Abstract
Objectives
High-intensity focused ultrasound (HIFU) is a noninvasive therapeutic modality with a variety of applications. It is approved for the treatment of essential tremors, ablation of prostate, hepatic, breast, and uterine tumors. Although not approved for use in the treatment of atherosclerotic arterial disease, there is a growing body of evidence investigating applications of HIFU. Currently, percutaneous endovascular techniques are predominant for the treatment of arterial pathology; however, there are no endovascular techniques of HIFU available. This study aims to review the state of current evidence for the application of HIFU in atherosclerotic arterial disease.
Methods
All English-language articles evaluating the effect of HIFU on arterial occlusive and thrombotic disease until 2021 were reviewed. Both preclinical and human clinical studies were included. Study parameters such as animal or clinical model and outcomes were reviewed. In addition, details pertaining to settings on the HIFU device used were also reviewed.
Results
In preclinical models, atherosclerotic plaque progression was inhibited by HIFU, through decreases in oxidized low-density lipoprotein cholesterol and increases in macrophage apoptosis. Additionally, HIFU promotes angiogenesis in hindlimb ischemic models by the upregulation of angiogenic and antiapoptotic factors, with increased angiogenesis at higher line densities of HIFU. HIFU also promotes thrombolysis and conversely induces platelet activation at low frequencies and higher intensities. Various clinical studies have attempted to translate some of these properties and demonstrated positive clinical outcomes for arterial recanalization after thrombotic stroke, decreased atherosclerotic plaque burden in carotid arteries, increase in tissue perfusion and a decrease in diameter stenosis in patients with atherosclerotic arterial disease.
Conclusions
In current preclinical and clinical data, the safety and efficacy of HIFU shows great promise in the treatment of atherosclerotic arterial disease. Future focused studies are warranted to guide the refinement of HIFU settings for more widespread adoption of this technology.
Keywords: Peripheral arterial disease, High-intensity focused ultrasound, Atherosclerosis, Arterial thrombosis
Peripheral arterial disease (PAD) affects more than 200 million people worldwide and 8 to 12 million people in the United States.1, 2, 3, 4 Chronic limb-threatening ischemia represents an advanced stage of PAD, associated with a dismal prognosis of approximately 25% mortality and 30% amputation rates at 1 year.5,6 Moreover, the rates of reinterventions after revascularization remain high, ranging from 20% to 60%, owing to various anatomic, medical, and behavioral factors.7, 8, 9, 10, 11, 12, 13, 14 Technological advances have introduced various novel minimally invasive therapeutic modalities such as atherectomy devices, drug-eluting stents and balloons, in an attempt to improve vessel patency and decrease the reintervention rate.15 However, these therapeutic modalities remain invasive and require intraarterial manipulation.
High-intensity focused ultrasound (HIFU) is a noninvasive therapeutic modality, that uses nonionizing ultrasonic waves for focused ablation of desired soft tissues, when acoustic windows are available. The earliest reported use of HIFU was by Lynn et al in 1942,16 who designed a focused ultrasound generator, which produced focused heating in paraffin blocks and liver tissue. They demonstrated that high-intensity ultrasound waves could alter the biologic structure of the targeted tissue and posited that these principles could be applied to humans. Around the same time, Fry et al17,18 in the 1950s, used HIFU for thermal ablation of various deep brain structures in experimental animal models. This technology, however, did not rapidly develop owing to the inability to precisely target the desired tissue. Since then, advances in medical physics, imaging and engineering principles have culminated in US Food and Drug Administration (FDA) approval of HIFU for use in the treatment of uterine fibroids, adenomyosis, essential tremors, neuropathic pain, ablation of bone metastases, and prostate cancer. Along with approved therapeutic applications, a growing body of evidence has emerged for use of HIFU in occlusive and thrombotic arterial disease. Although endovascular techniques are predominant for the treatment of arterial pathology, there are no endovascular techniques of HIFU available. This review aims to clarify the basic principles of HIFU related to occlusive and thrombotic disease, highlight the current translational and clinical data supporting the use of HIFU, underscore its limitations, and provide a glimpse into the future directions for HIFU technology in occlusive and thrombotic arterial disease.
Methods
A literature search of all English language articles in Medline, EMBASE, Web of Science, and Cochrane databases up till 2021 was conducted. The search terms used were “high intensity focused ultrasound” and “atherosclerosis” or “peripheral arterial disease” or “arterial thrombosis” and related terms or abbreviations. All abstracts and full text papers were reviewed by two independent reviewers (A.B and S.M.C), and all differences were resolved in consultation with the senior author (E.A). A total of 313 articles were initially identified. After reviewing for relevance, 303 articles were excluded because they did not meet inclusion criteria of being relevant to HIFU and arterial disease. Sixteen studies were snowballed into the final number of studies, using references and additional searching (Fig 1). Thus, 26 total articles were included in this qualitative review (15 preclinical studies and 11 clinical studies, including 2 that encompassed both preclinical and clinical data).
Fig 1.
Search criteria and methodology.
Results
Principles of HIFU
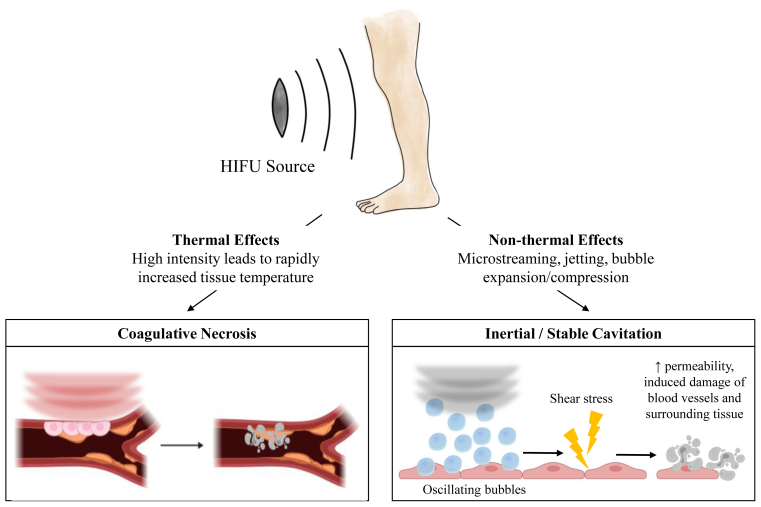
The therapeutic effect of HIFU relies on two different physical mechanisms– thermal and nonthermal (Fig 2). Both effects are achieved by using a higher intensity, when compared with diagnostic ultrasound imaging (<0.1W/cm2). The thermal effects of tissue ablation, and coagulative necrosis, are achieved with an intensity ranging between 100W/cm2 up to 10,000W/cm2,19, 20, 21 when the ultrasound energy is absorbed by the tissue. At these intensities, ultrasound energy absorbed by the desired tissue is converted to heat and results in coagulation necrosis; this process is presumed to be the primary mechanism of action for the FDA-approved uses of HIFU ablation for prostate carcinoma, uterine fibroids, and essential tremor.22, 23, 24 The nonthermal effects of HIFU are potentiated by cavitation. At high intensities and low frequencies, ultrasound energy transmitted to the tissues leads to the formation of microscopic bubbles, otherwise known as acoustic cavitation. These bubbles oscillate and enlarge, thereby transmitting shear stress to surrounding tissues, resulting in stable cavitation.21,25 The vascular effects of acoustic cavitation can be attributed to several potential mechanisms—microstreaming, jetting, bubble expansion, and compression.26, 27, 28 An alternate form of cavitation, known as inertial cavitation, results from unstable bubble expansion followed by collapse, resulting in damage to the blood vessels and surrounding tissue.20 Microstreaming results in shear stress transmission to endothelial cells from oscillating bubbles, whereas jetting results from asymmetric collapse of the bubbles and is potentially responsible for increased vascular permeability.26
Fig 2.
Principles of high-intensity focused ultrasound (HIFU) based on the settings of high intensity focused ultrasound devices, there are thermal and nonthermal effects on tissues. At intensities ranging between 100 W/cm2 up to 10,000 W/cm2, the absorbed ultrasound energy is converted to heat, resulting in coagulative necrosis. In contrast, at lower frequencies, ultrasound energy results in acoustic cavitation within the tissues, responsible for the nonthermal effects. The oscillatory energy from the bubbles transmits shear stress to the surrounding tissues, also known as microstreaming, resulting in stable cavitation. In contrast, asymmetric rapid bubble expansion and collapse results in damage to blood vessels and surrounding tissues, known as jetting, results in inertial cavitation.
