Abstract
Background
In the absence of adequate harm reduction opportunities, people who inject drugs (PWID) are at increased risk for serious infections. Infectious diseases guidelines recommend extended periods of intravenous antibiotic treatment through peripherally inserted central catheters (PICCs), but PWID are often deemed unsuitable for this treatment. We conducted semi-structured interviews and focus groups to understand the perspectives and opinions of patients and clinicians on the use of PICCs for PWID.
Methods
We approached patients and clinicians (doctors, nurses, PICC nurses, social workers, and case workers) involved in patient care at Tufts Medical Center (Boston, Massachusetts) between August 2019 and April 2020 for semi-structured interviews and focus groups.
Results
Eleven of 14 (79%) patients agreed to participate in an in-depth interview, and 5 role-specific clinician focus groups (1 group consisting of infectious diseases, internal medicine, and addiction psychiatry doctors, 2 separate groups of floor nurses, 1 group of PICC nurses, and 1 group of social workers) were completed. Emergent themes included the overall agreement that PICCs improve healthcare, patients’ feelings that their stage of recovery from addiction was not taken into consideration, and clinicians’ anecdotal negative experiences driving decisions on PICCs.
Conclusions
When analyzed together, the experiences of PWID and clinicians shed light on ways the healthcare system can improve the quality of care for PWID hospitalized for infections. Further research is needed to develop a system of person-centered care for PWID that meets the specific needs of patients and improves the relationship between them and the healthcare system.
Keywords: injection drug use, PICC line, OPAT, opioid use disorder, substance use disorder
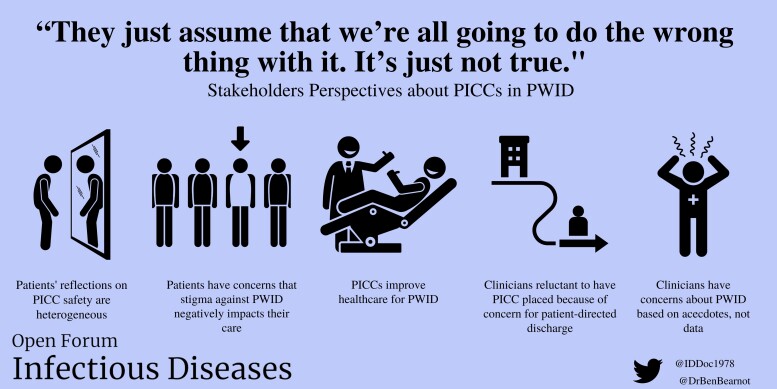
Graphical Abstract
Graphical Abstract.
Interview themes of this study include the use of peripherally inserted central catheters (PICCs) to improve healthcare for people who inject drugs, patients’ fears that stigma affects care, reflections on the safety of PICCs, and the influence of patient-directed discharges on clinicians’ concerns.
The combination of an increasing number of people who inject drugs (PWID) and barriers to accessing evidence based-harm reduction services has led to increases in overdose deaths and serious injection drug–related infections (SIRI) such as endocarditis and osteomyelitis [1–7]. The Infectious Diseases Society of America (IDSA) guidelines recommend treatment with intravenous (IV) antibiotics for SIRI [8], but there are limited data outside of expert opinion to support the route and duration of treatment. Alternatives to 6 weeks of IV treatment are both feasible and efficacious [9–11]. Fearing potential morbidity and mortality, many physicians are hesitant to recommend shortened IV treatment or switch to oral antibiotics [12].
When someone without a substance use disorder is admitted to the hospital with an infection, they are medically stabilized, and then discussions about long-term antibiotic treatments begin. The treatment of serious infections requires a peripherally inserted central catheter (PICC) for continuation of IV antibiotic treatment following discharge. When a PWID is admitted, this practice is complicated by discussions about safety, liability, and concerns that the person will end their hospitalization early, also known as “patient-directed discharge” [13]. A systematic review of the literature identified studies that found comparable outcomes between patients with and without substance use disorder when a PICC is used [14]; however, heterogeneity remains in clinical and organizational policies for PICC lines in PWID [14–17].
