Abstract
How do religious affiliation and beliefs shape vaccine attitudes and behaviors? This study examined the associations of attitudes and behaviors relevant to the flu, measles-mumps-rubella (MMR), and human-papillomavirus (HPV) vaccines with religious affiliations, as well as philosophical, spiritual, and moral beliefs. Respondents were 3005 adults from a probability-based, four-wave panel survey in the United States. Longitudinal structural equation modeling examined how religious affiliations and philosophical/moral beliefs shaped attitudes toward vaccines and actual vaccination. Stronger philosophical beliefs predicted more negative attitudes toward each vaccine and stronger moral beliefs more negative attitudes toward the HPV vaccine. Negative vaccine attitudes then predicted weaker intentions to encourage others to vaccinate and lower probability of receiving a vaccine. Theoretical and public health messaging implications are discussed.
Keywords: longitudinal survey, religious affiliations, religious beliefs, vaccine attitudes, vaccine intentions and behavior
Although the Church of the First Born advocates faith healing over medical care and Christian Scientists maintain that vaccines are unnecessary (Iannelli, 2019) and concerns with the use of gelatin in the vaccine itself (e.g. for Muslims) and the use of human fetus cell lineages in vaccine development (e.g. for Christians) vary across religions, Islam, Judaism, and Christianity are not explicitly against the idea of vaccination as well (Shurpin, 2015). Nonetheless, affiliation with specific denominations has in recent years been associated with outbreaks of flu and measles. For example, recent measles outbreaks in the United States (U.S.) emerged primarily in tightly-knit religious communities such as the Amish in Ohio and Orthodox Jews in New York (Belluz, 2019) and a fatwa by Muslim clerics plummeted the measles-mumps-rubella (MMR) vaccination rates in Indonesia (Rochmyaningsih, 2018). These developments raise questions about (a) the degree to which identification with certain religious groups predicts vaccine attitudes and behaviors and (b) the underlying beliefs that religious socialization might cultivate. This understanding is key to the design of health communication campaigns, and relevant to public health as the world embarks on massive vaccination efforts against the novel coronavirus disease (COVID-19).
To begin, although news accounts have chronicled a reluctance to vaccinate among those in some religious groups (Belluz, 2019; Otterman, 2019), scientific studies have generally ignored the link between religion and attitudes toward vaccines in the general population of countries studied. Most studies have been conducted with specific religious/ethnic communities including Gypsy communities in London or the Apostolic Church in Zimbabwe (Feder et al., 1993; Gerede et al., 2017). Empirical studies conducted have been generally restricted to specific regional and demographic groups for which religiosity is salient (e.g. 18–26 years-old insured women in Utah and religious leaders in Denver; Bodson et al., 2017; Williams and O’Leary, 2019), or focused on the human-papillomavirus (HPV) vaccine due to commonly cited religious concerns about the potential for these vaccines to promote teenage sexual activity. Yet, a review of the role of religious and philosophical beliefs in major religious affiliations in the U.S. has revealed common religious concerns with vaccines, such as the use of fetal tissue in vaccine development (Wombwell et al., 2015). However, to the best of our knowledge no prior research has simultaneously investigated the relations between religious affiliations, specific religious beliefs about vaccines, and attitudes toward vaccines and self-declared vaccination rates in a large-scale population-level approach. These relations, although potentially incomplete and simplified (Ammerman, 2013), are important to investigate because religious affiliation (institutional practice) and religious beliefs (as opposed to institutional practice of religion) are entirely distinct dimensions of religiosity (Versteeg and Roeland, 2011).
Against this background, this study contributes to this line of work by examining philosophical and moral beliefs about vaccines in the general U.S. population through a formal exploration of the processes leading from religious affiliation to attitudes and actual vaccination conducted with longitudinal causal analysis. Specifically, the current study investigated how religious affiliations might be associated with differing levels of two religious, philosophical and moral, which have been established as important predictors of vaccine hesitancy, thus interlinking the pathways between affiliation differences to cognitive predictors of both attitudinal and behavioral manifestations of vaccine hesitancy (Ajzen et al., 2019; Albarracín, 2020; Albarracín et al., 2001). In the following sections, we first review the existing research on religious affiliations and beliefs in conjunction with health beliefs and behaviors, particularly vaccination, before integrating their connections and predictive paths to attitudes and behaviors in the area of vaccination.
Religious affiliations
How institutionalized religion influences vaccine attitudes and actual vaccination is an important question. Religious considerations play an important role in vaccine attitudes, beliefs, and decisions (Natan et al., 2011; Rutjens et al., 2021). Prior research on vaccination intentions and behaviors has documented noteworthy associations with affiliation with an organized religion and level of religiosity (i.e. individual differences in how people interpret and practice their religion) particularly in the area of the HPV vaccine. For example, mothers who report being more religious are more reluctant to vaccinate their daughters against HPV than less religious ones (Natan et al., 2011; Shelton et al., 2013). Furthermore, according to an analysis of the U.S. Centers for Disease Control and Prevention (C.D.C.) National Teen Immunization Survey, across all religious affiliations, adolescents from non-orthodox households are more likely to get the HPV vaccine than are those from orthodox households (Sriram and Ranganathan, 2019). Also, people who frequently attend religious services tend to have lower HPV vaccination intentions (Barnack et al., 2010; Bernat et al., 2009) than do those who attend less frequently, and highly religious people in the U.S. are more likely to incorrectly believe that vaccines caused autism than are nonreligious (Rutjens et al., 2018). Recent research has shown that religiosity predicts lower intentions to get a potential COVID-19 vaccine as well (Olagoke et al., 2021). However, none of this work has looked at how affiliations and philosophical and moral beliefs may operate together to shape vaccination attitudes and behaviors.
With respect to specific religious affiliation, although some studies have found no associations with vaccination practices (Reynolds, 2014; Thomas et al., 2012; Williams et al., 2021), some of these null findings could be due to the reliance on specific samples, such as parents in a low income Latino community (e.g. Williams et al., 2021). Furthermore, even studies documenting differences among religious affiliations have also focused on specific communities. A comparison of multiple U.S. affiliations found that Jewish respondents had the lowest intentions to vaccinate against HPV (Fogel and Ebadi, 2011). A cross-national study found that Roman Catholics had more negative attitudes toward vaccines than did Russian/Eastern Orthodox adherents, atheists, and agnostics (Larson et al., 2016). Moreover, Muslim, Jewish, and people who identify as “Other Christians” appear to not differ from Roman Catholics (Larson et al., 2016), implying that affiliation with any Abrahamic religions (those referring to the Prophet Abraham as a common forefather: i.e. Judaism, Christianity, and Islam, (New World Encylopedia, 2009)) may be associated with more negative vaccine attitudes.1 Hence, in this study, we were interested in estimating differences in vaccine attitudes and behaviors (i.e. getting vaccinated and intentions to encourage others to get the vaccine) across religious affiliations in the general U.S. population through a large nationally representative survey focusing on how religious affiliations predict vaccine related attitudes and behaviors through two philosophical and moral religious beliefs about vaccination.
Philosophical and moral beliefs and their likely contributions to attitudes toward and actual vaccination
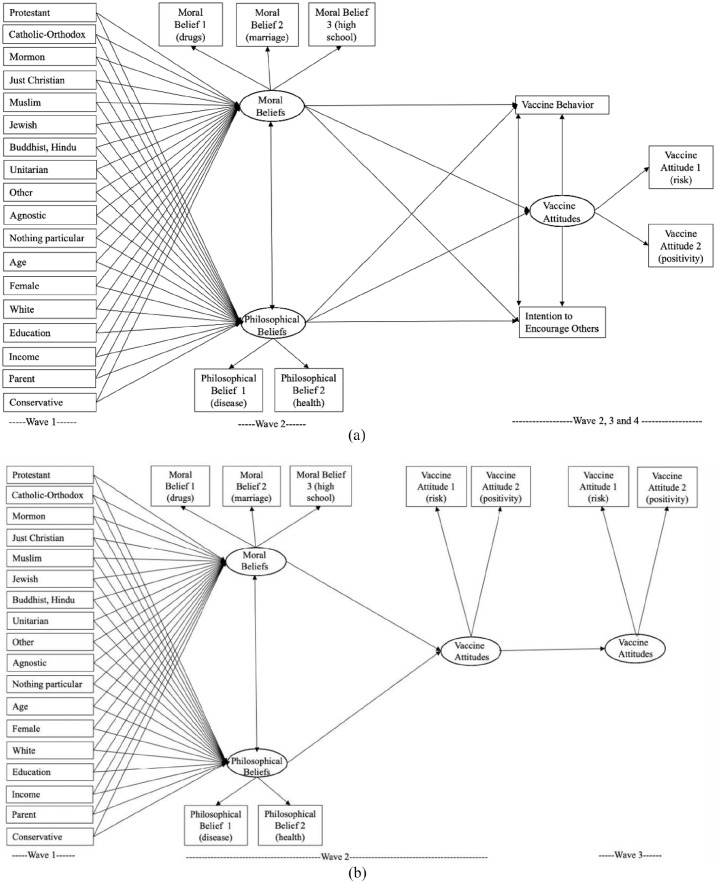
Differences among affiliations alone offer limited insights into the role of religion because individual adherents interpret their faith and form beliefs about vaccination in different ways (Wombwell et al., 2015). In this study, we are interested in the mediating role of two key and commonly discussed cognitions: (a) philosophical beliefs and (b) moral beliefs. These beliefs dovetail with two of Smart’s doctrinal and ethical dimensions of religiosity and are most relevant to the flu, MMR, and HPV vaccines (Smart, 1996). Our theoretical model illustrates how these beliefs, which may differ in intensity but are common to many religious affiliations, may subsequently influence vaccination attitudes and behaviors. By so doing, the model (See Figure 1a and b) provides a framework through which to understand the individual impact of religious affiliations on the philosophical and moral beliefs that may shape subsequent vaccine attitudes and behavior (Ajzen et al., 2019; Albarracín, 2020; Albarracín et al., 2001; Glasman and Albarracín, 2006). Next, we discuss these two beliefs in more detail.
Figure 1.
(a) Analytical model of the structural equation model for longitudinal flu vaccine model and (b) analytical model of the structural equation model for longitudinal MMR and HPV vaccine models.
The wave in which variables are collected are shown at the bottom respectively. Exogeneous variables’ covariances and error terms not shown. Reference category is Atheist.