The generated ultrasound energy can be focused on the desired tissues through various focusing techniques, such as geometric focusing, electronic focusing, or acoustic focusing. Geometric focusing uses a spherical, concave transducer surface, whereas acoustic focusing uses an acoustic lens for beam focusing. In contrast, electronic focusing relies on multiple piezoelectric crystals with varying excitation signals. An important discrimination is that the latter technique has the ability to displace the focal point without moving the transducer by altering the exciting signal; this technique is known as electronic steering.20,21 This feature of the HIFU system permits precision in tissue targeting with minimal to no effect to the surrounding area.29 In addition to the ability to generate and focus ultrasound beams, a HIFU device must also concomitantly be able to monitor the target tissue, under continuous image guidance, with magnetic resonance imaging or ultrasound examination. To achieve this goal, a real-time dual-mode ultrasound array (DMUA) system for simultaneous imaging and therapy has been developed and described.30,31
Current FDA-approved devices
Currently, there are several FDA-approved HIFU devices for prostate carcinoma, fibroids, and essential tremor. The recently initiated FDA approved trial of HIFU for varicose vein ablation (Sonovein, Theraclion, Malakoff, France) suggests interest from vascular specialists in this technology.32 At the time of this writing, however, there are no FDA-approved HIFU devices for use in the treatment of PAD, although it is evident that there is a growing body of literature surrounding its clinical applicability. Although HIFU may benefit certain patients, the slow uptake for these FDA-approved devices suggests the need for robust, comparative trials.
Comparison of HIFU with other acoustic therapeutic modalities
Currently available acoustic therapeutic modalities for intravascular use include EkoSonic (EKOS) system (Boston Scientific, Malborough, MA) and Shockwave Peripheral Lithoplasty System (Shockwave Medical Inc., Santa Clara, CA). Intravascular delivery of ultrasound has been assessed in prior in vitro and in vivo studies both for thrombus and atherosclerotic plaques.33, 34, 35 The EkoSonic (EKOS) system, which combines the principles of intravascular deliverance of ultrasound with fibrinolytic pharmacotherapy, changed treatment of thrombotic processes. EKOS is based on the longstanding principle that the mechanical effects of ultrasound allows for disruption of fibrin strands in thrombus, allowing for the increased uptake of fibrinolytic agents.36 Multiple large-scale studies such as the Ultrasound Accelerated Thrombolysis of Pulmonary Embolism (ULTIMA) trial and the EkoSonic Endovascular System and Activase for Treatment of Acute Pulmonary Embolism (SEATTLE II) trial have demonstrated clinical efficacy of intravascular ultrasonic energy to augment the effect of thrombolytic agents.37,38 In arterial thrombosis, a frequency of 2.2 MHz delivered at a low power (2.1 W) has been effectively used in conjunction with thrombolytic agents.39 Compared with the EKOS catheter system, which is an invasive modality, HIFU is an extracorporeal, noninvasive modality that requires higher ultrasonic energy to compensate for attenuation.40
Shockwave therapy is another acoustic modality with recent applications in occlusive atherosclerotic disease and intravascular or extracorporeal modes of delivery. The intravascular application of shockwave therapy was assessed in the Disrupt studies, using the Shockwave Peripheral Lithoplasty System (Shockwave Medical Inc.) and have demonstrated efficacy in treating stenotic, calcified lesions with a favorable safety profile.41,42 The most recent Disrupt III study assessed lithoplasty treatment in combination with drug-coated balloons versus standard balloon angioplasty with drug-coated balloons. In patients with claudication or chronic limb-threatening ischemia and moderate or severe calcification, an initial analysis demonstrated promising results, whereby the use of intravascular lithotripsy was effective at treating stenotic lesions with low rates of complications.43 Extracorporeal shockwave therapy for PAD is also being investigated as a noninvasive therapeutic modality, although data remain limited. The principles of shockwave therapy are multifactorial and may include effects on the growth and differentiation of vasculature, nitric oxide synthesis, and macrocirculation.44 In murine models, shockwave therapy can induce vascular endothelial growth factor receptor 2 and hypoxia-inducible factor-1 alpha, overall allowing for increased angiogenesis.45,46 It has further been suggested that shockwave therapy can mobilize endothelial progenitor cells to promote vasculogenesis.46 In multiple small human cohorts, low-energy, extracorporeal shockwave therapy has been shown to decrease arterial stenoses, improve microcirculation in limbs, and improve pain-free walking distance and pain severity scores.47, 48, 49
Translational data for applications in arterial disease
Owing to promising results from other applications of HIFU, the impact of HIFU on the progression of atherosclerosis, ability to assist targeted drug delivery for stenotic arterial lesions and sonothrombolysis for acute arterial thromboses are being investigated. Several in vivo and in vitro studies have elucidated the various potential mechanisms of HIFU in atherosclerotic arterial disease (Table I).
Table I.
Overview of Preclinical data of high-intensity focused ultrasound (HIFU) in occlusive and thrombotic arterial disease
| Author(s) | Year | Model | Device name | Proposed mechanism of action | Available specs | Clinical application |
|---|---|---|---|---|---|---|
| Effect on arterial plaque and arterial wall | ||||||
| Shehata et al30 | 2013 | Swine | Imasonic Dual-Mode US Array (Voray sur l’Ognon, France) | Thermal | Frequency: 3.5 MHz, 64-element phased array transducer with fenestrations, through which 10 MHz transducer is applied Intensity: 4100-5600 W/cm2 Pulse length: 250-2000 ms |
Disruption of atherosclerosis in swine PAD model, accompanied by aggregates of lipid laden macrophages with necrosis. No endothelial damage was noted |
| Nazer et al50 | 2015 | Sprague Dawley rats (PAD) | Duolith SD1 (Storz Medical, Tagerwilen, Switzerland) | Biomechanical | Frequency: 1.054 MHz Intensity: 0.1 mJ/mm2 |
Increase in angiogenesis in hindlimb ischemia model for PAD |
| Lu et al51 | 2016 | Diabetic C57BL./6J mice | Custom transducer (Institute of Acoustics of Tongji University, Shanghai, China) | Biomechanical | Frequency: 1 MHz Intensity: 0.3 W/cm2 |
Increased perfusion in hindlimb ischemia model for PAD accompanied by increased angiogenic factors, antiapoptotic factors, capillary density |
| Wang et al52 | 2017 | ApoE–/– Mice | Custom transducer (Harbin Institute of Technology, Harbin, China) | Biomechanical | Frequency: 1 MHz Intensity: 0.1-0.4 W/cm2 |
Inhibition of atherosclerosis via reduction of LDL oxidation |
| Sun et al53 | 2019 | New Zealand white rabbits, ApoE–/– mice | Custom transducer (Harbin Institute of Technology, Harbin, China) | Biomechanical | Frequency: 1 MHz Intensity: 1.5 W/cm2 (rabbits), 0.8 W/cm2 (mice) |
Decrease in atherosclerosis in femoral arteries through decrease in macrophages and lipids |
| Groen et al54 | 2020 | Swine | HIFU Synthesizer, International Cardio Corporation (Edina, MN) Imasonic Dual-Mode US Array (Voray sur l’Ognon, France) |
Thermal | Frequency: 3.5 MHz, 64-element phased array transducer with fenestrations, through which 10 MHz transducer is applied Intensity: 6250 W/cm2 |
Successful targeting of dorsal wall of the external femoral artery without endothelial damage or complications, accompanied by formation of scar tissue |
| Mason et al55 | 2020 | C57BL/6 mice | EPIQ 7 (Philips Healthcare, Andover, MA) | Biomechanical | Frequency: 1.3 MHz | Increased perfusion in hindlimb ischemia model for PAD via microcavitation-dependent mechanism |
| Yao et al56 | 2020 | New Zealand white rabbits | Custom transducer (Harbin Institute of Technology, Harbin, China) | Biomechanical | Frequency: 1 MHz Intensity: 1.5 W/cm2 (rabbits) |
Decrease in carotid artery atherosclerosis through decreased neointima formation, macrophage content, proliferation SMCs, and collagen |
| Effect on thrombolysis | ||||||
| Francis et al36 | 1995 | Blood samples from adult humans | Custom apparatus made with piezoelectric transducer (manufacturer not specified) | Biomechanical | Frequency: 1 MHz Intensity: 1 W/cm2 |
Enhanced thrombolysis via increased uptake of tPA with application of ultrasound |
| Poliachik et al57 | 1999 | Blood samples from adult humans | Sonic Concepts (Sonic Concepts Inc., Bothell, WA) | Biomechanical | Frequency: 1.1 MHz Intensity: 560-2360 W/cm2 |
Cavitation and hemolysis is greater in samples with contrast agent treated with ultrasound, versus without |
| Birnbaum et al58 | 2001 | Blood samples from adult humans | Sonicator model XL 2020 (Misonix Inc., Farmingdale, NY) | Biomechanical | Frequency: 20 kHz | Ultrasound and nongas-filled particles (HAEMACCEL and HAES) decreased clot burden |
| Hölscher et al59 | 2012 | New Zealand white rabbits | ExAblate 4000 (Insightec Inc., Tirat Carmel, Israel) | Biomechanical | Frequency 220 kHz Intensity: 66-200 W (arterial thrombus model), 100-500 W (venous thrombus model) Pulse length: 100-200 ms (arterial thrombus model), 0.1-100.0 ms (venous thrombus model) |
Mild recanalization in carotid artery stroke thrombosis model, dependent on platelet-activation and cavitation |
| Wright et al60 | 2012 | New Zealand white rabbits | Custom using function generator (model AFG 3102, Tektronix, Beaverton, OR) and amplifier (model A-500, ENI, Rochester, NY) | Biomechanical | Frequency: 1.51 MHz Intensity: 300 W Pulse length: 0.1-10.0 ms |
Increased thrombolysis and partial blood flow restoration in femoral artery clot model, accompanied by cavitation |
| Damianou et al61 | 2014 | New Zealand white rabbits | Custom device with amplifier (JJ&A Instruments, Duvall, WA) and piezoelectric ceramic transducer (Piezo-technologies, Etalon, Lebanon, IN) | Biomechanical | Frequency: 1 MHz Intensity: 10-40 W/cm2 |
Enhanced thrombolysis in rabbit carotid model via increased uptake of tPA with application of ultrasound |
| Miscellaneous effects | ||||||
| Williams et al62 | 1978 | Blood samples from adult humans | Sonacell Multiphone (Rank Stanley Cox (Ware, Hertfordshire) | Biomechanical | Frequency: 0.75, 1.5., 3.0 MHz | Release of β-thromboglobulin in platelets is mediated by ultrasound-induced cavitation and release of other aggregating factors |
| Vaezy et al63 | 1999 | Swine | Sonic Concepts (Sonic Concepts Inc., Woodinville, WA) | Thermal | Frequency: 3.5 MHz Intensity: 2500-3100 W/cm2 |
Control of arterial hemorrhage |
| Zderic et al64 | 2006 | New Zealand white rabbits | Custom made 111F-U applicator with piezo-electric discs (Stavely Sensors Inc., East Hartford, CT) and a solid aluminum coupling cone | Thermal | Frequency: 3.5 MHz Intensity: 3000 ± 100 W/cm2 |
Control of arterial hemorrhage |
| Lei et al65 | 2021 | N/A | N/A (mathematical model) | Thermal | Frequency: 1.1 MHz Power: 15 W at 20 s |
Mathematical model to predict damage of plaque ablation based on wall thickness; thermal effects depend on frequency and power |
LDL, Low-density lipoprotein cholesterol; PAD, peripheral artery disease; tPA, tissue plasminogen activator.
