Abstract
Background: Dysphagia and cognitive decline are frequently found in stroke patients. Dysphagia can reduce the patients’ quality of life and increase hospital stays and the risk of death.
Aim: To investigate the correlation between cognitive function and dysphagia in stroke patients.
Methods: A total of 37 stroke patients with oropharyngeal dysphagia participated in this cross-sectional study. Mini-Mental State Examination (MMSE) was used to assess their cognitive levels. In addition, the swallowing function of patients was assessed using the Mann Assessment Swallowing Ability (MASA).
Results: Most of patients (62.2%) were male, and the mean ± standard deviation of patients’ age was 62± 8. The results showed that 35.1% of patients had impaired cognitive function, and 56.8 % had severe dysphagia. Moreover, there was a fair positive correlation between MMSE and MASA with a correlation coefficient equal to 0.373 (P = 0.023), indicating that the severity of dysphagia increases with increasing cognitive decline.
Conclusion: Our findings suggest that cognitive function may have a role in the severity of dysphagia in stroke patients.
Keywords: Deglutition disorders, Cognition decline, Neglect, Swallowing, Decline, Nutrition.
Résumé
Contexte : La dysphagie et le déclin cognitif sont fréquemment observés chez les patients victimes d'un accident vasculaire cérébral (AVC). La dysphagie peut réduire la qualité de vie des patients et augmenter les séjours hospitaliers et le risque de décès.
Objectif : Étudier la corrélation entre la fonction cognitive et la dysphagie chez les patients victimes d'un AVC.
Méthodes : Au total, 37 patients victimes d'un AVC avec dysphagie oropharyngée ont participé à cette étude transversale. Le mini-examen de l'état mental (MEEM) a été utilisé pour évaluer leurs niveaux cognitifs. De plus, la fonction de déglutition des patients a été évaluée à l’aide du test d’évaluation de la capacité de déglutition (TECD).
Résultats : La plupart des patients à l'étude (62,2 %) des patients à l'étude étaient des hommes et la moyenne ± écart-type de l'âge des patients était de 62± 8. Les résultats ont montré que 35,1% des patients avaient une fonction cognitive altérée et 56,8% avaient une dysphagie sévère. De plus, il y avait un une équitable corrélation positive entre MEEM et TECD avec un coefficient de corrélation égal à 0,373 (P = 0,023), indiquant que la sévérité de la dysphagie augmente avec l'augmentation du déclin cognitif.
Conclusion : la fonction cognitive peut avoir un rôle dans la sévérité de la dysphagie chez les patients victimes d'AVC.
Mot clés: troubles de la déglutition, déclin cognitif, négligence, deglutition, déclin, La nutrition.
Introduction
Nutrition is an essential function carried out unconsciously for the acquisition of essential nutrients for the correct functioning of an organism (1, 2 ). Nutrition begins with the processing of food in the mouth, which includes chewing, bolus creation, and swallowing, and then continues with the bolus being carried to the digestive tract where digestion and subsequent absorption of the various nutrients take place (1, 3 ). As a result, swallowing is a critical step in meeting the body's requirements (1 ). Because the digestive tract runs parallel to the respiratory one, swallowing must be carried out in a synchronized way to prevent food from entering the airway (4 ).
Dysphagia is frequently found in stroke patients. The prevalence of dysphagia in stroke patients is around 50%-70% (5 ). Fortunately, most of these patients recover normal swallowing function within seven days (6 ). However, 11%-13% remain dysphagic even after six months (6, 7 ). A study reported that 80% of stroke patients with prolonged dysphagia required enteral feeding (8 ). Post-stroke dysphagia is a frequent cause of morbidity, including aspiration pneumonia, dehydration, and malnutrition (9 ). It might also lead to prolonged hospitalization and a higher mortality rate (10 ). Additionally, previous research showed that stroke increases the risk of future dementia. The population that experiences a stroke has double the risk of developing dementia at a later stage (11, 12 ). Moreover, a decline in cognitive function can impact the cognition or intake of food during swallowing (13 ). The correlation between cognitive function and dysphagia has received more attention (14 ). A study of Japanese elderly people requiring long-term care showed a negative relationship between dementia severity and swallowing function, indicating that when the dementia severity increased, swallowing ability decreased (15 ). Another cross-sectional study reported that elderly residents in nursing homes with lower cognitive function tended to have higher odds of dysphagia risk (16 ).
