This systematic review uses novel methods to describe mental health symptoms during the first year of the COVID-19 pandemic and how they relate to days since the start of the pandemic, stringency of containment measures, and cumulative numbers of cases and deaths.
Abstract
Background:
To what extent the COVID-19 pandemic and its containment measures influenced mental health in the general population is still unclear.
Purpose:
To assess the trajectory of mental health symptoms during the first year of the pandemic and examine dose–response relations with characteristics of the pandemic and its containment.
Data Sources:
Relevant articles were identified from the living evidence database of the COVID-19 Open Access Project, which indexes COVID-19–related publications from MEDLINE via PubMed, Embase via Ovid, and PsycInfo. Preprint publications were not considered.
Study Selection:
Longitudinal studies that reported data on the general population's mental health using validated scales and that were published before 31 March 2021 were eligible.
Data Extraction:
An international crowd of 109 trained reviewers screened references and extracted study characteristics, participant characteristics, and symptom scores at each timepoint. Data were also included for the following country-specific variables: days since the first case of SARS-CoV-2 infection, the stringency of governmental containment measures, and the cumulative numbers of cases and deaths.
Data Synthesis:
In a total of 43 studies (331 628 participants), changes in symptoms of psychological distress, sleep disturbances, and mental well-being varied substantially across studies. On average, depression and anxiety symptoms worsened in the first 2 months of the pandemic (standardized mean difference at 60 days, −0.39 [95% credible interval, −0.76 to −0.03]); thereafter, the trajectories were heterogeneous. There was a linear association of worsening depression and anxiety with increasing numbers of reported cases of SARS-CoV-2 infection and increasing stringency in governmental measures. Gender, age, country, deprivation, inequalities, risk of bias, and study design did not modify these associations.
Limitations:
The certainty of the evidence was low because of the high risk of bias in included studies and the large amount of heterogeneity. Stringency measures and surges in cases were strongly correlated and changed over time. The observed associations should not be interpreted as causal relationships.
Conclusion:
Although an initial increase in average symptoms of depression and anxiety and an association between higher numbers of reported cases and more stringent measures were found, changes in mental health symptoms varied substantially across studies after the first 2 months of the pandemic. This suggests that different populations responded differently to the psychological stress generated by the pandemic and its containment measures.
Primary Funding Source:
Swiss National Science Foundation. (PROSPERO: CRD42020180049)
The World Health Organization and mental health experts have warned about a potential upsurge in mental ill health due to the COVID-19 pandemic and highlighted the need for research into the pandemic's effect (1–3). Quantifying an increase in mental health problems resulting from the pandemic is important for designing public health interventions. These interventions should maximize the benefits of measures to contain the spread of infection while minimizing their potential for harm in mental health problems and disruption of physical and mental health services.
With many studies on the effects of the pandemic on population mental health continually being published, systematic reviews of the literature are needed to make sense of the vast amounts of information. A World Health Organization scientific brief summarized systematic reviews of longitudinal studies estimating the changes in mental health symptoms or prevalence of mental disorders (4). It concluded that there was “a significant increase in mental health problems in the general population in the first year of the pandemic” (4). However, some systematic reviews and individual studies emphasized that the effect of the pandemic and its containment measures had not been uniformly detrimental for mental health and that the effect of the pandemic on mental health overall had been limited (5–7).
The results from individual studies in the published systematic reviews varied widely, but the sources of the heterogeneity between studies were not elucidated. Possible reasons for the heterogeneous results include differences in time into the pandemic, the severity of the COVID-19 epidemic in study areas, and the severity of control measures implemented by the authorities.
To better understand the conflicting evidence about changes in mental health during the pandemic, we did a systematic review and Bayesian nonlinear dose–response meta-analysis. We aimed to describe how mental disorder symptoms changed in the general population during the first year of the pandemic and whether these changes were related to the severity of governmental containment measures or the total numbers of reported cases and deaths from COVID-19. Because this was an unprecedented global situation with several unknowns, we did not have specific hypotheses about the direction of the examined associations. We used “crowdsourcing,” where trained researchers from 5 continents screened articles and extracted data online, to deal with the extensive literature that has accumulated on this topic over a short period (8).
Methods
Data Sources and Searches
The protocol of this systematic review was registered with PROSPERO (CRD42020180049) (9). We searched MEDLINE (via PubMed), Embase (via Ovid), and PsycInfo without language restrictions using the living evidence database of the COVID-19 Open Access Project, which used broad search strategies to capture COVID-19–related literature from 1 January 2020 (Section 1.1 of Supplement 1) (10). The search terms used to populate this database and their bibliography deduplication method are described online (https://ispmbern.github.io/covid-19). We then applied our own search filter (11) to the records in this database. We restricted the search to reports published until 31 March 2021—the end of the first year of the pandemic—before widespread rollout of vaccination programs.
Study Selection
We included studies with participants from the general population that reported data on any mental health condition for at least 2 time points, with at least 1 time point during the pandemic, and used a validated rating scale. We included longitudinal studies (data from the same sample collected over time) and repeated cross-sectional studies (data from different samples drawn from the same population at multiple time points). Studies with participants enrolled on the basis of their gender (such as women) or age group (such as children) were eligible. We excluded studies of specific populations, such as people with a particular condition (for example, diabetes or anxiety disorder), occupation (for example, health care personnel or teachers), or setting (for example, nursing homes). We decided to exclude studies enrolling exclusively patients with COVID-19 as well, because at the time they represented only a small percentage of the population and because their burden in terms of containment measures often differed substantially from that of the rest of the population. We also excluded studies analyzing hospital records or databases of health care use and studies enrolling participants via social media (12). We list detailed inclusion and exclusion criteria and describe how we resolved disagreements in extracted data in Sections 1.3 and 1.4 of Supplement 1.
Data Extraction and Other Data Collected
We crowdsourced all screening tasks and the data extraction process by recruiting 109 health care or research professionals (the “crowd”) from 28 countries on 5 continents. Crowd members received training and worked in pairs (based on their geographic proximity) using pretested online forms in REDCap (13). The protocol used to train the crowd is described on the project's website (https://mhcovid.ispm.unibe.ch/crowd.html).
