Abstract
To assess the impact of the COVID-19 pandemic on the training of rheumatology trainees. We conducted an observational cross-sectional study using an online survey-based questionnaire sent to rheumatology trainees in India. Rheumatology trainees from India, including DM/DNB residents and fellows, were included. A total of 78 trainees from 24 institutes in 12 states participated in the study. An overwhelming majority of residents (84%) felt COVID-19 Pandemic Negatively impacted their residency and their Physical (65%), Mental (74%) and Social well-being (80%); 79% of trainees felt burnt out. Majority of trainees felt the pandemic negatively impacted their training with clinical teaching (91%), Clinical examination skills (74%), current (80%) and future (70%) research opportunities suffering during the pandemic. Most had significant reduction in the overall footfall (72%) of patients in rheumatology including OPD (77%) and indoor (67%) admissions along with academics (35%), procedures (66%) and exposure to musculoskeletal ultrasound (71%). Almost 60% and 40% of trainees had OPDs, and indoor admissions stopped during COVID-19 pandemic of these 20% had OPDs, and Admissions closed for more than 6 months. 85% of participants had one or the other psychological symptoms with almost half experiencing anxiety (44%), low mood (47%) or lack of sleep (41%). We found The COVID-19 Pandemic has significantly affected the physical, social and mental well-being of Rheumatology trainees. Academic and clinical training reduced, current and future Research became difficult, disruptions in OPDs and Admissions, recurrent COVID postings and reduction in patient footfall, procedures and MSK-US have been detrimental to trainees.
Keywords: COVID-19, Rheumatology Training, Education, Anxiety, Teleconsultation
Introduction
The COVID-19 (coronavirus disease 2019) pandemic has proven to be relentlessly challenging, leading to an unprecedented public health crisis impacting healthcare systems, healthcare workers, and communities substantively. The situation has been starker in developing countries with understaffed and overburdened healthcare. COVID-19 has been the great disrupter of our times, with almost all aspects of healthcare being severely affected, from medical education to clinical practice and research. The sudden transition from conventional in-person teaching to virtual training was not smooth, a number of social, economic, cultural, and mental factors interfered with full utilization and acclimatization of the virtual education platform initially. Stress from the multiple covid duties, self-isolations, and quarantines further added to the woes of trainees. A study revealed significantly higher rates of stress and burnout in COVID-19 exposed physician trainees compared to non-exposed trainees [1]. The stress was specially higher in female and unmarried trainees [2]. Planned interventions were severely disrupted in the pandemic, impacting intervention-based branches dearly.
COVID 19 Global Rheumatology Alliance trainee survey of 302 rheumatology trainees across different institutes depicted that sudden and unexpected changes in health services during the COVID-19 pandemic had significantly impacted the clinical training, research opportunities and health and well-being of rheumatology trainees [3]. The current study aims to gauge the magnitude of the effect the pandemic had on Rheumatology training (including the impact on clinical, academic and research activity) in India, their physical, mental and social wellbeing during the pandemic and the perceived changes in Rheumatology training and care during the pandemic from the trainee’s view.
Methods
Survey design and dissemination
Using an online survey platform (Google form), we conducted an observational cross-sectional study across India. A questionnaire was designed and distributed to all the current trainees and fellows pursuing their course (DM, DNB and Fellowship) in rheumatology. Candidates who had cleared their final examination before 2020 were excluded from the study population. The listed authors designed the questionnaire collaboratively regarding the impact of COVID-19 on rheumatology trainees in India. The survey questionnaire incorporated questions on impact on rheumatology training and research, patient care and trainee wellness. In addition, seven questions were asked to evaluate telemedicine status, vaccination coverage and covid exposure history among trainees. The questionnaire was generated by a web-based platform (Google Form) and distributed to all the participants a link on social media platforms (e.g., WhatsApp, Telegram and Email) after proper consent and the responses were received over 6 months.
Eligibility criteria
Participant selection was made on adult and paediatric rheumatology trainees from different institutes in India. Those included had not completed their rheumatology training before 2021, were older than 18, and consented to participate in the survey. This survey was conducted by pure voluntary engagement of the participants and did not include personal identifiers, protected health information or incentives. Convenience sampling was used, so the sample size was not calculated.
Ethical statement
The protocol was cleared by the Institutional Ethics Committee of King George’s Medical University protocol no. VI-PGTSC-IIA/P48 dated 27.10.2021.