With some exceptions [18, 19], research has focused mostly on perspectives of PWID about PICCs [20–22]. The goal of this study is to analyze perspectives of not only the patient, but other key stakeholders—doctors, social workers, floor nurses, and PICC nurses—to get a better appraisal of barriers and facilitators to providing safe, quality, evidence-guided antibiotics to PWID.
METHODS
We received institutional review board approval to conduct this study at Tufts Medical Center in Boston, Massachusetts. Two semi-structured interview guides—1 for patient interviews and another for clinicians—were developed and piloted with key stakeholders prior to research initiation (Supplementary Materials) [23]. The interview guide for PWID focuses on their history of drug use, knowledge of antibiotics, and their perspectives on previous hospital-based interactions. The clinician interviews guide focuses on experience with PICCs in PWID including perceptions of risk with PICCs and strategies to improve care for PWID. Patients were asked their age, self-identified race/ethnicity, and gender. Interviews were conducted by members of the research team (Y. M. and J. Z.) who were trained in qualitative data collection.
We recruited patients to participate in semi-structured interviews using a purposive sampling strategy [24] from the following groups: hospitalized PWID, attending physicians (internal medicine, infectious diseases, and addiction psychiatry), floor nurses, PICC nurses, social workers, and case workers. PWID were identified through communication with inpatient internal medicine teams and the inpatient addiction psychiatrist. Inclusion criteria for patients included self-report of injection drug use within the past year. If eligible, the addiction psychiatrist or medical team asked if the patient would like to speak with a member of the research team to learn more about the study. Then, a research team member (Y. M. or J. Z.) consented the patient and conducted the interview. Clinician inclusion criteria included working at Tufts Medical Center and involvement in the care of PWID. Clinicians were emailed with an invitation to participate in 1-hour-long focus groups. Verbal consent for interviews was obtained at the time of the focus group; demographics were not recorded for these to protect the identity of individuals working in small teams. Interviews were recorded with participant permission and transcribed. Patients were given an insulated water bottle as a gift for compensation. Staff received a complimentary meal during the focus group except for 1 post–COVID-19 pandemic focus group that met without food.
Transcripts were analyzed using Dedoose version 6.1.18 (SocioCultural Research Consultants, University of California, Los Angeles). After developing a preliminary set of codes into separate codebooks for each of the 2 interview types (Supplementary material), 2 research team members (J. Z. and Y. M.) coded a subsample of interviews to ensure consensus on codes used by researchers and revised the codebook to include any new codes and emergent themes (Supplementary material). The codebook was continually revised, with each new version used to recode interviews until no new codes emerged. The research team next analyzed data thematically. Discrepancies in coding were resolved using a comparison and consensus approach. After coding all interviews, the research team compared themes from each to determine overlaps or points of divergence to highlight in the results. Analysis revealed that we achieved thematic saturation with both samples, suggesting that interviewing more participants would not have added additional novel information.
RESULTS
We approached 14 patients, and 11 agreed to participate in an interview (Supplementary Table 1). We held 5 focus groups: 1 with physicians (n = 6), 2 with floor nurses (first group with 5 nurses, second group with 6 nurses), 1 with nurses who are trained to insert and remove PICCs (n = 5), and 1 with social workers (n = 2). No case workers whom we approached agreed to interview. We identified 5 themes, including beliefs that PICCs improve healthcare delivery to PWID, patient concerns about the effects of stigma on their care, patient reflections on the safety of PICCs, clinicians’ discomfort with PICCs in PWID, and the impact of patient-directed discharges on clinician concerns.
PICCs Improve Healthcare Delivery to PWID
Nurses and patients expressed how PICCs improved the quality of care. Nurses reported that drawing blood for laboratory tests was frequently challenging due to poor venous access among PWID. One nurse said that PWID are “really sensitive. You don’t know which way they’re going to go. Some just lie there and others are freaking out that you’re going to poke them with a needle.” However, PICCs made it easier for nurses to do their jobs: “If they have an extended indwelling line or a PICC where we know we have that security there, especially for our tough to stick patients, [that] definitely makes our job a lot easier and less stressful when those situations occur.” Another nurse commented that without a PICC, there can be barriers to delivering care: “You’re delaying those IV antibiotics for almost a whole day, because by the time … [doctors] decide [that they] finally want to [place a] PICC line … you know you’re pushing back a whole day’s worth of IV antibiotics.”