Molecular effects of HIFU on atherosclerotic plaque
Intimal retention of lipoproteins, macrophage consumption of lipids, the formation of foam cells and subsequent cell death are critical processes in the progression of atherosclerosis. These steps center around the role of macrophages, thus, intuitively, strategies targeting macrophages can arrest progression or reverse atherosclerotic plaques. To assess the effects of therapeutic ultrasound on macrophages and atherosclerotic plaque in an atherosclerotic mouse model, Wang et al52 used ultrasound beams at a lower intensity (0.4 W/cm2) administered via a 3.5-cm probe with a 1.0-MHz resonance frequency and a duty factor of 10%. They noted that administration of sonodynamic therapy significantly decreased oxidized low-density lipoprotein cholesterol induced macrophage impairment through a heme oxygenase-1. This process resulted in the inhibition of atherosclerotic plaque progression and increased stability of the plaque.52 To further this effort, Sun et al53 evaluated the efficacy of sonodynamic therapy on atherosclerotic burden in atherosclerotic rabbit and apoE-deficient mouse models. The atherosclerotic rabbits were treated with an intensity of 1.5 W/cm2, and the mice were treated with 0.8 W/cm2. In comparison with the nontreated animals, there was a significant inhibition of atherosclerotic progression as evidenced by approximately 39% increase in fractional flow reserve and a 26% increase in the mean luminal area. Additionally, in the animals treated with sonodynamic therapy there was a decrease in macrophages and lipid content within the plaque, as well as a decrease in intraplaque hemorrhage and increase in the fibrous cap. Importantly, the authors demonstrated sonodynamic therapy induced macrophage apoptosis through a mitochondrial-caspase pathway. The effect of sonodynamic therapy on neointimal hyperplasia re-endothelialization in a rabbit femoral artery balloon denudation model was evaluated by another group.56 Their histopathological analysis revealed that sonodynamic therapy inhibited neointima formation without impacting re-endothelialization, decreased the content of macrophages, proliferating smooth muscle cells, and collagen without impacting elastin. In vitro, they noted that therapeutic ultrasound induced macrophage apoptosis and decreased interleukin-6, interleukin-1, and tumor necrosis factor alpha via the reactive oxygen species-peroxisome proliferator- activated receptor-γ-nuclear factor-κB signaling pathway. These data show that there are various mechanisms, such as altering plaque lipid content, stabilization of plaque, and induction of macrophage apoptosis, through which HIFU inhibits the progression of atherosclerotic disease.
Effects of HIFU on hindlimb ischemia models
The various potential molecular responses to therapeutic ultrasound in inhibiting pathways of atherosclerosis, promoting angiogenesis, and limb perfusion are not completely established. Lu et al51 studied the effect of ultrasound therapy in a murine hindlimb ischemia model. After surgical induction of hindlimb ischemia, skeletal muscle groups in the mice were treated with lower intensity ultrasound beams of 0.3 W/cm2, through a 2-cm transducer, with a 1.0-MHz resonance frequency for 9 minutes per day for 14 days. Based on thermal infrared imaging analysis, they noted that therapeutic ultrasound normalized lower limb blood flow in diabetic mice with hindlimb ischemia. Immunofluorescence staining showed that capillary density was augmented in these mice. Importantly, they demonstrated that therapeutic ultrasound upregulated angiogenic factors and antiapoptotic factors, while downregulating apoptotic factors. In addition, in an in vitro evaluation of human umbilical vein endothelial cells, therapeutic ultrasound inhibited apoptosis and increased angiogenic factors. Importantly, these effects were blocked by phosphoinositide 3-kinase (PI3K) or endothelial nitric oxide synthase (eNOS) inhibitors, suggesting that therapeutic ultrasound restores angiogenesis through a PI3K-Akt-eNOS pathway. In a similar study, the acoustic effects of shockwave therapy were used and compared with HIFU in an ischemic hindlimb rat model, to evaluate angiogenic effects.50 Therapeutic ultrasound was administered three times a week for 2 weeks to the ischemic limbs, at an intensity of 0.1 mJ/mm2, with a resonance frequency of 1.05 MHz through a transducer focused to 63 mm. At the 2-week mark, approximately 60% improvement was noted in the ischemic limbs, and this was comparable between the shockwave and therapeutic ultrasound groups. Additionally, they noted an increase in microvascular density with therapeutic ultrasound and shockwave therapy. Interestingly, a three-fold increase in tissue vascular endothelial growth factor was observed only in the HIFU group. These data highlight the angiogenic potential of HIFU paving the way for clinical translation in PAD.
Another pathway impacted by therapeutic ultrasound through inertial cavitation, is thought to be mediated through adenosine triphosphate-related purinergic signaling. Mason et al55 used a matrix array transducer with a mechanical index of 1.3, at 1.3 MHz, generating 5-cycle or 40-cycle sinusoidal pulses, or a power Doppler cycle comprising eight 5-cycle pulses with a PRF of 10 kHz. In addition to a variable pulse duration, they also modified the line density, producing sectors of 17, 33, or 65 lines. Lipid microbubbles were injected into 50 mice, after which the mice hindlimbs were exposed to 10 minutes of HIFU. Spatial assessments in this study demonstrated that the higher line densities produced a more rapid and larger areas of inertial cavitation. Contrast enhanced ultrasound revealed a three- to four-fold increase in limb perfusion at higher line densities, and optical imaging showed that both high line density and longer pulse durations resulted in the most adenosine triphosphate release.
Transcutaneous applications of HIFU on atherosclerotic plaque
The role of therapeutic ultrasound in targeting atherosclerotic plaques for treatment by using the thermal effects of HIFU, has also been studied. Shehata et al30 targeted swine femoral arterial atherosclerotic plaques with a DMUA system. The DMUA system included a 10-MHz diagnostic transducer and a 3.5-MHz, 64-element phased-array transducer with a focal length of 40 mm. They subjected four swine to HIFU intensities ranging between 4100 and 5600 W/cm2 for durations ranging between 250 and 2000ms. Histopathological evaluation revealed that the areas of HIFU treatment contained aggregates of lipid-laden macrophages, with condensed basophilic nuclei, suggesting coagulative necrosis. Importantly, the corresponding endothelial lining was preserved, and no arterial rupture, dissection, or perforation was noted. Of note, one animal among the four was noted to have minimal mural thrombus without disruption of the endothelium at a nontreated segment and thrombosis of normal vasa vasora of the treated segment. In contrast with other systems, the DMUA system provides the inherent ability to seamlessly transition between the diagnostic imaging system and therapeutic mode. The presence of a real-time imaging mode, known as single-transmit focus, provides the ability to monitor tissue response before, during, and after HIFU shots. In a similar preclinical study, the effects of robot assisted DMUA HIFU on healthy femoral arteries of 18 swine was studied.54 At 3 and 14 days, there was no endothelial damage, and no significant decrease in arterial diameter. Histopathological evaluation at 14 days showed accumulation of activated fibroblasts and collagen deposition, suggesting scar formation. One animal, intentionally exposed to more than 100 HIFU shots was noted to have heat-induced skin blistering corresponding with the site of application of the HIFU probe. The in vivo safety profile was evaluated in study by Rosenschein et al,35 where histologic findings demonstrated selective disruption of ultrasound-sensitive plaques and thrombi, with minimal damage to healthy arterial wall. These data highlight the importance of combined high-resolution imaging and treatment ultrasound systems such as DMUA probes, to observe and evaluate the effects of therapy in real time.