We considered only studies that used validated rating scales, and we extracted data on anxiety, depression, alcohol and substance misuse, problematic social media and smartphone use, sleep disturbances, quality of life, life satisfaction, and mental (or psychological) well-being. Scales measuring more than 1 condition (such as anxiety and depression) or assessing general symptoms of mental ill health were considered under the category “psychological distress.” We extracted the mean score, its SD, and the sample size for each time point separately for each scale. For every time point with data, we defined the following 4 exposure variables:
Time point in the pandemic: Days elapsed between the date of the first case of SARS-CoV-2 infection recorded in a country and the time point of data collection.
Stringency of the containment measures: Score on the Oxford COVID-19 Government Response Tracker index (0 to 100) representing the stringency of governmental containment and closure policies and a cumulative sum of stringency scores at each time point (14). We also examined the economic support index, the containment and health index, and separate components of these indices (school closing, workplace closing, stay-at-home requirements, and restrictions on internal movement and facial covering) in post hoc analyses (Section 3 of Supplement 2) (14).
Cumulative cases: The cumulative number per 100 000 people of confirmed reported cases of SARS-CoV-2 infection at the time point of data collection in the study country since the date of the first case recorded in that country.
Cumulative deaths: The cumulative number per 100 000 people of reported COVID-19–related deaths at the time point of data collection in the study country since the date of the first case of SARS-CoV-2 infection recorded in that country.
We extracted data on study characteristics (data collection method, country, and study design) and participant characteristics (age, gender, ethnicity, and percentage with preexisting conditions or COVID-19). We also recorded data on gross domestic product per capita and the Gini inequality index in 2019 for each of the included countries. Section 2 of Supplement 2 provides details on variables and sources of information.
Risk of Bias Assessment
We developed a new tool to assess risk of bias in the included studies (Section 4.1 of Supplement 2). We examined items included in published instruments for prevalence studies and grouped them into categories according to the bias domain they address. We developed specific questions to evaluate how well the study sample represented the general population, the risk of nonresponse bias, and the risk of information bias. Each domain was judged to have low, high, or unclear risk of bias. Three investigators (N.P., G.S., and T.T.) piloted the instrument. We produced contour-enhanced funnel plots to explore possible publication bias (15).
Data Synthesis and Analysis
We estimated the standardized mean differences (SMDs) in symptom scores between the earliest reported time point (for example, a prepandemic measurement) and all subsequent time points reported in a study (for example, several measurements during the pandemic). A negative SMD meant that mental health worsened over time. We accounted for correlations between SMDs in studies reporting more than 2 time points and more than 1 condition using a multivariate normal likelihood. All models were fitted within a Bayesian framework as hierarchical random-effects models using JAGS in R, version 4.0.4 (16, 17). We present the posterior means, 95% credible intervals (CrIs), and 95% prediction intervals (PrIs) (18). Prediction intervals show the range of expected SMDs for any hypothetical study population similar to those in included studies. When interpreting the results, we distinguished between the average summary SMD from the meta-analysis and the expected SMDs shown in the range of the PrI. We estimated between-study heterogeneity by considering the SD of the random effects (τ) and the width of the PrI rather than the I 2 metric (18, 19). To enhance interpretation, we transformed summary SMDs into mean differences on the Patient Health Questionnaire-9 scale for depression and on the General Anxiety Disorder-7 scale for anxiety, using the observed pooled SDs of a large representative study (20).
We first used studies that report prepandemic scores to estimate a pre- versus during-pandemic summary SMD (henceforth “pre–during”). We used meta-regression to explore the relationship between SMDs and the following study and population characteristics: mean age, gender, risk of bias, sample size, timing of collection of prepandemic data, country (United States vs. China vs. other), gross domestic product per capita, and Gini index. We had planned to explore the role of preexisting physical and mental health conditions, but too few studies had relevant information.
We then used all studies (including those that provided data only during the pandemic) to model the trajectories in SMDs as nonlinear functions of each exposure variable. We synthesized study data in a Bayesian dose–response meta-analysis model with restricted cubic splines (21–23). Some exposure variables (such as cumulative cases) required log transformation. In sensitivity analyses, we used an alternative definition for days elapsed since the start of the pandemic: since 1 January 2020 in China and Hong Kong and 1 March 2020 for the rest of the world. We extended the model to include the linear effects of study and population characteristics. The statistical details of the analysis are presented in Section 5 of Supplement 2. We fitted all models with uninformative priors for summary SMDs and minimally informative priors for heterogeneity and regression coefficients (Section 5.9 of Supplement 2). To evaluate the convergence of the models, we monitored the mixing in trace plots with 3 different chains and the Gelman–Rubin statistic (24).
Certainty of the Evidence
For the pre–during meta-analysis, we used the GRADE (Grading of Recommendations Assessment, Development and Evaluation) approach to evaluate certainty in the evidence synthesis results, adapting the guidance for prognostic studies (25). There is no current guidance about how to evaluate certainty in a dose–response meta-analysis, so we adapted the GRADE guidance to our context (Section 4.2 of Supplement 2).
Role of the Funding Source
The Swiss National Science Foundation had no role in study design, data collection, data analysis, data interpretation, or writing and submission of the manuscript.
Results
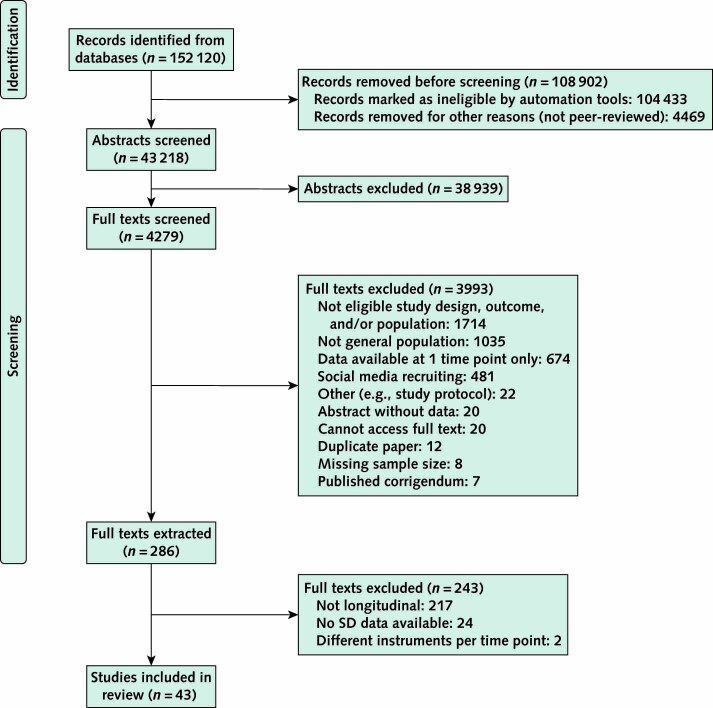
The flow of study selection is shown in the Appendix Figure. Overall, we included 43 studies with data from 331 628 participants and 153 combinations of conditions and time points (evidence profiles of the studies are in Section 10 of Supplement 2) (7, 20, 26–67). The 43 studies were done in 13 countries (with two thirds done in the United States, the United Kingdom, China, or Germany) (Table 1) and examined 11 conditions. Twenty-four studies (236 705 participants; 85 time points) contributed to the dose–response meta-analysis of depression and anxiety. The prepandemic data were collected as early as 2014, whereas the most recent data were from the end of November 2020.