Patients Expressed Concerns the Effects of Stigma on Care
Most patients reported that although they either currently or previously used drugs, they felt unfairly judged and expressed feeling stigmatized by the clinicians in terms of their suitability for a PICC. One said, “They just assume that we’re all going to do the wrong thing with [the PICC]. It’s just not true” (37-year-old White female). Patients wanted their substance use disorder to be evaluated on an individualized basis. “It depends what type of people you’re dealing with, you know what I mean? Stable or not stable, cause it’s a lot of different people out there. So, you got to know, it’s like who you give a gun to, you know, who you going to give a gun to? You know what I mean? If that person is going to be responsible or [not], that type of thing” (41-year-old White male). One patient expressed understanding that the clinicians may have concerns about sending PWID home with a PICC line, “There is people out there, like myself, I’ve been an IV drug user. I can go home with a PICC line. And I’d have no worries. But at the same time, I know [people] that will say that same thing when they’re totally full of [it]. I can honestly say I can go home with a PICC line, no problem. But you know, do I expect the doctor to believe that? No.” (41-year-old White male).
Patients Reflected on the Safety of PICCs for Themselves and Other PWID
Patients reflected on the nuances of safe use of PICCs for themselves and for other PWID, recognizing heterogeneity between themselves and other people who inject. Most people felt that injection into the PICC was very risky. Several patients discussed the risks of PICCs, including one who stated, “I know they don’t want people walking out with PICC lines that go straight to the heart, if they get dirt in there they’re done. I don’t think people would use it at home” (54-year-old Black male). Another patient reflected on their own illness, saying, “I would never get a PICC line. Like, they will give me the option to do that, but I don’t because I know that—unless I’m a hundred percent sure that I’m not going to use again, I wouldn’t do it … I’m not going to risk my life like that” (38-year-old female, race not reported). When asked about policies that prevent placing a PICC in injection drug users, 1 patient said, “I don’t know. I haven’t used in years and years. But I can see why they’d be concerned because of usage through that line. But I think even if you are using, it’s pretty stupid on your part” (36-year-old White female). Another patient agreed, saying “It’s probably the … most dangerous thing I’ve ever seen for some people to have PICC lines. I’m sure they are a very good thing overall for people who need them, but there’s a huge danger in giving them to IV drug users” (41-year-old White male). An additional patient believed that inserting PICCs in PWID creates an enticement for injecting drugs: “Someone who’s actively using should not be able to leave the hospital with a PICC line. It’s just too much of a temptation” (White female, unreported age). Another patient also believed that many PWID would use the line if possible: “Most of these people will use them, I think. If they’re not supervised. And I think that there needs to be some supervision along the lines of the PICC line, but I think we need to have some accessibility to fresh air and visits, and rights” (35-year-old female, unreported race). This patient additionally said, “They need to watch these people with PICC lines because they’re going to use them.” One patient said they didn’t know anyone who ever used the PICC to inject, and 2 people said they knew of people who did it. One patient said they injected into their PICC previously.
Physicians and Nurses Feel Uncomfortable When PWID Have PICCs
Physicians had strong opinions about the safety of PICCs in this patient population and relied on anecdotes for those opinions. Without providing specific supporting literature, 1 clinician estimated, “I would probably say it’s like 75% of those types of patients will abuse their line in an inappropriate way.” Another said, “I would never discharge a patient with an active substance use disorder who is not going to a facility with a PICC line to home … I’ve had patients with substance use disorder basically say, that is the golden line, if you walk out of the hospital with one of those.” A different physician said, “The risk [of a PICC in PWID] is too great. The VNA [Visiting Nurse Association] won’t even deal with it. No one will manage it; the risk is too great for the overdose. It’s sad because the patient themselves is making a conscious decision to use it. And they all know, I mean we all know that addiction is just—you know is so strong.” Another doctor said, “I would think that’s an unsafe discharge. Because it’s like we know your history. ‘Yeah bye, like good luck. Like try not to use that line.’ We’re kind of giving you a gateway to misuse. It’s a temptation and unfortunately when people are tempted, they don’t always make the right decisions.”