Transcutaneous application of HIFU on arterial thrombus
An additional effect of therapeutic ultrasound is potentiating thrombolysis, in conjunction with pharmacologic agents, or as a stand-alone modality. The effect of HIFU (1.51-MHz transducer, acoustic power = 300W, pulse length = 0.1-10.0 ms) was evaluated in a rabbit femoral artery thrombus in vivo model and found that 1-ms HIFU pulses resulted in partial flow restoration. Interestingly 10-ms HIFU pulses resulted in substantial bleeding from the femoral arteries.60 The thrombolytic effects of HIFU were evaluated in an in vivo model of rabbit carotid arteries by using the ExAblate 4000 system (InSightec Inc., Tirat Carmel, Israel).59 For the arterial model of thrombus, the authors used acoustic powers ranging between 66 and 200 W, at a 5% duty cycle and a pulse width of 100 to 200 ms. In contrast, the venous thrombus model was subject to acoustic powers between 100 and 500 W and a pulse width of 0.1 to 100.0 ms. In this study, only 9% recanalization was achieved. One possible explanation of this effect is platelet activation induced by HIFU. Williams et al62 showed that the lower therapeutic intensities of HIFU induced platelet activation, as evidenced by release of platelet-specific beta-thromboglobulin. In addition, they also noted increasing levels of beta-thromboglobulin with increasing intensity of HIFU. Interestingly, it has also been reported that lower frequencies (0.75-1.50 MHz) and higher intensities (3.4-4.5 W/cm2) counterbalance the thrombolytic potential, by induction of platelet-activation through inertial cavitation.59,62,66 Interestingly, when human clot was subjected in vitro to therapeutic ultrasound and nongas microparticles, there was a significantly higher percent reduction of the clot.58 In a similar in vitro model, human whole blood samples with and without microbubble contrast agents were subjected to 1.1-MHz ultrasound, at intensities ranging between 560 and 2360 W/cm2, resulting in a significant rate of hemolysis.57 The authors reported a 6- to 10-fold increase in cavitation and hemolysis with increasing quantities of microbubbles and increasing intensity of HIFU. This finding suggests a mechanical effect related to ultrasound-induced microstreaming resulting in a shear stress that augments clot disruption, related to inertial cavitation. In an in vitro model, a group of investigators studied the effect of therapeutic insonation on distribution of tissue plasminogen activator (tPA) using a 1-MHz therapeutic ultrasound at 1 W/cm2.36 They determined that the rate of tPA uptake was significantly faster when subjected to insonation. In addition, the use of radiolabeled tPA demonstrated significantly deeper penetration of tPA, upon exposure to ultrasound. Damianou et al61 evaluated the combined effect of magnetic resonance imaging-guided focused ultrasound (MRgFUS) and recombinant tPA on thrombolysis in a rabbit carotid model using a 5-cm spherical transducer, capable of focusing at 10 cm, operating at a frequency of 1 MHz and at intensities ranging from 10 to 40 W/cm2. They noted a decrease in time to carotid artery recanalization with increasing MRgFUS intensity and noted that, beyond an intensity of 20 W/cm2, there was significant heating of the focused tissue. These data suggest a clear augmentation of the pharmacologic effects of tPA in clot disruption. Conversely, HIFU has been evaluated as a tool for hemorrhage control in animal models.67 In a porcine model, Vaezy et al63 used a 3.5-MHz HIFU transducer with a focal length of 5.5 cm, diameter of 3.5 cm and intensity of 2500 to 3100 W/cm2 in femoral and carotid arteries, achieving hemostasis in 46 ± 15 seconds and 31 ± 15 seconds, respectively. Another group used a HIFU applicator of 9.6 MHz with a focal length of 2.5 cm and diameter of 1.9 cm in New Zealand White rabbits for hemostasis in femoral arteries.64 These animals were studied for 60 days after HIFU exposure. The intensity of this HIFU system was 3000 ± 100 W/cm2 requiring a mean HIFU-exposure time of 47 ± 41 seconds. These data support the safety and feasibility of acoustic technology to aid in control of hemorrhage. However, ambiguity regarding the exact HIFU settings, the ability to precisely focus the acoustic beams and the lack of data regarding the long-term molecular effects on endothelial homeostasis of this modality currently limit its use for hemorrhage control.
In total, there is robust preclinical data elucidating the various mechanisms of HIFU in atherosclerotic arterial disease. Notably, HIFU stabilizes atherosclerotic plaque and inhibits plaque progression through macrophage apoptosis potentially mediated through a reactive oxygen species-peroxisome proliferator- activated receptor-γ-nuclear factor-κB pathway. Interestingly, HIFU inhibits neointimal hyperplasia without impacting re-endothelialization. In hindlimb ischemic models, HIFU upregulates angiogenic factors and antiapoptotic factors, thus promoting angiogenesis. These effects are potentially mediated by a PI3K-Akt-eNOS pathway. In addition, the angiogenic potential is more dramatic with increasing HIFU line density. HIFU also potentiates thrombolysis, both in conjunction with pharmacologic agents and as a stand-alone modality. Based on the frequency and intensity of HIFU, thrombolytic or thrombotic effects are seen, with the latter potentiating platelet activation through inertial cavitation. However, the precise HIFU settings required to counter-balance these two effects remain unclear. Importantly, while the application of HIFU for hemorrhage control is feasible in animal models, long-term molecular effects on endothelial cell homeostasis is not clearly known.
Human clinical studies
The cardiovascular application of HIFU in humans was implemented initially in the treatment of acute stroke for augmenting thrombolysis. Based on the promising preclinical data, the applications of HIFU have also been attempted in carotid artery disease for reduction of plaque burden and in peripheral atherosclerotic disease to evaluate limb perfusion, and the degree of stenosis (Table II). The landmark Combined Lysis of Thrombus with Ultrasound and Systemic tPA for acute ischemic stroke (CLOTBUST) trial assessed the effects of sonothrombolysis, whereby patients with ischemic stroke to the middle cerebral artery were treated with transcranial ultrasound (delivered via a 2-MHz transducer) in addition to intravenous tPA (treatment group, 63 patients; control group, 63 patients).68 The mechanisms behind sonothrombolysis is presumably multifold, and include effects owing to improved drug delivery, thermal and mechanical effects, and molecular changes owing to sonography.19,35,68,69 Patients in the treatment group achieved higher rates of recanalization or dramatic clinical recovery within 2 hours compared with those in the control group (49.0% vs 30%; P < .05). Further subgroup analysis supported long-term functional outcomes at 90 days among those with severe ischemic stroke with National Institutes of Health Stroke Scale scores of 10 or more points treated with sonothrombolysis, in this cohort.70 The Combined Lysis of Thrombus with Ultrasound and Systemic tPA for Emergent Revascularization of acute ischemic stroke (CLOTBUST-ER) trial, implemented a novel operator-independent therapeutic device capable of 2 MHz ultrasound (intensity = 207 mW/cm2, pulse repetition frequency 8 × 3 kHz). This trial did not show significant clinical benefits among those treated with ultrasound (n = 317 patients) compared with those treated with standard stroke protocol (n = 329 patients) and was halted early.70, 71, 72 However, preliminary findings corroborated the safety features of sonothrombolysis found in previous CLOTBUST trials and analyses, and the study design using this novel device has since been reassessed to use vascular imaging for assessing pretreatment baseline, instead of clinical stroke severity.68,72
Table II.