Respondents were required to verify their consent before they began the survey to understand the nature and value of the questions.
Data collection and statistical analysis
All respondents were included in the analysis. Data were represented as absolute numbers and percentages. The questionnaire contains 5-point Likert scales, multiple-choice questions, and some leading questions. Leading inquiries were replied to in ‘yes/no’ format, and if ‘yes’, they must specify their answer. 5-point Likert scale was based on whether it has a positive and negative impact, in terms of agreeing and disagreeing to that question. In addition, the extent of each component is specified (i.e., Agree and strongly agree). A neutral response was kept for the no impact component of the Likert scale.
Data are presented using descriptive statistics and processed using SPSSv23. Descriptive statistics were performed by calculating measures of central tendency for quantitative variables and using counts and percentages for qualitative and nominal variables.
Results
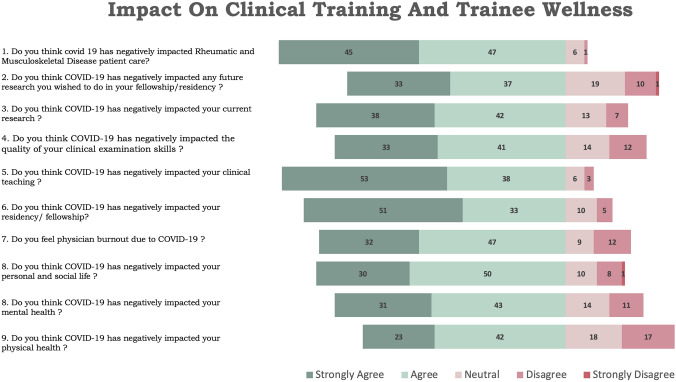
Seventy-eight trainees from 24 institutes in 12 states participated in the study. The mean age of the participants was 31, with 70% of trainees being male and 30% females. 56 (70%) participants were DM students, 15 (19%) were DNB students, five fellowship students and 2 Non-academic Senior Residents. An overwhelming majority of residents (84%) felt COVID-19 Pandemic negatively impacted their residency and their physical (65%), mental (74%) and social well-being (80%). 79% of trainees felt burnt out due to the pandemic. The majority of trainees felt the pandemic negatively impacted their training, with the majority of trainees feeling their clinical teaching(91%), clinical examination skills (74%), current(80%) and future(70%) research opportunities suffered during the pandemic (Fig. 1).
Fig. 1.
Impact on clinical training and trainee wellness are assessed by this questionnaire format. A five-point Likert scale response of trainees for each of the questions are represented as a horizontal bar diagram. Each bar represents color coded segment for different responses such as strongly agree (dark green), agree (light green), neutral (light brown), disagree (brown) and strongly disagree (red). Percentage of trainee’s response are expressed in numbers in each segment. Majority of them are responded in favor of the negative effect of COVID in their personal as well as professional life
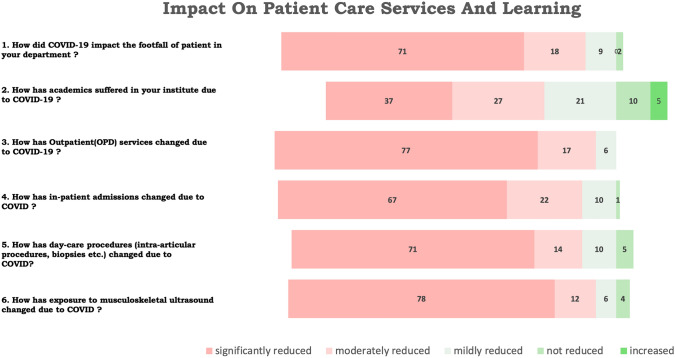
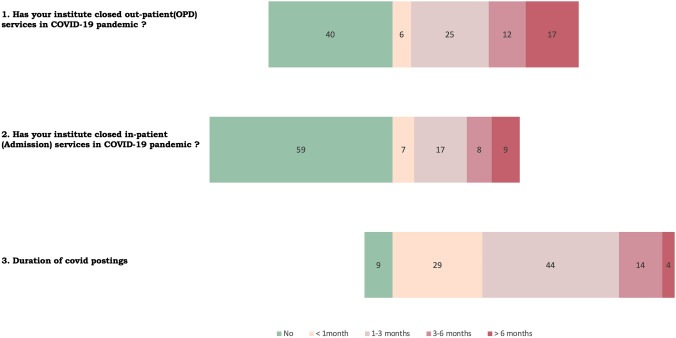
Most residents reported reduction of both indoor admission and out-patient department (OPD) registrations (99%) with majority claiming a significant reduction (Reduction to less than half of pre-COVID levels) (72%). Similar overall and significant reduction in patients attending OPD (100% & 77%) and indoor admissions (99% & 67%) was reported. Trainees also reported an overall and significant reduction in academics (85% & 35%), procedures and interventions including biopsies and intra-articular injections (97% & 66%) and exposure to musculoskeletal ultrasound (96% & 71%) (Fig. 2). Almost 60% and 40% of trainees had their OPDs and indoor admissions stopped during the COVID-19 pandemic. Of these, 20% had their OPDs and Admissions closed for more than 6 months (Fig. 3).
