. Treasure Island (FL) StatPearls Publishing; June 3, 2021. Segond fractures; p. 1. [Google Scholar]
- 2.Claes S., Luyckx T., Vereecke E., Bellemans J. The segond fracture: a bony injury of the anterolateral ligament of the knee. Arthrosc J Arthrosc Relat Surg. 2014;30(11):1475–1482. doi: 10.1016/j.arthro.2014.05.039. [DOI] [PubMed] [Google Scholar]
- 3.Shaikh H., Herbst E., Rahnemai-Azar A., et al. The segond fracture is an avulsion of the anterolateral complex. Am J Sports Med. 2017;45(10):2247–2252. doi: 10.1177/0363546517704845. [DOI] [PubMed] [Google Scholar]
- 4.Woods G., Stanley R., Tullos H. Lateral capsular sign: x-ray clue to a significant knee instability. Am J Sports Med. 1979;7(1):27–33. doi: 10.1177/036354657900700107. [DOI] [PubMed] [Google Scholar]
- 5.Cosgrave C.H., Burke N.G., Hollingsworth J. The Segond fracture: a clue to intra-articular knee pathology. Emerg Med J. 2012;29(10):846–847. doi: 10.1136/emermed-2011-200356. [DOI] [PubMed] [Google Scholar]
- 6.Dietz G.W., Wilcox D.M., Montgomery J.B. Segond tibial condyle fracture: lateral capsular ligament avulsion. Radiology. 1986;159(2):467–469. doi: 10.1148/radiology.159.2.3961179. [DOI] [PubMed] [Google Scholar]
- 7.Goldman A.B., Pavlov H., Rubenstein D. The Segond fracture of the proximal tibia: a small avulsion that reflects major ligamentous damage. AJR Am J Roentgenol. 1988;151(6):1163–1167. doi: 10.2214/ajr.151.6.1163. [DOI] [PubMed] [Google Scholar]
- 8.Hess T., Rupp S., Hopf T., Gleitz M., Liebler J. Lateral tibial avulsion fractures and disruptions to the anterior cruciate ligament. A clinical study of their incidence and correlation. Clin Orthop Relat Res. 1994;303:193–197. [PubMed] [Google Scholar]
- 9.Yoon K.H., Kim J.S., Park S.Y., Park S.E. The influence of segond fracture on outcomes after anterior cruciate ligament reconstruction. Arthroscopy. 2018;34(6):1900–1906. doi: 10.1016/j.arthro.2018.01.023. [DOI] [PubMed] [Google Scholar]
- 10.Bock G.W., Bosch E., Mishra D.K., Daniel D.M., Resnick D. The healed Segond fracture: a characteristic residual bone excrescence. Skeletal Radiol. 1994;23(7):555–556. doi: 10.1007/BF00223090. [DOI] [PubMed] [Google Scholar]
- 11.Slagstad I., Parkar A.P., Strand T., Inderhaug E. Incidence and prognostic significance of the segond fracture in patients undergoing anterior cruciate ligament reconstruction. Am J Sports Med. 2020;48(5):1063–1068. doi: 10.1177/0363546520905557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nagai K., Kamada K., Kay J., et al. Clinical outcomes after anterior cruciate ligament reconstruction in patients with a concomitant segond fracture: a systematic review. Am J Sports Med. 2021 doi: 10.1177/03635465211045689. [DOI] [PubMed] [Google Scholar]
- 13.Kumahara R., Kimura Y., Sasaki R., et al. Prevalence of segond fractures associated with anterior cruciate ligament injuries and their influence on knee joint stability; A case-control study. BMC Muscoskel Disord. 2022;23(1):180. doi: 10.1186/s12891-022-05127-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Klos B., Scholtes M., Konijnenberg S. High prevalence of all complex Segond avulsion using ultrasound imaging. Knee Surg Sports Traumatol Arthrosc. 2017;25(4):1331. doi: 10.1007/s00167-017-4532-8. [DOI] [PubMed] [Google Scholar]
- 15.Sulaiman Y., Li J., Chen G., Abudouaini H., Li Q., Tang X. The relationship between a segond fracture and meniscus injury in patients with anterior cruciate ligament tears. Knee. 2021;33:193–199. doi: 10.1016/j.knee.2021.09.008. [DOI] [PubMed] [Google Scholar]