Although previous studies showed that cognitive dysfunction impacts on the swallowing ability, the association between the severity of cognitive impairment and the severity of dysphagia in stroke patients is still unclear. Therefore, there is a need to investigate the correlation between cognitive deficit and dysphagia in stroke patients.
This study has three main purposes (1 ) to determine the level of cognitive function in stroke patients, (2 ) to determine the severity of dysphagia in stroke patients, (3 ) to investigate the correlation between the severity of cognitive dysfunction and the severity of dysphagia in stroke patients.
Methods
Study design and patients
This study was approved by the Research Ethics Committee of the Jordanian Ministry of Health, Amman, Jordan. Before any examination, the objective of this study was explained to the patients and they completed the informed consent form.
The design of this study was a cross-sectional study. Stroke patients with dysphagia were recruited from outpatient clinics of Al Basheer and Prince Hamza hospitals and Outpatient rehabilitation facilities of Amman city. This study was conducted between December 13, 2022 and April 11, 2022. Inclusion criteria include a medical diagnosis of stroke and oropharyngeal dysphagia, patients having no history of other neurological diseases affecting their swallowing function (e.g. Multiple sclerosis), and the ability to speak in Arabic. The exclusion criteria were oral language difficulties that made it impossible to conduct the cognitive function test, severe cognitive decline (Mini-Mental State Examination (MMSE) ≤9), and severe aphasia (severe communication difficulties that affect the patient's ability to speak and understand language) obstructing thorough assessment of cognitive function.
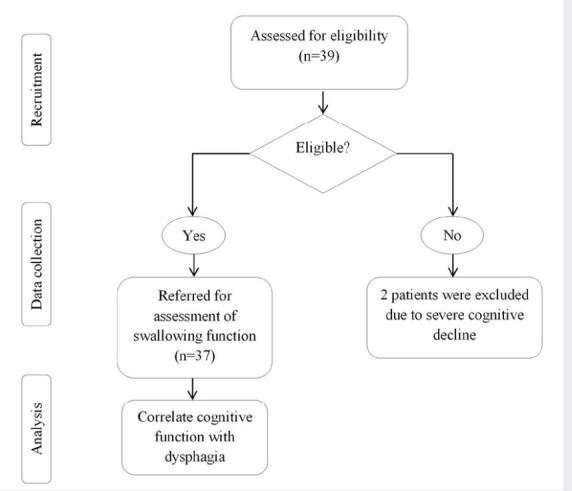
The patient’s cognitive function was evaluated using the MMSE (17 ). After diagnosing the cognitive function in patients, swallowing function was evaluated using the Mann Assessment of Swallowing Ability(MASA)(18 ). Figure one illustrates the study protocol.
Figure 1 . figure 1. study protocol.
Instruments
Mini-Mental State Examination
The MMSE is one of the most commonly used screening tools for cognitive function. It includes 6 subtests: orientation, registration, attention, recall, language, and constructional praxis. The total score is considered out of 30 with a cut-off point of 24 (≥ 24, intact cognitive function and <24, cognitive dysfunction). It is easy to use and requires up to 5-10 minutes (19 ). In this study, we used the validated Arabic version of the MMSE (17 ).
Mann Assessment of Swallowing Ability
The MASA was developed to evaluate dysphagia in stroke patients. This test consisted of 24 items. The total scores yielded from this test are 200, with a cut-off point of 177. Normal swallowing is defined as a score of 178 or higher, while mild dysphagia is defined as a score of 168–177, moderate dysphagia as a score of 139–167, and severe dysphagia by a score less than 138 (18 ).