Appendix Figure. Study flow diagram.
Table 1.
Characteristics of the Included Studies

The median sample size was 1035 participants. The median of the mean participant age was 42 years (range, 7 to 75 years), and more than half of the participants were women. The cumulative COVID-19 cases and deaths and the stringency, economic support, and containment and health indices varied widely across time points (Table 2). Of the 43 studies, 30 were repeated cross-sectional surveys. The risk for an unrepresentative sample and risk of nonresponse bias were high or unclear in most studies. In contrast, most studies showed a low risk of information bias (Table 1).
Table 2.
Characteristics of Study Participants, Countries, and the COVID-19 Epidemic

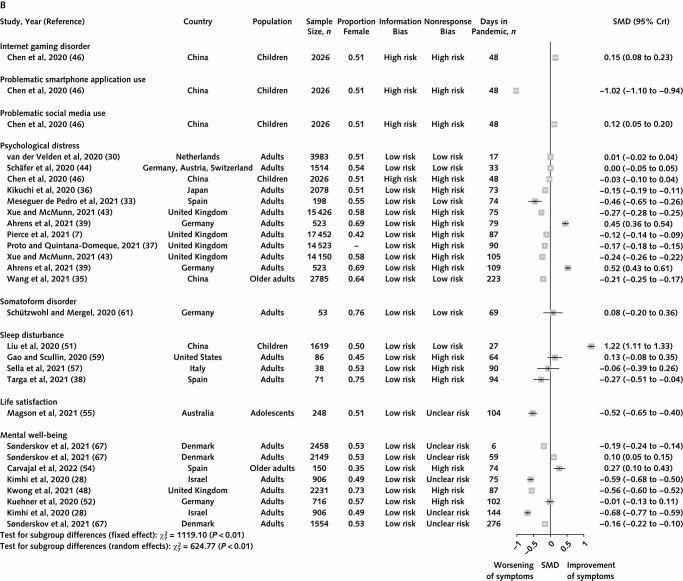
Meta-analysis of Pre- Versus During-Pandemic Mental Health Symptoms
Of the 43 included studies, 31 provided measurements before and during the pandemic and contributed 54 SMDs to the pre–during meta-analysis. The summary SMD for anxiety was −0.16 (95% CrI, −0.29 to −0.03; 95% PrI, −0.56 to 0.23; 1.6 [CrI, 0.3 to 2.9] points of change on the General Anxiety Disorder-7 scale); results were similar for depression (SMD, −0.22 [CrI, −0.33 to −0.11; PrI, −0.66 to 0.22; 2.9 {CrI, 1.4 to 4.3} points of change on the Patient Health Questionnaire-9 scale]) (Figure 1, A). Synthesis of these 2 conditions indicates an average worsening of symptoms during the pandemic compared with prepandemic levels (SMD, −0.20), albeit with considerable heterogeneity in SMDs resulting in a large PrI (−0.58 to 0.18; common τ = 0.18). In meta-regression analyses, none of the study and population characteristics in Tables 1 and 2 explained the heterogeneity and there was no evidence of an association between sample size and results (Section 2.1.2 of Supplement 1). The certainty of the evidence for the pre–during analysis for anxiety and depression was low, primarily because of the risk of bias in included studies and the high heterogeneity (see the summary of findings table in Section 2.1.6 of Supplement 1). The data for psychological distress were highly heterogeneous, with expected SMDs showing both important deterioration and alleviation of symptoms in study populations (PrI, −1.13 to 0.77) (Figure 1, B; Section 2.1.3 of Supplement 1). In meta-regressions, there was no evidence that any of the variables explained this heterogeneity. A potential reason is that scales for measuring personal distress are inherently more heterogenous than depression and anxiety scales. Whatever the reason, we decided to not synthesize the data. For the other conditions, the data were sparse, heterogeneous, or both, and we did not pursue any further synthesis. The only study on posttraumatic stress disorder did not provide prepandemic measurements.
Figure 1. Forest plot of SMDs of symptoms during the pandemic minus before the pandemic for anxiety and depression (A) and for other conditions, mental well-being, and life satisfaction (B).
Studies are ordered by days since the first recorded infection. CrI = credible interval; SMD = standardized mean difference; τ = heterogeneity SD.
Figure 1. Continued.
Dose–Response Meta-analysis for the Longitudinal Trajectory of Symptoms of Anxiety and Depression
We performed dose–response meta-analysis only for the studies on anxiety and depression (24 studies; 85 condition–time points) (Table 1) because the estimated heterogeneity in the other conditions was too large. Figure 2 (panel A) shows the SMDs for anxiety and depression combined as a function of days since the first recorded case. The association had a U shape, with the lower point at about 60 days. The average symptoms worsened until up to 2 months, but with large uncertainty around the mean (SMD at 30 days, −0.24 [CrI, −0.45 to −0.04]; SMD at 60 days, −0.39 [CrI, −0.76 to −0.03]). After 2 months, the slope became flatter, with even larger uncertainty, because of the small number of studies (SMD at 90 days, −0.38 [CrI, −0.90 to 0.15]). The PrIs calculated around these values were wide, suggesting that the expected trajectories in the study populations differed widely. A sensitivity analysis using a different definition of time elapsed since the beginning of the pandemic produced similar results (Section 6.2.1 of Supplement 2). We did 2 post hoc sensitivity analyses, including data only up to 120 days after the first case was recorded (because few data were available after this time point) and including only studies done in the Northern Hemisphere (where summer began approximately 3 months into the pandemic). Neither of these post hoc sensitivity analyses changed the interpretation of our results.