Fig. 2.
Patient care services and learning during COVID times are represented in a horizontal bar diagram with a five-point Likert scale response. Questions regarding IPD, OPD, access to health care, MSK ultrasound, Daycare procedure and academic strength are expressed in separate row with different color-coded bars. Each bar contains percentage of response in each color-coded segment such as strongly reduced (pink), moderately reduced (light pink), mildly reduced (light green), not reduced (green) and increased (dark green). Most of them agreed that COVID pandemic has restricted learning opportunity and patient care services. Significantly reduced (reduced less than half of pre-COVID), moderately reduced (reduced by 25–50%) mildly reduced (reduced by no more the 25%) not reduced
Fig. 3.
Duration of restricted access to health care services in institutes are observed with varying grades. Restriction to OPD as well as IPD services and deployment of trainees in COVID postings are depicted as a horizontal bar diagram with different color labels. Durations are mentioned as No restriction/duty (green), < 1 months (light pink), 1–3 months (light brown), 3–6 months (light red) and > 6 months (red)
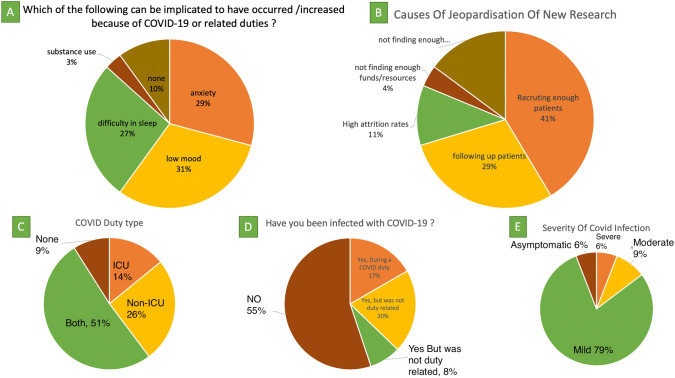
85% of the participants had one or the other psychological symptoms, with almost half experiencing anxiety (44%), low mood (47%) or lack of sleep (41%); 85% were concerned about their family members being infected, and 40% had lost a close relative to COVID. 91% of the trainee were posted in COVID duties, 2/3rd of them in ICUs, 50% being posted for 1–3 months and 20% more than 3 months, a quarter of trainees got infected during their duties (COVID and Non-COVID), and though most had asymptomatic to mild COVID, 15% still had moderate to severe COVID (Fig. 4).
Fig. 4.
Pie charts are made from separate multiple choice question responses to understand the attitude of trainees towards different aspects of training. A Pie chart represents personal difficulties created by COVID related duties; B different causes for retraction of new research; C type of COVID posting; D exposure to COVID infection; and E severity of COVID infection across trainees
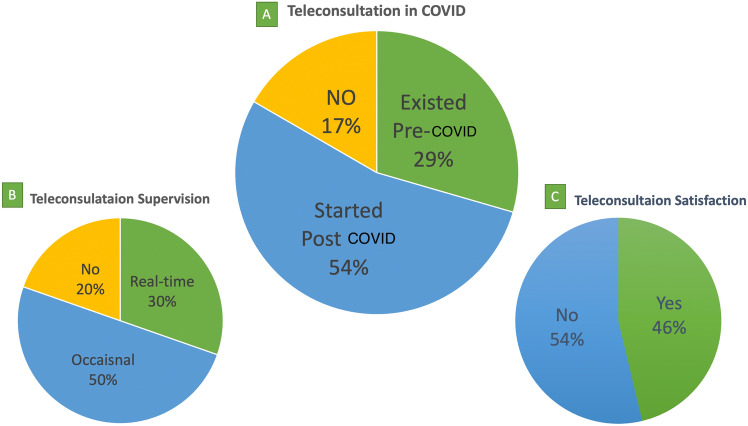
Teleconsultation was started by the institutes majorly in post COVID-19 era (54%). The teleconsultation platform existed as a model of patient follow-up in 29% of institutes before the COVID outbreak, but a significant proportion (15%) was unable to provide teleconsultation services in the COVID era also. The majority of teleconsultations (80%) were supervised by senior faculty members according to case-to-case basis, whether partial(50%) or full (30%) engagement was necessary (Fig. 5). Opinions regarding satisfaction with teleconsultation services were mixed, with 54% not truly satisfied.