Nurses also reported not feeling comfortable with PICCs. One nurse said, “All of us want them to get better, but then we end up babysitting, and I hate to use that word and the negative connotation …. You know so you feel horrible, you want them to get better, but at the same time, it can be exhausting.” Another nurse worried about patients who had PICCs and were in the hospital: “I’ve been here 40 years. You kind of have a sixth sense, you know you just say, huh, but there were some—there are always the 1 or 2 that just fool you and you think they’re absolutely fine, you have no idea that they had any type of substance abuse and they go home and they’re just going to try it because they’ve got access. It’d make you feel horrible.” Another nurse said that after the PICC is placed, “[w]e also are more vigilant as to you know what are they doing on their own, behind a closed door? You’re hypervigilant and then when they do something, you get so angry at them.”
Alternatively, a few physicians felt that PICCs did not increase the risk of substance use or overdose. One clinician said, “If they were going to overdose on a drug it didn’t matter that the PICC line was available to them.” Another clinician said, “Most of my patients don’t really need a PICC to inject. It’s just not a limiting factor, quite honestly. If you say, ‘this is for your medication,’ they're like, okay … but I think most adults are adults, like you can have a real conversation with them and tell them about risks and benefits.”
Negative Impact of “Against Medical Advice” Discharges on Clinicians’ Perspectives on PICCs
Throughout several interviews, clinicians talked about their perceptions of an association between hospitalized PWID and increased risk of “against medical advice” (AMA) discharges (patient-directed discharges). One doctor said, “It was this negotiating dance of wanting to grant her autonomy and trying to find rehab placement that met her criteria and met her insurance criteria. And I mean, frankly, it didn't even occur to me [to send her home], I think because she was particularly high risk for overdose and was engaging in some risky—like, some red flag behaviors in the hospital—that we, sending her home wasn’t even an option for me, and I certainly extended her stay as we looked at different rehab options. Ultimately, she did leave against medical advice.” Patient-directed discharge is perceived as a common occurrence and was often considered “failure” of treatment, resulting in a sense of futility from clinicians. One PICC nurse echoed this sentiment, stating, “We set them up to fail anyway. Well, they set themselves up to fail because they sign out AMA before the treatment is completed because they are in charge of themselves and they can do what they want, you know? At the end of the day the day they can leave.” After talking about the importance of substance use disorder treatment, one social worker said, “When you look at people with substance use disorder, if they’re deep into it they’ve given up their family, their friends, their job. So why not give up on antibiotics? I mean that’s way down the list if you think of it after all those other things I just named. So, I think it’s a big ask that most of us would, I would fail at it quite honestly.”
DISCUSSION
Our interviews with PWID and clinicians revealed several important themes. First, we found that both patients and clinicians felt that PICCs improve healthcare by increasing timely access to medications and laboratory testing. Second, we found that most patients felt stigmatized during their treatment for infections and preferred an individualized treatment approach considering their stage and severity of substance use disorder. Third, we found that many patients reflected that their views on PICCs were personal to them and may not reflect how other PWID think about them. Fourth, we found that clinicians were hesitant to discharge PWID from the hospital with a PICC and expressed concerns about patient-directed discharges.