- 16.Campos J.C., Chung C.B., Lektrakul N., et al. Pathogenesis of the Segond fracture: anatomic and MR imaging evidence of an iliotibial tract or anterior oblique band avulsion. Radiology. 2001;219(2):381–386. doi: 10.1148/radiology.219.2.r01ma23381. [DOI] [PubMed] [Google Scholar]
- 17.De Maeseneer M., Boulet C., Willekens I., et al. Segond fracture: involvement of the iliotibial band, anterolateral ligament, and anterior arm of the biceps femoris in knee trauma. Skeletal Radiol. 2015;44(3):413–421. doi: 10.1007/s00256-014-2044-x. [DOI] [PubMed] [Google Scholar]
- 18.Stoller D.W., Li A.E., Anderson L.J., Cannon W.D. In: Magnetic Resonance Imaging in Orthopaedicsand Sports Medicine. third ed. Stoller D.W., editor. Lippincott Williams and Wilkins; Philadelphia: 2007. The knee; pp. 305–731. [Google Scholar]
- 19.Claes S., Vereecke E., Maes M., Victor J., Verdonk P., Bellemans J. Anatomy of the anterolateral ligament of the knee. J Anat. 2013;223(4):321–328. doi: 10.1111/joa.12087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dodds A.L., Halewood C., Gupte C.M., Williams A., Amis A.A. The anterolateral ligament: anatomy, length changes and association with the Segond fracture. Bone Joint Lett J. 2014;96-B(3):325–331. doi: 10.1302/0301-620X.96B3.33033. [DOI] [PubMed] [Google Scholar]
- 21.Caterine S., Litchfield R., Johnson M., Chronik B., Getgood A. A cadaveric study of the anterolateral ligament: re-introducing the lateral capsular ligament. Knee Surg Sports Traumatol Arthrosc. 2015;23(11):3186–3195. doi: 10.1007/s00167-014-3117-z. [DOI] [PubMed] [Google Scholar]
- 22.Guenther D., Rahnemai-Azar A.A., Bell K.M., et al. The anterolateral capsule of the knee behaves like a sheet of fibrous tissue. Am J Sports Med. 2017;45(4):849–855. doi: 10.1177/0363546516674477. [DOI] [PubMed] [Google Scholar]
- 23.Saiegh Y.A., Suero E.M., Guenther D., et al. Sectioning the anterolateral ligament did not increase tibiofemoral translation or rotation in an ACL-deficient cadaveric model. Knee Surg Sports Traumatol Arthrosc. 2017;25(4):1086–1092. doi: 10.1007/s00167-015-3787-1. [DOI] [PubMed] [Google Scholar]
- 24.Thein R., Boorman-Padgett J., Stone K., Wickiewicz T.L., Imhauser C.W., Pearle A.D. Biomechanical assessment of the anterolateral ligament of the knee: a secondary restraint in simulated tests of the pivot shift and of anterior stability. J Bone Joint Surg Am. 2016;98(11):937–943. doi: 10.2106/JBJS.15.00344. [DOI] [PubMed] [Google Scholar]
- 25.Getgood A., Brown C., Lording T., et al. The anterolateral complex of the knee: results from the International ALC Consensus Group Meeting. Knee Surg Sports Traumatol Arthrosc. 2019;27(1):166–176. doi: 10.1007/s00167-018-5072-6. [DOI] [PubMed] [Google Scholar]
- 26.Pike A.N., Patzkowski J.C., Bottoni C.R. Meniscal and chondral pathology associated with anterior cruciate ligament injuries. J Am Acad Orthop Surg. 2019;27(3):75–84. doi: 10.5435/JAAOS-D-17-00670. [DOI] [PubMed] [Google Scholar]
- 27.Kluczynski M.A., Marzo J.M., Bisson L.J. Factors associated with meniscal tears and chondral lesions in patients undergoing anterior cruciate ligament reconstruction: a prospective study. Am J Sports Med. 2013;41(12):2759–2765. doi: 10.1177/0363546513503448. [DOI] [PubMed] [Google Scholar]