Philosophical beliefs entail judgments about the natural order and can include fatalistic ideas about God controlling health outcomes (Shen et al., 2009). A study of qualitative interviews in the UK has shown that some people oppose vaccination out of a belief that “God would protect against childhood diseases” (Sporton and Francis, 2001). Likewise, philosophical beliefs that God will intervene are positively associated with lower vaccination rates. For example, parents may conclude that fighting HPV and MMR does not require medical intervention because of their faith in divine protection (Browne et al., 2015; Thomas et al., 2012). Similarly, a recent study found that self-reported spirituality has been shown to be strongest positive predictor of vaccine hesitancy in Greece, although the survey measure in this study did define “spirituality” to respondents (Rutjens and van der Lee, 2020; Rutjens et al., 2021). Research in other health domains such as physical activity and alcohol use found mixed findings about the influence of such beliefs about God intervening to protect one’s health (Karvinen and Carr, 2013). Hence, given the differences in religiosity and health behavior shown in the prior literature on religious affiliations and people citing their religious affiliation as a reason for their health decisions (Holt et al., 2016), we expected that (1) individuals from different affiliations would differ in their degree of endorsing philosophical beliefs and (2) those having stronger philosophical beliefs would exhibit more negative vaccine attitudes and less vaccination.
Moral beliefs relevant to vaccination are associated with judgments about sex and, particularly, sex outside of a marital union and sex during the early teenage years (Krakow et al., 2015). This type of belief has been widely studied, particularly when it comes to the HPV vaccine. For example, some parents believe that the HPV vaccine may mistakenly signal their permission for sexual activity to teenagers (Brewer and Fazekas, 2007) or remove the “penalties” otherwise associated with the natural consequences of sexual activity (Holman et al., 2014; Krakow et al., 2015). Hence, like philosophical beliefs, we expected that (1) individuals from different affiliations would differ in endorsement of moral beliefs and (2) those with stronger moral beliefs would exhibit more negative vaccine attitudes and less vaccination.
To reiterate the expectations in our theoretical model, we tested the relations between religious beliefs (philosophical and moral) and vaccination following the theoretical model proposed, in the context of three different vaccines, two childhood/adolescence vaccines (MMR and HPV), and one seasonal adult vaccine. We predicted that religious affiliations may be associated with different endorsement of philosophical and moral beliefs. In turn, stronger religious beliefs may predict less positive attitudes toward vaccines over time, and these less favorable vaccine attitudes may predict weaker intentions to encourage others to vaccinate and lower vaccination rates.2 However, the degree to which different affiliations would correlate with stronger religious or moral beliefs was an empirical question, as was the overall fit of our model to the data from our sample, the relative influence of each type of belief on attitudes and actual vaccination, and possible differences across vaccines.3 We tested this conceptual model via path analysis with three different vaccines.4
Empirical context: Three distinct vaccines in the United States, 2018–2019
In this section, we contextualize the empirical context by focusing on the country of data collection, the three distinct vaccines examined, and the longitudinal nature of the empirical evidence.
The current study concentrated on the Unites States, where 70% of adults report being Christian (45% Protestant, 21% Catholic), 2% being Jewish, 1% being Muslim, 1% being Buddhist, 1% being Hindu, 3% being Atheist, 4% being Agnostic, and 16% being “nothing in particular” (Pew Research Center, 2014a).5 Comparing across countries, the U.S. ranks moderately on the religious diversity index, being the 68th most diverse country out of the 233 (Pew Research Center, 2014b). In the public health domain, religious affiliations, communities, and beliefs usually are most commonly discussed in relation to policymaking about abortion, sexual identities, and religion-based exemptions from mandatory school vaccinations (Stecula et al., 2020). Hence, a large-scale study of the U.S. population offers important empirical evidence that could generalize to other important contexts, although demographic, sociocultural, and political differences across societies should be very carefully considered when extrapolating these findings to other countries.
Studying three different vaccines provided a strong framework to assess whether attitudes toward them have a similar belief basis. Vaccines differed on numerous attributes (typical age given, nature of the viruses targeted, nature of the associated health outcomes, seasonality, etc.). The HPV vaccine is known to fuel moral concerns about adolescent sexual activity, whereas the flu and MMR vaccines are not. As mentioned previously, the MMR and HPV vaccines are either one time or composed of a few doses in a lifetime, whereas the flu vaccine is seasonal. The MMR vaccine had more prominence surrounding the emergence of a measles outbreak in the U.S. in late 2018 and early 2019 and the flu vaccine was relevant because of the season, whereas the HPV vaccine was not particularly salient. Investigating patterns for such different vaccines, combined with a large probability sample, should inform theory and practice in the area of religion and vaccine promotion.
Finally, the current study investigated this model with three different vaccines through a longitudinal design. Through a nationally representative probability-based panel survey, the same respondents were tracked over a 6-months long period through a total of four re-contacts. This strategy provided an opportunity to capture within-individual changes and stability across time, thereby providing stronger causal associations in predicting vaccine attitudes and behavior (Ajzen et al., 2019).
Methods
Sample
The study was approved by the Institutional Review Board of the University of Pennsylvania and included written consent. It shared time and was administered within a larger panel study on perceptions of infectious diseases and vaccination predictors during 2018–2019. The survey consisted of a probability-based nationally representative panel sample of adults living in the U.S. who were randomly selected from the AmeriSpeak panel of National Opinion Research Center (NORC) at the University of Chicago. The sampling frame covered 97% of U.S. households via a two-stage stratified sampling (Supplemental Information—SI-1). In this study, we utilized data from four different waves of the panel based on available space for questions. Four waves of data collection were implemented between September 21, 2018 and March 18, 2019, thus covering the 2018–2019 flu season; further details on waves are in the upper panel in Table 1.
Table 1.
Details for sample waves and measures.
| Wave number | Details |
|---|---|
| Wave 1 | September 21, 2018–October 6, 2018; N = 3005; 2725 Internet respondents and 280 phone respondents; Questions: demographics and religious affiliations |
| Wave 2 | November 5, 2018–November 27, 2018; N = 2470; 2227 Internet respondents and 193 phone respondents; Retention rate from Wave 1: 82%; Questions: philosophical and moral beliefs, vaccine attitudes, intentions, and behaviors |
| Wave 3 | January 15, 2019–February 4, 2019; N = 2091; 1929 Internet respondents and 162 phone respondents; Retention rate from Wave 2: 79% and from Wave 1: 70%; Questions: vaccine attitudes, intentions, and behaviors |
| Wave 4 | February 28, 2019–March 18, 2019; N = 1803; 1684 Internet respondents and 119 phone respondents; Retention rate from Wave 3: 86% and from Wave 1: 60%; Questions: vaccine attitudes, intentions, and behaviors |
| Variable name | Details |
| Age | Continuous, open-ended question (asked in Wave 1) |
| Sex | Two categories, male = 0, female = 1 (asked in Wave 1) |
| Race | Five categories, recoded into White = 1 versus Non-White = 0 dummy; original categories: White, non-Hispanic; Black, non-Hispanic; Other, non-Hispanic; Hispanic; Non-Hispanic; Asian, non-Hispanic (asked in Wave 1) |
| Educational attainment | Continuous, 14 response categories (coding range from 1 to 14): No formal education; 1st, 2nd, 3rd, or 4th grade; 5th or 6th grade; 7th or 8th grade; 9th grade; 10th grade; 11th grade; 12th grade NO DIPLOMA; High school graduate or equivalent; Some college, no degree; Associate degree; Bachelor’s degree; Master’s degree; Professional or Doctorate degree (asked in Wave 1) |
| Annual income | Last year total household income, continuous, 18 response categories (coding range from 1 to 18): Less than $5000; $5000 to $9999; $10,000 to $14,999; $15,000 to $19,999; $20,000 to $24,999; $25,000 to $29,999; $30,000 to $34,999; $35,000 to $39,999; $40,000 to $49,999; $50,000 to $59,999; $60,000 to $74,999; $75,000 to $84,999; $85,000 to $99,999; $100,000 to $124,999; $125,000 to $149,999; $150,000 to $174,999; $175,000 to $199,999; $200,000 or more (asked in Wave 1) |
| Parent (9–12 years old) | Version 1: Are you a parent of a child between 9 and 12 years of age? Yes (1), No (0) (asked in Wave 2). This question is used in HPV and flu models. Version 2: Are you a parent of a child under 6 years of age? Yes (1), No (0) (asked in Wave 2). This question is used specifically for MMR models. |
| Religious affiliation | “What is your present religion, if any?”, 11 response options, “Protestant (Baptist, Methodist, Non-denominational, Lutheran, Presbyterian, Pentecostal, Episcopalian, Reformed, Church of Christ, Jehovah’s Witness, etc.),” “Roman Catholic (Catholic),” “Mormon (Church of Jesus Christ of Latter-day Saints/LDS),” “Orthodox (Greek, Russian, or some other orthodox church),” “Jewish (Judaism),” “Muslim (Islam),” “Buddhist,” “Hindu,” “Atheist (do not believe in God),” “Agnostic (not sure if there is a God),” “Nothing in particular,” “Just Christian,” “Unitarian (Universalist),” and “Other, please specify” (asked in Wave 1) |
| Religious mandate on vaccines | “Does your religion forbid its members from getting vaccines?”, Yes (1)/No (0), (asked in Wave 1) |
| Follow religion statement on vaccines | “Do you follow what your religion says about vaccines or not?”, Yes (1)/No (0), (asked in Wave 1) |
| Conservatism | Generally speaking, would you describe your political views as: (1) very liberal, (2) somewhat liberal, (3) moderate, (4) somewhat conservative, and (5) very conservative. (W1) |
| Philosophical beliefs | |
| Philosophical belief, item 1 | “If someone is meant to get a serious disease, they will get it no matter what they do”, four categories, “Strongly disagree” (1), “Somewhat disagree” (2), “Somewhat agree” (3), and “Strongly agree” (4) (asked in Wave 2) |
| Philosophical belief, item 2 | “My health is determined not by me but by a greater spiritual force”, four categories, “Strongly disagree” (1), “Somewhat disagree” (2), “Somewhat agree” (3), and “Strongly agree” (4) (asked in Wave 2) |
| Philosophical belief average of items 1 and 2 | Average of the two items (Pearson r = 0.46, Cronbach’s alpha = 0.63, Spearman-Brown = 0.63), continuous, (asked in Wave 2). |
| Moral beliefs | |
| Moral belief, item 1 | “Using drugs (narcotics)”, three categories: “Morally acceptable,” “Morally wrong,” and “Not a moral issue”; first and third categories combined* (0), second item (1) indicates bolder moral belief, (asked in Wave 2) |
| Moral belief, item 2 | “Having sex before marriage”, three categories: “Morally acceptable,” “Morally wrong,” and “Not a moral issue”; first and third categories combined* (0), second item (1) indicates bolder moral belief, (asked in Wave 2) |
| Moral belief, item 3 | “Having sex in high school”, three categories: “Morally acceptable,” “Morally wrong,” and “Not a moral issue”; first and third categories combined* (0), second item (1) indicates bolder moral belief (asked in Wave 2) *These two response options combined for theoretical and empirical reasons. There is no meaningful theoretical difference between “not a moral issue” and “morally acceptable”; the question included both of these response options in order to prevent offending some respondents who might feel they are being forced to make a moral judgment. Empirically, as well, those respondents who chose “not a moral issue” and “morally acceptable” were indistinguishable in their responses to vaccine attitudes and other key measures. *Moral beliefs measure offers a mixture of items that both tap vaccine-relevant issues (e.g. premarital and teen sex in relation to HPV being sexually transmitted infection) and provides a more generalizable moral beliefs measure given the breadth of moral issue dimensions. This also makes the measure more applicable to distinct vaccines, not just the HPV vaccine. |
| Moral belief average of items 1–3 | Average of items 1–3 (Pearson r = 0.36 for drugs and sex before marriage, r = .46 for drugs and high school sex, and r = 0.65 for sex before marriage and high school sex; Cronbach’s alpha = 0.74, Spearman-Brown = 0.80). |
| Vaccine attitudes | |
| Flu/MMR/HPV vaccine risk perceptions | “Just your best guess, how risky, if at all, do you think the flu (the MMR; the HPV) vaccine is?”, four categories, “Not risky at all” (1), “Not too risky” (2), “Somewhat risky” (3), and “Very risky” (4), (Reversed) (asked in Wave 2, 3, and 4) |
| Flu/MMR/HPV vaccine positivity | “Based on what you know, how positive or negative do you feel about the flu [the MMR; the HPV) vaccine?”, four categories, “Very negative” (1), “Somewhat negative” (2), “Somewhat positive” (3), and “Very positive” (4), recoded so that higher scores indicate more vaccine positivity (asked in Wave 2, 3, and 4) |
| Vaccine attitude index | Indexes are additive combination of vaccine risk and vaccine negativity. The Cronbach’s alpha for the flu, MMR, and HPV vaccines were 0.76, 0.62, and 0.65, respectively. Greater scores represent more positive attitudes toward the vaccines. |
| Intention to encourage others to vaccinate against the flu | How likely, if at all, are you to encourage others to get the flu vaccine during this flu season? “Very likely” (1), “Somewhat likely” (2), “Not too likely” (3), “Not likely at all” (4). (reversed) Greater scores represent greater likelihood of encouraging vaccination. (asked in Wave 2, 3, and 4). Note that the question had an additional response option in Wave 4, which was “I already did”. For comparability, these respondents were imputed with the highest likelihood of encouraging others “Very likely” as they have already done it. |
| Actual vaccination behavior against the flu | Have you gotten the flu vaccine this season or not? Yes (1), No (0). Those who got the flu shot at Wave 1 were not asked this question at Wave 2, and so on with W3 and W4. Timing of vaccination across the waves was also accounted for in the analysis. |
In questions with ordinal response options, the response options were randomized to be either in increasing or decreasing order to each half of the sample. Varying the presentation of the scales was a safeguard against response biases. Numbers in parentheses indicate the coding of each response option in the dataset.