Fig. 5.
Telehealth services during COVID as a part of healthcare delivery are expressed in separate pie charts. A Teleconsultation status in pre and post COVID era; B supervision status of teleconsultation by senior faculty members; and C trainee satisfaction regarding teleconsultation services
Discussion
The study of 78 rheumatology trainees across India showed a substantial impact of COVID 19 on rheumatological training and trainees’ wellbeing. Different domains of rheumatology training were affected with a significant effect on patient care.
Impact on clinical training and patient care
Most trainees agreed that the COVID-19 pandemic had negatively impacted their rheumatology training. Though the recommendation and guidelines for rheumatology training vary across countries but most countries advocate appropriate patient exposure, ample research opportunities and adequate laboratory experience, MSK ultrasound and necessary interventions are essential for a good training experience [4, 5]. Different studies in other specialities across the globe reported a higher number of redeployment to a non-specialist role with an increase in working hours and often without proper personal protective measures [6, 7]. A paediatric gastroenterology residents survey [8], reported a significant reduction in clinical training (52%), research projects(46%), and procedural confidence (41%), which was similar to what we have observed in our study. Many rheumatology trainees were reassigned to new roles with mandatory COVID duty during their tenure. A survey conducted by allergy & immunology trainees in USA found that 12% of fellows in training were reassigned to COVID-19 duty, and a majority of them were concerned about the clinical experience they would gain during the fellowship [9]. In our study, most trainees were posted for 1–3 months in COVID duty in between specialists’ duty; however, a few had to work in covid up to 6 months, accounting for almost 20% of their total training duration. Outpatient and inpatient services were transiently hampered due to significant disruption in patient care services [7]. New research opportunities and ongoing research projects were affected in terms of acquisition of funds, reduction in sample size, and ability of physician to continue research after a significant increase in working hours [10–12].
Impact on trainee wellness
In our survey, most of the Rheumatology trainee agreed that the COVID pandemic had negatively impacted their general well-being. A global trainee survey of 1420 trainees noted that a strong predictor of physician burnout was related to more exposure to COVID-19 patients and having a COVID-positive colleague triggers emotional concern and stress [13]. Trainees in Saudi Arabia during the COVID pandemic reported low mood and anxiety [14]. Decreased clinical experience, reduced case volume, disrupted education activities and deteriorated mental health are significant concerns in the Trainee survey [15]. Though long-term effects of negative psychological impacts are not mentioned but physicians' burnout generates depression, suicidal ideation, substance abuse, relationship difficulties, decreased productivity, work dissatisfaction, medical errors and suboptimal patient care [16]. A global Rheumatology trainee survey showed that physician stress (> 75%) and burnouts (> 50%) were quite common among trainees [3]. Studies from the subcontinent echoed similar concerns [17] (Table 1).
Table 1.