Figure 2. Dose–response meta-analysis plots of SMDs for symptoms of anxiety and depression as a function of days since the first case in the study country (A), the stringency index (B), cumulative number of cases (C), and cumulative number of deaths (D).
Dark green shading indicates credible regions, and light green shading indicates prediction regions. SMD < 0 means that the symptoms worsen over time. SMD = standardized mean difference.
The association between the stringency index and depression and anxiety symptoms was approximately linear (Figure 2, B). Studies with a high stringency index (that is, >80; four studies from Spain, Chile, and China [26, 27, 38, 57]) showed on average a larger increase in symptoms than studies with a lower stringency index. We estimated median SMDs of stringency index values of 40 and 80 versus 0 to be −0.18 (CrI, −0.30 to −0.03; PrI, −0.42 to 0.11) and −0.27 (CrI, −0.39 to −0.15; PrI, −0.90 to 0.36), respectively.
Standardized mean differences decreased linearly with increasing values in the containment health index and similarly for the economic support index and the individual components, although these variables had small variability across studies and hence provide little information about the shape of association (Section 6.2.2 of Supplement 2). Restrictions in movement had the most precise and least heterogeneous detrimental association with anxiety and depression symptoms.
The association between log-cumulative cases and SMD was also almost linear (Figure 2, C), with the estimated SMDs ranging from −0.22 (CrI, −0.32 to −0.13; PrI, −0.74 to 0.29) for 100 cumulative cases per 100 000 people to −0.35 (CrI, −0.52 to −0.16; PrI, −1.28 to 0.59) for 2000 cumulative cases per 100 000 people. The SMD for 10 cumulative deaths per 100 000 people was −0.30 (CrI, −0.53 to −0.07; PrI, −1.59 to 0.99); for 30 deaths it was −0.25 (CrI, −0.63 to 0.12; PrI, −2.38 to 1.86). The association between cumulative deaths and depression and anxiety symptoms was uncertain, as shown by the increasing width of the CrIs and PrIs in Figure 2 (panel D).
We performed meta-regression for all 4 dose–response meta-analyses, but we did not consistently identify any variable that could explain heterogeneity in the dose–response associations (Section 2.2.2 of Supplement 1). In a post hoc analysis, we fitted a multivariable dose–response model to estimate jointly the effect of the stringency index and the cumulative cases using only linear terms. The model indicated only an association with cumulative cases; the coefficient for the stringency index was close to 0 (Section 6.2.3 of Supplement 2). A multivariable model that also included days since the first case had poor convergence to allow any reliable conclusions.
The certainty of the evidence for the examined associations was very low for the pandemic's duration and the cumulative number of deaths (downgraded for within-study limitations, imprecision, and heterogeneity) and low for the stringency index or the cumulative number of cases (downgraded for within-study limitations and heterogeneity) (Section 2.2.3 of Supplement 1).
Discussion
In this systematic review of 43 studies, the symptoms of mental health disorders in the general population worsened slightly, on average, during the first 2 months of the pandemic. The estimated and expected changes in symptoms varied in study populations from very detrimental to somewhat beneficial (expected SMDs ranged from −0.58 to 0.18 for anxiety and depression and from −1.13 to 0.77 for psychological distress). The heterogeneity could not be attributed to observed population or country characteristics. In dose–response meta-analyses, depression and anxiety symptoms increased during the first 2 months of the pandemic by up to a summary SMD of −0.39 and were positively associated with the stringency of governmental containment measures and with the cumulative numbers of reported cases and deaths. About half of the included studies had a sample that might not be representative of the general population or had unclear risk of information bias. Because of the heterogeneity and risk of bias in the studies, the certainty of these findings ranges from low to very low.
Strengths of this review include the methods used to quantify, present, and investigate the large amount of heterogeneity using PrIs and meta-regression. We took a conservative stance by refraining from synthesizing very heterogeneous data and by properly distinguishing between inferences about the average effect and expected effects in different study populations. The use of nonlinear dose–response meta-analysis is novel in systematic reviews of the pandemic's effect on mental health. We also developed a new risk of bias tool, tailored to our context, and we present the certainty in our conclusions following a prespecified methodology. The achievement of crowdsourcing the screening and data extraction process at such a large, global scale is another strength. Despite the dedication of more than 100 reviewers, a limitation of our study is the time taken to conduct the study and synthesize the findings up to 31 March 2021. The large number of records to be screened results from the volume of published literature about COVID-19 and the poor specificity of search terms to identify observational epidemiologic studies. We are currently updating our database, doing further analyses, and examining ways to improve the efficiency of the crowd's work to ensure sustainability.
Two previous systematic reviews of longitudinal studies focused on estimating the average effect of the pandemic on mental health, despite the very high heterogeneity between studies (5, 68). Considering only statistical significance or CIs of the average effect, these reviews concluded that the pandemic had a detrimental effect on people's mental health. A rapid systematic review concluded against a uniform effect of the lockdown on mental health (6). Most of the examined associations in these 3 reviews showed a heterogeneity index (I 2) greater than 90%, in which case many meta-analysts would refrain from drawing conclusions based on the summary mean and its statistical significance. In our data synthesis, we used nonlinear dose–response meta-analysis, which is more powerful than standard meta-regression because it can incorporate data from cohorts recruited exclusively during the pandemic; this may explain why Robinson and colleagues (5) did not find any evidence of association between changes in mean symptom score and various exposures.
Although our data showed an overall increase in mental health symptoms from before to during the pandemic, there were a few studies in which symptoms decreased from their prepandemic values. A small study of 99 mainly young people identified by snowball sampling suggested improvement in depression symptoms during the pandemic, and decreased academic stress during the initial phase of the pandemic is a possible explanation (31). A study by Kwong and colleagues (48) was based on a birth cohort with relatively high prevalence of depressive symptoms (25%) before the pandemic. Why this prevalence decreased to 18% during the pandemic remains unclear, and the authors do not provide any explanation.