Both the average and the median sample age was 48 years. Males (48%) and females (52%) were represented in balanced way. Racial groups were proportionally represented, although not perfectly, with Whites constituting 62% of the sample. The median income ranged from $50,000 to $59,999. Weighted distributions of key demographic variables (i.e. age, sex, race, and income) did not differ greatly from unweighted results and closely matched the census estimates (SI-1). The one exception was an inexact match between our sample and the latest census estimates for education. Among respondents of 25 years of age or older (excluding most college students), 49% had at least a college degree.6
Measures
All questions and operationalization details about question wording, response options, coding, and reliability scores, are provided in second section in Table 1. Frequency distributions and other summary statistics appear in SI-1. We formulated most of the questions after extensive piloting, and relied on and adopted validated measures of philosophical beliefs (Shen et al., 2009) and moral beliefs obtained from prior research (Poushter, 2014). We asked respondents questions about the vaccines against the flu, MMR, and HPV.7 These questions concerned attitudes toward the vaccines with two classic (i.e. perceived vaccine risk and positive evaluation of the vaccine) items that had good item-total correlations (Ajzen and Fishbein, 1980; Albarracín, 2020). These two items provide a comprehensive account of vaccine attitudes by tapping both cognitive and affective components, respectively. In the case of the flu vaccine, we also measured intentions to encourage others to get the vaccines and whether the respondent received the vaccine.8 Additionally, we asked a series of demographic questions including whether respondents were parents of children and political ideology (Table 1). Finally, we asked whether respondents’ religion had an explicit mandate against vaccination and if so, whether they followed it, although these were not included in the theoretical model.9
Panel attrition
Attrition analyses were conducted to compare sample composition across the four waves of the study with a focus on both demographic variables and the theoretical variables in our model (Figure 1). The demographic composition of different waves was similar as judged by nonsignificant differences in age, gender, education, income and race. For other variables, the great majority did not display any significant differences between those who dropped out and remained in the panel. Only two differences emerged. First, those who dropped out at Wave 3 had relatively lower HPV positive attitude (i.e. positivity towards the vaccine item) scores in Wave 2 than those who remained. Specifically, among Wave 2, 23% of those who returned to Wave 3 and 29% of those who did not stated that they felt somewhat or very negative towards the HPV vaccine, F(1, 2432) = 11.01, p = 0.001). Second, those who dropped out at Wave 2 had higher flu vaccine risk perceptions in Wave 1 than those who remained. That is, among Wave 1 respondents 30% of those who returned but 36% of those who dropped out at Wave 2 stated that the flu vaccine is somewhat or very risky, F(1, 2996) = 4.36, p = 0.04. However, these two differences were not paralleled by differences in the overall attitude index, intentions, behavior, or religious beliefs, leading to our conclusion that attrition was mostly random (SI-5).
Analytical strategy
Using the lavaan package in R (Rosseel et al., 2021), we conducted longitudinal Structural Equation Models (SEM) with latent factors and autoregressive effects to test our theoretical model. The SEM approach allowed us to gauge the manner in which affiliations and philosophical and moral beliefs might predict vaccine attitudes and behaviors over time. In these models, religious affiliations were positioned as exogeneous predictors of moral and philosophical views. The moral belief latent factor had three indicators and the philosophical beliefs latent factor had two indicators.10 These two latent factors then predict vaccine attitudes, which is itself a latent factor with two indicators (perceived risk of the vaccine and positive evaluation of the vaccine). This vaccine attitude factor in turn predicts the respondents’ (a) intentions to encourage others to vaccinate against the flu and (b) their actual flu vaccine behavior. Because intention and behaviors were only measured for the flu vaccine, we tested the analytical model in Figure 1a for the flu vaccine and the model in Figure 1b for the MMR and HPV vaccines. Each model controlled for the demographics and political ideology. The correlation matrix is in SI-2.
We ran the models with all religious affiliations entered as separate dummy variables (1 indicates that the participant was affiliated with that group and 0 that they were not). Because we had numerous religious groups with small representations, to maximize model fit, we combined a few of the affiliations based on similarity in their philosophical and moral beliefs and the broader religious categories they were part of: Catholics and Orthodox were combined into single category and Buddhists and Hindu were combined into another single category. Hence, the following groups were coded with dummy variables and each of them entered as exogeneous variable into the SEM: (1) Protestants, (2) Roman Catholics and Orthodox Catholics, (3) Mormon, (4) Just Christians, (5) Muslim, (6) Jewish, (7) Buddhists and Hindus, (8) Unitarian, (9) Other, (10) Agnostic, (11) Nothing in particular. Atheist respondents constituted a fairly large portion of our respondents (16%); although they were not the normative category their size was higher than numerous other groups, such as Muslims, Buddhists, and Hindus.11 Atheist was chosen as the reference category because atheists may differ from other respondents both theoretically and empirically (Shimron, 2021).
For the flu vaccine model, we tested our models fully longitudinally over four waves: demographics and religious affiliations (Wave 1), philosophical and moral beliefs (Wave 2), vaccine attitudes (Wave 3), and intentions/behaviors (to encourage flu vaccination and to receive the flu vaccine) (Wave 4). All attitudes and behavior variables were fitted across all times and wave number was included to properly incorporate time, which was an important goal of the longitudinal design to capture changes in attitudes toward vaccines and actual flu vaccination. For MMR and HPV as well, we longitudinally tested vaccine attitudes in Wave 2 and 3 and the coding was done in the same manner as for the flu vaccine analyses.
The models in Figure 1a (flu) and 1B (MMR and HPV) were fit to the variance-covariance matrices. We reported four model fit indices (the chi-square goodness of fit test, root mean square error of approximation—RMSEA, comparative fit index—CFI, standardized version of root mean square residuals—SRMS) (Kline, 2016).12 Given our categorical outcome variable (vaccine behavior), to be consistent across models, we employed diagonally weighted least squares estimation but also replicated the analyses with maximum likelihood estimation.
Additionally, we also used analysis of covariance (ANCOVA) to cross-sectionally compare beliefs, attitudes, intentions, and behaviors as a function of religious affiliations (all pairwise differences) while controlling for demographic differences and political ideology.13 These analyses reported in SI-6 provide supplementary evidence for all pairwise religious affiliation differences.
The data, code, and Supporting Information Files (Online Appendices) are provided in anonymized Open Science Framework (OSF) depository.14
Results
The sample included a variety of religious groups that represent the religious diversity of the U.S, specifically 877 Protestants (29%), 574 Roman Catholics (19%), 515 Just Christian (Nondenominational Christian, 17%), 343 Nothing in Particular (11%), 192 Agnostics (6%), 189 Atheists (6%), 71 Other (2%), 64 Jews (2%), 45 Buddhists (2%), 40 Mormons (1%), 32 Muslims (1%), 25 Unitarians (1%), and 15 Orthodox Catholics (less than 1%). When asked directly (see Table 1), only 3% (N = 67) of respondents reported that their religion forbids vaccination (mostly Roman Catholic and Protestant respondents), and only half of those 67 respondents (N = 30, 2% of the total sample) reported that they followed that mandate.