Overview of clinical data of HIFU in patients with atherosclerotic occlusive arterial disease
| Author(s) | Year | Study design | Experimental cohorts | Sample size | Device name | Route of application; proposed mechanism of action | Available specs | Clinical relevance |
|---|---|---|---|---|---|---|---|---|
| Peripheral arterial occlusive disease | ||||||||
| Siegel et al73 | 1993 | Prospective single-center cohort | Arterial lesions treated with ultrasound angioplasty | 45 | Ultrasound Angioplasty Ablation System (Baxter Edwards LIS Healthcare Corporation, Bentley Laboratories, Europe BV) | Invasive; biomechanical | Frequency: 19.5kHz Intensity: 115-V electrical generator |
86% lesions recanalized with ultrasound |
| Sun et al53 | 2019 | Randomized trial | PAD patients treated with either atorvastatin and sonodynamic therapy vs atorvastatin alone | 16 (treatment = 8, control = 8) | Dedicated ultrasound device (Harbin Institute of Technology, Harbin, China) | Noninvasive; biomechanical | Frequency: 1 MHz Intensity: Individually calculated |
Atorvastatin and sonodynamic therapy decreased diameter stenosis in PAD lesions after 4 weeks |
| Mason et al55 | 2020 | Cohort study | Healthy human subjects and PAD patients treated with either ultrasound and intravenous microbubble contrast infusion vs ultrasound alone | 20 (patients with PAD = 10, healthy control = 10) | Sonos 5500 (Philips, Bothell, WA) | Noninvasive; biomechanical | Frequency: 1.3 MHz | In healthy subjects, continuous ultrasound did not affect perfusion in limbs, but ultrasound + microbubble cavitation produced a 2.5-fold increase in perfusion. In PAD patients, ultrasound and microbubble cavitation increased perfusion by 2-fold. |
| Gandini et al74 | 2016 | Randomized trial | Patients with CLTI randomized to drug-eluting balloon or paclitaxel + focused ultrasound delivered intravascularly | 56 (treatment = 28, control = 28) | CardioProlific Genesis System (CardioProlific, Hayward, CA) | Invasive; biomechanical | Frequency: 20 kHz | Treatment group had improved primary patency rates at 6 and 12 months |
| Cerebrovascular disease | ||||||||
| Alexandrov et al75 | 2002 | Case series | Stroke patients treated with transcranial ultrasound + tPA | 55 | 500M Transcranial Doppler System (Multigon, Elmsford, NY); MultiDop-T (DWL, Singel, Germany) | Noninvasive; biomechanical | Frequency: 2 MHz Intensity: 100% (Multigon); ≥128 mW (MultiDop-T) |
Complete recanalization was achieved in 36% of patients; dramatic clinical recovery achieved in 20% of patients |
| Cintas et al76 | 2002 | Observational | All patients presenting with acute MCA main stem occlusion exposed to ultrasound | 6 | ATL Ultramark 9 HDI (Philips, Amsterdam, Netherlands) | Noninvasive; biomechanical | Frequency: 2 MHz Intensity: 415 mW/cm2 |
Partial recanalization achieved in 5 of 6 patients with ultrasound |
| Alexandrov et al68 | 2004 | Randomized controlled trial | Acute ischemic stroke patients randomized to either ultrasound and tPA vs tPA alone | 126 (treatment = 66, control = 66) | PMD 100 (Spencer Technologies, Seattle, WA); EZ-Dop (DWL, Singen, Germany); Multi-Dop (DWL, Singen, Germany); Multigon 100M; Nicolet Companion III | Noninvasive; biomechanical | Frequency: 2 MHz Intensity: 750 mW (maximum) |
Ultrasound and tPA administration resulted in complete recanalization or dramatic clinical recovery from acute ischemic stroke (49% vs 30%; P = .03) |
| Rubiera et al69 | 2008 | Case series | Patients with acute MCA occlusion treated with transcranial ultrasound + tPA | 138 | TCD 100M (Spencer Technologies, Seattle, WA) | Noninvasive; biomechanical | Frequency: 2 MHz Intensity: 385 mW/cm2 |
Type of microbubbles did not affect recanalization rates, clinical improvement, bleeding, in-hospital mortality, or long-term outcome |
| Zhang et al77 | 2015 | Case series | Patients with carotid plaques assigned to ultrasound vs conventional medical treatment | 357 | Dedicated cervical orthotic device (Luoyang Kangli Medical Intstrument Co, Luoyang, China, patent ZL 2012 2 0244630.X) | Noninvasive; biomechanical | Frequency: 800 KHz Intensity: 0.75-1 W/cm2 |
Decreased thickness and area of carotid plaques (79.94% vs 18.52%) in the ultrasound group |
CLTI, Chronic limb-threatening ischemia; MCA, middle cerebral artery; PAD, peripheral arterial disease; tPA, tissue plasminogen activator.
The applications of HIFU have also expanded to treating atherosclerosis of the lower extremities. Early clinical experience with this technology has been reported in 1990s. Siegel et al73 reported results of percutaneous peripheral ultrasound angioplasty. In that study, intravascularly applied ultrasound was successful in 86% of patients and resulted in luminal stenosis reduction. In 2016, Gandini et al74 conducted Ultrasound to Enhance Paclitaxel Uptake in Critical Limb Ischemia (PACUS) randomized trial in 56 patients (28 in the control group, 28 in the study group) using the CardioProlific Genesis System (CardioProlific, Hayward, CA) to assess ultrasound energy in conjunction with paclitaxel delivery for treatment of chronic limb-threatening ischemia of femoral popliteal segment.74 The treatment group reported no adverse effects related to the procedure at all follow-up points (6 and 12 months). Angiography demonstrated a higher patency rate among the study group compared with the control group at 6 months of follow-up (96.4% vs 78.5%; P = .04) as well as 12 months of follow-up (96.2% vs 68%; P = .008). This study was followed by the ongoing Ultrasound Plasty to Improve Outcome of Percutaneous Angioplasty in Below-the-Knee Lesions (ULYSSE) trial, which has so far suggested effectiveness of high-intensity ultrasonography preceding angioplasty among patients undergoing below-the-knee angioplasty.78 Also recently, Mason et al43 demonstrated that 1.3 MHz ultrasound exposure using the Sonos 550 (Philips Ultrasound) could increase perfusion among human subjects with PAD, assessed via cavitation of perflutren lipid microbubbles, offering another mechanism by which ultrasound may be used for PAD treatment.43 In addition to lower extremity treatment, HIFU has further been shown to effectively treat carotid atherosclerosis. In a single center, prospective, nonrandomized cohort of 309 carotid plaques treated with ultrasonography using an LHZ.B-100 ultrasound therapy device (intensity = 0.75 to 1 W/cm2, frequency = 800 KHz, pulse repetition of 1 H/0.5 seconds), 247 plaques demonstrated decreases in plaque thickness and area compared with those treated with standard medical treatment over 30 days (P < .0001). In this study, the plaque area was evaluated by ultrasound only and the ultrasound technicians were blinded to the treatment groups. Despite this, the study is limited by its design and the potential for interobserver bias. Concordant with other literature, the authors suggested that these results were due to the mechanical effects of ultrasound, cavitation-induced molecular changes, and increased uptake of thrombolytics.77
In summary, the outcomes from various clinical studies have demonstrated positive outcomes with adjunctive HIFU for arterial recanalization after thrombotic stroke, decreased atherosclerotic plaque burden in carotid arteries, a decrease in diameter stenosis in patients with PAD and increase in tissue perfusion. These current studies serve as a foundation to further optimize HIFU therapy by refining settings (frequency, intensity and treatment duration) to achieve more precise focusing and target lesion effect. Better designed probes with closed-loop real-time feedback systems could optimize therapy for various applications in arterial disease. Although these data are currently limited by their small sample sizes and, single-center or nonrandomized studies and the lack of multicenter randomized trials, they are promising to warrant investigation at a larger scale.
Limitations of HIFU
Although HIFU has been successfully incorporated into clinical practice, there are several factors limiting the widespread incorporation of this technology. Importantly, artifacts inherent to use of diagnostic ultrasound technology are applicable to HIFU as well. Factors such as acoustic shadowing or reverberation by gas or bony structures contribute to inability to penetrate these tissues, particularly for intrabdominal tissue such as the aorta or the iliac arteries.21 Because these ultrasound waves would be reflected toward the HIFU transducer, there is a high likelihood of soft tissue injury or burns. Next, the exact HIFU settings required for thrombolytic versus hemorrhage control applications remain unclear. Importantly, long-term molecular effects on vessel endothelial cell homeostasis from HIFU is not clearly known. Next, the ability to adequately image, focus, target, and monitor tissues with real-time imaging is a significant limitation of currently available HIFU devices. Importantly, although there is a robust body of evidence supporting HIFU in atherosclerotic arterial disease, data supporting the use of HIFU in specific settings correlating to an outcome benefit are lacking. In current iterations, this has been circumvented by using DMUA ultrasound probes or the aid of magnetic resonance imaging (MRgFUS). The use of MRgFUS provides the added benefit of real-time temperature monitoring as well, at a higher cost and being resource intensive. In contrast, although ultrasound-guided monitoring is less resource intensive and has shorter treatment times, reliable tissue temperature monitoring is not available. Multiple efforts to develop sonographic probes capable of temperature monitoring with closed-loop feedback system are underway.79, 80, 81 Next, device size remains a limitation with the majority of FDA-approved HIFU devices. The Exablate systems (Tirat Carmel, Israel) are based on HIFU focused by magnetic resonance imaging, requiring dedicated suites to accommodate the HIFU equipment. Similarly, the Ablatherm system (EDAP TMS, Lyon, France) and the Sonablate system (SonaCare Medical, Charlotte, NC) comprise a large treatment and control module that are difficult to transport. In addition, the probe requires constant cooling with degassed water that makes it cumbersome to use for arterial application. Last, as pertaining to arterial disease, the current evidence and heterogeneity of clinical data, the ideal configurations, and settings of HIFU devices are not established. Importantly, there is a paucity of consistent methodology for assessing and grading the histologic, radiographic and clinical effects of HIFU.30 Future research is needed to consolidate device parameters, as well as outcomes.