The observed associations between the exposure variables and changes in mental health symptoms should not be interpreted as causal relationships. The numbers of cases and the stringency of the measures are strongly correlated over time, and it is very difficult to disentangle their effects on mental health. Surges in cases can have a direct detrimental effect on mental health (for example, because of concerns about personal risk or infections of family members and friends) and in most countries prompted an increase in the stringency of containment measures. Strict containment measures may flatten the curve of cases, yielding a potentially positive effect on mental health, while also increasing isolation, intensifying caretaker duties, and creating concerns about the economic consequences of closures, yielding a potentially negative effect on mental health. In addition, fear of the unknown in the face of an unprecedented global crisis and concerns about authoritarian state control may have independently affected public mental health or mediated the effect of the number of cases and the stringency of containment measures.
Estimating the effect of participant-level variables, such as age, gender, and economic situation, without the risk of aggregation-level bias requires access to individual participant data from the included studies. Because we had access only to aggregated country-level data (for both the outcome and the stringency index), we could not account for individual differences in work and living conditions or for regional variations in policies within countries. For example, persons with young children would be more affected by schools closing, and regions relying economically on tourism would be affected mostly by travel restrictions and restaurant closures. Our findings apply to the general population at the beginning of the pandemic and do not include important developments, such as the Delta variant wave in India. Effective vaccines and treatments became available in 2021, but new SARS-CoV-2 variants of concern have also emerged. These developments, as well as prolonged economic difficulties, may introduce additional sources of heterogeneity in future studies, which will need to be investigated in updates of this systematic review. An individual participant data meta-analysis could potentially identify participant-level characteristics (such as changes in employment, financial situation, or living arrangement) associated with higher resilience or vulnerability in times of a global pandemic. Finally, the number of included longitudinal studies was small; implementing standardized longitudinal assessments of mental health in existing large cohorts would help address future major world events in a more uniform and efficient way.
The implications of our findings should be seen through the lens of our study's limitations discussed earlier. At the start of the pandemic, we found a worsening on average of symptoms of anxiety and depression, which increased with stringency in governmental measures; however, the degree and extent of this worsening and how much may be due to other factors, such as increased cumulative cases, are uncertain. Policymakers can balance the information from this study against evidence that containment measures efficiently controlled the spread of the virus, relieved pressure on health systems, and prevented deaths from COVID-19 (69, 70). Also, we found that some study populations clearly had a substantial worsening of anxiety and depression symptoms, particularly at the beginning of the pandemic and with increasing numbers of reported cases. Even if the degree of worsening of symptoms is relatively small, if many people are affected the overall effect can be large. This means that, while this pandemic continues and to prepare for future pandemics, governments need to ensure that adequate mental health service provision and appropriate interventions exist for those who need them (71). Further research is needed, particularly in low- and middle-income countries and for such conditions as alcohol and substance misuse. Overall, our analysis indicates that during a global pandemic we should never lose sight of the negative consequences on mental health for the average population or the community, but also that some populations have completely different trajectories in mental health. On the basis of these data, it is also reasonable to expect a wide range of reactions in future pandemics.
Supplementary Material
Appendix: Members of the MHCOVID Crowd Investigators
Every MHCOVID Crowd Investigator meets the criteria for authorship: Abdulkadir Usman Sambo, MBBS; Akira Onishi, MD; Akira Sato, MD, MScPH; Alessandro Rodolico, MD; Ana Cristina de Oliveira Solis, PhD; Anastasia Antoniou, MSc; Angelika Kapfhammer, MD; Anna Ceraso, MD; Aoife O’Mahony, MSc; Aurélie M. Lasserre, MD, PhD; Aziz Mert Ipekci, MD, MPH; Carmen Concerto, MD, PhD; Caroline Zangani, MD; Chinonso Igwesi-Chidobe, PhD; Christina Diehm, MD; Dicle Dilay Demir, MD; Dongfang Wang, MMed; Edoardo Giuseppe Ostinelli, MD; Ethan Sahker, PhD; Gabriel Henrique Beraldi, MD; Gamze Erzin, MD; Harrison Nelson; Helio Elkis, MD, PhD; Hissei Imai, PhD; Hui Wu, MD; Ilias Kamitsis, PhD; Ioannis Filis, MD; Ioannis Michopoulos, MD, PhD; Irene Bighelli, PhD; James S.W. Hong, MBBS; Javier Ballesteros, PhD; Katharine A. Smith, MD, PhD; Kazufumi Yoshida, MD, MSc; Kenji Omae, MD, DrPH; Marialena Trivella, DPhil; Masafumi Tada, MD; Matthias A. Reinhard, MD; Michael J. Ostacher, MD, MPH, MMSc; Monika Müller, MD, PhD; Nathalia Gonzalez Jaramillo, MD, MSc; Panagiotis P. Ferentinos, PhD; Rie Toyomoto, MHS; Samuele Cortese, MD, PhD; Sanae Kishimoto, MHS, MPH; Sergio A. Covarrubias-Castillo, MD; Spyridon Siafis, MD; Trevor Thompson, PhD; Vasilios Karageorgiou, MD; Virginia Chiocchia, MSc; Yikang Zhu, MD; and Yukiko Honda, MPH, DrPH.
Footnotes
This article was published at Annals.org on 18 October 2022.
* Dr. Salanti, Ms. Peter, Ms. Tonia, and Mr. Holloway contributed equally to this work.
† For members of the MHCOVID Crowd Investigators, see the Appendix.
Contributor Information
Collaborators: Abdulkadir Usman Sambo, Akira Onishi, Akira Sato, Alessandro Rodolico, Ana Cristina de Oliveira Solis, Anastasia Antoniou, Angelika Kapfhammer, Anna Ceraso, Aoife O’Mahony, Aurélie M. Lasserre, Aziz Mert Ipekci, Carmen Concerto, Caroline Zangani, Chinonso Igwesi-Chidobe, Christina Diehm, Dicle Dilay Demir, Dongfang Wang, Edoardo Giuseppe Ostinelli, Ethan Sahker, Gabriel Henrique Beraldi, Gamze Erzin, Harrison Nelson, Helio Elkis, Hissei Imai, Hui Wu, Ilias Kamitsis, Ioannis Filis, Ioannis Michopoulos, Irene Bighelli, James S.W. Hong, Javier Ballesteros, Katharine A. Smith, Kazufumi Yoshida, Kenji Omae, Marialena Trivella, Masafumi Tada, Matthias A. Reinhard, Michael J. Ostacher, Monika Müller, Nathalia Gonzalez Jaramillo, Panagiotis P. Ferentinos, Rie Toyomoto, Samuele Cortese, Sanae Kishimoto, Sergio A. Covarrubias-Castillo, Spyridon Siafis, Trevor Thompson, Vasilios Karageorgiou, Virginia Chiocchia, Yikang Zhu, and Yukiko Honda
References
- 1. World Health Organization. Mental health and psychosocial considerations during the COVID-19 outbreak. 18 March 2020. Accessed at www.who.int/docs/default-source/coronaviruse/mental-health-considerations.pdf on 15 August 2022.