SEM solutions in Figure 1a and b had an acceptable model fit for all three vaccines. The model fits were acceptable for all flu (Chi-square, χ2 (364) = 1048.305, p < 0.001; RMSEA = 0.033 (0.031, 0.035); CFI = 0.989; SRMS = 0.031), MMR (Chi-square, χ2 (147) = 345.992, p < 0.001; RMSEA = 0.026 (0.022, 0.029); CFI = 0.978; SRMS = 0.022), and HPV models (Chi-square, χ2 (147) = 296.350, p < 0.001; RMSEA = 0.023 (0.019, 0.026); CFI = 0.985; SRMS = 0.020). The chi-square indexes were significant, which is common with large samples, but, more importantly, the RMSEA and the SRMR indicated good fit. All latent factors (moral beliefs, philosophical beliefs, and vaccine attitudes) in all three vaccines had moderate to strong factor loadings, with majority of standardized coefficients ranging from 0.50 to 0.92, only one loading being 0.44 (top panel in Table 2), and all loadings being significant. Moral and philosophical beliefs covaried significantly and strongly for the flu vaccine model (r = 0.76, Table 2) and weakly for MMR and HPV vaccine (r = 0.33 and r = 0.09, Table 2). In addition, according to simple correlations, all of the items comprising philosophical and moral beliefs were positively correlated with each other, and philosophical and moral beliefs indexes were positively correlated as well (r = 0.28, p < 0.01, see Table B1 in Supporting Information 2). These results suggest that, generally, the direction of association of vaccine beliefs and behaviors with philosophical and moral beliefs is the same.
Table 2.
Standardized coefficients for factor loadings, paths, and covariances in the longitudinal autoregressive models.
| Row # | Factor loadings | Flu vaccine model | MMR vaccine model | HPV vaccine model |
|---|---|---|---|---|
| Std. Coef. (se) | Std. Coef. (se) | Std. Coef. (se) | ||
| 1 | Philosophical 1 (W2) by philosophical beliefs (W2) | 0.45 (0.00) | 0.51 (0.00) | 0.56 (0.00) |
| 2 | Philosophical 2 (W2) by philosophical beliefs (W2) | 0.42*** (0.04) | 0.57*** (0.05) | 0.65*** (0.06) |
| 3 | Moral 1 (W2) by moral beliefs (W2) | 0.52 (0.00) | 0.54 (0.00) | 0.54 (0.00) |
| 4 | Moral 2(W2) by moral beliefs (W2) | 0.71*** (0.05) | 0.75*** (0.05) | 0.77*** (0.05) |
| 5 | Moral 3 (W2) by moral beliefs (W2) | 0.78*** (0.06) | 0.82*** (0.06) | 0.81*** (0.06) |
| 6 | Vaccine attitude 1 (W2) by vaccine attitudes (W2) | 0.68 (0.00) | 0.69 (0.00) | 0.72 (0.00) |
| 7 | Vaccine attitude 2 (W2) by vaccine attitudes (W2) | 0.89*** (0.03) | 0.62*** (0.05) | 0.64*** (0.05) |
| 8 | Vaccine attitude 1 (W3) by vaccine attitudes (W3) | 0.66 (0.00) | 0.68 (0.00) | 0.72 (0.00) |
| 9 | Vaccine attitude 2 (W3) by vaccine attitudes (W3) | 0.91*** (0.03) | 0.65*** (0.05) | 0.66*** (0.05) |
| 10 | Vaccine attitude 1 (W4) by vaccine attitudes (W4) | 0.66 (0.00) | ||
| 11 | Vaccine attitude 2 (W4) by vaccine attitudes (W4) | 0.92*** (0.04) | ||
| Paths | ||||
| 12 | Age (W1) → Philosophical beliefs (W2) | 0.02 (0.00) | −0.01 (0.00) | −0.01 (0.00) |
| 13 | Female (W1) → Philosophical beliefs (W2) | 0.05† (0.02) | 0.05† (0.03) | 0.10** (0.03) |
| 14 | White (W1) → Philosophical beliefs (W2) | −0.10*** (0.03) | −0.22*** (0.03) | −0.16*** (0.04) |
| 15 | Education (W1) → Philosophical beliefs (W2) | −0.10** (0.04) | −0.22*** (0.06) | −0.18*** (0.07) |
| 16 | Income (W1) → Philosophical beliefs (W2) | −0.15*** (0.05) | −0.16*** (0.06) | −0.13*** (0.08) |
| 17 | Parent (W1) → Philosophical beliefs (W2) | 0.08** (0.04) | 0.08* (0.05) | 0.08* (0.05) |
| 18 | Conservative (W1) → Philosophical beliefs (W2) | 0.39*** (0.01) | 0.31*** (0.02) | 0.33*** (0.02) |
| 19 | Protestant (W1) → Philosophical beliefs (W2) | 0.36* (0.14) | 0.33† (0.18) | 0.36† (0.22) |
| 20 | Catholic-Orthodox (W1) → Philosophical beliefs (W2) | 0.19 (0.14) | 0.23 (0.18) | 0.24 (0.21) |
| 21 | Mormon (W1) → Philosophical beliefs (W2) | 0.09† (0.17) | 0.02 (0.20) | 0.02 (0.23) |
| 22 | Just Christian (W1) → Philosophical beliefs (W2) | 0.33* (0.15) | 0.35* (0.19) | 0.34* (0.22) |
| 23 | Muslim (W1) → Philosophical beliefs (W2) | 0.14* (0.21) | 0.14* (0.26) | 0.14* (0.31) |
| 24 | Jewish (W1) → Philosophical beliefs (W2) | 0.04 (0.14) | 0.07 (0.19) | 0.07 (0.23) |
| 25 | Buddhist-Hindu (W1) → Philosophical beliefs (W2) | 0.08 (0.15) | 0.09 (0.20) | 0.09 (0.24) |
| 26 | Unitarian (W1) → Philosophical beliefs (W2) | 0.00 (0.15) | 0.00 (0.20) | 0.00 (0.25) |
| 27 | Other (W1) → Philosophical beliefs (W2) | 0.08 (0.16) | 0.09 (0.21) | 0.12† (0.25) |
| 28 | Agnostic (W1) → Philosophical beliefs (W2) | −0.02 (0.13) | 0.01 (0.17) | 0.00 (0.20) |
| 29 | Nothing in particular (W1) → Philosophical beliefs (W2) | 0.08 (0.14) | 0.14 (0.18) | 0.16 (0.21) |
| 30 | Age (W1) → Moral beliefs (W2) | 0.16*** (0.00) | 0.15*** (0.00) | 0.13*** (0.00) |
| 31 | Female (W1) → Moral beliefs (W2) | 0.04 (0.01) | 0.03 (0.01) | 0.02 (0.01) |
| 32 | White (W1) → Moral beliefs (W2) | −0.08* (0.02) | −0.07* (0.02) | −0.07* (0.02) |
| 33 | Education (W1) → Moral beliefs (W2) | −0.07* (0.03) | −0.03 (0.03) | −0.03 (0.03) |
| 34 | Income (W1) → Moral beliefs (W2) | −0.13*** (0.03) | −0.10** (0.03) | −0.09** (0.03) |
| 35 | Parent (W1) → Moral beliefs (W2) | 0.06* (0.02) | 0.07* (0.02) | 0.07* (0.02) |
| 36 | Conservative (W1) → Moral beliefs (W2) | 0.36*** (0.01) | 0.34*** (0.01) | 0.36*** (0.01) |
| 37 | Protestant (W1) → Moral beliefs (W2) | 0.38* (0.10) | 0.38* (0.10) | 0.36* (0.10) |
| 38 | Catholic-Orthodox (W1) → Moral beliefs (W2) | 0.21 (0.10) | 0.20 (0.10) | 0.18 (0.10) |
| 39 | Mormon (W1) → Moral beliefs (W2) | 0.13* (0.13) | 0.16** (0.13) | 0.16** (0.13) |
| 40 | Just Christian (W1) → Moral beliefs (W2) | 0.31* (0.10) | 0.30* (0.10) | 0.30* (0.10) |
| 41 | Muslim (W1) → Moral beliefs (W2) | 0.15* (0.15) | 0.14* (0.14) | 0.14* (0.14) |
| 42 | Jewish (W1) → Moral beliefs (W2) | 0.05 (0.10) | 0.02 (0.10) | 0.02 (0.10) |
| 43 | Buddhist-Hindu (W1) → Moral beliefs (W2) | 0.07 (0.11) | 0.05 (0.10) | 0.04 (0.10) |
| 44 | Unitarian (W1) → Moral beliefs (W2) | −0.01 (0.11) | 0.00 (0.11) | 0.00 (0.10) |
| 45 | Other (W1) → Moral beliefs (W2) | 0.08 (0.11) | 0.06 (0.11) | 0.06 (0.11) |
| 46 | Agnostic (W1) → Moral beliefs (W2) | −0.02 (0.09) | −0.02 (0.09) | −0.01 (0.09) |
| 47 | Nothing in particular (W1) → Moral beliefs (W2) | 0.02 (0.09) | 0.01 (0.09) | 0.02 (0.09) |
| 48 | Philosophical beliefs (W2) → Vaccine attitudes (W2) | −10.88*** (0.13) | −0.73*** (0.06) | −0.45*** (0.04) |
| 49 | Moral beliefs (W2) → Vaccine attitudes (W2) | 10.42*** (0.23) | 0.18*** (0.07) | −0.15*** (0.05) |
| 50 | Vaccine attitudes (W2) → Vaccine attitudes (W3) | 0.99*** (0.02) | 0.96*** (0.05) | 0.94*** (0.05) |
| 51 | Vaccine attitudes (W3) → Vaccine attitudes (W4) | 0.96*** (0.02) | ||
| 52 | Philosophical beliefs (W2) → Vaccine behavior (W2) | −10.20*** (0.07) | ||
| 53 | Moral beliefs (W2) → Vaccine behavior (W2) | 10.08*** (0.13) | ||
| 54 | Vaccine behavior (W2) → Vaccine behavior (W3) | 0.75*** (0.02) | ||
| 55 | Vaccine behavior (W3) → Vaccine behavior (W4) | 0.92*** (0.03) | ||
| 56 | Vaccine attitudes (W2) → Vaccine behavior (W3) | 0.19*** (0.02) | ||
| 57 | Vaccine attitudes (W3) → Vaccine behavior (W4) | 0.06* (0.03) | ||
| 58 | Philosophical beliefs (W2) → Encourage others (W2) | −10.43*** (0.18) | ||
| 59 | Moral beliefs (W2) → Encourage others (W2) | 10.22*** (0.35) | ||
| 60 | Encourage others (W2) → Encourage others (W3) | 0.79*** (0.09) | ||
| 61 | Encourage others (W3) → Encourage others (W4) | 10.01*** (0.11) | ||
| 62 | Vaccine attitudes (W2) → Encourage others (W3) | 0.19** (0.14) | ||
| 63 | Vaccine attitudes (W3) → Encourage others (W4) | −0.04 (0.18) | ||
| Covariances | ||||
| 64 | Philosophical beliefs (W2) with moral beliefs (W2) | 0.76*** (0.00) | 0.33*** (0.00) | 0.09† (0.00) |
| 65 | Vaccine attitude 1 (W2) with vaccine attitude 1 (W3) | 0.38*** (0.02) | 0.03 (0.02) | 0.08 (0.03) |
| 66 | Vaccine attitude 1 (W2) with vaccine attitude 1 (W4) | 0.40*** (0.02) | ||
| 67 | Vaccine attitude 1 (W3) with vaccine attitude 1 (W4) | 0.40*** (0.02) | ||
| 68 | Vaccine attitude 2 (W2) with vaccine attitude 2 (W3) | −0.13 (0.03) | 0.32*** (0.02) | 0.33*** (0.03) |
| 69 | Vaccine attitude 2 (W2) with vaccine attitude 2 (W4) | −0.12 (0.03) | ||
| 70 | Vaccine attitude 2 (W3) with vaccine attitude 2 (W4) | −0.14 (0.03) | ||
| 71 | Encourage others (W2) with encourage others (W3) | −0.30* (0.06) | ||
| 72 | Encourage others (W2) with encourage others (W4) | −0.07 (0.05) | ||
| 73 | Encourage others (W3) with encourage others (W4) | −0.45** (0.06) | ||
| 74 | Encourage others (W2) with vaccine behavior (W2) | 0.30*** (0.01) | ||
| 75 | Encourage others (W3) with vaccine behavior (W3) | 0.28*** (0.01) | ||
| 76 | Encourage others (W4) with vaccine behavior (W4) | 0.18 (0.02) | ||
Significance levels for first items in factor loadings are not shown as they are set to variance 1. Reference: Atheist. Standardized coefficients are shown representing STDYX standardization. As clarified in Table 1, Philosophical 1 is disease item, Philosophical 2 is health item, Moral 1 is drugs item, Moral 2 is marriage item, Moral 3 is high school sex item, Attitude 1 is risk perception about vaccine, Attitude 2 is positivity about vaccine. Encourage Others is intention to encourage others to get the flu vaccine.