Notably, many of the clinicians relied on anecdotes and not data. There are now several studies showing that PICCs are safe in a subset of PWID, especially people with stable housing and those receiving medications for opioid use disorder (OUD), which are proven to reduce all-cause and opioid-related mortality [25–31]. There are data showing that a subset of people inject drugs through their PICC, but often this is in the situation of suboptimal addiction management [32]. However, there is evidence that PICCs help support healthcare in PWID [32]. Some of the perceived conflicts surrounding the care of PWID involves difficulty with vein access and appropriate pain management. These are often points of tension between healthcare workers and patients [33]. Pain management is essential to improve the hospital experience of all patients, but pain medications are often used conservatively in PWID, leading to inadequate pain management [21, 22, 34, 35]. Many of these issues may be alleviated if a PICC could be placed for these patients, providing a secure and reliable method of vein access for timely labs and delivery of medications. In fact, when discussing PICCs, both patients and clinicians seemed receptive to placement of a PICC for use in the hospital setting. There could be more opportunities to deliver high-quality care by earlier PICC placement for PWID who are hospitalized; however, concerns about the frequency and liability of patient-directed discharges will need to be addressed first.
It is worth noting that although discharges AMA do happen in PWID, they happen in all patients, including people who do not inject drugs [36]. One study found that patient-directed discharges are increasing among both people with injection drug–related endocarditis and people with non-injection-drug–related endocarditis [37]. Studies with PWID found that there are many reasons given for patient-directed discharges, including negative interactions with hospital staff, inadequate management of pain and withdrawal, boredom, and isolation from social support [21, 38]. To improve interactions with staff and adequately manage pain and withdrawal, consultation with addiction experts is both necessary and best-practice healthcare. There is evidence that people who leave prematurely have lower opioid dosing, suggesting that more could have been done to keep them comfortable [39, 40]. When the chronic disease of addiction is prioritized in tandem with what brought them to the hospital, patients frequently reported more positive hospital experiences and a greater willingness to engage in treatment. This willingness to engage in treatment ensures both better care for the patient, and less emotional distress in providing care for the nursing and clinical staff.
If a patient wants to leave the hospital earlier than clinicians feel is safe, shared decision making is necessary to offer alternative treatments, including oral and long-acting injectable antibiotics in addition to treatment options for OUD, including medications. There is some evidence among people without OUD that 6 weeks of IV antibiotics may not be necessary for endocarditis, suggesting that flexible treatment options may become available to reduce patient-directed discharges [41]. We posit that most medical treatments come with risk-benefit tradeoffs that teams of healthcare professionals must routinely consider. These difficult decisions must be made with an approach of shared decision making with patients. Strategies that alleviate the challenging aspects of PWID’s care, such as undertreated pain, psychological distress, and discrimination, may reduce the negative hospital experiences that feed into the biases that both patients and providers’ harbor.
Our work adds to a growing body of qualitative research among PWID and clinicians [18, 19, 42, 43]. Studies among PWID have identified common patterns of care, including early addiction treatment and intensive outpatient care leading to periods without rehospitalization, whereas individuals who left outpatient care and resumed drug use were more likely to be rehospitalized [20]. Despite this evidence, several stakeholders in the PICC decision making process felt underprepared to care with PWID, and believed there were not clear guidelines. Augmented training programs may help support clinicians working with this unique patient population [18, 32]. Nurses’ voices have largely been missing from this research [44]. Our research team’s qualitative work with nurses about caring for people with OUD found that nurses were understanding of the struggles that OUD patients endure during hospitalization, though the nurses similarly reported that patients’ struggles lead to professional and emotional distress for nurses and patients alike [43].
Our study has several limitations. First, our patient study sample lacked racial and ethnic diversity. More than 70% of patient study participants were White and non-Hispanic, limiting the study’s generalizability. Stakeholders were recruited from a single academic hospital center in a Medicaid expansion state, further liming generalizability. Second, we only were able to hold 1 focus group with physicians, limiting data collection from a group with significant influence on PICC decision making. Additionally, we were not able to recruit case managers, who play a key role in the discharge and follow-up care planning for patients. Our inability to recruit case workers may be reflective of overwhelming work conditions.
Despite these limitations, this study highlights the biases, tensions, and emotional stress that all stakeholders experience surrounding the use of PICCs in PWID. Both patients and clinicians had a diverse set of opinions that need to be considered to improve the care of these patients. Reflecting this heterogeneity in patients in hospital policies regarding the use of PICCs in PWID will be a critical step in not only improving the hospital experience of these patients, but also the lives and relationships that hospital staff have with this patient population.