Conclusions
HIFU is an established and exciting noninvasive therapeutic modality with a potential to revolutionize the treatment of atherosclerotic arterial disease. HIFU shows great promise in decreasing the progression of atherosclerotic plaque and stabilizing the plaque. As an adjunct to medical therapy, HIFU could be applied to various arterial beds to aid in decreasing plaque thickness and increasing vessel lumen, without the potential issues of neointimal hyperplasia plaguing current endovascular therapeutics. Future focused studies are warranted to guide the refinement of HIFU settings and provide capability to precisely focus HIFU with image guidance to safely achieve the desired biologic effect.
Author Contributions
Conception and design: AB, SMC, EA
Analysis and interpretation: AB, SMC, AD, NN, EA
Data collection: AB, SMC, EA
Writing the article: AB, SMC, EA
Critical revision of the article: AB, SMC, AD, NN, EA
Final approval of the article: AB, SMC, AD, NN, EA
Statistical analysis: Not applicable
Obtained funding: Not applicable
Overall responsibility: EA
AB and SMC contributed equally to this article and share co-first authorship.
Footnotes
Author conflict of interest: none.
The editors and reviewers of this article have no relevant financial relationships to disclose per the JVS-Vascular Science policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
References
- 1.Fowkes F.G.R., Rudan D., Rudan I., Aboyans V., Denenberg J.O., McDermott M.M., et al. Comparison of global estimates of prevalence and risk factors for peripheral artery disease in 2000 and 2010: a systematic review and analysis. Lancet. 2013;382:1329–1340. doi: 10.1016/S0140-6736(13)61249-0. [DOI] [PubMed] [Google Scholar]
- 2.Criqui M.H., Aboyans V. Epidemiology of peripheral artery disease. Circ Res. 2015;116:1509–1526. doi: 10.1161/CIRCRESAHA.116.303849. [DOI] [PubMed] [Google Scholar]
- 3.Conte M.S., Pomposelli F.B., Clair D.G., Geraghty P.J., McKinsey J.F., Mills J.L., et al. Society for Vascular Surgery practice guidelines for atherosclerotic occlusive disease of the lower extremities: Management of asymptomatic disease and claudication. J Vasc Surg. 2015;61:2S–41S.e1. doi: 10.1016/j.jvs.2014.12.009. [DOI] [PubMed] [Google Scholar]
- 4.Hirsch A.T., Hartman L., Town R.J., Virnig B.A. National health care costs of peripheral arterial disease in the Medicare population. Vasc Med. 2008;13:209–215. doi: 10.1177/1358863X08089277. [DOI] [PubMed] [Google Scholar]
- 5.Abu Dabrh A.M., Steffen M.W., Undavalli C., Asi N., Wang Z., Elamin M.B., et al. Mosby Inc.; Maryland Height, MO: 2015. The natural history of untreated severe or critical limb ischemia; pp. 1642–1651.e3. [DOI] [PubMed] [Google Scholar]
- 6.Farber A., Eberhardt R.T. American Medical Association; Chicago: 2016. The current state of critical limb ischemia: a systematic review; pp. 1070–1077. [DOI] [PubMed] [Google Scholar]
- 7.Fereydooni A., Gorecka J., Dardik A. Sage Publications Ltd; Newbury Park, CA: 2020. Using the epidemiology of critical limb ischemia to estimate the number of patients amenable to endovascular therapy; pp. 78–87. [DOI] [PubMed] [Google Scholar]
- 8.Laird J.R., Schneider P.A., Tepe G., Brodmann M., Zeller T., Metzger C., et al. Durability of treatment effect using a drug-coated balloon for femoropopliteal lesions: 24-month results of IN.PACT SFA. J Am Coll Cardiol. 2015;66:2329–2338. doi: 10.1016/j.jacc.2015.09.063. [DOI] [PubMed] [Google Scholar]
- 9.Secemsky E.A., Schermerhorn M., Carroll B.J., Kennedy K.F., Shen C., Valsdottir L.R., et al. Readmissions after revascularization procedures for peripheral arterial disease. Ann Intern Med. 2018;168:93. doi: 10.7326/M17-1058. [DOI] [PubMed] [Google Scholar]
- 10.Ochoa Chaar C.I., Gholitabar N., Goodney P., Dardik A., Abougergi M.S., editors. One-year readmission after open and endovascular revascularization for critical limb ischemia. Elsevier Inc; New York: 2019. [DOI] [PubMed] [Google Scholar]
- 11.Ochoa Chaar C.I., Gholitabar N., DeTrani M., Jorshery S.D., Zhuo H., Zhang Y., et al. The reintervention index: a new outcome measure for comparative effectiveness of lower extremity revascularization. Ann Vasc Surg. 2020;69:52–61. doi: 10.1016/j.avsg.2020.05.040. [DOI] [PubMed] [Google Scholar]
- 12.Goodney P.P., Holman K., Henke P.K., Travis L.L., Dimick J.B., Stukel T.A., et al., editors. Regional intensity of vascular care and lower extremity amputation rates. Mosby Inc; Maryland Height, MO: 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dick F., Diehm N., Galimanis A., Husmann M., Schmidli J., Baumgartner I. Surgical or endovascular revascularization in patients with critical limb ischemia: influence of diabetes mellitus on clinical outcome. J Vasc Surg. 2007;45:751–761. doi: 10.1016/j.jvs.2006.12.022. [DOI] [PubMed] [Google Scholar]
- 14.DeRubertis B.G., Pierce M., Chaer R.A., Rhee S.J., Benjeloun R., Ryer E.J., et al. Lesion severity and treatment complexity are associated with outcome after percutaneous infra-inguinal intervention. J Vasc Surg. 2007;46:709–716. doi: 10.1016/j.jvs.2007.05.059. [DOI] [PubMed] [Google Scholar]
- 15.Kim T.I., Schneider P.A. Sage Publications Inc.; Newbury Park, CA: 2020. New Innovations and devices in the management of chronic limb-threatening ischemia; pp. 524–539. [DOI] [PubMed] [Google Scholar]
- 16.Lynn J.G., Zwemer R.L., Chick A.J., Miller A.E. A new method for the generation and use of focused ultrasound in experimental biology. J Gen Physiol. 1942;26:179–193. doi: 10.1085/jgp.26.2.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fry W.J., Fry F.J. Fundamental neurological research and human neurosurgery using intense ultrasound. IRE Transact Med Electron. 1960;ME-7:166–181. doi: 10.1109/iret-me.1960.5008041. [DOI] [PubMed] [Google Scholar]
- 18.Fry W.J., Barnard J.W., Fry F.J., Brennan J.F. Ultrasonically produced localized selective lesions in the central nervous system. Am J Phys Med. 1955;34:413–423. [PubMed] [Google Scholar]
- 19.Nazer B., Gerstenfeld E.P., Hata A., Crum L.A., Matula T.J. Kluwer Academic Publishers; Dordrecth, the Netherlands: 2014. Cardiovascular applications of therapeutic ultrasound; pp. 287–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hynynen K.H. In: MRI-Guided Focused Ultrasound Surgery. Hynynen K.H., Jolesz F.A., editors. CRC Press; Boca Raton, FL: 2007. Fundamental principles of therapeutic ultrasound; pp. 16–35. [Google Scholar]
- 21.Elhelf I.A.S., Albahar H., Shah U., Oto A., Cressman E., Almekkawy M. Elsevier Masson SAS; Paris: 2018. High intensity focused ultrasound: the fundamentals, clinical applications and research trends; pp. 349–359. [DOI] [PubMed] [Google Scholar]
- 22.Duc N.M., Keserci B. Emerging clinical applications of high-intensity focused ultrasound. Diagn Interv Radiol. 2019;25:398–409. doi: 10.5152/dir.2019.18556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Duc N.M., Keserci B. Review of influential clinical factors in reducing the risk of unsuccessful MRI-guided HIFU treatment outcome of uterine fibroids. Diagn Interv Radiol. 2018;24:283–291. doi: 10.5152/dir.2018.18111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Blana A., Walter B., Rogenhofer S., Wieland W.F. High-intensity focused ultrasound for the treatment of localized prostate cancer: 5-year experience. Urology. 2004;63:297–300. doi: 10.1016/j.urology.2003.09.020. [DOI] [PubMed] [Google Scholar]
- 25.Shehata I.A. Treatment with high intensity focused ultrasound: secrets revealed. Eur J Radiol. 2012;81:534–541. doi: 10.1016/j.ejrad.2011.01.047. [DOI] [PubMed] [Google Scholar]