p < 0.10. *p < 0.05. **p < 0.01. ***p < 0.001.
Across the models, the variance in vaccine attitudes explained by philosophical and moral beliefs was 0.99 for the flu vaccine, 0.43 for the MMR vaccine, and 0.27 for the HPV vaccine at Wave 2, and 0.97 for the flu vaccine, 0.93 for the MMR vaccine, and 0.89 for the HPV vaccine at Wave 3, and 0.92 for the flu vaccine at Wave 4. Also, the variance in flu vaccine behavior explained by attitudes was 0.40, 0.77, and 0.93 for the Waves 2, 3, and 4, respectively (SI-7). The results of the models are not shown in a figure due to large number of coefficients, but are provided in Table 2, and indirect effects are provided in SI-3. These analyses led to the following results.
First, we found that religious affiliations predicted moral and philosophical beliefs and these results were consistent across the three vaccines (see center panel in Paths section in Table 2). For philosophical views (e.g. that health is controlled by God), we found that identifying as Protestant, Just Christian, and Muslim had consistently stronger beliefs, and Mormons tended have stronger beliefs in the case of the flu vaccine. Particularly, identifying as Just Christian had the stronger positive association with philosophical views (e.g. for flu, β = 0.33, se = 0.15, p < 0.05, Table 2, row 22). For moral beliefs (e.g. premarital sex is immoral), we observed a very similar pattern. Identifying as Protestant (e.g. for HPV, β = 0.36, se = 0.10, p < 0.05, Table 2, row 37), and to a lesser extent Just Christian, Muslim, and Mormon had consistently positive and significant associations with moral beliefs. We also note that these effects were stronger and more of them were positive when political ideology was not controlled for, showing the importance of ideology in association with religion.15 Additionally, having a higher income, being a parent, and being more conservative predicted stronger philosophical and moral beliefs.
Second, we found that philosophical and moral beliefs had different contributions to vaccine attitudes and intention/behaviors, and this differed across vaccine types. On the one hand, stronger philosophical beliefs (e.g. that health is controlled by God) predicted more negative vaccine attitudes consistently across the models (Table 2, row 48). On the other hand, moral beliefs (e.g. that premarital sex is immoral) were negatively associated with attitudes toward the HPV vaccine (β = −0.15, se = 0.03, p < 0.001, Table 2, row 49) but positively with attitudes towards the flu and MMR vaccines. For the flu vaccine, this association was similar for intentions to encourage vaccination and actual vaccination as well. Stronger philosophical beliefs predicted weaker intention to encourage others to vaccinate as well as less actual vaccination, whereas stronger moral beliefs predicted stronger intention to encourage vaccination as well as more vaccination (e.g. for Moral Belief—Vaccine Behavior, β = 1.08, se = 0.13, p < 0.001, Table 2, row 53).
Third, we found a positive association between attitude toward the flu vaccine and actual vaccination. Vaccine attitudes at Waves 2 and 3 predicted vaccination behavior at Waves 3 and 4, respectively (e.g. Vaccine Attitude W2—Vaccine Behavior W3, β = 0.19, se = 0.02, p < 0.001, Table 2, row 56). The association between attitudes and intention to encourage vaccination was only positive and significant going from Wave 2 to 3 but not from Wave 3 to 4.16
There were also numerous albeit small indirect effects for which the full results are provided in SI-3. Most of the indirect effects were observed only for the affiliation—religious belief—vaccine attitude path.
Discussion
Vaccine mandates and religious exemptions generate extensive policy discussion all over the world. In the U.S., where state level policies determine vaccination requirements, 45 states permit for some form of religious, personal, or philosophical exemption from vaccination (National Conference on State Legislatures, 2019). In the midst of the COVID-19 pandemic and conflicts between respect for religious freedom and public health (Silverman and May, 2001; Stecula et al., 2020), it is important to understand the role that religion plays in vaccine attitudes and related behaviors. Although longstanding research has documented that, overall, religion plays an important role in vaccine attitudes and behaviors (Feder et al., 1993; Rutjens et al., 2021; Williams and O’Leary, 2019; Wombwell et al., 2015), how institutional (religious affiliations) and personal interpretations (religious beliefs) may interact to shape vaccine confidence remains poorly understood. This study contributes to this literature by probing the pathways from affiliations to beliefs to attitudes to behaviors in the contexts of three vaccines and with a nationally representative sample of U.S. adults.
Our findings indicate that although a negligible percentage of respondents stated that their religion opposed vaccination, and only half of those stated that they followed that mandate, religious affiliation was correlated with vaccination attitudes and behavior. In this paper, we both identified religious affiliation differences and explained those associations by examining the mediating role of philosophical and moral beliefs across a four waves of survey data over a period of 6 months. This process allowed us to both empirically control for and test the influence of religious affiliations and religious beliefs on multiple vaccine confidence indicators simultaneously. Some of our findings were in line with previous studies on perceptions of the HPV vaccine (Barnack et al., 2010; Bernat et al., 2009) but described patterns that could generalize to other vaccines (i.e. the flu vaccine and the MMR vaccine).
Other findings were novel. We showed that there are notable differences among religious and non-religious groups such as Atheists, Unitarians and Agnostics and some among religious groups as well: SEM results showed that Protestant, Just Christian (Nondenominational Christian), and Muslim had both stronger philosophical and moral beliefs, while additionally, Mormons had also stronger moral beliefs.17 We also showed that stronger philosophical views predicted greater vaccine hesitancy, both in terms of attitudes toward vaccines as well as behavior. These results contribute to the prior evidence showing a positive association between philosophical beliefs and vaccine hesitancy (Browne et al., 2015; Rutjens et al., 2021; Thomas et al., 2012) and indicating important affiliation differences when it comes to philosophical beliefs.
However, the association between moral beliefs and vaccine attitudes differed across vaccines. As might be expected, moral beliefs, which in this case concern premarital sex, consistently predicted negative vaccine attitudes toward the HPV vaccine (Shelton et al., 2013; Thomas et al., 2012). Yet, moral beliefs were associated with positive attitudes toward the flu and MMR vaccines as well as greater vaccination against the flu. The way we measured moral beliefs could also partly explain this finding. The moral beliefs measure comprised a mixture of items that both tapped vaccine-relevant issues (e.g. premarital and teen sex in relation to HPV being sexually transmitted infection). They also provided a more generalizable moral beliefs measure given the breadth of moral issue dimensions, making the measure more applicable to vaccines outside of the HPV vaccine. Also, the differential weight of moral beliefs across vaccines reminds us that vaccines and populations are unique. At large, these variations underscore the complexity and multidimensionality of moral beliefs and how they might contribute to vaccine hesitancy, something future research could investigate. One interesting area to understand is whether and how moral religious beliefs interact with the influence of perceived (religious) norms and altruism in religious communities, which could explain positive associations with positive attitudes toward some vaccines (Pessi, 2011).
We also demonstrated that vaccine attitudes subsequently shaped related intentions to encourage others to get the vaccine—and behaviors—actual vaccination against the flu (Ajzen et al., 2019; Albarracín, 2020; Albarracín et al., 2001; Glasman and Albarracín, 2006). Our study is the first to uncover differences in vaccine attitudes and behaviors among religious affiliations and to consider the (mediating) role of different religious beliefs in this process. This aspect furthers our understanding of both the identity-based (religious affiliation) and cognitive dimensions (religious beliefs) in the structure of attitudes toward vaccines (cf. Krosnick et al., 1993). Additionally, the longitudinal model in this study strengthens the inference about a casual element in the demonstrated effects. It shows religious cognitions as antecedents of religious affiliation and demographic variables, which then shape vaccine attitudes and behaviors.
Although many studies focused on the role of religion in vaccination decisions, particularly in the case of HPV, much less is known about the role of religious beliefs concerning vaccines in general. We hypothesized and found evidence that religious identity shapes vaccine attitudes and behaviors through philosophical and moral beliefs about health and disease management. These philosophical and moral beliefs were previously hypothesized to be in conflict with the premises of vaccine technology (Gargano et al., 2013; Reynolds, 2014; Sporton and Francis, 2001). Thus, these results also speak to the individual differences in how people perceive and practice their religious affiliations when they form beliefs about vaccines. Second, our finding calls for greater focus on the mediating role of philosophical and moral beliefs and suggests a degree of interpretational malleability in religion-based attitudes. For example, health campaigns could focus on such beliefs instead of religious identity, as messages on identity may backfire more easily because of defensive psychological processes (Kahan, 2017). Messages could target religious beliefs more precisely and frame vaccination recommendations in ways that highlight compatibility with (or absence of direct antagonism toward) religious attitudes. It is also important to not essentialize religious identities or isolate them by pinpointing blame in the public discourse on vaccine hesitancy, a topic we discuss at greater length below. Moreover, our mixed findings pertaining to moral beliefs suggest the need for customized messages targeting vaccine attitudes versus uptake.