Impact of COVID 19 on Medical students and trainees in Asia
| Study | Country | Study population | Parameter | Tools | Impact |
|---|---|---|---|---|---|
| Chang et al. [22] | South Korea |
Orthopaedic residents (n = 221) |
Impact of COVID on Resident education | 58- question Web based survey |
Identified concern regarding significant increase in duty hours with reduction of operation room time Education time such as lecturers and clinical rotation was significantly decreased at the cost of online mode of learning 47.6% of orthopaedic residents experienced isolation or quarantine in their tenure and significant stressful event was observed due to family/ parental health priority Sharp decrease in average quality of life score was observed in pandemic |
| Mishra et al. [23] | India |
Ophthalmologists (n = 716) |
Impact on ophthalmological training | Online survey questionnaire |
80.7% of the trainees felt that the COVID-19 lockdown had negatively impacted their surgical training and 54.8% of the trainees perceived an increase in stress levels during the COVID-19 lockdown 24.6% were deployed in COVID screening duties Most of them found online learning platform as useful |
| Nguyen et al. [24] | Vietnam |
Medical students (n = 5423) |
Fear of COVID 19 | Fear of COVID-19 scale (FCoV-19 scale) |
Factors protective from fear—better health literacy, older age, later academic years, male gender and better financial status Students with higher FCoV-19 fear scores were more likely to engage in unhealthy lifestyle measures, such as smoking and drinking alcohol |
| Compton et al. [25] | Singapore |
Medical students (n = 179) |
Return to clinical setting in COVID pandemic | 3-domain conceptual frame work |
One-third of the students did not want to return to the clinical setting Those preferring return have higher internal motivation, greater sense of professional responsibility, and a lower self-perception of harbouring risk to patients |
| Khanna et al. [26] | India |
Practicing Ophthalmologists and ophthalmology trainee (n = 2355) |
Impact on training or professional Work Depression |
Symptoms of depression using PHQ-9 validated scale |
Majority of the population (52.8%) felt that their training or professional would be seriously affected by COVID-19 and 37% had difficulties meeting financial commitments 32.6% were depressed and 4.3% had severe depression requiring therapy. Depression was observed more at younger age and those non practicing |
| Li et al. [27] | China |
Health professional students (Medical, nursing, medical technology) (n = 1442) |
Psychological distress in COVID pandemic |
Psychological distress using the Kessler 6-item Psychological Distress Scale (K6) and acute stress reaction using the Impact of Event Scale-Revised (IES-R) |
Clinically significant psychological distress was observed in 26.63% of students Those with difficult childhood, stressful life event in last year and internet addiction were at greater risk, but good and functional family was protective |
| Liu et al. [28] | China |
Medical students in Wuhan (n = 217) |
Mental health status | Patient Health Questionnaire-9 (PHQ-9) and Generalized Anxiety Disorder-7 (GAD-7) scale |
35.5% of students were depressed and 22.1% were anxious Most affected students had mild to moderate symptoms |
| Abbasi et al. [29] | Pakistan |
Medical and Dentistry students (n = 382) |
Attitudes and perceptions surrounding e-learning |
Self-administered Questionnaire |
Most students had negative perceptions about e-learning and prefer face-to-face learning mode 77% students have negative perceptions towards e-learning and most of them uses mobile device for the same Administration and faculty members should take necessary measures for improving e-learning platform |
| Foong et al. [30] | Singapore | Orthopaedic residents | Challenges and adaptations in training during pandemic COVID-19: | Review of component and competencies | Significant decline in elective surgery and hand on procedures, such as arthroscopy |
| Sethi et al. [31] | Pakistan |
Healthcare professionals (n = 270) |
Impacts of the shutdown on daily lives and health |
Open-ended qualitative questionnaire | Few concerns were raised, such as work-life balance, mental health impacts, academic delays and subsequent financial impact, lack of proper PPE amidst COVID pandemic |
| Ikhlaq et al. [32] | Pakistan |
Medical, dental, nursing and allied health students (n = 384) |
Awareness and attitudes | Questionnaire format |
Majority had satisfactory level of awareness regarding pandemic, but in-depth knowledge was lacking Variation of awareness between medical, dental, and nursing students were noted Most students showed positive attitudes, but a substantial proportion had fears for transmission to family members |
| Lin et al. [33] | China |
Medical students (n = 2086) |
Impacts of mass and social media on psychobehavioural responses to the COVID-19 pandemic |
Health Belief Model | Both mass and social media catered a major role in disseminating health messages and contribute to the betterment of psychobehavioral responses to COVID-19 among medical students |
Telehealth
The concept of telemedicine has evolved at an unprecedented pace over the last few years with the advent of the pandemic. This concept was implemented in several institutes across globe during lockdown to maintain the platform for remote patient interaction [18–21]. Teleconsultation is technology-intensive, and its use has been limited by lack of access in the developing world. As echoed in our survey findings, lack of training regarding telehealth protocols, and difficulty in a comprehensive assessment of patient status are current limitations.