- 26.Chen H., Kreider W., Brayman A.A., Bailey M.R., Matula T.J. Blood vessel deformations on microsecond time scales by ultrasonic cavitation. Phys Rev Lett. 2011;106:034301. doi: 10.1103/PhysRevLett.106.034301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chen H., Brayman A.A., Kreider W., Bailey M.R., Matula T.J. Observations of translation and jetting of ultrasound-activated microbubbles in mesenteric microvessels. Ultrasound Med Biol. 2011;37:2139–2148. doi: 10.1016/j.ultrasmedbio.2011.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wu J. Shear stress in cells generated by ultrasound. Prog Biophys Mol Biol. 2007;93:363–373. doi: 10.1016/j.pbiomolbio.2006.07.016. [DOI] [PubMed] [Google Scholar]
- 29.Miller D.L., Smith N.B., Bailey M.R., Czarnota G.J., Hynynen K., Makin I.R.S. John Wiley and Sons Ltd; New York: 2012. Overview of therapeutic ultrasound applications and safety considerations; pp. 623–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shehata I.A., Ballard J.R., Casper A.J., Liu D., Mitchell T., Ebbini E.S. Feasibility of targeting atherosclerotic plaques by high-intensity-focused ultrasound: an in vivo study. J Vasc Interv Radiol. 2013;24:1880–1887.e2. doi: 10.1016/j.jvir.2013.08.013. [DOI] [PubMed] [Google Scholar]
- 31.Casper A.J., Liu D., Ballard J.R., Ebbini E.S. Real-time implementation of a dual-mode ultrasound array system: in vivo results. IEEE Trans Biomed Eng. 2013;60:2751–2759. doi: 10.1109/TBME.2013.2264484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Theraclion FDA approves the 1st trial with Theraclion's vein therapy in the US. 2021. www.theraclion.com/wp-content/uploads/2021/09/ENG-SEPT-2021_PR_US_SONOVEIN_Final.pdf Available at:
- 33.Steffen W., Fishbein M.C., Luo H., Lee D.Y., Nita H., Cumberland D.C., et al. High intensity, low frequency catheter-delivered ultrasound dissolution of occlusive coronary artery thrombi: an in vitro and in vivo study. J Am Coll Cardiol. 1994;24:1571–1579. doi: 10.1016/0735-1097(94)90157-0. [DOI] [PubMed] [Google Scholar]
- 34.Steffen W., Cumberland D., Gaines P., Luo H., Nita H., Maurer G., et al. Catheter-delivered high intensity, low frequency ultrasound induces vasodilation in vivo. Eur Heart J. 1994;15:369–376. doi: 10.1093/oxfordjournals.eurheartj.a060505. [DOI] [PubMed] [Google Scholar]
- 35.Rosenschein U., Bernstein J.J., DiSegni E., Kaplinsky E., Bernheim J., Rozenzsajn L.A. Experimental ultrasonic angioplasty: disruption of atherosclerotic plaques and thrombi in vitro and arterial recanalization in vivo. J Am Coll Cardiol. 1990;15:711–717. doi: 10.1016/0735-1097(90)90651-5. [DOI] [PubMed] [Google Scholar]
- 36.Francis C.W., Blinc A., Lee S., Cox C. Ultrasound accelerates transport of recombinant tissue plasminogen activator into clots. Ultrasound Med Biol. 1995;21:419–424. doi: 10.1016/0301-5629(94)00119-x. [DOI] [PubMed] [Google Scholar]
- 37.Piazza G., Hohlfelder B., Jaff M.R., Ouriel K., Engelhardt T.C., Sterling K.M., et al. A prospective, single-arm, multicenter trial of ultrasound-facilitated, catheter-directed, low-dose fibrinolysis for acute massive and submassive pulmonary embolism: the SEATTLE II Study. JACC Cardiovasc Interv. 2015;8:1382–1392. doi: 10.1016/j.jcin.2015.04.020. [DOI] [PubMed] [Google Scholar]
- 38.Kucher N., Boekstegers P., Muller O.J., Kupatt C., Beyer-Westendorf J., Heitzer T., et al. Randomized, controlled trial of ultrasound-assisted catheter-directed thrombolysis for acute intermediate-risk pulmonary embolism. Circulation. 2014;129:479–486. doi: 10.1161/CIRCULATIONAHA.113.005544. [DOI] [PubMed] [Google Scholar]
- 39.Raabe R.D. Ultrasound-accelerated thrombolysis in arterial and venous peripheral occlusions: fibrinogen level effects. J Vasc Interv Radiol. 2010;21:1165–1172. doi: 10.1016/j.jvir.2010.03.020. [DOI] [PubMed] [Google Scholar]
- 40.Kim Y.S., Rhim H., Choi M.J., Lim H.K., Choi D. High-intensity focused ultrasound therapy: an overview for radiologists. Korean J Radiol. 2008;9:291–302. doi: 10.3348/kjr.2008.9.4.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Brodmann M., Werner M., Holden A., Tepe G., Scheinert D., Schwindt A., et al. Primary outcomes and mechanism of action of intravascular lithotripsy in calcified, femoropopliteal lesions: results of Disrupt PAD II. Catheter Cardiovasc Interv. 2019;93:335–342. doi: 10.1002/ccd.27943. [DOI] [PubMed] [Google Scholar]
- 42.Brodmann M., Werner M., Brinton T.J., Illindala U., Lansky A., Jaff M.R., et al. Safety and performance of lithoplasty for treatment of calcified peripheral artery lesions. J Am Coll Cardiol. 2017;70:908–910. doi: 10.1016/j.jacc.2017.06.022. [DOI] [PubMed] [Google Scholar]
- 43.Adams G., Shammas N., Mangalmurti S., Bernardo N.L., Miller W.E., Soukas P.A., et al. Intravascular lithotripsy for treatment of calcified lower extremity arterial stenosis: initial analysis of the Disrupt PAD III Study. J Endovasc Ther. 2020;27:473–480. doi: 10.1177/1526602820914598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Raza A., Harwood A., Totty J., Smith G., Chetter I. Extracorporeal shockwave therapy for peripheral arterial disease: a review of the potential mechanisms of action. Ann Vasc Surg. 2017;45:294–298. doi: 10.1016/j.avsg.2017.06.133. [DOI] [PubMed] [Google Scholar]
- 45.Holfeld J., Tepekoylu C., Blunder S., Lobenwein D., Kirchmair E., Dietl M., et al. Low energy shock wave therapy induces angiogenesis in acute hind-limb ischemia via VEGF receptor 2 phosphorylation. PLoS One. 2014;9:e103982. doi: 10.1371/journal.pone.0103982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tepekoylu C., Wang F.S., Kozaryn R., Albrecht-Schgoer K., Theurl M., Schaden W., et al. Shock wave treatment induces angiogenesis and mobilizes endogenous CD31/CD34-positive endothelial cells in a hindlimb ischemia model: implications for angiogenesis and vasculogenesis. J Thorac Cardiovasc Surg. 2013;146:971–978. doi: 10.1016/j.jtcvs.2013.01.017. [DOI] [PubMed] [Google Scholar]
- 47.Tara S., Miyamoto M., Takagi G., Kirinoki-Ichikawa S., Tezuka A., Hada T., et al. Low-energy extracorporeal shock wave therapy improves microcirculation blood flow of ischemic limbs in patients with peripheral arterial disease: pilot study. J Nippon Med Sch. 2014;81:19–27. doi: 10.1272/jnms.81.19. [DOI] [PubMed] [Google Scholar]
- 48.Serizawa F., Ito K., Kawamura K., Tsuchida K., Hamada Y., Zukeran T., et al. Extracorporeal shock wave therapy improves the walking ability of patients with peripheral artery disease and intermittent claudication. Circ J. 2012;76:1486–1493. doi: 10.1253/circj.cj-11-1216. [DOI] [PubMed] [Google Scholar]
- 49.Ciccone M.M., Notarnicola A., Scicchitano P., Sassara M., Carbonara S., Maiorano M., et al. Shockwave therapy in patients with peripheral artery disease. Adv Ther. 2012;29:698–707. doi: 10.1007/s12325-012-0038-4. [DOI] [PubMed] [Google Scholar]
- 50.Nazer B., Ghahghaie F., Kashima R., Khokhlova T., Perez C., Crum L., et al. Therapeutic ultrasound promotes reperfusion and angiogenesis in a rat model of peripheral arterial disease. Circ J. 2015;79:2043–2049. doi: 10.1253/circj.CJ-15-0366. [DOI] [PubMed] [Google Scholar]
- 51.Lu Z.-Y., Li R.-L., Zhou H.-S., Huang J.-J., Su Z.-X., Qi J., et al. Therapeutic ultrasound reverses peripheral ischemia in type 2 diabetic mice through PI3K-Akt-eNOS pathway. Am J Transl Res. 2016;8:3666–3677. [PMC free article] [PubMed] [Google Scholar]
- 52.Wang Y., Wang W., Xu H., Sun Y., Sun J., Jiang Y., et al. Non-lethal sonodynamic therapy inhibits atherosclerotic plaque progression in ApoE-/- mice and attenuates ox-LDL-mediated macrophage impairment by inducing heme oxygenase-1. Cell Phys Biochem. 2017;41:2432–2446. doi: 10.1159/000475913. [DOI] [PubMed] [Google Scholar]