Supplementary Material
Contributor Information
Yoelkys Morales, Tufts University School of Medicine, Boston, Massachusetts, USA.
Emma Smyth, Division of Geographic Medicine and Infectious Diseases, Department of Medicine, Tufts Medical Center, Boston, Massachusetts, USA.
Julia Zubiago, Division of Geographic Medicine and Infectious Diseases, Department of Medicine, Tufts Medical Center, Boston, Massachusetts, USA.
Benjamin Bearnot, Department of Medicine, Massachusetts General Hospital, Boston, Massachusetts, USA; Harvard Medical School, Boston, Massachusetts, USA.
Alysse G Wurcel, Tufts University School of Medicine, Boston, Massachusetts, USA; Division of Geographic Medicine and Infectious Diseases, Department of Medicine, Tufts Medical Center, Boston, Massachusetts, USA.
Supplementary Data
Supplementary materials are available at Open Forum Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Notes
Author contributions. Y. M.: funding acquisition, conceptualization, methodology, data curation, formal analysis, investigation, writing–original draft, writing–review and editing. E. S.: formal analysis, investigation, data curation, writing–original draft, writing–review and editing, visualization. J. Z.: data curation, formal analysis, investigation, writing–review and editing. B. B.: methodology, writing–review and editing. A. G. W.: conceptualization, methodology, validation, writing–review and editing, project administration.
Acknowledgments. The authors thank the study participants for taking time to participate in this study.
Patient consent. We received consent to interview and publish interviews for all subjects in this study. The study design was approved by the Tufts University Health and Sciences Institutional Review Board.
Financial support. This work was supported by the Infectious Diseases Society of America (GERM Seed Grant to Y. M.) and the National Institutes of Health (grant numbers K08HS026008-01A and K12DA043490 to A. G. W. and B. B.).
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Capizzi J, Leahy J, Wheelock H, et al. . Population-based trends in hospitalizations due to injection drug use-related serious bacterial infections, Oregon, 2008 to 2018. PLoS One 2020; 15:e0242165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Levitt A, Mermin J, Jones CM, See I, Butler JC. Infectious diseases and injection drug use: public health burden and response. J Infect Dis 2020; 222(Suppl 5):S213–7. [DOI] [PubMed] [Google Scholar]
- 3. Ronan MV, Herzig SJ. Hospitalizations related to opioid abuse/dependence and associated serious infections increased sharply, 2002–12. Health Affairs 2016; 35:832–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sredl M, Fleischauer AT, Moore Z, Rosen DL, Schranz AJ. Not just endocarditis: hospitalizations for selected invasive infections among persons with opioid and stimulant use diagnoses—North Carolina, 2010–2018. J Infect Dis 2020; 222(Suppl 5):S458–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wurcel AG, Anderson JE, Chui KK, et al. . Increasing infectious endocarditis admissions among young people who inject drugs. Open Forum Infect Dis 2016; 3:ofw157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Serota DP, Tookes HE, Hervera B, et al. . Harm reduction for the treatment of patients with severe injection-related infections: description of the Jackson SIRI Team. Ann Med 2021; 53:1960–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Islam S, Piggott DA, Moriggia A, et al. . Reducing injection intensity is associated with decreased risk for invasive bacterial infection among high-frequency injection drug users. Harm Reduct J 2019; 16:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lavender TW, McCarron B. Acute infections in intravenous drug users. Clin Med 2013; 13:511–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Marks LR, Liang SY, Muthulingam D, et al. . Evaluation of partial oral antibiotic treatment for persons who inject drugs and are hospitalized with invasive infections. Clin Infect Dis 2020; 71:e650–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Vazquez Deida AA, Shihadeh KC, Preslaski CR, Young HL, Wyles DL, Jenkins TC. Use of a standardized dalbavancin approach to facilitate earlier hospital discharge for vulnerable