Because Arabic is the primary language in Jordan, we conducted face validity to MASA. First, it was translated into Arabic by three independent bilingual (in Arabic and English) experts. Then, the expert panel identified and corrected any inadequate concepts or expressions of the translation. After that, the Arabic version was translated back into English by three independent bilingual (in Arabic and English) experts. Finally, a number of researchers in the field reviewed it.
Statistical analysis
Data entry and analysis were conducted using the SPSS software ver. 28. Numerical variables were expressed as mean and standard deviation. For categorical variables, the frequency and its percentage were reported. The correlation between cognitive function and the severity of dysphagia was evaluated by the r.The Pearson r was considered “high” when it was >0.70, “good” when it was between 0.50 and 0.70, “fair” if it was between 0.30 and 0.50, and “weak or no association” if it was <0.30 (20 ).
Results
Patients’ characteristics
A total of 37 stroke patients with dysphagia were included in this cross-sectional study. The mean ± standard deviation of the disease duration was 7.86 ± 4.61 weeks. Most of the patients (64.9%) had intact cognitive function. Moreover, more than half patients (56.8%) had severe dysphagia (Table 1 ).
Table 1. Table 1. Demographic and clinical characteristics of patients.
|
Characteristics |
Frequency (%) |
Mean (SD) |
|
Age |
61.57 (8.1) |
|
|
Sex |
||
|
Male |
23 (62.2) |
|
|
Female |
14 (37.8) |
|
|
Time post-onset of stroke, wk |
7.86 (4.61) |
|
|
MMSE Scores |
||
|
24-30 |
24 (64.9) |
|
|
<24 |
13 (35.1) |
|
|
Dysphagia Severity |
||
|
Mild |
3 (8.1) |
|
|
Moderate |
13 (35.1) |
|
|
Severe |
21 (56.8) |
n = 37
SD: Standard deviation
MMSE: Mini-Mental State Examination
Bivariate Analysis
There was a fair positive correlation between the severity of cognitive decline and the severity of dysphagia (r = 0.373 and P = 0.023).
Discussion
The results of this study showed that the majority of patients (64.9%) had intact cognitive function, and 56.8% had severe dysphagia. Moreover, there was a fair positive correlation between MMSE and MASA (r = 0.373 and P = 0.023), indicating that the severity of dysphagia increases with increasing cognitive decline, confirming the hypothesis of our study.
Findings showed that 35.1% of patients had cognitive decline following a stroke. Moreover, results found that 56.1 % had severe dysphagia, 35.1% had moderate dysphagia, and 8.1% had mild dysphagia. Therefore, assessing cognitive and swallowing function after a stroke may be essential.
Our findings were in line with a number of studies that investigated the correlation between dysphagia and cognitive decline in patients with stroke and other neurological disorders. An earlier study, for instance, showed that hemispatial neglect was associated with dysphagia and yielded increased nonoral feeding in stroke patients (21 ). Moreover, a study in Parkinson's disease patients showed that there are significant correlations between learning/memory or frontal/executive domains and the oral phase of swallowing, while the pharyngeal phase of swallowing showed weak associations with frontal functions (22 ). In Alzheimer's disease, the severity of dysphagia has also been thought to be correlated with the severity of cognitive decline (23 ). That is, if cortical involvement and cognitive impairment progress, dysphagia worsens in Alzheimer's disease (23, 24 ). Furthermore, executive functions and dysphagia showed a significant correlation in amyotrophic lateral sclerosis patients (25 ). Although these studies were conducted on patients with other neurological disorders, they are in line with this study’s findings.
Limitation of the study
This study did not address the correlations between different components of the cognitive function evaluated by comprehensive neuropsychological tests with the swallowing function after a stroke.