- 53.Sun X., Guo S., Yao J., Wang H., Peng C., Li B., et al. Rapid inhibition of atherosclerotic plaque progression by sonodynamic therapy. Cardiovasc Res. 2019;115:190–203. doi: 10.1093/cvr/cvy139. [DOI] [PubMed] [Google Scholar]
- 54.Groen M.H.A., Slieker F.J.B., Vink A., de Borst G.J., Simons M.V., Ebbini E.S., et al. Safety and feasibility of arterial wall targeting with robot-assisted high intensity focused ultrasound: a preclinical study. Int J Hyperthermia. 2020;37:903–912. doi: 10.1080/02656736.2020.1795278. [DOI] [PubMed] [Google Scholar]
- 55.Mason N.R., Davidson B.P., Sheeran P., Muller M., Hodovan J.M., Sutton J., et al. Augmentation of tissue perfusion in patients with peripheral artery disease using microbubble cavitation. JACC Cardiovasc Imaging. 2020;13:641–651. doi: 10.1016/j.jcmg.2019.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Yao J., Zhao X., Tan F., Cao X., Guo S., Li X., et al. Early modulation of macrophage ROS-PPARγ-NF-κB signalling by sonodynamic therapy attenuates neointimal hyperplasia in rabbits. Sci Rep. 2020;10:11638. doi: 10.1038/s41598-020-68543-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Poliachik S.L., Chandler W.L., Mourad P.D., Bailey M.R., Bloch S., Cleveland R.O., et al. Effect of high-intensity focused ultrasound on whole blood with and without microbubble contrast agent. Ultrasound Med Biol. 1999;25:991–998. doi: 10.1016/s0301-5629(99)00043-5. [DOI] [PubMed] [Google Scholar]
- 58.Birnbaum Y. Augmentation of ultrasound-induced clot disruption by nongas-filled microparticles. Echocardiography. 2001;18:265–268. doi: 10.1046/j.1540-8175.2001.00265.x. [DOI] [PubMed] [Google Scholar]
- 59.Hölscher T., Fisher D.J., Ahadi G., Voie A. Introduction of a rabbit carotid artery model for sonothrombolysis research. Transl Stroke Res. 2012;3:397–407. doi: 10.1007/s12975-012-0194-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wright C., Hynynen K., Goertz D. In vitro and in vivo high-intensity focused ultrasound thrombolysis. Invest Radiol. 2012;47:217–225. doi: 10.1097/RLI.0b013e31823cc75c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Damianou C., Hadjisavvas V., Mylonas N., Couppis A., Ioannides K. MRI-guided sonothrombolysis of rabbit carotid artery. J Stroke Cerebrovasc Dis. 2014;23:e113–e121. doi: 10.1016/j.jstrokecerebrovasdis.2013.09.005. [DOI] [PubMed] [Google Scholar]
- 62.Williams A.R., Chater B.V., Allen K.A., Sherwood M.R., Sanderson J.H. Release of β-thromboglobulin from human platelets by therapeutic intensities of ultrasound. Br J Haematol. 1978;40:133–142. doi: 10.1111/j.1365-2141.1978.tb03647.x. [DOI] [PubMed] [Google Scholar]
- 63.Vaezy S., Martin R., Kaczkowski P., Keilman G., Goldman B., Yaziji H., et al. Use of high-intensity focused ultrasound to control bleeding. J Vasc Surg. 1999;29:533–542. doi: 10.1016/s0741-5214(99)70282-x. [DOI] [PubMed] [Google Scholar]
- 64.Zderic V., Keshavarzi A., Noble M.L., Paun M., Sharar S.R., Crum L.A., et al. Hemorrhage control in arteries using high-intensity focused ultrasound: a survival study. Ultrasonics. 2006;44:46–53. doi: 10.1016/j.ultras.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 65.Lei W., Hu J., Liu Y., Liu W., Chen X. Numerical evaluation of high-intensity focused ultrasound- induced thermal lesions in atherosclerotic plaques. Math Biosci Eng. 2021;18:1154–1168. doi: 10.3934/mbe.2021062. [DOI] [PubMed] [Google Scholar]
- 66.Chater B.V., Williams A.R. Platelet aggregation induced in vitro by therapeutic ultrasound. Thrombos Haemostas. 1977;38:640–651. [PubMed] [Google Scholar]
- 67.Zderic V., Brayman A.A., Sharar S.R., Crum L.A., Vaezy S. Microbubble-enhanced hemorrhage control using high intensity focused ultrasound. Ultrasonics. 2006;45:113–120. doi: 10.1016/j.ultras.2006.07.018. [DOI] [PubMed] [Google Scholar]
- 68.Alexandrov A.V., Molina C.A., Grotta J.C., Garami Z., Ford S.R., Alvarez-Sabin J., et al. Ultrasound-enhanced systemic thrombolysis for acute ischemic stroke. N Engl J Med. 2004;351:2170–2178. doi: 10.1056/NEJMoa041175. [DOI] [PubMed] [Google Scholar]
- 69.Rubiera M., Ribo M., Delgado-Mederos R., Santamarina E., Maisterra O., Delgado P., et al. Do bubble characteristics affect recanalization in stroke patients treated with microbubble-enhanced sonothrombolysis? Ultrasound Med Biol. 2008;34:1573–1577. doi: 10.1016/j.ultrasmedbio.2008.02.011. [DOI] [PubMed] [Google Scholar]
- 70.Barlinn K., Tsivgoulis G., Barreto A.D., Alleman J., Molina C.A., Mikulik R., et al. Outcomes following sonothrombolysis in severe acute ischemic stroke: subgroup analysis of the CLOTBUST trial. Int J Stroke. 2014;9:1006–1010. doi: 10.1111/ijs.12340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Barreto A.D., Alexandrov A.V., Shen L., Sisson A., Bursaw A.W., Sahota P., et al. Clotbust-hands free: pilot safety study of a novel operator-independent ultrasound device in patients with acute ischemic stroke. Stroke. 2013;44:3376–3381. doi: 10.1161/STROKEAHA.113.002713. [DOI] [PubMed] [Google Scholar]
- 72.Alexandrov A.V., Köhrmann M., Soinne L., Tsivgoulis G., Barreto A.D., Demchuk A.M., et al. Safety and efficacy of sonothrombolysis for acute ischaemic stroke: a multicentre, double-blind, phase 3, randomised controlled trial. Lancet Neurol. 2019;18:338–347. doi: 10.1016/S1474-4422(19)30026-2. [DOI] [PubMed] [Google Scholar]
- 73.Siegel R.J., Gaines P., Crew J.R., Cumberland D.C. Clinical trial of percutaneous peripheral ultrasound angioplasty. J Am Coll Cardiol. 1993;22:480–488. doi: 10.1016/0735-1097(93)90053-4. [DOI] [PubMed] [Google Scholar]
- 74.Gandini R., Del Giudice C. Local ultrasound to enhance paclitaxel delivery after femoral-popliteal treatment in critical limb ischemia: the PACUS Trial. JACC Cardiovasc Interv. 2016;9:2147–2153. doi: 10.1016/j.jcin.2016.07.019. [DOI] [PubMed] [Google Scholar]
- 75.Alexandrov A.V., Grotta J.C. Arterial reocclusion in stroke patients treated with intravenous tissue plasminogen activator. Neurology. 2002;59:862–867. doi: 10.1212/wnl.59.6.862. [DOI] [PubMed] [Google Scholar]
- 76.Cintas P., Le Traon A.P., Larrue V. High rate of recanalization of middle cerebral artery occlusion during 2-MHz transcranial color-coded Doppler continuous monitoring without thrombolytic drug. Stroke. 2002;33:626–628. doi: 10.1161/hs0202.103073. [DOI] [PubMed] [Google Scholar]
- 77.Zhang Y., Dong H., Xu Y., Shi R., Gu J., Lang H., et al. External ultrasound for carotid atherosclerotic plaque treatment. J Ultrasound Med. 2015;34:451–459. doi: 10.7863/ultra.34.3.451. [DOI] [PubMed] [Google Scholar]
- 78.Del Giudice C., Gandini R. CRT-200.04 Ultrasound plasty to improve outcome of percutaneous angioplasty in below-the-knee lesions: 24 months results of the ULYSSE Registry. JACC Cardiovasc Interv. 2020;13:S30. [Google Scholar]
- 79.Park S., Pham N.T., Huynh H.T., Kang H.W. Development of temperature controller-integrated portable HIFU driver for thermal coagulation. Biomed Eng Online. 2019;18:77. doi: 10.1186/s12938-019-0697-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Arora D., Cooley D., Perry T., Skliar M., Roemer R.B. Direct thermal dose control of constrained focused ultrasound treatments: phantom and in vivo evaluation. Phys Med Biol. 2005;50:1919–1935. doi: 10.1088/0031-9155/50/8/019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Qian Z.W., Xiong L., Yu J., Shao D., Zhu H., Wu X. Noninvasive thermometer for HIFU and its scaling. Ultrasonics. 2006;44(Suppl 1):e31–e35. doi: 10.1016/j.ultras.2006.06.036. [DOI] [PubMed] [Google Scholar]