Virtual education
Virtual conferences and multiple virtual educational resources were a boon to the trainees during the pandemic, virtual education allow easy access across regional and national boundaries and are less intimidating to students compared to their in-person counterparts although with lesser interaction and attention [34]. International collaborations such as the Global Rheumatology Alliance has shown how the pandemic bought us together as a community during times of adversity to fight an unknown enemy.
The way forward
The pandemic has helped streamline online education and conferences, we need to understand the lacunae/deficiencies and improve upon them to make the virtual learning process more immersive. Institutions need to devise/improve virtual examination and teleconsultation protocols to ensure future pandemics have a ready mechanism with minimal disruptions in patient care [34]. International Grand Rounds, greater collaborations and Virtual mentors would further help in improving trainee education and understanding.
Limitations
The Questionnaire was not independently validated though it was based on the Global Rheumatology alliance questionnaire with country and context-specific modifications.
We tried to include all the trainees in India but could manage 75% of those who were under training in the survey period. We did not ask questions on the effect of digital education and virtual conferences and no questions on cross-speciality interactions were asked.
Conclusions
The COVID-19 Pandemic has completely altered the status quo for rheumatology trainees and has affected their physical, social and mental wellbeing. Academic and clinical training has been significantly hampered, and conducting current, and future research has become difficult. Significant disruptions in OPDs, IPDs, daycare procedures and musculoskeletal ultrasound have adversely impacted training and patient care. Recurrent exhaustive COVID postings and redeployment increased burnout and psychosocial stress on trainees. New adaptation in patient care services such as telemedicine was welcomed, but the satisfaction with teleconsultation is low, and a lot needs to be done for proper acclimatisation with the system.
Acknowledgements
The Submitted article was accepted to be published as an abstract: AB1501 Effect of SARS-COV-19 Pandemic on Rheumatology Training in India at EULAR 2022 with a https://doi.org/10.1136/annrheumdis-2022-eular.325.
Author contribution
Conceptualisation: KC. Data curation: all authors. Formal analysis: KC; funding acquisition: N/A. Investigation: KC, KK, PD, JD, DE, SM. Methodology: KC; visualisation: KC, UD. Writing—original draft: SM, KC. Writing, review and editing—all authors.
Funding
No specific funding was received from any bodies in the public, commercial or not-for-profit sectors to carry out the work described in this article.
Data availability
Data are available upon reasonable request by any qualified researchers who engage in rigorous, independent scientific research, and will be provided following review and approval of a research proposal and Statistical Analysis Plan (SAP) and execution of a Data Sharing Agreement (DSA). All data relevant to the study are included in the article.
Declarations
Conflict of interest
All authors disclose that they do not have any direct or indirect interests (dual commitments), financial or otherwise, that might affect or be perceived to affect the conduct or reporting of the work they have submitted.
Ethical approval
The protocol was cleared by the Institutional Ethics Committee of King George’s Medical University protocol no. VI-PGTSC-IIA/P48 dated 27.10.2021.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Enujioke SC, McBrayer K, Soe KC, Imburgia TM, Robbins C. Impact of COVID-19 on post graduate medical education and training. BMC Med Educ. 2021;21(1):580. doi: 10.1186/s12909-021-03019-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kannampallil TG, Goss CW, Evanoff BA, Strickland JR, McAlister RP, Duncan J. Exposure to COVID-19 patients increases physician trainee stress and burnout. PLoS ONE. 2020;15(8):e0237301. doi: 10.1371/journal.pone.0237301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Young K, Yeoh SA, Putman M, Sattui S, Conway R, Graef E, et al. The impact of COVID-19 on rheumatology training—results from the COVID-19 Global Rheumatology Alliance trainee survey. Rheumatol Adv Pract. 2022;6(1):rkac001. doi: 10.1093/rap/rkac001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Core-Curriculum-Outline.pdf [Internet]. [cited 22 May 2022]. Available from: https://www.rheumatology.org/Portals/0/Files/Core-Curriculum-Outline.pdf