In conclusion, our findings suggest that cognitive function might contribute to dysphagia severity in stroke patients. Thus, detection and treatment for the coexisting cognitive decline may be helpful for efficient dysphagia therapy and successful rehabilitation.
Acknowledgements
The author would like to thank all of the study participants for their participation.
References
- Pérez-Cruz E, González-Muñoz A, Barrientos-Jiménez M. Assessment of dysphagia in neurological disease patients and its relation to risk factor for malnutrition. Med Interna Méx. 2018;34(3):359–365. [Google Scholar]
- Chen Y, Michalak M, Agellon L B. Importance of nutrients and nutrient metabolism on human health. Yale J Biol Med. 2018;91(2):95–103. [PMC free article] [PubMed] [Google Scholar]
- Bornhorst Gail M, Singh R Paul. Comprehensive Reviews in Food Science and Food Safety. 2. Vol. 11. Wiley; 2012. Bolus Formation and Disintegration during Digestion of Food Carbohydrates; pp. 101–118. [Google Scholar]
- Matsuo Koichiro, Palmer Jeffrey B. Japanese Dental Science Review. 1. Vol. 45. Elsevier BV; 2009. Coordination of mastication, swallowing and breathing; pp. 31–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon C, Hewer R L, Wade D T. BMJ. 6595. Vol. 295. BMJ; 1987. Dysphagia in acute stroke. pp. 411–414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smithard D G, O'neill P A, England R E. The natural history of dysphagia following a stroke. Dysphagia. 1997;12(4):188–193. doi: 10.1007/PL00009535. [DOI] [PubMed] [Google Scholar]
- Mann G, Hankey G J, Cameron D. Swallowing function after stroke: prognosis and prognostic factors at 6 months. Stroke. 1999;30(4):744–748. doi: 10.1161/01.str.30.4.744. [DOI] [PubMed] [Google Scholar]
- Broadley S, Croser D, Cottrell J, Creevy M, Teo E, Yiu D, Pathi R, Taylor J, Thompson P D. Journal of Clinical Neuroscience. 3. Vol. 10. Elsevier BV; 2003. Predictors of prolonged dysphagia following acute stroke; pp. 300–305. [DOI] [PubMed] [Google Scholar]
- Schindler A, Ginocchio D, Ruoppolo G. What we don't know about dysphagia complications? Rev Laryngol Otol Rhinol (Bord) 2008;129(2):75–78. [PubMed] [Google Scholar]
- Gonagalez-Fernadez M, Ottensteinet Lauren, Levan. Dysphagia after stroke: an overview. Curr Phys Med Rehabil Rep. 2013;1(3):187–196. doi: 10.1007/s40141-013-0017-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnold Marcel, Liesirova Kai, Broeg-Morvay Anne, Meisterernst Julia, Schlager Markus, Mono Marie-Luise, El-Koussy Marwan, Kägi Georg, Jung Simon, Sarikaya Hakan. PLOS ONE. 2. Vol. 11. Public Library of Science (PLoS); 2016. Dysphagia in Acute Stroke: Incidence, Burden and Impact on Clinical Outcome; pp. e0148424–e0148424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen Vu Q C, Prvubettger Janet, Guerrier Tami, Hirsch Mark A, Thomas J George, Pugh Terrence M, Rhoads Charles F. Archives of Physical Medicine and Rehabilitation. 7. Vol. 96. Elsevier BV; 2015. Factors Associated With Discharge to Home Versus Discharge to Institutional Care After Inpatient Stroke Rehabilitation; pp. 1297–1303. [DOI] [PubMed] [Google Scholar]