- 2. Mahase E. Covid-19: mental health consequences of pandemic need urgent research, paper advises. BMJ. 2020;369:m1515. [PMID: ] doi: 10.1136/bmj.m1515 [DOI] [PubMed] [Google Scholar]
- 3. Holmes EA, O’Connor RC, Perry VH, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7:547-560. [PMID: ] doi: 10.1016/S2215-0366(20)30168-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. World Health Organization. Mental health and COVID-19: early evidence of the pandemic's impact: scientific brief. 2 March 2022. Accessed at www.who.int/publications-detail-redirect/WHO-2019-nCoV-Sci_Brief-Mental_health-2022.1 on 7 March 2022.
- 5. Robinson E, Sutin AR, Daly M, et al. A systematic review and meta-analysis of longitudinal cohort studies comparing mental health before versus during the COVID-19 pandemic in 2020. J Affect Disord. 2022;296:567-576. [PMID: ] doi: 10.1016/j.jad.2021.09.098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Prati G, Mancini AD. The psychological impact of COVID-19 pandemic lockdowns: a review and meta-analysis of longitudinal studies and natural experiments. Psychol Med. 2021;51:201-211. [PMID: ] doi: 10.1017/S0033291721000015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Pierce M, McManus S, Hope H, et al. Mental health responses to the COVID-19 pandemic: a latent class trajectory analysis using longitudinal UK data. Lancet Psychiatry. 2021;8:610-619. [PMID: ] doi: 10.1016/S2215-0366(21)00151-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ipekci AM, Buitrago-Garcia D, Meili KW, et al. Outbreaks of publications about emerging infectious diseases: the case of SARS-CoV-2 and Zika virus. BMC Med Res Methodol. 2021;21:50. [PMID: ] doi: 10.1186/s12874-021-01244-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Salanti G, Cipriani A, Furukawa TA, et al. An efficient way to assess the effect of COVID-19 on mental health in the general population [Letter]. Lancet Psychiatry. 2021;8:e14-e15. [PMID: ] doi: 10.1016/S2215-0366(21)00067-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. The COAP team of ISPM. COVID-19 living evidence database. Accessed at https://ispmbern.github.io/covid-19/living-review/collectingdata.html on 11 March 2022.
- 11. The MHCOVID Project. Effects of the COVID-19 pandemic on the general population's mental health, alcohol/substance abuse, violence and aggression. 20 May 2020. Accessed at https://esm-ispm-unibe-ch.github.io/covid19-mhsr/search-strategy on 11 March 2022.
- 12. Topolovec-Vranic J, Natarajan K. The use of social media in recruitment for medical research studies: a scoping review. J Med Internet Res. 2016;18:e286. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377-81. [PMID: ] doi: 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hale T, Angrist N, Goldszmidt R, et al. A global panel database of pandemic policies (Oxford COVID-19 Government Response Tracker). Nat Hum Behav. 2021;5:529-538. [PMID: ] doi: 10.1038/s41562-021-01079-8 [DOI] [PubMed] [Google Scholar]
- 15. Peters JL, Sutton AJ, Jones DR, et al. Contour-enhanced meta-analysis funnel plots help distinguish publication bias from other causes of asymmetry. J Clin Epidemiol. 2008;61:991-6. [PMID: ] doi: 10.1016/j.jclinepi.2007.11.010 [DOI] [PubMed] [Google Scholar]
- 16. Plummer M, Stukalov A, Denwood M. rjags: Bayesian graphical models using MCMC. 19 April 2022. Accessed at https://CRAN.R-project.org/package=rjags on 15 August 2022.
- 17. R Core Team. Package ‘rjags.’ 12 April 2022. Accessed at https://cran.r-project.org/web/packages/rjags/rjags.pdf on 15 August 2022.
- 18. Riley RD, Higgins JP, Deeks JJ. Interpretation of random effects meta-analyses. BMJ. 2011;342:d549. [PMID: ] doi: 10.1136/bmj.d549 [DOI] [PubMed] [Google Scholar]
- 19. Migliavaca CB, Stein C, Colpani V, et al; Prevalence Estimates Reviews-Systematic Review Methodology Group (PERSyst). Meta-analysis of prevalence: I 2 statistic and how to deal with heterogeneity. Res Synth Methods. 2022;13:363-367. [PMID: ] doi: 10.1002/jrsm.1547 [DOI] [PubMed] [Google Scholar]
- 20. Peters A, Rospleszcz S, Greiser KH, et al. The impact of the COVID-19 pandemic on self-reported health. Dtsch Arztebl Int. 2020;117:861-867. [PMID: ] doi: 10.3238/arztebl.2020.0861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Crippa A, Discacciati A, Bottai M, et al. One-stage dose-response meta-analysis for aggregated data. Stat Methods Med Res. 2019;28:1579-1596. [PMID: ] doi: 10.1177/0962280218773122 [DOI] [PubMed] [Google Scholar]
- 22. Hamza T, Cipriani A, Furukawa TA, et al. A Bayesian dose-response meta-analysis model: a simulations study and application. Stat Methods Med Res. 2021;30:1358-1372. [PMID: ] doi: 10.1177/0962280220982643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Orsini N, Li R, Wolk A, et al. Meta-analysis for linear and nonlinear dose-response relations: examples, an evaluation of approximations, and software. Am J Epidemiol. 2012;175:66-73. [PMID: ] doi: 10.1093/aje/kwr265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Plummer M, Best N, Cowles K, et al. CODA: convergence diagnosis and output analysis for MCMC. 1 March 2006. Accessed at www.semanticscholar.org/paper/CODA%3A-convergence-diagnosis-and-output-analysis-for-Plummer-Best/de68accd3a2e4411c0931ca14b7eb46b44bdc9ed on 15 August 2022.