- 5.Woolf AD. Training Rheumatologists in Europe.19. [DOI] [PubMed]
- 6.Hope C, Reilly JJ, Griffiths G, Lund J, Humes D. The impact of COVID-19 on surgical training: a systematic review. Tech Coloproctology. 2021;25(5):505–520. doi: 10.1007/s10151-020-02404-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.An TW, Henry JK, Igboechi O, Wang P, Yerrapragada A, Lin CA, et al. How are orthopaedic surgery residencies responding to the COVID-19 pandemic? An assessment of resident experiences in cities of major virus outbreak. J Am Acad Orthop Surg. 2020 doi: 10.5435/JAAOS-D-20-00397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Irastorza LE, Hopson P, Ta A, Kemme S, Mallon D, Lee CK. The impact of COVID-19 on job prospects and educational training for pediatric gastroenterology fellows. J Pediatr Gastroenterol Nutr. 2021;72:514–519. doi: 10.1097/MPG.0000000000003037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kahwash BM, Deshpande DR, Guo C, Panganiban CM, Wangberg H, Craig TJ. Allergy/immunology trainee experiences during the COVID-19 pandemic: AAAAI work group report of the fellows-in-training committee. J Allergy Clin Immunol Pract. 2021;9(1):1–6.e1. doi: 10.1016/j.jaip.2020.09.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.The Impact of the COVID-19 Pandemic on the Extramural Scientific Workforce—outcomes from an NIH-Led Survey—NIH Extramural Nexus [Internet]. [cited 25 May 2022]. Available from: https://nexus.od.nih.gov/all/2021/03/25/the-impact-of-the-covid-19-pandemic-on-the-extramural-scientific-workforce-outcomes-from-an-nih-led-survey/
- 11.Squazzoni F, Bravo G, Grimaldo F, Garcıa-Costa D, Farjam M, Mehmani B. Only Second-Class Tickets for Women in the COVID-19 Race. A Study on Manuscript Submissions and Reviews in 2329 Elsevier Journals [Internet]. Rochester, NY: Social Science Research Network; 2020 Oct [cited 25 May 2022]. Report No.: 3712813. Available from: https://papers.ssrn.com/abstract=3712813
- 12.Breuning M, Fattore C, Ramos J, Scalera J. Gender, parenting, and scholarly productivity during the global pandemic. 2020 Jul 21 [cited 2022 May 25]; Available from: https://preprints.apsanet.org/engage/apsa/article-details/5f16fc5660b4ad001212f977
- 13.Cravero AL, Kim NJ, Feld LD, Berry K, Rabiee A, Bazarbashi N, et al. Impact of exposure to patients with COVID-19 on residents and fellows: an international survey of 1420 trainees. Postgrad Med J. 2021;97(1153):706–715. doi: 10.1136/postgradmedj-2020-138789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen SY, Lo HY, Hung SK. What is the impact of the COVID-19 pandemic on residency training: a systematic review and analysis. BMC Med Educ. 2021;15(21):618. doi: 10.1186/s12909-021-03041-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cubitt LJ, Im YR, Scott CJ, Jeynes LC, Molyneux PD. Beyond PPE: a mixed qualitative–quantitative study capturing the wider issues affecting doctors’ well-being during the COVID-19 pandemic. BMJ Open. 2021;11(3):e050223. doi: 10.1136/bmjopen-2021-050223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.De Hert S. Burnout in healthcare workers: prevalence, impact and preventative strategies. Local Reg Anesth. 2020;28(13):171–183. doi: 10.2147/LRA.S240564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sharma D, Bhaskar S. Addressing the Covid-19 Burden on Medical Education and Training: The Role of Telemedicine and Tele-Education During and Beyond the Pandemic. Front Public Health [Internet]. 2020 [cited 23 May 2022];8. Available from: https://www.frontiersin.org/article/10.3389/fpubh.2020.589669 [DOI] [PMC free article] [PubMed]
- 18.Jethwa H, Abraham S. Training the trainees: COVID-19 and rheumatologists of the future. Clin Med. 2021;21(1):e94–e95. doi: 10.7861/clinmed.2020-0907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhang Y, Wang J, Zhao L, Xiao J, Shi Z. Online management of rheumatoid arthritis during COVID-19 pandemic. Ann Rheum Dis. 2021;80:e4–e4. doi: 10.1136/annrheumdis-2020-217548. [DOI] [PubMed] [Google Scholar]