Our results also highlight the potential challenges for the acceptance of the COVID-19 vaccines. Of relevance to this topic, religious ceremonies (e.g. funerals, holy days) attended during the COVID lockdowns and public gathering bans, have been cited as key early community transmission hotspots as seen with Orthodox Jews in New York, Liberty University in Virginia, Shia shrines in Iran, and Shincheonji Church of Jesus in South Korea (ABC News, 2020). Moreover, because scientifically-unproven COVID-19 remedies touted by some religious and spiritual leaders potentially undercut the disposition to accept medicinal interventions among adherents, they deserve attention as well (Stewart, 2020; Yee, 2020). The generalizability of our results across three very different vaccines gives our findings relevance to efforts to vaccine against COVID-19. If communities are to achieve and maintain community immunity against COVID-19, a process that will require periodic booster shots, reaching vaccine hesitant communities is important.
Finally, it is important to not essentialize demographic groups such as religious affiliation groups and race. These measurements are a snapshot of the U.S. population in time and might not be generalizable across other geographies and time. For example, the impact of historical failures such as the U.S. Public Health System’s Tuskegee Syphilis Study on marginalized groups is important to keep in mind (Quinn et al., 2016). Similarly, equitable access to vaccines for all sociodemographic groups should come first to avoid overattributing lack of vaccination to cultural values or specific religious, racial, or ethnic minorities (Dembosky, 2021). Countries differ widely in the role of religion in society, social and political culture, the influence of religious leaders, and the historical background of religion. The plummeting MMR vaccination rates in Indonesia in response to a fatwa by Muslim clerics (Rochmyaningsih, 2018) is an important example. A U.S. intelligence agency admitted to collecting DNA samples during vaccination campaigns in Pakistan, which led to religious fatwas opposing vaccination within a complex social and political context (Iqbal, 2021). Future research should consider religious factors in tandem with other social and political issues.
Limitations and Future Research. Specific beliefs about religion span a wide range of issues beyond those tapped by our questions. Our focus here was not exhaustive. Other specific religion-related concerns about vaccines include use (or prior use) of human fetuses and gelatin in the vaccine production process and its final contents (Wombwell et al., 2015). Second, our measures of philosophical and moral are imperfect. Our philosophical belief measure tapped into only fate-related beliefs. One of our moral beliefs items is about using drugs, which is about health but may be less relevant to vaccination. Still, because we prioritized more generalizable health-relevant religious concepts as opposed to vaccine-relevant concepts only, we retained this item in the analysis. Future research might build on our findings by examining a larger range of items and religious beliefs as well as probing their potential interactions.
With a large-scale survey, we were able to track national patterns, which is a strength of our design. However, we were able to model respondents’ vaccine behavior only for the flu vaccine because decisions on the other two vaccines were likely not made by the adults in our study but by their parents. Finally, we combined some of the small-size religious and racial groups during the analysis for various statistical procedures. While there is ample research on specific religious communities and vaccination, studies should also oversample and focus on diverse race groups as well (Freimuth et al., 2017; Quinn et al., 2016) as these demographics predict important differences in COVID-19 related health protective behaviors (Breakwell et al., 2021). Future research should examine distinctions within affiliations too, such as between Orthodox Jews and other Jews.
Conclusion
Understanding the role of religious affiliations and beliefs in vaccine attitudes and behaviors is important both at the individual level but also at the macro level given the policy discussions on religious freedoms and exemptions. Since micro and macro level processes influence each other, greater vaccine hesitancy in the public could facilitate anti-vaccine policy-making that gives more weight to religious freedom in the public space at the expense of public health. Our findings suggest that some religious beliefs, particularly philosophical ones, are perceived to be in conflict with the premises of vaccines, which in turn fuels negative attitudes toward three different vaccines. These attitudes matter, as they predict both vaccination behavior and intention to encourage others to vaccinate (i.e. in the case of the flu vaccine) and they do so longitudinally over a span of 6 months. Findings suggest that the next generation of messages designed to increase vaccination should target religious beliefs more precisely. As the roll out of COVID-19 vaccines and booster shots raises questions regarding vaccinate mandates and religious reservations, our findings can help inform the discussion.
Research Data
This article is distributed under the terms of the Creative Commons Attribution 4.0 License (https://creativecommons.org/licenses/by/4.0/) which permits any use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access pages (https://us.sagepub.com/en-us/nam/open-access-at-sage).
sj-docx-2-hpq-10.1177_13591053221082770 for Religious affiliation and philosophical and moral beliefs about vaccines: A longitudinal study by Ozan Kuru, Man-pui Sally Chan, Hang Lu, Dominik Andrzej Stecula, Kathleen Hall Jamieson and Dolores Albarracín in Journal of Health Psychology
Supplemental material, sj-docx-8-hpq-10.1177_13591053221082770 for Religious affiliation and philosophical and moral beliefs about vaccines: A longitudinal study by Ozan Kuru, Man-pui Sally Chan, Hang Lu, Dominik Andrzej Stecula, Kathleen Hall Jamieson and Dolores Albarracín in Journal of Health Psychology
This article is distributed under the terms of the Creative Commons Attribution 4.0 License (https://creativecommons.org/licenses/by/4.0/) which permits any use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access pages (https://us.sagepub.com/en-us/nam/open-access-at-sage).
sj-jasp-3-hpq-10.1177_13591053221082770 for Religious affiliation and philosophical and moral beliefs about vaccines: A longitudinal study by Ozan Kuru, Man-pui Sally Chan, Hang Lu, Dominik Andrzej Stecula, Kathleen Hall Jamieson and Dolores Albarracín in Journal of Health Psychology
This article is distributed under the terms of the Creative Commons Attribution 4.0 License (https://creativecommons.org/licenses/by/4.0/) which permits any use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access pages (https://us.sagepub.com/en-us/nam/open-access-at-sage).
sj-R-6-hpq-10.1177_13591053221082770 for Religious affiliation and philosophical and moral beliefs about vaccines: A longitudinal study by Ozan Kuru, Man-pui Sally Chan, Hang Lu, Dominik Andrzej Stecula, Kathleen Hall Jamieson and Dolores Albarracín in Journal of Health Psychology
This article is distributed under the terms of the Creative Commons Attribution 4.0 License (https://creativecommons.org/licenses/by/4.0/) which permits any use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access pages (https://us.sagepub.com/en-us/nam/open-access-at-sage).
sj-sav-4-hpq-10.1177_13591053221082770 for Religious affiliation and philosophical and moral beliefs about vaccines: A longitudinal study by Ozan Kuru, Man-pui Sally Chan, Hang Lu, Dominik Andrzej Stecula, Kathleen Hall Jamieson and Dolores Albarracín in Journal of Health Psychology
This article is distributed under the terms of the Creative Commons Attribution 4.0 License (https://creativecommons.org/licenses/by/4.0/) which permits any use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access pages (https://us.sagepub.com/en-us/nam/open-access-at-sage).
sj-sav-7-hpq-10.1177_13591053221082770 for Religious affiliation and philosophical and moral beliefs about vaccines: A longitudinal study by Ozan Kuru, Man-pui Sally Chan, Hang Lu, Dominik Andrzej Stecula, Kathleen Hall Jamieson and Dolores Albarracín in Journal of Health Psychology
This article is distributed under the terms of the Creative Commons Attribution 4.0 License (https://creativecommons.org/licenses/by/4.0/) which permits any use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access pages (https://us.sagepub.com/en-us/nam/open-access-at-sage).
sj-sps-1-hpq-10.1177_13591053221082770 for Religious affiliation and philosophical and moral beliefs about vaccines: A longitudinal study by Ozan Kuru, Man-pui Sally Chan, Hang Lu, Dominik Andrzej Stecula, Kathleen Hall Jamieson and Dolores Albarracín in Journal of Health Psychology
This article is distributed under the terms of the Creative Commons Attribution 4.0 License (https://creativecommons.org/licenses/by/4.0/) which permits any use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access pages (https://us.sagepub.com/en-us/nam/open-access-at-sage).
sj-xlsx-5-hpq-10.1177_13591053221082770 for Religious affiliation and philosophical and moral beliefs about vaccines: A longitudinal study by Ozan Kuru, Man-pui Sally Chan, Hang Lu, Dominik Andrzej Stecula, Kathleen Hall Jamieson and Dolores Albarracín in Journal of Health Psychology
Acknowledgments
We thank the survey administration team 2018–2019 ASK (Annenberg Science Knowledge) Group which included Ozan Kuru, PhD, Dominik Stecula, PhD, Hang Lu, PhD, Yotam Ophir, PhD, Sally Chan, PhD, Ken Winneg, PhD, Kathleen Hall Jamieson, PhD, and Dolores Albarracin, PhD.
In contrast, the intensity of religiosity (such as frequency of praying, adherence to all practices) has been found to be not significantly associated with teenage females’ vaccination (Reynolds, 2014).
Given the exploratory question about differences across religious affiliations and the use of a path model for our prediction, we do not formally state or numerate specific hypotheses.
Our primary interest concerned the pathways in this model. We did not hypothesize differences between three distinct vaccines but treated the multi-vaccine data as a self-replication and vaccine-generalizability robustness test.
Measurement models differed slightly across vaccines. We did not have sufficient statistical power to analyze MMR and HPV vaccination among the respondents’ children although we asked parents to report on their children’s vaccination. Whether respondents themselves had the MMR and HPV vaccines was not measured since the respondents’ parents/caretakers, not themselves, were involved in that decision.
As, by law, the U.S. Census does not include any question about religious preferences and affiliations (Pew Research Center, 2010), these figures rely on large nationally representative surveys.
The U.S. Census Bureau 2018 estimates for this group is 35% (United States Census Bureau, 2019). This difference was largely due to a lower survey completion rate among respondents with lower education at Wave 1 (completion rates = 38% and 57% for high school graduates and those with college degree/more, respectively). The survey company NORC successfully employed adaptive targeting (e.g. more incentives, reminders) of this group of respondents in later waves to keep education distribution less skewed (SI-1).
Although there are multiple flu and HPV vaccines, we referred to the general name flu and HPV in singular for simplicity.
Aside from the fact that we cannot meaningfully test vaccine behavior for MMR and HPV, our study also had limited question space due to time-sharing with other questions. For example, for MMR and HPV, we asked the respondents’ intention to encourage others to vaccinate their children but only in one wave. In Wave 4, MMR encouragement intentions were asked but those variables were part of an unrelated experiment (the measures in this study were asked before experimental module in Wave 4).
This question was asked for descriptive purposes and was not in included in model testing due to extremely low variance and lack of a clear theoretical relation with religious beliefs.
We note that the philosophical belief items may correlate with locus of control, self-efficacy (Bandura, 1989) or decision power in the Health Belief Model (Rosenstock, 1974). However, our items are concerned with religious and supernatural forces, which is not the case for self-efficacy.