patients receiving prolonged inpatient antibiotic therapy. Open Forum Infect Dis 2020; 7:ofaa293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lewis S, Liang SY, Schwarz ES, et al. . Patients with serious injection drug use-related infections who experience patient-directed discharges on oral antibiotics have high rates of antibiotic adherence but require multidisciplinary outpatient support for retention in care. Open Forum Infect Dis 2022; 9:ofab633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mertz D, Viktorin N, Wolbers M, et al. . Appropriateness of antibiotic treatment in intravenous drug users, a retrospective analysis. BMC Infect Dis 2008; 8:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Fanucchi L, Leedy N, Li J, Thornton AC. Perceptions and practices of physicians regarding outpatient parenteral antibiotic therapy in persons who inject drugs. J Hosp Med 2016; 11:581–2. [DOI] [PubMed] [Google Scholar]
- 14. Suzuki J, Johnson J, Montgomery M, Hayden M, Price C. Outpatient parenteral antimicrobial therapy among people who inject drugs: a review of the literature. Open Forum Infect Dis 2018; 5:ofy194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Eaton EF, Mathews RE, Lane PS, et al. . A 9-point risk assessment for patients who inject drugs and require intravenous antibiotics: focusing inpatient resources on patients at greatest risk of ongoing drug use. Clin Infect Dis 2019; 68:1041–3. [DOI] [PubMed] [Google Scholar]
- 16. Ceniceros AG, Shridhar N, Fazzari M, Felsen U, Fox AD. Low use of outpatient parenteral antimicrobial therapy for drug use-associated infective endocarditis in an urban hospital system. Open Forum Infect Dis 2021; 8:ofab083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. D’Couto HT, Robbins GK, Ard KL, Wakeman SE, Alves J, Nelson SB. Outcomes according to discharge location for persons who inject drugs receiving outpatient parenteral antimicrobial therapy. Open Forum Infect Dis 2018; 5:ofy056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hayden M, Moore A. Attitudes and approaches towards repeat valve surgery in recurrent injection drug use-associated infective endocarditis: a qualitative study. J Addict Med 2020; 14:217–23. [DOI] [PubMed] [Google Scholar]
- 19. Wurcel AG, Zubiago J, Reyes J, et al. . Surgeons’ perspectives on valve surgery in people with drug use-associated infective endocarditis [manuscript published online ahead of print 31 January 2022]. Ann Thorac Surg 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Bearnot B, Mitton JA. “You’re always jumping through hoops”: journey mapping the care experiences of individuals with opioid use disorder–associated endocarditis. J Addict Med 2020; 14:494–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Pollini RA, Paquette CE, Drvar T, et al. . A qualitative assessment of discharge against medical advice among patients hospitalized for injection-related bacterial infections in West Virginia. Int J Drug Policy 2021; 94:103206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Biancarelli DL, Biello KB, Childs E, et al. . Strategies used by people who inject drugs to avoid stigma in healthcare settings. Drug Alcohol Depend 2019; 198:80–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Chun Tie Y, Birks M, Francis K. Grounded theory research: a design framework for novice researchers. SAGE Open Med 2019; 7:2050312118822927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Palinkas LA, Horwitz SM, Green CA, Wisdom JP, Duan N, Hoagwood K. Purposeful sampling for qualitative data collection and analysis in mixed method implementation research. Adm Policy Ment Health 2015; 42:533–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Camsari UM, Libertin CR. Small-town America’s despair: infected substance users needing outpatient parenteral therapy and risk stratification. Cureus 2017; 9:e1579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Fanucchi LC, Walsh SL, Thornton AC, Nuzzo PA, Lofwall MR. Outpatient parenteral antimicrobial therapy plus buprenorphine for opioid use disorder and severe injection-related infections. Clin Infect Dis 2020; 70:1226–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Seval N, Eaton E, Springer SA. Beyond antibiotics: a practical guide for the infectious disease physician to treat opioid use disorder in the setting of associated infectious diseases. Open Forum Infect Dis 2020; 7:ofz539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Jewell C, Weaver M, Sgroi C, Anderson K, Sayeed Z. Residential addiction treatment for injection drug users requiring intravenous antibiotics: a cost-reduction strategy. J Addict Med 2013; 7:271–6. [DOI] [PubMed] [Google Scholar]