- Malandraki Georgia A, Sutton Bradley P, Perlman Adrienne L, Karampinos Dimitrios C, Conway Charles. Human Brain Mapping. 10. Vol. 30. Wiley; 2009. Neural activation of swallowing and swallowing-related tasks in healthy young adults: An attempt to separate the components of deglutition; pp. 3209–3226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jo Soo Yung, Hwang Jeong-Won W, Pyun Sung-Bom B. Annals of Rehabilitation Medicine. 4. Vol. 41. Korean Academy of Rehabilitation Medicine; 2017. Relationship Between Cognitive Function and Dysphagia After Stroke; pp. 564–564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakai K, Hirano H, Watanabe Y, Tohara H, Sato E, Sato K, Katakura A. Journal of Oral Rehabilitation. 2. Vol. 43. Wiley; 2006. An examination of factors related to aspiration and silent aspiration in older adults requiring long-term care in rural Japan; pp. 103–110. [DOI] [PubMed] [Google Scholar]
- Yatabe Naoko, Takeuchi Kenji, Izumi Maya, Furuta Michiko, Takeshita Toru, Shibata Yukie, Suma Shino, Kageyama Shinya, Ganaha Seijun, Tohara Haruka, Yamashita Yoshihisa. Gerodontology. 4. Vol. 35. Wiley; 2018. Decreased cognitive function is associated with dysphagia risk in nursing home older residents; pp. 376–381. [DOI] [PubMed] [Google Scholar]
- El-Hayeck Rita, Baddoura Rafic, Wehbé Amine, Bassil Nazem, Koussa Salam, Abou Khaled Karine, Richa Sami, Khoury Rita, Alameddine Abbas, Sellal François. Journal of Alzheimer's Disease. 2. Vol. 71. IOS Press; 2019. An Arabic Version of the Mini-Mental State Examination for the Lebanese Population: Reliability, Validity, and Normative Data; pp. 525–540. [DOI] [PubMed] [Google Scholar]
- Mann Giselle. Vol. 1. Cengage learning; 2002. MASA: The Mann assessment of swallowing ability. [Google Scholar]
- Tombaugh Tom N, Mcintyre Nancy J. Journal of the American Geriatrics Society. 9. Vol. 40. Wiley; 1992. The Mini-Mental State Examination: A Comprehensive Review; pp. 922–935. [DOI] [PubMed] [Google Scholar]
- Hinkle Dennis E, Wiersma William, Jurs Stephen G. Vol. 663. Houghton Mifflin College Division; 2003. Applied statistics for the behavioral sciences. [Google Scholar]
- Schroeder Mae Fern, Daniels Stephanie K, Mcclain Maryellen, Corey David M, Foundas Anne L. The Journal of Rehabilitation Research and Development. 3. Vol. 43. Journal of Rehabilitation Research & Development; 2006. Clinical and cognitive predictors of swallowing recovery in stroke; pp. 301–301. [DOI] [PubMed] [Google Scholar]
- Kim Ji Sun, Youn Jinyoung, Suh Mee Kyung, Kim Tae-Eun S, Chin Juhee, Park Suyeon, Cho Jin Whan. Canadian Journal of Neurological Sciences / Journal Canadien des Sciences Neurologiques. 6. Vol. 42. Cambridge University Press (CUP); 2015. Cognitive and Motor Aspects of Parkinson’s Disease Associated with Dysphagia; pp. 395–400. [DOI] [PubMed] [Google Scholar]
- Seçil Y, Arıcı Ş, İncesu T K. Dysphagia in Alzheimer's disease. Neurophysiol Clin. 2016;46(3):171–178. doi: 10.1016/j.neucli.2015.12.007. [DOI] [PubMed] [Google Scholar]
- Chouinard J. Dysphagia in Alzheimer disease: a review. J Nutr Health Aging. 2000;4(4):214–217. [PubMed] [Google Scholar]
- Olchik Maira R, Ghisi Marciéle, Winckler Pablo B, Ayres Annelise. International Journal of Clinical Medicine. 12. 08. Scientific Research Publishing, Inc.; 2017. Correlation between Cognitive Aspects and Dysphagia in Patients with Amyotrophic Lateral Sclerosis: Preliminary Report; pp. 680–691. [Google Scholar]