The cross-sectional ANCOVA analysis (details in SI-6) showed that Atheists had the least vaccine hesitancy across all variables. All pairwise differences among religious affiliations are shown in SI-6 as well.
We assessed chi-square (model fit between the sample and fitted covariance matrices), RMSEA (refers to root mean square error of approximation; 90% Cis are given in parentheses), CFI (comparative fit index) and SRMS (standardized version of root mean square residuals; standardization provides more valuable statistic when measures have different number of response range).
We also document significant pairwise correlations between religious affiliations and our key outcome variables (SI-2).
The reference category in these results was Atheists; SI-6 provides cross-sectional pairwise differences among all religious affiliations as well.
We note that for intentions to encourage others, negative covariances observed at the bottom of Table 2 (intention to encourage others at W2 and W3 as well as at W3 and W4) suggest that path coefficients among intentions to encourage others across waves might not be as strong as estimated.
We also found similar pairwise differences among affiliations in the cross-sectional analysis in SI-6.
Footnotes
Author Contributions: Ozan Kuru contributed to the design, analyzed the data, wrote the first and other drafts of the paper and managed the paper as the first author. Man-pui Sally Chan contributed to the analysis and Dolores Albarracin and Kathleen Hall Jamieson procured funding, contributed to the writing of the paper and the framing of the results. All authors contributed to the design, interpretation of findings, and editions to the manuscript.
The current article includes the complete raw dataset collected in the study including the participants’ data set, syntax file and log files for analysis. These files are available in the Figshare repository and as Supplemental Material on the SAGE Journals platform.
The authors declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: No conflicts of interests. Dr. Ozan Kuru (2018-2020), Dr. Hang Lu (2018-2019), and Dr. Dominik Stecula (2018-2020) worked as postdoctoral fellows at the Annenberg Public Policy Center.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Funding for the current study comes from the Annenberg Public Policy Center, Annenberg Science Knowledge (ASK) surveys to Kathleen Hall Jamieson, and NIH Grants R01 AI147487, DP1 DA048570, and R01MH114847 to Dolores Albarracin.
The study received research oversight approval at the University of Pennsylvania Institutional Review Board.
ORCID iD: Ozan Kuru  https://orcid.org/0000-0002-0485-1705
https://orcid.org/0000-0002-0485-1705
References
- ABC News (2020) Coronavirus: California pastor continues to hold church services in Lodi despite stay-at-home order, citing First Amendment. Available at: https://abc7news.com/church-coronavirus-shelter-in-place-open-door-cross-culture/6071303/ (accessed 14 May 2020).
- Ajzen I, Fishbein M. (1980) Understanding Attitudes and Predicting Social Behavior. Englewood Cliffs, NJ: Prentice-Hall. [Google Scholar]
- Ajzen I, Fishbein M, Lohmann S, et al. (2019) The influence of attitudes on behavior. In: Albarracín D, Johnson BT. (eds) Handbook of Attitudes, VOL 1: Basic Principles, 2nd edn. London: Routledge, pp.197–255. [Google Scholar]
- Albarracín D. (2020) Action and Inaction in a Social World: Predicting and Changing Attitudes and Behaviors. Cambridge: Cambridge University Press. [Google Scholar]
- Albarracín D, Johnson BTBT, Fishbein M, et al. (2001) Theories of reasoned action and planned behavior as models of condom use: A meta-analysis. Psychological Bulletin 127(1): 142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ammerman NT. (2013) Spiritual but not religious? Beyond binary choices in the study of religion. Journal for the Scientific Study of Religion 52(2): 258–278. [Google Scholar]
- Bandura A. (1989) Social cognitive theory. In: Vasta R. (ed.) Annals of Child Development. Six Theories of Child Development, 6th edn. Greenwich, CT: JAI Press, pp.1–60. [Google Scholar]
- Barnack JL, Reddy DM, Swain C. (2010) Predictors of parents’ willingness to vaccinate for human papillomavirus and physicians’ intentions to recommend the vaccine. Women’s Health Issues 20(1): 28–34. [DOI] [PubMed] [Google Scholar]
- Belluz J. (2019) Washington measles outbreak: Why it’s mostly affecting Russian speakers. Vox. Available at: https://www.vox.com/2019/3/19/18263688/measles-outbreak-2019-clark-county (accessed 9 June 2019).
- Bernat DH, Harpin SB, Eisenberg ME, et al. (2009) Parental support for the human papillomavirus vaccine. Journal of Adolescent Health 45(5): 525–527. [DOI] [PubMed] [Google Scholar]
- Bodson J, Wilson A, Warner EL, et al. (2017) Religion and HPV vaccine-related awareness, knowledge, and receipt among insured women aged 18-26 in Utah. PLoS One 12(8): e0183725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breakwell GM, Fino E, Jaspal R. (2021) COVID-19 preventive behaviours in White British and Black, Asian and Minority Ethnic (BAME) people in the UK. Journal of Health Psychology 27(6): 1301–1317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer NT, Fazekas KI. (2007) Predictors of HPV vaccine acceptability: A theory-informed, systematic review. Preventive Medicine 45(2–3): 107–114. [DOI] [PubMed] [Google Scholar]
- Browne M, Thomson P, Rockloff MJ, et al. (2015) Going against the herd: Psychological and cultural factors underlying the ‘vaccination confidence gap’. PLoS One 10(9): e0132562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dembosky A. (2021) It’s not Tuskegee. Current medical racism fuels Black Americans’ vaccine hesitancy. Los Angeles Times, 25 March. Available at: https://www.latimes.com/science/story/2021-03-25/current-medical-racism-not-tuskegee-expls-vaccine-hesitancy-among-black-americans (accessed 5 May 2021).
- Feder GS, Vaclavik T, Streetly A. (1993) Traveller Gypsies and childhood immunization: A study in east London. The British Journal of General Practice: The Journal of the Royal College of General Practitioners 43(372): 281–284. Available at: http://www.ncbi.nlm.nih.gov/pubmed/8398244 (accessed 9 June 2019). [PMC free article] [PubMed] [Google Scholar]
- Fogel J, Ebadi C. (2011) Religious categories and the human papillomavirus (HPV) vaccine: Attitudes, intentions, and behaviors regarding vaccination. Journal of Medical Marketing: Device, Diagnostic and Pharmaceutical Marketing 11(4): 303–311. [Google Scholar]
- Freimuth VS, Jamison AM, An J, et al. (2017) Determinants of trust in the flu vaccine for African Americans and Whites. Social Science and Medicine 193: 70–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gargano LM, Herbert NL, Painter JE, et al. (2013) Impact of a physician recommendation and parental immunization attitudes on receipt or intention to receive adolescent vaccines. Human Vaccines & Immunotherapeutics 9(12): 2627–2633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerede R, Machekanyanga Z, Ndiaye S, et al. (2017) How to increase vaccination acceptance among apostolic communities: Quantitative results from an assessment in three provinces in Zimbabwe. Journal of Religion and Health 56(5): 1692–1700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasman LR, Albarracín D. (2006) Forming attitudes that predict future behavior: A meta-analysis of the attitude-behavior relation. Psychological Bulletin 132(5): 778–822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holman DM, Benard V, Roland KB, et al. (2014) Barriers to human papillomavirus vaccination among US adolescents. JAMA Pediatrics 168(1): 76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt CL, Lewellyn LA, Rathweg MJ. (2016) Exploring religion-health mediators among African American parishioners: Journal of Health Psychology 10(4): 511–527. [DOI] [PubMed] [Google Scholar]
- Iannelli V. (2019) Are there religious exemptions to vaccines? Available at: https://www.verywellfamily.com/religious-exemptions-to-vaccines-2633702 (accessed 9 June 2019).
- Iqbal H. (2021) How the CIA’s fake Hepatitis B vaccine program in Pakistan helped fuel vaccine distrust. Available at: https://www.vox.com/first-person/22256595/vaccine-covid-pakistan-cia-program (accessed 21 December 2021).
- Kahan DM. (2017) Misconceptions, misinformation, and the logic of identity-protective cognition. SSRN Electronic Journal. DOI: 10.2139/ssrn.2973067. [DOI] [Google Scholar]
- Karvinen KH, Carr LJ. (2013) Does the perception that God controls health outcomes matter for health behaviors? Journal of Health Psychology 19(4): 521–530. [DOI] [PubMed] [Google Scholar]
- Kline R. (2016) Methodology in the Social Sciences. Principles and Practice of Structural Equation Modeling, 4th edn. New York, NY: Guilford Press. Available at: https://psycnet.apa.org/record/2015-56948-000 (accessed 9 June 2019). [Google Scholar]
- Krakow MM, Jensen JD, Carcioppolo N, et al. (2015) Psychosocial predictors of human papillomavirus vaccination intentions for young women 18 to 26: Religiosity, morality, promiscuity, and cancer worry. Women’s Health Issues 25(2): 105–111. [DOI] [PubMed] [Google Scholar]
- Krosnick JA, Boninger DS, Chuang YC, et al. (1993) Attitude strength: One construct or many related constructs? Journal of Personality and Social Psychology 65(6): 1132–1151. [Google Scholar]
- Larson HJ, de Figueiredo A, Xiahong Z, et al. (2016) The state of vaccine confidence 2016: Global insights through a 67-country survey. EBioMedicine 12: 295–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Natan MB, Aharon O, Palickshvili S, et al. (2011) Attitude of Israeli mothers with vaccination of their daughters against human papilloma virus. Journal of Pediatric Nursing 26(1): 70–77. [DOI] [PubMed] [Google Scholar]
- National Conference on State Legislatures (2019) States with religious and philosophical exemptions from school immunization requirements. Available at: http://www.ncsl.org/research/health/school-immunization-exemption-state-laws.aspx (accessed 9 June 2019).
- New World Encylopedia (2009) Abrahamic religions. Available at: https://www.newworldencyclopedia.org/entry/Abrahamic_religions (accessed 15 November 2020).
- Olagoke AA, Olagoke OO, Hughes AM. (2021) Intention to vaccinate against the novel 2019 coronavirus disease: The role of health locus of control and religiosity. Journal of Religion and Health 60(1): 65–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Otterman S. (2019) New York confronts its worst measles outbreak in decades. The New York Times. Available at: https://www.nytimes.com/2019/01/17/nyregion/measles-outbreak-jews-nyc.html (accessed 9 June 2019).
- Pessi AB. (2011) Religiosity and altruism: Exploring the link and its relation to happiness. Journal of Contemporary Religion 26(1): 1–18. [Google Scholar]
- Pew Research Center (2010) A brief history of religion and the U.S. census. Available at: https://www.pewforum.org/2010/01/26/a-brief-history-of-religion-and-the-u-s-census/ (accessed 20 December 2021).