- 29. Price CN, Solomon DA, Johnson JA, Montgomery MW, Martin B, Suzuki J. Feasibility and safety of outpatient parenteral antimicrobial therapy in conjunction with addiction treatment for people who inject drugs. J Infect Dis 2020; 222(Suppl 5):S494–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Paras ML, Wolfe SB, Bearnot B, et al. . Multidisciplinary team approach to confront the challenge of drug use-associated infective endocarditis [manuscript published online ahead of print 5 November 2021]. J Thorac Cardiovasc Surg 2021. [DOI] [PubMed] [Google Scholar]
- 31. Weimer MB, Falker CG, Seval N, et al. . The need for multidisciplinary hospital teams for injection drug use-related infective endocarditis [published online ahead of print 10 September 2021]. J Addict Med 2021. [DOI] [PubMed] [Google Scholar]
- 32. Guta A, Perri M, Strike C, Gagnon M, Carusone SC. “With a PICC line, you never miss”: the role of peripherally inserted central catheters in hospital care for people living with HIV/HCV who use drugs. Int J Drug Policy 2021; 96:103438. [DOI] [PubMed] [Google Scholar]
- 33. Harris M, Rhodes T. Venous access and care: harnessing pragmatics in harm reduction for people who inject drugs. Addiction 2012; 107:1090–6. [DOI] [PubMed] [Google Scholar]
- 34. Voon P, Callon C, Nguyen P, et al. . Denial of prescription analgesia among people who inject drugs in a Canadian setting. Drug Alcohol Rev 2015; 34:221–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. McNeil R, Small W, Wood E, Kerr T. Hospitals as a “risk environment”: an ethno-epidemiological study of voluntary and involuntary discharge from hospital against medical advice among people who inject drugs. Soc Sci Med 2014; 105:59–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Alfandre D. Web exclusive. Annals for hospitalists inpatient notes—challenging the myths of the against medical advice discharge. Ann Intern Med 2021; 174:HO2–3. [DOI] [PubMed] [Google Scholar]
- 37. Kimmel SD, Kim JH, Kalesan B, Samet JH, Walley AY, Larochelle MR. Against medical advice discharges in injection and non-injection drug use–associated infective endocarditis: a nationwide cohort study. Clin Infect Dis 2021; 73:e2484–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Alfandre DJ. “I’m going home”: discharges against medical advice. Mayo Clin Proc 2009; 84:255–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Santos CJ, Shofer FS, Lowenstein M, Perrone J. Discharges “against medical advice” in patients with opioid-related hospitalizations. J Addict Med 2021; 15:49–54. [DOI] [PubMed] [Google Scholar]
- 40. Nolan NS, Marks LR, Liang SY, Durkin MJ. Medications for opioid use disorder associated with less against medical advice discharge among persons who inject drugs hospitalized with an invasive infection. J Addict Med 2021; 15:155–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Wald-Dickler N, Holtom PD, Phillips MC, et al. . Oral is the new IV. challenging decades of blood and bone infection dogma: a systematic review. Am J Med 2022; 135:369–79.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Bearnot B, Mitton JA, Hayden M, Park ER. Experiences of care among individuals with opioid use disorder-associated endocarditis and their healthcare providers: results from a qualitative study. J Subst Abuse Treat 2019; 102:16–22. [DOI] [PubMed] [Google Scholar]
- 43. Horner G, Daddona J, Burke DJ, Cullinane J, Skeer M, Wurcel AG. “You’re kind of at war with yourself as a nurse”: perspectives of inpatient nurses on treating people who present with a comorbid opioid use disorder. PLoS One 2019; 14:e0224335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Bartlett R, Brown L, Shattell M, Wright T, Lewallen L. Harm reduction: compassionate care of persons with addictions. Medsurg Nurs 2013; 22:349–53, 358. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.