- 28.Monaco E., Mazza D., Redler A., et al. Segond's fracture: a biomechanical cadaveric study using navigation. J Orthop Traumatol. 2017;18(4):343–348. doi: 10.1007/s10195-017-0460-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Parsons E.M., Gee A.O., Spiekerman C., Cavanagh P.R. The biomechanical function of the anterolateral ligament of the knee. Am J Sports Med. 2015;43(3):669–674. doi: 10.1177/0363546514562751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hoshino Y., Miyaji N., Nishida K., et al. The concomitant lateral meniscus injury increased the pivot shift in the anterior cruciate ligament-injured knee. Knee Surg Sports Traumatol Arthrosc. 2019;27(2):646–651. doi: 10.1007/s00167-018-5209-7. [DOI] [PubMed] [Google Scholar]
- 31.Cui W., Nakagawa Y., Katagiri H., et al. Knee laxity, lateral meniscus tear and distal femur morphology influence pivot shift test grade in ACL injury patients. Knee Surg Sports Traumatol Arthrosc. 2021;29(2):633–640. doi: 10.1007/s00167-020-05994-7. [DOI] [PubMed] [Google Scholar]
- 32.Minami T., Muneta T., Sekiya I., et al. Lateral meniscus posterior root tear contributes to anterolateral rotational instability and meniscus extrusion in anterior cruciate ligament-injured patients. Knee Surg Sports Traumatol Arthrosc. 2018;26(4):1174–1181. doi: 10.1007/s00167-017-4569-8. [DOI] [PubMed] [Google Scholar]
- 33.Tanaka M., Vyas D., Moloney G., Bedi A., Pearle A.D., Musahl V. What does it take to have a high-grade pivot shift? Knee Surg Sports Traumatol Arthrosc. 2012;20(4):737–742. doi: 10.1007/s00167-011-1866-5. [DOI] [PubMed] [Google Scholar]
- 34.Brambilla L., Pulici L., Carimati G., et al. Prevalence of associated lesions in anterior cruciate ligament reconstruction: correlation with surgical timing and with patient Age, sex, and body mass index. Am J Sports Med. 2015;43(12):2966–2973. doi: 10.1177/0363546515608483. [DOI] [PubMed] [Google Scholar]
- 35.Gupta R., Masih G.D., Chander G., Bachhal V. Delay in surgery predisposes to meniscal and chondral injuries in anterior cruciate ligament deficient knees. Indian J Orthop. 2016 Sep;50(5):492–498. doi: 10.4103/0019-5413.189606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cristiani R., Janarv P.M., Engström B., Edman G., Forssblad M., Stålman A. Delayed anterior cruciate ligament reconstruction increases the risk of abnormal prereconstruction laxity, cartilage, and medial meniscus injuries. Arthroscopy. 2021;37(4):1214–1220. doi: 10.1016/j.arthro.2020.11.030. [DOI] [PubMed] [Google Scholar]
- 37.Phelan N., Rowland P., Galvin R., O'Byrne J.M. A systematic review and meta-analysis of the diagnostic accuracy of MRI for suspected ACL and meniscal tears of the knee. Knee Surg Sports Traumatol Arthrosc. 2016;24(5):1525–1539. doi: 10.1007/s00167-015-3861-8. [DOI] [PubMed] [Google Scholar]
- 38.Ferretti A., Monaco E., Wolf M.R., Guzzini M., Carli A., Mazza D. Surgical treatment of segond fractures in acute anterior cruciate ligament reconstruction. Orthop J Sports Med. 2017;5(10) doi: 10.1177/2325967117729997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Melugin H.P., Johnson N.R., Wu I.T., Levy B.A., Stuart M.J., Krych A.J. Is treatment of segond fracture necessary with combined anterior cruciate ligament reconstruction? Am J Sports Med. 2018;46(4):832–838. doi: 10.1177/0363546517745280. [DOI] [PubMed] [Google Scholar]
- 40.Gaunder C.L., Bastrom T., Pennock A.T. Segond fractures are not a risk factor for anterior cruciate ligament reconstruction failure. Am J Sports Med. 2017;45(14):3210–3215. doi: 10.1177/0363546517726962. [DOI] [PubMed] [Google Scholar]