- Pew Research Center (2014. a) Religion in America: U.S. religious data, demographics and statistics. Available at: https://www.pewforum.org/religious-landscape-study/ (accessed 20 December 2021).
- Pew Research Center (2014. b) Table: Religious diversity index scores by country. Available at: https://www.pewforum.org/2014/04/04/religious-diversity-index-scores-by-country/ (accessed 20 December 2021).
- Poushter J. (2014) What’s morally acceptable? It depends on where in the world you live. Pew Research Center. Available at: https://www.pewresearch.org/fact-tank/2014/04/15/whats-morally-acceptable-it-depends-on-where-in-the-world-you-live/ (accessed 9 June 2019). [Google Scholar]
- Quinn S, Jamison A, Musa D, et al. (2016) Exploring the continuum of vaccine hesitancy between African American and White adults: Results of a qualitative study. PLoS Currents. Epub ahead of print 29 December 2016. DOI: 10.1371/currents.outbreaks.3e4a5ea39d8620494e2a2c874a3c4201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynolds D. (2014) Religiosity and parental acceptance of human papillomavirus (HPV) vaccine in 9-18 year-old girls. Journal of Christian Nursing: A Quarterly Publication of Nurses Christian Fellowship 31(3): 172–177. Available at: http://www.ncbi.nlm.nih.gov/pubmed/25004729 (accessed 9 June 2019). [DOI] [PubMed] [Google Scholar]
- Rochmyaningsih D. (2018) Indonesian ‘vaccine fatwa’ sends measles immunization rates plummeting. Science. American Association for the Advancement of Science (AAAS). DOI: 10.1126/SCIENCE.AAV9864. [DOI] [Google Scholar]
- Rosenstock IM. (1974) The health belief model and preventive health behavior. Health Education Monographs 2(4): 354–386. [DOI] [PubMed] [Google Scholar]
- Rosseel Y, Jorgensen TD, Rockwood N, et al. (2021) Package ‘lavaan’: Latent variable analysis. Available at: https://cran.r-project.org/web/packages/lavaan/index.html (accessed 31 May 2021).
- Rutjens BT, Sutton RM, van der Lee R. (2018) Not all skepticism is equal: Exploring the ideological antecedents of science acceptance and rejection. Personality and Social Psychology Bulletin 44(3): 384–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutjens BT, van der Lee R. (2020) Spiritual skepticism? Heterogeneous science skepticism in the Netherlands. Public Understanding of Science 29(3): 335–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutjens BT, Zarzeczna N, van der Lee R. (2021) Science rejection in Greece: Spirituality predicts vaccine scepticism and low faith in science in a Greek sample. Public Understanding of Science 31(4):428–436. [DOI] [PubMed] [Google Scholar]
- Shelton RC, Snavely AC, De Jesus M, et al. (2013) HPV vaccine decision-making and acceptance: Does religion play a role? Journal of Religion and Health 52(4): 1120–1130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen L, Condit CM, Wright L. (2009) The psychometric property and validation of a fatalism scale. Psychology & Health 24(5): 597–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shimron Y. (2021) Black Protestants aren’t least likely to get a vaccine; white evangelicals are. Available at: https://religionnews.com/2021/03/05/black-protestants-arent-least-likely-to-get-a-vaccine-white-evangelicals-are/ (accessed 5 January 2022).
- Shurpin Y. (2015) What does Jewish law say about vaccination? Questions & Answers. Available at: https://www.chabad.org/library/article_cdo/aid/2870103/jewish/What-Does-Jewish-Law-Say-About-Vaccination.htm (accessed 9 June 2019).
- Silverman RD, May T. (2001) Private choice versus public health: Religion, morality, and childhood vaccination law. Margins (Baltimore, Md.) 1(2): 505–521. Available at: http://www.ncbi.nlm.nih.gov/pubmed/15977365 (accessed 9 June 2019). [PubMed] [Google Scholar]
- Smart N. (1996) Dimensions of the sacred: An anatomy of the world’s beliefs. University of California Press. Available at: https://www.ucpress.edu/book/9780520219601/dimensions-of-the-sacred (accessed 9 June 2019). [Google Scholar]
- Sporton RK, Francis S-A. (2001) Choosing not to immunize: Are parents making informed decisions? Family Practice 18(2): 181–188. [DOI] [PubMed] [Google Scholar]
- Sriram S, Ranganathan R. (2019) Why human papilloma virus vaccination coverage is low among adolescents in the US? A study of barriers for vaccination uptake. Journal of Family Medicine and Primary Care 8(3): 866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stecula DA, Kuru O, Albarracín D, et al. (2020) Policy views and negative beliefs about vaccines in the United States, 2019. American Journal of Public Health 110(10): 1561–1563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart K. (2020) The religious right’s hostility to science is crippling our coronavirus response. The New York Times. Available at: https://www.nytimes.com/2020/03/27/opinion/coronavirus-trump-evangelicals.html?action=click&module=Opinion&pgtype=Homepage (accessed 18 April 2020).
- Thomas TL, Strickland OL, DiClemente R, et al. (2012) Rural African American parents’ knowledge and decisions about human papillomavirus vaccination. Journal of Nursing Scholarship: An Official Publication of Sigma Theta Tau International Honor Society of Nursing 44(4): 358–367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Census Bureau (2019) Educational attainment in the United States: 2018. Available at: https://www.census.gov/data/tables/2018/demo/education-attainment/cps-detailed-tables.html (accessed 11 June 2019).
- Versteeg P, Roeland J. (2011) Contemporary spirituality and the making of religious experience. Fieldwork in Religion 6(2): 120–133. [Google Scholar]
- Williams JTB, O’Leary ST. (2019) Denver religious leaders’ vaccine attitudes, practices, and congregational experiences. Journal of Religion and Health 58(4): 1356–1367. [DOI] [PubMed] [Google Scholar]
- Williams JTB, Rice JD, O’Leary ST. (2021) Associations between religion, religiosity, and parental vaccine hesitancy. Vaccine: X 9: 100121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wombwell E, Fangman MT, Yoder AK, et al. (2015) Religious barriers to measles vaccination. Journal of Community Health 40(3): 597–604. [DOI] [PubMed] [Google Scholar]
- Yee V. (2020) In a pandemic, religion can be a balm and a risk. The New York Times. Available at: https://www.nytimes.com/2020/03/22/world/middleeast/coronavirus-religion.html?action=click&module=TopStories&pgtype=Homepage (accessed 18 April 2020).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This article is distributed under the terms of the Creative Commons Attribution 4.0 License (https://creativecommons.org/licenses/by/4.0/) which permits any use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access pages (https://us.sagepub.com/en-us/nam/open-access-at-sage).
sj-docx-2-hpq-10.1177_13591053221082770 for Religious affiliation and philosophical and moral beliefs about vaccines: A longitudinal study by Ozan Kuru, Man-pui Sally Chan, Hang Lu, Dominik Andrzej Stecula, Kathleen Hall Jamieson and Dolores Albarracín in Journal of Health Psychology
Supplemental material, sj-docx-8-hpq-10.1177_13591053221082770 for Religious affiliation and philosophical and moral beliefs about vaccines: A longitudinal study by Ozan Kuru, Man-pui Sally Chan, Hang Lu, Dominik Andrzej Stecula, Kathleen Hall Jamieson and Dolores Albarracín in Journal of Health Psychology
This article is distributed under the terms of the Creative Commons Attribution 4.0 License (https://creativecommons.org/licenses/by/4.0/) which permits any use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access pages (https://us.sagepub.com/en-us/nam/open-access-at-sage).
sj-jasp-3-hpq-10.1177_13591053221082770 for Religious affiliation and philosophical and moral beliefs about vaccines: A longitudinal study by Ozan Kuru, Man-pui Sally Chan, Hang Lu, Dominik Andrzej Stecula, Kathleen Hall Jamieson and Dolores Albarracín in Journal of Health Psychology
This article is distributed under the terms of the Creative Commons Attribution 4.0 License (https://creativecommons.org/licenses/by/4.0/) which permits any use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access pages (https://us.sagepub.com/en-us/nam/open-access-at-sage).
sj-R-6-hpq-10.1177_13591053221082770 for Religious affiliation and philosophical and moral beliefs about vaccines: A longitudinal study by Ozan Kuru, Man-pui Sally Chan, Hang Lu, Dominik Andrzej Stecula, Kathleen Hall Jamieson and Dolores Albarracín in Journal of Health Psychology
This article is distributed under the terms of the Creative Commons Attribution 4.0 License (https://creativecommons.org/licenses/by/4.0/) which permits any use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access pages (https://us.sagepub.com/en-us/nam/open-access-at-sage).
sj-sav-4-hpq-10.1177_13591053221082770 for Religious affiliation and philosophical and moral beliefs about vaccines: A longitudinal study by Ozan Kuru, Man-pui Sally Chan, Hang Lu, Dominik Andrzej Stecula, Kathleen Hall Jamieson and Dolores Albarracín in Journal of Health Psychology
This article is distributed under the terms of the Creative Commons Attribution 4.0 License (https://creativecommons.org/licenses/by/4.0/) which permits any use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access pages (https://us.sagepub.com/en-us/nam/open-access-at-sage).
sj-sav-7-hpq-10.1177_13591053221082770 for Religious affiliation and philosophical and moral beliefs about vaccines: A longitudinal study by Ozan Kuru, Man-pui Sally Chan, Hang Lu, Dominik Andrzej Stecula, Kathleen Hall Jamieson and Dolores Albarracín in Journal of Health Psychology
This article is distributed under the terms of the Creative Commons Attribution 4.0 License (https://creativecommons.org/licenses/by/4.0/) which permits any use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access pages (https://us.sagepub.com/en-us/nam/open-access-at-sage).
sj-sps-1-hpq-10.1177_13591053221082770 for Religious affiliation and philosophical and moral beliefs about vaccines: A longitudinal study by Ozan Kuru, Man-pui Sally Chan, Hang Lu, Dominik Andrzej Stecula, Kathleen Hall Jamieson and Dolores Albarracín in Journal of Health Psychology
This article is distributed under the terms of the Creative Commons Attribution 4.0 License (https://creativecommons.org/licenses/by/4.0/) which permits any use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access pages (https://us.sagepub.com/en-us/nam/open-access-at-sage).
sj-xlsx-5-hpq-10.1177_13591053221082770 for Religious affiliation and philosophical and moral beliefs about vaccines: A longitudinal study by Ozan Kuru, Man-pui Sally Chan, Hang Lu, Dominik Andrzej Stecula, Kathleen Hall Jamieson and Dolores Albarracín in Journal of Health Psychology