- 25. Foroutan F, Guyatt G, Zuk V, et al. GRADE guidelines 28: use of GRADE for the assessment of evidence about prognostic factors: rating certainty in identification of groups of patients with different absolute risks. J Clin Epidemiol. 2020;121:62-70. [PMID: ] doi: 10.1016/j.jclinepi.2019.12.023 [DOI] [PubMed] [Google Scholar]
- 26. Herrera MS, Elgueta R, Fernández MB, et al. A longitudinal study monitoring the quality of life in a national cohort of older adults in Chile before and during the COVID-19 outbreak. BMC Geriatr. 2021;21:143. [PMID: ] doi: 10.1186/s12877-021-02110-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Wang C, Pan R, Wan X, et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav Immun. 2020;87:40-48. [PMID: ] doi: 10.1016/j.bbi.2020.04.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kimhi S, Eshel Y, Marciano H, et al. A renewed outbreak of the COVID-19 pandemic: a longitudinal study of distress, resilience, and subjective well-being. Int J Environ Res Public Health. 2020;17. [PMID: ] doi: 10.3390/ijerph17217743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Bräscher AK, Benke C, Weismüller BM, et al. Anxiety and depression during the first wave of COVID-19 in Germany - results of repeated cross-sectional surveys. Psychol Med. 2021:1-5. [PMID: ] doi: 10.1017/S0033291721000866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. van der Velden PG, Contino C, Das M, et al. Anxiety and depression symptoms, and lack of emotional support among the general population before and during the COVID-19 pandemic. A prospective national study on prevalence and risk factors. J Affect Disord. 2020;277:540-548. [PMID: ] doi: 10.1016/j.jad.2020.08.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Lau JF, Shariff R, Meehan A. Are biased interpretations of ambiguous social and non-social situations a precursor, consequence or maintenance factor of youth loneliness. Behav Res Ther. 2021;140:103829. [PMID: ] doi: 10.1016/j.brat.2021.103829 [DOI] [PubMed] [Google Scholar]
- 32. Sutin AR, Stephan Y, Luchetti M, et al. BMI, weight discrimination, and the trajectory of distress and well-being across the coronavirus pandemic. Obesity (Silver Spring). 2021;29:38-45. [PMID: ] doi: 10.1002/oby.23048 [DOI] [PubMed] [Google Scholar]
- 33. Meseguer de Pedro M, Fernández-Valera MM, García-Izquierdo M, et al. Burnout, psychological capital and health during COVID-19 social isolation: a longitudinal analysis. Int J Environ Res Public Health. 2021;18. [PMID: ] doi: 10.3390/ijerph18031064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Wang Y, Hu Z, Feng Y, et al. Changes in network centrality of psychopathology symptoms between the COVID-19 outbreak and after peak. Mol Psychiatry. 2020;25:3140-3149. [PMID: ] doi: 10.1038/s41380-020-00881-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Wang Y, Fu P, Li J, et al. Changes in psychological distress before and during the COVID-19 pandemic among older adults: the contribution of frailty transitions and multimorbidity. Age Ageing. 2021;50:1011-1018. [PMID: ] doi: 10.1093/ageing/afab061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Kikuchi H, Machida M, Nakamura I, et al. Changes in psychological distress during the COVID-19 pandemic in Japan: a longitudinal study. J Epidemiol. 2020;30:522-528. [PMID: ] doi: 10.2188/jea.JE20200271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Proto E, Quintana-Domeque C. COVID-19 and mental health deterioration by ethnicity and gender in the UK. PLoS One. 2021;16:e0244419. [PMID: ] doi: 10.1371/journal.pone.0244419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Targa ADS, Benítez ID, Moncusí-Moix A, et al. Decrease in sleep quality during COVID-19 outbreak. Sleep Breath. 2021;25:1055-1061. [PMID: ] doi: 10.1007/s11325-020-02202-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Ahrens KF, Neumann RJ, Kollmann B, et al. Differential impact of COVID-related lockdown on mental health in Germany [Letter]. World Psychiatry. 2021;20:140-141. [PMID: ] doi: 10.1002/wps.20830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Gulliver A, Banfield M, Batterham PJ, et al. Effects of previous exposure to psychotherapeutic strategies on depression and anxiety symptoms during the COVID-19 pandemic. BJPsych Open. 2021;7:e38. [PMID: ] doi: 10.1192/bjo.2020.170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Kujawa A, Green H, Compas BE, et al. Exposure to COVID-19 pandemic stress: associations with depression and anxiety in emerging adults in the United States. Depress Anxiety. 2020;37:1280-1288. [PMID: ] doi: 10.1002/da.23109 [DOI] [PubMed] [Google Scholar]
- 42. Sharman S, Roberts A, Bowden-Jones H, et al. Gambling in COVID-19 lockdown in the UK: depression, stress, and anxiety. Front Psychiatry. 2021;12:621497. [PMID: ] doi: 10.3389/fpsyt.2021.621497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Xue B, McMunn A. Gender differences in unpaid care work and psychological distress in the UK Covid-19 lockdown. PLoS One. 2021;16:e0247959. [PMID: ] doi: 10.1371/journal.pone.0247959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Schäfer SK, Sopp MR, Schanz CG, et al. Impact of COVID-19 on public mental health and the buffering effect of a sense of coherence. Psychother Psychosom. 2020;89:386-392. [PMID: ] doi: 10.1159/000510752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Hawes MT, Szenczy AK, Klein DN, et al. Increases in depression and anxiety symptoms in adolescents and young adults during the COVID-19 pandemic. Psychol Med. 2021:1-9. [PMID: ] doi: 10.1017/S0033291720005358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Chen IH, Chen CY, Pakpour AH, et al. Internet-related behaviors and psychological distress among schoolchildren during COVID-19 school suspension [Letter]. J Am Acad Child Adolesc Psychiatry. 2020;59:1099-1102.e1. [PMID: ] doi: 10.1016/j.jaac.2020.06.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. O’Connor RC, Wetherall K, Cleare S, et al. Mental health and well-being during the COVID-19 pandemic: longitudinal analyses of adults in the UK COVID-19 Mental Health & Wellbeing study. Br J Psychiatry. 2021;218:326-333. [PMID: ] doi: 10.1192/bjp.2020.212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Kwong ASF, Pearson RM, Adams MJ, et al. Mental health before and during the COVID-19 pandemic in two longitudinal UK population cohorts. Br J Psychiatry. 