- 20.López-Medina C, Escudero A, Collantes-Estevez E. COVID-19 pandemic: an opportunity to assess the utility of telemedicine in patients with rheumatic diseases. Ann Rheum Dis. 2020;80:e50. doi: 10.1136/annrheumdis-2020-218008. [DOI] [PubMed] [Google Scholar]
- 21.Kirby T. Rheumatologists rapidly adjust patient care during COVID-19 pandemic. Lancet Rheumatol. 2020;2(5):e258. doi: 10.1016/S2665-9913(20)30094-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chang DG, Park JB, Baek GH, Kim HJ, Bosco A, Hey HWD, et al. The impact of COVID-19 pandemic on orthopaedic resident education: a nationwide survey study in South Korea. Int Orthop. 2020;10:1–8. doi: 10.1007/s00264-020-04714-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mishra D, Nair AG, Gandhi RA, Gogate PJ, Mathur S, Bhushan P, et al. The impact of COVID-19 related lockdown on ophthalmology training programs in India—outcomes of a survey. Indian J Ophthalmol. 2020;68(6):999–1004. doi: 10.4103/ijo.IJO_1067_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nguyen HT, Do BN, Pham KM, Kim GB, Dam HTB, Nguyen TT, et al. Fear of COVID-19 scale—associations of its scores with health literacy and health-related behaviors among medical students. Int J Environ Res Public Health. 2020;17(11):4164. doi: 10.3390/ijerph17114164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Compton S, Sarraf-Yazdi S, Rustandy F, Kumar Radha Krishna L. Medical students’ preference for returning to the clinical setting during the COVID-19 pandemic. Med Educ. 2020 doi: 10.1111/medu.14268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Khanna RC, Honavar SG, Metla AL, Bhattacharya A, Maulik PK. Psychological impact of COVID-19 on ophthalmologists-in-training and practising ophthalmologists in India. Indian J Ophthalmol. 2020;68(6):994–998. doi: 10.4103/ijo.IJO_1458_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li Y, Wang Y, Jiang J, Valdimarsdóttir UA et al (2021) Psychological distress among health professional students during the COVID-19 outbreak. Psychol Med. 51(11):1952–1954. 10.1017/S0033291720001555 [DOI] [PMC free article] [PubMed]
- 28.Liu J, Zhu Q, Fan W, Makamure J, Zheng C, Wang J. Online mental health survey in a Medical College in China During the COVID-19 Outbreak. Front Psychiatry [Internet]. 2020 [cited 23 May 2022];11. Available from: https://www.frontiersin.org/article/10.3389/fpsyt.2020.00459 [DOI] [PMC free article] [PubMed]
- 29.Abbasi S, Ayoob T, Malik A, Memon SI. Perceptions of students regarding E-learning during Covid-19 at a private medical college. Pak J Med Sci. 2020;36(COVID19-S4):S57–61. doi: 10.12669/pjms.36.COVID19-S4.2766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Foong WS, Teo HLT, Wang DHB, Loh SYJ. Challenges and adaptations in training during pandemic COVID-19: observations by an orthopedic resident in Singapore. Acta Orthop. 2020;91(5):562–566. doi: 10.1080/17453674.2020.1786641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sethi BA, Sethi A, Ali S, Aamir HS. Impact of coronavirus disease (COVID-19) pandemic on health professionals. Pak J Med Sci. 2020;36(COVID19-S4):S6–11. doi: 10.12669/pjms.36.COVID19-S4.2779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ikhlaq A, Bint-E-Riaz H, Bashir I, Ijaz F. Awareness and attitude of undergraduate medical students towards 2019-novel corona virus. Pak J Med Sci. 2020;36(COVID19-S4):S32–S36. doi: 10.12669/pjms.36.COVID19-S4.2636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lin Y, Hu Z, Alias H, Wong LP. Influence of mass and social media on psychobehavioral responses among medical students during the downward trend of COVID-19 in Fujian, China: cross-sectional study. J Med Internet Res. 2020;22(7):e19982. doi: 10.2196/19982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chandwar K, Dixit J, Kishor K, Ekbote D, Dogga P. COVID-19 anniversary—the hits, the misses, and the way forward: a resident’s view. Indian J Rheumatol. 2021;16(4):481–482. doi: 10.4103/injr.injr_97_21. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available upon reasonable request by any qualified researchers who engage in rigorous, independent scientific research, and will be provided following review and approval of a research proposal and Statistical Analysis Plan (SAP) and execution of a Data Sharing Agreement (DSA). All data relevant to the study are included in the article.