2021;218:334-343. [PMID: ] doi: 10.1192/bjp.2020.242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Pierce M, Hope H, Ford T, et al. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry. 2020;7:883-892. [PMID: ] doi: 10.1016/S2215-0366(20)30308-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Fujita K, Inoue A, Kuzuya M, et al. Mental health status of the older adults in Japan during the COVID-19 pandemic [Letter]. J Am Med Dir Assoc. 2021;22:220-221. [PMID: ] doi: 10.1016/j.jamda.2020.11.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Liu Y, Finch BK, Brenneke SG, et al. Perceived discrimination and mental distress amid the COVID-19 pandemic: evidence from the Understanding America Study. Am J Prev Med. 2020;59:481-492. [PMID: ] doi: 10.1016/j.amepre.2020.06.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Kuehner C, Schultz K, Gass P, et al. [Mental health status in the community during the COVID-19-pandemic]. Psychiatr Prax. 2020;47:361-369. [PMID: ] doi: 10.1055/a-1222-9067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Daly M, Robinson E. Psychological distress and adaptation to the COVID-19 crisis in the United States. J Psychiatr Res. 2021;136:603-609. [PMID: ] doi: 10.1016/j.jpsychires.2020.10.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Carvajal BP, Molina-Martínez MÁ, Fernández-Fernández V, et al. Psychometric properties of the Cognitive Emotion Regulation Questionnaire (CERQ) in Spanish older adults. Aging Ment Health. 2022;26:413-422. [PMID: ] doi: 10.1080/13607863.2020.1870207 [DOI] [PubMed] [Google Scholar]
- 55. Magson NR, Freeman JYA, Rapee RM, et al. Risk and protective factors for prospective changes in adolescent mental health during the COVID-19 pandemic. J Youth Adolesc. 2021;50:44-57. [PMID: ] doi: 10.1007/s10964-020-01332-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Novotný JS, Gonzalez-Rivas JP, Kunzová Š, et al. Risk factors underlying COVID-19 lockdown-induced mental distress. Front Psychiatry. 2020;11:603014. [PMID: ] doi: 10.3389/fpsyt.2020.603014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Sella E, Carbone E, Toffalini E, et al. Self-reported sleep quality and dysfunctional sleep-related beliefs in young and older adults: changes in times of COVID-19 lockdown. Sleep Med. 2021;81:127-135. [PMID: ] doi: 10.1016/j.sleep.2021.02.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Giménez-Dasí M, Quintanilla L, Lucas-Molina B, et al. Six weeks of confinement: psychological effects on a sample of children in early childhood and primary education. Front Psychol. 2020;11:590463. [PMID: ] doi: 10.3389/fpsyg.2020.590463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Gao C, Scullin MK. Sleep health early in the coronavirus disease 2019 (COVID-19) outbreak in the United States: integrating longitudinal, cross-sectional, and retrospective recall data. Sleep Med. 2020;73:1-10. [PMID: ] doi: 10.1016/j.sleep.2020.06.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Liu Z, Tang H, Jin Q, et al. Sleep of preschoolers during the coronavirus disease 2019 (COVID-19) outbreak. J Sleep Res. 2021;30:e13142. [PMID: ] doi: 10.1111/jsr.13142 [DOI] [PubMed] [Google Scholar]
- 61. Schützwohl M, Mergel E. Social participation, inclusion and mental well-being following SARS-CoV-2 related lockdown restrictions in adults with and without mental disorders. Results from a follow-up study in Germany. PsyArXiv. Preprint posted online 28 May 2020. doi: 10.31234/osf.io/6svxw [DOI]
- 62. Wanberg CR, Csillag B, Douglass RP, et al. Socioeconomic status and well-being during COVID-19: a resource-based examination. J Appl Psychol. 2020;105:1382-1396. [PMID: ] doi: 10.1037/apl0000831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Krendl AC, Perry BL. The impact of sheltering in place during the COVID-19 pandemic on older adults' social and mental well-being. J Gerontol B Psychol Sci Soc Sci. 2021;76:e53-e58. [PMID: ] doi: 10.1093/geronb/gbaa110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Richardson DL, Duncan MJ, Clarke ND, et al. The influence of COVID-19 measures in the United Kingdom on physical activity levels, perceived physical function and mood in older adults: a survey-based observational study. J Sports Sci. 2021;39:887-899. [PMID: ] doi: 10.1080/02640414.2020.1850984 [DOI] [PubMed] [Google Scholar]
- 65. Holman EA, Thompson RR, Garfin DR, et al. The unfolding COVID-19 pandemic: a probability-based, nationally representative study of mental health in the United States. Sci Adv. 2020;6. [PMID: ] doi: 10.1126/sciadv.abd5390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Killgore WDS, Cloonan SA, Taylor EC, et al. Three months of loneliness during the COVID-19 lockdown [Letter]. Psychiatry Res. 2020;293:113392. [PMID: ] doi: 10.1016/j.psychres.2020.113392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Sønderskov KM, Dinesen PT, Vistisen HT, et al. Variation in psychological well-being and symptoms of anxiety and depression during the COVID-19 pandemic: results from a three-wave panel survey. Acta Neuropsychiatr. 2021;33:156-159. [PMID: ] doi: 10.1017/neu.2020.47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. COVID-19 Mental Disorders Collaborators. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. 2021;398:1700-1712. [PMID: ] doi: 10.1016/S0140-6736(21)02143-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Kwon S, Joshi AD, Lo CH, et al. Association of social distancing and face mask use with risk of COVID-19. Nat Commun. 2021;12:3737. [PMID: ] doi: 10.1038/s41467-021-24115-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Teslya A, Pham TM, Godijk NG, et al. Impact of self-imposed prevention measures and short-term government-imposed social distancing on mitigating and delaying a COVID-19 epidemic: a modelling study. PLoS Med. 2020;17:e1003166. [PMID: ] doi: 10.1371/journal.pmed.1003166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Campion J, Javed A, Sartorius N, et al. Addressing the public mental health challenge of COVID-19. Lancet Psychiatry. 2020;7:657-659. [PMID: ] doi: 10.1016/S2215-0366(20)30240-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.